Abstract
Background
Telemedicine plays an important role in the management of inflammatory bowel disease (IBD), particularly during a pandemic such as COVID-19. However, the effectiveness and efficiency of telemedicine in managing IBD are unclear.
Objective
This systematic review and meta-analysis aimed to compare the impact of telemedicine with that of standard care on the management of IBD.
Methods
We systematically searched the PubMed, Cochrane Library, EMBASE, Web of Science, and Scopus databases on April 22, 2020. Randomized controlled trials comparing telemedicine with standard care in patients with IBD were included, while conference abstracts, letters, reviews, laboratory studies, and case reports were excluded. The IBD-specific quality of life (QoL), disease activity, and remission rate in patients with IBD were assessed as primary outcomes, and the number of in-person clinic visits per patient, patient satisfaction, psychological outcome, and medication adherence were assessed as secondary outcomes. Review Manage 5.3 and Stata 15.1 were used for data analysis.
Results
A total of 17 randomized controlled trials (2571 participants) were included in this meta-analysis. The telemedicine group had higher IBD-specific QoL than the standard care group (standard mean difference 0.18, 95% CI 0.01 to 0.34; P.03). The number of clinic visits per patient in the telemedicine group was significantly lower than that in the standard care group (standard mean difference −0.71, 95% CI −1.07 to −0.36; P<.001). Subgroup analysis showed that adolescents in the telemedicine group had significantly higher IBD-specific QoL than those in the standard care group (standard mean difference 0.42, 95% CI 0.15 to 0.69; I2=0; P.002), but there was no significant difference between adults in the 2 groups. There were no significant differences in disease activity, remission rate, patient satisfaction, depression, self-efficacy, generic QoL, and medication adherence outcomes between the telemedicine and standard care groups.
Conclusions
Telemedicine intervention showed a promising role in improving IBD-specific QoL among adolescents and decreased the number of clinic visits among patients with IBD. Further research is warranted to identify the group of patients with IBD who would most benefit from telemedicine.
Keywords: telemedicine, inflammatory bowel disease, quality of life, disease activity, mobile phone
Introduction
Inflammatory bowel disease (IBD), including Crohn disease and ulcerative colitis, is a group of chronic inflammatory disorders of the gut. The prevalence of IBD is increasing worldwide, with 3 million cases recorded in the United States in 2015 and 4 million cases projected in Canada by 2030 [1,2]. Because of its recurrent relapsing-remitting nature, IBD exerts a substantial economic and health burden on patients and their families, health organizations, and nations [3,4]. The lack of curative therapy for this condition entails lifelong medication and follow-up that need to be effectively monitored in patients with IBD [5].
Telemedicine was first defined by the World Health Organization as health care service provided to patients at a distance through information communication technologies (ie, SMS text messaging, web-based applications, real-time telephone) [6]. It is a broad term. Although the specific telemedicine subtypes (telemonitoring, tele-education, and teleconsulting) exhibit significant heterogeneity, they are closely tied together by the concept of remote health care resources delivery [7]. Given the convenience of communication technologies, clinicians have been increasingly using eHealth interventions as a supplementary tool to conduct follow-up and provide education, including disease status and medication instruction. Electronic medical technology has been proven to change the course of certain chronic diseases such as diabetes and asthma [8-11]. Patients with IBD, commonly diagnosed as having the condition at a young age and deemed to need lifelong follow-up for long-term remission, could also potentially benefit from telemedicine intervention for preventing disease progression and reducing complications and operation rates [12-14]. Telemedicine has played an important role in the management of IBD during the recent COVID-19 pandemic [15]. Specific tools such as the IBD Monitoring Index for Mobile Health have been developed and validated for clinical management [16-21]. Others tools such as the IBD disk have been adapted to smartphone apps to monitor IBD-associated disability [22,23].
However, there is no consensus on remote health care technology preferences for IBD management because of contradictory results and high heterogeneity among studies. Few studies precisely quantified the magnitude of intervention effects [24-26], although many studies demonstrated that telemedicine had a major impact on the management of IBD [7,27,28]. We aimed to estimate the differences between telemedicine and standard care in the management of IBD by conducting a systematic review and meta-analysis of randomized controlled trials (RCTs).
Methods
This study was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Search Strategy and Selection Criteria
Literature Search Strategy
Two investigators (LLP and ZDL) independently searched publications in the PubMed, Cochrane Library, EMBASE, Web of Science, and Scopus databases (search date April 22, 2020) using the following search terms: (telemedicine OR telemonitor OR e-health OR telehealth OR telecommunication OR telemanagement OR telecare OR (telephone monitoring) OR telenursing OR ((remote and short) message service) OR (mobile health) OR (mobile applications) OR teleconsultation) AND ((inflammatory bowel disease) OR (ulcerative colitis) OR (Crohn’s disease)). The search in the Web of Science, Cochrane Library, and Scopus Google Scholar databases was limited to titles and abstracts. However, no limitations were applied to the search of PubMed and EMBASE. We also manually searched the reference lists and related literature to identify additional publications. The data sets used in this study can be obtained from the corresponding author on request. Records were imported into EndNote X 9.0 software (Clarivate) to eliminate duplications.
Eligibility Criteria and Study Selection
Two authors (LLP and HYL) independently screened the titles, abstracts, and keywords of the identified articles and selected suitable papers for full review. Disagreements were resolved by a third investigator (ZDL) or by consensus.
The studies included had to meet the following PICOS (participants, interventions, control, outcomes, study design) criteria described in Textbox 1 [6].
Inclusion criteria.
1. P (participants)
Patients diagnosed as having IBD
2. I (interventions)
Telemedicine defined as “the use of electronic information and communication technologies for the delivery of health care when there exist distances between patents and health care providers” such as internet, mobile phone applications, and SMS text messaging
3. C (control)
Standard care or usual care provided by the medical center according to IBD treatment guidelines
4. O (outcomes)
At least one of the following outcomes: inflammatory bowel disease–specific quality of life, disease activity, remission rate, generic quality of life, self-efficacy, depression, medication adherence, patient satisfaction, and the number of clinic visits per patient
5. S (study design)
Only randomized controlled trials
The exclusion criteria were as follows: conference abstracts, letters, reviews, laboratory studies, and case reports in which the necessary information could not be extracted; non-English publications; and studies that did not report the outcomes required.
Risk of Bias
Two reviewers (LLP and HYL) independently assessed the quality and risk of bias of the included studies using the Cochrane Handbook of Systematic Reviews of Interventions [29]. In addition, the revised Jadad scale was also applied to assess the quality of the included articles [30]. Any disagreement was resolved by the third reviewer (ZDL).
