Abstract
The COVID-19 crisis has exposed the public to considerable scientific uncertainty, which may promote vaccine hesitancy among individuals with lower tolerance of uncertainty. In a national sample of US adults in May–June 2020, we examined how both perceptions of uncertainty about COVID-19 and trait-level differences in tolerance of uncertainty arising from various sources (risk, ambiguity, and complexity) are related to vaccine hesitancy-related outcomes, including trust in COVID-19 information, COVID-19 vaccine intentions, and beliefs that COVID-19 vaccines should undergo a longer testing period before being released to the public. Overall, perceptions of COVID-19 uncertainty were not associated with trust in information, vaccine intentions, or beliefs about vaccine testing. However, higher tolerance of risk was associated with lower intentions to get vaccinated, and lower tolerance of ambiguity was associated with lower intentions to get vaccinated and preferring a longer period of vaccine testing. Critically, perceptions of COVID-19 uncertainty and trait-level tolerance for uncertainty also interacted as predicted, such that greater perceived COVID-19 uncertainty was more negatively associated with trust in COVID-19 information among individuals with lower tolerance for risk and ambiguity. Thus, although perceptions of uncertainty regarding COVID-19 may not reduce trust and vaccine hesitancy for all individuals, trait-level tolerance of uncertainty arising from various sources may have both direct and moderating effects on these outcomes. These findings can inform public health communication or other interventions to increase COVID-19 vaccination uptake.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10865-022-00302-9.
Keywords: Uncertainty, Uncertainty tolerance, COVID-19, Vaccine hesitancy, Trust, Ambiguity
Uncertainty about the COVID-19 pandemic has been a major challenge in its management. This uncertainty has had multiple manifestations, including conflicting and changing recommendations from public health entities about how to control the pandemic, inability to predict how long the pandemic will last, and debates regarding the efficacy or safety of treatment and prevention measures (Nagler et al., 2020).
Although uncertainty in medicine can be focused on a variety of substantive issues (Han et al., 2011), perhaps the most salient type of uncertainty raised by the COVID-19 pandemic and other novel health threats is scientific uncertainty about disease-centered issues—e.g., prognosis, cause, prevention and treatment. Although these scientific uncertainties reflect fundamental limits in existing medical knowledge, particularly for dynamic problems such as COVID-19, such uncertainty can be psychologically aversive. Past research has shown that perceptions of scientific uncertainty, as well as experimental exposure to scientific uncertainty in health information, are associated with a variety of negative cognitive, affective, and behavioral responses. Negative cognitive responses to scientific uncertainty include distrust in scientists and public health recommendations (Jensen & Hurley, 2012), a response that has particularly important implications for the control of the COVID-19 pandemic and in the context of vaccination in particular. Distrust in public health experts and recommendations likely contributes to vaccine hesitancy and inhibits widespread adoption of COVID-19 vaccination, which has been advocated by public health agencies across the US and throughout the world. Past studies have shown that individuals with low trust in scientific experts and information have low confidence in vaccines (Larson, 2016) and are less likely to get them (Benin et al., 2006; Fahlquist, 2017; Hornsey et al., 2020).
Other negative cognitive responses to scientific uncertainty include pessimistic risk appraisals (Taber et al., 2015), and lower beliefs in the preventability of disease (Han et al., 2006). In one recent experimental study, the communication of scientific uncertainty about the COVID-19 pandemic increased deliberative and affective risk perceptions about COVID-19 (Han et al., 2021). Negative emotional responses to scientific uncertainty include fear, worry, and distress. A recent study found that uncertainty perceptions were associated with acute stress disorder during COVID-19 among Chinese college students (Lin et al., 2020).
The negative response of perhaps greatest concern for efforts to control the COVID-19 pandemic, however, is lower vaccination uptake. Perceptions of scientific uncertainty have been associated with reduced intentions for health-promoting behaviors (Han et al., 2006; Nagler, 2014; Taber et al., 2015)—a reliable proximal predictor of behavior itself; (Ajzen & Madden, 1986; Webb & Sheeran, 2006). With respect to vaccinations in general, past studies utilizing hypothetical scenarios have suggested that perceptions of uncertainty regarding vaccine safety may increase vaccine hesitancy (Meszaros et al., 1996; Ritov & Baron, 1990). Han and colleagues (2018) found that communicating scientific uncertainty about a novel pandemic reduced vaccine intentions, and that this effect was moderated by health literacy, such that individuals with higher health literacy had a stronger aversive response to uncertainty communication than those with lower health literacy. Another qualitative study of childhood vaccine hesitancy suggested that scientific uncertainty about the harms of vaccination—manifest by perceptions of the missing, conflicting, changing, or otherwise unreliable nature of information about vaccines—was a primary driver of parental vaccine hesitancy (Blaisdell et al., 2016).
Yet, negative effects of scientific uncertainty on vaccine-related perceptions and behaviors have not been consistently observed. For example, Han et al. (2021) showed that although communicating scientific uncertainties surrounding COVID-19 affected risk perceptions, it did not affect intentions for risk-reducing behaviors or vaccination against COVID-19. Another recent study examining the communication of scientific uncertainty about a broader array of topics (e.g., in the form of imprecision in estimates of climate change) found only minor effects on trust (van der Bles et al., 2020). These findings suggest that the psychological effects of scientific uncertainty are likely moderated by various factors that remain to be elucidated.
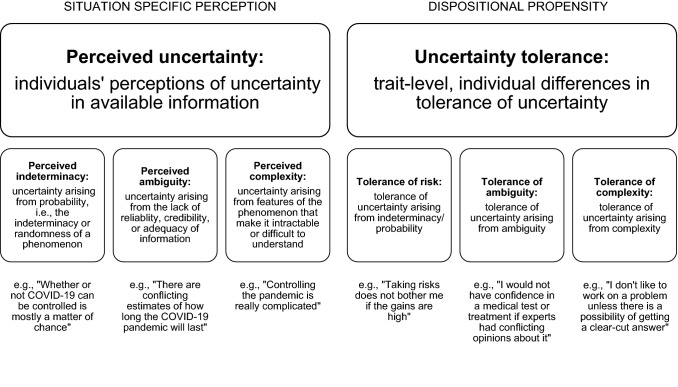
One potential moderating factor may be the specific source of scientific uncertainty, which can vary and have different effects (Bammer & Smithson, 2012; Han et al., 2011). Uncertainty can be classified as arising from three main sources: (1) probability (manifesting the indeterminacy of a phenomenon), (2) ambiguity (manifesting the indeterminability of a phenomenon due to the lack of reliability, credibility, or adequacy of existing information), and (3) complexity (manifesting the intractability of a phenomenon due to features that make it difficult to understand). To elaborate, uncertainty arising from probability ultimately reflects ignorance about a given outcome, due to fundamental randomness in the underlying phenomenon; this uncertainty is experienced even when evidence-based probability estimates—e.g,. of COVID-19 mortality—are available, given due to the limited applicability of such estimates to individual futures. Uncertainty arising from ambiguity, however, ultimately reflects ignorance about the state of knowledge of a given outcome, due to shortcomings in available evidence; this uncertainty is experienced whenever information is missing, changing, conflicting (e.g,. as a result of discrepant findings from multiple studies, or expert disagreement), or imprecise (e.g., a range rather than a point estimate of probability). Finally, uncertainty arising from complexity ultimately reflects ignorance about a given outcome, due to the inability to make sense of available evidence; this uncertainty is experienced whenever existing information has multiple attributes, dependencies, or interrelationships (see Fig. 1 for a visual schematic of these distinctions).
Fig. 1.
