Abstract
As the coronavirus disease 2019 (COVID-19) spreads globally, people are at risk of developing disinhibited eating behaviors. This study aimed to examine whether perceived mortality threat and negative affect mediate the relationship between trait self-control and disinhibited eating during the pandemic. A longitudinal survey was administered to a sample of college students (N = 634) before the outbreak (September 2019, T1), during the mid-term (February 2020, T2), and in the later stage of the pandemic (April 2020, T3). Self-report measures of trait self-control (T1), perceived mortality threat (T2, T3), negative affect (T2, T3), and disinhibited eating (T2, T3) were successively completed. Trait self-control was found to be negatively associated with negative affect, perceived mortality threat, and disinhibited eating during the mid-term and later stage of the pandemic. Disinhibited eating was positively associated with negative affect and perceived mortality threat. The longitudinal mediation results demonstrated that trait self-control (T1) could negatively predict disinhibited eating (T3) through negative affect (T2) rather than through perceived mortality threat. These findings suggest that trait self-control is of great importance in regulating psychological discomfort and disinhibited eating during stressful periods and that negative affect might be the main psychological mechanism underlying the relationship between self-control ability and disinhibited eating.
Keywords: COVID-19 pandemic, Trait self-control, Disinhibited eating, Negative affect, Perceived mortality threat, Young adult
1. Introduction
In December 2019, a novel coronavirus, later named COVID-19, was detected in the city of Wuhan, China. Owing to its high infectivity, COVID-19 quickly spread across the globe, causing an outbreak of acute pneumonia (Bao, Sun, Meng, Shi, & Lu, 2020). A recent survey of COVID-19 involving 11,479 people from 31 provinces and autonomous regions in China demonstrated that most people showed anxiety (66.9%), worry (71.7%), and fear (58.2%), whereas only 3%–4% did not display any of these discomforts. In addition, research indicates that people are at risk of developing disinhibited eating behaviors during the COVID-19 pandemic (Rodgers et al., 2020).
Disinhibited eating refers to a range of eating behaviors (e.g., binge eating, uncontrolled eating, and emotional eating) that involve a lack of restraint over food intake (Shomaker, Tanofsky-Kraff, & Yanovski, 2011), which can result in obesity and obesity-related diseases (Goldschmidt et al., 2015; Tanofsky-Kraff et al., 2009). Studies have found that the deficiency of self-control capacity plays an important role in disinhibited eating (Byrne et al., 2021; Kelly et al., 2020). Thus, the present study primarily aimed to investigate whether and how trait self-control (TSC) was associated with disinhibited eating propensity in the context of the COVID-19 pandemic.
1.1. TSC and disinhibited eating
As the core component of self-regulation, self-control is defined as the ability to override and alter one's prepotent response and promote desirable long-term goals (Baumeister, Vohs, & Tice, 2007; Hofmann, Baumeister, Forster, & Vohs, 2012), which is closely associated with disinhibited eating. Specifically, research based on children and adolescents has shown that individuals with higher impulsivity/poorer executive function are more likely to show uncontrolled eating, emotional eating, and binge eating (Ames et al., 2014; Byrne et al., 2021; Calvo, Galioto, Gunstad, & Spitznagel, 2014; Reinblatt et al., 2015). Neuroimaging evidence also indicates that obese adolescents with executive dysfunction are associated with high rating of uncontrolled eating (Maayan, Hoogendoorn, Sweat, & Convit, 2011; Shapiro et al., 2019). In addition, longitudinal studies also reveal that a high level of TSC can predict a successful weight management (Crescioni et al., 2011; Tsukayama, Toomey, Faith, & Duckworth, 2010). Therefore, we assumed that TSC might be negatively associated with disinhibited eating during the pandemic.
1.2. Perceived mortality threat and disinhibited eating
Studies have indicated that salient threats to an individual's mortality are associated with both risk aversion and risk inclination (Miller & Mulligan, 2002; Taubman – Ben-Ari & Skvirsky, 2019). The terror management health model posits that an awareness of mortality could instigate health-oriented responses aimed at removing death-related thoughts (Courtney, Goldenberg, & Boyd, 2020; Goldenberg & Arndt, 2008). Some studies support this assumption and show that people become motivated to avoid such thoughts by engaging in health-promoting behaviors, such as fitness (Arndt, Schimel, & Goldenberg, 2003; Bevan, Maxfield, & Bultmann, 2014). However, the research also shows that individuals under the initiation of mortality threats are likely to begin implementing a quick life history strategy (Ellis, Figueredo, Brumbach, & Schlomer, 2009), such as exhibiting impulsive behaviors and pursuing immediate rewards (Griskevicius, Delton, Robertson, & Tybur, 2011). Specifically, individuals perceiving higher life stress were more likely to show disinhibited eating (O'Neill, Kamper-DeMarco, Chen, & Orom, 2020). Luo, Niu, and Chen (2020) recently reported that perceived mortality threat could expand the effect of environmental unpredictability on disinhibited eating. Consequently, we assumed that perceived mortality threat caused by the COVID-19 pandemic might be positively associated with disinhibited eating.