Data Extraction
Two authors (LLP and HYL) independently extracted data, and disagreements were resolved by a third investigator (ZDL). Extracted data included first author, publication year, country, participant characteristics (age, gender, disease type, and disease activity status), intervention, follow-up time, and outcomes. The investigators contacted authors to obtain original data not reported in the published papers. If the number of telemedicine intervention groups was more than one, amalgamation of these groups was performed. If outcomes were reported more than once, the updated data would be evaluated on priority.
Outcomes and Definitions
Primary outcomes in our study included IBD-specific QoL, disease activity, and remission rate. Secondary outcomes included generic QoL, self-efficacy, depression, medication adherence, patient satisfaction, and the number of in-person clinic visits per patient.
Except the number of clinic visits, reported outcomes were measured by specific questionnaires or scales. For instance, IBD-specific QoL was assessed by the IBD questionnaire (IBDQ) [31]. Disease activity was assessed by the Mayo score, Walmsley index, or Seo index for ulcerative colitis or indeterminate colitis and by the Harvey Bradshaw Index for Crohn disease [32-35]. Additionally, remission rate was defined as the proportion of patients in clinical remission at the endpoint or during the intervention [36,37]. Patient satisfaction was defined by scales (eg, consultation satisfaction questionnaire) evaluating the acceptance of care provided by clinical staff [38].
Data Synthesis and Statistical Analysis
All data were analyzed using Review Manager 5.3 (The Cochrane Collaboration) and Stata 15.1 (StataCorp). We used standardized mean difference (SMD) with 95% CI to calculate continuous variables and relative risk with 95% CI to calculate discontinuous variables. Owing to the heterogeneity between the included studies, we used a random-effects model to assess a relatively more conservative estimate of the 95% CI. Heterogeneity was evaluated using the Cochrane Q statistic and I2 statistic. Subgroup analysis was conducted if needed, focusing on predefined stratification including the follow-up time (<12 months or not) and patient characteristics (adults or adolescents or patients aged above 18 years or not). Funnel plots, Egger test, and Begg test were used to examine potential publication bias.
Results
Search Process, Study Characteristics, and Quality Assessment
A total of 1422 articles were identified after searching the databases, and 2 additional articles were included through search of the references. Of the 711 unique studies obtained after removing duplications, 617 irrelevant articles were eliminated and 94 were assessed in full text. The following publications were excluded: 12 articles because of a lack of accessible full text, 13 because of incomplete data, 7 for being unrelated to the topic, and 11 for failure of randomization; 21 conference abstracts; and 13 reviews. Finally, 17 RCTs were considered potentially eligible and comprised 2571 patients from 2010 to 2020; most of these RCTs were conducted in the United States [39-45], followed by the Netherlands [46-48], New Zealand [49,50], Denmark [12,51], the United Kingdom [52], Spain [53], Ireland [12], and Turkey [13]. The process of selecting enrolled studies is shown in Figure 1.
Figure 1.
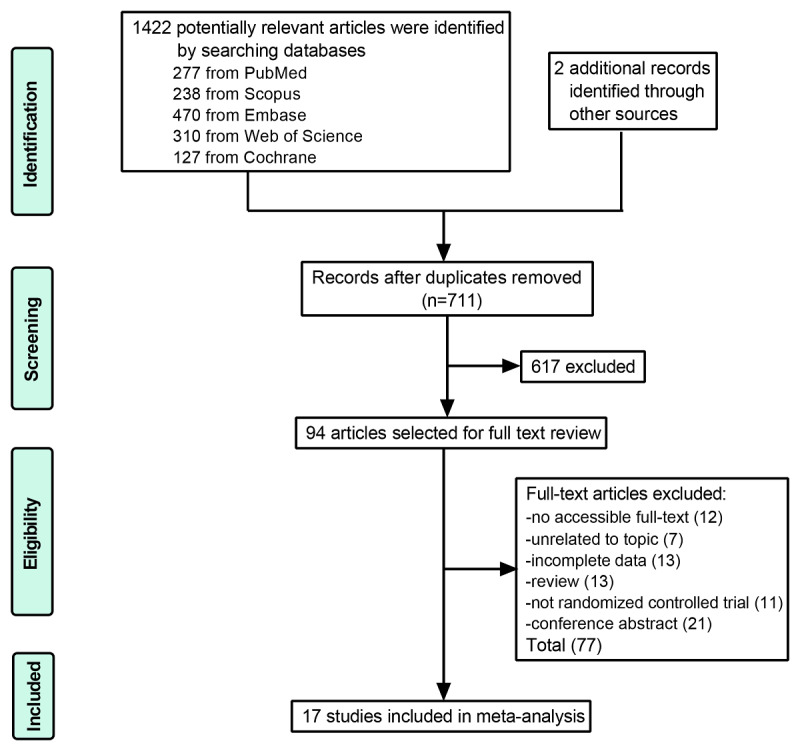
Flow diagram of the selection of enrolled studies.
Table 1 summarizes the key characteristics of the included studies and participants. The results of the revised Jadad scale for the enrolled studies are also shown in Table 1 and indicate that 13 identified studies were of high quality (ranging from 5 to 7). Three of the included studies are from the same clinical trial but report different outcomes. The methodological quality of enrolled studies is shown in Figure 2 and Figure 3.
Table 1.
Characteristics of the included studies and participants.
