Abstract
Background
Centers of excellence (COEs) are interdisciplinary healthcare organizations created with the goal of improving health/economic outcomes in medical treatment for both individuals and health systems, compared to traditionally structured counterparts. Multiple studies have highlighted both societal/individual burdens associated with back pain, underscoring the importance of identifying new avenues for improving both cost/clinical outcomes for this patient population. Here, we utilize available literature to better characterize the features of a spine COE at a tertiary care center and determine the impact of COEs on patient satisfaction and outcomes.
Methods
A systematic review describing spine COEs was performed. PubMed, OVID, Cochrane, Web of Science, and Scopus were utilized for electronic literature search. Data including institution, department, pathologies treated, patient satisfaction scores, patient outcomes, and descriptions of the COE, were extracted and analyzed by two reviewers per full-text article. Inclusion criteria consisted of literature describing the organization, purpose, or outcomes of a spine COE, all publication types (except technical/operative report), adult or pediatric patients, publication from inception through September 2021. Exclusion criteria consisted of articles that do not discuss spinal COEs, technical/operative reports, studies unavailable in English language, unavailable full text, or non-human subjects. The Newcastle-Ottawa Quality Assessment Scale was used to assess the quality of the included studies.
Results
Five hundred and sixty-seven unique publications were obtained from the literature search. Of these articles, 20 were included and 547 were excluded based on inclusion and exclusion criteria. Following full-text review of the 20 publications, 6 contained pertinent data. Quantitative data comparing COE versus non-COE was contradictory in comparing complication rates and episodic costs. Qualitative data included descriptions of spine COE features and cited improved patient care, technical advancements, and individualized care paths as positive aspects of the COE model. Mean risk of bias assessment was 3.67.
Discussion
There is little evidence regarding if spine COEs provide an advantage over traditionally organized facilities. The current number and heterogeneity of publications, and lack of standardized metrics used to define a spinal COE are limiting factors. Spinal COE may offer higher value care, reduced complication rates and advancements in knowledge and technical skill.
Keywords: Spine, center of excellence, center of excellence (COE), neurosurgery, spine surgery
Introduction
Advances in surgical care over the last century are breathtaking. Operations like repairing the thoracic aorta or performing liver transplants that were once nearly uniformly fatal now are able to be performed routinely with fatalities being a rarity. This innovation emerged from surgical teams dissecting their cases, learning from their mistakes, reexamining their decisions, techniques and processes, and implementing improvements. We believe the next phase of surgical innovation will be to reapply the approach used by Ernest Codman, taking lessons learned out of the operating room and applying them to the entire continuum of care, in order to eliminate defects in value and improve the patient experience. A recently published study showed that potentially $900 billion are wasted in the US healthcare system, and projected savings could reduce this figure by over 25% signaling that healthcare efficiency should be a focus for all specialties within medicine (1).
Centers of excellence (COEs) are interdisciplinary groups with the goal of improving health outcomes for a given disease process while reducing costs for patients. As healthcare progresses toward individualized medicine and emphasizes more efficient healthcare utilization, many medical specialties are attempting to enhance patient experience and improve health outcomes through the creation of COE. There is emerging literature that suggests COE reduce mortality and morbidity and also improve patient satisfaction across multiple specialties (2-5).
Given these outcomes, there is a push towards having more standardized implementation of COEs, particularly for conditions that require multidisciplinary collaboration, such as deformity correction, degenerative spine, and back pain. According to a 2013 Mayo Clinic Rochester Epidemiology Project paper, back problems were the third-most prevalent disease group for which patients sought out healthcare, making up 24% of the studied population, behind only skin disorders and joint disorders (6). Furthermore, the 2010 Global Burden of Disease study found that out of 291 conditions studied, low back pain ranked highest globally in terms of years with disability (7). These studies, paired with recent estimates that the cost of treating low back and neck pain reached $86 billion per year (8), highlight the importance of finding new methods for improving both the cost and clinical outcomes associated with back pain.
