Abstract
Periodontal diseases are one of the most common chronic inflammatory diseases of the oral cavity, which are initiated and sustained by pathogenic plaque biofilms. Central to modern periodontology is the idea that dysbiosis of periodontal microecology and disorder of host inflammatory response gives rise to degradation of periodontal tissues together, which eventually leads to tooth loss, seriously affecting the life quality of patients. Probiotics were originally used to treat intestinal diseases, while in recent years, extensive studies have been exploring the utilization of probiotics in oral disease treatment and oral healthcare. Probiotic bacteria derived from the genera Lactobacillus, Bifidobacterium, Streptococcus, and Weissella are found to play an effective role in the prevention and treatment of periodontal diseases via regulating periodontal microbiota or host immune responses. Here, we review the research status of periodontal health-promoting probiotic species and their regulatory effects. The current issues on the effectiveness and safety of probiotics in the management of periodontal diseases are also discussed at last. Taken together, the use of probiotics is a promising approach to prevent and treat periodontal diseases. Nevertheless, their practical use for periodontal health needs further research and exploration.
Keywords: probiotic, periodontal disease, periodontopathogen, microecological balance, immunoregulation
Probiotic and Oral Health
The term “probiotic” was put forward by Lilly and Stillwell in 1965, defined as “growth-promoting factors produced by microorganisms” (Lilly and Stillwell, 1965). Since then, the definition of “probiotic” has changed several times until the WHO and the Food and Agriculture Organization of the United States (FAO) in 2002 came up with a new definition that was generally accepted: probiotics are “living microorganisms that can have a beneficial effect on the host when taken in sufficient doses” (Hill et al., 2014). The origins of probiotics could be traced back to ancient Roman records, and Plinius Secundus Maior recorded that fermented milk products are beneficial to stomach healing. In the early 20th century, Elie Metchnikoff, a Nobel laureate, recorded in “The Prolongation of Life” that Bulgarians lived longer than others because they drank fermented milk (Metchnikoff, 1907). Through the study of human gut flora, he concluded that harmful products of some bacteria could be a reason for aging, and he recommended milk fermented by Lactobacillus to prevent the harmful effects of bacterial products.
Probiotics were originally used to treat intestinal diseases. Studies have shown that they could help control intestinal infections, relieve constipation and diarrhea, improve lactose intolerance, etc. (Lourenshattingh and Viljoen, 2001). The beneficial effects of probiotics defined by WHO and FAO are not only on the intestines but also on other body systems. In fact, many probiotics have been demonstrated to play a role in maintaining a healthy urogenital system and fighting against cancers, diabetes, obesity, and allergies (Waigankar and Patel, 2011; Sunita et al., 2012; Kang et al., 2013; Takeda et al., 2014; Kahouli et al., 2015). In recent decades, extensive studies also explored the application of probiotics in oral disease treatment and oral healthcare. Currently, it is found that probiotics contributing to oral health are concentrated in the genera Lactobacillus, Bifidobacterium, Streptococcus, and Weissella, as well as certain scattered species like Bacillus subtilis and Saccharomyces cerevisiae. Several strains of Lactobacillus reuteri, Lactobacillus brevis, Streptococcus salivarius, etc., have been commercially produced as oral health-promoting probiotics, all of which are microorganisms isolated from the oral cavity (Allaker and Stephen, 2017; Mahasneh and Mahasneh, 2017). Effects of probiotics on improving oral health have been observed in common oral diseases such as dental caries, periodontal diseases, oral candida infection, and halitosis (Ince et al., 2015; Ohshima et al., 2016; Yoo et al., 2019; Sivamaruthi et al., 2020).
Periodontal Diseases
Periodontal diseases are chronic inflammatory diseases that destroy bone and gum tissues that support the teeth, of which gingivitis and periodontitis are the most common types. Gingivitis is a mild form of periodontal disease, but the progression of untreated gingivitis can lead to more serious periodontitis by creating deep periodontal pockets that could cause teeth to loosen or lead to tooth loss, which has a marked impact on patients’ life. It is reported that as of 2019, there are 1.1 billion patients with severe periodontitis worldwide, and the prevalence of severe periodontitis has increased by 8.44% from 1990 to 2019 (Chen et al., 2021). Dental plaque, which is a microbial biofilm that forms on the teeth and gingiva, is thought to be the initial factor of periodontal diseases. The understanding of the pathogenicity of dental plaque biofilms has evolved over time, and several hypotheses were proposed in history, from the “Specific Plaque Hypothesis” (1976) (Loesche, 1976), the “Non-Specific Plaque Hypothesis” (1986) (Theilade, 1986), to the “Ecological Plaque Hypothesis” (1994) (Marsh, 1994). Modern periodontology, however, not only focuses on the pathogenicity of dental plaque biofilms but also emphasizes the interaction between oral microbes and the host. In recent years, the “Keystone-Pathogen Hypothesis” (KPH) (2012) and polymicrobial synergy and dysbiosis (PSD) model (2012) have attracted wide attention. The KPH (Hajishengallis et al., 2012) proposed that certain low-abundance periodontopathogens such as Porphyromonas gingivalis could weaken the bactericidal effect of the host immune system and promote host inflammatory response, thus destroying the host–microbe homeostasis and balance of periodontal microecosystem that finally lead to the occurrence of periodontal diseases. The PSD model (Hajishengallis and Lamont, 2012) emphasized that the synergistic effect between polymicrobial communities and the host inflammatory response disorder caused periodontal diseases, and moreover, the ecological imbalance and inflammatory response could reinforce each other and constitute the actual driving factors of diseases. In fact, subversion of host immunity by dysbiotic periodontal microbiota not only gives rise to periodontal diseases but also contributes to systemic inflammation (Hajishengallis, 2015).
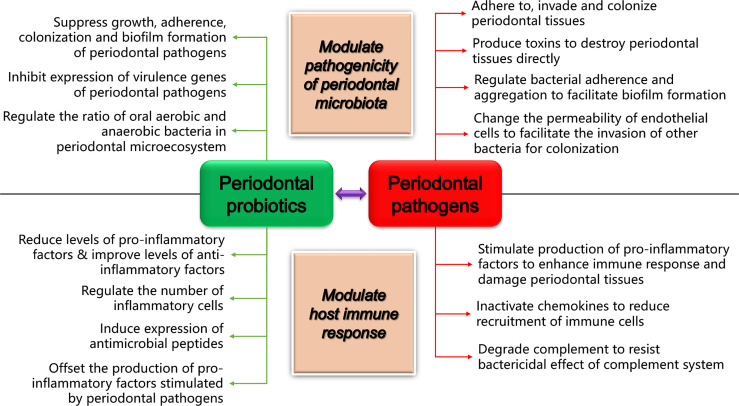
Studies on oral microorganisms show that there are more than 700 bacterial species colonizing the mouth (Kumar et al., 2005). However, only a few bacteria are proved to initiate and advance periodontal diseases, such as P. gingivalis, Aggregatibacter actinomycetemcomitans, Tannerella forsythia, Prevotella intermedia, and Fusobacterium nucleatum (Hajishengallis et al., 2012). When reviewing the studies focusing on the action of probiotics in managing periodontal diseases, we noticed that the majority referred to four periodontopathogens, namely, P. gingivalis (chronic periodontitis), A. actinomycetemcomitans (aggressive periodontitis), P. intermedia (pregnancy gingivitis, moderate and severe gingivitis, acute necrotizing gingivitis, and chronic periodontitis), and F. nucleatum (chronic periodontitis and acute necrotizing ulcerative gingivitis), indicating that periodontal probiotics are often related with or applied to specific periodontal diseases driven by them. With the help of various virulence factors that cause direct destruction to periodontal tissues or stimulate host cells to activate a wide range of inflammatory responses (Figure 1), these pathogens destroy the host–microbe homeostasis and cause or promote the occurrence and development of multiple periodontal diseases (Zhao et al., 2012; Jaffar et al., 2016; Zhao et al., 2019; Ishikawa et al., 2020; Moman et al., 2020; Ding et al., 2021; Jansen et al., 2021).
Figure 1.
How periodontal probiotics and pathogens play their roles in regulating periodontal health and disease. The diagram shows the primary mechanisms of periodontopathogens and probiotics in regulating periodontal microbiota and host immune responses, respectively.
Application of Probiotics in Managing Periodontal Diseases
There is an increasing interest in the use of probiotics in periodontal therapy and periodontal care. The existing published studies have revealed that probiotics could effectively inhibit periodontopathogens and improve various clinical indices related to periodontal health, including plaque index (PI), gingival index (GI), bleeding on probing (BOP), periodontal pocket depth (PPD), clinical attachment loss (CAL), and gingival crevicular fluid (GCF) volume, as well as inflammation-associated biochemical markers, such as interleukin (IL)-1β, matrix metalloproteinase (MMP)-8, and tissue inhibitor of metalloproteinase (TIMP)-1. Although there are various forms of probiotics applied in managing periodontal diseases, such as tablets, mouthwash, and toothpaste, probiotics commercialized and studied in periodontal therapy are usually made into tablets, while probiotics in the forms of mouthwash and toothpaste are often applied in periodontal health care.
Periodontal Health Care
Some studies have focused on the role of probiotics in periodontal care. Amizic et al. found that probiotic toothpaste could prevent caries and periodontal diseases more effectively than non-probiotic toothpaste, and the capacity of the toothpaste to inhibit bacteria was even better than that of mouthwash. It was speculated that toothpaste could contact the tooth surface for a longer time, and it would be easy to enter gingival sulcus with the help of a toothbrush (Amizic et al., 2017). However, the study of Alkaya et al. (2016) had a different conclusion. Forty patients with gingivitis were recruited and divided into 2 groups, using placebo or experimental probiotic B. subtilis-, Bacillus megaterium-, and Bacillus pumulus-containing toothpaste, mouthwash, and toothbrush cleaner for 8 weeks. After evaluation of PI, GI, PPD, and BOP at baseline and 8 weeks, it was reported that there was no intergroup difference detected, suggesting that genetically distinct probiotics perhaps have different effects on periodontal health.