| Reference | Country | Jadad score | Age (years), mean (SD)/mean (IQR)/mean (range)a |
Male/totala (%) | Participants a, n | Participant characteristics |
Intervention/applicationa |
Follow-up time (months) |
Outcomes |
| Linn et al, 2018 [48] |
Netherlands | 1+1+0+1=3 | 40.84 (14.51) vs 45.21(17.15) |
40.4 vs 51.5 | 52 vs 33 |
|
Telemonitoring through web or SMS text messaging vs usual care | 6 |
|
| Ako Beng et al, 2015 [52] |
United Kingdom | 2+2+0+1=5 | 13.9 (12.1,15.9) vs 13.8 (11.2,15.3) |
68 vs 57 | 44 vs 42 |
|
Teleconsulting through telephone vs usual care |
12 |
|
| Bil Grami et al, 2019d [42] |
United States | 2+2+0+1=5 | 39.7 (13) vs 37.7 (11.6) vs 40.2 (11) |
38.5 vs 47.4 vs 36.9 |
75 vs 72 vs 75 |
|
Telemonitoring and tele-education through mobile phone with SMS text messaging vs standard care | 12 |
|
| Carlsen, 2017 [51] | Denmark | 1+2+1+1=5 | 15.1 (1.82) vs 14.7 (2.11) |
37 vs 46 | 27 vs 26 |
|
Telemonitoring through web-based applications, SMS text messaging, and phone call vs standard care |
24 |
|
| Cross et al, 2012 [39] |
United States | 2+2+0+1=5 | 41.7 (13.9) vs 40.3 (14.4) |
40 vs 32 | 25 vs 22 |
|
Telemonitoring through home unit-server PC provider vs standard care |
12 |
|
| Cross, 2018d [40] |
United States | 2+2+0+1=5 | 40.1 (13.2) vs 36.4 (11.5) vs 40.1 (11.7) |
41.7 vs 43.1 vs 45.3 |
115 vs 116 vs 117 |
|
Telemonitoring and tele-education through mobile phone with SMS text messaging vs standard care |
12 |
|
| De Jong, 2017[47] | Netherlands | 2+2+0+1=5 | 44.0 (±14.1) vs 44.1 (14.2) |
42 vs 41 | 465 vs 444 |
|
Telemonitoring through web-based applications on a tablet or smartphone vs standard care |
12 |
|
| Del Hoyo et al, 2018 and 2019 [18,53] |
Spain | 2+2+0+1=5 | 41.32(19-66) vs 40.91(24-60) vs 39.31(22-61) |
42.9 vs 57.1 vs 57.1 |
21 vs 21 vs 21 |
|
Telemonitoring through a web-based system with smartphone apps or a tablet or through the telephone vs standard care |
6 |
|
| Elkjaer et al, 2010 [12] |
Denmark and Ireland |
2+2+2+1=7 | Denmark: 40 (21-69) vs 44 (21-69) Ireland: 41 (18-66) vs 46 (19-65) |
Denmark: 49.5 vs 31.1 Ireland: 60.8 vs 41.5 |
Denmark: 105 vs 106 Ireland: 51 vs 41 |
|
Tele-education through web-based applications vs usual care | 12 |
|
| Heida et al, 2017 [46] |
Netherlands | 2+2+0+1=5 | 15 (12-16) vs 15 (13-17) |
64 vs 45 | 84 vs 86 |
|
Telemonitoring through web-based applications, email, and phone calls vs usual care |
13 |
|
| Hunt et al, 2017 [44] |
United States | 0+0+0+1=1 | 36 (10) (total participants) |
20.6 (total participants) |
32 vs 31 |
|
Tele-education through cognitive behavioral therapy delivered online vs usual care |
1.5 |
|
| Krier et al, 2011 [45] |
United States | 1+2+1+1=5 | 62.8 (11.5) vs 58.5 (9.6) |
87 vs 68 | 15 vs 19 |
|
Teleconsulting through real-time image vs standard care |
9 |
|
| McCombie et al, 2020 [49] | New Zealand | 2+2+0+1=5 | 35.2 (12.4) vs 34.3 (12.9) |
52 vs 46 | 50 vs 50 |
|
Telemonitoring through smartphone apps vs standard care | 12 |
|
| McCombie et al, 2016 [50] | New Zealand | 2+0+0+1=3 | 38.3 (12.8) vs 39.6 (11.8) |
33.6 vs 38.4 |
113 vs 86 |
|
Tele-education through computerized cognitive behavioral therapy vs usual care | 6 |
|
| Miloh et al, 2017 [43] |
United States | 1+1+1+0=3 | — | — | 21 vs 30 |
|
Telemonitoring through SMS text messaging vs standard care | 12 |
|
| Ozgur Soy et al, 2019 [13] |
Turkey | 2+2+2+1=7 | 37.26(12.99) vs 41.63(11.85) |
56.7 vs 60 |
30 vs 30 |
|
Tele-education through web-based applications on the computer or phone vs standard care |
2 |
|
| Schliep et al, 2020d [41] | United States | 2+2+0+1=5 | 37.3 (11.6) vs 39.3 (13.4) vs 39.5 (12.0) |
45 vs 40.5 vs 37.5 |
71 vs 74 vs 72 |
|
Telemonitoring and tele-education through a mobile phone with SMS text messaging vs standard care | 12 |
|
aThese items were recorded as experimental vs control group.
bIBD: inflammatory bowel disease.
cQoL: quality of life.
dThese studies came from the same clinical trial but reported different outcomes.
Figure 2.
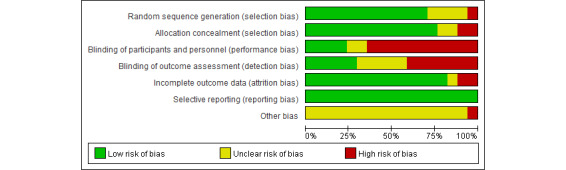
Risk of bias graph.
Figure 3.
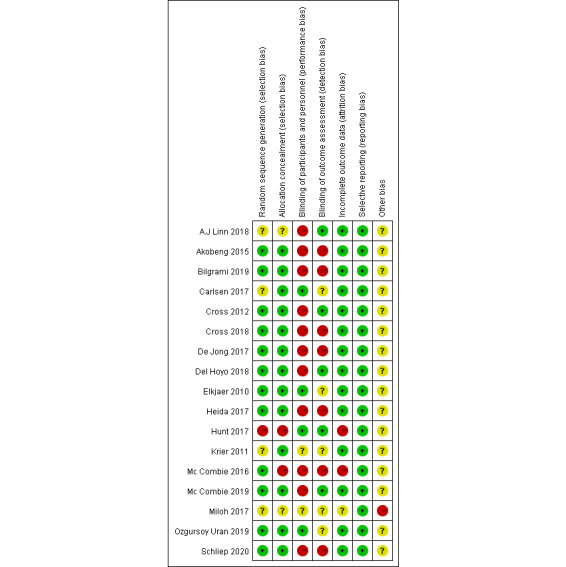
Risk of bias summary.
Primary Outcomes
IBD-Specific Quality of Life
A total of 10 clinical trials including 1632 participants were enrolled to compare IBD-specific QoL in the telemedicine and standard care groups. We found that IBDQ scores were higher in the telemedicine group than in the standard care group (SMD 0.18, 95% CI 0.01 to 0.34; I2=47; P=.03; Figure 4). Subgroup analysis stratified by follow-up time (<12 months or not) and participants characteristics (adults or adolescents) was conducted to examine the relatively high heterogeneity and identify the type of patients in need of telemedicine care. There was no significant difference in the IBDQ scores in the short-term (SMD 0.23, 95% CI −0.22 to 0.68; I2=61; P=0.31) or long-term subgroups (SMD 0.17, 95% CI 0 to 0.34; I2=47; P=.05; Multimedia Appendix 1). Furthermore, adolescents in the telemedicine group had significantly higher IBDQ scores than those in the standard care group (SMD 0.42, 95% CI 0.15 to 0.69; I2=0; P=.002), but no significant difference was found for adults between the groups (SMD 0.11, 95% CI −0.06 to 0.28; I2=41; P=.21; Multimedia Appendix 2).
