Abstract
The acquisition of resistance to one antibiotic sometimes leads to collateral sensitivity to a second antibiotic. Here, we show that vancomycin resistance in Enterococcus faecium is associated with a remarkable increase in susceptibility to pleuromutilin antibiotics (such as lefamulin), which target the bacterial ribosome. The trade-off between vancomycin and pleuromutilins is mediated by epistasis between the van gene cluster and msrC, encoding an ABC-F protein that protects bacterial ribosomes from antibiotic targeting. In mouse models of vancomycin-resistant E. faecium colonization and septicemia, pleuromutilin treatment reduces colonization and improves survival more effectively than standard therapy (linezolid). Our findings suggest that pleuromutilins may be useful for the treatment of vancomycin-resistant E. faecium infections.
Subject terms: Bacteria, Antimicrobial resistance, Pathogens, Antibiotics
The acquisition of resistance to one antibiotic sometimes leads to collateral sensitivity to a second antibiotic. Here, the authors show that vancomycin resistance in Enterococcus faecium is associated with a remarkable increase in susceptibility to pleuromutilin antibiotics, such as lefamulin.
Introduction
The patterns of evolutionary cross-resistance to clinical antibiotics are a major driving force for accelerating the emergence and dissemination of multidrug resistant (MDR) bacteria1. Potential avenues for antibiotic resistance are co-selection for resistance driven by antimicrobial‐producing organisms and harmful substances in natural environments where active compounds compete for the same targets2. The possibility of such cross‐resistance to clinical antibiotics has received intensive attention previously. Antibiotic resistance often carries various fitness costs in the absence of selective pressures, and such trade-offs in turn occasionally result in rugged fitness landscapes to channel the evolutionary trajectory3. However, the understanding that whether and how negative responses to antibiotic selective pressure modulate the trajectory of evolution in bacteria remains unclear4,5. Indeed, pioneering works have recently implicated the patterns of collateral sensitivity in Escherichia coli6, Pseudomonas aeruginosa7, Staphylococcus aureus8,9 and other pathogens, wherein resistance to one antibiotic simultaneously induces susceptibility to another by forming either homogeneous or heterogeneous populations10 (Fig. 1a). The clinical implications of collateral sensitivity therefore supply prioritized rational therapies such as the sequential or concurrent deployment of reciprocal collateral sensitivity antibiotic pairs, to combat the antibiotic resistance crisis.
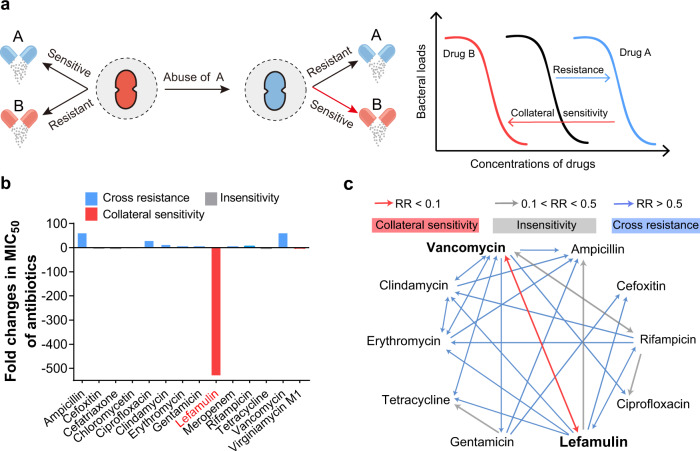
Fig. 1. Vancomycin-resistant E. faecium show collateral sensitivity to lefamulin.
a Scheme of collateral sensitivity. Bacterial evolution of resistance to one antibiotic is usually accompanied by collateral sensitivity to another antibiotic. b Fold changes in MIC50 of 14 antibiotics between VREfm (n = 20) and VSEfm (n = 20). c Collateral sensitivity network among antibiotics in E. faeicums. For collateral sensitivity network, the directed paths of each arrow represent the collateral sensitivity (red), cross resistance (blue) and insensitivity (gray). Resistance ratio (RR) = MIC50 (resistance)/MIC50 (parental). Collateral sensitivity (CS): RR < 0.1, insensitivity: 0.1 < RR < 0.5, cross resistance (CR): RR > 0.5.
The increasing vancomycin-resistant enterococci (VRE) particularly vancomycin-resistant Enterococcus faecium (VREfm), with high genomic plasticity and metabolic flexibility, seriously compromise the effectiveness of existing antibiotics11. The persistence and spread of VREfm within health care settings has become one of the most challenging nosocomial pathogens, leading to at least 5400 estimated deaths and more than $500 million in excess health care costs annually in the United States (U.S.)12 and accounting for 37% nosocomial infections in Germany13. Although vancomycin resistance is widely mediated by mega-plasmids containing diverse van gene clusters, these resistance alleles have been persistently maintained in VRE with low or without fitness cost14. Therefore, a better mechanistic understanding of antibiotic resistance is urgently required to combat VREfm associated infections. However, the evolutionary and pharmacological consequences of dedicated van genes remain largely unknown. In this work, we exploit the evolutionary trade-offs to identify the collateral sensitivity patterns of 102 clinical VREfm isolates nationwide for antibiotic repurposing. Our observations indicate that pleuromutilin antibiotics are promising candidates targeting VREfm in vitro and in animal models, shedding light on the evolution-directed rational design of antibiotic therapies against MDR bacterial infections.
Results and discussion
VREfm show collateral sensitivity to pleuromutilins
To identify the trade-offs in VREfm, we first determined the susceptibility and constructed the network of collateral sensitivity of 10 main classes of antibiotics routinely used in the clinic against both 20 VREfm and 20 vancomycin sensitive E. faecium (VSEfm) isolates. Markedly, compared to VSEfm, we observed that VREfm exhibited specific susceptibility to lefamulin (Fig. 1b, Supplementary Tables 1, 2), an approved pleuromutilin antibiotic by the U.S. Food and Drug Administration (FDA) for community-acquired bacterial pneumonia (CABP) in 201915, although they displayed general cross-resistance to multiple antibiotics as expected (Fig. 1c). The susceptibility to lefamulin increased more than 500 folds, from ≥16 μg/mL to 0.03 μg/mL. To extend whether other ribosome-targeting antibiotics display similar behaviors, we tested eight antibiotics with different binding sites16. It confirmed a strong collateral sensitivity to lefamulin with the minimum inhibitory concentration required to inhibit the growth of 50% bacteria (MIC50) of 0.03 μg/mL in VREfm, whereas most VSEfm were resistant to lefamulin with MIC50 of 16 μg/mL (Fig. 2a). Therefore, we hypothesized that such collateral response could be due to the distinct modes of action of pleuromutilins (PLEs).
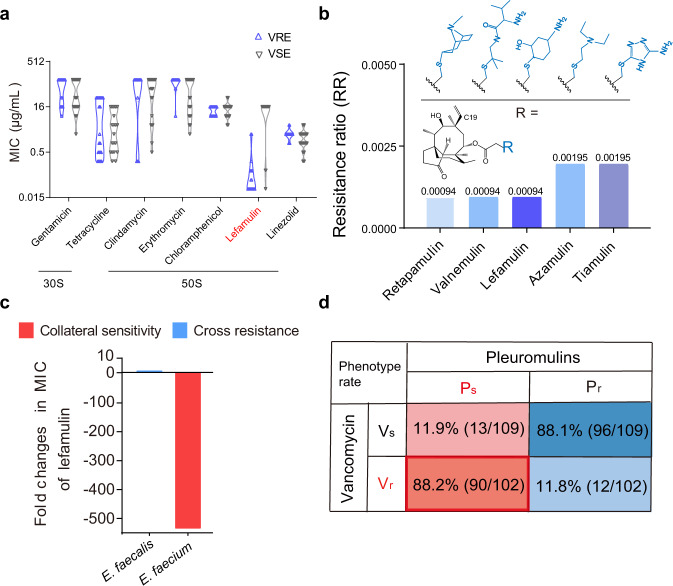
Fig. 2. Collateral response to pleuromutilins is universal in VREfm.
a MIC50 of eight ribosome-targeting antibiotics against E. faeciums (n = 40). b Resistance ratios of pleuromutilins against 210 E. faecium isolates. Structures of five pleuromutilins, where the C19 of the tricyclic mutilin core is single bond in azamulin. (c) Fold changes in MIC50 of lefamulin against E. faeciums (n = 210) and E. faecalis (n = 10). d Proportion of four phenotypes in E. faeciums. ~90% VREfm (n = 102) are sensitive to pleuromutilins, whereas ~90% of VSEfm (n = 109) are resistant. Vs: sensitivity to vancomycin, Vr: resistance to vancomycin, Ps: sensitivity to pleuromutilins, Pr: resistance to pleuromutilins.
