Abstract
Domestic animals play a vital role in the development of human civilization. Plants are utilized as remedies for a variety of domestic animals, in addition to humans. The tribes of North Waziristan are extremely familiar with the therapeutic potential of medicinal plants as ethnoveterinary medicines. The present study was carried out during 2018–2019 to record ethnoveterinary knowledge of the local plants that are being used by the tribal communities of North Waziristan, Khyber Pakhtunkhwa, Pakistan. In all, 56 medicinal plant species belonging to 42 families were identified, which were reported to treat 45 different animal diseases. These included 32 herbs, 12 shrubs, and 12 trees. Among the plant families, Asteraceae contributed the most species (5 spp.), followed by Amaranthaceae (4 spp.), Solanaceae (4 species), and Alliaceae, Araceae, and Lamiaceae (2 spp. each). The most common ethnoveterinary applications were documented for the treatment of blood in urine, bone injury, colic, indigestion, postpartum retention, skin diseases, constipation, increased milk production, mastitis, foot, and mouth diseases.
Keywords: ethnoveterinary practices, livestock, traditional medicine, Tribal Area, traditional knowledge, North Waziristan
Introduction
Plants have long been used as food (1), feed (2, 3), fiber (4), and shelter (5) by humans (6) and animals, as well as to control and alleviate diseases (7–9). Ethnoveterinary medicine (EVM) plays an essential role in animal production and livelihood development in many poor rural areas (10, 11) and is frequently the only option for farmers to treat their sick animals (12–14). The term “ethnoveterinary” is defined as “local people's beliefs and aboriginal knowledge and practice used for the treatment of animal diseases” (15–17). According to McCorkle and Schilihorn-van-Veen (7), it is a systematic study and application of indigenous knowledge for theory and practice in ethnoveterinary medicine (EVM). The information and ability of ethnoveterinary practices (EVPs) are recognized by means of experience and passed on verbally from one generation to the next (18, 19). Due to industrial and technological development, this local information remains in some parts of developed countries (20). Such knowledge and practices are passed down and retained from generation to generation (21), particularly by livestock owners. So, EVM is playing an important role in viable livestock farming in various parts of the world (22–24).
Pakistan is an agricultural country, with agriculture and livestock supporting up to 80% of the population (25, 26). Pakistan is the world's third largest milk producer, demonstrating the importance of cattle (27). Many Pakistani livestock producers are impoverished, and owing to financial restrictions (28), the majority of these farmers are unable to buy current allopathic medications, resulting in poor animal productivity and health. In such circumstances, ethnoveterinary medicine may be advocated as an alternative to contemporary pharmaceuticals (29), and it can aid in poverty reduction by enabling people to cure their animals using their own resources. Traditional indigenous medicine is still used in rural regions for human (30) and cattle diseases (31) and for the maintenance of excellent animal health in emerging nations, despite advances in the pharmaceutical industry and the creation of therapeutic agents (32–34). EVM knowledge, like all other traditional knowledge systems (35), is passed down orally from generation to generation and may become extinct (36) as a result of fast social, environmental, and technological changes (20, 37), as well as the loss of cultural legacy disguised as civilization (34). Traditional knowledge must be documented via systematic investigations (38–40) in order to be preserved before it is lost forever (21).
According to the literature, tremendous work has been done worldwide on the documentation of ethnoveterinary practices (8, 10, 18, 19, 41–43), but in Pakistan very little attention has been given to the documentation of EVM, resulting in limited reports on this important ethnoveterinary knowledge (12, 21, 44), revealing a significant gap in knowledge. For instance, Farooq et al. (45) reported 18 plant species representing 14 families to cure parasite disorders of livestock from the Cholistan desert of Pakistan, while Dilshad et al. (46) reported 66 plant species from Sargodha, Pakistan. Zia-ud-Din et al. (47) identified 35 plant species belonging to 25 families in a similar survey from the hilly area of Pakistan. Shoaib et al. (48) reported 41 medicinal plants belonging to 30 families to treat various livestock ailments from the Kaghan Valley, Western Himalayas–Pakistan. Siddique et al. (49) documented 80 medicinal plants belonging to 50 families to treat various livestock diseases from Haripur District, Khyber Pakhtunkhwa, Pakistan.
Various ethnoveterinary studies have been conducted in the allied areas of the study area (50–52), but no single ethnoveterinary documentation has been carried out in this unexplored, remote region of the tribal district of North Waziristan, Pakistan, highlighting the dire need to report this important knowledge. As a result, the current study is the first to investigate the entire ethnoveterinary practices of North Waziristan, Pakistan, where indigenous people have extensive traditional knowledge and rely heavily on medicinal plants to treat livestock ailments and supplement their income. This study might be beneficial to fill the gap that might have not been covered due to the negligence in documentation of ethnoveterinary practices. Therefore, it is extremely necessary to document and disseminate indigenous knowledge to help and share the different uses of plants as animal healthcare and to promote different conservation measures. Thus, the aim of this study was to evaluate and record the precious ethnoveterinary information of North Waziristan that is used by the area's indigenous inhabitants to treat domestic animals' diseases and disorders.
Materials and Methods
Study Area
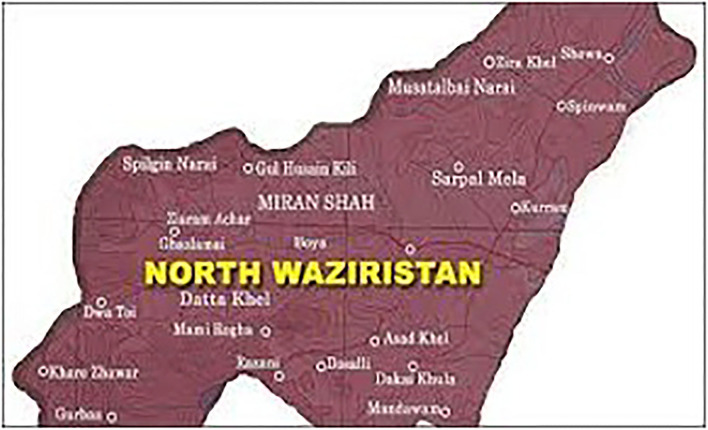
The tribal district of North Waziristan, Khyber Pakhtunkhwa, Pakistan, is a hilly region that lies between 32–35° and 33–20° north latitudes and 69–25° and 70–40° east longitudes with an altitude of 2143–7717 feet (Figure 1). North Waziristan is bounded on the south by the district of South Waziristan; on the north by Kurram Agency, Hangu District, and Afghanistan; on the east by the district of Bannu; and on the west also by Afghanistan. North Waziristan falls under the Irano-Turanian Region. The area is bounded by mountains, which are connected with Koh-e-Sulaiman in the south and Koh-e-Sufaid in the north. The tribal district is well-populated with various small dynamized villages. The main hills are Alexandra, Larema, Kalenjer Ser, Vezda, Ebulnki, and Sedgai Gher. The area is divided into three sub-divisions and nine tehsils. The Tochi Valley is 101 km long. The annual rainfall is 10“−13.” The summer period starts from May to September. The hottest month is June. The winter season starts from October to March. The coldest months are December, January, and February.
Figure 1.
Map of the study area.
According to the census report of 2017, the total population of North Waziristan is 543,254. The total forest area is 475,000 acres. Wazir and Dawar are the major tribes in the research area. Pashto is the major language. The joint family system is practiced in the study area. The funeral and death ceremonies are mutually attended by the relatives and friends. The citizens of the area follow the jirga to determine their administrative and social problems. This is one of the strongest and most active common institutions in the area. The people in the area are mostly poor and earn their income from basic jobs. These include wood sellers, farmers, shopkeepers, horticulturists, local health healers, pastoralists, and government employees. In the study area, the domestic animals kept by the pastoralists are considered a better source of income.
Field Survey and Data Collection
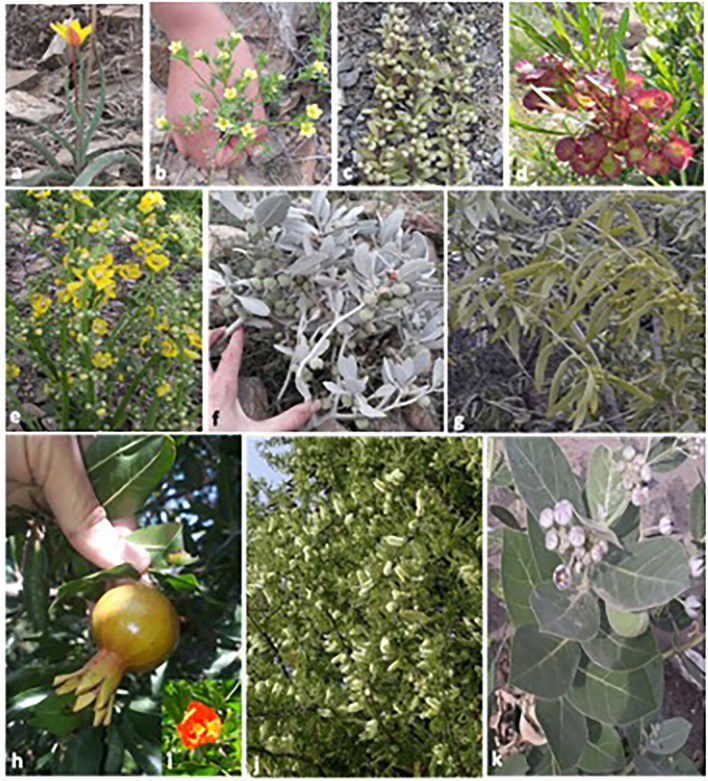
The area of the study was visited during March and October 2018–2019 in order to collect ethnoveterinary data. The assessment was organized to collect data by using a semi-structured interview based on folk knowledge (35, 53) about plants that are used for the curing of various animal ailments (21, 54). The local people have valuable information about ethnoveterinary uses of the plants. All the collected plant species were photographed (Figure 2). During the study period, different types of herbal medicine were sold on the market, and the multi-use roles of some ethnoveterinary herbal plants were noted. Moreover, herbal remedy suppliers were interviewed. During the survey, every care was taken to note the vernacular names, dosage, parts used, mode of application, drug preparation method, and uses. Overall, 130 informants, 92 men and 38 women, were interviewed during the survey.