Figure 4.
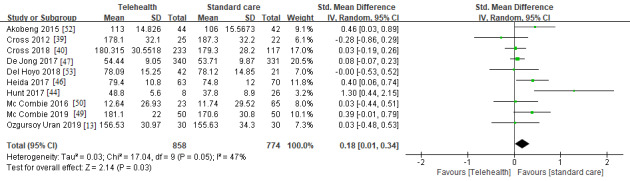
IBD-specific quality of life compared between telemedicine and standard care groups. IBD: inflammatory bowel disease [13,39,40,44,46,47,49,50,52,53].
Funnel plot showed potential publication bias in our meta-analysis (Figure 5), contrary to the results of the Begg (P=.86) and Egger test (P=.26). This inconformity could be explained by the relatively small number of enrolled studies.
Figure 5.
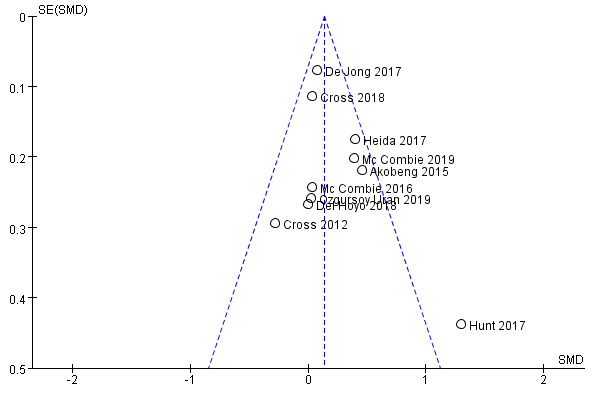
Funnel plot for potential publication bias. SMD: standard mean difference.
Disease Activity and Remission Rate
To examine the effectiveness of telemedicine in managing disease activity, 7 RCTs with a total of 955 patients were included. Disease activity was not significantly different between the telemedicine and standard care groups (SMD 0.08, 95% CI −0.09 to 0.24; I2=0; P=.38; Figure 6). Meanwhile, the remission rate in the telemedicine group was not significantly lower than that in the standard care group (relative risk 0.94, 95% CI, 0.83 to 1.05; I2=6; P=.26; Multimedia Appendix 3).
Figure 6.
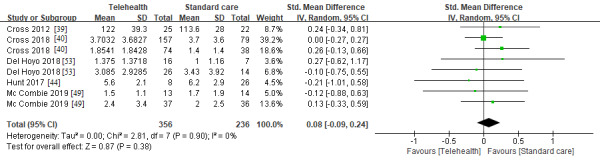
Disease activity in the telemedicine and standard care groups [39,40,44,53].
Secondary Outcomes
Number of Clinic Visits per Patient
To investigate whether telemedicine intervention could lower the number of clinic or outpatient visits, we analyzed 6 articles that included 1479 patients with IBD. The number of clinic visits per patient was significantly lower in the telemedicine group than in the standard care group (SMD −0.71, 95% CI −1.07 to −0.36; I2=85; P<.001; Multimedia Appendix 4).
Patient Satisfaction
In 3 studies that included 183 participants, patient satisfaction was not significantly different between the telemedicine and standard care groups (SMD 0.21, 95% CI −0.12 to 0.54; I2=14; P=0.21; Multimedia Appendix 5).
Psychological Outcomes (Depression, General QoL, and Self-efficacy)
In the assessment of psychological outcomes, 7 clinical trials with 1165 participants showed no significant difference in the mental health of patients with IBD between the telemedicine and standard care groups (SMD −0.31, 95% CI −0.79 to 0.17; I2=66; P=.21 for depression score; SMD 1.37, 95% CI −0.42 to 3.15; I2=97; P=.13 for generic QoL; SMD 0.01, 95% CI −0.16 to 0.17, I2=23%; P=.95 for self-efficacy; Multimedia Appendices 6-8).
Medication Compliance
A total of 5 RCTs with 1169 patients with IBD were included to assess medication compliance. Considering that some articles reported the Morisky Scale score while others merely reported the medication compliance rate, we pooled data into 2 measures (medication compliance score and rate). Medication compliance in the telemedicine group did not improve significantly compared with that in the standard care group in terms of medication compliance score and rate (SMD 0.11, 95% CI −0.09 to 0.30; I2=19; P=.27 and relative risk 1.29, 95% CI 0.77 to 2.17; I2=88; P=.33, respectively; Multimedia Appendix 9).
Discussion
There is high demand for long-term personalized care and medication to maintain remission and reduce the risk of relapse in patients with IBD [5,54]. Because of the convenience of use, telemedicine intervention may play an increasingly important role in managing IBD [27,55]. We aimed to investigate whether patients with IBD could benefit from telemedicine technology by performing a systematic review and meta-analysis. It was evident that enrolled studies exhibited obvious heterogeneity in the specific intervention used. The reason for this heterogeneity could not be identified because of the diversity and physical limitations of the IBD centers delivering telemedicine and their purposes and areas of application. However, regardless of the heterogeneity, we did find that patients who received telemedicine intervention had higher IBDQ scores and a significantly lower number of clinic visits per patient than those who received standard care. Importantly, adolescent patients with IBD benefit more from telemedicine and had significantly higher IBDQ scores that those who received standard care.
One possible reason is that there are more opportunities for the youth to access this relatively new form of care via the internet or mobile phones. Unlike in other chronic diseases (eg, chronic obstructive pulmonary disease), the peak onset of IBD is seen at a younger age [3,56]. This implies that telemedicine would be more acceptable in such patients with IBD. In addition, it seemed obvious that telemedicine could decrease the number of in-person clinic visits compared with standard care. However, none of the studies reported exact data or definitive conclusions on this issue. Considerable time and cost could be saved through the reduction of travel and waiting hours for regular office visits.
Given the robust effects of relapse or disease course on the daily life of patients with IBD, attention should be focused on relieving the psychological burden on these patients [57]. It is necessary to note that telemedicine aiming to improve outcomes in patients with IBD, such as through the incorporation of impactful web-based cognitive behavioral therapy (a form of tele-education), has proven to be an effective method for the management of mental health in patients with chronic gastrointestinal tract diseases [25]. However, our study showed no significant differences in psychological outcomes, such as depression, generic QoL, and self-efficacy, between the telemedicine and standard care groups. One potential explanation is that standard care provided by the referral center had built in emphasis on the importance of mental health care.