Spine COEs entail collaboration between neurological surgery, orthopedic surgery, radiology, physical medicine and rehabilitation, physiatry, behavioral medicine, pain management, occupational therapy, physical therapy, nursing, acupuncture, and other specialties. Housed under one roof, these specialties share the common goal of contributing streamlined care to their patients. The Joint Commission (JCO) defines broad criteria for a COE as the ability of a hospital system to earn specific care certifications and designation for various disease states, conditions, and procedures (9). Specific to spine, there is currently no set criteria or centralized body that defines or designates spine COE. Furthermore, studies comparing the health outcomes of designated spine COEs versus non-designated centers have shown conflicting results (2,10). The overall lack of studies on this topic emphasizes the need for evaluating the effectiveness of these centers, as they are inevitably created across the country.
Here, we have compiled existing literature describing spine COEs in a systematic review, with the aims of examining the features of a spine COE at tertiary care centers, determining if spine COEs impact patient satisfaction and patient outcomes at tertiary care centers, and examining if principles that guide creation and operation of spine COE can be extracted from the existing literature.
We identified systematic review as the appropriate methodology to address these research questions as it provided us with a template through the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist to locate all pertinent, existing literature and extract relevant data. We identified features of spine COEs at tertiary care centers identified in the literature, as well as patient satisfaction and outcomes, and principles of creation and operation of spine COEs. This allowed us to provide a description of our own tertiary care center spine COE and create our own working definition of a spine COE. We present the following article in accordance with the PRISMA reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-21-46/rc).
Methods
Literature search
The following databases were searched from inception through September 2021 for relevant studies: PubMed (MEDLINE), Ovid (MEDLINE), Cochrane CENTRAL, Web of Science, and Scopus. The search strategies combined text words and relevant indexing using appropriate Boolean operators to capture the papers discussing the features of spine COE. The literature search used the following terms (including synonyms and other closely related words): “spine” or “neuro*” or “cranial” and “center of excellence”. These search terms are thought to cover all pertinent literature because “center of excellence” is the only term used in the medical literature to describe an institution that formally endorses interdisciplinary collaboration aimed at improving both clinical outcomes and research for a given disease process. The date range searched was 1961 to present. The searches were not limited by study design or date of publication, but only to references published in the English language. The reference lists of included papers were assessed for additional relevant studies not retrieved in the databases. The full publication search strategy is shown in the appendix. To assure standardization and independent validation we have conducted our research according to PRISMA guidelines, addressed quality and risk of bias, and provided our full publication search strategy.
Inclusion and exclusion criteria
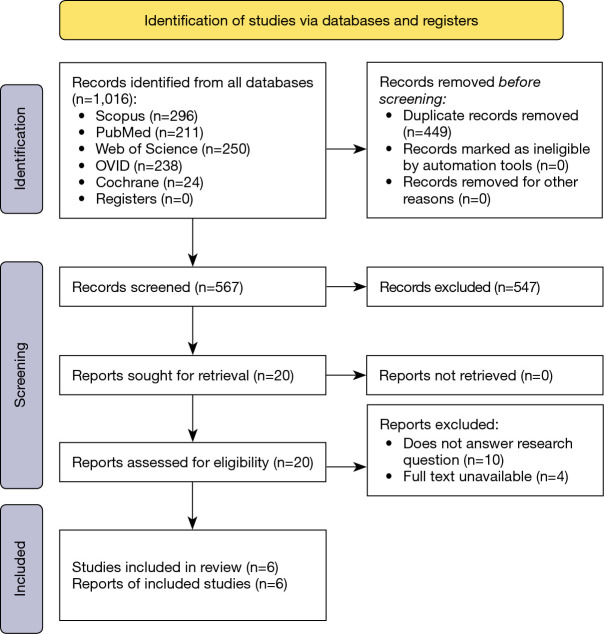
Inclusion of articles into the study was based on four criteria: (I) papers describe the organization, purpose, or outcomes of a spine COE; (II) cohort study, observational study, randomized controlled trial, systematic review, case series, case reports, database study, literature review, or data analysis; (III) adult or pediatric patients undergoing spinal surgery; (IV) publication from inception through September 2020. Exclusion from the study consisted of six criteria: (I) does not discuss spinal COEs; (II) technical or operative reports regarding spine surgeries; (III) unavailable in English language; (IV) full text unavailable; (V) non-human subjects. Initial screening of the articles was conducted independently by five reviewers. Titles and abstracts were screened by two individual reviewers for the inclusion and exclusion criteria, with a third reviewer to decide any conflicts. A full text screen was then performed in the same fashion to produce the final included articles (Figure 1).