Definition schematic of uncertainty perceptions and tolerance and their subtypes
A large body of behavioral decision research suggests that uncertainties arising from probability, ambiguity, and complexity have independent effects (Han et al., 2011). A recent review by Gustafson and Rice found that scientific uncertainty resulting from disagreement or conflict (which the authors labelled “consensus uncertainty”) typically had negative effects, whereas uncertainty resulting from error ranges and probabilities (which the authors labelled “technical uncertainty”) typically had positive or null effects (Gustafson & Rice, 2020). Although these classification schemes differ in how they characterize sources of uncertainty, they both suggest that scientific uncertainties arising from different sources have distinct effects.
Individual differences in people’s tolerance of uncertainty are another factor that may moderate the psychological effects of scientific uncertainty. That is, although specific beliefs and perceptions about uncertainty that are relevant to a specific situation or context (e.g., COVID-19) often have negative psychological effects—including heightened perceptions and feelings of risk, and avoidance of decision making—these effects vary among individuals, depending on trait-level differences in uncertainty tolerance (Hillen et al., 2017). In a systematic review, uncertainty tolerance was associated with a variety of cognitive, emotional, and behavioral outcomes related to health and healthcare—including likelihood of deferring to expert opinions in medical decision-making, as well as emotional well-being (Strout et al., 2018). In the context of cancer screening, individuals with lower uncertainty tolerance (i.e., higher aversion to ambiguity) perceive fewer benefits of cancer screening, greater harm, and greater ambivalence about cancer screening tests, and have lower cancer screening intentions (Han et al., 2014). In the context of COVID-19, it is plausible that trait-level differences in uncertainty tolerance may either moderate individuals’ responses to scientific uncertainty, or directly increase vaccine hesitancy. To our knowledge, few studies have assessed relationships between uncertainty tolerance and COVID-19-related behaviors, but one recent study found that uncertainty tolerance was associated with greater appraisals of threat and stress from the pandemic, which were in turn associated with greater pandemic-related anxiety (Wright, Faul et al., 2021).
Yet because uncertainty itself is not a monolithic but a multidimensional phenomenon, uncertainty tolerance can also be disaggregated into distinct sub-types that correspond to the three main sources of uncertainty (probability, ambiguity, complexity) (Han et al., 2015), and measures of these sub-types of individual, trait-level uncertainty tolerance have been previously developed. For example, tolerance of uncertainty arising from probability (often referred to in this context as “risk”) describes individuals’ dispositional level of comfort taking risks when outcomes are indeterminate and has been assessed by measures such as the Pearson Risk Attitude scale, e.g., “Taking risks does not bother me if the gains involved are high”; Pearson et al., 1995). Tolerance of uncertainty arising from ambiguity (in the decision theory sense signifying the lack of reliability, credibility, or adequacy of information; Ellsberg, 1961), describes trait-level aversion to situations where information is inadequate, imprecise, or conflicting, and has been assessed by measures such as the Ambiguity Aversion in Medicine (AA-Med) scale, with items such as “I would not have confidence in a medical test or treatment if experts had conflicting opinions about it” (Han et al., 2009, 2015). Finally, tolerance of uncertainty arising from complexity describes individuals’ disposition to react negatively to situations where information is difficult to comprehend, and has been assessed by measures such as the tolerance for ambiguity scale (TFA; Geller et al., 1990), which includes items such as, “I don’t like to work on a problem unless there is a possibility of getting a clear-cut and unambiguous answer.” Fig. 1 contains a visual schematic defining and organizing each subtype of uncertainty perception and tolerance in the current framework.
Emerging empirical evidence supports the existence of different sub-types of trait-level uncertainty tolerance that may have distinct effects (Anderson et al., 2020; Han et al., 2015). For example, findings from one study suggest that tolerance of uncertainty arising from probability, ambiguity, and complexity changes at different rates over time among medical students (Han et al., 2015). In another study, the three types of uncertainty tolerance discussed above (risk tolerance, ambiguity tolerance, and complexity tolerance) differentially moderated the relationships between oncologists’ perceptions of uncertainty and attitudes and self-efficacy about genomic tumor testing (Anderson et al., 2020). Specifically, all three types of trait-level uncertainty tolerance moderated the relationship between perceived uncertainty and attitudes about genomic tumor testing (such that greater perceived uncertainty was associated with more negative attitudes among oncologists with low uncertainty tolerance), but only tolerance of risk moderated the relationship between perceived uncertainty and self-efficacy. In the context of COVID-19, intolerance of ambiguity (measured by the Need for Closure scale; Roets & Van Hiel, 2007; Webster & Kruglanski, 1994) was associated with higher distress and mediated by increased worry, health information seeking, and beliefs about the perceived utility of lockdown among Italians (Petrocchi et al., 2021). However, risk tolerance was not predictive of distress. Furthermore, one recent preprint reported that the effects of uncertainty about COVID-19 related outcomes differed depending on participants’ attitudes towards ambiguity; specifically, the authors found that higher uncertainty was associated with increased social distancing for “ambiguity-loving” respondents, but not among ambiguity-averse participants (Kishishita et al., 2021). Thus, although some studies have examined uncertainty tolerance in the context of COVID-19, the potential moderating effects of different subtypes of uncertainty tolerance remain to be elucidated.
In summary, it is not currently known whether: (a) perceptions of scientific uncertainty surrounding COVID-19 are related to trust in science and/or vaccine hesitancy; (b) perceptions of scientific uncertainty arising from different sources (i.e., probability, ambiguity, or complexity) are more or less related to trust/vaccine hesitancy; and (c) individual differences in tolerance of uncertainty arising from these specific sources are independently associated with trust/vaccine hesitancy, either directly or indirectly (through their interactions with uncertainty perceptions). The current study was an effort to begin to address these knowledge gaps. Understanding how perceptions of scientific uncertainty and individual differences in uncertainty tolerance contribute to COVID-19 vaccine hesitancy is an important first step to helping individuals respond to scientific uncertainty in a less uncertainty-averse manner.
The study consisted of a secondary data analysis from a large COVID-19 health communication experimental study, conducted in the earlier months of the pandemic in 2020 (see [citation masked for review]), designed to test the effects of different strategies for communicating scientific uncertainty surrounding COVID-19. The current study focused on participants who did not receive an active experimental manipulation, and its objective was to examine the relationship between perceptions of COVID-19 uncertainty, individual, trait-level differences in tolerance of uncertainty arising from different sources, and two main outcomes of interest: (1) trust in health information about COVID-19; and (2) COVID-19 vaccine hesitancy. We focused on trust in public health information as an important outcome of interest given that it is a likely correlate and/or precursor to vaccine hesitancy (Hornsey et al., 2020; Larson, 2016; Schernhammer et al., 2021).
We hypothesized that differences in individuals’ (1) perceived uncertainty regarding COVID-19, and (2) trait-level uncertainty tolerance would each explain unique variance in trust in health information and vaccine hesitancy. We did not have an a priori hypothesis regarding which specific sub-types of uncertainty (probability, ambiguity, or complexity) or uncertainty tolerance would be more strongly associated with the dependent variables of interest; nevertheless, we sought to explore potential differences in the observed associations based on these sub-types. Finally, we also hypothesized interactive effects between perceptions of COVID-19 uncertainty and trait-level tolerance for uncertainty. Specifically, we hypothesized that perceptions of uncertainty would show a stronger negative relationship with trust in COVID-19 information and a stronger positive relationship with vaccine hesitancy among individuals with lower tolerance for uncertainty.
Method
Design and procedure
This cross-sectional study utilized data from a larger online experiment designed to compare the effects of alternative strategies for communicating scientific uncertainty about the nature, transmission, prevention, and treatment of COVID-19 ([citation masked for review]). The strategy used in the control condition consisted of basic information about the nature and prevention of COVID-19, which was developed by a US state public health department and contained no explicit language on scientific uncertainty. In the alternative experimental conditions, this basic information was supplemented by language designed to communicate scientific uncertainty, with and without additional language aimed at “normalizing” uncertainty as an expected state of affairs, promoting hope, and promoting prosocial values. Because the objective of the current study was to examine the influence of pre-existing uncertainty perceptions about COVID-19 and trait-level tolerance of uncertainty, we tested our hypotheses within the control condition alone, to exclude any potential effects of language designed to convey scientific uncertainty or to alter people’s responses to it.