An Adjuvant Therapy for Periodontal Non-Surgical Treatment
Some researchers have evaluated the short-term and long-term effects of probiotics as a supplementary therapy for periodontal non-surgical treatment. For example, in the study of Kuru et al. (2017), 51 periodontal healthy volunteers were first given non-surgical periodontal therapy, and 7 days later (baseline), they were randomized into two groups receiving yogurt containing either placebo or Bifidobacterium animalis subsp. lactis DN-173010 for 28 days, followed by a 5-day non-brushing period. PI, GI, BOP, PPD, GCF volume, and total amount and concentration of IL-1β in GCF were measured on days 0 (baseline), 28, and 33. It was reported that there was no intergroup difference detected on day 0 and day 28. However, after plaque accumulation, all parameters in the probiotic group were significantly better than those in the placebo group on day 33, indicating that the short-term use of probiotics has a positive effect on plaque accumulation and gingival inflammatory parameters, even without oral hygiene measures. The long-term clinical benefits of probiotic were proved by İnce et al. Thirty patients with chronic periodontitis were randomly given either L. reuteri-containing lozenge or placebo twice a day after scaling and root planing (SRP) for 3 weeks, and clinical parameters were collected at baseline and on days 21, 90, 180, and 360 after SRP. It was found that the probiotic group’s PI, GI, BOP, and PPD were much better than those of the placebo group at all time points. Decreased MMP-8 and increased TIMP-1 levels in GCF were found to be significant up to day 180. From day 90, mean values of attachment gain were significantly higher in the probiotic group (Ince et al., 2015). In a meta-analysis about the effects of using probiotics as the supplemental therapy after periodontal non-surgical treatment for 42–360 days, Kumar et al. concluded that probiotics could help reduce CAL significantly in moderately deep periodontal pockets. However, the three of four studies included for meta-analysis showed significant heterogeneity, though the risk of bias was low (Kumar and Madurantakam, 2017). Studies have suggested that short-term and long-term applications of probiotics can achieve certain clinical benefits, but relevant studies are not enough, and limited probiotics are involved.
As for peri-implant disease, some studies on the effect of L. reuteri ATCC PTA 5289 and DSM 17938 as adjuvant therapy to mechanical debridement revealed the potential of probiotics in treating peri-implant mucositis. Using L. reuteri for at least 30 days relieved PI, GI, PPD, and BOP in peri-implant mucositis and reduced the concentrations of IL-1β, IL-6, and IL-8 in GCF (Flichy-Fernández et al., 2015; Galofré et al., 2018). Moreover, compared to mechanical debridement followed by rinsing with 0.12% chlorhexidine (CHX), utilization of L. reuteri did not make a difference (Peña et al., 2019). However, with respect to implantitis, only one study reported significant PD and BOP improvement in 90 days after mechanical treatment and L. reuteri application (Galofré et al., 2018). L. reuteri might improve PI, but the subgingival microbial community of the implant was not changed markedly (Galofré et al., 2018; Tada et al., 2018; Laleman et al., 2020).
Alternatives to Antimicrobials
Because of the overuse of antimicrobial drugs, antimicrobial resistance becomes serious day by day. Therefore, there is an urgent need to find alternatives to antimicrobials. In this background, Shah et al. compared the effects of probiotics and antibiotics as the supplemental therapies of periodontal non-surgical treatment (Shah and Gujjari, 2017). They recruited 18 patients with aggressive periodontitis and divided them into 3 groups after SRP, which were given L. brevis CD2, L. brevis CD2 with doxycycline, or doxycycline alone for 14 days. PI, GI, PPD, CAL, and salivary levels of Lactobacillus and A. actinomycetemcomitans were measured at baseline, 14 days, 2 months, and 5 months. It was reported that GI in all the three groups was significantly improved at 5 months, and the intergroup results were also statistically significant. Besides, L. brevis CD2 showed a similar effect to doxycycline, but a synergistic effect was not detected when the probiotic and doxycycline were given simultaneously. It was concluded that L. brevis CD2 could be used as an alternative to antibiotics to treat aggressive periodontitis, without the risk of promoting antibiotic resistance.
The broad-spectrum bactericide CHX is widely used in dental clinical therapy. In a study comparing effects of CHX, probiotics, and herbs, 45 healthy volunteers were randomly divided into three groups and used CHX mouthwash, probiotic mouthwash, or herbal mouthwash for 14 days. The probiotic mouthwash contained Lactobacillus acidophilus, Lactobacillus rhamnosus, Bifidobacterium longum, Saccharomyces boulardii; the herbal mouthwash contained Belleric Myrobalan (Bibhitaki), Betel (Nagavalli), and Meswak (Salvadora Persica). PI, GI, and Oral Hygiene Index-Simplified (OHI-S) were collected on days 0, 7, and 14. The effects of all three types of mouthwash were demonstrated to be similar, and there were few side effects reported, suggesting that both probiotic mouthwash and herbal mouthwash are effective substitutes for CHX mouthwash (Deshmukh et al., 2017).
Periodontal Health-Promoting Probiotic Species and Their Regulatory Effects
The mechanisms of probiotics promoting periodontal health have not been fully elucidated. Nevertheless, a considerable amount of research results from clinical trials, animal experiments, and in vitro experiments have revealed that probiotics confer periodontal-health benefits upon the host by regulating periodontal microbiota or immune responses via various mechanisms (Figure 1). Specifically, regulatory effects of various periodontal health-promoting probiotics, which mainly belong to genera Lactobacillus, Bifidobacterium, Streptococcus, and Weissella, as well as the emerging recombinant probiotics, have been widely observed (Table 1). For the genera Lactobacillus and Streptococcus, probiotic species whose periodontal health-modulating effects were reported by at least three research articles in the past 5 years are chosen as the typical and important periodontal health-promoting probiotics in their genera to introduce here, as listed in Table 1.
Table 1.
The regulatory effects of known probiotic species promoting periodontal health.
| Genus/type | Species | Regulate immune responses | Regulate periodontal microbiota |
|---|---|---|---|
| Lactobacillus | Lactobacillus acidophilus |
|
|
| Lactobacillus brevis | Produce arginine deiminase to reduce the level of pro-inflammatory factors (TNF-α, IL-1β, IL-6, and IL-17) (animal experiment) (Maekawa and Hajishengallis, 2014) |
|
|
| Lactobacillus casei | Reduce the F. nucleatum-induced pro-inflammatory IL-6 production in oral epithelial cells (in vitro experiment) (Kang et al., 2011) |
|
|
| Lactobacillus fermentum | Reduce the F. nucleatum-induced pro-inflammatory IL-6 production in oral epithelial cells (in vitro experiment) (Kang et al., 2011) |
|
|
| Lactobacillus gasseri |
|
|
|
| Lactobacillus reuteri |
|
|
|
| Lactobacillus rhamnosus | Reduce the number of TRAP-positive cells and infiltrating inflammatory cells (animal experiment) (Gatej et al., 2018) |
|
|
| Lactobacillus salivarius | – |
|
|
| Lactobacillus johnsonii, Lactobacillus fructosum, Lactobacillus delbrueckii subsp. casei | – | Degrade A. actinomycetemcomitans biofilms by producing enzymes such as lipase (in vitro experiment) (Jaffar et al., 2016) | |
| Bifidobacterium | Bifidobacterium animalis subsp. lactis |
|
|
| Streptococcus | Streptococcus salivarius | Inhibit the expression of IL-6 and IL-8 induced by P. gingivalis, A. actinomycetemcomitans, and F. nucleatum in gingival fibroblasts (in vitro experiment) (Adam et al., 2011; MacDonald et al., 2021). |
|
| Streptococcus dentisani | Increase the secretion of IL-10 and decline the level of IFN-γ induced by F. nucleatum in HGF-1 (in vitro experiment) (Esteban-Fernandez et al., 2019) |
|
|
| Streptococcus cristatus | Reduce the F. nucleatum-induced pro-inflammatory IL-8 production in oral epithelial cells (in vitro experiment) (Zhang et al., 2008) |
|
|
| Streptococcus gordonii, Streptococcus sanguinis, Streptococcus mitis | – |
|
|
| Weissella | Weissella cibaria |
|
|
| Recombinant probiotics | Recombinant Lactobacillus paracasei | – | Express single-chain antibody fragments against RgpA gingipain to co-aggregate with P. gingivalis and kill it (in vitro experiment) (Marcotte et al., 2006) |
| Recombinant L. acidophilus | Express FomA to induce the production of antibodies against FomA protein and prevent the infection of F. nucleatum and its co-aggregated P. gingivalis (in vitro experiment) (Ma et al., 2013) | Present similar antibacterial activity and antibiotic sensitivity to the wild L. acidophilus, and its adhesive ability was improved (in vitro experiment) (Ma et al., 2018) |
GCF, gingival crevicular fluid; OPG, osteoprotegerin.
Lactobacillus
Lactobacillus is a type of gram-positive facultative anaerobic or obligate anaerobic bacteria that widely colonize the human digestive system, urinary system, and reproductive system. Probiotics derived from the genus Lactobacillus have been used in the prevention and treatment of numerous gastrointestinal tract disorders, urogenital diseases, vaginal infection, atopic disease, food hypersensitivity, and oral diseases like dental caries, periodontal diseases, and oral candida infection (Lebeer et al., 2008; Ishikawa et al., 2015; James et al., 2016). The genus Lactobacillus contributes the majority of the current known periodontal health-promoting probiotic species.
Lactobacillus acidophilus
The studies of periodontal health-promoting L. acidophilus are concentrated on in vitro experiments. L. acidophilus plays an important role in the inhibition of P. gingivalis growth in vitro and regulation of the interaction between P. gingivalis and gingival epithelial cells (GEC) (Zhao et al., 2011; Zhao et al., 2012; Zhao et al., 2019). L. acidophilus ATCC 4356 could offset the pro-inflammatory process induced by P. gingivalis ATCC 33277 at both protein and mRNA levels and could antagonize the regulatory effects of P. gingivalis on the proliferation and apoptosis of GEC in a dose-dependent manner (Zhao et al., 2012; Zhao et al., 2019). Recently, L acidophilus LA5 was observed to downregulate multiple virulence factors of P. gingivalis, such as the fimbriae encoding genes mfa1 and fimA in P. gingivalis ATCC 33277 and mfa1 in P. gingivalis W83, the gingipains encoding genes kgp and rgpA, and the quorum-sensing gene luxS in ATCC 33277 or W83 interacting with GECs (Ishikawa et al., 2020).
L. acidophilus ATCC 4356 also shows its universal regulatory effects on different F. nucleatum strains, via inhibiting the expression of virulence factors and the adhesion ability of F. nucleatum or reducing the levels of cytokines in oral epithelial cells stimulated by F. nucleatum. It is worth noting that live and heat-killed L. acidophilus ATCC 4356 have similar adhesion ability to KB and HOK cells, and both forms do not affect the viability of cells (Ding et al., 2021). The live L. acidophilus ATCC 4356 has been proved to decrease the production of IL-6 in KB cells activated by F. nucleatum ATCC 10953 (Kang et al., 2011). In a recent study, the heat-killed L. acidophilus ATCC 4356 was observed to downregulate the expression of IL-6/8 in KB and HOK cells activated by F. nucleatum ATCC 23726, co-aggregate with F. nucleatum ATCC 23726 and ATCC 25586, and inhibit the expression of their virulence factor fap2 involved in adhesion and invasion, thus interfering F. nucleatum self-aggregation and adhesion to epithelial cells, which is another way to inhibit F. nucleatum infecting oral epithelial cells in addition to competing for adhesion sites (Ding et al., 2021). The heat-killed L. acidophilus ATCC 4356 drew interest, as it could avoid drug resistance and dysbacteriosis and could be more safe (Ding et al., 2021).