1.3. Negative affect and disinhibited eating
Negative emotions or difficulties with emotional regulation have been found to be a risk factor for various forms of disinhibited eating in clinical, restrained, and healthy populations (Berg et al., 2014; Byrne et al., 2020; Haedt-Matt & Keel, 2011; Stice, 2001, 2002). According to the affect theory, negative affect drives the onset of disinhibited eating episodes as a maladaptive attempt to reduce uncomfortable emotions (Heatherton & Baumeister, 1991; Macht, 2008). Specifically, studies have shown that negative affects have been strongly associated with uncontrolled eating (Byrne et al., 2020; Haedt-Matt & Keel, 2011; Heron, Scott, Sliwinski, & Smyth, 2014). In addition, difficulties in regulating negative emotions can predict binge eating (Goldschmidt, Aspen, Sinton, Tanofsky-Kraff, & Wilfley, 2008; Whiteside et al., 2007), as well as the future onset of eating disorder symptoms (Michopoulos et al., 2015; Stice, 2002; Vannucci et al., 2015). Because disinhibited eating is often attributed to experiencing negative emotions, we assumed that negative affect might be positively associated with disinhibited eating during the pandemic.
1.4. The mediating role of perceived mortality threat and negative affect
According to the general reaction of people under the pandemic, this study aimed to investigate whether perceived death threat and negative affect mediate the relationship between TSC and disinhibited eating. According to the dual-system model, self-control ability is recognized as the result of competition between the impulse system and the reflective system (Hofmann, Friese, & Strack, 2009). The impulse system is easily triggered by automatic and affective stimuli, while the reflective system can inhibit impulses and facilitate deliberative processing (Knoch & Fehr, 2010). For individuals with high TSC, the stronger reflective system could enable them be rational and reduce automatic and affective interference, even in threatening situation. For instance, Gailliot, Schmeichel, and Baumeister (2006) found that participants with high (vs. low) level of self-control reported fewer death-related thoughts while being primed with death. Studies have also shown that individuals possessing high TSC can avoid intrusive and distracting thoughts that affects their pursuit of goals, focus on meaningful activities (Bertrams, Baumeister, & Englert, 2016; Massar, Bělostíková, & Sui, 2020), and think rationally when problem-solving and decision-making (Ballard et al., 2017; Peters & Desposito, 2016). On the other hand, people with high TSC tend to adopt effective emotion regulation (Paschke et al., 2016) and experience less negative and more positive affects (Hofmann, Luhmann, Fisher, Vohs, & Baumeister, 2014; Li, Xiang, Song, Huang, Chen, 2021; Wiese et al., 2017). Based on the existing empirical and theoretical evidence, possessing high TSC is associated with better psychological adjustment, which may alleviate disinhibited eating in the pandemic. Therefore, we assumed that high TSC could predict lower disinhibited eating during the pandemic by regulating adverse thoughts and negative affect.
1.5. Research aims and hypotheses
Three follow-up surveys were conducted over eight months (before the outbreak, September 2019, T1; during the middle stage, February 2020, T2; and during the later stage, April 2020, T3) to investigate whether TSC (T1) could be associated with an disinhibited eating (T3) during the COVID-19 pandemic and reveal the longitudinal mediating effect of perceived mortality threat (T2) and negative affect (T2) in this link. We initially proposed that TSC was negatively associated with perceived mortality threat, negative affect, and disinhibited eating and that perceived mortality threat and negative affect were positively correlated with disinhibited eating (H1); that perceived mortality threat would mediate the relationship between TSC and disinhibited eating (H2); and that TSC also would be negatively associated with disinhibited eating through negative affect (H3).
2. Methods
2.1. Participants and procedure
The data were derived from the Behavioral-Brain Research Project which is designed to investigate the neural basis of personality in young Chinese adults. This project used a random method to recruit college students from various departments of a university in Chongqing, China. The first wave (T1, September 2019) obtained personality-related data (e.g., TSC) for 901 college students; the second wave (T2, February 2020) obtained data (e.g., negative affect, perceived death threat, and disinhibited eating) by following up with 765 of the initial 901 students; and the third wave (T3, April 2020) obtained data (e.g., negative affect, perceived death threat, and disinhibited eating) by following up with 634 students who completed three collections and entered into the analysis (age ranged from 17 to 20 years, M = 18.75, SD = 1.56; female: N = 443; male: N = 191). From T1 to T3, the effective recovery rate was 70.37%. To examine whether these cases were missing randomly or missing completely randomly, Little’ s missing completely at random (MCAR) test was used to examine missing data mechanisms and determine whether the data was MCAR. The MCAR test was no significant (χ2 (6) = 3.86, p > .05) and indicated that the data were missing completely randomly (Enders, 2010; Little, 1988). The full information maximum likelihood method was used to address missing data and generate unbiased and effective parameter estimates. Ethical approval for this study was granted by the Ethics Committee of the University.
2.2. Measurements
TSC was measured with a brief and well-validated Chinese version of the Self-Control Scale containing 19 items (Tan & Guo, 2008; Tangney, Baumeister, & Boone, 2004). The participants responded to a five-point Likert scale (e.g., “I am good at resisting temptation”) ranging from 1 (not at all) to 5 (very much) to indicate their general self-control capacities. Higher scores on this scale indicated greater self-control capacity. The reliability of TSC was 0.87 in the current sample.