Participants
The study population consisted of a US national sample recruited by Qualtrics® panels from May 7 to June 11, 2020. During this time, the number of total coronavirus infections in the United States increased from > 1.2 million to > 1.6 million, total deaths increased from > 77,200 to > 98,000 (Han et al., 2021), and no effective treatments nor vaccines against COVID-19 were available. Panel members were eligible to participate if they were ≥ 18 years living in the US and belonged to Qualtrics® opt-in web survey panel. Study recruitment employed quotas aimed at balancing the study sample based on age, gender, race, geographic region, education, and income. Participants who reported a previous or current COVID-19 diagnosis were excluded. 303 participants were in the control condition that made up the subsample of interest in the current study. Participant demographic information is reported in Table 1.
Table 1.
Demographic characteristics for analytic sample
| Characteristic | Value (n = 301), % (100%) |
|---|---|
| Age group | |
| < 30 | 69 (22.8) |
| 30–39 | 49 (16.2) |
| 40–49 | 34 (11.2) |
| 50–59 | 39 (12.9) |
| 60–69 | 57 (18.8) |
| > = 70 | 55 (18.2) |
| Race/Ethnicity | |
| White | 173 (57.1) |
| Asian | 34 (11.2) |
| Black or African American | 53 (17.5) |
| Hispanic or Latino | 21 (6.9) |
| Other race | 8 (2.6) |
| More than one race | 14 (4.6) |
| Gender | |
| Male | 129 (42.6) |
| Female | 174 (57.4) |
| US Region | |
| Midwest | 52 (17.2) |
| Northeast | 83 (27.4) |
| South | 102 (33.7) |
| West | 66 (21.8) |
| Education | |
| Less than 4-year college degree | 198 (65.3) |
| 4-year college degree or higher | 105 (34.7) |
| Essential worker statusa | |
| Yes, essential worker | 55 (18.2) |
| Not an essential worker | 230 (75.9) |
| Unsure | 18 (5.9) |
aBased on participants response to the question, “Have you been deemed an essential worker, meaning you are still required to work outside your home during the COVID-19 outbreak? (Yes/No/Unsure).”
Measures
Perceived uncertainty about COVID-19
Perceived uncertainty about COVID-19 was assessed using a 6-item scale (α = 0.71) developed for this study. This measure assessed participants’ perceptions of uncertainty arising from the sources discussed above, with two items each for perceived uncertainty due to probability (hereafter referred to as perceived indeterminacy), perceived ambiguity, and perceived complexity. The full measure can be found in Appendix B. Likert scale response options ranged from 1 (strongly disagree) to 7 (strongly agree). Additionally, we computed subscales defining the different types of perceived uncertainty captured above (perceived indeterminacy, r = 0.62, ambiguity, r = 0.42, and complexity, r = 0.47).
Uncertainty tolerance
Uncertainty tolerance was measured using three scales assessing trait-level tolerance of uncertainty arising respectively from indeterminacy, ambiguity, and complexity.
Pearson risk attitude (PRA)
The PRA scale (Pearson et al., 1995) uses six items (α = 0.72) that measure tolerance of uncertainty arising from indeterminacy/probability (hereafter referred to as tolerance of risk). Higher scores on this scale indicate higher risk tolerance. Example items include: “I enjoy taking risks” and “I try to avoid situations that have uncertain outcomes” (reverse-coded). Likert scale response options ranged from 1 (strongly disagree) to 6 (strongly agree).
Ambiguity aversion in medicine (AA-Med)
The AA-Med scale (Han et al., 2009) is comprised of 5 items (α = 0.70) measuring tolerance of uncertainty arising from ambiguity (hereafter referred to as tolerance of ambiguity) in medicine. Higher scores on the scale indicate lower tolerance of ambiguity. Example items include: “I would not have confidence in a medical test or treatment if experts had conflicting opinions about it” and “If experts had conflicting opinions about a medical test or treatment, I would still be willing to try it” (reverse-coded). Likert scale response options ranged from 1 (strongly disagree) to 6 (strongly agree).
Tolerance for ambiguity (TFA)
The TFA scale (Geller et al., 1990) is a 7-item measure (α = 0.76) that arguably measures tolerance of uncertainty arising specifically from complexity (Han et al., 2015)—e.g., “I don't like to work on a problem unless there is a possibility of getting a clear-cut and unambiguous answer” and “If I am uncertain about the responsibilities involved in a particular task, I get very anxious.” Likert scale response options ranged from 1 (strongly disagree) to 6 (strongly agree). Higher scores on this scale can thus be interpreted as indicating lower tolerance of uncertainty arising from complexity (hereafter referred to as tolerance of complexity).
Outcome variables
Trust in COVID-19 Information
Was measured with a single item measured after participants were exposed to the COVID-19 message. Participants responded to the item, “How much do you trust the information you just read?” on a scale from 1 (not at all) to 7 (completely).
Vaccine hesitancy
Was operationalized with two items examining different components of vaccine confidence/caution: preferences for further vaccine testing and intentions for vaccination.
Preferences for vaccine delay As one element of vaccine hesitancy, we measured participants’ beliefs that vaccine release to the public should be delayed to allow further testing. The text for this item read, “COVID-19 researchers believe that it may take 1–2 years to develop a COVID-19 vaccine, but it could take several years to go through the normal testing for safety and effectiveness. Would you prefer that a full longer testing period be completed before a COVID-19 vaccine is made available to the public, or that the vaccine be released as soon as possible?” Participants responded on a scale from 1 (definitely release the vaccine as soon as possible) to 7 (definitely wait to release the vaccine until full testing has been completed).
Vaccination intentions
Vaccination intentions were measured with a single item: “If a vaccine becomes available for COVID-19, how likely would you be to get vaccinated against COVID-19?” Participants responded on a scale from 1 (definitely would not get a vaccination) to 7 (definitely would get a vaccination).
Covariates: demographics and participant characteristics
A variety of sociodemographic and other relevant participant characteristics were measured and used as covariates in the current analyses, to adjust for their potential confounding effects on the primary associations of interest. We specifically adjusted for race given prior evidence of higher vaccine hesitancy and distrust of healthcare institutions among Black adults in the US, arising at least in part to negative healthcare experiences and the historical abuse of Black individuals by the medical system (Webb Hooper et al., 2021). Covariates included political affiliation (Democrat, Republican, or Independent), race, age group (e.g., < 30, 30–39…70 +), gender, US region, education level (< 4-year college degree, ≥ 4-year college degree), and whether the participant was an essential worker during the COVID-19 pandemic (yes, no, unsure). Covariates were entered into regression models using dummy variables—Table 1 indicates the number of categories that were included for each covariate. In ANOVA models examining differences in the outcomes of interest as a function of each covariate separately, age group (F(5, 297) = 2.49, p = 0.03) and education (F(1, 301) = 6.81, p = 0.01) were significantly associated with trust; political affiliation (F(2, 300) = 4.50, p = 0.01), race (F(5, 297) = 2.38, p = 0.04), and age (F(5, 297) = 2.59, p = 0.03) were significantly associated with vaccine intentions; and age (F(5, 297) = 2.31, p = 0.04) was significantly associated with vaccine testing beliefs.
Statistical analysis
We began by obtaining descriptive statistics and bivariate relationships for the primary variables of interest. Analyses to address the study hypotheses were conducted using multiple regression models examining the main effects and interactions of interest. Specific details are provided within the Results section. Analysis syntax and output are available at https://osf.io/m5nye/?view_only=9ee8d045678c4164a305c1e347d7c6c1.