Theoretically, patients receiving telemedicine intervention have more access to report a flare than conventional follow-up and therefore receive more prompt consultation from health care givers. However, no significant differences were observed for disease activity and remission rates between these 2 groups in our meta-analysis. The reasons for this may be as follows: most patients were in remission at baseline, which led to a ceiling effect; it remains uncertain whether eHealth technologies could better influence the natural course of IBD compared with standard care; and evaluation of disease activity was based on the score self-reported by patients or their families without objective measurements. Hence, it is difficult to conclusively state the impact of telemedicine intervention on disease activity in patients with IBD.
In terms of therapeutic compliance, medication adherence was adequate in only around 45% of patients with IBD [58]. Nonadherence to medical therapy could cause a 5-fold increase in the risk of relapse, and low medication compliance correlates with lower QoL and higher cost of hospitalizations [59,60]. Thus, there is an urgent need to promote better medication compliance in patients with IBD. Our findings did not show a significant improvement in medication compliance in the telemedicine group, which was inconsistent with the outcomes reported by Rohde et al [26]. It is reasonable to speculate that this may be related to the compliance rate at baseline, as noncompliant patients might be more reluctant to participate in RCTs. Consequently, the participants enrolled are more compliant with the medication, which results in a ceiling effect.
Because of the superiority and popularity of mobile technology, intervention restricted to mobile phones is considered to be promising for the management of chronic diseases [61,62]. Our meta-analysis not only investigated the effectiveness of telemedicine in IBD, but also focused on the specific type of telemedicine, including mobile technology. All enrolled studies in our meta-analysis incorporated mobile devices into the telemedicine intervention, except 2 in which the intervention was confined to a computerized web-based system [45,50]. Therefore, we anticipate that our findings of the use of telemedicine for the management of IBD could also be applied to mobile technology.
Despite the strengths of this meta-analysis, there are certain limitations. First, there was an unavoidable high attrition rate in some studies that used the per protocol analysis. Second, some RCTs did not use the blinded-method design because of intervention characteristic limitations, which led to performance and detection biases. Third, the number of enrolled studies in the meta-analysis was relatively modest, which led to the contradictory results ascribed to potential publication bias. Finally, the specific population that would most benefit from telemedicine could not be identified because of a lack of complete reported data in the included studies.
In conclusion, constrained by the current limited material to provide telemedicine for IBD patients, the heterogeneity of specific telemedicine intervention was obviously evident. However, in accordance with the idea of providing health care from a distance, telemedicine should not be regarded as a uniform therapeutic method as is done for drug treatments but as a mode of health care delivery and even as an important adjuvant to routine clinical practice. Meanwhile, telemedicine intervention did show a promising role in improving IBDQ scores among adolescents and decreased the number of clinic visits by patients with IBD. Further research is needed to identify the patients with IBD who would most benefit from telemedicine.
Acknowledgments
We would like to thank the National Natural Science Foundation of China for providing funding for this meta-analysis. The funder of this study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Abbreviations
- IBD
inflammatory bowel disease
- IBDQ
inflammatory bowel disease questionnaire
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL
quality of life
- RCT
randomized controlled trial
Subgroup analysis of the inflammatory bowel disease questionnaire comparing the telemedicine with standard care by follow-up time.
Subgroup analysis of the inflammatory bowel disease questionnaire comparing the telemedicine with standard care by the age of patients.
Remission rate comparing the telemedicine versus the standard care.
The number of clinic visits per patient comparing telemedicine with standard care.
Patient satisfaction comparing telemedicine with standard care.
Depression comparing the telemedicine with the standard care.
Generic quality of life comparing the telemedicine with the standard care.
Self-efficacy comparing the telemedicine with the standard care.
(A) Medication compliance score comparing the telemedicine with the standard care.(B) Medication compliance rate comparing the telemedicine with the standard care.
Footnotes
Authors' Contributions: LLP designed the search strategy. LLP and ZDL performed the search. LLP and HYL performed the abstract screening, full-text screening, data extraction, and risk of bias assessment. All the authors drafted and revised the manuscript. RM and MHC supervised the overall study.
Conflicts of Interest: None declared.
References
- 1.Dahlhamer JM, Zammitti EP, Ward BW, Wheaton AG, Croft JB. Prevalence of inflammatory bowel disease among adults aged ≥18 years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016 Oct 28;65(42):1166–1169. doi: 10.15585/mmwr.mm6542a3. doi: 10.15585/mmwr.mm6542a3. [DOI] [PubMed] [Google Scholar]
- 2.Coward S, Clement F, Benchimol Ei, Bernstein Cn, Bitton A, Carroll M, Hazlewood G, Jelinski S, Jones Jl, Kuenzig E, Leddin D, McBrien K, Murthy Sk, Nguyen Gc, Otley A, Rezaie A, Peña-Sánchez Jn, Singh H, Targownik Le, Kaplan G. Tu1698 - Analyzing the rising prevalence of IBD: predicting the prevalence in 2030 by age group. Gastroenterology. 2018 May;154(6):S-992–S-993. doi: 10.1016/S0016-5085(18)33324-9. [DOI] [Google Scholar]
- 3.Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015 Apr 3;12(4):205–17. doi: 10.1038/nrgastro.2015.34.nrgastro.2015.34 [DOI] [PubMed] [Google Scholar]
- 4.Windsor JW, Kaplan GG. Evolving epidemiology of IBD. Curr Gastroenterol Rep. 2019 Jul 23;21(8):40. doi: 10.1007/s11894-019-0705-6.10.1007/s11894-019-0705-6 [DOI] [PubMed] [Google Scholar]
- 5.Kemp K, Griffiths J, Campbell S, Lovell K. An exploration of the follow-up up needs of patients with inflammatory bowel disease. J Crohns Colitis. 2013 Oct;7(9):e386–95. doi: 10.1016/j.crohns.2013.03.001.S1873-9946(13)00103-7 [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization . Telehealth and Telemedicine Will Henceforth Be Part of the Strategy for Health-for-All. Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 7.Siegel CA. Placing value on telemedicine for inflammatory bowel disease. Am J Gastroenterol. 2019 Mar 30;114(3):382–383. doi: 10.14309/ajg.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 8.Wu C, Wu Z, Yang L, Zhu W, Zhang M, Zhu Q, Chen X, Pan Y. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 2018 Oct;97(43):e12962. doi: 10.1097/MD.0000000000012962. doi: 10.1097/MD.0000000000012962.00005792-201810260-00059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao J, Zhai Y, Zhu W, Sun D. Effectiveness of telemedicine for controlling asthma symptoms: a systematic review and meta-analysis. Telemed J E Health. 2015 Jun;21(6):484–92. doi: 10.1089/tmj.2014.0119. [DOI] [PubMed] [Google Scholar]
