This cohort study assesses the association of the COVID-19 pandemic with prostate biopsy and prostate cancer diagnosis rates among Black vs White patients in the Veterans Affairs Health Care System.
Key Points
Question
What is the association of the COVID-19 pandemic with prostate biopsy and prostate cancer (PC) diagnosis rates, evaluated by race, in the Veterans Affairs Health Care System?
Findings
Among 51 606 included men, the estimated number of missed PC diagnoses from March 2020 through March 2021 ranged from 97 to 573 cases. Prior to the pandemic, biopsy rates were statistically significantly higher among Black vs White men; however, there were no statistically significant changes in biopsy rates associated with race at the onset of the pandemic nor during the recovery period from June 2020 through March 2021, with similar trends observed for PC diagnosis rates.
Meaning
These results suggest that prostate biopsy volume and PC diagnosis rates decreased in the Veterans Affairs Health Care System during the COVID-19 pandemic, with no statistically significant changes noted by race.
Abstract
Importance
Several studies have assessed the negative effect of the COVID-19 pandemic on cancer screening and diagnosis rates. However, this has not been evaluated for prostate biopsy and prostate cancer (PC) diagnosis in an equal-access health care system.
Objective
To determine the association of the pandemic with prostate biopsy and PC diagnosis rates among Black vs White patients in the Veterans Affairs Health Care System (VAHCS).
Design, Setting, and Participants
This cohort study included a retrospective analysis of all prostate biopsies performed on patients in the VAHCS without a preexisting PC diagnosis between January 2018 and March 2021. The base population included all living male patients who had at least 1 visit to the VAHCS during the 3 years prior to each month of the study.
Exposure
The COVID-19 pandemic.
Main Outcomes and Measures
The main outcomes were the number of prostate biopsies and PC diagnoses by month. The influence of the pandemic on prostate biopsy volume and the incidence of PC diagnoses was modeled using an interrupted time-series analysis. Poisson generalized linear models were fitted to project the expected number of prostate biopsies and PC diagnoses had there been no pandemic interruption. Additional models were used to test for differences by race.
Results
Prior to the pandemic (January 2018 through February 2020), monthly biopsy numbers among 51 606 included men ranged between 1230 and 1695, of which 56% to 60% of results were positive for PC. The estimated number of missed PC diagnoses from March 2020 through March 2021 ranged from 97 cases (October 2020: 752 cases expected, 655 cases observed) to 573 cases (April 2020: 794 cases expected, 221 cases observed). Prior to the pandemic, biopsy rates were statistically significantly higher among Black vs White men (incidence rate ratio, 2.25; 95% CI, 2.06-2.46; P < .001). There was no change in biopsy rates associated with race at the onset of the pandemic nor during the recovery period from March 2020 to March 2021. Similar trends were observed for PC diagnosis rates.
Conclusions and Relevance
Results of this cohort study demonstrate that during the COVID-19 pandemic, prostate biopsy and PC diagnosis rates decreased, particularly during the peak of the pandemic. However, there were no statistically significant changes in rates by race.
Introduction
During the COVID-19 pandemic, health care professionals have been forced to triage patients for screening and treatment of urologic cancers,1,2 weighing the risk of disease progression with risk of COVID-19 infection, in addition to considering the added burden on health care systems. With the emergence of SARS-CoV-2 variant strains and an uptick in COVID-19 hospitalizations, it is likely the ongoing pandemic will continue to affect timely cancer diagnoses.
Previous studies have demonstrated that the COVID-19 pandemic has resulted in a decrease in cancer diagnoses across many disease sites, both in the US3,4,5,6,7,8 and internationally.9 As such, we assessed the association of the pandemic with prostate biopsy volume and incidence of prostate cancer (PC) diagnoses in the equal-access Veterans Affairs Health Care System (VAHCS), highlighting the projected number of biopsies and new PC diagnoses if the pandemic had not occurred. Importantly, these outcomes were evaluated by race given that Bernstein et al4 previously reported considerably fewer Black patients receiving a radical prostatectomy during the pandemic vs before the pandemic, and Englum et al8 showed that prostate biopsies decreased by 29% in the VAHCS during the pandemic, though without evaluating by race. We hypothesized that the pandemic would be associated with a reduction in prostate biopsies and fewer PC diagnoses with no difference in outcomes by race.