Given that the sample size collected was determined based upon power considerations for the parent study, we conducted a post hoc power analysis using G*Power. For a multiple regression model with 23 predictors (e.g., the model testing general uncertainty perceptions and tolerance of risk, ambiguity, and complexity with all the included covariates dummy coded), the analytic sample size of n = 303 equates to power ranging from 0.69 to 0.97 to detect effect size f2 ranging from 0.02 to 0.05 respectively (equivalent to effect sizes observed in the current study) for a 1 degree of freedom test at an alpha level of 0.05.
Results
Correlations between uncertainty constructs and outcomes of interest
Bivariate correlations between uncertainty perceptions, uncertainty tolerance measures, and outcomes of interest are presented in Table 2.
Table 2.
Bivariate correlations between key variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Perceived uncertainty (general) | |||||||||
| 2. Perceived indeterminacy | 0.73*** | ||||||||
| 3. Perceived ambiguity | 0.69*** | 0.20*** | |||||||
| 4. Perceived complexity | 0.77*** | 0.29*** | 0.44*** | ||||||
| 5. Tolerance of risk | − 0.05 | 0.06 | − 0.10** | − 0.10** | |||||
| 6. Tolerance of ambiguity | 0.08* | 0.01 | 0.11*** | 0.06 | − 0.25*** | ||||
| 7. Tolerance of complexity | 0.26*** | 0.17*** | 0.16*** | 0.23*** | − 0.16*** | 0.22*** | |||
| 8. Vaccine intentions | 0.02 | − 0.08* | 0.02 | 0.13*** | − 0.15*** | − 0.11*** | 0.12*** | ||
| 9. Preferences for further testing | 0.05 | 0.05 | 0.06 | 0 | − 0.01 | 0.28*** | 0.11*** | − 0.18*** | |
| 10. Trust in COVID-19 information | 0.11** | 0.06 | 0 | 0.17*** | − 0.10** | 0 | 0.13*** | 0.35*** | − 0.07* |
*p < .05
**p < .01
***p < .01
Associations among perceived uncertainty about COVID-19, uncertainty tolerance, trust in COVID-19 information, and vaccine hesitancy
To test our first hypothesis—that perceptions of COVID-19 uncertainty and uncertainty tolerance would each explain unique variance in trust in public health information and vaccine hesitancy—each outcome of interest was regressed on COVID-19 uncertainty perceptions (first, using the full uncertainty perception scale, ignoring type of uncertainty, for purposes of parsimony) and each type of uncertainty tolerance (tolerance of risk, ambiguity, and complexity), controlling for the covariates described above. Results from these models are presented in Table 3. Next, we ran an additional multiple regression model for each outcome, where perceptions of uncertainty were broken down into the three uncertainty subtypes—perceived indeterminacy, ambiguity, and complexity, to examine whether type of uncertainty perception was differentially associated with the dependent variables of interest. Results from these models are presented in Table 4. All results are summarized below.
Table 3.
Regression model results with average (general) uncertainty perceptions, n = 303
| Variable | b | 2.5% CI | 97.5% CI | t− value | p−value | partial η2 |
|---|---|---|---|---|---|---|
| Outcome: trust in COVID− 19 information1 | ||||||
| Perceived uncertainty (general) | 0.028 | − 0.108 | 0.163 | 0.401 | 0.689 | .001 |
| Tolerance of risk | 0.002 | − 0.167 | 0.172 | 0.027 | 0.978 | < .001 |
| Tolerance of ambiguity | − 0.095 | − 0.259 | 0.069 | − 1.139 | 0.256 | .005 |
| Tolerance of complexity | 0.108 | − 0.062 | 0.277 | 1.252 | 0.212 | .006 |
| Outcome: vaccine intentions2 | ||||||
| Perceived uncertainty (general) | 0.006 | − 0.192 | 0.204 | 0.059 | 0.953 | < .001 |
| Tolerance of risk | − 0.258 | − 0.506 | − 0.011 | − 2.054 | 0.041* | .015 |
| Tolerance of ambiguity | − 0.280 | − 0.520 | − 0.039 | − 2.290 | 0.023* | .018 |
| Tolerance of complexity | 0.124 | − 0.123 | 0.372 | 0.989 | 0.323 | .003 |
| Outcome: preferences for further vaccine testing3 | ||||||
| Perceived uncertainty (general) | 0.135 | − 0.077 | 0.347 | 1.252 | 0.211 | .006 |
| Tolerance of risk | − 0.022 | − 0.288 | 0.243 | − 0.167 | 0.867 | < .001 |
| Tolerance of ambiguity | 0.487 | 0.230 | 0.744 | 3.725 | < .001*** | .047 |
| Tolerance of complexity | 0.003 | − 0.262 | 0.268 | 0.021 | 0.983 | < .001 |
1R2 for all uncertainty predictors = .01
2R2 for all uncertainty predictors = .03
3R2 for all uncertainty predictors = .06
Models control for political affiliation, race, age, gender, region, education, and essential worker status. Perceptions of uncertainty = average perceptions of uncertainty across uncertainty subtype. ***p < .01, **p < .01, *p < .05
Table 4.
Regression model results with uncertainty perception subtypes, n = 303
| Variable | b | 2.5% CI | 97.5% CI | t− value | p− value | partial η2 |
|---|---|---|---|---|---|---|
| Outcome: trust in COVID-19 information1 | ||||||
| Perceived indeterminacy | − 0.019 | − 0.115 | 0.077 | − 0.384 | 0.701 | .001 |
| Perceived ambiguity | − 0.016 | − 0.144 | 0.112 | − 0.247 | 0.805 | < .001 |
| Perceived complexity | 0.068 | − 0.053 | 0.190 | 1.104 | 0.271 | .004 |
| Tolerance of risk | 0.013 | − 0.160 | 0.185 | 0.144 | 0.886 | < .001 |
| Tolerance of ambiguity | − 0.084 | − 0.251 | 0.084 | − 0.981 | 0.327 | .003 |
| Tolerance of complexity | 0.100 | − 0.07 | 0.270 | 1.159 | 0.248 | .005 |
| Outcome: vaccine intentions2 | ||||||
| Perceived indeterminacy | − 0.101 | − 0.241 | 0.039 | − 1.418 | 0.157 | .007 |
| Perceived ambiguity | 0.064 | − 0.123 | 0.250 | 0.675 | 0.500 | .002 |
| Perceived complexity | 0.073 | − 0.104 | 0.250 | 0.809 | 0.419 | .002 |
| Tolerance of risk | − 0.222 | − 0.473 | 0.030 | − 1.737 | 0.084 | .011 |
| Tolerance of ambiguity | − 0.282 | − 0.527 | − 0.038 | − 2.276 | 0.024* | .018 |
| Tolerance of complexity | 0.108 | − 0.140 | 0.356 | 0.855 | 0.393 | .003 |
| Outcome: preferences for further vaccine testing3 | ||||||
| Perceived indeterminacy | − 0.015 | − 0.165 | 0.135 | − 0.193 | 0.847 | < .001 |
| Perceived ambiguity | 0.197 | − 0.003 | 0.396 | 1.938 | 0.054 + | .013 |
| Perceived complexity | − 0.023 | − 0.213 | 0.167 | − 0.240 | 0.811 | < .001 |
| Tolerance of risk | − 0.002 | − 0.271 | 0.267 | − 0.013 | 0.990 | < .001 |
| Tolerance of ambiguity | 0.451 | 0.190 | 0.713 | 3.397 | 0.001*** | .040 |
| Tolerance of complexity | 0.001 | − 0.264 | 0.267 | 0.010 | 0.992 | < .001 |
1R2 for all uncertainty predictors = .02
2R2 for all uncertainty predictors = .04
3R2 for all uncertainty predictors = .07
Models control for political affiliation, race, age, gender, region, education, and essential worker status. ***p < .01, **p < .01, *p < .05, + p < .10. “R2 for all uncertainty predictors” reflects the change in R2 for the described model vs. a model that includes only these covariates
Perceived uncertainty about COVID-19
Perceptions of uncertainty were not significantly associated with trust in COVID-19 information. This remained true when the type of uncertainty perception (indeterminacy, ambiguity, and complexity) was considered. Perceptions of uncertainty were not significantly associated with vaccine intentions in models using overall uncertainty perceptions as the independent variable. These results were similar when uncertainty perception subtypes were considered: regardless of subtype, uncertainty perceptions were not associated with vaccine intentions. Finally, uncertainty perceptions were not significantly associated with vaccine testing preferences. Again, in the model separating specific uncertainty perceptions, perceived uncertainty was not associated with vaccine testing beliefs regardless of subtype.