It was reported that live L. acidophilus JCM1021 could degrade biofilms of A. actinomycetemcomitans Y4 (more than 90%), and SUNY75 and OMZ 534 (more than 50%) by lipase and other hydrolases (Jaffar et al., 2016). Ishikawa et al. further revealed part of the mechanisms in A. actinomycetemcomitans (serotype b, JP2 clone) biofilm degradation with cell-free pH-neutralized supernatants (CFS) of L. acidophilus LA5 and NCFM (Ishikawa et al., 2021). L. acidophilus LA5 CFS could reduce the number of planktonic bacteria, as well as biofilm biomass and viable counts in biofilm by releasing postbiotics, which can assist antibiotics in removing A. actinomycetemcomitans, as bacteria in biofilm are difficult to eliminate. Besides, L. acidophilus LA5 CFS could downregulate the expression of vital virulence factors leukocyte toxin (LtxA) and cytolethal distending toxin (CdtB) related to evading host defenses. Another strain, L. acidophilus NCFM CFS, could decrease biofilm biomass and viable counts in biofilm by postbiotics but downregulate the transcription of dspB, hindering its application to control periodontitis. Moreover, both L. acidophilus LA5 and NCFM downregulated katA, a gene encoding catalase, attenuating the resistance of oxidative stress of A. actinomycetemcomitans.
Lactobacillus reuteri
Many in vitro experiments proved the inhibitory effects of L. reuteri on periodontopathogens, which is probably attributed to its specific by-products, such as reuterin, which is a non-protein broad-spectrum antibiotic and could suppress the growth of many gram-positive/negative bacteria, yeast, and fungi (Stevens et al., 2011). L. reuteri ATCC PTA 5289 is a good inhibitor of many periodontopathogens, including P. gingivalis ATCC 33277, P. intermedia ATCC 25611, and F. nucleatum ATCC 25586, except for A. actinomycetemcomitans ATCC 33384 (Jansen et al., 2021). As for the forms of the probiotics, both live L. reuteri PTA 5289 and DSM 17938 and their CFS showed inhibition on P. gingivalis ATCC 33277 and F. nucleatum ATCC 25586, while only the live form of the two L. reuteri attenuated the growth of A. actinomycetemcomitans ATCC 29522 in vitro (Geraldo et al., 2020; Santos et al., 2020). Another subspecies, L. reuteri ATCC 55730, also inhibited the growth of F. nucleatum ATCC 10953, P. gingivalis ATCC 33277, and A. actinomycetemcomitans ATCC 33384 and protected HOK cells infected by periodontal pathogens from death (Moman et al., 2020). Besides, exopolysaccharide (EPS) produced by L. reuteri DSM 17938 benefits its adhesion to epithelial cells to compete with pathogenic bacteria for adhesion sites (Kšonžeková et al., 2016). In another in vitro experiment, L. reuteri KCTC 3594 was shown to inhibit the secretion of IL-6 induced by F. nucleatum in KB cells (Kang et al., 2011).
In clinical trials, application of L. reuteri inhibited P. gingivalis in saliva, supragingival plaque and subgingival plaque, and P. intermedia in saliva (Invernici et al., 2018). However, for peri-implant diseases, L. reuteri DSM 17938 and PTA 5289, could only reduce the load of P. gingivalis in patients with peri-implant mucositis (Galofré et al., 2018). In animal experiments, the live L. reuteri DSM 17938 and PTA 5289 could raise the hemocyte density in Galleria mellonella infected by P. gingivalis ATCC 33277, thereby upregulating immune responses (Geraldo et al., 2020; Santos et al., 2020). The clinical trials also proved the immunomodulatory effects of L. reuteri such as regulating the imbalance between MMP and TIMP (Ince et al., 2015) or reducing the production of pro-inflammatory cytokines (tumor necrosis factor-α (TNF-α), IL-1β, and IL-17) (Szkaradkiewicz et al., 2014), which could contribute to relieving inflammatory response and reducing periodontal tissues destruction.
Lactobacillus rhamnosus
In vitro experiments, L. rhamnosus could inhibit several vital periodontopathogens and downregulate the virulence factors about biofilm formation and immune escape in A. actinomycetemcomitans (Moman et al., 2020; Ishikawa et al., 2021). L. rhamnosus ATCC 53103 could inhibit the growth of F. nucleatum ATCC 10953, P. gingivalis ATCC 33277, and A. actinomycetemcomitans ATCC 33384 in vitro and could protect HOK cells infected by periodontal pathogens from death (Moman et al., 2020). L. rhamnosus Lr32 and HN001 CFS could reduce the biofilm biomass and viable counts in the biofilm of A. actinomycetemcomitans (serotype b, JP2 clone) by releasing postbiotics to facilitate antibiotics removing this pathogen (Ishikawa et al., 2021). Besides, L. rhamnosus Lr32 CFS could downregulate the expression of LtxA and CdtB to interfere with the process of evading host defenses. Both L. rhamnosus Lr32 and HN001 downregulated katA, damaging the resistance of oxidative stress of A. actinomycetemcomitans. However, it was observed that L. rhamnosus HN001 CFS upregulated the transcription of dspB to degrade EPS of the biofilm but raised the transcription of LtxA, thus hindering its application to control periodontitis (Ishikawa et al., 2021). L. rhamnosus could also regulate in vivo immune responses. L. rhamnosus GG reduced inflammatory cell, osteoclast, and TRAP-positive cell number in periodontal tissues in a mouse model of experimental periodontitis (Gatej et al., 2018).
Bifidobacterium
Bifidobacterium is a type of gram-positive anaerobic bacteria that could be found in the human intestines, vagina, oral cavity, and breast milk. Bifidobacterium probiotics have been proved to relieve multiple intestinal diseases such as irritable bowel syndrome and constipation (Agrawal et al., 2009) and inflammatory bowel disease (Kim et al., 2007), improve lactose intolerance (He et al., 2008), prevent infectious diarrhea (Qiao et al., 2002), and reduce incidence and duration of respiratory infections (Jungersen et al., 2014) and exhibit anticancer effects (You et al., 2004). They also play a role in controlling oral infectious diseases including periodontal diseases (Ricoldi et al., 2017) and oral candida infection (Ishikado et al., 2007).
Bifidobacterium animalis subsp. lactis
Recent studies have evaluated the effects of the B. animalis subsp. lactis (B. lactis) on periodontopathogens. In in vitro experiments, B. lactis ATCC 27673 antagonized the biofilm formation of F. nucleatum ATCC 25585 and P. gingivalis ATCC 33277 after co-incubating for 168 h, without interfering with the growth of Streptococcus oralis (Argandoña Valdez et al., 2021). B. lactis HN019 not only inhibits P. gingivalis W83, P. intermedia ATCC 25611, F. nucleatum ATCC 25586, and A. actinomycetemcomitans ATCC 33393 but also significantly reduces the adhesion of P. gingivalis W83 to buccal epithelial cells (Invernici et al., 2020). In animal experiments, B. lactis could also regulate the ratio between aerobic and anaerobic bacteria, as reported in the study of Ricoldi et al. (2017). Oliveira et al. had a consistent conclusion in their study since they found that the B. lactis HN019 treatment resulted in lower proportions of P. intermedia-like species in subgingival plaque of EP animals (Oliveira et al., 2017). In clinical trials, when B. lactis HN019 was taken for 30 days, P. gingivalis, Treponema denticola, and F. nucleatum vincentii were reduced markedly in deep periodontal pockets (≥7 mm) (Invernici et al., 2018). B. lactis BB-12 combined with L. rhamnosus GG could decrease F. nucleatum and A. actinomycetemcomitans in saliva and dental plaque as well as P. gingivalis in dental plaque, and the amounts of bacteria in saliva become lower (Alanzi et al., 2018).
B. lactis HN019 is observed to regulate immune responses in animal experiments and clinical trials. Oliveira et al. reported that the EP-B. lactis HN019 group presented higher levels of osteoprotegerin (OPG) and β-defensins as well as lower levels of IL-1β and receptor activator of nuclear factor-kappa B (NF-κB) ligand (RANKL) than the EP-only group (Oliveira et al., 2017). B. lactis HN019 application could markedly decrease the levels of IL-1β and the ratio of RANKL/OPG in rats with periodontitis and metabolic syndrome and could downregulate the expression of TNF-α and IL-6 in rats only with periodontitis (Silva et al., 2021). In clinical trials, when B. lactis HN019 was taken for 30 days, 4 weeks, or 15 days after SRP, the mean ratios between the levels of IL-1β or IL-6 and those at baseline in GCF were lower than those in groups without B. lactis HN019; fewer osteoclasts, increased expression of anti-inflammatory factors (IL-10 and TGF-β1), and reduced expression of IL-1β and cytokine-induced neutrophil chemoattractant (CINC) were also induced (Kuru et al., 2017; Ricoldi et al., 2017; Invernici et al., 2018). B. lactis HN019 treatment as adjuvant therapy of SRP for 30 days could obviously raise the expression of β-defensin-3, toll-like receptor 4 (TLR4), and cluster of differentiation (CD)-4 in gingiva (Invernici et al., 2020).
Streptococcus
Streptococcus is a type of gram-positive, aerobic to facultatively anaerobic bacteria that is a member of the normal flora of the human mouth and intestines. Some Streptococcus spp. are identified as sources of invasive infections in humans that range from subacute to acute or even chronic, while others have been proved their health benefits in improving digestive problems such as ulcerative colitis (Ohland and Macnaughton, 2010) and antibiotic-associated diarrhea (Correa et al., 2005), regulating immunity (Dargahi et al., 2020) and treating various oral diseases including dental caries (Di Pierro et al., 2015), periodontal diseases (López-López et al., 2017; Esteban-Fernandez et al., 2019), oral candida infection (Ishijima et al., 2012) and halitosis (Jamali et al., 2016).
Streptococcus salivarius
The regulatory effects of S. salivarius on many periodontopathogens have been observed in vitro experiments. S. salivarius M18 shows stable inhibition to common periodontopathogens, including P. gingivalis ATCC 33277, P. intermedia ATCC 25611, F. nucleatum ATCC 25586, and A. actinomycetemcomitans ATCC 33384 (Jansen et al., 2021). Another strain S. salivarius K12 shows distinct inhibitory effects on P. intermedia ATCC 25611, A. actinomycetemcomitans ATCC 33384, F. nucleatum ATCC 10953, and P. gingivalis ATCC 33277 (Moman et al., 2020; Jansen et al., 2021). S. salivarius K12 could raise the viability of HOK cells infected by P. gingivalis and F. nucleatum, thus increasing the defense capability of epithelium (Moman et al., 2020). Apart from M18 and K12, S. salivarius TOVE could cause 1.5% and 71.3% reduction of A. actinomycetemcomitans adhesion by pre-colonization of glass coverslips (Sliepen et al., 2008) or epithelial cells (Sliepen et al., 2009), as well as inhibiting the adhesion of P. gingivalis and P. intermedia (Van Hoogmoed et al., 2008).
