Abstract
People tested positive for BRCA1/2 face an increased risk of cancer; to help them cope with the genetic information received, support to BRCA1/2 families should be continued after testing. Nonetheless how such support should be provided has not been established yet. As a potentially valuable option is represented by support groups, the aim of this systematic review was to assess studies exploring the outcomes of support groups for BRCA1/2 carriers. This study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42021238416). Peer-reviewed papers published between January 1995 and February 2021 were searched for, using four databases. Among 1586 records identified, 34 papers were reviewed in full-text and eleven were included in the qualitative synthesis of the results. Three themes emerged as major focuses of support groups: risk management decisions, family dynamics and risk communication, and psychosocial functioning. Our findings show that support groups proved helpful in supporting women’s decision-making on risk-reducing options. Moreover, during those interventions, BRCA1/2 carriers had the opportunity to share thoughts and feelings, and felt that mutual support through interacting with other mutation carriers help them release the emotional pressure. However, no significant impact was reported in improving family communication. Overall, a high level of satisfaction and perceived helpfulness was reported for support group. The findings suggest that support groups represent a valuable tool for improving BRCA1/2 families care.
Subject terms: Quality of life, Genetic counselling
Introduction
People tested positive for BRCA1/2 face an increased risk of cancer: the estimated lifetime risk of developing breast cancer is 72% for BRCA1 and 69% for BRCA2 carriers, while the lifetime risk of developing ovarian cancer is 44% for BRCA1 and 17% for BRCA2 carriers [1]. Consequently, the decision to undergo genetic testing involves the ability to cope with such risks and is therefore very personal and complex [2]. Overall, higher levels of distress, anxiety and depression in BRCA carriers, compared with non-carriers, were reported, which also correlated with familial (having daughters or being unmarried) and individual (female gender, young age, prior cancer diagnosis, personality) features [3]. Distress in carriers failed to reduce over time, however, protective factors were identified, including having received adequate pre-test information and having direct communication exchanges in the family [3]. Beyond being recommended to undertake risk-reducing strategies, BRCA1/2 carriers are advised to share genetic information with relatives; actual disclosure depends on the degree and quality of the relationships, and the proportion of BRCA1/2 carriers communicating test results to their offspring ranged from 49% to 75% [4, 5]. Den Heijer and colleagues [6] and Patenaude and colleagues [7] showed that one-third of the daughters of BRCA1/2 carriers reported high cancer-related distress levels, which were not significantly different from distress levels of women with known BRCA1/2 variants. One of the scopes of genetic counselling is providing support to individuals and families both to promote informed choices and to help coping with the carrier status [8]. However, in recent studies on presymptomatic testing for hereditary cancer syndromes in young adults, we found that awareness about the supportive and educational role of genetic services is limited among families, and that, among young adults belonging to hereditary cancer families, only those who had already decided to undergo testing were shown to come for genetic counselling, despite part of them did not really understand the implications of genetic test but just complied with parental pressure [9–11]. This evidence highlights the need for initiatives, alternative or additional with respect to the formal genetic counselling process, favouring awareness about BRCA testing meaning and implications among relatives of BRCA carriers.
Moreover, the process of genetic counselling is limited in time, whereas needs and family dynamics may change over time. Therefore, it is clear that support to BRCA1/2 families should be continued after testing, in order to help them cope with the genetic information received, which has been reported as a need by this specific population [2, 12]. A recent systematic review demonstrated that there are limited high quality interventions aimed at improving psychological adjustment in individuals with a BRCA1/2 carriers [13]. Metcalfe and colleagues [12] found that two thirds of BRCA1/2 carriers included in their study felt the need for psychosocial support, and half of them would join a support group [12]. Generally, support groups are interventions based on an educational, psychological, or combined approach aimed at providing education, mutual/peer support and opportunities to express feelings and concerns [14], which have proven effective in establishing social networks by building an identity based on social ties with others in several settings [15]. Therefore, support groups appear as a suitable approach to extend the effects of genetic counselling for BRCA carriers over time, thus enhancing awareness, helping reduce distress, anxiety and depression, and favouring communication with relatives and decision-making. For this reason, we sought to investigate whether support groups had proven effective in meeting the needs of this population.
Objective
The purpose of this systematic review was to systematically identify and analyse studies reporting on support groups for people tested positive for BRCA1/2 and their relatives.
This study sought to answer the following questions: “Are support groups helpful for people tested positive for BRCA1/2 and their relatives? What are the outcomes of these interventions on this specific population?”
Materials and methods
The study was designed according to the Recommendation of “Preferred Reporting Items for Systematic Reviews and MetaAnalysis (PRISMA)” and was registered in the “International Prospective Register of Systematic Review” (PROSPERO) in 2021 (CRD42021238416; Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021238416); the protocol is available upon request.
Search strategy
Four databases used for indexing medical and psychosocial research (PsychoInfo, Pubmed, SocIndex, Social Science) were searched for papers published between January 1995 and February 2021. We chose to start at 1995 because BRCA1 and BRCA2 genes were discovered in the mid-1990s, therefore BRCA1/2 testing was not available before. The literature search employed variations and Boolean connectors of the key terms. Databases were searched for terms: ((BRCA*) AND ((psychoeducat* intervent*) OR (psychosocial* support*)) AND ((support group*) OR (focus group*) OR (follow-up))). The reference lists of all included studies were hand-searched for additional relevant reports or key terms. Targeted internet searching using Google Scholar was also examined for any additional studies of interest. Resultant articles were screened as title and abstracts. After the exclusion of those which did not meet our inclusion criteria, the full texts of the remaining articles were assessed for eligibility.