Disinhibited eating was measured with the uncontrolled eating questionnaire, a sub-dimension of the Three Factor Eating Questionnaire-R18 (TFEQ-R18, Anglé et al., 2009), and refers to the tendency to eat with the feeling of being out of control (e.g., “I get so hungry that my stomach often seems like a bottomless pit”). The participants were asked to respond to nine items of uncontrolled eating on a four-point scale (1 = not at all, 4 = very much), with a high score indicating a high tendency to engage in disinhibited eating. In the present study, the Cronbach's alpha values of disinhibited eating in T2 and T3 were 0.91 and 0.92, respectively.
Perceived mortality threat was measured with four items (“How much do you feel that the environment has become unsafe?“) on a seven-point Likert-type scale (1 = not at all, 7 = strongly feel) (Wang & Chen, 2016). Higher scores on this scale indicated greater perceptions of a threat to mortality. The overall Cronbach's alpha of perceived mortality threat in T2 and T3 were 0.93 and 0.94, respectively.
Negative affect was measured using the 10 negative affect items (e.g., distressed) from the Positive and Negative Affect Schedule (PANAS, Watson, Clark, & Tellegen, 1988). The participants indicated the extent to which they were currently feeling each emotion on a five-point Likert-type scale ranging from 1 (very slightly) to 5 (extremely). The Cronbach's alpha of negative affect in T2 and T3 were 0.91 and 0.92, respectively.
2.3. Statistical analysis
This study conducted descriptive statistics and bivariate correlations with SPSS 22.0. Subsequently, longitudinal path analysis controlling for stability in the constructs over time were computed to evaluate the main study hypotheses using the M-plus 7.0. The path analysis including TSC (T1) before the pandemic, and perceived mortality threat, negative affect, and disinhibited eating in the middle and later stage of the pandemic (T2, T3), with sex, age, and BMI as the controlling variables. In addition to calculating the cross-sectional correlations between the study variables, the analysis also include stability for perceived mortality threat, negative affect, and disinhibited eating from T2 to T3 (i.e., auto-regressive path) and structural paths for them (i.e., cross-lagged path). The measurement model fit was evaluated based on the chi-square, comparative fit index (CFI), root–mean–square error of approximation (RMSEA), and standardized root–mean–square residual (SRMR). The following criteria were used to indicate the goodness of fit: CFI ≥0.90, and RMSEA ≤0.10, and SRMR ≤0.10 (Hu & Bentler, 1999). To examined the longitudinal mediation model by assessing the indirect effect of TSC on disinhibited eating through negative affect and perceived mortality threat. To this end, TSC before the pandemic (T1) was considered the independent variable (X); perceived mortality threat and negative affect in the middle stage of the pandemic (T2) were considered the mediator variable (M); and disinhibited eating in the later stages (T3) was considered the dependent variable (Y). The mediating effect was tested by a bootstrapping analysis with 5000 iterations using the M-plus 7.0.
3. Results
3.1. Descriptive statistics
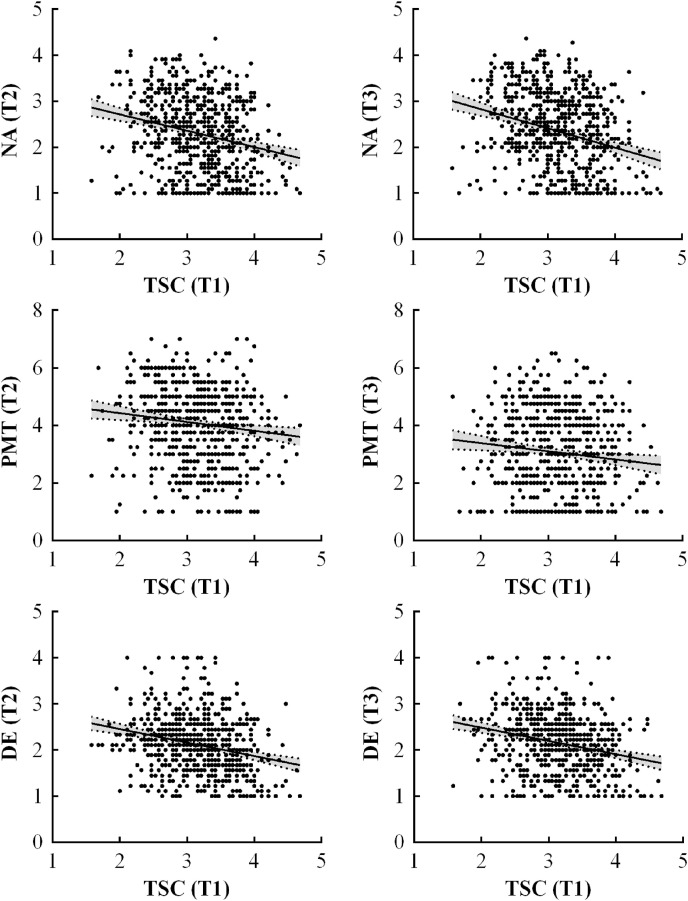
The kurtosis and skewness values of all variables were between −1 and +1, indicating that the data had a normal distribution. Table 1 and Fig. 1 present the results of the descriptive analysis. The correlation results showed that TSC (T1) was significantly and negatively related to negative affect (T2, T3), perceived mortality threat (T2, T3), and disinhibited eating (T2, T3). Negative affect and perceived mortality threat were found to be significantly and positively correlated with disinhibited eating. Negative affect was significantly and positively associated with perceived mortality threat. Bonferroni correction was used to control for multiple-comparisons. The relation among all the variables supported the testing of subsequent hypotheses.
Table 1.
Correlations, means, and standard deviations among variables.