To test the generality of VREfm channeled evolution toward elevated susceptibility to pleuromutilins, we first performed the structure-activity relationship (SAR) analysis of five pleuromutilins routinely used in human and veterinary medicine (Fig. 2b, Supplementary Fig. 2a). We expanded the number of E. faecium isolates to 210, including 102 VREfm isolates of human origins and 109 VSEfm isolates of human, animals and probiotics in China. These VREfm isolates validated the robust collateral sensitivity to pleuromutilins, particularly the decreased MICs of lefamulin, retapamulin and valnemulin with resistance ratios of <0.002 (Fig. 2b, Supplementary Table 1). Our results are consistent with previous empirical observations that the analogs of pleuromutilin tend to be efficacious against VREfm17,18. To further verify this phenomenon, we compared the genomes of 79 global VREfm isolates (Supplementary Table 3) with 21 domestic ones, and found that the allelic profiles in China showed high genetic relationships with that in Europe and North America (Supplementary Fig. 1a). Notably, the vanA gene clusters are dominant (95%, 20/21) in 21 clinic VREfm isolates (Supplementary Fig. 1b), consisting with the vanA genotype most frequently recorded11,13. To further assess the generality of collateral sensitivity in other van gene clusters, we found that a clinical vanB-type E. faecium isolate showed similar collateral patterns to five pleuromutilins (Supplementary Table 2). Then, we tested the activity of lefamulin against E. faecalis including vancomycin resistant/ sensitive isolates. In contrast to VREfm, vancomycin-resistant E. faecalis (VREfs) were resistant to lefamulin (Fig. 2c), implying the species specificity of collateral sensitivity in enterococci. The collateral pattern indicates the species-specific effect19, where the collateral sensitivity to pleuromutilins in VREfm is contingent upon the intrinsic genomics. It is consistent with previous studies20,21 that the van gene clusters are located on pMG1-like and pheromone sensing plasmids in VREfm and VREfs, respectively. Additionally, the ubiquity of plasmid-encoded toxin-antitoxin gene systems may also account for the species-specific effect22. Collectively, it suggests that the antibiotic pairs of vancomycin and pleuromutilins exhibit ubiquitous collateral sensitivity in VREfm.
To further characterize the collateral response, we noticed the susceptibility of 210 E. faeciums isolates in four patterns that approx. 90% isolates (89/102) of VREfm display collateral sensitivity to pleuromutilins using lefamulin as a model (PsVr) (Fig. 2d). Intriguingly, we observed the contrary pattern of pleuromutilin susceptibility in VSEfm, in which approx. 90% isolates (96/109) of VSEfm were resistant to pleuromutilins (PrVs). Therefore, E. faecium shape the divergent evolution upon pleuromutilins to four patterns, including PsVr, PsVs, PrVs and PrVr, and in turn such contingency can be used to design rational approaches to treating the prevalent VREfm associated infections.
Heterogeneous collateral responses are channeled by ribosomes
The unique collateral sensitive antibiotics suggest that the interaction between pleuromutilins and the target may shed light on elucidating the evolutionary conservation in VSEfm. First, lefamulin showed moderate bacteriostatic activity against VREfm at a high level (1.2 μg/mL, 40 × MIC) (Supplementary Fig. 3). Furthermore, we quantified the accumulation of lefamulin in eight E. faecium isolates including all four phenotypes of heterogeneous collateral responses and found no difference (Supplementary Fig. 5a, b). Last, we confirmed there was almost no further modifications for the accumulated lefamulin in E. faecium (Supplementary Fig. 5c–j). These data denote that the intrinsic properties of pleuromutilins should be excluded and the main target of pleuromutilins should eventually dominate the trajectory of collateral response in VREfm.
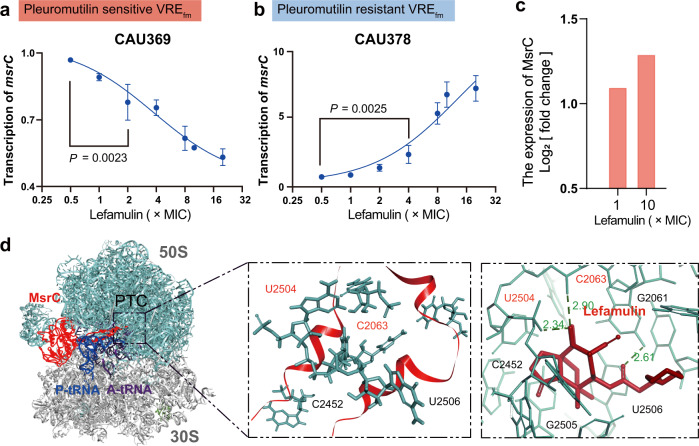
Pleuromutilins exhibit distinctive recognition to the peptidyl transferase center (PTC) by blocking bacterial protein biosynthesis16. Pleuromutilins mainly interact with eight nucleotides in the PTC domain. We first confirmed that there were no mutations at such sites in 20 VREfm and 20 VSEfm isolates based on whole-genome sequence analysis (Fig. 4a, Supplementary Figs. 2c, 6b). Moreover, we found no genes such as cfr23 encoding methyltransferases to confer universal resistance (Supplementary Fig. 7a–c). Interestingly, we found that pleuromutilins had a higher affinity to ribosomes in PsVr than PrVs type strains through fluorescence polarization analysis24 (Supplementary Fig. 8a, b), implying that VREfm may modulate the susceptibility to pleuromutilins through the mechanism of ribosomal protection. The ATP-binding cassette F (ABC-F) protein family protects bacterial ribosomes from multiple classes of ribosome-targeting antibiotics25. We found the presence of four prevailing genes (msrC, eatA/eatAv and lsaE) of the 26 members of the ABC-F family26 in 40 E. faecium isolates (Supplementary Fig. 6b). Nevertheless, both lsaE and eatA/eatAv were partially carried by clinical isolates and expressed at similar levels in the presence and absence of pleuromutilins (Supplementary Fig. 9a, b). Extremely, we noticed that the species-specific gene msrC27 expressed more than 70-fold higher in model strain VSEfm CAU310 than VREfm CAU369 (Supplementary Fig. 9c), suggesting that the low expression of msrC may potentiate the efficacy of pleuromutilins. Meanwhile, we observed that the decreased transcription of msrC in two lefamulin sensitive VREfm isolates (Fig. 3a, Supplementary Fig. 10a) is in a dose-dependent manner of lefamulin. Furthermore, we found the increased transcription of msrC in all 12 lefamulin resistant isolates as well (Fig. 3b, Supplementary Figs. 10b, 11). Constantly, we obtained the increased expression of MsrC in a lefamulin resistant VREfm CAU378 treated with lefamulin for 1 h (Fig. 3c), based on proteomics analysis. Additionally, the MsrC overexpression strain was constructed in a pleuromutilins-sensitive strain using conjugative transformation (Supplementary Fig. 12a). We found that the conjugant (pAM401 + msrC) shows high expression of msrC and are resistant to all pleuromutilins (Supplementary Fig. 12b–d). Taken together, these results indicate that msrC is linked with the collateral sensitivity in VREfm.