Eligibility criteria
Papers did fulfil criteria for inclusion in this systematic review if they were:
published in English or Italian;
published in peer-reviewed journals since 1995 and reporting original research (using any methods);
where the study sample explicitly included BRCA1/2 carriers and/or their relatives;
where the study explicitly included support groups.
Papers were excluded from the review if they were:
abstract;
educational or opinion papers;
books.
Studies selection
Relevant articles were screened as title and abstracts. After the exclusion of those which did not meet our inclusion criteria, the full texts of the remaining articles were assessed for eligibility by two reviewers independently (B.B. and L.G.) and the final decision for inclusion will be reached by consensus between all the authors. Data extraction form was prepared. The data extraction content includes: aim, authors, year, country, study design, sample size, scales used (if any), findings, analyses, statistical methods, effect size, findings and quality of the studies.
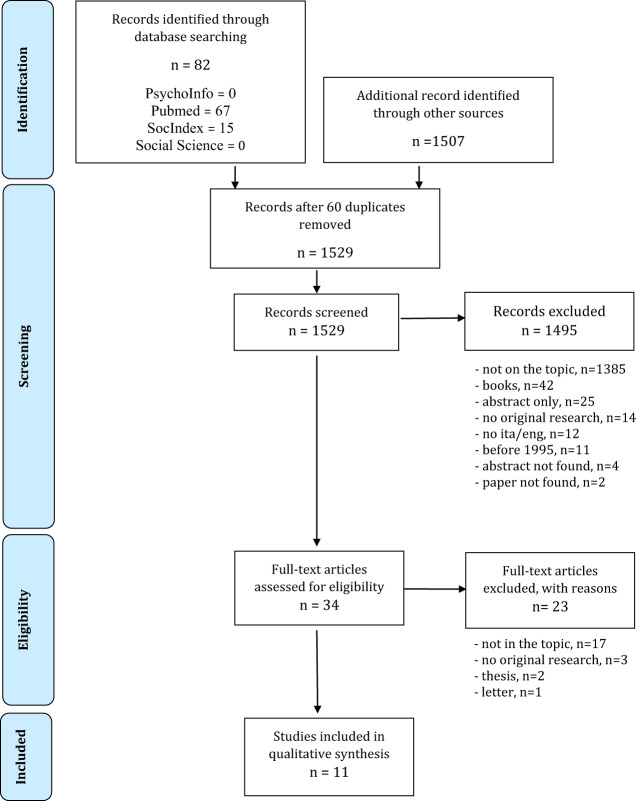
The results of study selection process were summarised in a PRISMA flowchart [16].
Search outcome
The results of study selection process is summarised in the “Preferred Reporting Items for Systematic Review” (PRISMA) flowchart [16] showing the consecutive methodological steps of this systematic review (Fig. 1). The search of four databases initially produced 82 potential papers. With the use of Google Scholar, 1507 records were found. On the total of 1589, 60 were duplicates, leaving 1529 for examination. Following review of the title and abstract, 34 papers were read in detail by the authors. Eleven papers were included in the review. The main characteristics of the included studies are detailed in Table 1.
Fig. 1. PRISMA flowchart of study selection.
This PRISMA flowchart demonstrates the process of identifying and screening relevant studies. The screening process identified eleven studies from an initial pool of 1589 as being relevant to the current review.
Table 1.
Main characteristics of included studies.
| Author | Country | Aim | Study design | Results | Kmet et al. score (2004) |
|---|---|---|---|---|---|
| Bober et al. (2015) | United States of America | To promote interventions of sexual health education with mindfulness-based cognitive therapy for women with BRCA1/2 mutations who previously underwent RRSO. | A cross-sectional study | All the participants reported to have acquired new skills, women were satisfied, felt less isolated and put into practice at least one of the new strategies learned. | 95% |
| Clarke et al. (2008) | Canada | To examine the experiences of BRCA1/2 carriers in communicating genetic information to their offspring. | A qualitative study using thematic analysis | Complexity around the disclosure of genetic information emerged, the ethical dilemmas, emotional consequence about telling or not telling where deeply analysed. | 80% |
| Esplen et al. (2004) | Canada | To evaluate whether a supportive-expressive group therapy for women with a BRCA1/2 mutation can help them to cope with their status. | Longitudinal prospective study | Significant improvements were observed in cancer worries, anxiety, depression and in the decision-making process, four women at post-intervention measurement had undergone prophylactic oophorectomy and six prophylactic mastectomy. | 100% |
| Kwiatkowski et al. (2013) | France | To help young BRCA mutation carriers cope with difficult issues. | Prospective psycho educational cohort study | Several themes emerged concerning prophylactic surgery, fear about partners’ reaction to surgery, childbearing and cancer. An increase in quality of life and self-esteem during the follow-up year was reported. | 90% |
| Landsbergen et al. (2010a) | The Netherlands | To determine risk management preferences (between breast cancer surveillance and prophylactic mastectomy) and the effect of an educational-support group. | Cross-sectional study | Women with a preference for mastectomy who participated to a support group decided to undergo surgery in higher proportion than those who did not attend (89% versus 63% P = 0.04). Age between 30 and 50 was a predictor for mastectomy. Participants in educational support groups were less likely to opt for surveillance than non-participants. | 94,4% |
| Landsbergen et al. (2010b) | The Netherlands | To evaluate educational-support groups for women with a BRCA mutation. | Cross-sectional study | Participants declared that educational-support group supported their decision-making process regarding surveillance or prophylactic surgery. Conversely, intrafamilial communication decreased after group participation. | 85% |
| Listøl et al. (2017) | Norway | To characterise women attending a group-basedassess symptoms of anxiety and depression among the participants, and their changes after the course session. | Longitudinal prospective study | Anxiety levels decreased significantly during follow-up, satisfaction levels were high among participants, the majority of whom reported to have learned something new during the course. | 100% |
| Mendes et al. (2010) | Portugal | To examine a multi-family group intervention for women tested positive for a BRCA mutation and their relatives. | Qualitative study | Participants reported that one of the benefits of the multi-family discussion format was the sharing personal experiences, which prevented isolation and sense of inadequacy. Moreover, the integration of medical information was felt as very important. | 80% |
| McKinnon et al. (2007) | United States of America | To give information and support to the families with hereditary cancer syndromes. | Longitudinal prospective | The retreat helped in the decision-making process regarding genetic testing, and family communication. Lifestyle changes were observed, in particular increased cancer prevention and screening. | 94,4% |
| Myklebust et al. (2015) | United States of America | To explore and describe the experiences of female Brca1/2 carriers with the increased risk of cancer and their experience with educational support groups (ESG). | A qualitative study using thematic analysis. | Three main themes were identified: expectations and experience with ESG reported as positive, experience of loneliness and isolation, and the feelings of living with ‘something else’. Participants declared the need of clear and unified information. | 85% |