S. salivarius probiotic strains are also found to regulate immune responses in vitro experiments. S. salivarius K12 and M18 could inhibit immune activation by periodontopathogens and reduce the levels of IL-6/8 in human gingival fibroblasts stimulated by A. actinomycetemcomitans, P. gingivalis, and F. nucleatum when S. salivarius is co-incubated with pathogens and fibroblasts simultaneously or S. salivarius is pretreated with fibroblasts before infection (Adam et al., 2011; MacDonald et al., 2021).
Weissella
Weissella is a type of gram-positive facultative anaerobes that are classified from the genus Lactobacillus and occur in a great variety of habitats, including human saliva, breast milk, intestines, feces, vagina, and skin. Among them, there are opportunistic pathogens as well as probiotic bacteria with beneficial effects such as antibacterial activities (Srionnual et al., 2007), antifungal activities (Quattrini et al., 2020), and immunoregulation (Lee et al., 2013). Certain probiotic Weissella such as Weissella cibaria strains have been shown to play a role in inhibiting dental caries, halitosis, and periodontal diseases (Kang et al., 2006a; Kang et al., 2006b; Jang et al., 2016; Do et al., 2019; Kim et al., 2020a).
Weissella cibaria
Some W. cibaria strains have shown strong antibacterial activities against periodontopathogens in vitro experiments. Kang et al. found that W. cibaria CMU, CMS2, and CMS3 co-aggregated most strongly with F. nucleatum, the proliferation of which was decreased by 5-log cycles as a result (Kang et al., 2006b). Jang et al. obtained a consistent result, as 95% P. gingivalis and F. nucleatum were inhibited because of co-aggregation with W. cibaria CMU (Jang et al., 2016). It can be inferred that co-aggregation with W. cibaria does not interfere with the colonization of periodontal pathogens but suppresses their growth. W. cibaria CFS was also found to be against pathogens, which is mainly related to acidic pH, the presence of hydroxyl, and the secretion of specific proteins with antimicrobial activities (Lim et al., 2018). Organic acids, including lactic acid, acetic acid, citric acid, fatty acids, and oleic acid, could interfere with the basic metabolism of the pathogens and inhibit the growth of P. gingivalis KCTC 5352, F. nucleatum KCTC 2488, and P. intermedia ATCC 25611. Besides, hydrogen peroxide (H2O2) in CFS could suppress P. gingivalis and P. intermedia, and W. cibaria CMU could produce the most H2O2 in commercial probiotics for oral healthcare (Lim et al., 2018). On the other hand, the bacteriocin-like compounds (BLCs) of CFS, N-acetylmuramidase, were only against the P. gingivalis effectively by binding to cell walls and causing lysis (Lim et al., 2018). In animal experiments, the application of W. cibaria significantly lowered the amount of plaque; the level of F. nucleatum, P. gingivalis, P. intermedia, and T. forsythia in the oral cavity; and the level of P. gingivalis in gingival tissues (Do et al., 2019; Kim et al., 2020a). A recent clinical trial indicated that taking W. cibaria CMU for 8 weeks significantly reduced F. nucleatum in GCF (Kang et al., 2020), corresponding to its strong co-aggregation ability with F. nucleatum in vitro (Kang et al., 2006b).
W. cibaria was also observed to regulate the inflammatory response in vitro experiments. W. cibaria CMU could reduce the production of IL-6 and IL-8 in KB cells activated by F. nucleatum, as well as the cell attachment of F. nucleatum, while the viability and co-aggregation of W. cibaria CMU may not play an essential role in this process (Kang et al., 2011). The anti-inflammatory activity of W. cibaria CMU is related to inhibiting NF-κB activation in response to periodontopathogen stimulation and NO production. In RAW 264.7 macrophages stimulated by formalin-inactivated A. actinomycetemcomitans ATCC 3338, W. cibaria CMU downregulated the expression of inducible NO synthase (iNOS) and the mRNA of IL-1β and IL-6 to reduce NO production. The inhibition of NF-κB inhibitor α (IκBα) kinase (IKK) phosphorylation, IκBα degradation, and the nuclear translocation of p65 were also observed in W. cibaria CMU-treated RAW 264.7 macrophages (Kim et al., 2020b). In animal models, W. cibaria CMU decreased the level of both pro-inflammatory (TNF-α, IL-1β, and IL-6) and anti-inflammatory (IL-10) cytokines (Kim et al., 2020a).
Recombinant Probiotics
In addition to the application of conventional forms, such as the live, heat-killed, freeze-dried probiotics and the probiotics CFS, recombinant probiotics produced by genetic engineering could express more diverse antibacterial substances and present an enhanced antibacterial activity. A recombinant Lactobacillus paracasei strain was constructed by Marcotte et al. to express single-chain antibody fragments (scFv) against RgpA gingipain, a virulence factor of P. gingivalis, to co-aggregate with P. gingivalis; the antibacterial activity of L. paracasei was not damaged. It is worth mentioning that co-aggregation may facilitate the colonization of P. gingivalis via L. paracasei adhesion, but the pathogen may be killed by the locally high concentration of antibacterial substances secreted by L. paracasei (Marcotte et al., 2006). In 2013, Ma et al. reported a recombinant L. acidophilus, some wild strains of which have shown periodontal beneficial characteristics, expressing F. nucleatum outer membrane protein FomA. The recombinant L. acidophilus strain could stimulate the antibodies against FomA protein to prevent the infection of F. nucleatum and its co-aggregated pathogens such as P. gingivalis in periodontal tissues (Ma et al., 2013). Animal studies proved that oral administration of the recombinant L. acidophilus reduced the infection by F. nucleatum and P. gingivalis (Ma et al., 2013). Particularly, the recombinant L. acidophilus presents a similar antibacterial activity and antibiotic sensitivity to the wild L. acidophilus, and its adhesive ability is further improved (Ma et al., 2018). In these studies, the genome of parent probiotics is modified by genetic engineering techniques to construct recombinant strains of probiotic with new genetic characteristics, providing a new idea for the development and application of probiotics.
Issues in Current Application of Periodontal Health-Related Probiotics
Effectiveness
Although a multitude of studies have suggested that probiotics are beneficial to periodontal health, the effectiveness of probiotics in managing periodontal disease and health is still controversial. Even in studies that used the same probiotic bacteria, the observed improvements in clinical measurements, inflammation, and microbiota related to periodontal diseases are not consistent. The causes of the conflicting observations and conclusions on the effectiveness of probiotics in different periodontal-health research are complicated and diverse.
Multiple factors are considered to affect the results of probiotic research, such as probiotic species or strains, administration dosage or modes, sample size, the combination of different probiotics, and reaction time. In a randomized controlled clinical trial of Laleman et al. (2015), 48 periodontitis patients were included, divided evenly into two groups after SRP (baseline), and then given either a placebo or a probiotic tablet containing S. oralis KJ3, Streptococcus uberis KJ2, and Streptococcus rattus JH145 twice a day for 12 weeks. No significant difference in clinical indices including PPD, BOP, and CAL could be detected between the probiotic group and the control group at the baseline, 12-week, or 24-week time points. Nevertheless, a post hoc power analysis conducted by them revealed that eight times more patients were needed to show a statistically significant intergroup difference for PPD at 12 weeks. The results of the study indicate that sample size is a non-negligible factor that affects the observations of probiotic studies. In addition, for different probiotic strains, the effective dose and the best application mode should be considered first when studying the effects of probiotics in modulating periodontal health. Inappropriate dose or mode in applying probiotics may result in the failure in obtaining expected outcomes and correct conclusions. However, the problem is that up to now, there are not enough references to determine effective dose and application mode for numerous probiotic strains. As for the combination of probiotics, L. reuteri DSM 17938 could regulate L. reuteri ATCC PTA 5289 to stabilize its antibacterial activity (Jansen et al., 2021). The antibacterial activity of P. gingivalis is related to the double or triple combination of B. longum, B. lactis, and Bifidobacterium infantis. The growth of P. gingivalis was inhibited by 41.8% with exposure to B. longum with B. lactis and 50.1% to triple combination (Argandoña Valdez et al., 2021). Besides, reaction time is another factor, as 11.3% F. nucleatum was shown to be suppressed at 24 h after exposure to probiotics, and growth inhibition rates rose to 18.4%–51.6% until 72 h (Argandoña Valdez et al., 2021). Thus, the combination manner of probiotics and action time also affect the effectiveness of judgment. Consequently, sometimes, it is difficult for researchers to scientifically assess the effectiveness of probiotics.
Experimental design and evaluation indices selected of a study also have an important impact on the understanding of probiotic effectiveness. For example, in some studies, it is concluded that probiotic treatment was not able to significantly improve the clinical symptoms of periodontal diseases, which may be partly attributed to the inappropriate selection of evaluation indices. As observed by Montero et al. in a study evaluating the efficacy of the adjunctive use of probiotics on gingivitis (Montero et al., 2017), gingivitis subjects were recruited and administered with tablets containing placebo or the probiotic combination of Lactobacillus plantarum, L. brevis, and Pediococcus acidilactici for 6 weeks. Their results showed no significant differences in the average GI between the placebo and probiotic groups. When focusing on the change in the number of sites with higher GI scores (GI = 3 at baseline), a significantly higher reduction was observed in the probiotic group. In other words, the average GI may be not the optimum evaluation index for probiotic intervention in the study, because the improvement effect of probiotics on sites with severe inflammation was diluted by other sites when calculating the mean value of GI.
Sometimes, it is reported that although the clinical parameters are improved by probiotics, periodontal microbiota and related inflammatory factors do not show detectable differences. Keller et al. found that after treating moderate-gingivitis patients with tablets containing a mix of L. rhamnosus PB01, DSM 14869 and Lactobacillus curvatus EB10, and DSM 32307 for 4 weeks, BOP and GCF volume were obviously improved, while all the selected cytokines (IL-1β, IL-6, IL-8, IL-10, and TNF-α) in GCF and the salivary microbiome were unaffected by the intervention (Keller et al., 2017). The researchers speculated that cytokine concentrations in GCF of some samples were lower than the detectable levels and thus could not be analyzed and evaluated. In addition, subgingival plaques were not collected in the study for microbial diversity and abundance analysis, which may be one of the reasons for not observing microbial alterations.
What is particularly noteworthy is that a recent study on intestinal colonization by probiotics suggested that the effectiveness of probiotics might vary from person to person. Through using endoscopy to collect flora at multiple intestine sites to analyze the flora composition of volunteers who were given probiotic supplements, Zmora et al. found that humans featured person-, region-, and strain-specific mucosal colonization patterns of probiotics, hallmarked by predictive pretreatment microbiome and host features (Zmora et al., 2018). Consequently, probiotic interventions are likely to exert differential influences on different individuals, which is thought to possibly explain the high variability in probiotic effects on the host or gut microbiome observed in different studies. Since periodontal diseases are related to original periodontal microbiota and host immunity, differential colonization resistance and responsiveness of individuals to probiotics may also exist and impact the research results observed with probiotic use in periodontal diseases.