Trait-Level uncertainty tolerance
Dependent variable: trust in information
Neither trait-level tolerance of risk, ambiguity, nor complexity were associated with trust in information.
Dependent variable: vaccine intentions
Tolerance of both risk and ambiguity were significantly associated with vaccine intentions, demonstrating associations in opposite directions, such that higher tolerance of risk was associated with lower vaccine intentions (p = 0.04), and lower tolerance of ambiguity (higher ambiguity aversion) was associated with lower vaccine intentions (p = 0.02). Tolerance of complexity was not significantly associated with vaccine intentions. In the regression models where uncertainty perception subtypes were considered separately, the association between risk tolerance and vaccine intentions became nonsignificant (p = 0.08), but tolerance of ambiguity remained a significant predictor of vaccine intentions (p = 0.02).
Dependent variable: preferences for vaccine delay
Neither tolerance of risk nor tolerance of complexity were not significantly associated with preferences for vaccine delay. However, tolerance of ambiguity was associated with these preferences: lower tolerance of ambiguity was associated with believing that vaccines should go through a relatively longer vs. shorter testing period (p < 0.001). This association remained significant in the model separating type of uncertainty perception.
Sensitivity analyses: main effects
As noted earlier, in addition to the control condition that served as the analytical sample for the current paper, the parent study included two additional conditions that did not receive a theoretical manipulation of uncertainty: these conditions read the same basic information about the nature and prevention of the COVID-19 pandemic as those in the control condition (with no language explicitly discussing uncertainty), plus additional content that promoted either prosociality or hope. Given that these conditions did not receive an explicit manipulation of uncertainty, we conducted a sensitivity analysis in this larger subsample (N = 901; n = 303 in control condition, n = 301 hope promoting condition, n = 297 in prosocial condition), while statistically adjusting for experimental condition, to evaluate the robustness of our findings.
We began by examining whether the independent variables of interest differed across these three study conditions. Even though uncertainty was not explicitly manipulated in the three study conditions of interest, we found that perceptions of uncertainty about COVID-19 were lower in the no uncertainty + prosocial condition compared to the other two conditions: F(2, 898) = 2.93, p = 0.054, Mdiff hope promoting vs. prosocial = 0.18, p = 0.04, Mdiff control vs. prosocial = 0.20, p = 0.03. Individual differences in tolerance of uncertainty did not differ by condition (all p’s < 0.52).
The results of the sensitivity analyses in the larger subgroup of participants largely confirmed the above results from analyses of the non-uncertainty + control group. All significant relationships in the main study sample remained significant in the larger sample. The analyses in the larger sample also identified significant effects not observed in the smaller sample. Specifically, uncertainty perceptions and tolerance of complexity were both positively associated with trust in information, and tolerance for ambiguity was negatively associated with vaccine intentions in the larger sample for the analyses that did not separate type of uncertainty perception. In the analyses that separated type of uncertainty perception, perceived uncertainty due to ambiguity was negatively associated with trust, perceived uncertainty due to complexity was significantly positively associated with trust, and perceived uncertainty due to complexity was significantly positively associated with intentions (see Supplemental Tables 1 and 2).
Interactions between perceptions and tolerance of uncertainty
To test our hypothesis that the potential effects of uncertainty perceptions would be moderated by individuals’ trait-level tolerance of different types of uncertainty, we conducted three multiple regression models for each outcome that included a term for the two-way interaction between general uncertainty perceptions and each type of uncertainty tolerance. We included only the general measure of perceived uncertainty in the interactions for two reasons: (1) at the level of main effects, general uncertainty perceptions performed similarly compared to breaking this construct out by subtype—i.e., neither general uncertainty perceptions nor uncertainty perception subtypes were significantly associated with outcomes, and (2) probing interactions between all uncertainty perception subtypes and uncertainty tolerance subtypes would have involved a multiplicative increase in the number of statistical tests conducted, for which the study lacked power. Predictors were mean-centered.
We observed significant interactions between uncertainty perceptions and tolerance, but only for trust in information.1 Tolerance of risk significantly moderated the effect of uncertainty perceptions on trust in information (b = 0.196, 95% CI [0.068, 0.032], p = 0.003, partial η2 = 0.03), such that the negative relationship between perceived uncertainty and trust in information about COVID-19 was stronger for individuals with lower tolerance of risk (see Fig. 2a). Specifically, in simple slopes analysis, we found that the relationship between uncertainty perceptions and trust was not significantly different from zero for individuals with mean levels of risk tolerance (b = 0.04, p = 0.53); the simple slope for uncertainty perceptions was negative, but not significantly different from zero for individuals with risk tolerance one standard deviation below the mean (b = − 0.15, p = 0.10); finally, the simple slope for uncertainty perceptions was negative and significantly different from zero for individuals with risk tolerance two standard deviations below the mean (b = − 0.33, p = 0.02). The proportion of variance in trust explained by all the uncertainty-related predictors, including the interaction between perceived uncertainty and tolerance of risk, in this model was 0.04.
Fig. 2.
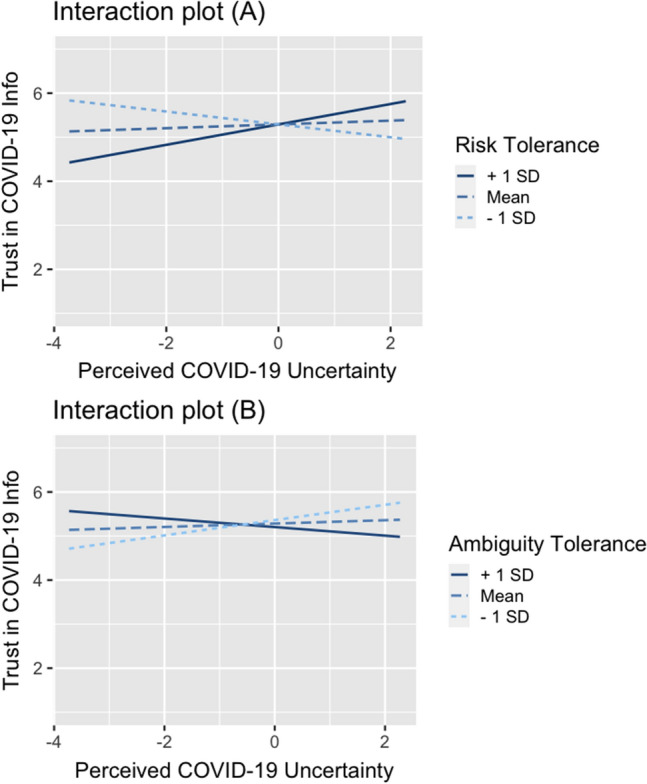
Interactions between general COVID-19 uncertainty perceptions and tolerance of risk (A) and tolerance of ambiguity (B) on trust
Tolerance of ambiguity also moderated the relationship between uncertainty perceptions and trust in information, b = − 0.142, 95% CI [− 0.252, − 0.031], p = 0.012, partial η2 = 0.02, such that greater perceived uncertainty was associated with higher trust for individuals with higher tolerance of ambiguity (less ambiguity aversion) (see Fig. 2b). Specifically, simple slopes analysis demonstrated that the relationship between uncertainty perceptions and trust was not significantly different from zero for individuals with mean levels of ambiguity aversion (b = 0.04, p = 0.57), and the simple slopes for uncertainty perceptions were negative, but not significantly different from zero for individuals with ambiguity aversion one (b = − 0.10, p = 0.25) and two (b = − 0.23, p = 0.06) standard deviations above the mean; finally, individuals with ambiguity aversion scores one (b = 0.17, p = 0.05) and two (b = 0.31, p = 0.02) standard deviations below the mean had significant, positive simple slopes for uncertainty perceptions and trust. The proportion of variance explained by all the uncertainty-related predictors, including the interaction between perceived uncertainty and tolerance of risk, in this model was 0.03.