Figure 1.
PRISMA 2020 flow diagram.
Data extraction
The data extracted from the studies include the institution involved, the department using a COE model, pathologies treated at the COE, patient satisfaction scores, and a general description of the COE. Qualitative as well as quantitative data regarding the COEs was obtained. When available, qualitative descriptions regarding the importance of a COE in general was also extracted.
Data analysis and assessment of articles
The limited number of relevant articles as well as variation in study design prevented analysis beyond a descriptive study. Extracted data from articles was used to answer the two questions: (I) what are the features of a spine COE at tertiary care centers and (II) how do these COEs impact patient satisfaction and outcomes. A combination of quantitative and qualitative data was used in this process.
Assessment of quality and risk of bias
A modified Newcastle-Ottawa Scale was used to assess the quality of the included studies. The Newcastle-Ottawa Scale is a rating tool for quality assessment of studies that are non-randomized for systematic reviews using three categories: selection, comparability, and outcome. Possible total points are 3 points for Selection, 2 points for Comparability, and 3 points for Outcomes.
Results
Literature search
The literature search noted above returned a total of 1,016 published articles, 211 citations were obtained from PubMed, 296 citations were obtained from Scopus, 238 citations were obtained from OVID, 24 citations were obtained from Cochrane, and 250 citations were obtained from Web of Science. Following removal of duplicates, 567 publications met criteria for screening. After title and abstract screening, 20 articles underwent full-text screening, six of which met final inclusion criteria (Tables 1,2).
Table 1. Included publications.
| Title | Author | Year | Type of study | Institution/location | Summary |
|---|---|---|---|---|---|
| Forty years of Clinical Excellence at the Dr A Lakshmipathi Neurosurgical Centre and Post-Graduate Institute of Neurological Surgery, Voluntary Health Services Hospital | Sridhar et al. | 2019 | Review article | Lakshmipathi Neurosurgical Center Tamil Nadu, India | Outlines the improvements in surgical technique, research, and surgical outcomes that occurred at a neurosurgery center of excellence |
| Finding the Value in ‘Value’ Designation: Evidence and Opportunity in the United States | Sze-Jung Wu et al. | 2016 | Retrospective observational | United States | Retrospective study examining which metrics designating a COE were associated with superior outcomes |
| Annual Number of Spinal Cord Stimulation Procedures Performed in the State of Florida During 2018: Implications for Establishing Neuromodulation COE | Richard Epstein | 2018 | Retrospective, quantitative | Florida | Assess the volume of spinal cord stimulation procedures per physician: a feature used to identify COE, in which 100 procedures performed is a factor that helps indicate a center of excellence in specialized surgical procedures |
| Spine COE: Applications for the Ambulatory Care Setting | Sheha & Iyer | 2019 | Review article | N/A | Explains the design, tenets, benefits, and limitations that are found within a center of excellence through the lens of an ever-changing landscape of healthcare economics |
| Evaluation of a Center of Excellence Program for Spine Surgery | Mehotra et al. | 2013 | Retrospective, quantitative |
University of California Los Angeles; University of Pittsburgh | Compares spine surgery outcomes for patients at hospitals designated as spine COE versus patients at undesignated hospitals, eventually seeing minimal differences in surgical outcomes between the two types of centers |
| Great Hospitals in North America: The Medical College of Wisconsin Neurological Surgery | Montoure et al. | 2019 | Review article | Medical College of Wisconsin |
Describes how MCW, Medical College of Wisconsin integrates a multidisciplinary approach when it comes to running their neurosurgical center of excellence, which encompasses surgery of the spine |
COE, center of excellence.