Safety
With the deepening of probiotic research and the recognition of more potential probiotic species and strains, there has been growing concern about the safety of probiotics, in particular, when applied to humans with the purpose of managing diseases and improving health. In fact, there are some studies reporting that probiotics have limited benefits to the body and may even be harmful to health (De Groote et al., 2005; Doron and Snydman, 2015). It has been recommended by the WHO/FAO working group to conduct a series of safety assessments of probiotics including antibiotic resistance, toxin production, potential hemolysis, metabolic activities, and side effects in humans and post-market surveillance of commercial consumers (Araya et al., 2002). Classical probiotics such as some Lactobacillus and Bifidobacterium species that have a long history of use in fermented foods or dairy products are generally recognized as safe (Kang et al., 2019). However, there are no adequate systematic safety studies, and indeed, complications of probiotic use occur sometimes. Some studies have revealed that treatment with probiotics caused bacteremia, including the most commonly used Lactobacillus spp. (De Groote et al., 2005). Despite no existing evidence of the occurrence of bacteremia induced by probiotic use in periodontal therapy or care, people with damaged periodontal tissues or tooth bleeding after SRP seem to be susceptible to bacterial invasion, and therefore such a possibility could not be ruled out.
The application of probiotics may have unexpected impacts on host immune responses and microecology. Recently, Suez et al. (2018) evaluating the probiotic impact on post-antibiotic reconstitution of the intestinal host–microbiome homeostasis showed that antibiotic treatment enhanced human gut mucosal colonization by probiotics, and more importantly, compared to spontaneous post-antibiotic recovery, probiotics significantly delayed rather than aided in gut microbiome and host transcriptome reconstitution. It was noticed that probiotic presence led to elevated transcription levels of certain inflammatory mediators and antimicrobial peptides, which may affect the restoration of the original intestinal flora. In many probiotic-periodontal disease studies, probiotics were attempted to be used as adjuvant therapy after non-surgical periodontal therapy. However, it is reminded by this study that probiotic use may influence or even interfere with periodontal microbiome recolonization and restoration of periodontal microecological balance after removal of dental plaques by periodontal non-surgical treatment.
Collectively, these findings suggest that studies on periodontal health-promoting probiotics need to focus more on the safety in use, although there are few relevant adverse events reported. Just as the effects of probiotics depend on strain traits, each probiotic strain would be anticipated to have a different safety profile. Thus, it is quite essential to verify the identities, phenotypic characteristics, and non-pathogenicity of different probiotics for safe use in humans (Kang et al., 2019). Furthermore, it is proposed that perhaps the safety of a commercially available probiotic product depends not only on the probiotic organism but also on the other constituents of the product, whether in food or medicinal formulation (Doron and Snydman, 2015). This highlights the importance of systematic and persistent assessment of probiotic products by researchers in the overall process of probiotic research, development, and application.
Concluding Remarks and Future Perspectives
The emergence of probiotics provides more options for the prevention and treatment of periodontal diseases. Different from antibiotics and bactericides that are widely used in clinical practice, probiotics generally play a role in periodontal therapy and healthcare through regulating host immune function and restoring the balance of periodontal microecology. Consequently, probiotics have unique advantages and considerable potential in application to maintain periodontal health.
Different probiotic species exert their periodontal health-regulatory effects through diverse mechanisms such as competition for adhesion sites to epithelial cells, antagonism against growth, biofilm formation and virulence expression of periodontopathogens, and influence on host immune responses. Currently, the majority of known periodontal health-promoting probiotics is derived from the classical probiotic genera Lactobacillus and Bifidobacterium and seems to be more effective and safe when applied in human health management. Nevertheless, taking account of the controversy on effectiveness and concerns on safety, these probiotics, as well as probiotics derived from other genera or remolded by genetic engineering techniques, need more investigation to support their role in periodontal therapy and care.
The studies on probiotic use in the intestine have highlighted a need for developing personalized probiotic approaches according to the host individual’s flora and immune status so that probiotics could better colonize and play a more effective role in promoting health. In order to ensure universal and persistent efficacy, such a personalized strategy should also be considered and developed when applying probiotics in the prevention and treatment of periodontal diseases. Furthermore, a diverse combination of different probiotic species and probiotic strains is probably one of the major development directions for probiotic application, which may provide combinational or synergistic effects on regulating host microbiota and immunity, especially when considering the high complexity of subgingival plaques and the presence of various oral environmental stress factors. Genetic engineering would provide more ideas and possibilities for probiotic research and development. The probiotic function could be further enhanced and improved by directional genetic modifications on existing probiotics that strengthen or remold their immunoregulation capabilities, antimicrobial activities against periodontopathogens, adaptive capacities to the oral environment, etc.
Author Contributions
YZ and QG conceptualized the review. YZ drafted the manuscript, and QG edited the manuscript, with YD providing critical revisions. All authors contributed significantly and read and approved the final manuscript.
Funding
This work was supported by grants from the Youth Science Fund Project of the National Natural Science Foundation of China (No. 81500842) and the Science and Technology Department of Sichuan Province (No. 2021YJ0133).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Adam E., Jindal M., Seney S., Summers K., Hamilton D., Hatibović-Kofman S., et al. (2011). Streptococcus Salivarius K12 and M18 Probiotics Reduce Periodontal Pathogen-Induced Inflammation. In: IADR General Session 2011. (San Diego, California, United States: ) [Google Scholar]
- Agrawal A., Houghton L. A., Morris J., Reilly B., Guyonnet D., Goupil Feuillerat N., et al. (2009). Clinical Trial: The Effects of a Fermented Milk Product Containing Bifidobacterium Lactis DN-173 010 on Abdominal Distension and Gastrointestinal Transit in Irritable Bowel Syndrome With Constipation. Aliment. Pharmacol. Ther. 29, 104–114. doi: 10.1111/j.1365-2036.2008.03853.x [DOI] [PubMed] [Google Scholar]
- Alanzi A., Honkala S., Honkala E., Varghese A., Tolvanen M., Söderling E. (2018). Effect of Lactobacillus Rhamnosus and Bifidobacterium Lactis on Gingival Health, Dental Plaque, and Periodontopathogens in Adolescents: A Randomised Placebo-Controlled Clinical Trial. Benef Microbes 9, 593–602. doi: 10.3920/BM2017.0139 [DOI] [PubMed] [Google Scholar]
- Alkaya B., Laleman I., Keceli S., Ozcelik O., Cenk H. M., Teughels W. (2016). Clinical Effects of Probiotics Containing Bacillus Species on Gingivitis: A Pilot Randomized Controlled Trial. J. Periodontal Res. 52 (3), 497–504. doi: 10.1111/jre.12415. [DOI] [PubMed] [Google Scholar]
- Allaker R. P., Stephen A. S. (2017). Use of Probiotics and Oral Health. Curr. Oral. Health Rep. 4, 309–318. doi: 10.1007/s40496-017-0159-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amizic I. P., Cigić L., Gavić L., Radić M., Barišić I. G. (2017). Antimicrobial Efficacy of Probiotic-Containing Toothpastes: An In Vitro Evaluation. Med. Glas. 14, 139–144. doi: 10.17392/870-16 [DOI] [PubMed] [Google Scholar]
- Araya M., Morelli L., Reid G., Sanders M., Stanton C., Pineiro M., et al. (2002). “Guidelines for the Evaluation of Probiotics in Food,” Joint FAO/WHO Working Group Report. (London Ontario, Canada: ), 1–11. [Google Scholar]
- Argandoña Valdez R. M., Ximenez-Fyvie L. A., Caiaffa K. S., Rodrigues Dos Santos V., Gonzales Cervantes R. M., Almaguer-Flores A., et al. (2021). Antagonist Effect of Probiotic Bifidobacteria on Biofilms of Pathogens Associated With Periodontal Disease. Microb. Pathog. 150, 104657. doi: 10.1016/j.micpath.2020.104657 [DOI] [PubMed] [Google Scholar]
- Chen M. X., Zhong Y. J., Dong Q. Q., Wong H. M., Wen Y. F. (2021). Global, Regional, and National Burden of Severe Periodontitis 1990-2019: An Analysis of the Global Burden of Disease Study 2019. J. Clin. Periodontol. 48 (9), 1165–1188. doi: 10.1111/jcpe.13506 [DOI] [PubMed] [Google Scholar]
- Correa N. B. O., Peret L. A., Penna F. J., Lima R., Nicoli J. R. (2005). A Randomized Formula Controlled Trial of Bifidobacterium Lactis and Streptococcus Thermophilus for Prevention of Antibiotic-Associated Diarrhea in Infants. J. Clin. Gastroenterol. 39, 385–389. doi: 10.1097/01.mcg.0000159217.47419.5b [DOI] [PubMed] [Google Scholar]