Figure 2.
Photographs of some ethnoveterinary medicinal plant species of the study area.
Herbarium Work
Plant specimens were collected, pressed, dried, poisoned, and mounted on standard herbarium sheets (55, 56). The mounted specimens were then identified using published literature (57–59). For authentication purposes, Quaid-e-Azam University Islamabad, Pakistan, was also consulted. The identified specimens were deposited for future records in the Department of Botany at Hazara University, Mansehra, Pakistan.
Statistical Data Analysis
The indigenous knowledge data were collected and analyzed statistically (36, 60, 61) using different quantitative indices: fidelity level (FL%) and informant consensus factor (ICF).
Fidelity Level (FL%)
The fidelity level (FL%) was the percentage of informants who reported the uses of certain plant species to cure a specific disease reported from the area of study. The fidelity level was calculated as follows (62, 63):
where Np is the number of informants that mention a use of a plant species to cure a specific disease and N is the number of informants that use the plant species to cure any other disease.
Informant Consensus Factor
The informant consensus factor (ICF) was used to seek agreement among the informants on the documented cures for each ailment category (64).
where Nur is the number of use reports from informers in each disease category and Nt is the number of taxa used.
Results
Demographic Data
A total of 130 informants were interviewed. Most informants were men (83.85%) rather than women (16.15%). Many of them were over 60 years old (46.79%), 51–60 years old (39.23%), and 35–50 years old (23.88%). Due to the lack of educational facilities in that area, most of the informants were illiterate (45.38%; Table 1). But some were educated, showing that they had an awareness of education (8.46%). Many informants had completed primary (31.54%) and middle-level education (14.62%). All the informants spoke Pashto.
Table 1.
Demographic details of the informants interviewed during ethnoveterinary survey in the study area.
| Gender | Number of informants N = 130 | Percentage (%) |
|---|---|---|
| Male | 109 | 83.85 |
| Female | 21 | 16.15 |
| Age groups | ||
| 35–50 | 17 | 13.08 |
| 51–60 | 51 | 39.23 |
| >60 years | 62 | 47.69 |
| Educational attainment | ||
| Illiterate | 59 | 45.38 |
| Primary | 41 | 31.54 |
| Middle | 19 | 14.62 |
| Secondary | 11 | 8.46 |
| Social livelihood | ||
| Herbalists | 38 | 29.23 |
| Farmers | 12 | 9.23 |
| Shepherds | 25 | 19.23 |
| Gardeners | 17 | 13.08 |
| Local healers | 28 | 21.54 |
| Shopkeepers | 6 | 4.62 |
| Traders | 4 | 3.08 |
Ethnoveterinary Plant Species
During the present study, a total of 56 plant species belonging to 42 families were documented to be used in the treatment of 45 different ailments by the local herders, farmers, and shepherds in the tribes of North Waziristan, Pakistan. The results collected during the study are summarized, which provide the following knowledge for each plant species: botanical name, family name, vernacular name, habitat, part used, and disease treated (Table 2).
Table 2.
List of ethnoveterinary plants (EVPs) used by tribes for healing of different ailments in North Waziristan, Pakistan.
|
Sr # |
Plant species | Family | Local name | Parts used | Habitat | Ethnoveterinary medicinal usage |
|---|---|---|---|---|---|---|
| 1 | Trianthema portulacastrum L. | Aizoaceae | Deravenay Botay | Shoots | Herb | A shoot decoction is given orally to cows, sheep, and goats to expel abdominal worms. |
| 2 | Allium sativum L. | Alliaceae | Yeza | Bulb | Herb | The bulbs are crushed and mixed in wheat grain husk; the mixture is fed to cows and buffaloes 2 times a day to treat indigestion and abdominal pain. |
| 3 | Allium cepa L. | Alliaceae | Pyaz | Bulb, seeds | Herb | The seeds are given to birds and hens in case of twisting of neck and head (torticollis) disease. Crushed bulbs are mixed with brown sugar (Gur) and given to cows and buffaloes to treat fever. |
| 4 | Aerva javanica (Burm. f.) Juss. | Amaranthaceae | Gher valanai | Seed | Herb | The seeds (850 g) are mixed with 500 ml yogurt. The mixture is given 2 times a day for 12 days to cows, buffaloes, and goats for the treatment of blood in urine and diarrhea. Dry leaves (250 g) are ground into powder and mixed with 120 g hot butter oil. This mixture is given two times a day for 5 days to cows and goats to treat female sex organ infection. |
| 5 | Amaranthus spinosus L. | Amaranthaceae | Ghota surmi | Roots | Herb | A root decoction of about two cups mixed with brown sugar (Gur) is given to cows and buffaloes to increase the milk amount. |
| 6 | Amaranthus viridis L. | Amaranthaceae | Sormi | Leaves | Herb | Fresh plant leaves are crushed and mixed with pure ghee (butter oil). The paste is given twice a day for 3 days to goats, sheep, and cows to relieve constipation. |
| 7 | Achyranthes aspera L. | Amaranthaceae | Ghoskai | Leaves, root | Shrub | The juice made from the leaves of about one cup is given orally two times a day for 5 days to goats to remove urinary bladder stone. The fresh extract of the root is mixed with brown sugar (Gur), and 1 L mustard oil is given orally twice a day to buffaloes, cows, goats, and sheep to remove the placenta after birth. |
| 8 | Trachyspermum ammi L. | Apiaceae | Spirkay | Whole plant | Herb | A mixture of ajwain, black salt, and mint leaves at a ratio of 4:1:2 is given to cows, buffaloes, and donkeys to improve digestion. The whole plants are sliced and mixed with pickle and are given to goats, cows, and buffaloes to improve digestion. Seed powder of about 85–110 g is mixed with Gur. This mixture is given orally twice a day for 2 days to buffaloes and cows to expel the placenta. |
| 9 | Arisaema flavum (Forssk) | Araceae | Mangore botai | Rhizome | Herb | Roasted rhizomes are crushed and mixed with wheat flour and mustard oil and are given to cows and buffaloes for increasing milk yield. |
| 10 | Arisaema jacquemontii Blume | Araceae | Ghot mangore bote | Rhizome | Herb | One tablespoon of powdered rhizome is given orally with water to sheep and goats to expel intestinal worms. |
| 11 | Calotropis procera (Wild) R. Brown. | Asclepiadaceae | Spelmai | Latex, whole plant | Shrub | The fruits and leaves are crushed and are mixed with mustard oil and 90 g sulfur to form paste, and the paste is applied externally on cows and buffaloes to treat skin infection. |
| 12 | Aloe vera L. | Asphodelaceae | Zargya | Aerial parts | Herb | The fresh plant is crushed and put in drinking water to treat respiratory problems in goats, sheep, cows, and buffaloes. |
| 13 | Artemisia martima L. | Asteraceae | Terkha | Aerial parts | shrub | A 100-ml cup of decoction obtained from the aerial parts of the plants is given orally once a day for 3 days to cows and buffaloes for the killing and expelling of intestinal worms. |
| 14 | Helianthus annuus L. | Asteraceae | Ghurmasterge gul | Seeds | Shrub | The seeds are finely ground into powder, and the powders are given to hens with drinking water for 7 days to enhance egg yield. |
| 15 | Sonchus oleraceus L. | Asteraceae | Tareza | Leaves | Herb | Fresh plants are chopped and mixed with wheat grain husk and are given to goats, sheep, and cows to increase milk yield. |
| 16 | Tagetes minuta L. | Asteraceae | - | Shoots | Herb | About one cup of the concentrated infusion obtained from the shoots is given orally to buffaloes and cows to remove endoparasites like intestinal worms and liver flukes. |
| 17 | Xanthium strumarium L. | Asteraceae | Chechan botai | Leaves | Herb | Fresh juice extracted from the leaves is applied externally once a day for 3 days to kill larvae in wounds and to heal wounds. |
| 18 | Berberis lycium Royle | Berberidaceae | Nenakai boti | Bark | Shrub | Bark powder of about 250 g is mixed with butter oil and wheat flour. This mixture paste is given twice a day for 7 days to cows and buffaloes as body tonic, to treat internal fractures and strengthen the bone. |
| 19 | Eruca sativa Mill. | Brassicaceae | Khatel | Shoots | Herb | Young fresh shoots with leaves (4 kg) are boiled in 10 kg water to obtain an herbal tea. The herbal tea is mixed with 2 kg millet flour and is given orally to the horses 2 times a day for 5 days for the treatment of horse scabies. |
| 20 | Bauhinia variegata L. | Caesalpiniaceae | Kachnar | Leaves, flower | shrub | The paste made from crushed leaves and flowers is mixed with 5 g black salt and is given orally twice a day for 3 days to cows, buffaloes, goats, and sheep for the treatment of diarrhea. |
| 21 | Cannabis sativa L. | Cannabinaceae | Bhanga | Leaves | Herb | Powder made from leaves is mixed with black salt and is given orally once a day for 5 days to cows, buffaloes, and donkeys to increase appetite. |
| 22 | Capparis decidua (Forssk.) Edgew. | Capparidaceae | - | Tender branches | Tree | Tender branches are crushed to form fine powder. The powder is mixed with millet flour and given to cows and buffaloes to reduce their body pain and to improve the milk taste. |