Table 2. Publications that met many inclusion criteria but were not included.
| Title | Author | Year | Reason for exclusion |
|---|---|---|---|
| Centers of excellence for neuromodulation: a critical proposal | Levy | 2014 | Does not answer the research question |
| Managing orthopedics and neurosciences costs through standard treatment protocols | McGinnity and Pluth | 1994 | Full text unavailable |
| Neurotrauma at the All India Institute of Medical Sciences Bhubaneswar: An Overview | Dash et al. | 2019 | Does not answer the research question |
| Partnerships for science-based development: Neuroscience Network as a practical model | Kenney Wallace et al. | 1996 | Full text unavailable |
| Quality Spine Care: Healthcare Systems, Quality Reporting, and Risk Adjustment | Ratliff et al. | 2018 | Does not answer the research question |
| Overcoming barriers to neurosurgical training in Tanzania: International exchange, curriculum development, and novel methods of resource utilization and subspecialty development | Ormond et al. | 2018 | Does not answer the research question |
| Improving Outcomes with Subspecialization and Regionalization | Das and Guillaume | 2018 | Does not answer the research question |
| Neuroscience - Your Next Center of Excellence | Souhrada | 1988 | Full text unavailable |
| Development of the Neurological Institute: a strategic, improvement, and systems approach | Tinsley et al. | 2011 | Does not answer the research question |
| Neuroimaging to develop in African centers of excellence | Kalaria | 2001 | Full text unavailable |
| Under one roof: The Miami Project to Cure Paralysis model for spinal cord injury research | Kleitman | 2001 | Does not answer the research question |
| Neurosurgery at All India Institute of Medical Sciences, a center of excellence: A success story | Singh et al. | 2015 | Does not answer the research question |
| Neurosciences: creating a center of excellence | Coile and Markham | 2003 | Does not answer the research question |
| Advances in management of neurosurgical trauma in different continents | Coile et al. | 2001 | Does not answer the research question |
Study quality and risk of bias
The NOS scores for the assessed studies are included (Table 3). Scores ranged from 1 to 7 and averaged 3.67±2.68. A limitation of our NOS is the lack of outcome and comparability scores for three of the included articles as they are both review articles focusing on a description of spine COE, rather than a comparative study design with exposed cohorts and statistical analysis. All studies had ascertainment of exposure to spine COE.
Table 3. Risk of bias assessment—modified Newcastle-Ottawa Scale.
| Study (first author, publication year) | Selection | Comparability | Outcome | Total NOS Scoring | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Representative of the exposed cohort | Selection of external control | Ascertainment of exposure | Comparability of groups (0= no groups, 1= no matching of subjects, 2= subjects were comparable) | Ascertainment of Assessment (independent or blind, record linkage, self-report, or no description) | Statistical test (0= statistical test, not described or incomplete, 1= statistical test is appropriate and described in a comprehensive manner) |
Complete follow-up of all subjects accounted for | ||||||
| Sridhar, 2019† | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | ||||
| Sze-Jung Wu, 2016 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 7 | ||||
| Epstein, 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | ||||
| Sheha, 2019† | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | ||||
| Mehrotra, 2013 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 6 | ||||
| Montour, 2019† | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | ||||
†, indicates review articles: limited by study design that lacks comparability or outcomes. NOS, Newcastle-Ottawa Scale.
Outcomes
A 2019 paper by Sridhar et al. discusses the 40-year history and benefits of the Achanta Lakshmipathi Neurosurgical Center in Tamil Nadu, India (11). Sridhar et al. outline the improvements in surgical technique, research, and surgical outcomes that occurred as a result of the neurosurgery COE. For example, as a result of the high case volume and centralized system for complex cases, surgeons discovered that the diagnosis of opacification of the posterior longitudinal ligament (OPLL) was considerably underdiagnosed within the region. The authors also report that the resources and faculty available led to technical advancement in operative technique, specifically involving the craniovertebral junction. While Sridhar et al. discuss the several benefits of the COE, they do not report objective findings in this publication to quantify its impact.
A 2016 retrospective study by Wu et al. examined which metrics designating a COE were associated with superior outcomes (2). A large-scale analysis of 33,827 adults who received spinal surgery revealed that value-based COE programs were able to identify facilities with lower costs and equivalent or better patient outcomes. The study reported a significantly higher number of operations performed by COEs compared to other facilities (5,511.8 vs. 4,034.2). It also reported that the COEs tended to have academic affiliation significantly more often than other facilities (68.6% vs. 34.8%). Interestingly, the study did not find a difference in COEs compared to other facilities when examining patient experiences. The criteria used to evaluate patient experience were: patients given information about what to do after discharge (85.4% vs. 85.2%); doctors always communicated well (79.5% vs. 79.3%); nurses always communicated well (76.9% vs. 77.4%); and definitely would recommend the hospital (74% vs. 73%).