- Dargahi N., Johnson J., Apostolopoulos V. (2020). Streptococcus Thermophilus Alters the Expression of Genes Associated With Innate and Adaptive Immunity in Human Peripheral Blood Mononuclear Cells. PloS One 15 (2), e0228531. doi: 10.1371/journal.pone.0228531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Groote M. A., Frank D. N., Dowell E., Glode M. P., Pace N. R. (2005). Lactobacillus Rhamnosus GG Bacteremia Associated With Probiotic Use in a Child With Short Gut Syndrome. Pediatr. Infect. Dis. J. 24, 278. doi: 10.1097/01.inf.0000154588.79356.e6 [DOI] [PubMed] [Google Scholar]
- Deshmukh M. A., Dodamani A. S., Karibasappa G., Khairnar M. R., Naik R. G., Jadhav H. C. (2017). Comparative Evaluation of the Efficacy of Probiotic, Herbal and Chlorhexidine Mouthwash on Gingival Health: A Randomized Clinical Trial. J. Clin. Diagn. Res. 11, ZC13. doi: 10.7860/JCDR/2017/23891.9462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Q., Sun X., Cao S., Zhao C., Wang Y., Wang X. (2021). Heat-Killed Lactobacillus Acidophilus Mediates Fusobacterium Nucleatum Induced Pro-Inflammatory Responses in Epithelial Cells. FEMS Microbiol. Lett. 368 (5), fnaa160. doi: 10.1093/femsle/fnaa160 [DOI] [PubMed] [Google Scholar]
- Di Pierro F., Zanvit A., Nobili P., Risso P., Fornaini C. (2015). Cariogram Outcome After 90 Days of Oral Treatment With Streptococcus Salivarius M18 in Children at High Risk for Dental Caries: Results of a Randomized, Controlled Study. Clin. Cosmet. Investig. Dent. 7, 107–113. doi: 10.2147/CCIDE.S93066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do K.-H., Park H.-E., Kang M., Kim J.-T., Yeu J.-E., Lee W.-K. (2019). Effects of Weissella Cibaria CMU on Halitosis and Calculus, Plaque, and Gingivitis Indices in Beagles. J. Vet. Dent. 36 (2), 135–142. doi: 10.1177/0898756419872562 [DOI] [PubMed] [Google Scholar]
- Doron S., Snydman D. R. (2015). Risk and Safety of Probiotics. Clin. Infect. Dis. 60 Suppl 2, S129–S134. doi: 10.1093/cid/civ085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteban-Fernandez A., Ferrer M. D., Zorraquin-Pena I., Lopez-Lopez A., Moreno-Arribas M. V., Mira A. (2019). In Vitro Beneficial Effects of Streptococcus Dentisani as Potential Oral Probiotic for Periodontal Diseases. J. Periodontol. 90, 1346–1355. doi: 10.1002/JPER.18-0751 [DOI] [PubMed] [Google Scholar]
- Flichy-Fernández A. J., Ata-Ali J., Alegre-Domingo T., Candel-Martí E., Ata-Ali F., Palacio J. R., et al. (2015). The Effect of Orally Administered Probiotic Lactobacillus Reuteri-Containing Tablets in Peri-Implant Mucositis: A Double-Blind Randomized Controlled Trial. J. Periodontal Res. 50, 775–785. doi: 10.1111/jre.12264 [DOI] [PubMed] [Google Scholar]
- Galofré M., Palao D., Vicario M., Nart J., Violant D. (2018). Clinical and Microbiological Evaluation of the Effect of Lactobacillus Reuteri in the Treatment of Mucositis and Peri-Implantitis: A Triple-Blind Randomized Clinical Trial. J. Periodontal Res. 53, 378–390. doi: 10.1111/jre.12523 [DOI] [PubMed] [Google Scholar]
- Gatej S. M., Marino V., Bright R., Fitzsimmons T. R., Gully N., Zilm P., et al. (2018). Probiotic Lactobacillus Rhamnosus GG Prevents Alveolar Bone Loss in a Mouse Model of Experimental Periodontitis. J. Clin. Periodontol. 45 (2), 204–212. doi: 10.1111/jcpe.12838 [DOI] [PubMed] [Google Scholar]
- Geraldo B. M. C., Batalha M. N., Milhan N. V. M., Rossoni R. D., Scorzoni L., Anbinder A. L. (2020). Heat-Killed Lactobacillus Reuteri and Cell-Free Culture Supernatant Have Similar Effects to Viable Probiotics During Interaction With Porphyromonas Gingivalis. J. Periodontal Res. 55, 215–220. doi: 10.1111/jre.12704 [DOI] [PubMed] [Google Scholar]
- Hajishengallis G. (2015). Periodontitis: From Microbial Immune Subversion to Systemic Inflammation. Nat. Rev. Immunol. 15, 30–44. doi: 10.1038/nri3785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajishengallis G., Darveau R. P., Curtis M. A. (2012). The Keystone-Pathogen Hypothesis. Nat. Rev. Microbiol. 10, 717–725. doi: 10.1038/nrmicro2873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajishengallis G., Lamont R. J. (2012). Beyond the Red Complex and Into More Complexity: The Polymicrobial Synergy and Dysbiosis (PSD) Model of Periodontal Disease Etiology. Mol. Oral. Microbiol. 27, 409–419. doi: 10.1111/j.2041-1014.2012.00663.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- He T., Priebe M. G., Zhong Y., Huang C., Harmsen H. J., Raangs G. C., et al. (2008). Effects of Yogurt and Bifidobacteria Supplementation on the Colonic Microbiota in Lactose-Intolerant Subjects. J. Appl. Microbiol. 104, 595–604. doi: 10.1111/j.1365-2672.2007.03579.x [DOI] [PubMed] [Google Scholar]
- Hill C., Guarner F., Reid G., Gibson G. R., Merenstein D. J., Pot B., et al. (2014). Expert Consensus Document. The International Scientific Association for Probiotics and Prebiotics Consensus Statement on the Scope and Appropriate Use of the Term Probiotic. Nat. Rev. Gastroenterol. Hepatol. 11, 506–514. doi: 10.1038/nrgastro.2014.66 [DOI] [PubMed] [Google Scholar]
- Imran F., Das S., Padmanabhan S., Rao R., Suresh A., Bharath D. (2015). Evaluation of the Efficacy of a Probiotic Drink Containing Lactobacillus Casei on the Levels of Periodontopathic Bacteria in Periodontitis: A Clinico-Microbiologic Study. Indian J. Dental Res. 26, 462. doi: 10.4103/0970-9290.172033 [DOI] [PubMed] [Google Scholar]
- Ince G., Gursoy H., Ipci S. D., Cakar G., Emekli-Alturfan E., Yilmaz S. (2015). Clinical and Biochemical Evaluation of Lozenges Containing Lactobacillus Reuteri as an Adjunct to Non-Surgical Periodontal Therapy in Chronic Periodontitis. J. Periodontol. 86, 746–754. doi: 10.1902/jop.2015.140612 [DOI] [PubMed] [Google Scholar]
- Invernici M. M., Furlaneto F., Salvador S. L., Ouwehand A. C., Salminen S., Mantziari A., et al. (2020). Bifidobacterium Animalis Subsp Lactis HN019 Presents Antimicrobial Potential Against Periodontopathogens and Modulates the Immunological Response of Oral Mucosa in Periodontitis Patients. PloS One 15, e0238425. doi: 10.1371/journal.pone.0238425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Invernici M. M., Salvador S. L., Silva P. H. F., Soares M. S. M., Casarin R., Palioto D. B., et al. (2018). Effects of Bifidobacterium Probiotic on the Treatment of Chronic Periodontitis: A Randomized Clinical Trial. J. Clin. Periodontol. 45, 1198–1210. doi: 10.1111/jcpe.12995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishijima S. A., Hayama K., Burton J. P., Reid G., Okada M., Matsushita Y., et al. (2012). Effect of Streptococcus Salivarius K12 on the In Vitro Growth of Candida Albicans and Its Protective Effect in an Oral Candidiasis Model. Appl. Environ. Microbiol. 78, 2190–2199. doi: 10.1128/AEM.07055-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikado A., Suido H., Sato T., Makino T. Preventive/therapeutic Agent for Diseases Associated With Candida Infection, Such as Allergy, Atopic Dermatitis, Periodontal Disease, Comprises Bifidobacterium Fermented Product of Plant Chosen From Brassicaceae Plant and Carrot, WO2007086573-A1 WOJP051465 30 Jan 2007 JP2007556044-X JP556044 30 Jan 2007 JP5328158-B2 JP556044 30 Jan 2007. [Google Scholar]
- Ishikawa K. H., Bueno M. R., Kawamoto D., Simionato M. R. L., Mayer M. P. A. (2021). Lactobacilli Postbiotics Reduce Biofilm Formation and Alter Transcription of Virulence Genes of Aggregatibacter Actinomycetemcomitans. Mol. Oral. Microbiol. 36, 92–102. doi: 10.1111/omi.12330 [DOI] [PubMed] [Google Scholar]
- Ishikawa K. H., Mayer M. P., Miyazima T. Y., Matsubara V. H., Silva E. G., Paula C. R., et al. (2015). A Multispecies Probiotic Reduces Oral Candida Colonization in Denture Wearers. J. Prosthodont. Implant Esthet. Reconstr. Dent. 24, 194–199. doi: 10.1111/jopr.12198 [DOI] [PubMed] [Google Scholar]
- Ishikawa K. H., Mita D., Kawamoto D., Nicoli J. R., Albuquerque-Souza E., Lorenzetti Simionato M. R., et al. (2020). Probiotics Alter Biofilm Formation and the Transcription of Porphyromonas Gingivalis Virulence-Associated Genes. J. Oral. Microbiol. 12, 1805553. doi: 10.1080/20002297.2020.1805553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffar N., Ishikawa Y., Mizuno K., Okinaga T., Maeda T. (2016). Mature Biofilm Degradation by Potential Probiotics: Aggregatibacter Actinomycetemcomitansversuslactobacillusspp. PloS One 11, e0159466. doi: 10.1371/journal.pone.0159466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamali Z., Aminabadi N. A., Samiei M., Deljavan A. S., Shokravi M., Shirazi S. (2016). Impact of Chlorhexidine Pretreatment Followed by Probiotic Streptococcus Salivarius Strain K12 on Halitosis in Children: A Randomised Controlled Clinical Trial. Oral. Health Prev. Dent. 14, 305–313. doi: 10.3290/j.ohpd.a36521 [DOI] [PubMed] [Google Scholar]
- James K. M., Macdonald K. W., Chanyi R. M., Cadieux P. A., Burton J. P. (2016). Inhibition of Candida Albicans Biofilm Formation and Modulation of Gene Expression by Probiotic Cells and Supernatant. J. Med. Microbiol. 65, 328. doi: 10.1099/jmm.0.000226 [DOI] [PubMed] [Google Scholar]
- Jang H. J., Kang M. S., Yi S. H., Hong J. Y., Hong S. P. (2016). Comparative Study on the Characteristics of Weissella Cibaria CMU and Probiotic Strains for Oral Care. Molecules 21 (12), 1752. doi: 10.3390/molecules21121752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen P. M., Abdelbary M. M. H., Conrads G. (2021). A Concerted Probiotic Activity to Inhibit Periodontitis-Associated Bacteria. PloS One 16, e0248308. doi: 10.1371/journal.pone.0248308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungersen M., Wind A., Johansen E., Christensen J. E., Stuer-Lauridsen B., Eskesen D. (2014). The Science Behind the Probiotic Strain Bifidobacterium Animalis Subsp. Lactis BB-12((R)). Microorganisms 2, 92–110. doi: 10.3390/microorganisms2020092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahouli I., Malhotra M., Alaouijamali M., Prakash S. (2015). In-Vitro Characterization of the Anti-Cancer Activity of the Probiotic Bacterium Lactobacillus Fermentum NCIMB 5221 and Potential Against Colorectal Cancer. J. Cancer Sci. Ther. 07 (7). doi: 10.4172/1948-5956.1000354 [DOI] [Google Scholar]