| 23 | Gymnosporia nemorosa (Eckl. & Zeyh.) Szyszyl. | Celastraceae | Saghrzai | Leaves | Shrub | Infusions obtained from leaves of about 1 L are given orally twice a day for 3 days to cows and buffaloes for the treatment of diarrhea and dysentery. |
| 24 | Convolvulus arvensis L. | Convolvulaceae | Purvatia | Whole plant | Herb | The whole plant is crushed along with brown sugar (Gur), and the mixture is given to goats and sheep for 4–5 days to increase milk production and to treat constipation. |
| 25 | Citrullus colocynthis (L.) Schrad. | Cucurbitaceae | Marayghunye | Fruit | Herb | Powder (620 g) made from dried fruit is mixed with 130 g seed powder of Withania coagulans. This mixture is given 2 times a day for 7 days to horses and camels to treat rheumatoid arthritis. |
| 26 | Cucumis melo subsp. agrestis (Naud.) Grebensc. | Cucurbitaceae | Kukundai ghonde | Seeds | Herb | Whole seed powder of about 6–12 spoons is given to cattle and goats with drinking water to expel intestinal worms and liver flukes. |
| 27 | Equisetum arvense L. | Equisetaceae | Bandkai | Stem | Herb | Shoots (800 g) are crushed and mix with 1 L mustard oil. This mixture is given 2 times a day for 7 days to cows and buffaloes to treat urinary tract infection (blood in urine). |
| 28 | Ricinus communis L. | Euphorbiaceae | Arand | Leaves | Shrub | From the seeds, oil is extracted and is used as a laxative in animals. The extracts made from leaves are mixed with brown sugar. This mixture is given orally 2 times a day for 2 days to cows and buffaloes to speed up the expelling of the placenta. |
| 29 | Indigofera heterantha Wall. | Fabaceae | - | Young twigs, leaves | Shrub | The leaves and young twigs are given to cows and buffaloes to treat abdominal pain. |
| 30 | Quercus incana Roxb. | Fagaceae | Tora serai | Seeds | Tree | Powder (900 g) made from the seeds is mixed with 2 kg boiled millet and 1 kg brown sugar (Gur). This mixture is given orally once a day for 7 days to cows and buffaloes to increase milk production. |
| 31 | Geranium wallichianum D.Don. | Geraniaceae | Dhania ghonde | Roots | Herb | About 1–2 kg of roots is chopped, cooked, and mixed with 1 L of mustard oil. This mixture is given to cows, buffaloes, donkeys, and horses as body tonic. |
| 32 | Mentha longifolia L. | Lamiaceae | Zangali valanai | Roots | Herb | The root decoction (1 L) is mixed with half a liter of mustard oil and half a kilogram of brown sugar (Gur). This mixture is given to cows and buffaloes to increase the milk amount and to treat fever. |
| 33 | Mentha spicata L. | Lamiaceae | Serkare valanai | Leaves | Herb | Leaves (830 g) are crushed and mixed with 100 g black salt. This mixture is given orally to cows, buffaloes, goats, and sheep to improve digestion and to remove external parasites, e.g., anti-lice. |
| 34 | Tulipa clusiana DC. | Liliaceae | Shandai | Whole plant | Herb | The plants (2 kg) are chopped and mixed with 3 kg wheat grain husk. This mixture is given once a day for 12 days to cows, goats, and sheep to increase milk production. |
| 35 | Linum strictum L. | Linaceae | Showde tengavanai | Whole plant | Herb | Chopped plants (3 kg) are mixed with 3 kg wheat grain husk. This mixture is given once a day for 7 days to increase the concentration of milk. |
| 36 | Melia azedarach L. | Meliaceae | Bakana | Seed | Tree | Powder (500 g) made from the ripe seeds is mixed with 1 kg brown sugar (Gur). This mixture is given to cows and buffaloes as a lactagogue (promotes lactation). |
| 37 | Acacia modesta Wall. | Mimosaceae | Palosa | Bark | Tree | The bark decoction (500 ml) is mixed with 200 g butter oil. This mixture is given orally twice a day for 5 days to cows and buffaloes for easy parturition and for expelling the placenta. |
| 38 | Morus alba L. | Moraceae | Spin tooth | Fruit | Tree | Fresh fruit of about 3 kg is given once a day to cows, buffaloes, goats, and sheep to increase milk production and to treat constipation. |
| 39 | Olea europaea L. | Oleaceae | Zaiton | Fruit | Tree | The oil extracted from the fruits is given orally to animals for 4–7 days to treat indigestion and colic. |
| 40 | Argyrolobium roseum (Camb.) Jaub | Papilionaceae | Makhani booti | Shoots | Herb | The fresh plant (4 kg) is chopped and mixed with 2 kg wheat grain husk. This mixture is given once a day to cows, sheep, and goats to increase milk production. |
| 41 | Cedrus deodara (Roxb.) G. Don | Pinaceae | Almanza | Wood oil | Tree | The fresh heartwood is cut, and oil locally called “Ranzana” is extracted and applied externally on buffaloes to treat scabies and is also used as a mosquito and louse repellent. |
| 42 | Plantago major L. | Plantaginaceae | Ispaghul | Whole plant | Herb | The crushed plant material is applied externally on the affected hooves of cows and buffaloes for 6 days to treat mouth and foot disease locally called “Thabak.” |
| 43 | Pennisetum glaucum (L.) R.Br | Poaceae | Bajra | Seed | Mature grains (2 kg) are boiled in water and mixed with 1 kg brown sugar (Gur) and one cup of mustard oil. This mixture is feed to cows and buffaloes once a day to enhance milk production. | |
| 44 | Punica granatum L. | Punicaceae | Velngai | Peel/husk | Tree | Fruits peels (700 g) are mixed with 500 ml curd. This mixture is given orally cows, buffaloes, goats, and sheep 2 times a day to treat dietary diarrhea. The outer fleshy part of the fruit is dried to make powder (600 g) and mixed in 500 ml curd. This mixture is given orally twice a day for 7 days to animal to treat kidney inflammation. |
| 45 | Prunus armeniaca L. | Rosaceae | Mondata | Leaves | Tree | Fresh or dry leaves are given to animal to treat constipation. |
| 46 | Salvadora oleoides Decne. | Salvadoraceae | Plawan | Fruit | Tree | Fresh fruit (2 kg) is given once a day for 12 days to cows, goats, and sheep in order to increase the milk concentration. Dried fruit (1 kg) is given once a day for 8 days to animals to treat rheumatism. Dried fruit (1 kg) is also given to cows and buffaloes after childbirth to make easy the removal of lochia (bleeding after childbirth). |
| 47 | Dodonaea viscosa (Linn.) Jacq. | Sapindaceae | Ghojara | Leaves | Shrub | The leaves of the plant are warmed and tied about 20–30 times to treat the fractured leg of animals. |
| 48 | Monotheca buxifolia (Falc.) A. DC. | Sapotaceae | Gurgora | Leaves | Tree | The plant leaves are orally fed to buffaloes and cows for 3 days to cure the unusual taste of milk; after 3–4 days, the original taste of the milk is retained. |
| 49 | Verbascum thapsus L. | Scrophulariaceae | Neshe botai | Leaves | Herb | Fresh chopped leaves (920 g) are mixed with 600 ml curd. This mixture is given orally 2 times a day for 5 days to cows, buffaloes, sheep, and goats to cure cough, diarrhea, and abdominal pain. Dried leaf powder is applied topically on wounds for quick healing. |
| 50 | Datura alba Nees. | Solanaceae | Berbaka | Leaves | Shrub | Warm leaves are applied externally to eliminate swellings from the animal body. |
| 51 | Solanum melongena L. | Solanaceae | Bengan | Fruit | herb | The fresh fruit is cut into minute parts and fed for 7 days to animals (cows, buffaloes) to boost female fertility. |
| 52 | Solanum surattense Brum. F. | Solanaceae | Korkendai | Fruit, leaves | Herb | Powder (850 g) made from ripened fruits is mixed with 500 ml honey. This mixture is given orally twice a day to cows, buffaloes, and horses to relieve abdominal pain. From the leaves and fresh fruit, poultice is made, which is applied externally to relieve pain in the animal body. |
| 53 | Withania coagulans (Stocks) Dun. | Solanaceae | Shafianga | Fruit, leaves | Shrub | From ripened fruits, 930 g powder is made and is given with drinking water once a day to sheep and goats to relieve abdominal pain. The powders of leaves are dissolved in water and are given to animals as a cooling agent. |
| 54 | Tamarix aphylla (L.) Karst. | Tamaricaceae | Ghez | Bark, leaves | Tree | The bark is finely ground to make powder, which is applied externally on animal skin to cure burning wounds. In animals the leaf smoke is used as an antiseptic after childbirth. |
| 55 | Vitis negundo L. | Verbenaceae | Marwandai | Leaves | shrub | Crushed leaves (800 g) are mixed with 90 g black salt and 350 g mint leaves. This mixture is given to cows, buffaloes, and donkeys to treat stomach problems and fever. A high dosage of dried leaves mixed with honey is used orally to expel worms in camels and cattle. |
| 56 | Peganum harmala L. | Zygophyllaceae | Sponda | Whole plant | Herb | The extraction made from the plant is externally applied on the animal body to kill lice (anti-lice). The poultice made from the leaves is externally applied to reduce pain from the crack bone in goats and sheep. The smoke from branches and leaves is used for 7 days to treat mastitis (breast inflammation) in animals. |
Habitat of Medicinal Plants
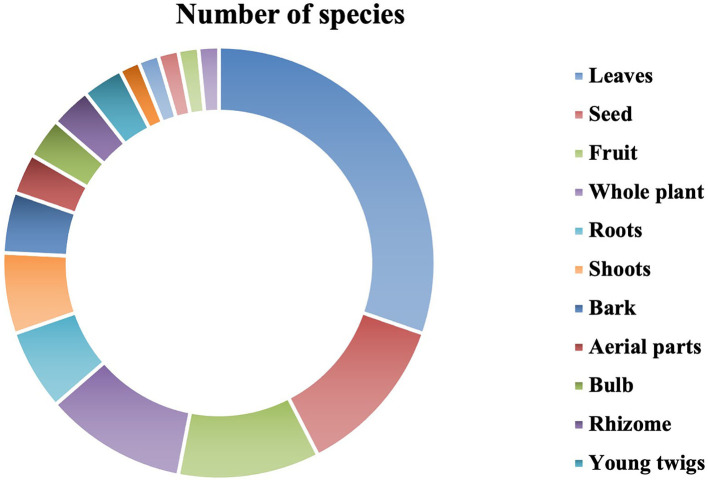
In the present study, it was revealed that the herbs were the most commonly used life form by the inhabitants, with 32 species (57.14%; Figure 3). It was followed by shrubs and trees (12 spp., 21.43% each). The dominant use of herbaceous plants in the study area in the preparation of remedies is due to profuse growth and easy availability in the wild as compared to other life forms.