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| 1 TSC(T1) | 3.15 | 0.54 | – | ||||||
| 2 NA(T2) | 2.28 | 0.79 | −0.24** | – | |||||
| 3 NA(T3) | 2.35 | 0.83 | −0.28** | 0.54** | – | ||||
| 4 PMT(T2) | 4.07 | 1.32 | −0.13** | 0.48** | 0.20** | – | |||
| 5 PMT(T3) | 3.06 | 1.38 | −0.11** | 0.39** | 0.46** | 0.33** | – | ||
| 6 DE(T2) | 2.12 | 0.63 | −0.25** | 0.35** | 0.25** | 0.21** | 0.16** | – | |
| 7 DE(T3) | 2.15 | 0.64 | −0.24** | 0.26** | 0.30** | 0.11** | 0.22** | 0.60** | – |
Note:M = means. SD = standard deviations; TSC = trait self-control; NA = negative affect; PMT = perceived mortality threat; DE = disinhibited eating; T1 = the first time (September 2019, before the outbreak). T2 = the second time (February 2020, the middle stage). T3 = the third time (April 2020, the later stage). **p < .01.
Fig. 1.
Scatter figures of the associations of TSC with negative affect, perceived mortality threat, and disinhibited eating.
3.2. Testing for the proposed model
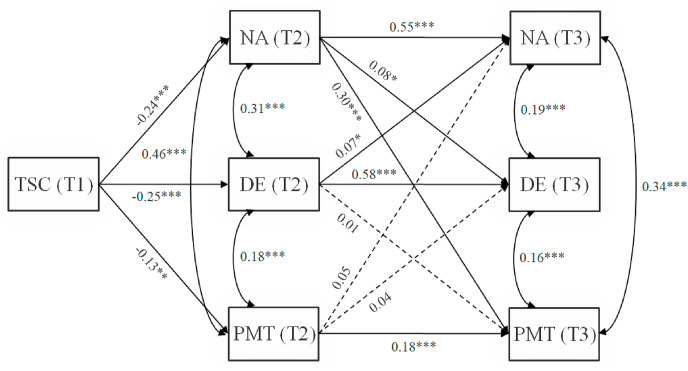
The model fit the data adequately, χ2 (24) = 90.42, p < .001; CFI = 0.97; RMSEA = 0.07, 90%confidence interval [CI: 0.05, 0.08]; SRMR = 0.06. As portrayed in Fig. 2 , all autoregressive paths in the model were positive and significant. In terms of hypothesized relations among the constructs, TSC (T1) could predict negative affect, perceived mortality threat, and disinhibited eating during the middle stage (T2) of the pandemic. Negative affect (T2) could predict perceived mortality threat and disinhibited eating during the later stage (T3) of the pandemic. However, the path from perceived mortality threat (T2) to negative affect or disinhibited eating (T3) was not significant. In addition, disinhibited eating (T2) did not predict perceived mortality threat (T3), but the path from disinhibited eating (T2) to negative affect (T3) was positive and significant.
Fig. 2.
The model with standardized estimates. Solid lines are significant, dashed lines are not significant. TSC = trait self-control, NA = negative affect, PMT = perceived mortality threat, DE = disinhibited eating. T1 = the first time (September 2019, before the outbreak). T2 = the second time (February 2020, the middle stage). T3 = the third time (April 2020, the later stage).
With TSC (T1) as the independent variable and disinhibited eating (T3) as the dependent variable, the mediation model was established to examine the mediating effect of perceived mortality threat (T2) and negative affect (T2). As predicted, a significant direct path existed from TSC to disinhibited eating through negative affect (indirect effect = −0.02, 95% CI [-0.05, −0.003]) rather than through perceived mortality threat (indirect effect coefficient = 0.003, SE = 0.006, 95% CI = [-0.007, 0.02]).
4. Discussion
This study conducted a longitudinal survey (over eight months across different stages of the COVID-19 pandemic) in a sample of college students to investigate the association of TSC with disinhibited eating and explore the mediating effect of perceived mortality threat and negative affect in this link. The correlation results verified H1 and revealed that TSC before the outbreak (September 2019, T1) was negatively associated with negative affect, perceived mortality threat, and disinhibited eating in the middle (February 2020, T2) and later (April 2020, T3) stages. These findings concur with previous studies that showed that possessing high TSC is positively associated with the ability to regulate negative emotion and adverse cognition (Bertrams et al., 2016; Hofmann et al., 2014; Gailliot et al., 2006; Massar et al., 2020; Wiese et al., 2017). Furthermore, individuals with high self-control capacity are associated with less disinhibited eating behaviors including uncontrolled eating, emotional eating, and binge eating (Ames et al., 2014; Byrne et al., 2021; Calvo et al., 2014; Reinblatt et al., 2015) as well as more likely to success in weight management (Crescioni et al., 2011; Tsukayama et al., 2010). The findings corroborate the existing studies, suggest that TSC is of great importance in regulating psychological discomfort and disinhibited eating during stressful events.