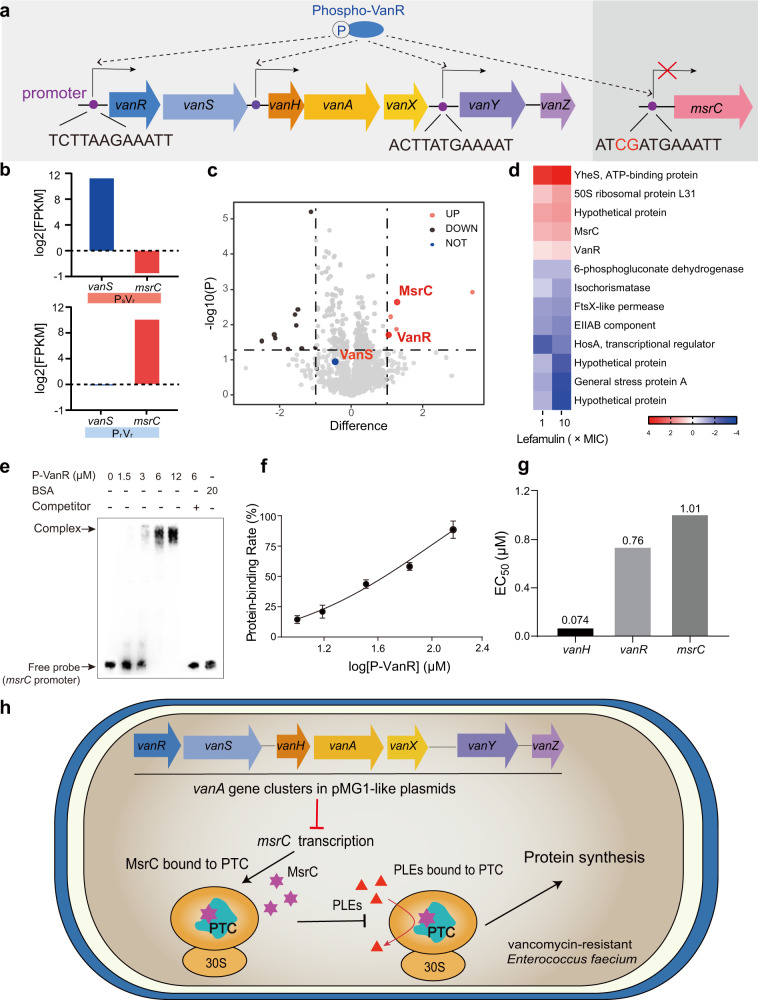
Fig. 4. Epistasis between the van gene cluster and msrC.
a Promoters in genes vanR, vanH, vanY and msrC. b Fold changes in log2 [FPKM] values of relative expression of vanS and msrC. Transcriptome analysis of E. faeciums under the treatment of lefamulin at levels of 1× and 10 × MIC for 1 h. c Volcano plot represents the protein expression ratios of lefamulin treated bacterial cells (VREfm CAU378). For each protein, the -log 10 (P-value) is plotted against its log2 (fold change). Proteins upregulated (P < 0.05, fold change > 2) in 1× and 10 × MIC lefamulin treated samples are colored in red, proteins downregulated (P < 0.05, fold change < −2) are colored in blue, while unchanged in black. d Proteomics analysis of VREfm CAU378 treated with 1× and 10 × MIC lefamulin for 1 h. Proteins were identified as significantly different with fold changes of log2 [fold changes] values of at fold-increase or fold-decrease of expression levels. e Binding reactions between P-VanR (12–1.5 μM) and msrC promoter fragment (212-bp, 0.3 ng) based on the gel electrophoretic mobility shift assay. Free probe: biotin-labeled promoter; Competitor: Unlabeled promoter; BSA: Bovine serum albumin. Experiments were performed as three biologically independent experiments. f Calculated protein-binding rates of P-VanR and vanH/vanR/msrC promoters, based on the gray values in Fig. 4e. g Binding constants of vanH/vanR/msrC promoters and P-VanR. h Scheme of collateral sensitivity in VREfm. The decreased transcription of msrC by van genes enhances ribosome-targeting pleuromutilins binding to PTC to block protein synthesis. Data were presented as means ± S.D. n.s., not significant, determined by non-parametric one-way ANOVA (n = 3).
Fig. 3. Low expression of msrC is linked with collateral sensitivity.
a–b Transcription analysis of msrC in pleuromutilin-sensitive VREfm CAU369 (a) and pleuromutilin-resistant VREfm CAU378 (b). c Proteomics analysis of VREfm CAU378 treated with 1× and 10 × MIC lefamulin for 1 h. Proteins were identified as significantly different with fold changes of log2 [fold changes] values of at fold-increase or fold-decrease of expression levels. d Comparison of lefamulin binding sites within the MsrC-ribosome complex. The 50S (green) and 30S (gray) subunits (PDB 5AA0 [https://www.rcsb.org/structure/5AA0]), and the A-site tRNA (purple) and P-site tRNA (blue) are shown. Binding of MsrC (red, homology of the template with PDB 5ZLU [https://www.rcsb.org/structure/5ZLU], middle) blocks the binding of lefamulin (brick-red, PDB 5HL7 [https://www.rcsb.org/structure/5HL7], right) to PTC in the 50S subunit. Data were presented as means ± S.D. n.s., not significant, determined by non-parametric one-way ANOVA (n = 3).
To explore how MsrC reduces the susceptibility to pleuromutilins, we performed a simulation analysis on the interaction between MsrC and the PTC domain28. Compared to the affinity between pleuromutilins and PTC with Z-docker interaction energy of −146.324 kcal, the residues of R241 and L242, and K233 and K246 in MsrC competitively bound to the shared binding sites U2504 and C2063 of MsrC and lefamulin in PTC domain, respectively, with Z-docker interaction energy of −170.611 kcal (Fig. 3d). These findings indicate that high expression of species-specific MsrC tends to block pleuromutilins targeting PTC in VSEfm, whereas the low expression of MsrC facilitate the binding of pleuromutilins in VREfm accordingly.
Epistasis between van gene clusters and msrC
To understand how msrC mediates collateral response in VREfm, we first observed the delayed growth curves of a constructed conjugant containing the vanA-plasmid from E. faecium CAU369 (pCAU369) in E. faecium BM4105-RF20, in the presence of sub-inhibitory levels of lefamulin (Supplementary Fig. 14b, c). It suggested that the plasmid carrying the van gene cluster plays a crucial role in the increased susceptibility to pleuromutilins in VREfm. Subsequently, we showed that most van gene clusters are dominant vanA-type (95%, 19/20) (Supplementary Fig. 6b), consisting with previous reports that the increasing dissemination of vanA-VREfm is prevalent world widely, particularly in the U.S. and Europe29,30. Therefore, we compared 14 plasmids containing vanA gene clusters in global E. faecium isolates (Supplementary Table 5) with that in E. faecium CAU369, and noticed only the vanA gene clusters were present in all isolates (Supplementary Fig. 13). Thus, we deduced that the vanA gene clusters (~ 6–7 kbp), instead of the other motifs in the vanA-type megaplasmids31 (~ 30–150 kbp), contribute to the collateral sensitivity to pleuromutilins in VREfm.
Given that the decreased expression of msrC in VREfm (Fig. 3a, Supplementary Fig. 9c), we hypothesized a negative feedback between msrC and the vanA gene clusters. To verify such epistasis, we found the sequence in the promoter of msrC shared high similarity (83.3%, 10/12) to the promoters of vanR/H/Y32 (Fig. 4a) and the promoters are conserved in both vanA- and vanB-type isolates globally (Supplementary Fig. 15), indicating that phosphorylated VanR may simultaneously induce van transcription but inhibit msrC transcription. Toward this goal, we exploited transcriptome analysis on VREfm treated with lefamulin. Remarkably, we observed vanRS activation and decreased msrC transcription in pleuromutilin-sensitive VREfm CAU369, whereas there was no vanS activation and 33.1% vanR transcription, and increased msrC transcription in pleuromutilin-resistant VREfm CAU378 (Supplementary Fig. 16). Consistently, we confirmed the opposite patterns of vanS and msrC transcription in pleuromutilin-resistant isolates under lefamulin treatments based on qRT-PCR and proteomics analysis (Fig. 4b–d, Supplementary Fig. 17a, b). To validate that vanR modulates msrC expression, we constructed a conjugant by receiving a recombinant vanRS plasmid in a pleuromutilin resistant E. faecium (Supplementary Fig. 18). The transcription of vanR and vanS were activated in a dose-dependent manner under lefamulin treatments (Supplementary Fig. 19a, b), in turn, the transcription of msrC in the conjugant (pAM401 + vanRS) was dramatically inhibited (Supplementary Fig. 19c). Correspondingly, the conjugant with vanRS expression is sensitive to pleuromutilins, with more than 16-fold decreased MICs (Supplementary Fig. 19d). These results support our hypothesis that the negative epistasis between the van gene cluster and msrC is responsible for the collateral sensitivity to pleuromutilins in VREfm.