In 2018, a data analysis review by Epstein et al., examined spinal cord stimulation procedures that were performed by physicians in the state of Florida, using the FloridaHealth database (12). The volume of spinal cord stimulation procedures (set at 100 in this study) per physician was used as a feature to identify COEs. The assumption here is that better outcomes following surgical procedures are associated with higher caseloads at the hospital or physician level. Out of 10,762 spinal cord stimulation cases, 606 physicians performed at least one spinal cord stimulation procedure, however 78.4% of physicians performed less than 2 cases per month. Nine physicians performed at least 100 cases in the span of 2018, and 56.9% of all cases were provided by physicians performing less than four cases per month. All together, close to 1% of physicians in the state of Florida in 2018 would be considered as high volume, in respect to spinal cord stimulation procedures, meeting the threshold indicated for center of excellence status. Neither outcomes nor indications of medical necessity were reported to compare between groups.
In 2019, Sheha and Iyer explain the design, tenets, benefits, and limitations that are found within a center of excellence (9). They define a healthcare center of excellence using an Elrod & Fortenberry definition, “A program within a healthcare institution which is assembled to supply an exceptionally high concentration of expertise and related resources centered on a particular area of medicine, delivering associated care in a comprehensive, interdisciplinary fashion to afford the best patient outcomes possible” (13), and add that the goal of these centers is to provide successful, cost-effective treatment to its patients. Several studies are noted comparing designated COEs and non-designated centers, separately showing: no difference in complications or readmissions among the two populations secondary to cervical fusions, lumbar fusions, and lumbar discectomies/decompressions (10), designated COE for hip and knee surgery showed lower complication rates for hip surgery (10), and BlueCross value-designated facilities showed decreased cost and complication rates in lumbar and cervical spine surgery (2). They define key tenets for a successful COE including: creating value through the highest quality of care at the lowest cost, centralization of organization benefits, and multidisciplinary team building and protocol creation to transition spine care safely and effectively into the outpatient setting as medical advances continue.
Mehrotra et al. at the University of California Los Angeles and University of Pittsburgh conducted a case control study that focused on comparing spine surgery outcomes in spine COE versus undesignated hospitals (10). They examined cervical fusions with or without discectomy/decompression, lumbar fusions with or without discectomy/decompression, and lumbar discectomies/decompressions without fusion from 2007–2009. Findings include statistically significant improvements in surgical care. Comparing COE (N=369) to non-designated hospitals (N=1,499), patients were more often given antibiotics within one hour before surgery (95.2% vs. 93.5%), antibiotics were stopped at the appropriate time more often (92.4% vs. 90.1%), more often the correct antibiotics were given (97.6% vs. 96.7%), more often patients received DVT prophylaxis (95.1% vs. 91.7%), and glucose was more often controlled (90.7% vs. 84.0%), all of which were significant differences (P<0.01). However, the differences in complications rates and readmission rates for patients 30 days post op as well as the differences in cost of procedures at 90 days post op were statistically insignificant between designated and undesignated hospitals for the procedures studied.
Montoure et al. describes how the Medical College of Wisconsin (MCW) integrates a multidisciplinary approach when it comes to running their neurosurgical COE (14). Their expansion of the department of neurosurgery started with biomechanical spine research that focused on areas such as cerebellar and spinal cord stimulation, with their capacity for translational neurosurgery research increasing as the department grew. As their institution expanded, they created a $32.5 million federally funded spinal cord injury unit, and have been able to focus efforts towards spine biomechanics, vehicle crash trauma, and stem cell transplantation for spinal cord injury. As a COE, they have been able to provide an interdisciplinary approach towards translational medicine that has positively impacted patient care.
Discussion
Spine COE are a designation that falls under the broader umbrella of neurosurgical COE, which are intended to provide comprehensive care through the seamless integration of research and clinical practices. The designation of “center of excellence” has been implemented since 2006, but more than a decade later there have been limited critical appraisals of spine COE in the literature (3). From our search of the literature, there appears to be a paucity of articles addressing the surgical outcomes at spine COE, with most data sources already being multiple decades old. Moreover, the literature lacks explicit measurable criteria for defining a COE in spine and as a result, the variation in what defines a COE likely influences the evidence regarding the impact of spine COEs. The practice of spine surgery has changed drastically over the last twenty years, with the vast expansion of minimally invasive techniques, deformity correction, and operative imaging/equipment available. Given these considerations, further investigation is warranted into the true value of spine COE in the modern era.