Figure 3.
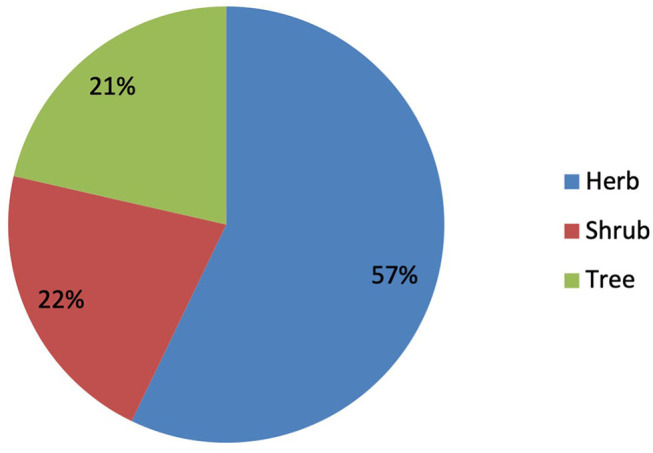
Growth form of the plant species reported from North Waziristan.
Medicinal Plant Families
The families that represented the highest number of plant species for the indigenous ethnoveterinary medicines were Asteraceae (5 spp., 8.93%), followed by Amaranthaceae and Solanaceae (4 spp., 7.14% each), Alliaceae, Araceae, Cucurbitaceae, and Lamiaceae (2 spp., 3.57% each), while the remaining families were represented by 1 species (1.79% each) in Table 2.
Diseases Cured
Among all the 45 diseases in the study area, the indigenous healers and other local informants reported milk production (increased milk yield) as the most common problem treated through 12 plant species. It is followed by intestinal worms with 6 species each; abdominal pain with 5 species; constipation, diarrhea, and expulsion of placenta with 4 species each; and fever and indigestion with 3 species each. However, all the remaining 37 diseases were treated by <3 species each (Table 2).
Plant Parts Used as Indigenous Medicine
Different parts of the plant were used to prepare ethnoveterinary medicine recipes to treat various ailments and are summarized in Figure 4 and Table 2. Out of 16 plant parts, leaves were heavily used to prepare medication (20 spp., 30.30%), followed by seeds (8 spp., 12.12%); fruits and whole plants (7 spp., 10.61%); roots and shoots (4 spp., 6.06%); bark (3 spp., 4.55%); aerial parts, bulbs, rhizomes, and young twigs (2 spp., 3.03% each); and flowers, latex, husk, stems, and wood oil (1 spp., 1.520% each). The collection of leaves and recipes for preparation from the leaves is much easier. So, leaves were the most used plant part in the preparation of remedies for the treatment of livestock ailments.
Figure 4.
Plant species parts used in preparation of indigenous medicines.
Mode of Preparation in Indigenous Medicine
For treating 45 different diseases and ailments, about 11 different types of formulations were prepared from different plants (Table 3), in which most of the ethnoveterinary remedies were prepared as powders (16 spp., 25.81%), followed by raw (12 spp., 19.35%), crushed (9 spp., 14.52%), decoction and paste (4 spp., 6.45% each), and extract and infusion (3 spp., 4.84% each). Nonetheless, juice, oil, poultice, smoke, and wrapping (2 spp., 3.23% each), followed by the roasted mode of preparation for treating diseases, were recorded with the smallest number of species (1 spp., 1.61%). The most dominant method for the preparation of remedies was powder, which was used in the treatment of animals' diseases.
Table 3.
Modes of preparation of the recorded species used in indigenous medicine.
| Mode of preparation | No. of species | Percentage (%) of species |
|---|---|---|
| Crushed | 9 | 14.52 |
| Decoction | 4 | 6.45 |
| Extract | 3 | 4.84 |
| Infusion | 3 | 4.84 |
| Juice | 2 | 3.23 |
| Oil | 2 | 3.23 |
| Paste | 4 | 6.45 |
| Poultice | 2 | 3.23 |
| Powder | 16 | 25.81 |
| Raw | 12 | 19.35 |
| Roasted | 1 | 1.61 |
| Smoke | 2 | 3.23 |
| Wrapping | 2 | 3.23 |
Mode of Administration
In the current study, the most common mode of application/administration is oral application (48 spp., 81.36%), followed by topical application (9 spp., 15.25%) and inhalation (2 spp., 3.39%) (Figure 4). The majority of remedies were administered orally in the study area for the treatment of different ailments.
Quantitative Analysis
Informant Consensus Factor
In the present study, we recorded ICF values ranging from 0.75 to 0.92 (Table 4). With 230 use reports, gastrointestinal disorder had the highest ICF value (0.92), followed by general health ailments (0.88); parasitic diseases (0.87); skeleto-muscular pain and inflammation (0.86); uterine disorders (0.83); analgesic, fever, and wound healing (0.82); dermatological disorders and antiseptic (0.80); urino-genital disorder (0.79); and respiratory diseases (0.75).
Table 4.
Ailment categories and informant consensus factors or ICFs.
| Ailment categories | Biomedical term | Nt | Nur | ICF |
|---|---|---|---|---|
| Analgesic, fever, and wound healing | Body pain, fever, wound healing, bone fracture, burning wounds | 8 | 39 | 0.82 |
| Dermatological disorders and antiseptic | Skin infection, scabies, antiseptic | 4 | 16 | 0.80 |
| Gastrointestinal disorder | Indigestion, increasing appetite, abdominal pain, constipation, colic, diarrhea, dysentery, stomach problems | 19 | 230 | 0.92 |
| General health ailments (GHAs) | Enhancing egg yield, increasing milk yield, increasing milk concentration, improving the milk taste, lactagogue | 20 | 155 | 0.88 |
| Parasitic diseases | Intestinal worms, larva in wounds, liver flukes, mosquito repellent, anti-lice | 12 | 85 | 0.87 |
| Respiratory diseases | Cough, respiratory problem | 2 | 5 | 0.75 |
| Skeleto-muscular pain and inflammation | Rheumatism, rheumatoid arthritis, mastitis, body swellings, torticollis, foot and mouth disease | 6 | 37 | 0.86 |
| Urino-genital disorder | Urinary bladder stone, blood in urine, kidney inflammation, urinary tract infection | 4 | 15 | 0.79 |
| Uterine disorders | Easy parturition, expel placenta, female sex organ infection, boost female fertility, lochia | 8 | 43 | 0.83 |
Fidelity Level (FL%) of the Reported Ethnoveterinary Plants
In the present survey, the FL of medicinal plants varied between 40.91 and 100%. Four medicinal plants, viz., Trachyspermum ammi, Salvadora oleoides, Peganum harmala, and Withania coagulans, were the most important medicinal plants in the study area, which were particularly used to treat indigestion, lochia, mastitis, and abdominal pain, determined by 45 interviewers with 100% fidelity (Table 5), followed by Berberis lycium, which was the 2nd most important ethnoveterinary plant, having a fidelity level of 97.78% used in body tonic. Aloe vera was the third most important medicinal plant, having a fidelity level of 97.50% FL and used in respiratory problems, while Capparis decidua had the lowest fidelity level (40.91%) and is used in body pain. However, the rest of the medicinal plants were within the fidelity range of 41.38–95.56%.
Table 5.