- Kang M. S., Chung J., Kim S. M., Yang K. H., Oh J. S. (2006. a). Effect of Weissella Cibaria Isolates on the Formation of Streptococcus Mutans Biofilm. Caries Res. 40, 418–425. doi: 10.1159/000094288 [DOI] [PubMed] [Google Scholar]
- Kang M. S., Kim B. G., Chung J., Lee H. C., Oh J. S. (2006. b). Inhibitory Effect of Weissella Cibaria Isolates on the Production of Volatile Sulphur Compounds. J. Clin. Periodontol. 33, 226–232. doi: 10.1111/j.1600-051X.2006.00893.x [DOI] [PubMed] [Google Scholar]
- Kang M. S., Lee D. S., Lee S. A., Kim M. S., Nam S. H. (2020). Effects of Probiotic Bacterium Weissella Cibaria CMU on Periodontal Health and Microbiota: A Randomised, Double-Blind, Placebo-Controlled Trial. BMC Oral. Health 20, 243. doi: 10.1186/s12903-020-01231-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang M., Lim H.-S., Kim S.-M., Lee H., Oh J.-S. (2011). Effect of Weissella Cibaria on Fusobacterium Nucleatum -Induced Interleukin-6 and Interleukin-8 Production in KB Cells. J. Bacteriol. Virol. 41, 9. doi: 10.4167/jbv.2011.41.1.9 [DOI] [Google Scholar]
- Kang M., Yeu, Hong (2019). Safety Evaluation of Oral Care Probiotics Weissella Cibaria CMU and CMS1 by Phenotypic |and Genotypic Analysis. Int. J. Mol. Sci. 20, 2693. doi: 10.3390/ijms20112693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang J. H., Yun S. I., Park M. H., Park J. H., Jeong S. Y., Park H. O. (2013). Anti-Obesity Effect of Lactobacillus Gasseri BNR17 in High-Sucrose Diet-Induced Obese Mice. PloS One 8, e54617. doi: 10.1371/journal.pone.0054617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller M. K., Brandsborg E., Holmstrøm K., Twetman S. (2017). Effect of Tablets Containing Probiotic Candidate Strains on Gingival Inflammation and Composition of the Salivary Microbiome: A Randomised Controlled Trial. Benef. Microbes. 9 (3), 487–494. doi: 10.3920/BM2017.0104 [DOI] [PubMed] [Google Scholar]
- Kim J. W., Jung B. H., Lee J. H., Yoo K. Y., Lee H., Kang M. S., et al. (2020. a). Effect of Weissella Cibaria on the Reduction of Periodontal Tissue Destruction in Mice. J. Periodontol. 91 (10), 1367–1374. doi: 10.1002/JPER.19-0288 [DOI] [PubMed] [Google Scholar]
- Kim N., Kunisawa J., Kweon M. N., Eog Ji G., Kiyono H. (2007). Oral Feeding of Bifidobacterium Bifidum (BGN4) Prevents CD4(+) CD45RB(high) T Cell-Mediated Inflammatory Bowel Disease by Inhibition of Disordered T Cell Activation. Clin. Immunol. 123, 30–39. doi: 10.1016/j.clim.2006.11.005 [DOI] [PubMed] [Google Scholar]
- Kim M. J., You Y. O., Kang J. Y., Kim H. J., Kang M. S. (2020. b). Weissella Cibaria CMU Exerts an Anti−Inflammatory Effect by Inhibiting Aggregatibacter Actinomycetemcomitans−Induced Nf−κb Activation in Macrophages. Mol. Med. Rep. 22, 4143–4150. doi: 10.3892/mmr.2020.11512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi R., Kobayashi T., Sakai F., Hosoya T., Yamamoto M., Kurita-Ochiai T. (2017). Oral Administration of Lactobacillus Gasseri SBT2055 is Effective in Preventing Porphyromonas Gingivalis-Accelerated Periodontal Disease. Sci. Rep. 7 (1), 545. doi: 10.1038/s41598-017-00623-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kšonžeková P., Bystrický P., Vlčková S., Pätoprstý V., Pulzová L., Mudroňová D., et al. (2016). Exopolysaccharides of Lactobacillus Reuteri: Their Influence on Adherence of E. Coli to Epithelial Cells and Inflammatory Response. Carbohydr. Polym. 141, 10–19. doi: 10.1016/j.carbpol.2015.12.037 [DOI] [PubMed] [Google Scholar]
- Kumar P. S., Griffen A. L., Moeschberger M. L., Leys E. J. (2005). Identification of Candidate Periodontal Pathogens and Beneficial Species by Quantitative 16s Clonal Analysis. J. Clin. Microbiol. 43, 3944–3955. doi: 10.1128/JCM.43.8.3944-3955.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Madurantakam P. (2017). Limited Evidence Shows Short-Term Benefit of Probiotics When Used as an Adjunct to Scaling and Root Planing in the Treatment of Chronic Periodontitis. Evid. Based Dent. 18, 109–110. doi: 10.1038/sj.ebd.6401270 [DOI] [PubMed] [Google Scholar]
- Kuru B. E., Laleman I., Yalnızoğlu T., Kuru L., Teughels W. (2017). The Influence of a Bifidobacterium Animalis Probiotic on Gingival Health: A Randomized Controlled Clinical Trial. J. Periodontol. 88, 1115–1123. doi: 10.1902/jop.2017.170213 [DOI] [PubMed] [Google Scholar]
- Laleman I., Pauwels M., Quirynen M., Teughels W. (2020). The Usage of a Lactobacilli Probiotic in the non-Surgical Therapy of Peri-Implantitis: A Randomized Pilot Study. Clin. Oral. Implants Res. 31, 84–92. doi: 10.1111/clr.13555 [DOI] [PubMed] [Google Scholar]
- Laleman I., Yilmaz E., Ozcelik O., Haytac C., Pauwels M., Herrero E. R., et al. (2015). The Effect of a Streptococci Containing Probiotic in Periodontal Therapy: A Randomized Controlled Trial. J. Clin. Periodontol. 42, 1032–1041. doi: 10.1111/jcpe.12464 [DOI] [PubMed] [Google Scholar]
- Lebeer S., Vanderleyden J., De Keersmaecker S. C. (2008). Genes and Molecules of Lactobacilli Supporting Probiotic Action. Microbiol. Mol. Biol. Rev. 72, 728–764, Table of Contents. doi: 10.1128/MMBR.00017-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee W., Cho S. M., Kim M., Ko Y. G., Yong D., Lee K. (2013). Weissella Confusa Bacteremia in an Immune-Competent Patient With Underlying Intramural Hematomas of the Aorta. Ann. Lab. Med. 33, 459–462. doi: 10.3343/alm.2013.33.6.459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly D. M., Stillwell R. H. (1965). Probiotics: Growth-Promoting Factors Produced by Microorganisms. Science 147, 747–748. doi: 10.1126/science.147.3659.747 [DOI] [PubMed] [Google Scholar]
- Lim H. S., Yeu J. E., Hong S. P., Kang M. S. (2018). Characterization of Antibacterial Cell-Free Supernatant From Oral Care Probiotic Weissella Cibaria, CMU. Molecules 23 (8), 1984. doi: 10.3390/molecules23081984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loesche W. J. (1976). Chemotherapy of Dental Plaque Infections. Oral. Sci. Rev. 9, 65–107. [PubMed] [Google Scholar]
- López-López A., Camelo-Castillo A., Ferrer M. D., Simon-Soro, Mira A. (2017). Health-Associated Niche Inhabitants as Oral Probiotics: The Case of Streptococcus Dentisani. Front. Microbiol. 8, 379. doi: 10.3389/fmicb.2017.00379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lourenshattingh A., Viljoen B. C. (2001). Yogurt as Probiotic Carrier Food. Int. Dairy J. 11, 1–17. doi: 10.1016/S0958-6946(01)00036-X [DOI] [Google Scholar]
- Macdonald K. W., Chanyi R. M., Macklaim J. M., Cadieux P. A., Reid G., Burton J. P. (2021). Streptococcus Salivarius Inhibits Immune Activation by Periodontal Disease Pathogens. BMC Oral. Health 21, 245. doi: 10.1186/s12903-021-01606-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Ding Q., Feng X., Li F. (2013). The Protective Effect of Recombinant FomA-Expressing Lactobacillus; Acidophilus Against Periodontal Infection. Inflammation 36, 1160–1170. doi: 10.1007/s10753-013-9651-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maekawa T., Hajishengallis G. (2014). Topical Treatment With Probiotic Lactobacillus Brevis CD2 Inhibits Experimental Periodontal Inflammation and Bone Loss. J. Periodontal Res. 49, 785. doi: 10.1111/jre.12164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahasneh S. A., Mahasneh A. M. (2017). Probiotics: A Promising Role in Dental Health. Dent. J. (Basel) 5 (4), 26. doi: 10.3390/dj5040026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Li F., Zhang X., Feng X. (2018). Biochemical Characterization of a Recombinant Lactobacillus Acidophilus Strain Expressing Exogenous FomA Protein. Arch. Oral. Biol. 92, 25–31. doi: 10.1016/j.archoralbio.2018.04.016 [DOI] [PubMed] [Google Scholar]
- Marcotte H., Kõll-Klais P., Hultberg A., Zhao Y., Gmür R., Mändar R., et al. (2006). Expression of Single-Chain Antibody Against RgpA Protease of Porphyromonas Gingivalis in Lactobacillus. J. Appl. Microbiol. 100, 256–263. doi: 10.1111/j.1365-2672.2005.02786.x [DOI] [PubMed] [Google Scholar]
- Marsh P. D. (1994). Microbial Ecology of Dental Plaque and its Significance in Health and Disease. Adv. Dent. Res. 8, 263–271. doi: 10.1177/08959374940080022001 [DOI] [PubMed] [Google Scholar]
- Metchnikoff E. (1907). The Prolongation of Life: Optomistic Studies Vol. 31 (Berlin, Germany: Nabu Press; ), 133. [Google Scholar]
- Moman R., O’neill C. A., Ledder R. G., Cheesapcharoen T., Mcbain A. J. (2020). Mitigation of the Toxic Effects of Periodontal Pathogens by Candidate Probiotics in Oral Keratinocytes, and in an Invertebrate Model. Front. Microbiol. 11, 999. doi: 10.3389/fmicb.2020.00999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montero E., Iniesta M., Rodrigo M., Marín M. J., Figuero E., Herrera D., et al. (2017). Clinical and Microbiological Effects of the Adjunctive Use of Probiotics in the Treatment of Gingivitis: A Randomized Controlled Clinical Trial. J. Clin. Periodontol. 44 (7), 708–716. doi: 10.1111/jcpe.12752 [DOI] [PubMed] [Google Scholar]
- Nissen L., Sgorbati B., Biavati B., Belibasakis G. N. (2014). Lactobacillus Salivarius and L-Gasseri Down-Regulate Aggregatibacter Actinomycetemcomitans Exotoxins Expression. Ann. Microbiol. 64, 611–617. doi: 10.1007/s13213-013-0694-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohland C. L., Macnaughton W. K. (2010). Probiotic Bacteria and Intestinal Epithelial Barrier Function. Am. J. Physiol. Gastrointest. Liver Physiol. 298, G807–G819. doi: 10.1152/ajpgi.00243.2009 [DOI] [PubMed] [Google Scholar]