The two papers that present objective data on patient outcomes (9,10) show conflicting evidence towards the effectiveness of these designated centers. The exclusion of complex spine procedures from many studies examining COE is one explanation for this as the small subset of common procedures that these studies focused on may reduce the variability of post-operative outcomes given that these procedures have been widely practiced and standardized. Additionally, many COE offer procedures not commonly performed elsewhere. As such, improved outcomes may be more evident when considering these complex procedures, as they are not as widely practiced or standardized, which may show more notable differences in surgical and post-operative outcomes. Furthermore, the current literature does not explore whether patients evaluated at a spine COE suffer an equivalent or greater degree of comorbidity and disease to the general population. Overall, differences in outcomes may be more evident in comparing COE to non-COE institutions when examining the value advanced, high volume, diverse care teams provide for complex surgeries in complicated and sick patients.
Although spine COE have been found to show no significant, empirical improvements in patient outcomes, there are limitations to the findings of the studies included. Most notably, it appears that the procedural outcomes measured did not specifically address the variation in and definition of COE. For instance, a key metric that can be used to evaluate the effectiveness of spinal COE is cost effectiveness, but this metric was minimally studied. Additionally, since the primary goal of COEs is to minimize costs for patients, the cost for each service could be compared using the “allowed amount,” the sum of health plan reimbursement and any patient copayment or deductible. Evaluating the change of this amount from traditional hospitals to COEs would be an effective way for determining the benefits of COEs that has not been well studied in the spine COE literature. Another component that would be helpful in evaluating spine COEs is considering the appropriateness of procedures performed. A number of groups are producing appropriateness criteria for various spine pathology and spine COEs may be able to standardize the use of these criteria in an effort to limit unnecessary operations (15,16).
One aspect that is not often addressed in the COE spine literature is improvements in the patient experience. Aside from the actual operation a patient may undergo, patients need access to specialty care, preoperative evaluation, and effective postoperative coordination with multiple teams upon discharge. For many patients, accessing and evaluating specialty care can be difficult; patients generally have little to no information about the quality of the surgeon or the hospital, even information as basic as how many cases the surgeon and hospital perform each year. Effective preoperative evaluation potentially involves evaluation by multiple teams, which can be more efficient in a center that has a standardized pathway. After a procedure, patients are sent back to their primary care physician and often require home health, physical therapy and durable medical equipment. Too many patients experience gaps in care transitions, increasing the risk for readmission and reducing the patients’ experience. While these defects may not drive up cost, they compromise patient experience and are ways that spine COEs may provide added value.
Mehotra et al. suggests criteria for spine COEs include a comprehensive inpatient facility, full facility accreditation, duration of spinal surgery greater than 12 months, at least two qualified surgeons performing spinal surgery, program employs shared decision making, a high volume of spinal surgery, hospital and surgeons are providers in the local health plan network (10). As there is no overarching body to define spinal COE, our group’s working definition would include Mehotra et al. suggested criteria as stated above, as well as including intensive care unit as part of the comprehensive inpatient facility, a focus on cost sharing across divisions within the COE with standardization of equipment and practices, the implementation of quality improvement teams that track operative and postoperative benchmarks, implementation and adherence of appropriateness criteria in evaluating surgical candidates, and comprehensive patient feedback surveying to capture and improve upon the patient experience.
Description of a single institution’s spine center of excellence
Our health system is a Midwest academic tertiary care center with both orthopedic and neurosurgical departments with associated residency programs. The departments have collaborated under the direction of two spine surgeons (one from each department) and the hospital’s Chief Clinical Transformation Officer to create a spine COE. The COE’s mission entails three primary emphases: value, quality, and accountability. Current goals within our COE include standardization of protocols for the workup of suspected spinal cord compression across the regional hospital system to improve time to diagnosis, transport, and intervention. Additionally, vendors and equipment are being unified and standardized across surgeons and the two departments to improve cost savings and resource utilization.