To further verify that P-VanR regulates msrC transcription, we first demonstrated that P-VanR binds to the msrC promoter using electrophoretic mobility shift assay (Fig. 4e, f). Furthermore, we calculated the EC50 (effective concentration for 50% response) as 1.01 μmol/L for P-VanR binding to the fragment of msrC promoter, which is much lower than the binding affinity between P-VanR and the vanH promoter (Fig. 4g). When in the presence of inducers such as classic vancomycin and lefamulin, VanS switches its activity from phosphatase to kinase, phosphorylating the cognate response regulator VanR33. Phospho-VanR then binds to similar promoter sequences triggering the transcription of the van gene cluster, and inhibits msrC transcription to induce VREfm sensitive to pleuromutilins accordingly (Fig. 4h). Altogether, these results indicate that P-VanR co-regulates vanR/vanH and msrC by binding to similar promoter fragments, to facilitate pleuromutilins against VREfm.
In addition, antibiotic resistance/tolerance can be regulated by metabolic reprogramming34,35, which, in principle, could boost the effectiveness of antibiotics, consistent with the observation that anaerobic glycolysis further exacerbated the growth of VREfm with vanA-plasmid in the presence of subinhibitory levels of lefamulin (Supplementary Fig. 14c). To test this possibility, we dissect whether metabolites modulate collateral response in VREfm. Since there is no Krebs cycle in enterococci36, the dominant pyruvate metabolism kept steadily (Supplementary Fig. 21a–c). Considering the abundance of metabolic versatility and the challenge to genetically manipulate clinical isolates, its contribution to collateral sensitivity in most VREfm with mega-plasmids remains unclear.
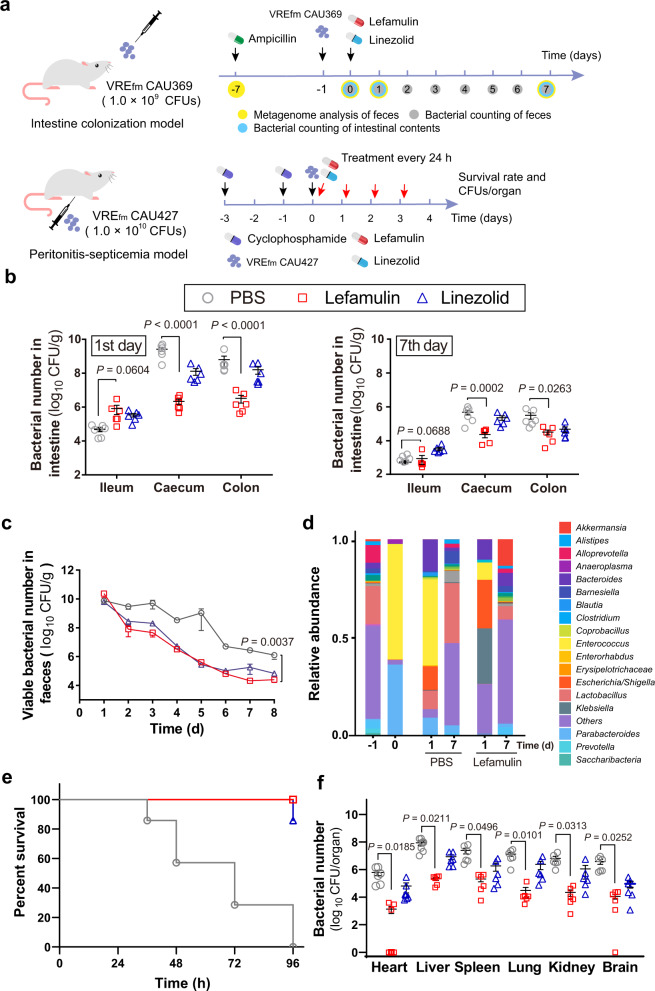
Collateral sensitivity in vivo
Given that VRE usually resists multiple classes of antibiotics, we hypothesized that pleuromutilins might be used to treat VRE associated infections based on our observation. Lefamulin was recently approved in the U.S. and European Union for the treatment of CABP in adults. To further assess the efficacy of lefamulin, we empirically evaluated its efficacy in two mouse models including an intestinal colonization model (VREfm CAU369) and in a peritonitis-septicemia model in mice (VREfm CAU427) (Fig. 5a). First, we found that VREfm CAU369 mainly colonized in the cecum and colon with remarkably decreased bacterial burden after a single dose of lefamulin (Fig. 5b). Remarkably, lefamulin showed better antibacterial efficacy than linezolid, the only antibiotic with the U.S. Food and Drug Administration (FDA) approval for treating VRE infections, especially in the cecum and colon on the first day after administrations. Meanwhile, we collected daily the feces for bacterial counting. Compared to clinically recommended linezolid, lefamulin similarly produced time-dependent reduction in bacterial burden of feces over the 7-day treatment period (Fig. 5c). In addition, VREfm promptly dominated mouse gut microbiota after intragastric inoculum based on bacterial community analysis, whereas lefamulin administration notably reduced its abundance through the upregulated the genera of Akkermansia and Klebsiella (Fig. 5d). After 7 days, all mice nearly eliminated the pathogens and appeared healthy. Intriguingly, lefamulin could restore the homeostasis of fecal microbiota faster than the untreated group according to the Chao1 and Shannon indexes (Supplementary Fig. 22a, b), particularly the patterns of Bacteroides, Prevotella, Clostridium, and Escherichia/Shigella on the 7th day (Supplementary Fig. 22c–f). In the peritonitis-septicemia model, the survival curve showed that all mice survived under the treatment of a dose of 10 mg/kg lefamulin after 96 h (Fig. 5e), with reduced bacterial counts in organs (Fig. 5f). Altogether, our results suggest that lefamulin efficiently remedies the severity of VREfm infections, which may be extended to treat and diminish bacterial colonization since that there are limited effective agents available to treat such infections in clinic.
Fig. 5. Efficacy of lefamulin against VREfm in vivo.
a Scheme of mouse intestinal colonization model and VREfm peritonitis-septicemia model. b Bacterial loads in the ileum, cecum and colon. Mice (n = 6 per group) were given 1 × 109 CFUs of VREfm CAU369, under the treatment of a single dose of 5 mg/kg lefamulin or linezolid. c Bacterial loads in feces. Mice (n = 6 per group) were given 1 × 109 CFUs of VREfm CAU369 by oral gavage, with administration of 5 mg/kg lefamulin or linezolid. d Fecal microbiota was profiled of mice infected with VREfm CAU369 in the presence of 5 mg/kg lefamulin at different points using 16S rRNA gene sequencing. e Survival rates of peritonitis-septicemia mice infected with VREfm CAU427 (1.0 × 1010 CFUs) in the presence of lefamulin (10 mg/kg). f Lefamulin decreased bacterial loads in different organs in the mouse peritonitis-septicemia model (n = 6 per group). Data in b, c and d were presented as mean values ± S.D, f was presented as mean values ± SEM. P-values in b, c and d were determined by non-parametric one-way ANOVA and in f was determined by two-tailed t-test.