| Speice et al. (2002) | United States of America | To provide information and support to women with a BRCA mutation. | A qualitative study using thematic analysis. | Several themes emerged: distress about the transmission to children, dilemma about disclosure, different coping styles and decision making, conflict about testing and the experience of feeling coerced. | 45%a |
aThe study describes a family-oriented psychoeducation group accurately analysing intra-familial issues concerning genetic testing. Despite the score, also dependent on the standards of papers publication period, it has been included because of the strong contribution on the psychological aspects and on intrafamilial communication.
Quality appraisal
All articles considered for inclusion in the review were subjected to independent analysis by B.B. and L.G. using standard quality assessment criteria for evaluating research papers from a variety of fields [17]. This method of evaluation allows the analysis of both quantitative and qualitative original research. Specific aspects of the paper relating to methodology and reporting of results are assessed and assigned 0 point (not addressed), 1 point (partially addressed) or 2 points (completely addressed). The total scores were then reported in percentage using the Kmet and colleagues’ methods of scoring. Any disagreement about scoring of papers was discussed between the authors until consensus was reached. Kmet and colleagues do not enforce a minimum score for inclusion in a review, although they suggest 60% as a reasonable cut-off point. However, we decided to include in this systematic review one paper that scored 45%, since it provides a relevant contribution on psychological aspects and intra-familial communication, and considering that the standards of papers at the time of publication differed from those currently adopted, and included in the quality appraisal approach.
Results
Characteristics of included studies
Eleven studies were selected and reviewed: four qualitative [18–21] and seven quantitative studies [22–28], published between 1995 and February 2021 and focusing on support groups addressed to BRCA1/2 carriers and their relatives. Three studies had been conducted in USA [18, 23, 25], six in Europe [20, 21, 24, 26–28], one in Canada [19], while one was multicentric (USA, Canada and Australia) [22]. Of the 11 studies selected, three were longitudinal studies [22, 23, 27], four cross-sectional studies [24–26, 28], and four qualitative studies based on focus groups [18–21]. Six studies were mainly focussed on education [20, 23–25, 27, 28], while five involved psychological interventions [18, 19, 21, 22, 26]. Tools for evaluating the outcomes of support groups included self-administered questionnaires [20–28] and semi-structured interviews [18, 19, 21, 25]. Features and findings of the included studies are detailed in Tables 1 and 2.
Table 2.
Methods used in the included studies.
| Study | Type of Intervention | Duration | Measures |
|---|---|---|---|
| Bober et al. (2015) | Educational session | Half-day session | Baseline questionnaire (FSFI, BSI-18, Sexual self-efficacy scale, Sexual knowledge)a plus two follow-up telephone counselling sessions. |
| Clarke et al. (2008) | Multi-site group therapy | Twelve sessions in six months | Semi-structured interviews. |
| Esplen et al. (2004) | Supportive-expressive group therapy | Twelve sessions in six months (eight weekly sessions and four booster monthly sessions) | Demographic and medical variables were collected. Before and after interventions women completed questionnaires (IES, BSI, TRIG,QLI and ad hoc questionnaires)a. |
| Kwiatkowski et al. (2019) | Psychoeducational intervention | A weekend group workshop | Questionnaire (Rosenberg’s Self-Esteem scale, STAI, Levenson’s IPC, HHI, WHOQOL)a at inclusion, at the conclusion, then 6 and 12 months after the workshop. |
| Landsbergen et al. (2010a) | Educational support group | Eight sessions (four to six weeks interval) | Sociodemographic, medical, family cancer and genetic test related characteristics were retrieved from medical records. Participants were interviewed about breast cancer risk management preferences. After two years the status was checked by medical file. |
| Landsbergen et al. (2010b) | Educational-Support group | Eight sessions (every four-six weeks) | Data were collected through medical records and questionnaires (POMS, VAS, ODHCF) administered one week before (T1) and within two weeks after the last group (T2). |
| Listøl et al. (2017) | Group-based patient education course | A seven hours session | Questionnaires (BGCSES, HaDS, TMSI)a administered two weeks before and two weeks after the course. |
| McKinnon et al. (2007) | Educational sessions and group discussion | One day retreat | Questionnaire (IES)a administered before and 6 months after the retreat |
| Mendes et al. (2010) | Multi-family discussion group | Four 90-min sessions | Demographic and psychosocial data were collected. Analysis of records of the sessions. The sessions were evaluated through a focus group semi-structured interview. |
| Myklebust et al. (2016) | Educational support groups | Two educational support groups | Focus group interviews were performed immediately prior to and following educational support groups. |
| Speice et al. (2002) | Family-oriented psychoeducation group | Six sessions | Baseline questionnaire to gain information and level of interest in attending the group. |
BSI-18 Brief symptom inventory-18, IES Impact of event scale, BSI Brief Symptom inventory, TRIG Texas Revised Inventory of Grief, QLI Quality of Life Index, STAI State Trait Anxiety, HHI Hearth Hope Inventory, WHOQOL World Health Organization questionnaires, POMS Profile of Mood States, VAS Visual Analogue Scale, ODHCF Openness to Discuss Hereditary Cancer in the Family Sacale, BGCSES Bergen genetic counselling self-efficacy scale, HADS Hospital anxiety and depression scale, TMSI Threatening medical situation inventory.
