Abstract
Mechanical thrombectomy is highly effective for the recovery of acute ischemic stroke with large vessel occlusion. However, refractory occlusions are still encountered despite the use of currently available devices. In this article, we present a case of refractory terminal internal carotid artery occlusion treated with the “crossing double stent retriever technique.” Two thrombectomy procedures with the combined technique using a stent retriever and aspiration catheter failed to recanalize the terminal internal carotid artery occlusion that involved the dominant anterior cerebral artery. We then applied the crossing double stent retriever technique as a rescue technique. Two microcatheters were advanced across the occlusion: one to the anterior cerebral artery and the other to the middle cerebral artery. First, a Trevo NXT 4 mm stent retriever was deployed from the anterior cerebral artery. Next, an additional Trevo NXT 4 mm stent retriever was deployed from the middle cerebral artery, and full immediate restoration of flow was achieved on angiography. Intraprocedural radiological images showed that the 2 microcatheters traversed different pathways, and the 2 stent retrievers completely covered the entire vessel with apparent in-stent clot sign. Both stent retrievers were then pulled back together, and a hard clot was retrieved. Subsequent angiography revealed complete recanalization. The crossing double stent retriever technique seems an effective rescue technique for treating refractory terminal internal carotid artery occlusion, especially with the anatomical feature of branching of the dominant anterior cerebral artery. This technique can facilitate the device-clot-vessel interaction by engaging the clot via 2 different device pathways.
Keywords: Acute ischemic stroke, Large vessel occlusion, Endovascular treatment, Mechanical thrombectomy, Stent retriever, Device-clot-vessel interaction
Abbreviations: MT, mechanical thrombectomy; SR, stent retriever; ICA, internal carotid artery; MRI, magnetic resonance imaging; ACA, anterior cerebral artery
Introduction
Endovascular recanalization by mechanical thrombectomy (MT) is highly effective for the recovery of patients with acute ischemic stroke who have large vessel occlusion [1]. However, refractory occlusions are still encountered despite the use of currently available thrombectomy devices [2]. Recently, the “double stent retriever (SR) technique,” in which 2 SRs are used simultaneously at the occlusion site, has been reported as a rescue thrombectomy technique [3], [4], [5], [6], [7], [8], [9], [10], [11]. Previously, we reported that adding one more SR in the same axis at the occlusion facilitates the device-clot interaction, which can be recognized as improved stent coverage in radiographic images during device deployment [11]. In addition, to address the impact of complicated vascular anatomy, it is necessary to gain insight into the mechanism underlying the effectiveness of the procedure, taking into account the “device-clot-vessel interaction” [12,13].
In this report, we present a case of refractory terminal internal carotid artery (ICA) occlusion treated with the “crossing double SR technique,” which is a method of intentionally changing the course of the devices across the clot to better match the vascular geometry.
Case presentation
An 87-year-old man with a history of chronic heart failure was admitted to our institute because of trauma. The patient suddenly developed reduced consciousness with a National Institutes of Health Stroke Scale score of 26. Magnetic resonance imaging (MRI) revealed occlusion of the left ICA with slight acute ischemic changes (Fig. 1A, B). The bilateral anterior cerebral arteries (ACAs) were also not observed. Emergency endovascular treatment was performed without intravenous thrombolysis because of the presence of traumatic intracranial hemorrhage. Written informed consent was obtained from the patient's family member before the procedure.
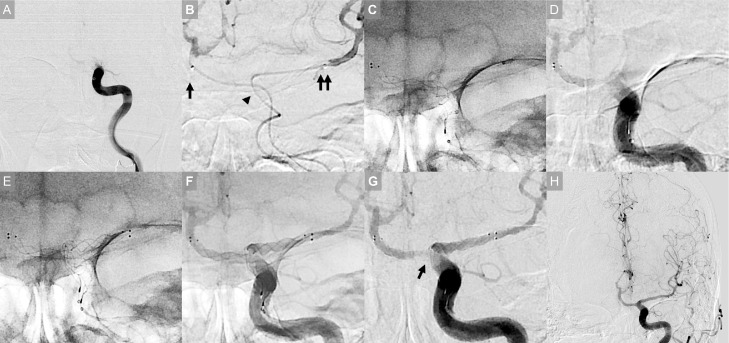
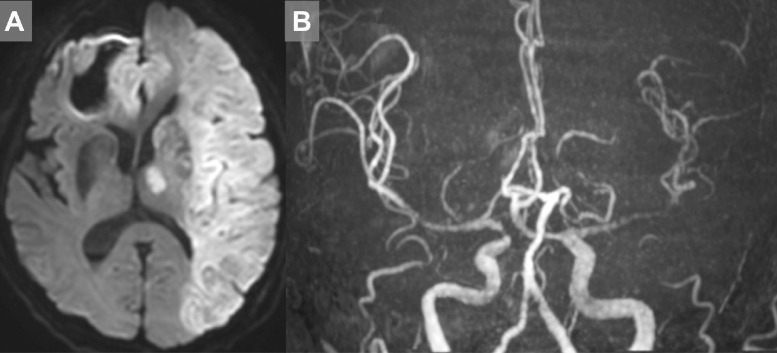
Fig. 1.