For the foreseeable future, VRE especially VREfm will remain an important nosocomial problem37,38, particularly the steady increase in the U.S. since the early 1990s in hospitals11. Because VREfm has developed resistance to essentially every antibiotic used in clinic, novel therapeutic strategies to explore collateral sensitivity may be attempted. A better understanding of the evolutionary biology particularly epistasis by which the van genes manipulate ribosome protection could shed light on intervention strategies against VREfm pathogens. Notably, plasmid mediated epistasis is not restricted to E. faecium, and we postulate that such collateral response may be widespread phenomenon in other bacteria. Mobile plasmids drive the spread of many critical antibiotic resistance genes in clinical pathogens39. Most recently, it has been demonstrated the collateral sensitivity associated with transferable plasmids in clinical E. coli isolates40, compared to previous empirical observations and mutations in chromosome and plasmids5–9. Our results suggest that the evolutionally collateral response has already dominated the prevalent VREfm carrying conjugative plasmids (Supplementary Fig. 14a). To argue for preclinical development of pleuromutilins as leads against VREfm, continued studies should further focus on the evaluation whether pleuromutilins reduce VREfm colonization in patients and maintain microbiota recovery after its expansion.
In conclusion, our results demonstrate the epistasis between van genes and msrC mediating collateral sensitivity in most clinically relevant VREfm strains, to potentiate the efficacy of pleuromutilins. These observations in vitro and in vivo provide proof-of-concept for an efficient therapeutic option against the increasingly aggravating VREfm associated infections by revitalizing existing antibiotics. Pleuromutilins not only exhibit robust bacteriostatic activity against clinical isolates nationwide but also attenuate the colonization possibly improving clinical outcomes. Overall, our work expands the knowledge of evolutionary compensatory phenomenon for the implementation of existing antibiotics to combat MDR bacterial pathogens.
Methods
Antimicrobial-susceptibility test
Minimum inhibitory concentrations (MICs) of antibiotics were performed using the standard broth microdilution method, according to the CLSI 2020 guideline. Briefly, single bacterial colonies (including E. faecalis ATCC 29212 and 210 E. faeciums isolates) were cultured in Mueller Hinton Broth (MHB) at 37 °C at 220 r.p.m. for 8–12 h. Subsequently, antibiotics with two-fold dilution in MHB were mixed with an equal volume of bacterial suspensions in MHB containing approximately 1.5 × 106 colony-forming units (CFUs)/mL in a clear UV-sterilized 96-well microtiter plate. The plate was placed in the incubator for 16–18 h at 37 °C and then the MIC values were read. MIC values were defined as the lowest concentrations of antibiotics with no visible growth of bacteria.
Time-dependent killing assay
An overnight culture of VREfm CAU369 was diluted 1:100 in MHB and incubated at 37 °C, 200 r.p.m. for 4 h, to obtain bacteria at exponential phase. Then the bacterial suspension was challenged with lefamulin at 4 × MIC, 10 × MIC and 40 × MIC. Subsequently, 10-fold serially diluted suspensions were plated on BHI agar plates for overnight incubation at 37 °C. Finally, colonies were counted and CFUs per mL were calculated accordingly.
Membrane integrity assay
An overnight culture of VREfm CAU369 were inoculated in 0.01 M phosphate-buffered saline (PBS) (pH 7.4) to adjust bacterial suspensions to approximately an OD600 of 0.5, following by the addition of propidium iodide (PI) to a final concentration of 10 nM, then treated with lefamulin and linezolid at the levels of 1 × MIC, 5 × MIC and 10 × MIC for 34 min after centrifugation. The fluorescence was measured at the excitation wavelength of 535 nm and emission wavelength of 615 nm in two-min intervals using the Infinite M200 Microplate reader (Tecan).
Membrane fluidity assay
An overnight culture of VREfm CAU369 was incubated with 10 µM Laurdan at 37 °C for 20 min in the dark. The stained bacterial cell was washed with PBS for three times. Then, 190 µL of the culture was mixed with 10 μL of PBS containing lefamulin at the level of 1 × MIC, 5 × MIC and 10 × MIC in the black, clear-bottom, 96-well plates. Benzyl alcohol (50 mM) was used as a positive control. Last, the fluorescence intensities of Laurdan were measured at the excitation wavelength of 350 nm and emission wavelengths of 435 nm and 490 nm in two-min intervals using the Infinite M200 Microplate reader (Tecan). The Laurdan GP was calculated using the formula GP = (I435− I490)/ (I435 + I490).
ROS measurement
An overnight culture VREfm CAU369 grown from a single colony in Brain Heart Infusion (BHI) broth were washed and resuspended in 0.01 M of PBS (pH 7.4) to obtain an OD600 of 0.5. Subsequently, 2′,7′-dichlorofluorescein diacetate (DCFH-DA) was added to a final concentration of 10 μM and the mixture was incubated at 37 °C for 30 min. After washing with 0.01 M of PBS for three times, 190 μl of probe-labeled bacterial cells were added to a 96-well plate treated with 10 μl of lefamulin at the level of 1 × MIC, 5 × MIC and 10 × MIC. After incubation for another 30 min, fluorescence intensity was immediately measured with the excitation wavelength at 488 nm and the emission wavelength at 525 nm in two-min intervals using the Infinite M200 Microplate reader (Tecan).
Membrane depolarization assay
An overnight culture of VREfm CAU369 bacterial cells were washed and resuspended to obtain an OD600 of 0.5 with 5 mM of HEPES (pH 7.0, + 5 mM of glucose). Then 3,3-dipropylthiadicarbocyanine iodide DiSC3(5) (Aladdin, ≥98%, 1 μM) was added. The dissipated membrane potential of VREfm CAU369 in the presence and absence of lefamulin at the level of 1 × MIC, 5 × MIC and 10 × MIC were measured at the excitation wavelength of 622 nm and emission wavelength of 670 nm using the Infinite M200 Microplate reader (Tecan).
△pH measurement
△pH was measured in the presence of pH-sensitive fluorescent probe BCECF-AM (10 μM). An overnight culture of VREfm CAU369 bacterial cells treated with lefamulin at the level of 1 × MIC, 5 × MIC and 10 × MIC were measured at the excitation wavelength of 500 nm and emission wavelength of 522 nm for 40 min, using the Infinite M200 Microplate reader (Tecan).
ATP determination
Extracellular and intracellular levels of ATP were determined using an Enhanced ATP Assay Kit (Beyotime). VREfm CAU369 grown overnight at 37 °C with shaking at 200 r.p.m. were washed and resuspended to obtain an OD600 of 0.5 with 0.01 M of PBS (pH 7.4). After treatment with 1 × MIC, 5 × MIC and 10 × MIC lefamulin for 1 h, bacterial cultures were centrifuged at 12,000 r.p.m. and 4 °C for 5 min, and the supernatants were collected for the determination of extracellular ATP levels. Meanwhile, bacterial precipitates were lysed by lysozyme, and centrifuged, then the supernatants were prepared for the measurement of intracellular ATP levels. The detecting solution was added to a 96-well plate and incubated at room temperature for another 5 min. Last, the supernatants were added to the well and mixed quickly, before recording in the model of luminescence using the Infinite M200 Microplate reader (Tecan).
Antibiotic accumulation test
The accumulation of intracellular antibiotics in bacteria was determined based on the established liquid chromatography with tandem mass spectrometry (LC-MS/MS) method41. Overnight cultures of bacterial cells (VREfm CAU369, VREfm CAU372, VREfm CAU378, VREfm CAU419, VSEfm CAU259, VSEfm CAU277, VREfm CAU309, VREfm CAU310, S. aureus 29213, MASA T144, E. faecalis 29212, VRE CAU 475) were diluted to 100 mL fresh BHI broth at 1:100 and resuspended to OD600 of 0.5 at 37 °C. Bacteria were then centrifuged at 3,000 g for 10 mins at 4 °C and the supernatants were collected for three times. Subsequently, bacterial cells were diluted to 1010 CFU per mL with fresh PBS and aliquoted in 1.5 mL tubes. The aliquots were treated with subinhibitory levels of lefamulin at 37 °C for 1 h and the samples were collected to destroy the cell envelopes for LC-MS/MS analysis (Waters 2695). Additionally, structure elucidation of accumulated lefamulin in four phenotypes of E. faeciums isolates were based on UHPLC-Q-Orbitrap analysis (UHPLC-Q-Exactive Plus, Thermo Fisher Scientific). Extracted ion chromatogram of lefamulin obtained in the positive ESI mode at retention time of 7.08 min. Elucidation of lefamulin and its product ions based on the molecular weights of m/z 508.31 (lefamulin), and product ions of m/z 188.07 and 206.08.