Methods
Study Design and Population
We performed a retrospective analysis of all prostate biopsies performed on patients in the VAHCS without a preexisting PC diagnosis between January 2018 and March 2021. Preexisting PC was defined as a diagnosis date more than 30 days prior to a patient’s biopsy date. Newly diagnosed PC cases were identified by the presence of a diagnosis date within 30 days of the corresponding biopsy date. The base population used to evaluate screening and diagnosis rates included all living male patients who had at least 1 visit to the VAHCS during the 3 years prior to each month of the study. Analyses evaluating the association of race were limited to Black and White patients because the VAHCS population primarily includes patients who identify as these 2 racial categories. This study received approval from the Durham VA Health Care System institutional review board, which also waived the need for patient informed consent owing to the use of deidentified data.
Statistical Analysis
We modeled the influence of the pandemic on prostate biopsy volume and the incidence of PC diagnoses using an interrupted time-series analysis.10,11 For each outcome, we fit Poisson generalized linear models that included a linear trend for time initiating at the beginning of the study period (January 2018), a level change following the onset of the pandemic (March 2020), and an interaction term initiating at the onset of the pandemic to capture changes in the slope of the linear trend associated with pandemic recovery. The models accounted for month-to-month variability in the base population using an offset term for population size and included indicator variables to control for the 3 months during the peak of the pandemic lockdown (March through May 2020).10
To evaluate differences in prostate biopsy and PC diagnosis rates by race (among the subset of Black vs White patients), we fit models that included, in addition to the variables previously indicated, an indicator variable for Black (vs White) race to capture level changes during the prepandemic period, an interaction term between the indicator for Black race and the linear trend for time initiating at the beginning of the study to capture differences in the slope during the prepandemic period, an interaction between the indicator for Black race and the level change following the onset of the pandemic, a 3-way interaction to allow the slope of the linear trend associated with pandemic recovery to vary by race, and additional interaction terms to control for race effects associated with the 3 months during the peak of the pandemic. To assess whether the pandemic was associated with prostate biopsy and PC diagnosis rates by race (in comparison with the prepandemic period), we performed a joint test of the parameters corresponding to variables with interaction terms involving race that captured level and slope changes during the pandemic onset and recovery periods.