- 10.Lundell S, Holmner. Rehn B, Nyberg A, Wadell K. Telehealthcare in COPD: a systematic review and meta-analysis on physical outcomes and dyspnea. Respir Med. 2015 Jan;109(1):11–26. doi: 10.1016/j.rmed.2014.10.008. https://linkinghub.elsevier.com/retrieve/pii/S0954-6111(14)00358-8 .S0954-6111(14)00358-8 [DOI] [PubMed] [Google Scholar]
- 11.Knox L, Rahman RJ, Beedie C. Quality of life in patients receiving telemedicine enhanced chronic heart failure disease management: A meta-analysis. J Telemed Telecare. 2017 Aug;23(7):639–649. doi: 10.1177/1357633X16660418.1357633X16660418 [DOI] [PubMed] [Google Scholar]
- 12.Elkjaer M, Shuhaibar M, Burisch J, Bailey Y, Scherfig H, Laugesen B, Avnstrøm Søren, Langholz E, O'Morain C, Lynge E, Munkholm P. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided 'Constant-care' approach. Gut. 2010 Dec 11;59(12):1652–61. doi: 10.1136/gut.2010.220160.59/12/1652 [DOI] [PubMed] [Google Scholar]
- 13.Ozgursoy UBN, Yildirim Y, Senuzun Aykar F, Unsal B. N031 The effect of web-based education on disease activity, symptom management and quality of life in patients with inflammatory bowel disease. J Crohns Colitis. 2018;12(Suppl 1):S582–S582. doi: 10.1093/ecco-jcc/jjx180.1045. [DOI] [Google Scholar]
- 14.Avery P. Using e-health tools and PROMs to support self-management in patients with inflammatory bowel disease. Br J Nurs. 2021 Apr 08;30(7):394–402. doi: 10.12968/bjon.2021.30.7.394. https://www.magonlinelibrary.com/doi/abs/10.12968/bjon.2021.30.7.394?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 15.Mao R, Liang J, Wu K, Chen M. Responding to COVID-19: perspectives from the Chinese Society of Gastroenterology. Gastroenterology. 2020 Jun;158(8):2024–2027. doi: 10.1053/j.gastro.2020.03.046. http://europepmc.org/abstract/MED/32314563 .S0016-5085(20)30400-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Jong M, van der Meulen-de Jong A, Romberg-Camps M, Degens J, Becx M, Markus T, Tomlow H, Cilissen M, Ipenburg N, Verwey M, Colautti-Duijsens L, Hameeteman W, Masclee A, Jonkers D, Pierik M. Development and feasibility study of a telemedicine tool for all patients with IBD: MyIBDcoach. Inflamm Bowel Dis. 2017 Apr;23(4):485–493. doi: 10.1097/MIB.0000000000001034. [DOI] [PubMed] [Google Scholar]
- 17.Habashi P, Bouchard Shelley, Nguyen Geoffrey C. Transforming access to specialist care for inflammatory bowel disease: the PACE Telemedicine Program. J Can Assoc Gastroenterol. 2019 Dec;2(4):186–194. doi: 10.1093/jcag/gwy046. http://europepmc.org/abstract/MED/31616860 .gwy046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Del Hoyo J, Nos P, Faubel R, Bastida G, Muñoz Diana, Valero-Pérez Elena, Garrido-Marín Alejandro, Bella P, Peña Beatriz, Savini C, Aguas M. Adaptation of TECCU app based on patients' perceptions for the telemonitoring of inflammatory bowel disease: a qualitative study using focus groups. Int J Environ Res Public Health. 2020 Mar 13;17(6):1871. doi: 10.3390/ijerph17061871. https://www.mdpi.com/resolver?pii=ijerph17061871 .ijerph17061871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atreja A, Khan S, Rogers JD, Otobo E, Patel NP, Ullman T, Colombel JF, Moore S, Sands BE, HealthPROMISE Consortium Group Impact of the mobile HealthPROMISE platform on the quality of care and quality of life in patients with inflammatory bowel disease: study protocol of a pragmatic randomized controlled trial. JMIR Res Protoc. 2015 Feb 18;4(1):e23. doi: 10.2196/resprot.4042. https://www.researchprotocols.org/2015/1/e23/ v4i1e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh S, Brill JV, Proudfoot JA, Metcalfe L, Vu L, Sandborn WJ, Kosinski LR. Project Sonar: a community practice-based intensive medical home for patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2018 Dec;16(12):1847–1850.e1. doi: 10.1016/j.cgh.2018.08.052.S1542-3565(18)30891-7 [DOI] [PubMed] [Google Scholar]
- 21.Van Deen WK, van der Meulen-de Jong AE, Parekh NK, Kane E, Zand A, DiNicola CA, Hall L, Inserra EK, Choi JM, Ha CY, Esrailian E, van Oijen MG, Hommes DW. Development and validation of an inflammatory bowel diseases monitoring index for use with mobile health technologies. Clin Gastroenterol Hepatol. 2016 Dec;14(12):1742–1750.e7. doi: 10.1016/j.cgh.2015.10.035.S1542-3565(15)01546-3 [DOI] [PubMed] [Google Scholar]
- 22.Louis E, Dotan I, Ghosh S, Mlynarsky L, Reenaers C, Schreiber S. Optimising the inflammatory bowel disease unit to improve quality of care: expert recommendations. J Crohns Colitis. 2015 Aug;9(8):685–91. doi: 10.1093/ecco-jcc/jjv085. http://europepmc.org/abstract/MED/25987349 .jjv085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghosh S, Louis E, Beaugerie L, Bossuyt P, Bouguen G, Bourreille A, Ferrante M, Franchimont D, Frost K, Hebuterne X, Marshall JK, OʼShea C, Rosenfeld G, Williams C, Peyrin-Biroulet L. Development of the IBD disk: a visual self-administered tool for assessing disability in inflammatory bowel diseases. Inflamm Bowel Dis. 2017 Mar;23(3):333–340. doi: 10.1097/MIB.0000000000001033. http://europepmc.org/abstract/MED/28146002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang VW, Reich Krista M, Fedorak Richard N. Distance management of inflammatory bowel disease: systematic review and meta-analysis. World J Gastroenterol. 2014 Jan 21;20(3):829–42. doi: 10.3748/wjg.v20.i3.829. https://www.wjgnet.com/1007-9327/full/v20/i3/829.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanlon I, Hewitt C, Bell K, Phillips A, Mikocka-Walus A. Systematic review with meta-analysis: online psychological interventions for mental and physical health outcomes in gastrointestinal disorders including irritable bowel syndrome and inflammatory bowel disease. Aliment Pharmacol Ther. 2018 Aug 14;48(3):244–259. doi: 10.1111/apt.14840. [DOI] [PubMed] [Google Scholar]
- 26.Rohde J, Barker Joshua O, Noar Seth M. Impact of eHealth technologies on patient outcomes: a meta-analysis of chronic gastrointestinal illness interventions. Transl Behav Med. 2021 Feb 11;11(1):1–10. doi: 10.1093/tbm/ibz166.5626447 [DOI] [PubMed] [Google Scholar]
- 27.George LA, Cross RK. Remote monitoring and telemedicine in IBD: are we there yet? Curr Gastroenterol Rep. 2020 Feb 10;22(3):12. doi: 10.1007/s11894-020-0751-0.10.1007/s11894-020-0751-0 [DOI] [PubMed] [Google Scholar]
- 28.Atanasov P, Gauthier A, Cobos D. The place of eHealth interventions in the management pathway of inflammatory bowel disease (IBD) patients: a systematic review. Value Health. 2018 Sep;21:S42–S43. doi: 10.1016/j.jval.2018.07.326. [DOI] [Google Scholar]
- 29.Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Training. [2020-11-09]. http://handbook.cochrane.org .