Sensitivity analyses: interactions
In sensitivity analyses conducted with the larger sample, the significant interactions between uncertainty perceptions and risk tolerance (b = 0.16, 95% CI [0.94, 0.088], p < 0.001) and uncertainty perceptions and tolerance of ambiguity (b = − 0.07, 95% CI [− 0.138, − 0.001], p = 0.046) were also present. Sensitivity analyses in the larger sample also demonstrated significant interactions between uncertainty perceptions and risk tolerance on vaccine intentions, such that uncertainty perceptions were more negatively associated with vaccine intentions among individuals with lower risk tolerance, b = 0.137, 95% CI [0.031, 0.244], p = 0.012. Additionally, tolerance of complexity moderated the effect of uncertainty perceptions on vaccine testing beliefs, such that perceived uncertainty was more positively associated with preferences for vaccine delay among individuals with lower tolerance of complexity (b = 0.123, 95% CI [0.006, 0.239], p = 0.039).
Discussion
Scientific uncertainty about COVID-19 is prevalent, but the extent to which public perceptions of scientific uncertainty may explain variability in important pandemic control behaviors and their antecedents has not been previously investigated. In this study, we sought to examine the relationship between perceptions of scientific uncertainty about COVID-19, trait-level individual differences in uncertainty tolerance (and interactions between these two factors), and trust in COVID-19 information and COVID-19 vaccine hesitancy. We found that, on average, uncertainty perceptions about COVID-19 were not independently associated with trust in information or vaccine hesitancy. This was true when considering perceived uncertainty broadly, as well as when considering perceptions of specific types of uncertainty (i.e., indeterminacy, ambiguity, or complexity). However, consistent with hypotheses, we found that individual trait-level differences in tolerance of uncertainty were associated with vaccine hesitancy—though these associations differed depending on the type of uncertainty tolerance. Specifically, higher tolerance of risk and lower tolerance of ambiguity were both associated with lower vaccine intentions. Lower tolerance of ambiguity was also associated with stronger preferences for delaying vaccination. These findings are consistent with previous work demonstrating negative relationships between uncertainty tolerance and health cognition-related outcomes (Han et al., 2014; Strout et al., 2018), and supports the importance of considering the type of uncertainty tolerance, as different forms of uncertainty tolerance can have different effects (Han et al., 2015).
The fact that we observed associations in the opposite directions for tolerance of risk and tolerance of ambiguity on vaccine intentions was unexpected. It is possible that individuals with high risk tolerance may be predisposed to focus on the risk posed by COVID-19 itself (as opposed to risk related to vaccines); these individuals may thus have been less interested in vaccination because of their willingness to accept the risk posed by COVID-19. On the other hand, individuals with lower tolerance of ambiguity had lower vaccine intentions, suggesting that among these individuals, aversion to ambiguity may have been directed toward ambiguities about the vaccine, rather than aspects of COVID-19 itself. Notably, we also did not observe significant associations between either uncertainty perceptions or tolerance of uncertainty and trust in information (i.e., when not considering interactive effects between these factors). The reasons for these null findings are not clear; they may reflect either methodological shortcomings of our study (e.g., measurement error, limited power to detect associations) or the influence of unmeasured variables that may moderate or mediate the relationship between uncertainty perceptions, tolerance, and outcomes. Examples include personality traits (e.g., dispositional optimism and hope), perceptions of the effectiveness of alternative risk-reducing behaviors, and past experiences with illness and health care. Notably, however, our findings are consistent with recent work from van der Bles and colleagues (2020), which found minor or null relationships between uncertainty and trust in science. Together, these findings may offer some reassurance to public health officials and policymakers that communicating scientific uncertainty may not diminish public trust—at least at a broad, population level.
Although we did not observe significant associations between either uncertainty perceptions or tolerance of uncertainty and trust in COVID-19 information, we did find that the association between uncertainty perceptions and trust was moderated by uncertainty tolerance. Consistent with hypotheses, we found that perceived uncertainty about COVID-19 had a stronger negative association with trust in information among participants having a lower tolerance of risk and ambiguity. These findings relate to previous work showing that individual differences in uncertainty tolerance may modify relationships between uncertainty perceptions and relevant outcomes in health contexts (Anderson et al., 2020). In this case, our findings suggest that individual differences in tolerance of uncertainty may be an important determinant of the effects of scientific uncertainty on public trust in the science, and may explain the inconsistent or null findings of past work. Notably, we did not observe similar moderating effects for the vaccine hesitancy outcomes. Although the cross-sectional nature of our study restricts causal inferences, it is conceivable that although perceptions of scientific uncertainty about the COVID-19 pandemic may not lead to lower trust in public health information or vaccine hesitancy for all individuals, perceived uncertainty may reduce trust (i.e., an element of hesitancy) particularly for individuals who are especially averse to uncertainty. If these findings are confirmed, they may help future inform public health communication or other interventions to increase COVID-19 vaccination uptake.
We acknowledge several important limitations of the current study. Above all, the cross-sectional design of the study limits causal claims about the observed associations. We therefore cannot rule out alternative causal explanations; for example, it is conceivable that vaccine-hesitant individuals may endorse higher tolerance of risk and lower tolerance of ambiguity as a means of rationalizing their opposition to vaccination (manifesting motivated reasoning). We believe this explanation is less likely, given that uncertainty tolerance is thought to be a stable trait-level characteristic; however, further experimental and longitudinal studies are needed to establish the causal directions of the associations between these variables. Our post hoc power analysis indicated that the subsample of participants that was used in the primary analyses for the current paper was also likely insufficient for testing main/interaction effects with small effect sizes—thus, some of the null effects we observed may have resulted from a lack of statistical power to observe significant associations. Additionally, since we conducted multiple statistical tests (the independent and interactive effects of multiple independent variables on three separate dependent variables), we cannot rule out Type I errors; our findings thus need to be replicated in larger studies. Furthermore, perceived uncertainty was queried with regard to the COVID-19 pandemic more broadly, rather than about COVID-19 vaccination itself, and trust in information was queried regarding the message participants read for the study specifically (e.g., rather than trust in public health experts or scientists more broadly). Although we believe that the current measures were reasonable proxies for the constructs they represent, it is possible that our pattern of results would have differed had these items been alternatively worded. Similarly, responses to the question on preferences for vaccine delay may have been biased by the response anchor, “definitely release the vaccines as soon as possible,” which may have implied to participants that no testing would be completed. Finally, the study was conducted in June 2020—before vaccines or treatments had been released to the public. The subsequent evolution of social norms and mandates for various COVID-19 preventive behaviors, as well as other systemic factors influencing vaccination behavior, may reduce to some degree the generalizability of our findings to present circumstances.
These limitations are offset by a number of strengths. The overall study sample was sociodemographically diverse, enhancing the external validity of our findings. Additionally, although our primary analytic sample was relatively small, the sensitivity analysis conducted in a larger subset of our sample confirmed all of the associations observed in the smaller sample, supporting the robustness of our findings.