aFSFI female sexual function index.
Findings
Three majors’ themes emerged from the analysis of the studies: risk management decision, family dynamics and risk communication, and psychosocial functioning.
Risk management decision
Groups proved helpful to women’s decision-making on prophylactic surgery [22–24, 26] or surveillance [23, 24]. Increased consciousness of choices regarding risk management and help in decision-making process were reported as results of participating in support groups [20–24, 28]. For example, a woman said that the support group helped her “To decide to do a double mastectomy versus just take off the one side recommended. Thank God, because prophylactic side had invasive cancer” (McKinnon et al., 2007; p.440). In some cases prior preference of breast cancer surveillance or prophylactic mastectomy was reinforced [24, 28]; in particular, those who attended a support group were more likely to proceed with their choice within two years (89%), in comparison to those not attending (63%; p = 0.04) [24].
In general, expectations and decisions about surgery were reported as a commonly discussed theme, particularly among young women (aged 23–30 years): many asked for real examples of breast reconstruction and many raised issues about emotional implications and possible changes in the couple’s relationship. However, a young woman stated “If this induce a separation, it’s because there was no love before; the surgery is just a trigger” (Kwiatkowski et al., 2019; p 7). A strong desire of a clear and consistent information about risk management after genetic testing was reported, since having received different information regarding risk-reducing surgery from various health professionals made participants feel frustrated. A woman declared that she was participating in the support group because of the unclear information received by her surgeon “I didn’t get the information that I needed. That’s why it is interesting to talk to others who have had the surgery, I think, in order to know”(Myklebust et al., 2016; p.1201). Participants in those studies generally reported high levels of satisfaction [20, 22, 25, 27].
Family dynamics and risk communication
Based on participants’ reports, support groups allowed for the creation of an atmosphere which encouraged sharing of personal and family experience [18, 19, 21, 23, 24, 26], and decreased the feelings of isolation [25]. However, a benefit on intra-familial communication was not clearly demonstrated. Indeed, in one study, family communication was shown to be significantly reduced after the support group in comparison to the baseline (p = 0.02) [24]. In addition, attending a support group did not modify the attitude regarding disclosure to offspring [19]; the dilemma on if and when to disclose the genetic information to offspring and the related distress, as well as the perceived need of providing emotional support and reframing the genetic information to the offspring, emerged in the studies [18, 19]. People tested positive for BRCA1/2 enjoyed the opportunity to meet younger women at risk of cancer to better understand their daughters’ perspectives [22]. Some expressed worry about future health decisions of daughters, if they would test positive, as well as about problems and discrimination they might face, including finding a partner, and securing adequate insurance [18, 19]. Some participants felt the need to explore the will of their offspring in order to respect their choice, while some others delayed disclosure to children, which, however, made them feeling dishonest towards them. Attending support groups brought out other feelings and experiences: for example a woman reported she felt coerced to be tested by a family member, while another woman felt guilty when she realised that some of her family members could have felt coerced by her [18]. Changes in family relationship, both positive and negative were also reported. Among positive changes, a participant reported that: “Having my parents attend the retreat and understand more deeply what my sister and I face has helped me feel closer to my parents” (McKinnon et al., 2007; p. 439); another one said that attending the support group with her daughter helped her to feel more educated and freer to talk. Conversely, a participant reported that her father refused to talk about BRCA status, despite her desire to discuss the situation in order to make him understand [23].
Psychosocial functioning
Reaction at communication of test result
Attending a support group was an opportunity to share reactions and feelings experienced during the communication of test results in the clinic [18, 26]. Several individuals reported they felt unprepared to the intensity of the reactions to a positive test disclosure; feelings of discordance among family members and uncertainty were also reported [18]. Kwiatkowski and colleagues [26] reported that all their participants had reacted crying to the positive test disclosure and that they recalled that moment as a trauma, with a distress deeper than expected.