All models used a scaling adjustment and heteroscedasticity and autocorrelation-consistent standard errors to account for overdispersion and residual autocorrelation, respectively.12,13 Analyses were conducted using R statistical software, version 4.1.0 (R Core Team), and statistical significance was set at 1-sided P < .05.
Results
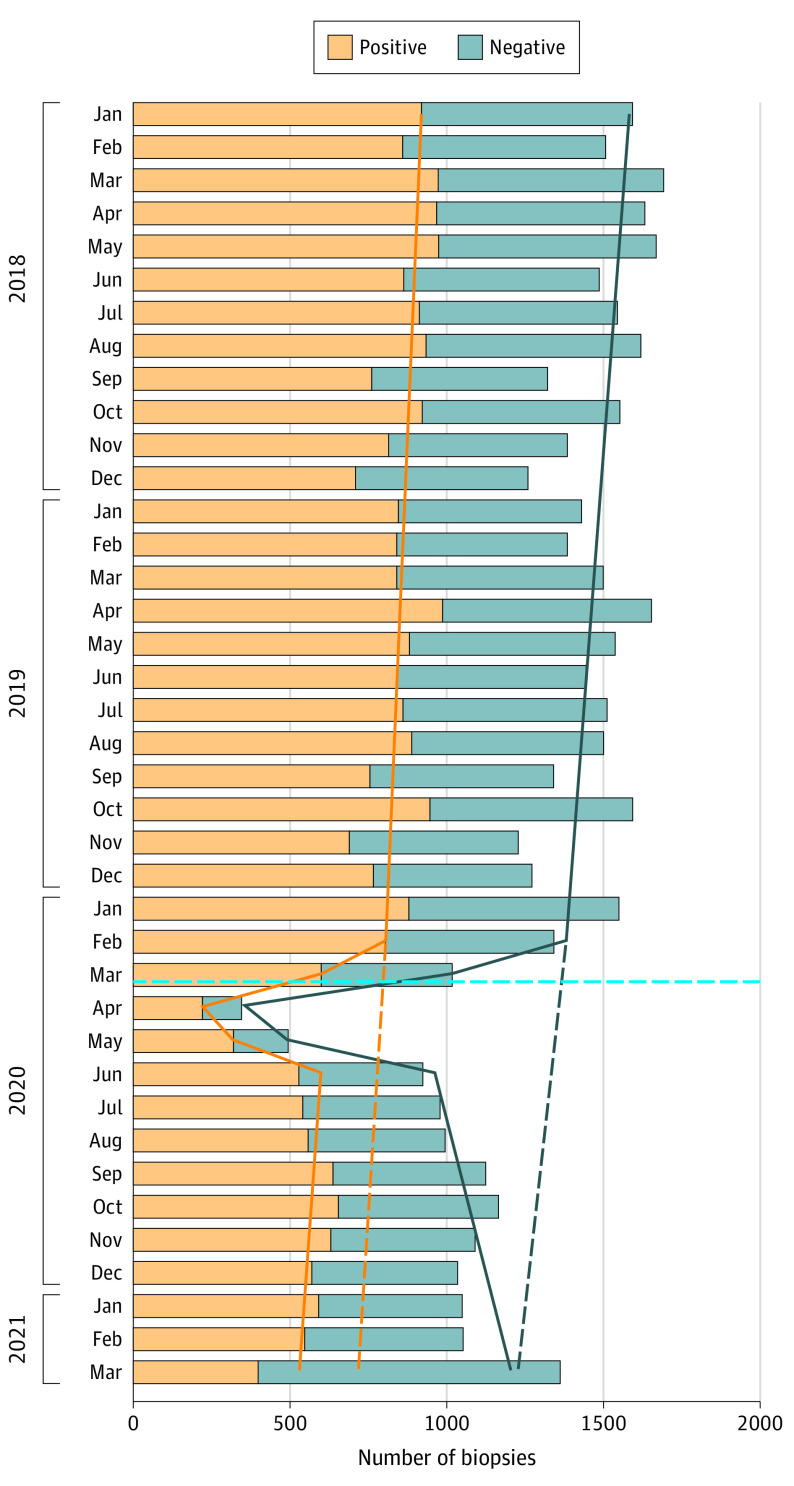
There were 51 606 men who received at least 1 biopsy during the study period, with monthly biopsy numbers ranging between 1230 and 1695, of which 56% to 60% of results were positive for PC (Figure 1). During the pandemic peak from March through May 2020, there was a sharp decrease in the number of biopsies performed and a higher proportion of positive biopsy results. From the interrupted time-series analysis, the number of missed PC diagnoses from March 2020 through March 2021 ranged from an estimated 97 cases (October 2020: 752 cases expected, 655 cases observed) to an estimated 573 cases (April 2020: 794 cases expected, 221 cases observed) (Table).
Figure 1. Prostate Biopsies and Newly Diagnosed Cases of Prostate Cancer Stratified by Month.
Bars represent the observed counts; solid lines represent the expected counts from the interrupted time-series analysis; dashed lines project the expected counts had there not been a COVID-19 pandemic interruption; and the horizontal dashed light blue line indicates March 11, 2020, when the World Health Organization declared COVID-19 a global pandemic.
Table. Observed Number of Prostate Biopsies and New Prostate Cancer Diagnoses vs Expected Biopsies and Diagnoses Had There Not Been a COVID-19 Pandemic Interruption.
| Month | No. of prostate biopsies | No. of new prostate cancer diagnoses | ||
|---|---|---|---|---|
| Observed | Expected (95% CI)a | Observed | Expected (95% CI)a | |
| 2020 | ||||
| March | 1019 | 1375 (1288-1468) | 602 | 802 (748-860) |
| April | 344 | 1362 (1272-1460) | 221 | 794 (738-855) |
| May | 491 | 1350 (1256-1452) | 317 | 788 (728-851) |
| June | 925 | 1339 (1240-1445) | 529 | 781 (719-848) |
| July | 980 | 1327 (1225-1438) | 542 | 774 (710-844) |
| August | 996 | 1315 (1209-1430) | 557 | 767 (701-840) |
| September | 1126 | 1302 (1192-1422) | 638 | 760 (691-835) |
| October | 1167 | 1289 (1176-1413) | 655 | 752 (682-830) |
| November | 1092 | 1276 (1159-1404) | 630 | 745 (672-825) |
| December | 1036 | 1262 (1142-1395) | 546 | 737 (662-820) |
| 2021 | ||||
| January | 1051 | 1253 (1129-1390) | 592 | 731 (654-818) |
| February | 1054 | 1242 (1116-1384) | 544 | 726 (646-814) |
| March | 1364 | 1234 (1104-1380) | 399 | 721 (639-813) |
Expected counts were estimated using interrupted time-series analyses based on Poisson generalized linear models.
At the beginning of the study (January 2018), biopsy rates were statistically significantly higher among Black vs White men (incidence rate ratio, 2.25; 95% CI, 2.06-2.46; P < .001; eTables 1 and 2 in the Supplement and Figure 2A). There were no statistically significant changes in biopsy rates associated with race during the pandemic onset or recovery period from March 2020 through March 2021 (eTable 2 in the Supplement). Similar trends were observed for PC diagnosis rates (eTables 1 and 2 in the Supplement and Figure 2B).