To summarize, we explored whether and how both perceptions of uncertainty about COVID-19 and individual, trait-level differences in uncertainty tolerance might affect trust in public health information and vaccine hesitancy—two important outcomes in efforts to control the COVID pandemic. We found that overall perceptions of uncertainty about COVID-19 were not related to trust or vaccine hesitancy, but that uncertainty is linked to lower trust among individuals who are less tolerant of uncertainty. Additionally, individual differences in tolerance of uncertainty were associated with vaccine hesitancy in nuanced ways. These results suggest that uncertainty tolerance might play a critical role in moderating the public’s responses to scientific uncertainty about COVID-19, and endorse the value of further research to better understand its mechanisms. Our findings also suggest the need to better account for trait-level differences in uncertainty tolerance among individuals in the design of public health interventions and communication strategies aimed at promoting vaccination uptake and other risk-reducing measures for COVID-19 and other public health threats.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix A: COVID-19 information provided to participants in analytic sample (n = 303)
2019 Novel Coronavirus (COVID-19)
This survey is about the 2019 Novel Coronavirus (COVID-19) outbreak, or pandemic—a public health crisis that has affected the whole world and every state in the US. The survey begins with some information about COVID-19. Please take your time and read this information carefully. The survey will then ask you about your attitudes and opinions regarding the COVID-19 pandemic.
Spread and Symptoms of COVID-19
COVID-19 is a respiratory illness caused by a coronavirus, a type of virus that infects human beings. It is extremely contagious and spreads from person to person through contact with respiratory secretions from an infected person (e.g., through sneezing and coughing). Anybody can get COVID-19, and nobody is risk-free.
Illness caused by COVID-19 can range from mild to severe. Some people can be infected and have no symptoms at all. More commonly, people with COVID-19 have cough and difficulty breathing, or at least two of these other symptoms: fever, chills, repeated shaking with chills, muscle pain, headache, sore throat, or new loss of taste or smell. Some people have serious illness which can include pneumonia, kidney failure, and death. People who are older and who have other medical problems are at higher risk of dying from COVID-19.
Prevention and Treatment of COVID-19
Currently, there is no vaccine that can prevent COVID-19 infection. The only way to prevent COVID-19 and to control the pandemic is to keep it from spreading. Current recommendations include the following:
Practice good hygiene, including handwashing and use of hand sanitizers
Practice social distancing (putting space between you and other people)
Wear a mask
Self-isolation and self-quarantine: stay home and avoid contact with other people if you’re sick with COVID-19, or have symptoms of it (Self-isolation), or if you may have been exposed to someone with COVID-19 (Self-quarantine)
In addition to these measures, state and local governments in the US have enacted strict sheltering-in-place regulations, travel bans, and “lock-downs” of businesses and schools, in order to limit the spread of the coronavirus.
Currently, there is no effective, widely available treatment that can cure COVID-19 infection. Most people recover at home, without treatment. Some people need to be hospitalized, and require oxygen or breathing machines (mechanical ventilation) to help them recover. But there is no cure for COVID-19 and some people, especially those who are older and who have other medical problems, do not recover.
Appendix B: Perceived uncertainty measure
Items are rated on a scale from 1 (Strongly Disagree) to 7 (Strongly Agree).
Whether or not the COVID-19 pandemic can be controlled is mostly a matter of chance.
There are conflicting recommendations about how to control the COVID-19 pandemic.
Controlling the COVID-19 pandemic is really complicated.
How long the COVID-19 pandemic will last is mostly a matter of chance.
There are conflicting estimates of how long the COVID-19 pandemic will last.
Predicting how long the COVID-19 pandemic will last is really complicated.
Scoring:
Perceived uncertainty (general) mean of items 1–6.
Perceived indeterminacy subscale mean of items 1 & 4.
Perceived ambiguity subscale mean of items 2 & 5.
Perceived complexity subscale mean of items 3 & 6.
Author contributions
Conceptualization: ASG, PKJH, LS, PEB. Data curation: LS, ASG. Formal analysis: ASG. Funding acquisition, PKJH. Investigation: PKJH, LS. Methodology: ASG, PKJH, LS, PEB, WMPK, RAF. Project administration: PKJH, LS. Resources: PH. Software: n/a. Supervision: PKJH, WMPK, RAF. Validation: ASG. Visualization: ASG. Writing – original draft: ASG. Writing – review and editing: ASG, PKJH, LS, PEB, WMPK, RAF.
Funding
This work was supported by a Pilot Project Program Award to Paul Han from the Northern New England Clinical & Translational Research Network (1U54GM115516-01). The funding agreement ensured the authors’ independence in designing the study, interpreting the data, and in writing and publishing the report.
Data availability
Data and reproducible code can be found at https://osf.io/m5nye/?view_only=9ee8d045678c4164a305c1e347d7c6c1.
Code availability
Data and reproducible code can be found at https://osf.io/m5nye/?view_only=9ee8d045678c4164a305c1e347d7c6c1.
Declarations
Conflict of interest
The authors have no conflicts to declare.
Consent to participate
Informed consent was collected online from all participants.
Ethics approval
This study was approved by the MaineHealth Institutional Review Board.
Human and animal rights and Informed Consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Footnotes
Test statistics for nonsignificant interaction effects: for vaccine intentions, risk tolerance and perceived uncertainty interaction b = 0.084, 95% CI [− 0.106, 0.274], p = .385, tolerance of ambiguity and perceived uncertainty interaction b = 0.039, 95% CI [− 0.124, 0.202], p = .639, and tolerance of complexity and perceived uncertainty interaction b = 0.076, 95% CI [− 0.104, 0.255], p = .408. For vaccine testing beliefs, risk tolerance and perceived uncertainty interaction b = 0.023, 95% CI [− 0.181, 0.226], p = .827, tolerance of ambiguity and perceived uncertainty interaction b = − 0.122, 95% CI [− 0.297, 0.052], p = .568, and tolerance of complexity and perceived uncertainty interaction b = 0.094, 95% CI [− 0.098, 0.286], p = .337. For trust, tolerance of complexity and perceived uncertainty interaction b = 0.006, 95% CI [− 0.117, 0.129], p = .923.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ajzen, I., & Madden, T. (1986). Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology. Retrieved from /citations?view_op=view_citation&continue=/scholar%3Fhl%3Den%26start%3D40%26as_sdt%3D0,6%26scilib%3D1&citilm=1&citation_for_view=IGoukmgAAAAJ:M05iB0D1s5AC&hl=en&oi=p
- Anderson, E. C., Hinton, A., Lary, C. W., Strout, T., Antov, A., Edelman, E., Helbig, P., Reed, K., Rueter, J., Han, P. K. J. (2020). The influence of uncertainty and uncertainty tolerance on attitudes and self-efficacy about genomic tumor testing. Https://Doi.Org/10.1080/13548506.2020.1764989. http://doi.org/10.1080/13548506.2020.1764989 [DOI] [PubMed]
- Bammer, G., & Smithson, M. (2012). The nature of uncertainty. In G. Bammer & M. Smothson (Eds.), Uncertainty and risk (pp. 307–322). Routledge.