Anxiety and depression
Support groups were described by participants as having effectively provided emotional support. Indeed, participation seemed to reduce distress, depression and anxiety [22, 25–27], while helping to raise hope, self-esteem, sense of personal growth and quality of life [22, 25, 26]. People tested positive for BRCA1/2, who reported to have experienced feelings of anxiety and depression, also admitted they went to a therapist to discuss their family or personal cancer history [23].
Guilt toward children
Guilt about BRCA variant transmission was widely described during support groups [18, 19, 22], especially by mothers. Moreover, the fear of passing the variant in future pregnancies, anxiety for children adulthood and the consequent desire to know their genetic status were discussed by participants [18].
Couple relationship
People tested positive for BRCA1/2 who attended support groups were highly satisfied with the group sessions and reported an improvement in sexual function including desire, arousal and satisfaction [25]. Couple relationships were brought to discussion by young women, some of whom reported to be afraid of possible changes in the solidity of the couple even related to body image modification after prophylactic mastectomy. For example, a young woman said: “To see a breast without a nipple is difficult for a woman: what must be for a man?” (Kwiatkowski et al., 2019; p.7). Moreover, support groups also proved helpful to discuss maternity desire, whether pregnancy was a risk factor for cancer, the right timing of mastectomy and the implications on breast feeding, however no one mentioned an interest in prenatal or preimplantation diagnosis [26].
Discussion
The present systematic review was conducted with the aim of assessing the outcomes of support groups for people tested positive for BRCA1/2 and their relatives. Following the PRISMA guidelines and considering the inclusion and exclusion criteria, eleven studies were selected for the analysis.
The results of the analysis show that support groups proved helpful to improve accurate information and knowledge and to facilitate women’s decision-making both on prophylactic surgery and surveillance [29–32]. On the other hand, some women had the opportunity to share their experiences reporting that surgical risk-reduction decisions had been forced upon them from either a family member or a physician [33, 34], or that they had cancelled their scheduled risk-reducing surgery because they had received limited, conflicting and confusing information [20]. According to Antonovsky, if clients can recognise available resources, the future may be more manageable [35]. In this view, support groups appeared able to satisfy the needs of people tested positive for BRCA1/2 in terms of providing relevant information regarding cancer risk assessment and management. These benefits may extend also to other family members [21, 23].
Several studies included in our systematic review explicitly or implicitly highlighted both barriers and facilitators of intra-familial communication. Intra-familial communication is a highly complex process, especially when an inherited genetic condition is involved. Members of the family can start to feel isolated from each other [36], thus it is understandable that parents face the dilemma of when, how and what to tell their children about it [9–11, 37, 38]. The impact of sharing genetic test results was felt as a stressor among BRCA1/2 carriers [39], and low rates of disclosure of BRCA1/2 genetic test results to relatives were also reported [40]. In a recent systematic review, we found that communication generally occurred due to the parents’ initiative and in a casual way [9]; moreover, it was showed that the result itself influenced the disclosure because of complex personal, cultural and social factors [41, 42]. An appropriate communication of genetic risk information by parents to their children is highly desirable, since it has been shown to have long-term consequences in terms of informed reproductive decision making and better family cohesion [43]. To achieve this, health professionals may have a role in both supporting parents and young people, but their involvement in parents’ decisions to communicate genetic risk to young family members was found to be limited in previous studies [10, 11, 44–46]. Although this may be partly due to the parents’ wish to undertake this task alone, it is reported that some parents desired health professionals to be available in a supporting role, but found that this support was limited [43, 47]. Although support groups could then be expected to help intra-familial communication, the studies here analysed failed to show a positive effect.
Although it had been hypothesised that only a minority of people tested positive for BRCA genes may desire such a service [2], our findings support a high level of interest and satisfaction among participants in support groups. According to Antonovsky, social support helps increase a person’s health and well-being [35], which has been confirmed by evidence [48]; increased resilience was also shown in people receiving high social support [49]; while people with low social support tend to present with more sub-clinical signs of depression and anxiety [50]. Consistently, during the interventions here reviewed, people tested positive for BRCA1/2 appreciated to have the opportunity to share thoughts, feelings, and reactions and felt that the emotional pressure could be released. Through the reciprocal process of listening and narrating their medical family history, people have been helped to share emotions, to create a sense of empowerment concerning living with a genetic condition, to remove the inadequacy of some feelings and thoughts and to feel less alone [6, 51, 52].
This systematic review has some potential limitations that should not be overlooked. A potential limitation is that the papers analysed were conducted in a limited number of countries, thus the findings may not generalise to other countries with different sociocultural backgrounds. Secondly, the studies we reviewed used different types of intervention, for instance psychological or information-based support, and different settings and tools of assessment, not allowing data pooling and direct comparisons. Replication studies in other contexts with homogeneous setting and study design would allow to draw firmer conclusions on the outcomes of group interventions in this population. Anyway, the qualitative synthesis of the data included eleven studies that are believed to represent the only existing studies assessing the effectiveness of support groups for people tested positive for BRCA1/2 and their relatives. To the authors’ knowledge, this is the only study presenting a systematic review analysing these topics to date.