List of reported species with treated disorders and their fidelity level (FL%).
| Preferred species | Application | Np | N | FL (%) |
|---|---|---|---|---|
| Acacia modesta Wall | Easy parturition | 24 | 44 | 54.55 |
| Achyranthes aspera Linn. | Urinary bladder stone | 28 | 47 | 59.57 |
| Aerva javanica (Burm. f.) Juss | Female sex organ infection | 8 | 12 | 66.67 |
| Allium cepa Linn. | Torticollis | 11 | 20 | 55.00 |
| Allium sativum L | Indigestion | 9 | 15 | 60.00 |
| Aloe vera L. | Respiratory problems | 39 | 40 | 97.50 |
| Amaranthus spinosus L. | Increasing milk amount | 28 | 45 | 62.22 |
| Amaranthus viridis L. | Constipation | 25 | 46 | 54.35 |
| Argyrolobium roseum (Camb.) Jaub | Increasing milk production | 23 | 45 | 51.11 |
| Arisaema flavum (Forssk) | Increasing milk yield | 11 | 16 | 68.75 |
| Arisaema jacquemontii Blume. | Expelling intestinal worms | 17 | 29 | 58.62 |
| Artemisia martima L | Expelling intestinal worms | 38 | 45 | 84.44 |
| Bauhinia variegata L. | Diarrhea | 3 | 6 | 50.00 |
| Berberis lyceum Royle. | Body tonic | 44 | 45 | 97.78 |
| Calotropis procera (Wild) R. Brown | Skin infection | 13 | 14 | 92.86 |
| Cannabis sativa L. | Appetizer | 9 | 20 | 45.00 |
| Capparis decidua (Forssk.) Edgew. | Body pain | 9 | 22 | 40.91 |
| Cedrus deodara (Roxb.) G. Don | Scabies | 41 | 45 | 91.11 |
| Citrullus colocynthis (L.) Schrad | Rheumatoid arthritis | 27 | 38 | 71.05 |
| Convolvulus arvensis L. | Constipation | 43 | 45 | 95.56 |
| Cucumis melo subsp. agrestis (Naud.) Grebensc | Expelling intestinal worms | 12 | 23 | 52.17 |
| Datura alba Nees. | Eliminating swellings | 25 | 45 | 55.56 |
| Dodonaea viscosa (Linn.) Jacq. | Fractured leg | 28 | 40 | 70.00 |
| Equisetum arvense L. | Urinary tract infection | 40 | 47 | 85.11 |
| Eruca sativa Mill. | Scabies | 43 | 46 | 93.48 |
| Geranium wallichianum D.Don | Body tonic | 25 | 30 | 83.33 |
| Gymnosporia nemorosa (Eckl. & Zeyh.) Szyszyl | Diarrhea and dysentery | 40 | 46 | 86.96 |
| Helianthus annuus L. | Enhancing egg yield | 38 | 45 | 84.44 |
| Indigofera heterantha Wall. | Abdominal pain | 13 | 15 | 86.67 |
| Linum strictum L. | Increasing the concentration of milk | 24 | 37 | 64.86 |
| Melia azedarach L. | Lactagogue | 3 | 5 | 60.00 |
| Mentha longifolia L | Fever | 24 | 46 | 52.17 |
| Mentha spicata L. | Indigestion | 26 | 44 | 59.09 |
| Monotheca buxifolia (Falc.) A. DC. | Unusual milk taste | 37 | 45 | 82.22 |
| Morus alba L. | Increasing milk production | 28 | 55 | 50.91 |
| Olea europaea L. | Colic | 25 | 43 | 58.14 |
| Peganum harmala L. | Mastitis | 45 | 45 | 100.00 |
| Pennisetum glaucum (L.) R.Br | Enhancing milk production | 12 | 15 | 80.00 |
| Plantago major L. | Foot and mouth disease | 42 | 45 | 93.33 |
| Prunus armeniaca L. | Constipation | 34 | 45 | 75.56 |
| Punica granatum Linn. | Kidney inflammation | 31 | 43 | 72.09 |
| Quercus incana Roxb. | Increasing milk production | 14 | 23 | 60.87 |
| Ricinus communis L. | Expelling the placenta | 40 | 45 | 88.89 |
| Salvadora oleoides Decne. | Lochia | 45 | 45 | 100.00 |
| Solanum melongena L. | Boosting female fertility | 28 | 41 | 68.29 |
| Solanum surattense Brum. F. | Abdominal pain | 39 | 42 | 92.86 |
| Sonchus oleraceus L. | Increasing milk yield | 10 | 19 | 52.63 |
| Tagetes minuta L. | Expelling liver flukes | 12 | 23 | 52.17 |
| Tamarix aphylla (L.) Karst. | Burning wounds | 44 | 47 | 93.62 |
| Trachyspermum ammi L. | Indigestion | 45 | 45 | 100.00 |
| Trianthema portulacastrum L. | Expelling abdominal worms | 35 | 45 | 77.78 |
| Tulipa clusiana DC. | Increasing milk production | 12 | 29 | 41.38 |
| Verbascum thapsus L. | Wound healing | 23 | 43 | 53.49 |
| Vitis negundo Linn. | Stomach disorder | 21 | 39 | 53.85 |
| Withania coagulans (Stocks) Dun. | Abdominal pain | 45 | 45 | 100.00 |
| Xanthium strumarium L. | Wound healing | 6 | 11 | 54.55 |
Discussion
One of the most important income sources for rural populations in the tribal district (North Waziristan) is livestock raising. According to the findings of the present study, farmers in the region rely on plants not only for food for their livestock but also for usage as medications to treat livestock diseases. In the present study, we have documented 56 plant species belonging to 42 families. Khan et al. (65) documented various animal diseases that were cured using indigenous herbal medicines. Similarly, Hassan et al. (34) reported 28 medicinal plants belonging to 23 families for treating various livestock diseases from Lower Dir District of Khyber Pakhtunkhwa, Pakistan. Badar et al. (66) recorded 46 medicinal plants belonging to 31 families for treating 26 various livestock ailments from the district of Jhang, Pakistan. Traditional remedies were little known to the younger generation, but the elders knew a lot more about how to cure livestock problems. These results are in accordance with Zerabruk and Yirga (67) and Khattak et al. (36). They found that the majority of respondents were elderly, with very few youngsters engaging in traditional livestock treatment.
The families that represented the highest number of plant species for the indigenous ethnoveterinary medicines were the Asteraceae (5 spp., 8.93%), followed by Amaranthaceae and Solanaceae (4 spp., 7.14% each). The higher distribution and richness of medicinal plant species from the aforementioned families might be linked to their dominance in the area (68). Furthermore, the widespread use of species from these groups might be linked to the existence of beneficial bioactive chemicals (69, 70) that protect livestock against diseases (71). Moreover, it was revealed that herbs were the most used growth form by the inhabitants, with 32 species (57.14%). They were followed by shrubs and trees (12 spp., 21.43% each). Herbaceous plants are also widely used in other parts of the world (72). The dominant use of herbs was also documented in other ethnoveterinary studies carried out by various researchers around the world (20, 21, 36, 37, 54, 73, 74). Indigenous healers used herbs most often as medication due to their availability in nature (75, 76), which are used by local people for the treatment of 45 animal diseases (blood in urine, bone injury, colic, indigestion, after-birth retention, constipation, milk production, foot and mouth disease, mastitis, and diarrhea, etc.). These diseases are usually observed in various animals, i.e., sheep, cows, goats, buffaloes, and horses.
The aboriginal people were collecting various plant parts (i.e., fruit, seeds, roots, bark, leaves, stems, aerial parts, and whole plants) used in the preparation of various remedies. Some important plants that are present but not in abundance are severely threatened due to maximum collection, trading, and grazing. The most frequently used plant parts are leaves (18, or 18.4% each), followed by seeds (6, or 6.1% each), fruits (6, or 6.1% each), whole plants (4, or 4.1% each), and roots and bark (2, or 2.0% each). Throughout the world, ethnic communities use leaves for the preparation of herbal ethnoveterinary medicine (77, 78). Similar findings were reported by Erarslan and Kultur (79); they reported that the local inhabitants of Turkey used leaves for most ethnoveterinary remedies. Poffenberger et al. (80) found that collecting leaves does not constitute a major threat to plant species' survival as compared to collecting underground parts such as stems, bark, or the entire plant. The usage of certain plant parts implies that these portions have the most therapeutic potential, although biochemical testing is required as well as pharmaceutical screening to double-check the location information (34). Traditional knowledge about indigenous ethnomedicine is mainly transmitted by oral tradition from generation to generation without any written record. Such practices are still common among rural and tribal communities in many parts of the world. Aged and uneducated people were more familiar with the preparation and use of remedies. The addition of scientifically validated ethnoveterinary applications in rural areas helps in poor quality improvement and raises livestock production (15, 81).
The common mode of application/administration is oral application (48 spp., 81.36%). The majority of remedies were administered orally in the study area for the treatment of different ailments. Similar results were also documented in previously reported literature (82). In the present work, some of the therapeutic properties of the plant species mentioned have already been validated based on pharmacology. For example, Kumar and Roy (83) prove practically that C. procera latex is used against inflammation. But the administration of ethnoveterinary recipes is a huge problem in the area because there is no standardized measurement unit for the plant remedies. Although the dosage was determined by using glass, cups, and plant parts like seeds and bulbs, the amount of dosage is usually dependent on the age, intensity of disease, and size of the animal. This type of dose measurement method is not appropriate. That is why veterinarians are dissatisfied with EVMs (84–86). The most dominant method for the preparation of remedies was powder, which was used in the treatment of animal diseases and showed similar results to the previously documented literature (87). However, the most common procedure of drug preparation, according to Deeba et al. (88) is grinding or crushing followed by soaking or boiling. In many cases, the procedure of medicine preparation differs from individual to individual person to the next. Traditional veterinary therapists preferred the same plant for treating the same disease in different ways (34).