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics. 2006;117:1532–1541. doi: 10.1542/PEDS.2005-1728. [DOI] [PubMed] [Google Scholar]
- Blaisdell LL, Gutheil C, Hootsmans NAM, Han PKJ. Unknown risks: Parental hesitation about vaccination. Medical Decision Making. 2016;36:479–489. doi: 10.1177/0272989X15607855. [DOI] [PubMed] [Google Scholar]
- Ellsberg D. Risk, ambiguity, and the Savage axioms. The Quarterly Journal of Economics. 1961;75(4):643–669. doi: 10.2307/1884324. [DOI] [Google Scholar]
- Fahlquist JN. Vaccine hesitancy and trust. Ethical Aspects of Risk Communication. 2017;46:182–188. doi: 10.1177/1403494817727162. [DOI] [PubMed] [Google Scholar]
- Geller G, Faden RR, Levine DM. Tolerance for ambiguity among medical students: Implications for their selection, training and practice. Social Science & Medicine. 1990;31:619–624. doi: 10.1016/0277-9536(90)90098-D. [DOI] [PubMed] [Google Scholar]
- Gustafson A, Rice RE. A review of the effects of uncertainty in public science communication. Public Understanding of Science. 2020;29(6):614–633. doi: 10.1177/0963662520942122. [DOI] [PubMed] [Google Scholar]
- Han, P. K. J., Williams, A. E., Haskins, A., Gutheil, C., Lucas, F. L., Klein, W. M. P., & Mazor, K. M. (2014). Individual differences in aversion to ambiguity regarding medical tests and treatments: association with cancer screening cognitions. Cancer Epidemiology, Biomarkers & Prevention : A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 23(12), 2916. http://doi.org/10.1158/1055-9965.EPI-14-0872 [DOI] [PMC free article] [PubMed]
- Han PKJ, Klein WMP, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Medical Decision Making. 2011;31:828–838. doi: 10.1177/0272989X10393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: relationship to perceptions of cancer preventability, risk, and worry. Journal of Health Communication. 2006;11:51–69. doi: 10.1080/10810730600637541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Reeve BB, Moser RP, Klein WMP. Aversion to ambiguity regarding medical tests and treatments: Measurement, prevalence, and relationship to sociodemographic factors. Journal of Health Communication. 2009;14:556–572. doi: 10.1080/10810730903089630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Scharnetzki E, Scherer AM, Thorpe A, Lary C, Waterston LB, Fagerlin A, Dieckmann NF. communicating scientific uncertainty about the COVID-19 pandemic: Online experimental study of an uncertainty-normalizing strategy. Journal of Medical Internet Research. 2021;23:e27832. doi: 10.2196/27832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Schupack D, Daggett S, Holt CT, Strout TD. Temporal changes in tolerance of uncertainty among medical students: insights from an exploratory study. Medical education online. 2015 doi: 10.3402/MEO.V20.28285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han PKJ, Zikmund-Fisher BJ, Duarte CW, Knaus M, Black A, Scherer AM, Fagerlin A. Communication of scientific uncertainty about a novel pandemic health threat: Ambiguity aversion and its mechanisms. Journal of Health Communication. 2018;23(5):435–444. doi: 10.1080/10810730.2018.1461961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillen MA, Gutheil CM, Strout TD, Smets EMA, Han PKJ. Tolerance of uncertainty: Conceptual analysis, integrative model, and implications for healthcare. Social Science & Medicine. 2017;180:62–75. doi: 10.1016/J.SOCSCIMED.2017.03.024. [DOI] [PubMed] [Google Scholar]
- Hornsey MJ, Lobera J, Díaz-Catalán C. Vaccine hesitancy is strongly associated with distrust of conventional medicine, and only weakly associated with trust in alternative medicine. Social Science & Medicine. 2020;255:113019. doi: 10.1016/J.SOCSCIMED.2020.113019. [DOI] [PubMed] [Google Scholar]
- Jensen JD, Hurley RJ. Conflicting stories about public scientific controversies: Effects of news convergence and divergence on scientists’ credibility. Social Science & Medicine. 2012;21(6):689–704. doi: 10.1177/0963662510387759. [DOI] [PubMed] [Google Scholar]
- Kishishita D, Tung H, Wang C. Ambiguity and self-protection: Evidence from social distancing under the COVID-19 pandemic. SSRN Electronic Journal. 2021 doi: 10.2139/SSRN.3778645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson HJ. Vaccine trust and the limits of information. Science. 2016;353(6305):1207–1208. doi: 10.1126/science.aah6190. [DOI] [PubMed] [Google Scholar]
- Lin D, Friedman DB, Qiao S, Tam CC, Li X, Li X. Information uncertainty: a correlate for acute stress disorder during the COVID-19 outbreak in China. BMC Public Health. 2020;20(1):1–9. doi: 10.1186/S12889-020-09952-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. Journal of Clinical Epidemiology. 1996;49(6):697–703. doi: 10.1016/0895-4356(96)00007-8. [DOI] [PubMed] [Google Scholar]
- Nagler RH. Adverse outcomes associated with media exposure to contradictory nutrition messages. Journal of Health Communication. 2014;19(1):24–40. doi: 10.1080/10810730.2013.798384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagler RH, Vogel RI, Gollust SE, Rothman AJ, Fowler EF, Yzer MC. Public perceptions of conflicting information surrounding COVID-19: Results from a nationally representative survey of U.S adults. PLOS ONE. 2020;15(10):e0240776. doi: 10.1371/JOURNAL.PONE.0240776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson SD, Goldman L, Orav EJ, Guadagnoli E, Garcia TB, Johnson PA, Lee TH. Triage decisions for emergency department patients with chest pain. Journal of General Internal Medicine. 1995;10(10):557–564. doi: 10.1007/BF02640365. [DOI] [PubMed] [Google Scholar]
- Petrocchi S, Iannello P, Ongaro G, Antonietti A, Pravettoni G. The interplay between risk and protective factors during the initial height of the COVID-19 crisis in Italy: The role of risk aversion and intolerance of ambiguity on distress. Current Psychology. 2021;2021:1–12. doi: 10.1007/S12144-021-01601-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritov I, Baron J. Reluctance to vaccinate: Omission bias and ambiguity. Journal of Behavioral Decision Making. 1990;3(4):263–277. doi: 10.1002/bdm.3960030404. [DOI] [Google Scholar]
- Roets A, Van Hiel A. Separating ability from need: Clarifying the dimensional structure of the need for closure scale. Personality and Social Psychology Bulletin. 2007;33(2):266–280. doi: 10.1177/0146167206294744. [DOI] [PubMed] [Google Scholar]
- Schernhammer E, Weitzer J, Laubichler MD, Birmann BM, Bertau M, Zenk L, Caniglia G, Jäger CC, Steiner G. Correlates of COVID-19 vaccine hesitancy in Austria: Trust and the government. Journal of Public Health (Oxford, England) 2021 doi: 10.1093/PUBMED/FDAB122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strout TD, Hillen M, Gutheil C, Anderson E, Hutchinson R, Ward H, Kay H, Mills GJ, Han PKJ. Tolerance of uncertainty: A systematic review of health and healthcare-related outcomes. Patient Education and Counseling. 2018;101(9):1518–1537. doi: 10.1016/J.PEC.2018.03.030. [DOI] [PubMed] [Google Scholar]
- Taber JM, Klein WMP, Ferrer RA, Han PKJ, Lewis KL, Biesecker LG, Biesecker BB. Perceived ambiguity as a barrier to intentions to learn genome sequencing results. Journal of Behavioral Medicine. 2015;38(5):715–726. doi: 10.1007/s10865-015-9642-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Bles AM, van der Linden S, Freeman ALJ, Spiegelhalter DJ. The effects of communicating uncertainty on public trust in facts and numbers. Proceedings of the National Academy of Sciences. 2020;117(14):7672–7683. doi: 10.1073/PNAS.1913678117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper M, Nápoles AM, Pérez-Stable EJ. No populations left behind: Vaccine hesitancy and equitable diffusion of effective COVID-19 vaccines. Journal of General Internal Medicine. 2021;36(7):2130–2133. doi: 10.1007/s11606-021-06698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin. 2006;132(2):249. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Webster DM, Kruglanski AW. Individual differences in need for cognitive closure. Journal of Personality and Social Psychology. 1994;67(6):1049. doi: 10.1037/0022-3514.67.6.1049. [DOI] [PubMed] [Google Scholar]
- Wright RN, Faul L, Graner JL, Stewart GW, LaBar KS. Psychosocial determinants of anxiety about the COVID-19 pandemic. Journal of Health Psychology. 2021 doi: 10.1177/13591053211030981. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data and reproducible code can be found at https://osf.io/m5nye/?view_only=9ee8d045678c4164a305c1e347d7c6c1.
Data and reproducible code can be found at https://osf.io/m5nye/?view_only=9ee8d045678c4164a305c1e347d7c6c1.