Conclusion
Overall, support groups for people tested positive for BRCA1/2 and their relatives have been well-received by participants and have been shown to help women’s decision-making and to improve knowledge. None of the studies reported negative consequences of support groups. Results also confirm the perceived need of psychosocial and family-oriented interventions, but in standard care it is difficult to offer individual follow-up sessions to all BRCA carriers and their relatives. In order to meet that need, regularly held support groups could be offered/integrated in the genetic healthcare to overcome the limitations of a time-restricted genetic counselling process. The genetic clinic staff should ideally arrange the meetings and/or be involved in them, including medical geneticists, genetic nurses/counsellors, and psychologists. They should encourage discussing perception of cancer risk, worry about cancer, communication with immediate family members, attitudes toward surveillance and other prevention options, satisfaction with the decision to undergo genetic testing and with clinical services, and needs for additional support. In addition, the participating BRCA carriers and their relatives would provide peer support for each other, and the genetics professionals could be available to answer any questions asked, thus prolonging and reinforcing the supportive and educational role of genetic services. Concluding, those interventions may provide needed support to people tested positive for BRCA1/2 and their relatives.
Acknowledgements
BB was supported by a grant awarded by Italian Ministry of Health (RF-2011-02352088).
Author contributions
All the authors conceived the study. LG and DT designed the analytical plan and the bias assessment approach. BB and LG performed the literature search and draughted the manuscript. LG supervised the study. DT revised the manuscript. All authors approved the final version.
Data availability
Data on subsequent steps of literature search and selection are available upon request.
Competing interests
The authors declare no competing interests.
Ethical approval
Approval by an Ethical Board was not required as this is a systematic review of published literature. However, it was registered in the “International Prospective Register of Systematic Review” (PROSPERO) in 2021 (CRD42021238416; Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=%20CRD42021238416).
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317:2402–16. doi: 10.1001/jama.2017.7112. [DOI] [PubMed] [Google Scholar]
- 2.Di Prospero LS, Seminsky M, Honeyford J, Doan B, Franssen E, Meschino W, et al. Psychosocial issues following a positive result of genetic testing for BRCA1 and BRCA2 mutations: findings from a focus group and a needs-assessment survey. CMAJ. 2001;164:1005–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Lombardi L, Bramanti SM, Babore A, Stuppia L, Trumello C, Antonucci I, et al. Psychological aspects, risk and protective factors related to BRCA genetic testing: a review of the literature. Support Care Cancer. 2019;27:3647–56. doi: 10.1007/s00520-019-04918-7. [DOI] [PubMed] [Google Scholar]
- 4.Claes E, Evers-Kiebooms G, Boogaerts A, Decruyenaere M, Denayer L, Legius E. Communication with close and distant relatives in the context of genetic testing for hereditary breast and ovarian cancer in cancer patients. Am J Med Genet. 2003;116A:11–9. doi: 10.1002/ajmg.a.10868. [DOI] [PubMed] [Google Scholar]
- 5.Di Pietro ML, Zaçe D, Orfino A, Di Raimo FR, Poscia A, de Matteis E, et al. Intrafamilial communication of hereditary breast and ovarian cancer genetic information in Italian women: towards a personalised approach. Eur J Hum Genet. 2020;29:250–61. [DOI] [PMC free article] [PubMed]
- 6.den Heijer M, Seynaeve C, Vanheusden K, Duivenvoorden HJ, Bartels CCM, Menke-Pluymers MBE, et al. Psychological distress in women at risk for hereditary breast cancer: the role of family communication and perceived social support. Psychooncology. 2011;20:1317–23. doi: 10.1002/pon.1850. [DOI] [PubMed] [Google Scholar]
- 7.Patenaude AF, Tung N, Ryan PD, Ellisen LW, Hewitt L, Schneider KA, et al. Young adult daughters of BRCA1/2 positive mothers: what do they know about hereditary cancer and how much do they worry? Psychooncology. 2013;22:2024–31.. doi: 10.1002/pon.3257. [DOI] [PubMed] [Google Scholar]
- 8.Resta R, Biesecker BB, Bennett RL, Blum S, Estabrooks Hahn S, Strecker MN, et al. A new definition of genetic counseling: National Society of Genetic Counselors’ Task Force report. J Genet Couns. 2006;15:77–83. doi: 10.1007/s10897-005-9014-3. [DOI] [PubMed] [Google Scholar]
- 9.Godino L, Turchetti D, Jackson L, Hennessy C, Skirton H. Impact of presymptomatic genetic testing on young adults: a systematic review. Eur J Hum Genet. 2016;24:496–503. doi: 10.1038/ejhg.2015.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godino L, Jackson L, Turchetti D, Hennessy C, Skirton H. Decision making and experiences of young adults undergoing presymptomatic genetic testing for familial cancer: a longitudinal grounded theory study. Eur J Hum Genet. 2018;26:44–53. doi: 10.1038/s41431-017-0030-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godino L, Turchetti D, Jackson L, Hennessy C, Skirton H. Presymptomatic genetic testing for hereditary cancer in young adults: a survey of young adults and parents. Eur J Hum Genet. 2019;27:291–9. doi: 10.1038/s41431-018-0262-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metcalfe KA, Liede A, Hoodfar E, Scott A, Foulkes WD, Narod SA. An evaluation of needs of female BRCA1 and BRCA2 carriers undergoing genetic counselling. J Med Genet. 2000;37:866–74. doi: 10.1136/jmg.37.11.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warner NZ, Matthews S, Groarke A, McSharry J. A systematic review of psycho‐social interventions for individuals with a BRCA1/2 pathogenic variant. J Genet Couns. 2021;00:jgc4.1436. doi: 10.1002/jgc4.1436. [DOI] [PubMed] [Google Scholar]
- 14.Schmall V. What makes a support group good? It doesn’t just happen. Generations. 1984;9:64–7. [Google Scholar]
- 15.Mason E, Clare L, Pistrang N. Processes and experiences of mutual support in professionally-led support groups for people with early-stage dementia. Dementia. 2016;4:87–112.