In the present study, with 230 use reports, gastrointestinal disorder had the highest ICF value (0.92), followed by general health ailments (0.88) and parasitic diseases (0.87). The maximum number of informant citations for these infections indicates a high frequency of these ailments in the area. It has previously been reported that stomach disorders are more prevalent in lactating livestock, possibly as a result of poor feed and drinking water quality (89, 90). Medicinal plants utilized to treat disease categories with high ICF values are likely to have high potency, making them potential candidates for pharmacological and phytochemical research (91). The fidelity value of a medicinal plant species determines whether it is preferred for the treatment of a specific ailment (63). In the present survey, four medicinal plants, viz., Trachyspermum ammi, Salvadora oleoides, Peganum harmala, and Withania coagulans, were the most important medicinal plants that were particularly used to treat indigestion, lochia, mastitis, and abdominal pain, as determined by 45 interviewers with 100% fidelity. Moreover, Berberis lycium was found as the 2nd most important ethnoveterinary plant, having 97.78% FL and was reported as a body tonic, and Aloe vera was the 3rd most important medicinal plant, with 97.50% FL, used for respiratory problems. The maximum level of fidelity is always gained by widely utilized medicinal plants for specific ailments (90).
Conclusion
This is the first ever study to document medicinal plants that are being used by the shepherds of North Waziristan, Pakistan, to treat livestock diseases. Due to modernization, the younger generations do not pay attention to the traditional knowledge of plants, and this knowledge was restricted only to shepherds, herders, farmers, and the elderly. Therefore, the present study is an important contribution to preserving the botanical wisdom of the local communities in treating animal diseases. The results showed that 56 medicinal plants are used in treating 45 diseases, of which 12 plant species are used in enhancing milk production. Among the highest uses of plants, five species, viz., Trachyspermum ammi, Salvadora oleoides, Peganum harmala, and Withania coagulans, were particularly used to treat indigestion, lochia, mastitis, and abdominal pain. Based on the results, it can be concluded that phytochemical and pharmacological screening of these plants is required to isolate the bioactive compounds, coupled with in vitro and in vivo studies for the reported veterinary diseases.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the first author.
Author Contributions
SR collected the data. SR, RQ, and IR analyzed and interpreted the data and results. IR and SR wrote first draft of the manuscript. SS, IK, AH, A-BA-A, KA, EA, NA, MK, and FI helped in gathering literature and discussion section. AH, A-BA-A, EA, and FI helped in revising the manuscript. ZI and RQ supervised the work. All authors have read and approved the final manuscript.
Funding
The authors would like to extend their sincere appreciation to Researchers Supporting Project Number RSP-2021/356, King Saud University, Riyadh, Saudi Arabia.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are thankful to the local community members of the study area for sharing their valuable information. This manuscript is part of the PhD dissertation of the first author. The authors would like to extend their sincere appreciation to Researchers Supporting Project Number RSP-2021/356, King Saud University, Riyadh, Saudi Arabia.
References
- 1.Bussmann RW, Paniagua Zambrana NY, Ur Rahman I, Kikvidze Z, Sikharulidze S, Kikodze D, et al. Unity in diversity—food plants and fungi of Sakartvelo (Republic of Georgia), Caucasus. J Ethnobiol Ethnomed. (2021) 17:1–46. 10.1186/s13002-021-00490-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oliveira M, Hoste H, Custodio L. A systematic review on the ethnoveterinary uses of Mediterranean salt-tolerant plants: exploring its potential use as fodder, nutraceuticals or phytotherapeutics in ruminant production. J Ethnopharmacol. (2021) 267:113464. 10.1016/j.jep.2020.113464 [DOI] [PubMed] [Google Scholar]
- 3.Shaheen H, Qureshi R, Qaseem MF, Bruschi P. The fodder grass resources for ruminants: a indigenous treasure of local communities of Thal desert Punjab, Pakistan. PLoS ONE. (2020) 15:e0224061. 10.1371/journal.pone.0224061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahman IU, Afzal A, Iqbal Z, Ijaz F, Ali N, Shah M, et al. Historical perspectives of ethnobotany. Clin Dermatol. (2019), 37: 382–8. 10.1016/j.clindermatol.2018.03.018 [DOI] [PubMed] [Google Scholar]
- 5.Scheel-Ybert R, Bachelet C. A good place to live: plants and people at the Santa Elina rock shelter (Central Brazil) from Late Pleistocene to the Holocene. Lat Am Antiq. (2020) 31:273–91. 10.1017/laq.2020.3 [DOI] [Google Scholar]
- 6.Ahmed J, Rahman IU, AbdAllah EF, Ali N, Shah AH, Ijaz F, et al. Multivariate approaches evaluated in the ethnoecological investigation of Tehsil Oghi, Mansehra, Pakistan. Acta Ecol Sin. (2019) 39: 443–50. 10.1016/j.chnaes.2018.11.006 [DOI] [Google Scholar]
- 7.McCorkle CM, Schilihorn-van-Veen TW. Ethnoveterinary research & development. (Studies in Indigenous Knowledge and Development). Intermediate Technology Publications. (1996). p. 450. [Google Scholar]
- 8.Güler O, Polat R, Karaköse M, Çakilcioglu U, Akbulut S. An ethnoveterinary study on plants used for the treatment of livestock diseases in the province of Giresun (Turkey). South African J Bot. (2021) 142:53–62. 10.1016/j.sajb.2021.06.003 [DOI] [Google Scholar]
- 9.Prakash P, Kumar M, Pundir A, Puri S, Prakash S, Kumari N, et al. Documentation of commonly used ethnoveterinary medicines from wild plants of the high mountains in Shimla District, Himachal Pradesh, India. Horticulturae. (2021) 7:351. 10.3390/horticulturae7100351 [DOI] [Google Scholar]
- 10.Chaachouay N, Azeroual A, Bencharki B, Douira A, Zidane L. Ethnoveterinary medicines plants for animal therapy in the Rif, North of Morocco. South African J Bot. (2022) 147:176–91. 10.1016/j.sajb.2021.12.037 [DOI] [Google Scholar]
- 11.Scialabba NE-H. “Full-cost accounting for decision-making related to livestock systems,” in Managing Health Livestock Production and Consumption (Academic Press; ), p. 223–44. 10.1016/B978-0-12-823019-0.00026-X [DOI] [Google Scholar]
- 12.Akhtar MS, Iqbal Z, Khan MN, Lateef M. Anthelmintic activity of medicinal plants with particular reference to their use in animals in the Indo–Pakistan subcontinent. Small Rumin Res. (2000) 38:99–107. 10.1016/S0921-4488(00)00163-2 [DOI] [Google Scholar]
- 13.Hassen A, Muche M, Muasya AM, Tsegay BA. Exploration of traditional plant-based medicines used for livestock ailments in northeastern Ethiopia. South African J Bot. (2022) 146:230–42. 10.1016/j.sajb.2021.10.018 [DOI] [Google Scholar]
- 14.Agani ZA, Boko C, Orou DB, Dossou J, Babatounde S. Ethnoveterinary study of galactogenic recipes used by ruminant breeders to improve milk production of local cows in Benin Republic. J Ethnopharmacol. (2022) 285:114869. 10.1016/j.jep.2021.114869 [DOI] [PubMed] [Google Scholar]
- 15.Mathias E. Ethnoveterinary medicine in the era of evidence-based medicine: mumbo-jumbo, or a valuable resource? Vet J. (2006) 173:241–2. 10.1016/j.tvjl.2005.12.005 [DOI] [PubMed] [Google Scholar]
- 16.Oyda S. Review on traditional ethno-veterinary medicine and medicinal plants used by indigenous people in Ethiopia: practice and application system. Int J Res. (2017) 5:109–19. 10.29121/granthaalayah.v5.i8.2017.2193 [DOI] [Google Scholar]
- 17.Wanzala W, Zessin KH, Kyule NM, Baumann MPO, Mathia E, Hassanali A. Ethnoveterinary medicine: a critical review of its evolution, perception, understanding and the way forward. Livestock Research for Rural Development (2005). [Google Scholar]
- 18.Stucki K, Cero MD, Vogl CR, Ivemeyer S, Meier B, Maeschli A, et al. Ethnoveterinary contemporary knowledge of farmers in pre-alpine and alpine regions of the Swiss cantons of Bern and Lucerne compared to ancient and recent literature – Is there a tradition? J Ethnopharmacol. (2019) 234:225–44. 10.1016/j.jep.2018.12.022 [DOI] [PubMed] [Google Scholar]