Preprocedural image (A and B) Emergency magnetic resonance imaging showing slight acute ischemic changes and occlusion of the left internal carotid artery. The bilateral anterior cerebral arteries were not visualized.
Initial angiography revealed occlusion of the left terminal ICA (Fig. 2A). The microcatheter tended to enter A1 of the ACA, and it was challenging to be directed to M1 of the middle cerebral artery. Despite the considerable difficulty, the microcatheter was placed at the distal M1. However, 2 passes of MT procedures with the combined technique using both an SR and aspiration catheter failed to recanalize the occlusion and did not retrieve any piece of the clot.
Fig. 2.
Intraprocedural image (A) Initial angiography showing occlusion of the left terminal internal carotid artery (ICA). (B) After 2 unsuccessful thrombectomy procedures, we applied the “crossing double SR technique.” Two microcatheters were advanced across the occlusion, one to A1 of the anterior cerebral artery (arrow) and the other to the distal M1 of the middle cerebral artery (double arrow). Note the apparent difference in the course of the 2 microcatheters at the occlusion site (arrowhead). (C) A Trevo NXT 4 × 28 mm stent retriever (SR) was deployed from the A1 to ICA. (D) Angiography showing partial immediate restoration of flow. (E) One more Trevo NXT 4 × 28 mm SR was deployed from the M1 to ICA (F) Angiography showing full immediate restoration of flow. Native angiography image showing that the 2 SRs in total fully covered the inside of the vessel. (G) Digital subtraction angiography image showing the “in-stent clot sign,” which is the filling defect of the clot in the strut and the sign indicating the device-clot interaction (arrow). Thereafter, both deployed SRs were pulled back together, and a hard clot was retrieved. (H) Subsequent angiography revealing complete recanalization.
We then applied the “crossing double SR technique” as a rescue thrombectomy technique during the third pass. Two microcatheters were advanced across the occlusion, one to A1 and the other to the distal M1 (Fig. 2B). First, a Trevo NXT 4 × 28 mm SR (Stryker, Kalamazoo, MI, USA) was deployed from A1 to ICA, and partial immediate restoration of flow was confirmed on angiography (Fig. 2C, D). Next, an additional Trevo NXT 4 × 28 mm SR was deployed from M1 to ICA, and full immediate full restoration of flow was noted (Fig. 2E–G). Both deployed SRs were then pulled back together under aspiration through a balloon guide catheter, and a hard clot was retrieved. Subsequent angiography revealed Thrombolysis in Cerebral Infarction 3 recanalization (Fig. 2H). The time from femoral access to recanalization was 79 minutes, and the time from stroke onset to recanalization was 145 minutes.
Computed tomography performed after the procedure did not reveal any intracranial hemorrhage associated with the endovascular procedure. The day after the procedure, MRI - showed successful revascularization, but with extensive infarction. (Fig 3A, B). The patient did not recover and died 2 days after the procedure.
Fig. 3.
Postprocedural image (A and B) Magnetic resonance imaging performed on the day after the procedure, showing successful revascularization but extensive infarction.
Discussion
We reported a case of refractory terminal ICA occlusion that was treated using the crossing double SR technique. This technique seems effective for treating refractory terminal ICA occlusion, especially with the anatomical feature of dominant ACA branching. This technique can facilitate device-clot-vessel interaction- by engaging the clot via 2 different device pathways.
Our current case suggests that the crossing double SR technique is an effective rescue technique to treat refractory terminal ICA occlusion involving the dominant ACA. Although recanalization was achieved in this case, it did not benefit the patient because of the time delay. However, this case suggests that special consideration may be required for terminal ICA occlusion involving the dominant ACA. The following pitfalls can exist with such vascular geometry: difficulty navigating the microcatheter into the middle cerebral artery, low impact of the thrombectomy device on the clot if used from M1, and limited cerebral ischemic tolerance [14], [15], [16]. In such cases, it should be noted to take effective rescue measures at an early stage that are different from the conventional strategies.