Figure 2. Prostate Biopsy Rates and Newly Diagnosed Prostate Cancer Rates Stratified by Race.
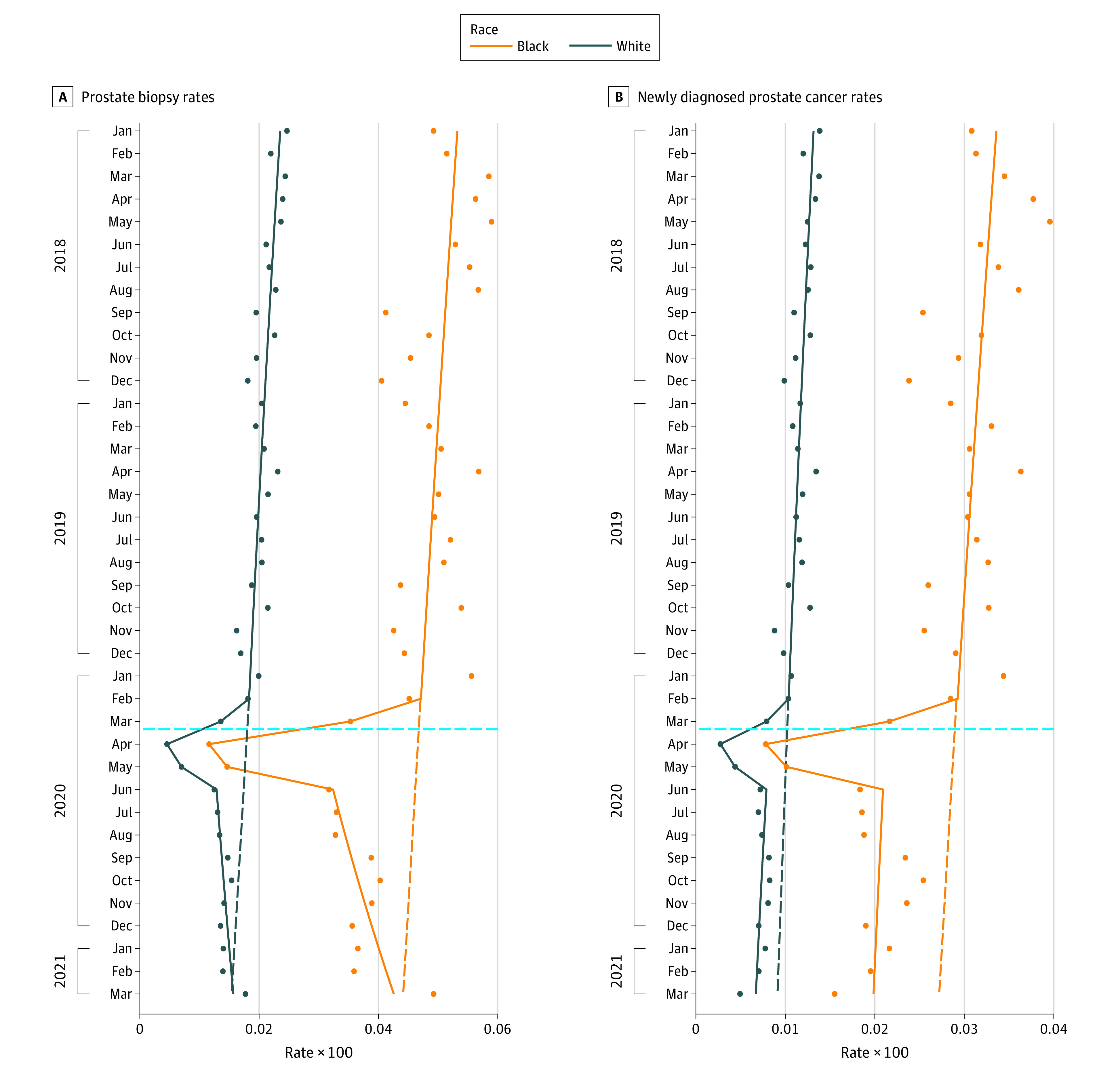
The solid lines represent the expected rates estimated by the interrupted time-series analysis; the dashed lines project the expected rates had there not been a COVID-19 pandemic interruption; the dots represent the observed rates of biopsies and prostate cancer diagnoses; and the horizontal dashed light blue line indicates March 11, 2020, when the World Health Organization declared COVID-19 a global pandemic.