- 19.McGaw LJ, Famuyide IM, Khunoana ET, Aremu AO. Ethnoveterinary botanical medicine in South Africa: a review of research from the last decade (2009 to 2019). J Ethnopharmacol. (2020) 257:112864. 10.1016/j.jep.2020.112864 [DOI] [PubMed] [Google Scholar]
- 20.Tabuti JRS, Dhillion SS, Lye KA. Ethnoveterinary medicines for cattle (Bos indicus) in Bulamogi county, Uganda: plant species and mode of use. J Ethnopharmacol. (2003) 88:279–86. 10.1016/S0378-8741(03)00265-4 [DOI] [PubMed] [Google Scholar]
- 21.Khan K, Rahman IU, Soares EC, Ali N, Ijaz F, Calixto ES, et al. Ethnoveterinary therapeutic practices and conservation status of the medicinal flora of Chamla Valley, Khyber Pakhtunkhwa, Pakistan. Front Vet Sci. (2019) 6:122. 10.3389/fvets.2019.00122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin JH, Kaphle K, Wu LS, Yang NYJ, Lu G, Yu C, et al. Sustainable veterinary medicine for the new era. Rev Sci Tech Int des épizooties. (2003) 22:949–64. 10.20506/rst.22.3.1451 [DOI] [PubMed] [Google Scholar]
- 23.Mwale M, Masika PJ. Ethno-veterinary control of parasites, management and role of village chickens in rural households of Centane district in the Eastern Cape, South Africa. Trop Anim Health Prod. (2009) 41:1685–93. 10.1007/s11250-009-9366-z [DOI] [PubMed] [Google Scholar]
- 24.Adekunmi AO, Ajiboye A, Awoyemi AO, Osundare FO, Oluwatusin FM, Toluwase SOW, et al. Assessment of ethno-veterinary management practices among sheep and goat farmers in Southwest Nigeria. Annu Res Rev Biol. (2020) 35:42–51. 10.9734/arrb/2020/v35i330199 [DOI] [Google Scholar]
- 25.Raheem A, Hassan MY, Shakoor R. Bioenergy from anaerobic digestion in Pakistan: Potential, development and prospects. Renew Sustain Energy Rev. (2016) 59:264–75. 10.1016/j.rser.2016.01.010 [DOI] [Google Scholar]
- 26.Nanda AS, Nakao T. Role of buffalo in the socioeconomic development of rural Asia: current status and future prospectus. Anim Sci J. (2003) 74:443–55. 10.1046/j.1344-3941.2003.00138.x [DOI] [Google Scholar]
- 27.Akbar N, Nasir M, Naeem N, Ahmad M-D, Iqbal S, Rashid A, et al. Occurrence and seasonal variations of aflatoxin M1 in milk from Punjab, Pakistan. Toxins. (2019) 11:574. 10.3390/toxins11100574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hashmi HA, Belgacem AO, Behnassi M, Javed K, Baig MB. “Impacts of Climate Change on Livestock and Related Food Security Implications—Overview of the Situation in Pakistan and Policy Recommendations,” In; Emerging Challenges to Food Production and Security in Asia, Middle East, and Africa (Springer; ). [Google Scholar]
- 29.Ganesan S, Chandhirasekaran M, Selvaraj A. Ethnoveterinary healthcare practices in southern districts of Tamil Nadu. Ind. J. Tradition. Knowl. (2008) 7:347–54. [Google Scholar]
- 30.Rahman IU, Hart R, Afzal A, Iqbal Z, Ijaz F, Abd_Allah EF, et al. A new ethnobiological similarity index for the evaluation of novel use reports. Appl Ecol Environ Res. (2019) 17:2765–77. 10.15666/aeer/1702_27652777 [DOI] [Google Scholar]
- 31.Xiong Y, Long C. An ethnoveterinary study on medicinal plants used by the Buyi people in Southwest Guizhou, China. J Ethnobiol Ethnomed. (2020) 16:1–20. 10.1186/s13002-020-00396-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pandey AK, Kumar P, Saxena MJ. “Feed Additives in Animal Health,” In Nutraceuticals In Veterinary Medicine (Cham: Springer; ). p. 345–62. [Google Scholar]
- 33.Leeflang P. Some observations on ethnoveterinary medicine in Northern Nigeria. Vet Q. (1993) 15:72–4. 10.1080/01652176.1993.9694376 [DOI] [PubMed] [Google Scholar]
- 34.Hassan HU, Murad W, Tariq A, Ahmad A. Ethnoveterinary study of medicinal plants in Malakand Valley, district Dir (lower), Khyber Pakhtunkhwa, Pakistan. Ir Vet J. (2014) 67:1–6. 10.1186/2046-0481-67-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rahman IU, Afzal A, Iqbal Z, Hart R, Abd_Allah EF, Hashem A, et al. Herbal teas and drinks: folk medicine of the Manoor valley, Lesser Himalaya, Pakistan. Plants. (2019) 8:1–18. 10.3390/plants8120581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khattak NS, Nouroz F, Rahman IU, Noreen S. Ethno veterinary uses of medicinal plants of district Karak, Pakistan. J Ethnopharmacol. (2015) 171:273–9. 10.1016/j.jep.2015.05.048 [DOI] [PubMed] [Google Scholar]
- 37.Bhardwaj AK, Lone PA, Dar M, Parray JA, Shah KW. Ethnoveterinary medicinal uses of plants of district Bandipora of Jammu and Kashmir, India. Int J Trad Nat Med. (2013) 2:164–78. [Google Scholar]
- 38.Kumar M, Rawat S, Nagar B, Kumar A, Pala NA, Bhat JA, et al. Implementation of the use of ethnomedicinal plants for curing diseases in the Indian Himalayas and its role in sustainability of livelihoods and socioeconomic development. Int J Environ Res Public Health. (2021) 18:1509. 10.3390/ijerph18041509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haq SM, Yaqoob U, Calixto ES, Rahman IU, Hashem A, Abd_Allah EF, et al. Plant resources utilization among different ethnic groups of Ladakh in trans-Himalayan region. Biology. (2021) 10:827. 10.3390/biology10090827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khan KU, Shah M, Ahmad H, Khan SM, Rahman IU, Iqbal Z, et al. Exploration and local utilization of medicinal vegetation naturally grown in the Deusai plateau of Gilgit, Pakistan. Saudi J Biol Sci. (2018) 25:326–31. 10.1016/j.sjbs.2017.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kulkarni S, Kulkarni DK, Deo AD, Pande AB, Bhagat RL. Use of ethno-veterinary medicines (EVM) from Vidarbha region (MS) India. Biosci Discov. (2014) 5:180–6. [Google Scholar]
- 42.Lans C, Turner N, Khan T, Brauer G, Boepple W. Ethnoveterinary medicines used for ruminants in British Columbia, Canada. J Ethnobiol Ethnomed. (2007) 3:11. 10.1186/1746-4269-3-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mayer M, Vogl CR, Amorena M, Hamburger M, Walkenhorst M. Treatment of organic livestock with medicinal plants: a systematic review of European ethnoveterinary research. Complement Med Res. (2014) 21:375–86. 10.1159/000370216 [DOI] [PubMed] [Google Scholar]
- 44.Hammond JA, Fielding D, Bishop SC. Prospects for plant anthelmintics in tropical veterinary medicine. Vet Res Commun. (1997) 21:213–28. 10.1023/A:1005884429253 [DOI] [PubMed] [Google Scholar]
- 45.Farooq Z, Iqbal Z, Mushtaq S, Muhammad G, Iqbal MZ, Arshad M. Ethnoveterinary practices for the treatment of parasitic diseases in livestock in Cholistan desert (Pakistan). J Ethnopharmacol. (2008) 118:213–9. 10.1016/j.jep.2008.03.015 [DOI] [PubMed] [Google Scholar]
- 46.Dilshad SMR, Rehman NU, Ahmad N, Iqbal A. Documentation of ethnoveterinary practices for mastitis in dairy animals in Pakistan. Pak Vet J. (2010) 30:167–71. [Google Scholar]
- 47.Zia-ud-Din S, Zafar I, Khan MN, Jonsson NN, Muhammad S. Documentation of ethnoveterinary practices used for treatment of different ailments in a selected hilly area of Pakistan. Int J Agric Biol. (2010) 12:353–8. [Google Scholar]
- 48.Shoaib G, Shah G-M, Shad N, Dogan Y, Siddique Z, Shah A-H, et al. Traditional practices of the ethnoveterinary plants in the Kaghan Valley, Western Himalayas-Pakistan. Rev Biol Trop. (2021) 69:1–11. 10.15517/rbt.v69i1.42021 [DOI] [Google Scholar]
- 49.Siddique Z, Shad N, Shah GM, Naeem A, Yali L, Hasnain M, et al. Exploration of ethnomedicinal plants and their practices in human and livestock healthcare in Haripur District, Khyber Pakhtunkhwa, Pakistan. J Ethnobiol Ethnomed. (2021) 17:1–22. 10.1186/s13002-021-00480-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Adnan M, Ullah I, Tariq A, Murad W, Azizullah A, Khan AL, et al. Ethnomedicine use in the war affected region of northwest Pakistan. J Ethnobiol Ethnomed. (2014) 10:1–16. 10.1186/1746-4269-10-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aziz MA, Adnan M, Khan AH, Sufyan M, Khan SN. Cross-cultural analysis of medicinal plants commonly used in ethnoveterinary practices at South Waziristan Agency and Bajaur agency, federally administrated tribal areas (FATA), Pakistan. J Ethnopharmacol. (2018) 210:443–68. 10.1016/j.jep.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 52.Ali M, Aldosari A, Tng DYP, Ullah M, Hussain W, Ahmad M, et al. Traditional uses of plants by indigenous communities for veterinary practices at Kurram District, Pakistan. Ethnobot Res Appl. (2019) 18:1–19. 10.32859/era.18.24.1-19 [DOI] [Google Scholar]
- 53.Rahman IU, Afzal A, Iqbal Z, Ijaz F, Ali N, Bussmann RW. Traditional and ethnomedicinal dermatology practices in Pakistan. Clin Dermatol. (2018) 36:310–9. 10.1016/j.clindermatol.2018.03.016 [DOI] [PubMed] [Google Scholar]