The crossing double SR technique can facilitate the device-clot-vessel interaction by intentionally changing the course of the devices across the clot to better match the vessel geometry. It is now well recognized that in addition to the device-clot relationship, vessel morphology also influences the success of MT, a concept referred to as the device-clot-vessel interaction [12,13]. The intraprocedural images in the current case clearly showed the “in-stent clot sign,” which is the filling defect of the clot in the strut and the sign indicating the device-clot interaction according to our previous study (Fig. 4) [17]. The device may more successfully engage the clot in a complex vascular morphology situation by intentionally changing the pathway.
Fig. 4.
Crossing double SR technique (A) Single stent retriever (SR). The dotted line indicates the area covered by the SR, and the solid line indicates the clot. (B) Double SR. (C) Native angiography image. Note that the 2 SRs notably covered the entire vessel, traversing different pathways. (D) Digital subtraction angiography (DSA) image showing the “in-stent clot sign,” which is the filling defect of the clot in the strut and the sign indicating the device-clot interaction (arrow). (E) Schematic of the crossing double SR technique for a terminal internal carotid artery. This technique can facilitate the device-clot-vessel interaction by intentionally changing the course of the device across the clot to better match the vessel geometry.
The crossing double SR technique has some potential disadvantages. The main concern is the risk of vascular damage, which may be higher than that associated with the usual single SR use. Clinicians should carefully monitor live angiographic images and device resistance [18], [19], [20]. The potential for breakage of the 2 SRs also exists but may be avoided by a simultaneous slow retraction maneuver through the balloon guide catheter [11]. Another problem related to this technique is the increased cost of using 2 SRs. Therefore, this technique should be used in selected cases of refractory occlusion. Further studies are needed to clarify the situations in which this technique is more beneficial than other methods.
Conclusions
Our case suggests that the crossing SR technique is an effective rescue technique for treating refractory terminal ICA occlusion, especially with the anatomical feature of dominant ACA branching. This technique can facilitate device-clot-vessel interaction by intentionally changing the course of the devices across the clot to better match the vessel geometry.
Patient consent
Informed consent has been obtained from the patients family member for publication of the case report and accompanying images.
Footnotes
Acknowledgments: Part of this research was supported by the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (grant number: JP20K17968 and 21KK0289) and medical research fund of Hyogo medical association (grant number: MRF-R-2-20).
References
- 1.Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 2.Abdalla RN, Cantrell DR, Shaibani A, Hurley MC, Jahromi BS, Potts MB, et al. Refractory stroke thrombectomy: prevalence, etiology, and adjunctive treatment in a north american cohort. AJNR Am J Neuroradiol. 2021;42:1258–1263. doi: 10.3174/ajnr.A7124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klisch J, Sychra V, Strasilla C, Taschner CA, Reinhard M, Urbach H, et al. Double solitaire mechanical thrombectomy in acute stroke: effective rescue strategy for refractory artery occlusions? AJNR Am J Neuroradiol. 2015;36:552–556. doi: 10.3174/ajnr.A4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asadi H, Brennan P, Martin A, Looby S, O'Hare A, Thornton J. Double stent-retriever technique in endovascular treatment of middle cerebral artery saddle embolus. J Stroke Cerebrovasc Dis. 2016;25:e9–11. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Okada H, Matsuda Y, Chung J, Crowley RW, Lopes DK. Utility of a Y-configured stentriever technique as a rescue method of thrombectomy for an intractable rooted thrombus located on the middle cerebral artery bifurcation. Neurosurg Focus. 2017;42:E17. doi: 10.3171/2017.1.FOCUS16511. [DOI] [PubMed] [Google Scholar]