Notably, the present study fills the gap concerning the potential mechanisms underlying the relationship between TSC and disinhibited eating. In line with the existing studies indicating that negative emotions and difficulties in regulating negative emotions are key factors for disinhibited eating (Berg et al., 2014; Byrne et al., 2020; Haedt-Matt & Keel, 2011; Stice, 2001, 2002), our results supported H3 rather than H2, demonstrating that TSC could indirectly predicted disinhibited eating through negative affect rather than through perceived mortality threat. The relationship between mortality threats and impulsive behavior has been found to be controversial (Miller & Mulligan, 2002; Taubman – Ben-Ari & Skvirsky, 2019). It suggests that there might be critical mechanism that account for the relationship between threat of mortality and disinhibited eating. Unexpectedly, the results showed that disinhibited eating also could predict negative affect. The reciprocal relationship indicated that individuals’ disinhibited eating in the pandemic could aggravate their negative emotional experience. In summary, our findings suggest that negative affect might be the main psychological mechanism underlying the relationship TSC and disinhibited eating during stressful events and contribute to a deeper understanding of the relationship among these factors.
According to the strength model, engaging in tasks or activities that demand self-control will consume limited self-control resources and impair subsequent activities (Baumeister et al., 2007). Individuals under the pandemic have to regulate the frequent pessimistic thoughts and negative affect triggered by the COVID-19, which would deplete their limited self-control resources. Prior studies indicated that a relative lack of self-regulatory resources, combined with a high tendency to regulate negative affect, were associated with an unfavorable dietary pattern (Sproesser, Strohbach, Schupp, & Renner, 2011). Compared to individuals with high TSC, those with low TSC were in a state of inadequate self-control and hardly realized the persistent regulation of negative affect during the pandemic, thereby exhibiting disinhibited eating. Furthermore, studies have shown that individuals with high self-control show experience less conflict for undesired foods than their low self-control counterparts (Gillebaart, Schneider, & De Ridder, 2016). For the group with high self-control, perceiving less conflict and temptation means a lower depletion of self-control resources; therefore, individuals with high TSC can cope with negative affect adequately, maintaining a healthy eating pattern during the pandemic.
Some limitations of this study should be noted. First, the sample group was limited to the college students; accordingly, it is unclear whether these findings can be generalized to other groups. Because the pandemic's influence may vary among different populations, future research should assess the influence of TSC in various samples across different ages and careers. Second, the measurement limitations herein included the use of brief self-report measures to assess eating- and affect-related constructs. Behavioral indicators with ecological validity, such as third-party reports, changes in weight, and experience sampling methods should be considered in future studies. Furthermore, disinhibited eating was employed from one dimension of three disordered eating, which may not capture all the dietary characteristics during the pandemic. Finally, because the timing of the assessments in the study were unevenly distributed and did not include all the variable data, we could not strictly determine the direction of causality regarding the associations among these variables. Recent studies suggest that conflict experience and behavior habits may be instrumental in the positive outcomes of TSC. Further investigations should explore the effects of conflict experience and healthy habits in the links between TSC and eating behavior.
Existing studies has indicated that practicing small acts of self-control can increase self-control capacity (Friese, Frankenbach, Job, & Loschelder, 2017; Muraven, 2010). Upon encountering temptations and impulses, adopting abstract thinking or a third-person perspective can improve one's self-control ability during decision-making (Basso et al., 2018; Chiou, Wu, & Chang, 2013). The strength model of self-control also assumes that self-control ability, similar to a muscle, can be improved through regular behavior training (Baumeister et al., 2007). Moreover, studies have shown that the inhibition of spontaneous dominant responses, such as avoiding colloquialisms while speaking and using one's non-dominant hand (Finkel, Dewall, Slotter, Oaten, & Foshee, 2009; Miles et al., 2016), has been confirmed to improve participants' self-control ability. Future research can be conducted online or offline to investigate the effects of cognitive strategies and behavioral trainings targeted at strengthening self-control capacity on mental and behavioral health during stressful events. Furthermore, our findings will be instructive for some restricted diet groups and self-control interventions could improve their health goals and quality of life.
This study conducted a longitudinal survey to investigate the relationship between TSC and disinhibited eating during different periods of the COVID-19 pandemic. The findings suggest that disinhibited eating is associated with perceived mortality threat and negative affect. Moreover, self-control capacity negatively indirectly predicted the level of disinhibited eating in the pandemic through negative affect rather than through perceived mortality threat. Given the well-documented positive outcomes associated with TSC, self-regulation and control training aimed at improving individuals’ self-control ability should be implemented to minimize future health-related concerns—even during stressful events.
Author contributions
Qingqing Li: Conceptualization, Data Curation, Methodology, Formal analysis, Writing – original draft, Writing-Review & Editing; Guangcan Xiang: Visualization, Methodology, Formal analysis, Writing – original draft; Shiqing Song and Xiaobao Li: Data Curation, Methodology, Formal analysis; Yong Liu and Yanli Wang: Methodology, Formal analysis; Yijun Luo and Mingyue Xiao: Software, Investigation, Resources; Hong Chen: Conceptualization, Supervision, Project administration, Funding acquisition, Writing – review & editing.
Funding sources
This study was funded by National Natural Science Foundation of China (No. 31771237); the Fundamental Research Funds for the Central Universities (No. SWU1709106).
Data availability statement
Data can be found from DOI: 10.13140/RG.2.2.29987.68647.
Ethics approval statement
The findings reported have not been previously published and that the manuscript is not being simultaneously submitted elsewhere and is not under consideration by another journal. All co-authors have approved the manuscript and agree with submission to Appetite.
Declarations of interest
None.
Acknowledgements
None.