Whole-genome sequencing
Genomic DNA were extracted from the overnight culture of E. faeciums (including 20 VREfm and 20 VSEfm) isolates in BHI, according to the manufacturer instructions (Genome Extraction Kit, Magen). Obtained DNA was sequenced by Illumina Seq and the whole-genomes were aligned with the resistance gene database from the Center for Genomic Epidemiology (CGE).
Molecular simulation
Models of the complexes of lefamulin-ribosome and MsrC- ribosome were built on Discovery Studio 2018 Client. The model of MsrC was generated using the sequence from VREfm CAU369. The receptor-ligand interaction and the Z-Docker reaction energy in the 50S and 30S subunits, and tRNA were performed according to a previous study28.
Methylation modification analysis
Methylation modification analysis is based on the SELECT approach according to a previous study42. Briefly, total RNA (1500 ng) was mixed with 40 nM up primer, 40 nM down primer and 5 M dNTP in 17 μL CutSmart buffer. SELECT qPCR was performed with the following program: 90 °C for 1 min, 80 °C for 1 min, 70 °C for 1 min, 60 °C for 1 min, 50 °C for 1 min and 40 °C for 6 min. Afterward, the qRT-PCR was performed using SYBR premix Ex Taq qPCR Kit (TaKaRa). qRT-PCR was performed with the following program: 95 °C, 5 min; 95 °C, 10 s then 60 °C, 35 s for 40 cycles; 95 °C, 15 s; 60 °C, 1 min; 95 °C, 15 s. Primers for SELECT qPCR or qRT-PCR are listed in Table S6, respectively. Ct values of samples were normalized to their corresponding Ct values of control. All assays were performed with three independent experiments.
Fluorescence polarization assay
The fluorescence polarization value (FP value) was detected as described previously43. Briefly, the assay was conducted by adding 70 μL per well of VAL-DTAF (valnemulin-([4,6-dichlorotriazine-2-yl] amino)-fluorescein) tracer working solution at 0.5 μM and 70 μL per well of prepared ribosome at the level 0–2 nM to the microplate, followed by the addition of 70 μL per well of liquid A buffer (10 mM Tris [pH 7.5], 60 mM KCl, 10 mM NH4Cl, 300 mM NaCl, 6 mM MgCl2, 0.1 mM ATP). After the mixture was shaken for 10 s in the microplate reader, FP values were measured with the excitation wavelength at 485 nm and the emission wavelength at 530 nm using the Infinite M200 Microplate reader (Tecan).
Growth dynamics
Overnight cultures of E. faeciums BM4105-RF and conjugant BM369-1 grown from a single colony in BHI broth were diluted 1:100 in MHB and made the final concentration approximately 1× 106 CFU per mL. Lefamulin (1/8 × MIC, 1/4 × MIC, 1/2 × MIC and 1 × MIC) was added into 96 well microplates and mixed with an equal volume of cultures. Growth curves were established by OD600 determination with an interval of 1 h at 37 °C, by Infinite M200 Microplate reader (Tecan).
Conjugation assay
Filter mating was performed using VREfm CAU369 as the donor and E. faecium BM4105 (resistant to rifampicin and fusidic acid) as the recipient, according to previous study22. The mating mixtures of donor and recipient were filtered through a sterile membrane filter (pore size, 0.45 μm). The filters were incubated on BHI agar plates for 24 h at 37 °C. After mating, the conjugants were selected on BHI agar containing rifampin (100 μg/mL), fusidic acid (20 μg/mL) and vancomycin (20 μg/mL) after incubated at 37 °C for 24–48 h.
msrC overexpression mutant
The msrC overexpression mutant was constructed based on a modified conjugative transformation assay, according to previous study22. The overexpression plasmid pAM401+msrC was recombined by the linearized pAM401 and the amplification of msrC sequence. msrC gene was amplified from the genome of E. faecium BM4105 by PCR reaction. The overexpression plasmid pAM401+msrC was transferred into E. faecalis JH2-2. Filter mating was performed using E. faecalis JH2-2 (pAM401 + msrC) as the donor and E. faecium GE-1 as the recipient. After mating, the conjugants were selected on BHI agar containing chloramphenicol (50 μg/mL) and arabinose after incubated at 37 °C for 24–48 h.
Isogenic mutant constuaction
The vanRS isogenic mutant was constructed based on a modified conjugative transformation assay, according to previous study22. The plasmid pAM401+vanRS was recombined by the linearized pAM401 and the amplification of vanRS sequence. vanRS gene was amplified from the genome of VREfm CAU369 by PCR reaction. The plasmid pAM401+vanRS was transferred into E. faecalis JH2-2. Filter mating was performed using E. faecalis JH2-2 (pAM401 + vanRS) as the donor and E. faecium BM4105 as the recipient. After mating, the conjugants were selected on BHI agar containing chloramphenicol (50 μg/mL) and arabinose after incubated at 37 °C for 24–48 h.
qRT-PCR assay
An overnight culture of VREfm CAU369 was diluted 1:100 in BHI and incubated at 37 °C, 200 r.p.m. for 4 h. Bacteria were obtained at exponential phase and treated with or without lefamulin and vancomycin (0.5 × MIC, 1 × MIC, 10 × MIC) for 1 h at 37 °C. Total RNA was extracted using the EASYspin Plus kit (Aidlab, cat. RN4301) and quantified by the ratio of absorbance (260 nm/280 nm) using a Nanodrop spectrophotometer (Thermo Scientific, MA, USA). The qRT-PCR was performed using SYBR premix Ex Taq qPCR Kit (TaKaRa, catalog no. RR820A). Cycling conditions consisted of an initial denaturation step at 95 °C for 30 s, followed by 40 cycles at 95 °C for 5 s, 60 °C for 30 s, and 72 °C for 30 s. All samples were analyzed in triplicate and the gene 16 S rRNA was used as an endogenous control as described in our previous publication44. The fold changes of gene expression were analyzed by 2−∆∆CT method. Genes names and primer sequences used in the qRT-PCR analysis are listed in Table S7. GraphPad Prism 8 was used to plot graphs
Transcriptome analysis
Overnight cultures (VREfm CAU369 and VREfm CAU378) were diluted 1:100 in BHI and incubated at 37 °C, 200 r.p.m. for 4 h, to obtain bacteria at exponential phase. Then the bacterial suspensions were treated with lefamulin at the level of 1 × MIC and 10 × MIC for 15 min and 1 h. Then the bacteria were washed with fresh PBS (0.01 M, pH 7.4) three times and the bacterial cells were spun down by centrifuging at 8,000 r.p.m. for 10 min at 4 °C. RNA-Seq library building and RNA-seq data analysis are described as described previously45.
Metabolomics analysis
Metabolomics were determined based on UPLC-QTOF MS analysis. Overnight cultures (VREfm CAU369 and VSEfm CAU309) grown in BHI broth were harvested and washed with 0.01 M PBS (pH 7.4) three times. Then, approximately 50 mg precipitation of bacteria was mixed with 0.5 mL 80% methanol containing 0.1% formic acid (FA). After shaking for 30 s and ultrasonic treatment for 20 min, all samples were frozen for 1 h at −20 °C for protein precipitation. The samples were then centrifuged at 10,000 × g and 4 °C for 10 min and the supernatant (200 μL) was obtained. (O)PLS-DA (Orthogonal signal correction partial least square discrimination analysis) was performed and VIP (variable importance in projection) was calculated by MetaboAnalyst 4.0 and R project.