- 16.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev Esp Nutr Hum Diet. 2016;20:148–60. doi: 10.14306/renhyd.20.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kmet LM, Lee RC, Cook L. AHFMR Alberta Heritage Foundation for Medical Research. Standard quality assessment criteria for evaluating primary research papers from avariety of fields. HTA Initiat. 2004;13:1–28. [Google Scholar]
- 18.Speice J, McDaniel SH, Rowley PT, Loader S. Family issues in a psychoeducation group for women with a BRCA mutation. Clin Genet. 2002;62:121–7. [DOI] [PubMed]
- 19.Clarke S, Butler K, Esplen MJ. The phases of disclosing BRCA1/2 genetic information to offspring. Psychooncology. 2008;17:797–803. doi: 10.1002/pon.1344. [DOI] [PubMed] [Google Scholar]
- 20.Myklebust M, Gjengedal E, Strømsvik N. Experience of Norwegian female BRCA1 and BRCA2 mutation-carrying participants in educational support groups: a qualitative study. J Genet Couns. 2016;25:1198–206. doi: 10.1007/s10897-016-9954-9. [DOI] [PubMed] [Google Scholar]
- 21.Mendes Á, Chiquelho R, Santos TA, Sousa L. Family matters: examining a multi-family group intervention for women with BRCA mutations in the scope of genetic counselling. J Community Genet. 2010;1:161–8. doi: 10.1007/s12687-010-0022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Esplen MJ, Hunter J, Leszcz M, Warner E, Narod S, Metcalfe K, et al. A multicenter study of supportive-expressive group therapy for women with BRCA1/BRCA2 mutations. Cancer. 2004;101:2327–40. doi: 10.1002/cncr.20661. [DOI] [PubMed] [Google Scholar]
- 23.McKinnon W, Naud S, Ashikaga T, Colletti R, Wood M. Results of an intervention for individuals and families with BRCA mutations: a model for providing medical updates and psychosocial support following genetic testing. J Genet Couns. 2007;16:433–56. doi: 10.1007/s10897-006-9078-8. [DOI] [PubMed] [Google Scholar]
- 24.Landsbergen KM, Brunner EG, Manders P, Hoogerbrugge N, Prins JB. Educational-support groups for BRCA mutation carriers satisfy need for information but do not affect emotional distress. Genet Couns. 2010b;21:423–37. [PubMed]
- 25.Bober SL, Recklitis CJ, Bakan J, Garber JE, Patenaude AF. Addressing sexual dysfunction after risk-reducing Salpingo-oophorectomy: effects of a brief, psychosexual intervention. J Sex Med. 2015;12:189–97. doi: 10.1111/jsm.12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kwiatkowski F, Gay-Bellile M, Dessenne P, Laquet C, Boussion V, Béguinot M, et al. BRACAVENIR: An observational study of expectations and coping in young women with high hereditary risk of breast and ovarian cancer. Hered Cancer Clin Pract. 2019;17:7. [DOI] [PMC free article] [PubMed]
- 27.Listøl W, Høberg-Vetti H, Eide GE, Bjorvatn C Anxiety and depression symptoms among women attending group-based patient education courses for hereditary breast and ovarian cancer. Hered Cancer Clin Pract. 2017;15:2. [DOI] [PMC free article] [PubMed]
- 28.Landsbergen KM, Prins JB, Kamm YJL, Brunner HG, Hoogerbrugge N. Female BRCA mutation carriers with a preference for prophylactic mastectomy are more likely to participate an educational-support group and to proceed with the preferred intervention within 2 years. Fam Cancer. 2010a;9:213–20. [DOI] [PubMed]
- 29.MacDonald DJ, Sarna L, Weitzel JN, Ferrell B. Women’s perceptions of the personal and family impact of genetic cancer risk assessment: focus group findings. J Genet Couns. 2010;19:148–60. doi: 10.1007/s10897-009-9267-3. [DOI] [PubMed] [Google Scholar]
- 30.Visser A, Prins JB, Hoogerbrugge N, Van Laarhoven HWM. Group medical visits in the follow-up of women with a BRCA mutation: design of a randomized controlled trial. BMC Womens Health. 2011;11:39. [DOI] [PMC free article] [PubMed]
- 31.Segerer R, Peschel C, Kämmerer U, Häussler S, Wöckel A, Segerer S. Factors impacting on decision-making towards prophylactic surgeries in BRCA mutation carriers and women with familial predisposition. Breast Care (Basel). 2020;15:253–9. [DOI] [PMC free article] [PubMed]
- 32.Alonzo MD’, Piva E, Pecchio S, Liberale V, Modaffari P, Ponzone R, et al. Satisfaction and impact on quality of life of clinical and instrumental surveillance and prophylactic surgery in BRCA-mutation carriers. Clin Breast Cancer. 2018;18:e1361–6 [DOI] [PubMed]
- 33.Lodder LN, Frets PG, Trijsburg RW, Meijers-Heijboer EJ, Klijn JGM, Seynaeve C, et al. One year follow-up of women opting for presymptomatic testing for BRCA1 and BRCA2: Emotional impact of the test outcome and decisions on risk management (Surveillance or prophylactic surgery) Breast Cancer Res Treat. 2002;73:97–112. doi: 10.1023/A:1015269620265. [DOI] [PubMed] [Google Scholar]
- 34.Patenaude AF, Orozco S, Li X, Kaelin CM, Gadd M, Matory Y, et al. Support needs and acceptability of psychological and peer consultation: Attitudes of 108 women who had undergone or were considering prophylactic mastectomy. Psychooncology. 2008;17:831–43. doi: 10.1002/pon.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Antonovsky A. Unraveling the mystery of health: how people manage stress and stay well. San Francisco: CA: Jossey-Bass; 1987.