References
- Ames S.L., Kisbu-Sakarya Y., Reynolds K.D., Boyle S., Cappelli C., Cox M.G.…Stacy A.W. Inhibitory control effects in adolescent binge eating and consumption of sugar-sweetened beverages and snacks. Appetite. 2014;81:180–192. doi: 10.1016/j.appet.2014.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglé S., Engblom J., Eriksson T., Kautiainen S., Saha M.-T., Lindfors P.…Rimpelä A. Three factor eating questionnaire-R18 as a measure of cognitive restraint, uncontrolled eating and emotional eating in a sample of young Finnish females. International Journal of Behavioral Nutrition and Physical Activity. 2009;6(1):41. doi: 10.1186/1479-5868-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arndt J., Schimel J., Goldenberg J.L. Death can Be good for your health: Fitness intentions as a proximal and distal defense against mortality salience. Journal of Applied Social Psychology. 2003;33(8):1726–1746. doi: 10.1111/j.1559-1816.2003.tb01972.x. [DOI] [Google Scholar]
- Ballard I.C., Kim B., Liatsis A., Aydogan G., Cohen J.D., Mcclure S.M. More is meaningful: The magnitude effect in intertemporal choice depends on self-control. Psychological Science. 2017 doi: 10.1177/0956797617711455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: Address mental health care to empower society. The Lancet. 2020;395(10224) doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basso F., Petit O., Bellu S.L., Lahlou S., Cancel A., Anton J. Taste at first (person) sight: Visual perspective modulates brain activity implicitly associated with viewing unhealthy but not healthy foods. Appetite. 2018;128:242–254. doi: 10.1016/j.appet.2018.06.009. [DOI] [PubMed] [Google Scholar]
- Baumeister R.F., Vohs K.D., Tice D.M. The strength model of self-control. Current Directions in Psychological Science. 2007;16(6):351–355. doi: 10.1111/j.1467-8721.2007.00534.x. [DOI] [Google Scholar]
- Berg K.C., Peterson C.B., Crosby R.D., Cao L., Crow S.J., Engel S.G., et al. Relationship between daily affect and overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Psychiatry Research. 2014;215(1):185–191. doi: 10.1016/j.psychres.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrams A., Baumeister R.F., Englert C. Higher self-control capacity predicts lower anxiety-impaired cognition during math examinations. Frontiers in Psychology. 2016;7:485. doi: 10.3389/fpsyg.2016.00485. 485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan A.L., Maxfield M., Bultmann M.N. The effects of age and death awareness on intentions for healthy behaviours. Psychology and Health. 2014;29(4):405–421. doi: 10.1080/08870446.2013.859258. [DOI] [PubMed] [Google Scholar]
- Byrne M.E., Shomaker L.B., Brady S.M., Kozlosky M., Yanovski J.A., Tanofsky-Kraff M. Associations between latent trait negative affect and patterns of food-intake among girls with loss-of-control eating. International Journal of Eating Disorders. 2020;53(4):618–624. doi: 10.1002/eat.23253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne M.E., Tanofsky-Kraff M., Lavender J.M., Parker M.N., Shank L.M., Swanson T.N.…Yanovski J.A. Bridging executive function and disinhibited eating among youth: A network analysis. International Journal of Eating Disorders. 2021;54(5):721–732. doi: 10.1002/eat.23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvo D., Galioto R., Gunstad J., Spitznagel M.B. Uncontrolled eating is associated with reduced executive functioning. Clinical Obesity. 2014;4(3):172–179. doi: 10.1111/cob.12058. [DOI] [PubMed] [Google Scholar]
- Chiou W., Wu W., Chang M. Think abstractly, smoke less: A brief construal-level intervention can promote self-control, leading to reduced cigarette consumption among current smokers. Addiction. 2013;108(5):985–992. doi: 10.1111/add.12100. [DOI] [PubMed] [Google Scholar]
- Courtney E.P., Goldenberg J.L., Boyd P. The contagion of mortality: A terror management health model for pandemics. British Journal of Social Psychology. 2020;59:607–617. doi: 10.1111/bjso.12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crescioni A.W., Ehrlinger J., Alquist J.L., Conlon K.E., Baumeister R.F., Schatschneider C., et al. High trait self-control predicts positive health behaviors and success in weight loss. Journal of Health Psychology. 2011;16(5):750–759. doi: 10.1177/1359105310390247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis B.J., Figueredo A.J., Brumbach B.H., Schlomer G.L. Fundamental dimensions of environmental risk : The impact of harsh versus unpredictable environments on the evolution and development of life history strategies. Human Nature. 2009;20(2):204–268. doi: 10.1007/s12110-009-9063-7. [DOI] [PubMed] [Google Scholar]
- Enders C.K. Guilford Press; New York, NY: 2010. Applied missing data analysis. [Google Scholar]
- Finkel E.J., Dewall C.N., Slotter E.B., Oaten M.J., Foshee V.A. Self-regulatory failure and intimate partner violence perpetration. Journal of Personality and Social Psychology. 2009;97(3):483–499. doi: 10.1037/a0015433. [DOI] [PubMed] [Google Scholar]
- Friese M., Frankenbach J., Job V., Loschelder D.D. Does self-control training improve self-control? A meta-analysis. Perspectives on Psychological Science. 2017;174569161769707 doi: 10.1177/1745691617697076. [DOI] [PubMed] [Google Scholar]