Conclusions
COE are established paragons for institutions within many areas of medicine. The concept of COE for the field of spine have been developing for multiple decades, but at this point specific characteristics of these institutions based on objective evidence of the value they provide is lacking. Our study reports the literature that is currently published regarding spine COE and presents directions for future research into the field. Ultimately, the landscape of healthcare is changing, and the further development of spine COE may lead to significant gains within the field and improvement upon the delivery of high-quality care to patients where there is an urgent need to address these defects. If we are to finally improve the value of care, we will need to make visible and eliminate all defects in value in surgical care.
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-21-46/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-21-46/coif). GS presently receives consulting fees as a Stryker consultant. The other authors have no conflicts of interest to declare.
References
- 1.Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA 2019;322:1501-9. 10.1001/jama.2019.13978 [DOI] [PubMed] [Google Scholar]
- 2.Wu SJ, Ma Q, Martin P, et al. Finding the Value in 'Value' Designation: Evidence and Opportunity in the United States. Manag Care 2016;25:36-42. [PubMed] [Google Scholar]
- 3.Livingston EH. Bariatric surgery outcomes at designated centers of excellence vs nondesignated programs. Arch Surg 2009;144:319-25; discussion 325. 10.1001/archsurg.2009.23 [DOI] [PubMed] [Google Scholar]
- 4.Das P, Guillaume DJ. Improving Outcomes With Subspecialization and Regionalization. In: Guillaume DJ, editors. Quality and Safety in Neurosurgery: Academic Press, 2018:225-36. [Google Scholar]
- 5.Basso A, Previgliano I, Duarte JM, et al. Advances in management of neurosurgical trauma in different continents. World J Surg 2001;25:1174-8. 10.1007/s00268-001-0079-3 [DOI] [PubMed] [Google Scholar]
- 6.St Sauver JL, Warner DO, Yawn BP, et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined American population. Mayo Clin Proc 2013;88:56-67. 10.1016/j.mayocp.2012.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968-74. 10.1136/annrheumdis-2013-204428 [DOI] [PubMed] [Google Scholar]
- 8.Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. 10.1001/jama.299.6.656 [DOI] [PubMed] [Google Scholar]
- 9.Sheha ED, Iyer S. Spine centers of excellence: applications for the ambulatory care setting. J Spine Surg 2019;5:S133-8. 10.21037/jss.2019.04.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehrotra A, Sloss EM, Hussey PS, et al. Evaluation of a center of excellence program for spine surgery. Med Care 2013;51:748-57. 10.1097/MLR.0b013e31829b091d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sridhar K, Vasudevan MC, Krishnan SS, et al. Forty years of clinical excellence at the Dr A Lakshmipathi Neurosurgical Centre and Post-Graduate Institute of Neurological Surgery, Voluntary Health Services (VHS) Hospital. Neurol India 2019;67:516-29. 10.4103/0028-3886.257984 [DOI] [PubMed] [Google Scholar]
- 12.Epstein RH, Dexter F, Podgorski EM, 3rd, et al. Annual Number of Spinal Cord Stimulation Procedures Performed in the State of Florida During 2018: Implications for Establishing Neuromodulation Centers of Excellence. Neuromodulation 2021;24:1341-6. 10.1111/ner.13066 [DOI] [PubMed] [Google Scholar]
- 13.Elrod JK, Fortenberry JL, Jr. Centers of excellence in healthcare institutions: what they are and how to assemble them. BMC Health Serv Res 2017;17:425. 10.1186/s12913-017-2340-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montoure A, Janich K, Cusick JF, et al. Great Hospitals in North America: The Medical College of Wisconsin Neurological Surgery. World Neurosurg 2019;125:55-66. 10.1016/j.wneu.2018.12.210 [DOI] [PubMed] [Google Scholar]
- 15.Reitman CA, Cho CH, Bono CM, et al. Management of degenerative spondylolisthesis: development of appropriate use criteria. Spine J 2021;21:1256-67. 10.1016/j.spinee.2021.03.005 [DOI] [PubMed] [Google Scholar]
- 16.Mannion AF, Pittet V, Steiger F, et al. Development of appropriateness criteria for the surgical treatment of symptomatic lumbar degenerative spondylolisthesis (LDS). Eur Spine J 2014;23:1903-17. 10.1007/s00586-014-3284-0 [DOI] [PubMed] [Google Scholar]