- Ohshima T., Kojima Y., Seneviratne C. J., Maeda N. (2016). Therapeutic Application of Synbiotics, a Fusion of Probiotics and Prebiotics, and Biogenics as a New Concept for Oral Candida Infections: A Mini Review. Front. Microbiol. 7, 10. doi: 10.3389/fmicb.2016.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira L. F., Salvador S. L., Silva P. H., Furlaneto F. A., Figueiredo L., Casarin R., et al. (2017). Benefits of Bifidobacterium Animalis Subsp. Lactis Probiotic in Experimental Periodontitis. J. Periodontol. 88, 197–208. doi: 10.1902/jop.2016.160217 [DOI] [PubMed] [Google Scholar]
- Peña M., Barallat L., Vilarrasa J., Vicario M., Violant D., Nart J. (2019). Evaluation of the Effect of Probiotics in the Treatment of Peri-Implant Mucositis: A Triple-Blind Randomized Clinical Trial. Clin. Oral. Investig. 23, 1673–1683. doi: 10.1007/s00784-018-2578-8 [DOI] [PubMed] [Google Scholar]
- Qiao H., Duffy L. C., Griffiths E., Dryja D., Leavens A., Rossman J., et al. (2002). Immune Responses in Rhesus Rotavirus-Challenged BALB/c Mice Treated With Bifidobacteria and Prebiotic Supplements. Pediatr. Res. 51, 750–755. doi: 10.1203/00006450-200206000-00015 [DOI] [PubMed] [Google Scholar]
- Quattrini M., Korcari D., Ricci G., Fortina M. G. (2020). A Polyphasic Approach to Characterize Weissella Cibaria and Weissella Confusa Strains. J. Appl. Microbiol. 128, 500–512. doi: 10.1111/jam.14483 [DOI] [PubMed] [Google Scholar]
- Ricoldi M. S. T., Furlaneto F., Oliveira L. F. F., Teixeira G. C., Pischiotini J. P., Moreira A. L. G., et al. (2017). Effects of the Probiotic Bifidobacterium Animalis Subsp. Lactis on the non-Surgical Treatment of Periodontitis. A Histomorphometric, Microtomographic and Immunohistochemical Study in Rats. PloS One 12, e0179946. doi: 10.1371/journal.pone.0179946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajedinejad N., Paknejad M., Houshmand B., Sharafi H., Jelodar R., Zahiri H. S., et al. (2017). Lactobacillus Salivarius NK02: A Potent Probiotic for Clinical Application in Mouthwash. Probiotics Antimicrob. Proteins. 10 (3), 485–495. doi: 10.1007/s12602-017-9296-4. [DOI] [PubMed] [Google Scholar]
- Santos T. A., Scorzoni L., Correia R., Junqueira J. C., Anbinder A. L. (2020). Interaction Between Lactobacillus Reuteri and Periodontopathogenic Bacteria Using In Vitro and In Vivo (G. Mellonella) Approaches. Pathog. Dis. 78 (8), ftaa044. doi: 10.1093/femspd/ftaa044. [DOI] [PubMed] [Google Scholar]
- Shah M. P., Gujjari S. K. (2017). Long-Term Effect of Lactobacillus Brevis CD2 (Inersan ®) and/or Doxycycline in Aggressive Periodontitis. J. Indian Soc. Periodontol. 21, 341–343. doi: 10.4103/jisp.jisp_215_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva G. A., Moreira A. L. G., Silva P. H. F., Salvador S. L., Casarin R. C. V., Vicente R. M., et al. (2021). The Use of Probiotics can Reduce the Severity of Experimental Periodontitis in Rats With Metabolic Syndrome: An Immunoenzymatic and Microtomographic Study. J. Periodontol. 93 (2), e1–12. doi: 10.1002/JPER.21-0285 [DOI] [PubMed] [Google Scholar]
- Sivamaruthi B. S., Kesika P., Chaiyasut C. (2020). A Review of the Role of Probiotic Supplementation in Dental Caries. Probiotics Antimicrob. Proteins. 12 (4), 1300–1309. doi: 10.1007/s12602-020-09652-9 [DOI] [PubMed] [Google Scholar]
- Sliepen I., Hofkens J., Van E. M., Quirynen M., Teughels W. (2008). Aggregatibacter Actinomycetemcomitans Adhesion Inhibited in a Flow Cell. Oral. Microbiol. Immunol. 23, 520–524. doi: 10.1111/j.1399-302X.2008.00456.x [DOI] [PubMed] [Google Scholar]
- Sliepen I., Van Essche M., Loozen G., Van Eldere J., Quirynen M., Teughels W. (2009). Interference With Aggregatibacter Actinomycetemcomitans: Colonization of Epithelial Cells Under Hydrodynamic Conditions. Oral. Microbiol. Immunol. 24, 390–395. doi: 10.1111/j.1399-302X.2009.00531.x [DOI] [PubMed] [Google Scholar]
- Srionnual S., Yanagida F., Lin L. H., Hsiao K. N., Chen Y. S. (2007). Weissellicin 110, a Newly Discovered Bacteriocin From Weissella Cibaria 110, Isolated From Plaa-Som, a Fermented Fish Product From Thailand. Appl. Environ. Microbiol. 73, 2247–2250. doi: 10.1128/AEM.02484-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens M., Vollenweider S., Lacroix C., Zurich E. T. H. (2011). The Potential of Reuterin Produced by Lactobacillus Reuteri as a Broad Spectrum Preservative in Food. (Sawston. Cambridge, United Kingdom: Woodhead Publishing; ), 129–160. [Google Scholar]
- Suez J., Zmora N., Zilberman-Schapira G., Mor U., Dori-Bachash M., Bashiardes S., et al. (2018). Post-Antibiotic Gut Mucosal Microbiome Reconstitution Is Impaired by Probiotics and Improved by Autologous FMT. Cell 174, 1406–1423.e1416. doi: 10.1016/j.cell.2018.08.047 [DOI] [PubMed] [Google Scholar]
- Sunita G., Mallapa R. H., Kumar S. A., Kumar B. V. (2012). Probiotics for Human Health –New Innovations and Emerging Trends. Gut Pathog. 4, 15–15. doi: 10.1186/1757-4749-4-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkaradkiewicz A. K., Stopa J., Karpiński T. M. (2014). Effect of Oral Administration Involving a Probiotic Strain of Lactobacillus Reuteri on Pro-Inflammatory Cytokine Response in Patients With Chronic Periodontitis. Arch. Immunol. Ther. Exp. 62, 495–500. doi: 10.1007/s00005-014-0277-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tada H., Masaki C., Tsuka S., Mukaibo T., Kondo Y., Hosokawa R. (2018). The Effects of Lactobacillus Reuteri Probiotics Combined With Azithromycin on Peri-Implantitis: A Randomized Placebo-Controlled Study. J. Prosthodont. Res. 62, 89–96. doi: 10.1016/j.jpor.2017.06.006 [DOI] [PubMed] [Google Scholar]
- Takeda S., Hidaka M., Yoshida H., Takeshita M., Kikuchi Y., Tsend-Ayush C., et al. (2014). Antiallergic Activity of Probiotics From Mongolian Dairy Products on Type I Allergy in Mice and Mode of Antiallergic Action. J. Funct. Foods 9, 60–69. doi: 10.1016/j.jff.2014.04.013 [DOI] [Google Scholar]
- Terai T., Okumura T., Imai S., Nakao M., Yamaji K., Ito M., et al. (2015). Screening of Probiotic Candidates in Human Oral Bacteria for the Prevention of Dental Disease. PloS One 10, e0128657. doi: 10.1371/journal.pone.0128657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teughels W., Kinder H. S., Sliepen I., Pauwels M., Van E. J., Cassiman J. J., et al. (2007). Bacteria Interfere With A. Actinomycetemcomitans Colonization. J. Dental Res. 86, 611–617. doi: 10.1177/154405910708600706 [DOI] [PubMed] [Google Scholar]
- Theilade E. (1986). The non-Specific Theory in Microbial Etiology of Inflammatory Periodontal Diseases. J. Clin. Periodontol. 13, 905–911. doi: 10.1111/j.1600-051X.1986.tb01425.x [DOI] [PubMed] [Google Scholar]
- Van Hoogmoed C. G., Geertsema-Doornbusch G. I., Teughels W., Quirynen M., Busscher H. J., van der Mei H. C. (2008). Reduction of Periodontal Pathogens Adhesion by Antagonistic Strains. Oral. Microbiol. Immunol. 23, 43–48. doi: 10.1111/j.1399-302X.2007.00388.x [DOI] [PubMed] [Google Scholar]
- Waigankar S. S., Patel V. (2011). Role of Probiotics in Urogenital Healthcare. J. Midlife Health 2, 5–10. doi: 10.4103/0976-7800.83253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie H., Cook G. S., Costerton J. W., Bruce G., Rose T. M., Lamont R. J. (2000). Intergeneric Communication in Dental Plaque Biofilms. J. Bacteriol. 182, 7067–7069. doi: 10.1128/JB.182.24.7067-7069.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie H., Lin X., Wang B. Y., Wu J., Lamont R. J. (2007). Identification of a Signalling Molecule Involved in Bacterial Intergeneric Communication. Microbiology 153, 3228–3234. doi: 10.1099/mic.0.2007/009050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo J. I., Shin I. S., Jeon J. G., Yang Y. M., Kim J. G., Lee D. W. (2019). The Effect of Probiotics on Halitosis: A Systematic Review and Meta-Analysis. Probiotics Antimicrob. Proteins 11, 150–157. doi: 10.1007/s12602-017-9351-1 [DOI] [PubMed] [Google Scholar]
- You H. J., Oh D. K., Ji G. E. (2004). Anticancerogenic Effect of a Novel Chiroinositol-Containing Polysaccharide From Bifidobacterium Bifidum Bgn4. FEMS Microbiol. Lett. 240, 131–136. doi: 10.1016/j.femsle.2004.09.020 [DOI] [PubMed] [Google Scholar]
- Zhang G., Chen R., Rudney J. D. (2008). Streptococcus Cristatus Attenuates Fusobacterium Nucleatum-Induced Interleukin-8 Expression in Oral Epithelial Cells. J. Periodontal Res. 43, 408–416. doi: 10.1111/j.1600-0765.2007.01057.x [DOI] [PubMed] [Google Scholar]
- Zhao J.-J., Feng X.-P., Zhang X.-L., Le K.-Y. (2012). Effect of Porphyromonas Gingivalis and Lactobacillus Acidophilus on Secretion of IL1B, IL6, and IL8 by Gingival Epithelial Cells. Inflammation 35, 1330–1337. doi: 10.1007/s10753-012-9446-5 [DOI] [PubMed] [Google Scholar]
- Zhao J. J., Jiang L., Zhu Y. Q., Feng X. P. (2019). Effect of Lactobacillus Acidophilus and Porphyromonas Gingivalis on Proliferation and Apoptosis of Gingival Epithelial Cells. Adv. Med. Sci. 64, 54–57. doi: 10.1016/j.advms.2018.04.008 [DOI] [PubMed] [Google Scholar]
- Zhao J. J., Ke-Yi L. E., Feng X. P., Li M. (2011). Antagonistic Effects of Lactobacillus Acidophilus and Bifidobacterium Adolescents on Periodontalpathogens In Vitro . Shanghai J. Stomatol. 20, 364–367. [PubMed] [Google Scholar]
- Zmora N., Zilberman-Schapira G., Suez J., Mor U., Dori-Bachash M., Bashiardes S., et al. (2018). Personalized Gut Mucosal Colonization Resistance to Empiric Probiotics Is Associated With Unique Host and Microbiome Features. Cell 174, 1388–1405.e1321. doi: 10.1016/j.cell.2018.08.041 [DOI] [PubMed] [Google Scholar]