Discussion
Using data from a large nationwide equal-access health care system, we demonstrated that the COVID-19 pandemic was associated with fewer biopsies and fewer new PC cases, which was particularly pronounced during the pandemic peak. Although previous studies using civilian3,4,5,6,7,9 and VAHCS8 cohorts have demonstrated the negative association of the pandemic with cancer screening and diagnosis rates, this is the first study, to our knowledge, showing this association, evaluating by race, in the VAHCS population. Using data from New England, Bakouny et al3 also reported a considerable decrease in screening tests for cancer (mammography, prostate-specific antigen, colonoscopy, Papanicolaou test, low-dose computed tomography) and decreased diagnoses during the pandemic. Taken together, these studies suggest that the pandemic has negatively affected cancer diagnosis rates regardless of jurisdiction or payment model.
We found that Black men had statistically significantly higher biopsy and PC diagnosis rates compared with White men prior to the pandemic, with no statistically significant changes by race during the pandemic peak or during the recovery period. Importantly, this suggests that Black men did not receive marginalized care relative to White men during the pandemic, perhaps as a result of equal-access care at VA hospitals. This is in contrast with Bernstein et al,4 who reported that prior to the pandemic, Black patients made up 19.5% of patients undergoing prostatectomy in Pennsylvania, which dropped to 2.9% during the initial pandemic period (P = .001).
Limitations
The data from the current study are limited by lacking information on cancer stage and grade at diagnosis. Thus, the effect of delayed/deferred diagnoses in these men warrants long-term study. We also limited the present study of race to Black and White men, thus we do not know if other racial and ethnic groups may have different biopsy or PC diagnosis trends.
Conclusions
This cohort study demonstrates that during the COVID-19 pandemic, prostate biopsy and PC diagnosis rates decreased, particularly during the peak of the pandemic. However, there were no statistically significant changes in rates by race. With COVID-19 variant strains, it is possible that continued ongoing delays in PC screening may occur.
eTable 1. The observed and expected number of prostate biopsies and new prostate cancer diagnoses had there not been a pandemic interruption, stratified by race
eTable 2. Incidence rate ratios from the Poisson generalized linear models
References
- 1.Wallis CJD, Novara G, Marandino L, et al. Risks from deferring treatment for genitourinary cancers: a collaborative review to aid triage and management during the COVID-19 pandemic. Eur Urol. 2020;78(1):29-42. doi: 10.1016/j.eururo.2020.04.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ribal MJ, Cornford P, Briganti A, et al. ; GORRG Group; EAU Section Offices and the EAU Guidelines Panels . European Association of Urology Guidelines Office Rapid Reaction Group: an organisation-wide collaborative effort to adapt the European Association of Urology Guidelines recommendations to the coronavirus disease 2019 era. Eur Urol. 2020;78(1):21-28. doi: 10.1016/j.eururo.2020.04.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bakouny Z, Paciotti M, Schmidt AL, Lipsitz SR, Choueiri TK, Trinh QD. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. 2021;7(3):458-460. doi: 10.1001/jamaoncol.2020.7600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernstein AN, Talwar R, Handorf E, et al. Impact of COVID-19 on initial management and evaluation of prostate cancer. Urol Pract. 2021;8(6):668-675. doi: 10.1097/UPJ.0000000000000261 [DOI] [PubMed] [Google Scholar]
- 5.Vose JM. Delay in cancer screening and diagnosis during the COVID-19 pandemic: what is the cost? Oncology (Williston Park). 2020;34(9):343. doi: 10.46883/ONC.2020.3409.0343 [DOI] [PubMed] [Google Scholar]
- 6.Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059-1071. doi: 10.1200/CCI.20.00134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;3(8):e2017267. doi: 10.1001/jamanetworkopen.2020.17267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Englum BR, Prasad NK, Lake RE, et al. Impact of the COVID-19 pandemic on diagnosis of new cancers: a national multicenter study of the Veterans Affairs Healthcare System. Cancer. 2022;128(5):1048-1056. doi: 10.1002/cncr.34011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurney JK, Millar E, Dunn A, et al. The impact of the COVID-19 pandemic on cancer diagnosis and service access in New Zealand—a country pursuing COVID-19 elimination. Lancet Reg Health West Pac. 2021;10:100127. doi: 10.1016/j.lanwpc.2021.100127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299-309. doi: 10.1046/j.1365-2710.2002.00430.x [DOI] [PubMed] [Google Scholar]
- 11.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42(4):1187-1195. doi: 10.1093/ije/dyt092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zeileis A. Object-oriented computation of Sandwich estimators. J Stat Softw. 2006;16(9):1-16. doi: 10.18637/jss.v016.i09 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. The observed and expected number of prostate biopsies and new prostate cancer diagnoses had there not been a pandemic interruption, stratified by race
eTable 2. Incidence rate ratios from the Poisson generalized linear models