- Gailliot M.T., Schmeichel B.J., Baumeister R.F. Self-regulatory processes defend against the threat of death: Effect of self-control depletion and trait self-control on thoughts and fears of dying. Journal of Personality and Social Psychology. 2006;91(1):49–62. doi: 10.1037/0022-3514.91.1.49. [DOI] [PubMed] [Google Scholar]
- Gillebaart M., Schneider I.K., De Ridder D.T.D. Effects of trait self-control on response conflict about healthy and unhealthy food. Journal of Personality. 2016;84(6):789–798. doi: 10.1111/jopy.12219. [DOI] [PubMed] [Google Scholar]
- Goldenberg J.L., Arndt J. The implications of death for health: A terror management health model for behavioral health promotion. Psychological Review. 2008;115(4):1032–1053. doi: 10.1037/a0013326. [DOI] [PubMed] [Google Scholar]
- Goldschmidt A.B., Aspen V.P., Sinton M.M., Tanofsky-Kraff M., Wilfley D.E. Disordered eating attitudes and behaviors in overweight youth. Obesity. 2008;16(2):257–264. doi: 10.1038/oby.2007.48. [DOI] [PubMed] [Google Scholar]
- Goldschmidt A.B., Loth K., Maclehose R.F., Pisetsky E.M., Berge J.M., Neumarksztainer D. Overeating with and without loss of control: Associations with weight status, weight‐related characteristics, and psychosocial health. International Journal of Eating Disorders. 2015;48(8):1150–1157. doi: 10.1002/eat.22465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griskevicius V., Delton A.W., Robertson T.E., Tybur J.M. Environmental contingency in life history strategies: The influence of mortality and socioeconomic status on reproductive timing. Journal of Personality and Social Psychology. 2011;100(2):241–254. doi: 10.1037/a0021082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haedt-Matt A.A., Keel P.K. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137(4):660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton T.F., Baumeister R.F. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Heron K.E., Scott S.B., Sliwinski M.J., Smyth J.M. Eating behaviors and negative affect in college women's everyday lives. International Journal of Eating Disorders. 2014;47(8):853–859. doi: 10.1002/eat.22292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann W., Baumeister R.F., Forster G., Vohs K.D. Everyday temptations: An experience sampling study of desire, conflict, and self-control. Journal of Personality and Social Psychology. 2012;102(6):1318–1335. doi: 10.1037/a0026545. [DOI] [PubMed] [Google Scholar]
- Hofmann W., Friese M., Strack F. Impulse and self-control from a dual-systems perspective. Perspectives on Psychological Science. 2009;4(2):162–176. doi: 10.1111/j.1745-6924.2009.01116.x. [DOI] [PubMed] [Google Scholar]
- Hofmann W., Luhmann M., Fisher R.R., Vohs K.D., Baumeister R.F. Yes, but are they happy? Effects of trait self-control on affective well-being and life satisfaction. Journal of Personality. 2014;82(4):265–277. doi: 10.1111/jopy.12050. [DOI] [PubMed] [Google Scholar]
- Hu L.T., Bentler P.M. Cutoff criteria for ft indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Kelly N.R., Jaramillo M., Ramirez S., Altman D.R., Rubin S.G., Yang S.B.…Yanovski J.A. Executive functioning and disinhibited eating in children and adolescents. Pediatric obesity. 2020;15(6) doi: 10.1111/ijpo.12614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoch D., Fehr E. Resisting the power of temptations: The right prefrontal cortex and self-control. Annals of the New York Academy of Sciences. 2010;1104(1):123–134. doi: 10.1196/annals.1390.004. [DOI] [PubMed] [Google Scholar]
- Little R.J. A test of missing completely at random for multivariatedata with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. doi: 10.1080/01621459.1988.10478722. [DOI] [Google Scholar]
- Li Q.Q., Xiang G.C., Song S.Q., Xiao M.Y., Chen H. Trait self-control mediates the association between resting-state neural correlates and emotional well-being in late adolescence. Social Cognitive and Affective Neuroscience. 2021;16(6):632–641. doi: 10.1093/scan/nsab046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y.J., Niu G.F., Chen H. Early life environmental unpredictability and overeating: Life history theory-based research. Acta Psychology Sinica. 2020;52(10):1224–1236. doi: 10.3724/SP.J.1041.2020.01224. [DOI] [Google Scholar]
- Maayan L., Hoogendoorn C., Sweat V., Convit A. Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity. 2011;19(7):1382–1387. doi: 10.1038/oby.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macht M. How emotions affect eating: A five-way model. Appetite. 2008;50(1):1–11. doi: 10.1016/j.appet.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Massar K., Bělostíková P., Sui X. It's the thought that counts: Trait self-control is positively associated with well-being and coping via thought control ability. Current Psychology. 2020 doi: 10.1007/s12144-020-00746-9. Online. [DOI] [Google Scholar]
- Michopoulos V., Powers A., Moore C.J., Villarreal S., Ressler K.J., Bradley B. The mediating role of emotion dysregulation and depression on the relationship between childhood trauma exposure and emotional eating. Appetite. 2015;91:129–136. doi: 10.1016/j.appet.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles E., Sheeran P., Baird H.M., Macdonald I.A., Webb T.L., Harris P.R. Does self-control improve with practice? Evidence from a six-week training program. Journal of Experimental Psychology: General. 2016;145(8):1075–1091. doi: 10.1037/xge0000185. [DOI] [PubMed] [Google Scholar]