Proteomics analysis
Overnight cultures VREfm CAU378 were diluted 1:100 in BHI and incubated at 37 °C, 200 r.p.m. for 4 h, to obtain bacteria at exponential phase. Then the bacterial suspension were treated with lefamulin at the level of 1 × MIC and 10 × MIC for 1 h. Then cells were lysed and the protein was reduced and alkylated by heating at 95 °C for 5 min followed by sonication for 20 min. The resulting mixture was diluted 10 times with the dilution buffer composed of 25 mM Tris–HCl (pH 8.5) and 10% acetonitrile (ACN) and the protein was digested with trypsin at 37 °C overnight. After digestion, the total protein was acidated with 5% TFA and loaded onto a C18-column which had been pretreated and equili- brated with methanol and 0.2% acetic acid respectively. For MS analysis, total peptides were dissolved in 0.1% FA and analyzed by Orbitrap Fusion Lumos mass spectrometer (Thermo Scientific). Raw data were processed with PD software package against the sequence data of VREfm.
Electrophoretic mobility shift assay
VanR purified and P-VanR prepared according to a previously described protocol46. Binding reactions between P-VanR (12–1.5 μM) and msrC promoter fragment (212-bp, 0.3 ng) based on the gel electrophoretic mobility shift assay. Briefly, P-VanR was incubated with different concentrations. After 15 min incubation, the reaction mixture was subjected to 5% nondenaturing polyacrylamide gel and electrophoresis was performed at 80 V in ice-cold bath. The images were visualized and acquired by the PharosFX imaging system (Bio-Rad, CA, USA).
Intestinal colonization model
To evaluate the in vivo efficacy of lefamulin, a mouse intestinal colonization model was involved according to a previous publication44. Briefly, 6–8 weeks old female ICR mice (20 g, n = 6 per group) were treated with PBS, lefamulin and linezolid. First, mice were administered 0.5 g per L ampicillin in drinking water for 5 days. On day 0, mice were infected with VREfm CAU369 (1 × 109 CFUs) by gavage. After the treatments with drugs, CFUs of VREfm CAU369 were enumerated in the feces from 1 to 7 days. Meanwhile, intestinal contents (including ileum, cecum and colon) were collected on the first and seventh day for bacterial counting and the evaluation of the abundance and diversity of intestinal flora, using a previously described method44. The alpha analysis and the beta diversity analysis were performed based on PCoA/NMDS analysis. GraphPad Prism 8 was used to plot graphs
Mouse peritonitis-septicemia model
To construct an immunosuppressive mice model, the 6–8 weeks old ICR female mice (20 g, n = 6 per group, 18 mice were used in total) were treated with 200 mg/kg cyclophosphamide intraperitoneally at the 1st day and 3rd day. After the second cyclophosphamide was treated for 24 h, mice were infected with 0.5 mL of VREfm CAU427 suspension (1 × 1010 CFU per mouse) via intraperitoneal injection. At 1 h post-infection, all mice were treated with lefamulin and linezolid with 10 mg/kg every 24 h. PBS was used as the negative control. The survival rates of treated mice were recorded during a 96 h period and the bacterial number in the mice organs was counted on the plates.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
This work is dedicated to Prof. S.Y. Ding for her retirement. We thank all patients for clinical VREfm isolates in China. This study is supported by the Guangdong Major Project of Basic and Applied Basic Research (2020B0301030007), National Natural Science Foundation of China (31922083), Beijing Municipal Science and Technology (Z201100008920001), and Chinese Universities Scientific Fund (2021RC005).
Source data
Author contributions
J.Z.S. and K.Z. conceived and supervised the project. Q.L. and S.C. performed all the experiments. Q.L. and Y.C.H. conducted the antibacterial tests and animal infection model. S.C. and Q.L. conducted outer-membrane permeability, membrane depolarization, ATP and ROS assays, and membrane fluidity assay. Q.L. performed the transcriptome assay. Z.Q.S., S.Y.D., R.Z., and K.Z. did the data analysis. R.Z., D.X.G., Q.W.Y., H.L.S., F.P.H., H.W., J.C.C. and B.M. shared the clinical VREfm isolates in this study. Q.L., S.C. and K.Z. wrote the manuscript. All authors read and approved the manuscript.
Peer review
Peer review information
Nature Communications ature Communicationson: aria Van Tyne for their contribution to the peer review of this work. Peer reviewer reports are available.
Data availability
DNA and RNA sequencing data are available in NCBI SRA with accession number PRJNA628015. The MS raw files and proteome sequences data used in this study are available in the Proteome Xchange Consortium under accession code PXD030906. The metabolomic data have been deposited in the CNCB-NGDC repository under accession code PRJCA008528 and in MetaboLights under submission code MTBLS4498. Other data generated in this study are provided in the Supplementary Information and the Source Data file. Source data are provided with this paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Qian Li, Shang Chen.
Contributor Information
Kui Zhu, Email: zhuk@cau.edu.cn.
Rong Zhang, Email: zhang-rong@zju.edu.cn.
Jianzhong Shen, Email: sjz@cau.edu.cn.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-022-29493-0.
References
- 1.Theuretzbacher U, et al. Critical analysis of antibacterial agents in clinical development. Nat. Rev. Microbiol. 2020;18:286–298. doi: 10.1038/s41579-020-0340-0. [DOI] [PubMed] [Google Scholar]
- 2.Culp EJ, et al. Evolution-guided discovery of antibiotics that inhibit peptidoglycan remodelling. Nature. 2020;578:582–587. doi: 10.1038/s41586-020-1990-9. [DOI] [PubMed] [Google Scholar]
- 3.Nichol D, et al. Antibiotic collateral sensitivity is contingent on the repeatability of evolution. Nat. Commun. 2019;10:334. doi: 10.1038/s41467-018-08098-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baym M, Stone LK, Kishony R. Multidrug evolutionary strategies to reverse antibiotic resistance. Science. 2016;351:aad3292. doi: 10.1126/science.aad3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pal C, Papp B, Lazar V. Collateral sensitivity of antibiotic-resistant microbes. Trends Microbiol. 2015;23:401–407. doi: 10.1016/j.tim.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lázár V, et al. Antibiotic-resistant bacteria show widespread collateral sensitivity to antimicrobial peptides. Nat. Microbiol. 2018;3:718–731. doi: 10.1038/s41564-018-0164-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imamovic L, et al. Drug-driven phenotypic convergence supports rational treatment strategies of chronic infections. Cell. 2018;172:121–134. doi: 10.1016/j.cell.2017.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzales PR, et al. Synergistic, collaterally sensitive beta-lactam combinations suppress resistance in MRSA. Nat. Chem. Biol. 2015;11:855–861. doi: 10.1038/nchembio.1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harrison EM, et al. Genomic identification of cryptic susceptibility to penicillins and beta-lactamase inhibitors in methicillin-resistant Staphylococcus aureus. Nat. Microbiol. 2019;4:1680–1691. doi: 10.1038/s41564-019-0471-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu JF, et al. Effect of tolerance on the evolution of antibiotic resistance under drug combinations. Science. 2020;367:200–204. doi: 10.1126/science.aay3041. [DOI] [PubMed] [Google Scholar]
- 11.Arias CA, Murray BE. The rise of the Enterococcus: beyond vancomycin resistance. Nat. Rev. Microbiol. 2012;10:266–278. doi: 10.1038/nrmicro2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antibiotic resistance threats in the United States, 2019. (Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2019. https://stacks.cdc.gov/view/cdc/82532/CS298822-B-2019-ar-threats-report-508.pdf).