- 6.Peker A, Akgoz A, Arsava EM, Topçuoglu MA, Arat A. Dual mechanical thrombectomy for recanalization of a resistant acute posterior circulation stroke. J Cerebrovasc Endovasc Neurosurg. 2017;19:96. doi: 10.7461/jcen.2017.19.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patro SN, Iancu D. Dual-stent retrieval for mechanical thrombectomy of refractory clot in acute stroke as a rescue technique. Can Med Assoc J. 2017;189:E634–E637. doi: 10.1503/cmaj.160472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crosa R, Spiotta AM, Negrotto M, Jaume A, Casagrande W. Y-stent retriever”: a new rescue technique for refractory large-vessel occlusions? J Neurosurg. 2018;128:1349–1353. doi: 10.3171/2016.12.JNS161233. [DOI] [PubMed] [Google Scholar]
- 9.Aydin K, Barburoglu M, Cakmak OO, Yesilot N, Vanli ENY, Akpek S. Crossing Y-Solitaire thrombectomy as a rescue treatment for refractory acute occlusions of the middle cerebral artery. J Neurointerv Surg. 2019;11:246–250. doi: 10.1136/neurintsurg-2018-014288. [DOI] [PubMed] [Google Scholar]
- 10.Moreu M, Pérez-García C, Gómez-Escalonilla C, Rosati S. Dual SAVE technique for mechanical thrombectomy rescue on MCA bifurcation clots. J Neurointerv Surg. 2020;12:1034. doi: 10.1136/neurintsurg-2020-016061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Imahori T, Miura S, Sugihara M, Mizobe T, Aihara H, Kohmura E. Double Stent Retriever (SR) technique: a novel mechanical thrombectomy technique to facilitate the device-clot interaction for refractory acute cerebral large vessel occlusions. World Neurosurg. 2020;141:175–183. doi: 10.1016/j.wneu.2020.05.268. [DOI] [PubMed] [Google Scholar]
- 12.Yoo AJ, Andersson T. Thrombectomy in acute ischemic stroke: challenges to procedural success. J Stroke. 2017;19:121–130. doi: 10.5853/jos.2017.00752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alverne FJAM, Lima FO, Rocha F de A, Bandeira D de A, Lucena AF de, Silva HC, et al. Unfavorable vascular anatomy during endovascular treatment of stroke: challenges and bailout strategies. J Stroke Cerebrovasc Dis. 2020;22:185–202. doi: 10.5853/jos.2020.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kane AG, Dillon WP, Barkovich AJ, Norman D, Dowd CF, Kane TT. Reduced caliber of the internal carotid artery: a normal finding with ipsilateral absence or hypoplasia of the A1 segment. AJNR Am J Neuroradiol. 1996;17:1295–1301. [PMC free article] [PubMed] [Google Scholar]
- 15.Rinaldo L, McCutcheon BA, Murphy ME, Bydon M, Rabinstein AA, Lanzino G. Relationship of A1 segment hypoplasia to anterior communicating artery aneurysm morphology and risk factors for aneurysm formation. J Neurosurg. 2017;127:89–95. doi: 10.3171/2016.7.JNS16736. [DOI] [PubMed] [Google Scholar]
- 16.Shapiro M, Raz E, Nossek E, Chancellor B, Ishida K, Nelson PK. Neuroanatomy of the middle cerebral artery: Implications for thrombectomy. J Neurointerv Surg. 2020;12:768–773. doi: 10.1136/neurintsurg-2019-015782. [DOI] [PubMed] [Google Scholar]
- 17.Imahori T, Okamura Y, Sakata J, Shose H, Yokote A, Matsushima K, et al. Stent expansion and in-stent thrombus sign in the trevo stent retriever predict recanalization and possible etiology during mechanical thrombectomy: a case series of 50 patients with acute middle cerebral artery occlusion. World Neurosurg. 2018;124:e303–e311. doi: 10.1016/j.wneu.2018.12.087. [DOI] [PubMed] [Google Scholar]
- 18.Imahori T, Tanaka K, Koyama J, Arai A, Shiomi R, Iwahashi H, et al. Mechanical thrombectomy using the Trevo ProVue in 50 consecutive patients with anterior circulation stroke: a single-center experience after approval of the stent retriever in Japan. Neurol Med Chir. 2017;57:128–135. doi: 10.2176/nmc.oa.2016-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Imahori T, Okamura Y, Sakata J, Shose H, Yamanishi S, Kohmura E. Delayed rebleeding from pseudoaneurysm after mechanical thrombectomy using stent retriever due to small artery avulsion confirmed by open surgery. World Neurosurg. 2020;133:150–154. doi: 10.1016/j.wneu.2019.09.141. [DOI] [PubMed] [Google Scholar]
- 20.Nakahara M, Imahori T, Tanaka K, Okamura Y, Arai A, Yamashita S, et al. Iatrogenic intracranial vessel dissection during mechanical thrombectomy rescued by emergent stenting: 2 case reports. Radiol Case Rep. 2021;16:835–842. doi: 10.1016/j.radcr.2021.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]