- Miller R.L., Mulligan R.D. Terror management: The effects of mortality salience and locus of control on risk-taking behaviors. Personality and Individual Differences. 2002;33(7):1203–1214. doi: 10.1016/S0191-8869(02)00009-0. [DOI] [Google Scholar]
- Muraven M. Building self-control strength: Practicing self-control leads to improved self-control performance. Journal of Experimental Social Psychology. 2010;46(2):465–468. doi: 10.1016/j.jesp.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill J., Kamper-DeMarco K., Chen X., Orom H. Too stressed to self-regulate? Associations between stress, self-reported executive function, disinhibited eating, and BMI in women. Eating Behaviors. 2020;39:101417. doi: 10.1016/j.eatbeh.2020.101417. [DOI] [PubMed] [Google Scholar]
- Paschke L.M., Denise D., Rosa S., Ima T., Amadeus M., Ludwig V.U.…Henrik W. Individual differences in self-reported self-control predict successful emotion regulation. Social Cognitive and Affective Neuroscience. 2016;8:1193–1204. doi: 10.1093/scan/nsw036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters J., Desposito M. Effects of medial orbitofrontal cortex lesions on self-control in intertemporal choice. Current Biology. 2016;26(19):2625–2628. doi: 10.1016/j.cub.2016.07.035. [DOI] [PubMed] [Google Scholar]
- Reinblatt S.P., Mahone E.M., Tanofsky-Kraff M., Lee-Winn A.E., Yenokyan G., Leoutsakos J.-M.S.…Riddle M.A. Pediatric loss of control eating syndrome: Association with attention-deficit/hyperactivity disorder and impulsivity. The International Journal of Jating Disorders. 2015;48(6):580–588. doi: 10.1002/eat.22404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers R.F., Lombardo C., Cerolini S., Franko D.L., Omori M., Fuller-Tyszkiewicz M.…Guillaume S. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders. 2020;53(7):1166–1170. doi: 10.1002/eat.23318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro A.L.B., Johnson S.L., Sutton B., Legget K.T., Dabelea D., Tregellas J.R. Eating in the absence of hunger in young children is related to brain reward network hyperactivity and reduced functional connectivity in executive control networks. Pediatric obesity. 2019;14(6) doi: 10.1111/ijpo.12502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shomaker L.B., Tanofsky-Kraff M., Yanovski J.A. In: Handbook of behavior, food and nutrition. Preedy V., Watson R., Martin C., editors. Springer; New York, NY: 2011. Disinhibited eating and body weight in youth. [DOI] [Google Scholar]
- Sproesser G., Strohbach S., Schupp H.T., Renner B. Candy or apple? How self-control resources and motives impact dietary healthiness in women. Appetite. 2011;56(3):784–787. doi: 10.1016/j.appet.2011.01.028. [DOI] [PubMed] [Google Scholar]
- Stice E. In: Eating disorders: Innovative directions in research and practice. Striegel-Moore R.H., Smolak L., editors. American Psychological Association; Washington, DC, US: 2001. Risk factors for eating pathology: Recent advances and future directions; pp. 51–73. [DOI] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Tangney J.P., Baumeister R.F., Boone A.L. High self‐control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality. 2004;72(2):271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Tan S., Guo Y. Revision of self-control scale for Chinese college students. Chinese Journal of Clinical Psychology. 2008;5:468–470. CNKI:SUN:ZLCY.0.2008-05-010. [Google Scholar]
- Tanofsky-Kraff M., Yanovski S.Z., Schvey N.A., Olsen C.H., Gustafson J., Yanovski J.A. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. International Journal of Eating Disorders. 2009;42(1):26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taubman – Ben-Ari O., Skvirsky V. In: Handbook of terror management theory. Routledge C., Vess M., editors. Academic Press; 2019. The terror management underpinnings of risky behavior; pp. 559–576. [Google Scholar]
- Tsukayama E., Toomey S.L., Faith M.S., Duckworth A.L. Self-control as a protective factor Against overweight status in the transition from childhood to adolescence. JAMA Pediatrics. 2010;164(7):631–635. doi: 10.1001/archpediatrics.2010.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannucci A., Nelson E.E., Bongiorno D.M., Pine D.S., Yanovski J.A., Tanofskykraff M. Behavioral and neurodevelopmental precursors to binge-type eating disorders: Support for the role of negative valence systems. Psychological Medicine. 2015;45(14):2921–2936. doi: 10.1017/S003329171500104X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Chen B.B. The influence of childhood stress and mortality threat on mating standards. Acta Psychology Sinica. 2016;48(7):857–866. doi: 10.3724/SP.J.1041.2016.00857. [DOI] [Google Scholar]
- Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Whiteside U., Chen E.Y., Neighbors C., Hunter D., Lo T.T.Y., Larimer M.E. Difficulties regulating emotions: Do binge eaters have fewer strategies to modulate and tolerate negative affect? Eating Behaviors. 2007;8(2):162–169. doi: 10.1016/j.eatbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Wiese C.W., Tay L., Duckworth A.L., Dmello S.K., Kuykendall L., Hofmann W.…Vohs K.D. Too much of a good thing? Exploring the inverted-U relationship between self-control and happiness. Journal of Personality. 2017;86(3):380–396. doi: 10.1111/jopy.12322. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be found from DOI: 10.13140/RG.2.2.29987.68647.