- 13.Werner G, et al. Thirty years of VRE in Germany - “expect the unexpected”: the view from the national reference centre for Staphylococci and Enterococci. Drug. Resist. Updat. 2020;53:100732. doi: 10.1016/j.drup.2020.100732. [DOI] [PubMed] [Google Scholar]
- 14.Andersson DI, Hughes D. Antibiotic resistance and its cost: is it possible to reverse resistance? Nat. Rev. Microbiol. 2010;8:260–271. doi: 10.1038/nrmicro2319. [DOI] [PubMed] [Google Scholar]
- 15.Alexander E, et al. Oral lefamulin vs moxifloxacin for early clinical response among adults with community-acquired bacterial pneumonia: the LEAP2 randomized clinical trial. JAMA. 2019;322:1661–1671. doi: 10.1001/jama.2019.15468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin J, Zhou DJ, Steitz TA, Polikanov YS, Gagnon MG. Ribosome-targeting antibiotics: modes of action, mechanisms of resistance, and implications for drug design. Annu. Rev. Biochem. 2018;87:451–478. doi: 10.1146/annurev-biochem-062917-011942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sader HS, Biedenbach DJ, Paukner S, Ivezic-Schoenfeld Z, Jones RN. Antimicrobial activity of the investigational pleuromutilin compound BC-3781 tested against Gram-positive organisms commonly associated with acute bacterial skin and skin structure infections. Antimicrob. Agents Chemother. 2012;56:1619–1623. doi: 10.1128/AAC.05789-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paukner S, Riedl R. Pleuromutilins: potent drugs for resistant bugs-mode of action and resistance. Cold Spring Harb. Perspect. Med. 2017;7:a027110. doi: 10.1101/cshperspect.a027110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Apjok G, et al. Limited evolutionary conservation of the phenotypic effects of antibiotic resistance mutations. Mol. Biol. Evol. 2019;36:1601–1611. doi: 10.1093/molbev/msz109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomita H, et al. Highly conjugative pMG1-like plasmids carrying Tn1546-like transposons that encode vancomycin resistance in Enterococcus faecium. Bacteriol. 2003;185:7024–7028. doi: 10.1128/JB.185.23.7024-7028.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tanimoto K, Ike Y. Complete nucleotide sequencing and analysis of the 65-kb highly conjugative Enterococcus faecium plasmid pMG1: identification of the transfer-related region and the minimum region required for replication. FEMS Microbiol. Lett. 2008;288:186–195. doi: 10.1111/j.1574-6968.2008.01342.x. [DOI] [PubMed] [Google Scholar]
- 22.Moritz EM, Hergenrother PJ. Toxin-antitoxin systems are ubiquitous and plasmid-encoded in vancomycin-resistant enterococci. Proc. Natl Acad. Sci. USA. 2007;104:311–316. doi: 10.1073/pnas.0601168104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Y, et al. First report of the multidrug resistance gene cfr in Enterococcus faecalis of animal origin. Antimicrob. Agents Chemother. 2012;56:1650–1654. doi: 10.1128/AAC.06091-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y, Fu Z, Li D, Yue Y, Liu X. Optimizations of a novel fluorescence polarization-based high-throughput screening assay for beta-catenin/LEF1 interaction inhibitors. Anal. Biochem. 2021;612:113966. doi: 10.1016/j.ab.2020.113966. [DOI] [PubMed] [Google Scholar]
- 25.Wilson DN, Hauryliuk V, Atkinson GC, O’Neill AJ. Target protection as a key antibiotic resistance mechanism. Nat. Rev. Microbiol. 2020;18:637–648. doi: 10.1038/s41579-020-0386-z. [DOI] [PubMed] [Google Scholar]
- 26.Sharkey LK, Edwards TA, O’Neill AJ. ABC-F Proteins mediate antibiotic resistance through ribosomal protection. mBio. 2016;7:e01975. doi: 10.1128/mBio.01975-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh KV, Malathum K, Murray BE. Disruption of an Enterococcus faecium species-specific gene, a homologue of acquired macrolide resistance genes of Staphylococci, is associated with an increase in macrolide susceptibility. Antimicrob. Agents Chemother. 2001;45:263–266. doi: 10.1128/AAC.45.1.263-266.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Su WX, et al. Ribosome protection by antibiotic resistance ATP-binding cassette protein. Proc. Natl Acad. Sci. USA. 2018;115:5157–5162. doi: 10.1073/pnas.1803313115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao W, Howden BP, Stinear TP. Evolution of virulence in Enterococcus faecium, a hospital-adapted opportunistic pathogen. Curr. Opin. Microbiol. 2018;41:76–82. doi: 10.1016/j.mib.2017.11.030. [DOI] [PubMed] [Google Scholar]
- 30.Harten RMV, Willems RJL, Martin NI, Hendrickx APA. Multidrug-resistant enterococcal infections: new compounds, novel antimicrobial therapies? Trends Microbiol. 2017;25:467–479. doi: 10.1016/j.tim.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 31.Wardal E, et al. Diversity of plasmids and Tn1546-type transposons among vanA Enterococcus faecium in Poland. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36:313–328. doi: 10.1007/s10096-016-2804-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holman TR, Wu Z, Wanner BL, Walsh CT. Identification of the DNA-binding site for the phosphorylated VanR protein required for vancomycin resistance in Enterococcus faecium. Biochemistry. 1994;33:4625–4631. doi: 10.1021/bi00181a024. [DOI] [PubMed] [Google Scholar]
- 33.Novotna GB, Kwun MJ, Hong HJ. In vivo characterization of the activation and interaction of the VanR-VanS two-component regulatory system controlling glycopeptide antibiotic resistance in two related streptomyces species. Antimicrob. Agents Chemother. 2015;60:1627–1637. doi: 10.1128/AAC.01367-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lopatkin AJ, et al. Clinically relevant mutations in core metabolic genes confer antibiotic resistance. Science. 2021;371:eaba0862. doi: 10.1126/science.aba0862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zampieri M, Zimmermann M, Claassen M, Sauer U. Nontargeted metabolomics reveals the multilevel response to antibiotic perturbations. Cell Rep. 2017;19:1214–1228. doi: 10.1016/j.celrep.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 36.Kawai Y, et al. Crucial role for central carbon metabolism in the bacterial L-form switch and killing by beta-lactam antibiotics. Nat. Microbiol. 2019;4:1716–1726. doi: 10.1038/s41564-019-0497-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stein-Thoeringer CK, et al. Lactose drives Enterococcus expansion to promote graft-versus-host disease. Science. 2019;366:1143–1149. doi: 10.1126/science.aax3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim SG, et al. Microbiota-derived lantibiotic restores resistance against vancomycin-resistant Enterococcus. Nature. 2019;572:665–669. doi: 10.1038/s41586-019-1501-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.MacLean RC, Millan AS. The evolution of antibiotic resistance. Science. 2019;365:1082–1083. doi: 10.1126/science.aax3879. [DOI] [PubMed] [Google Scholar]
- 40.Herencias C, et al. Collateral sensitivity associated with antibiotic resistance plasmids. eLife. 2021;10:e65130. doi: 10.7554/eLife.65130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li Y, et al. Efficient killing of multidrug-resistant internalized bacteria by AIEgens in vivo. Adv. Sci. 2021;8:2001750. doi: 10.1002/advs.202001750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang Y, et al. LEAD-m(6) A-seq for Locus-Specific Detection of N(6) - Methyladenosine and quantification of differential methylation. Angew. Chem. Int Ed. Engl. 2020;60:873–880. doi: 10.1002/anie.202007266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li CL, et al. Development of a screening fluorescence polarization immunoassay for the simultaneous detection of fumonisins B(1) and B(2) in maize. Agric Food Chem. 2015;63:4940–4946. doi: 10.1021/acs.jafc.5b01845. [DOI] [PubMed] [Google Scholar]
- 44.Kim SG, et al. Microbiota-derived lantibiotic restores resistance against vancomycin-resistant. Enterococcus. Nature. 2019;572:665–669. doi: 10.1038/s41586-019-1501-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Song MR, et al. A broad-spectrum antibiotic adjuvant reverses multidrug-resistant gram-negative pathogens. Nat. Microbiol. 2020;5:1040–1050. doi: 10.1038/s41564-020-0723-z. [DOI] [PubMed] [Google Scholar]
- 46.Kim SG, et al. Identification of the DNA-binding site for the phosphorylated VanR protein required for vancomycin resistance in Enterococcus faecium. Biochemistry. 1994;33:4625–4631. doi: 10.1021/bi00181a024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
DNA and RNA sequencing data are available in NCBI SRA with accession number PRJNA628015. The MS raw files and proteome sequences data used in this study are available in the Proteome Xchange Consortium under accession code PXD030906. The metabolomic data have been deposited in the CNCB-NGDC repository under accession code PRJCA008528 and in MetaboLights under submission code MTBLS4498. Other data generated in this study are provided in the Supplementary Information and the Source Data file. Source data are provided with this paper.