- 30.Jadad AR, Moore R, Carroll D, Jenkinson C, Reynolds DM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996 Feb;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4.0197-2456(95)00134-4 [DOI] [PubMed] [Google Scholar]
- 31.Guyatt G, Mitchell A, Irvine E, Singer J, Williams N, Goodacre R, Tompkins C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989 Mar;96(3):804–10.0016-5085(89)90905-0 [PubMed] [Google Scholar]
- 32.Harvey R, Bradshaw J. A simple index of Crohn's-disease activity. Lancet. 1980 Mar 08;1(8167):514. doi: 10.1016/s0140-6736(80)92767-1.S0140-6736(80)92767-1 [DOI] [PubMed] [Google Scholar]
- 33.Seo M, Okada M, Yao T, Ueki M, Arima S, Okumura M. An index of disease activity in patients with ulcerative colitis. Am J Gastroenterol. 1992 Aug;87(8):971–6. [PubMed] [Google Scholar]
- 34.Walmsley RS, Ayres RCS, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998 Jul;43(1):29–32. doi: 10.1136/gut.43.1.29. https://gut.bmj.com/lookup/pmidlookup?view=long&pmid=9771402 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987 Dec 24;317(26):1625–9. doi: 10.1056/NEJM198712243172603. [DOI] [PubMed] [Google Scholar]
- 36.Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG Clinical Guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019 Mar;114(3):384–413. doi: 10.14309/ajg.0000000000000152.00000434-201903000-00010 [DOI] [PubMed] [Google Scholar]
- 37.Best WR. Predicting the Crohn's disease activity index from the Harvey-Bradshaw Index. Inflamm Bowel Dis. 2006 Apr;12(4):304–10. doi: 10.1097/01.MIB.0000215091.77492.2a.00054725-200604000-00007 [DOI] [PubMed] [Google Scholar]
- 38.Larsen DL, Attkisson C, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6.0149-7189(79)90094-6 [DOI] [PubMed] [Google Scholar]
- 39.Cross RK, Cheevers N, Rustgi A, Langenberg P, Finkelstein J. Randomized, controlled trial of home telemanagement in patients with ulcerative colitis (UC HAT) Inflamm Bowel Dis. 2012 Jun;18(6):1018–25. doi: 10.1002/ibd.21795. http://europepmc.org/abstract/MED/21688350 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cross RK, Langenberg P, Regueiro M, Schwartz DA, Tracy JK, Collins JF, Katz J, Ghazi L, Patil SA, Quezada SM, Beaulieu D, Horst SN, Russman K, Riaz M, Jambaulikar G, Sivasailam B, Quinn CC. A randomized controlled trial of TELEmedicine for Patients with Inflammatory Bowel Disease (TELE-IBD) Am J Gastroenterol. 2019 Mar;114(3):472–482. doi: 10.1038/s41395-018-0272-8.10.1038/s41395-018-0272-8 [DOI] [PubMed] [Google Scholar]
- 41.Schliep M, Chudy-Onwugaje Kenechukwu, Abutaleb Ameer, Langenberg Patricia, Regueiro Miguel, Schwartz David A, Tracy J Kathleen, Ghazi Leyla, Patil Seema A, Quezada Sandra, Russman Katharine, Horst Sara, Beaulieu Dawn, Quinn Charlene, Jambaulikar Guruprasad, Cross Raymond K. TELEmedicine for Patients With Inflammatory Bowel Disease (TELE-IBD) does not improve depressive symptoms or general quality of life compared with standard care at tertiary referral centers. Crohns Colitis 360. 2020 Jan;2(1):otaa002–8. doi: 10.1093/crocol/otaa002. http://europepmc.org/abstract/MED/32201859 .otaa002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bilgrami Z, Abutaleb A, Chudy-Onwugaje K, Langenberg P, Regueiro M, Schwartz DA, Tracy JK, Ghazi L, Patil SA, Quezada SM, Russman KM, Quinn CC, Jambaulikar G, Beaulieu DB, Horst S, Cross RK. Effect of TELEmedicine for inflammatory bowel disease on patient activation and self-efficacy. Dig Dis Sci. 2020 Jan 02;65(1):96–103. doi: 10.1007/s10620-018-5433-5. http://europepmc.org/abstract/MED/30604373 .10.1007/s10620-018-5433-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miloh T, Shub Mitchell, Montes Ramon, Ingebo Kristy, Silber Gary, Pasternak Brad. Text messaging effect on adherence in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2017 Jun;64(6):939–942. doi: 10.1097/MPG.0000000000001399. [DOI] [PubMed] [Google Scholar]
- 44.Hunt M, Rodriguez L, Marcelle E. A cognitive behavioral therapy workbook delivered online with minimal therapist feedback improves quality of life for inflammatory bowel disease patients. Intern Med J. 2017:1–16. [Google Scholar]
- 45.Krier M, Kaltenbach Tonya, McQuaid Kenneth, Soetikno Roy. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol. 2011 Dec;106(12):2063–7. doi: 10.1038/ajg.2011.329.ajg2011329 [DOI] [PubMed] [Google Scholar]
- 46.Heida A, Dijkstra Alie, Muller Kobold Anneke, Rossen John W, Kindermann Angelika, Kokke Freddy, de Meij Tim, Norbruis Obbe, Weersma Rinse K, Wessels Margreet, Hummel Thalia, Escher Johanna, van Wering Herbert, Hendriks Daniëlle, Mearin Luisa, Groen Henk, Verkade Henkjan J, van Rheenen Patrick F. Efficacy of home telemonitoring versus conventional follow-up: a randomized controlled trial among teenagers with inflammatory bowel disease. J Crohns Colitis. 2018 Mar 28;12(4):432–441. doi: 10.1093/ecco-jcc/jjx169.4710333 [DOI] [PubMed] [Google Scholar]
- 47.de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, Cilissen M, van Bodegraven AA, Mahmmod N, Markus T, Hameeteman WM, Dijkstra G, Masclee AA, Boonen A, Winkens B, van Tubergen A, Jonkers DM, Pierik MJ. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017 Sep 02;390(10098):959–968. doi: 10.1016/S0140-6736(17)31327-2.S0140-6736(17)31327-2 [DOI] [PubMed] [Google Scholar]