- 54.Monteiro MVB, Bevilaqua CML, Palha M das DC, Braga RR, Schwanke K, Rodrigues ST, et al. Ethnoveterinary knowledge of the inhabitants of Marajó Island, Eastern Amazonia, Brazil. Acta Amaz. (2011) 41:233–42. 10.1590/S0044-59672011000200007 [DOI] [Google Scholar]
- 55.Ijaz F. Biodiversity and Traditional Uses of Plants of Sarban Hills. Abbottabad: (2014). [Google Scholar]
- 56.Ijaz F, Rahman I, Iqbal Z, Alam J, Ali N, Khan S. “Ethno-ecology of the healing forests of Sarban Hills, Abbottabad, Pakistan: an economic and medicinal appraisal,” In; Plant and Human Health. Ozturk M, Hakeem KR. editors. Berlin/Heidelberg, Germany: Springer International Publishing AG. [Google Scholar]
- 57.Nasir E, Ali SI. Flora West of Pakistan. University of Karachi, Karachi and National Herbarium, Islamabad (1971). [Google Scholar]
- 58.Ali SI, Qaiser M. Flora of Pakistan. Karachi: Department of Botany, University of Karachi; (1995). [Google Scholar]
- 59.Ali SI, Nasir YJ. Flora of Pakistan. Islamabad: Department of Botany, University of Karachi, Karachi and National Herbarium; (1989). [Google Scholar]
- 60.Ijaz F, Iqbal Z, Rahman IU, Alam J, Khan SM, Shah GM, et al. Investigation of traditional medicinal floral knowledge of Sarban Hills, Abbottabad, KP, Pakistan. J Ethnopharmacol. (2016) 179:208–33. 10.1016/j.jep.2015.12.050 [DOI] [PubMed] [Google Scholar]
- 61.Rahman IU, Ijaz F, Afzal A, Iqbal Z, Ali N, Khan SM. Contributions to the phytotherapies of digestive disorders: traditional knowledge and cultural drivers of Manoor Valley, Northern Pakistan. J Ethnopharmacol. (2016) 192:30–52. 10.1016/j.jep.2016.06.049 [DOI] [PubMed] [Google Scholar]
- 62.Rahman IU, Ijaz F, Iqbal Z, Afzal A, Ali N, Afzal M, et al. Novel survey of the ethno medicinal knowledge of dental problems in Manoor Valley (Northern Himalaya), Pakistan. J Ethnopharmacol. (2016) 194:877–94. 10.1016/j.jep.2016.10.068 [DOI] [PubMed] [Google Scholar]
- 63.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. (1986) 16:275–87. 10.1016/0378-8741(86)90094-2 [DOI] [PubMed] [Google Scholar]
- 64.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers' consensus and cultural importance. Soc Sci Med. (1998) 47:1859–71. 10.1016/S0277-9536(98)00181-6 [DOI] [PubMed] [Google Scholar]
- 65.Khan MA, Ullah A, Rashid A. Ethnoveterinary medicinal plants practices in district Peshawar, Khyber Pakhtunkhwa Pakistan. Pak J Bot. (2015) 47:105–14. [Google Scholar]
- 66.Badar N, Iqbal Z, Sajid MS, Rizwan HM, Jabbar A, Babar W, et al. Documentation of ethnoveterinary practices in district Jhang, Pakistan. J Anim Plant Sci. (2017) 27:398–406. [Google Scholar]
- 67.Zerabruk S, Yirga G. Traditional knowledge of medicinal plants in Gindeberet district, Western Ethiopia. South African J Bot. (2012) 78:165–9. 10.1016/j.sajb.2011.06.006 [DOI] [Google Scholar]
- 68.Rahman IU. Ecophysiological Plasticity and Ethnobotanical Studies in Manoor Area, Kaghan Valley, Pakistan (2020) [Google Scholar]
- 69.El-Saadony MT, Zabermawi NM, Zabermawi NM, Burollus MA, Shafi ME, Alagawany M, et al. Nutritional aspects and health benefits of bioactive plant compounds against infectious diseases: a review. Food Rev Int. (2021) 1–23. 10.1080/87559129.2021.194418330716999 [DOI] [Google Scholar]
- 70.Rahman IU, Bussmann RW, Afzal A, Iqbal Z, Ali N, Ijaz F. “Folk Formulations of Asteraceae Species as Remedy for Different Ailments in Lesser Himalayas, Pakistan,” In; Ethnobiology of Mountain Communities in Asia. Abbasi AM, Bussmann RW. editors. Berlin/Heidelberg, Germany: Springer International Publishing AG. [Google Scholar]
- 71.Gazzaneo LRS, de Lucena RFP, de Albuquerque UP. Knowledge and use of medicinal plants by local specialists in an region of Atlantic Forest in the state of Pernambuco (Northeastern Brazil). J Ethnobiol Ethnomed. (2005) 1:9. 10.1186/1746-4269-1-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Addo-Fordjour P, Belford EJD, Akonnor D. Diversity and conservation of medicinal plants in the Bomaa community of the Brong Ahafo region, Ghana. J Med plants Res. (2013) 2:226–33. [Google Scholar]
- 73.Tadesse B, Mulugeta G, Fikadu G, Sultan A, Nekemte E. Survey on ethno-veterinary medicinal plants in selected Woredas of east Wollega zone, western Ethiopia. J Biol Agric Healthc. (2014) 4:97–105. [Google Scholar]
- 74.Birhanu T, Abera D. Survey of ethno-veterinary medicinal plants at selected Horro Gudurru Districts, Western Ethiopia. African J Plant Sci. (2015) 9:185–92. 10.5897/AJPS2014.1229 [DOI] [Google Scholar]
- 75.Uniyal SK, Singh KN, Jamwal P, Lal B. Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. J Ethnobiol Ethnomed. (2006) 2:1–8. 10.1186/1746-4269-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sanz-Biset J, Campos-de-la-Cruz J, Epiquién-Rivera MA, Canigueral S. A first survey on the medicinal plants of the Chazuta valley (Peruvian Amazon). J Ethnopharmacol. (2009) 122:333–62. 10.1016/j.jep.2008.12.009 [DOI] [PubMed] [Google Scholar]
- 77.Ullah M, Khan MU, Mahmood A, Malik RN, Hussain M, Wazir SM, et al. An ethnobotanical survey of indigenous medicinal plants in Wana district south Waziristan agency, Pakistan. J Ethnopharmacol. (2013) 150:918–24. 10.1016/j.jep.2013.09.032 [DOI] [PubMed] [Google Scholar]
- 78.Vijayakumar S, Yabesh JEM, Prabhu S, Manikandan R, Muralidharan B. Quantitative ethnomedicinal study of plants used in the Nelliyampathy hills of Kerala, India. J Ethnopharmacol. (2015) 161:238–54. 10.1016/j.jep.2014.12.006 [DOI] [PubMed] [Google Scholar]
- 79.Erarslan ZB, Kultur S. Ethnoveterinary medicine in Turkey: a comprehensive review. Turkish J Vet Anim Sci. (2019) 43:55–582. 10.3906/vet-1904-8 [DOI] [Google Scholar]
- 80.Poffenberger M, McGean B, Khare A, Campbell J. Community Forest Economy and Use Patterns: Participatory Rural Appraisal (PRA) Methods in South Gujarat, India, Volumes 1 and 2. Jt For Manag Support Program, Ford Found New Delhi (1992). [Google Scholar]
- 81.Iqbal Z, Jabbar A, Akhtar MS, Muhammad G, Lateef M. Possible role of ethnoveterinary medicine in poverty reduction in Pakistan: use of botanical anthelmintics as an example. J Agric Soc Sci. (2005) 1:187–95. [Google Scholar]
- 82.Chermat S, Gharzouli R. Ethnobotanical study of medicinal flora in the North East of Algeria-an empirical knowledge in Djebel Zdimm (Setif). J Mater Sci Eng. (2015) 5:50–9. 10.17265/2161-6213/2015.1-2.007 [DOI] [Google Scholar]
- 83.Kumar VL, Roy S. Calotropis procera latex extract affords protection against inflammation and oxidative stress in Freund's complete adjuvant-induced monoarthritis in rats. Mediators Inflamm. (2007) 2007:047523. 10.1155/2007/47523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Niwa Y, Miyachi Y, Ishimoto K, Kanoh T. Why are natural plant medicinal products effective in some patients and not in others with the same disease? Planta Med. (1991) 57:299–304. 10.1055/s-2006-960102 [DOI] [PubMed] [Google Scholar]
- 85.Bakhiet AO, Adam SE. Therapeutic utility, constituents and toxicity of some medicinal plants: a review. Vet Hum Toxicol. (1995) 37:255–8. [PubMed] [Google Scholar]
- 86.Longuefosse J-L, Nossin E. Medical ethnobotany survey in Martinique. J Ethnopharmacol. (1996) 53:117–42. 10.1016/0378-8741(96)01425-0 [DOI] [PubMed] [Google Scholar]
- 87.Aziz MA, Khan AH, Pieroni A. Ethnoveterinary plants of Pakistan: a review. J Ethnobiol Ethnomed. (2020) 16:1–18. 10.1186/s13002-020-00369-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Deeba F, Muhammad G, Iqbal Z, Hussain I. Appraisal of ethno-veterinary practices used for different ailments in dairy animals in peri-urban areas of Faisalabad (Pakistan). Int J Agric Biol. (2009) 11:535–41. [Google Scholar]
- 89.Luseba D, Van der Merwe D. Ethnoveterinary medicine practices among Tsonga speaking people of South Africa. Onderstepoort J Vet Res. (2006) 73:115–22. 10.4102/ojvr.v73i2.156 [DOI] [PubMed] [Google Scholar]
- 90.Meen ML, Dudi A, Singh D. Ethnoveterinary study of medicinal plants in a tribal society of Marwar region of Rajasthan, India. J Pharmacogn Phytochem. (2020) 9:549–54. [Google Scholar]
- 91.Khan MA, Khan MA, Hussain M. Ethno veterinary medicinal uses of plants of Poonch valley Azad Kashmir. Pakistan J Weed Sci Res. (2012) 18:495–507. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the first author.