- 36.Kenen R, Ardern-Jones A, Eeles R. “Social separation” among women under 40 years of age diagnosed with breast cancer and carrying a BRCA1 or BRCA2 mutation. J Genet Couns. 2006;15:149–62. doi: 10.1007/s10897-005-9015-2. [DOI] [PubMed] [Google Scholar]
- 37.Sobel SK, Cowan DB. Impact of genetic testing for Huntington disease on the family system. Am J Med Genet. 2000;90:49–59. doi: 10.1002/(SICI)1096-8628(20000103)90:1<49::AID-AJMG10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 38.Sobel S, Cowan CB. Ambiguous loss and disenfranchised grief: the impact of DNA predictive testing on the family as a system. Fam Process. 2003;42:47–57. doi: 10.1111/j.1545-5300.2003.00047.x. [DOI] [PubMed] [Google Scholar]
- 39.Wagner Costalas J, Itzen M, Malick J, Babb JS, Bove B, Godwin AK, et al. Communication of BRCA1 and BRCA2 results to at-risk relatives: a cancer risk assessment program’s experience. Am J Med Genet C Semin Med Genet. 2003;119C:11–8. doi: 10.1002/ajmg.c.10003. [DOI] [PubMed] [Google Scholar]
- 40.Cheung EL, Olson AD, Yu TM, Han PZ, Beattie MS. Communication of BRCA results and family testing in 1,103 high-risk women. Cancer Epidemiol Biomark Prev. 2010;19:2211–9. doi: 10.1158/1055-9965.EPI-10-0325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Forrest K, Simpson SA, Wilson BJ, van Teijlingen ER, McKee L, Haites N, et al. To tell or not to tell: barriers and facilitators in family communication about genetic risk. Clin Genet. 2003;64:317–26. doi: 10.1034/j.1399-0004.2003.00142.x. [DOI] [PubMed] [Google Scholar]
- 42.Lafrenière D, Bouchard K, Godard B, Simard J, Dorval M. Family communication following BRCA1/2 genetic testing: A close look at the process. J Genet Couns. 2013;22:323–35. doi: 10.1007/s10897-012-9559-x. [DOI] [PubMed] [Google Scholar]
- 43.Metcalfe A, Coad J, Plumridge GM, Gill P, Farndon P. Family communication between children and their parents about inherited genetic conditions: a meta-synthesis of the research. Eur J Hum Genet. 2008;16:1193–200. doi: 10.1038/ejhg.2008.84. [DOI] [PubMed] [Google Scholar]
- 44.Bradbury AR, Dignam JJ, Ibe CN, Auh SL, Hlubocky FJ, Cummings SA, et al. How often do BRCA mutation carriers tell their young children of the family’s risk for cancer? A study of parental disclosure of BRCA mutations to minors and young adults. J Clin Oncol J Am Soc Clin Oncol. 2007;25:3705–11. doi: 10.1200/JCO.2006.09.1900. [DOI] [PubMed] [Google Scholar]
- 45.Rew L, Mackert M, Bonevac D. A systematic review of literature about the genetic testing of adolescents. J Spec Pediatr Nurs. 2009;14:284–94. doi: 10.1111/j.1744-6155.2009.00210.x. [DOI] [PubMed] [Google Scholar]
- 46.Werner-Lin A, Ratner R, Hoskins LM, Lieber C. A survey of genetic counselors about the needs of 18-25 year olds from families with hereditary breast and ovarian cancer syndrome. J Genet Couns. 2015;24:78–87. doi: 10.1007/s10897-014-9739-y. [DOI] [PubMed] [Google Scholar]
- 47.Gaff CL, Lynch E, Spencer L. Predictive testing of eighteen year olds: counseling challenges. J Genet Couns. 2006;15:245–51. doi: 10.1007/s10897-006-9028-5. [DOI] [PubMed] [Google Scholar]
- 48.Langeland E, Wahl AK. The impact of social support on mental health service users’ sense of coherence: a longitudinal panel survey. Int J Nurs Stud. 2009;46:830–7. doi: 10.1016/j.ijnurstu.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 49.Machisa MT, Christofides N, Jewkes R. Social support factors associated with psychological resilience among women survivors of intimate partner violence in Gauteng, South Africa. Glob Health Action. 2018;11(sup3):491114 [DOI] [PMC free article] [PubMed]
- 50.Ahuja K, Hagerty M, Townsend J. Social support, depression, and life stress: a meta-analytic path analysis. Celebr Learn. 2018: https://digitalcommons.augustana.edu/celebrationoflearning/2018/posters/12
- 51.Peterkin A. Self-help movement experiencing rapid growth in Canada. CMAJ. 1993;148;817–8. [PMC free article] [PubMed]
- 52.Corines MJ, Hamilton JG, Glogowski E, Anrig CA, Goldberg R, Niehaus K, et al. Educational and psychosocial support needs in lynch syndrome: implementation and assessment of an educational workshop and support group. J Genet Couns. 2017;26:232–43. doi: 10.1007/s10897-016-0015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data on subsequent steps of literature search and selection are available upon request.