- 48.Linn AJ, van Dijk L, van Weert JC, Gebeyehu BG, van Bodegraven AA, Smit EG. Creating a synergy effect: a cluster randomized controlled trial testing the effect of a tailored multimedia intervention on patient outcomes. Patient Educ Couns. 2018 Aug;101(8):1419–1426. doi: 10.1016/j.pec.2018.03.017.S0738-3991(18)30121-6 [DOI] [PubMed] [Google Scholar]
- 49.McCombie A, Walmsley R, Barclay M, Ho C, Langlotz T, Regenbrecht H, Gray A, Visesio N, Inns S, Schultz M. A noninferiority randomized clinical trial of the use of the smartphone-based health applications IBDsmart and IBDoc in the care of inflammatory bowel disease patients. Inflamm Bowel Dis. 2020 Jun 18;26(7):1098–1109. doi: 10.1093/ibd/izz252.5603780 [DOI] [PubMed] [Google Scholar]
- 50.McCombie A, Gearry R, Andrews J, Mulder R, Mikocka-Walus A. Does computerized cognitive behavioral therapy help people with inflammatory bowel disease? a randomized controlled trial. Inflamm Bowel Dis. 2016 Jan;22(1):171–81. doi: 10.1097/MIB.0000000000000567. [DOI] [PubMed] [Google Scholar]
- 51.Carlsen K, Jakobsen C, Houen G, Kallemose T, Paerregaard A, Riis LB, Munkholm P, Wewer V. Self-managed eHealth disease monitoring in children and adolescents with inflammatory bowel disease: a randomized controlled trial. Inflamm Bowel Dis. 2017 Mar;23(3):357–365. doi: 10.1097/MIB.0000000000001026.00054725-201703000-00004 [DOI] [PubMed] [Google Scholar]
- 52.Akobeng AK, O'Leary N, Vail A, Brown N, Widiatmoko D, Fagbemi A, Thomas AG. Telephone consultation as a substitute for routine out-patient face-to-face consultation for children with inflammatory bowel disease: randomised controlled trial and economic evaluation. EBioMedicine. 2015 Sep;2(9):1251–6. doi: 10.1016/j.ebiom.2015.08.011. https://linkinghub.elsevier.com/retrieve/pii/S2352-3964(15)30104-3 .S2352-3964(15)30104-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Del Hoyo J, Nos P, Faubel R, Muñoz Diana, Domínguez David, Bastida G, Valdivieso B, Correcher M, Aguas M. A web-based telemanagement system for improving disease activity and quality of life in patients with complex inflammatory bowel disease: pilot randomized controlled trial. J Med Internet Res. 2018 Nov 27;20(11):e11602. doi: 10.2196/11602. https://www.jmir.org/2018/11/e11602/ v20i11e11602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vachon A, Scott Frank I. The treatment approach to inflammatory bowel disease in 2020. Curr Opin Gastroenterol. 2020 Jul;36(4):247–256. doi: 10.1097/MOG.0000000000000653.00001574-202007000-00003 [DOI] [PubMed] [Google Scholar]
- 55.Jackson BD, Gray K, Knowles SR, De Cruz P. EHealth technologies in inflammatory bowel disease: a systematic review. J Crohns Colitis. 2016 Sep;10(9):1103–21. doi: 10.1093/ecco-jcc/jjw059.jjw059 [DOI] [PubMed] [Google Scholar]
- 56.Shpoliansky M, Shouval DS. [APPROACH TO VERY EARLY ONSET INFLAMMATORY BOWEL DISEASE] Harefuah. 2020 Mar;159(3):206–211. [PubMed] [Google Scholar]
- 57.Topal F, Camyar H, Saritas Yuksel E, Gunay S, Topal F, Gür Emine Özlem. Work productivity loss in inflammatory bowel disease patients in Turkey. Gastroenterol Res Pract. 2020 Jan 08;2020:6979720–6. doi: 10.1155/2020/6979720. doi: 10.1155/2020/6979720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martelli L, Lopez A, Strobel S, Danese S, Roblin X, Baumann C, Peyrin-Biroulet L. Adherence to infliximab therapy in inflammatory bowel disease patients in a real-life setting. J Dig Dis. 2017 Oct;18(10):566–573. doi: 10.1111/1751-2980.12539. [DOI] [PubMed] [Google Scholar]
- 59.Kane S, Shaya F. Medication non-adherence is associated with increased medical health care costs. Dig Dis Sci. 2008 Apr;53(4):1020–4. doi: 10.1007/s10620-007-9968-0. [DOI] [PubMed] [Google Scholar]
- 60.Hommel KA, Davis CM, Baldassano RN. Medication adherence and quality of life in pediatric inflammatory bowel disease. J Pediatr Psychol. 2008 Sep;33(8):867–74. doi: 10.1093/jpepsy/jsn022. http://europepmc.org/abstract/MED/18337262 .jsn022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Di Toro R, Lama G. [A case of nephroblastoma associated with the nephrotic syndrome] Minerva Pediatr. 1974 Apr 21;26(14):724–7. [PubMed] [Google Scholar]
- 62.Thakkar J, Kurup R, Laba T, Santo K, Thiagalingam A, Rodgers A, Woodward M, Redfern J, Chow CK. Mobile telephone text messaging for medication adherence in chronic disease: a meta-analysis. JAMA Intern Med. 2016 Mar;176(3):340–9. doi: 10.1001/jamainternmed.2015.7667.2484905 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Subgroup analysis of the inflammatory bowel disease questionnaire comparing the telemedicine with standard care by follow-up time.
Subgroup analysis of the inflammatory bowel disease questionnaire comparing the telemedicine with standard care by the age of patients.
Remission rate comparing the telemedicine versus the standard care.
The number of clinic visits per patient comparing telemedicine with standard care.
Patient satisfaction comparing telemedicine with standard care.
Depression comparing the telemedicine with the standard care.
Generic quality of life comparing the telemedicine with the standard care.
Self-efficacy comparing the telemedicine with the standard care.
(A) Medication compliance score comparing the telemedicine with the standard care.(B) Medication compliance rate comparing the telemedicine with the standard care.


