Abstract
Purpose
The Liver Disease and Reproductive Ageing (LIVRA) study leverages the infrastructure of the decades-long multicentre prospective Women’s Interagency HIV Study (WIHS) to examine the contributions of HIV, hepatitis C virus (HCV) and ageing to liver disease progression in women.
Participants
From 2013 to 2018, LIVRA enrolled 1576 participants (77 HCV-seropositive only, 248 HIV/HCV-seropositive, 868 HIV-seropositive only and 383 HIV/HCV-seronegative) who underwent vibration controlled transient elastography (VCTE). A VCTE quality assurance programme was established to ensure consistency and accuracy for longitudinal assessment of steatosis (fatty liver) via the controlled attenuation parameter (CAP) and fibrosis via liver stiffness (LS). Demographic, lifestyle factors, anthropometry, clinical and medication history, host genetics, immune markers and hormone levels were collected as part of the WIHS.
Findings to date
At baseline, 737 of 1543 women with CAP measurements had steatosis (CAP ≥248 dB/m) and 375 of 1576 women with LS measurements had significant fibrosis (LS ≥7.1 kPa), yielding a prevalence of 48% and 24%, respectively. On multivariable analysis, waist circumference (WC) and insulin resistance were independently associated with higher CAP (17.8 dB/m per 10 cm (95% CI:16.2 to 19.5) and 1.2 dB/m per doubling (95% CI:0.8 to 1.6), respectively). By contrast, HIV/HCV seropositivity and HCV seropositivity alone were associated with less steatosis compared with HIV/HCV-seronegative women, although the latter did not reach statistical significance (−9.2 dB/m (95% CI:–18.2 to –0.3) and −10.4 dB/m (95% CI: −23.8 to 3.1), respectively). Factors independently associated with higher LS were age (4.4% per 10 years (95% CI: 0.4% to 8.4%)), WC (5.0% per 10 cm (95% CI: 3.3% to 6.6%)), CAP steatosis (0.6% per 10 dB/m (95% CI: 0.1% to 1.0%)), HIV/HCV seropositivity (33% (95% CI: 24% to 44%)) and HCV seropositivity alone (43% (95% CI: 28% to 60%)). Excluding scans that were invalid based on traditional criteria for unreliability did not affect the results.
Future plans
Enrolled women undergo VCTE at 3-year intervals unless LS is ≥9.5 kPa, indicating advanced fibrosis, in which case VCTE is performed annually. Participants also undergo VCTE every 6 months until 18 months after HCV treatment initiation. Analysis of the data collected will provide insights into the impact of ageing/ovarian function, host genetics, immune function and contemporary HIV and HCV treatments on liver disease progression.
Keywords: hepatology, infectious diseases, HIV & AIDS
Strengths and limitations of this study.
The Liver Disease and Reproductive Ageing (LIVRA) study is designed to examine the contributions of HIV, hepatitis C virus, ageing and ovarian function, immune function, host genomics and contemporary antiviral treatments on hepatic steatosis (or fatty liver) and fibrosis progression measured via longitudinal vibration controlled transient elastography (VCTE).
The study leverages the infrastructure of the decades-long multicentre prospective Women’s Interagency HIV Study (WIHS), which collects biological specimens, sociodemographic data, lifestyle (substance use, food insecurity and physical activity) factors, anthropometry, clinical and medication history, host genetics, immune markers and hormone levels.
A rigorous VCTE quality assurance programme was developed to ensure consistency and accuracy of hepatic steatosis and fibrosis assessments.
Although limited to women, the LIVRA VCTE protocol is currently being implemented in men enrolled into the newly integrated Multicenter AIDS Cohort Study (MACS)-WIHS Combined Cohort Study.
The LIVRA study will allow investigation into the natural history of and potentially modifiable risk factors for hepatic steatosis and fibrosis in women with and without HIV.
Introduction
Liver disease is a leading cause of morbidity and mortality among persons living with HIV (PLWH).1 However, the determinants of hepatic steatosis (fatty liver) and fibrosis progression among women living with HIV in the modern era of HIV and hepatitis C virus (HCV) treatment are not well known. Seminal fatty liver disease cohort studies have excluded PLWH and those with cleared HCV,2 3 and studies of hepatic steatosis in PLWH are often small in sample size. Moreover, the vast majority of studies of hepatic steatosis among PLWH have been conducted in men even though women represent over 50% of all PLWH worldwide4 and close to 25% of all PLWH in the USA.5
In HIV-seronegative populations, women have a lower overall risk of steatosis than men but a higher risk of advanced fibrosis once steatosis is established, particularly after age 50 years.6 Understanding the factors associated with steatosis and its impact on fibrosis among women in general, and especially in those living with HIV, is of essential importance. The Liver Disease and Reproductive Ageing (LIVRA) study was designed as an ancillary study of the Women’s Interagency HIV Study (WIHS) to evaluate the contributions of HIV, HCV and reproductive ageing to steatosis and fibrosis progression as measured by longitudinal vibration controlled transient elastography (VCTE) among a large cohort of women living with or without HIV.
Cohort description
Study population and design
The WIHS (now part of the MACS-WIHS Combined Cohort Study7 (MWCCS)) was a multicentre prospective cohort study established to investigate the course of HIV and associated conditions among women living with and without HIV. The WIHS enrolled 4982 women (3678 living with HIV infection and 1304 living without HIV infection) during four recruitment waves: 1994–1995, 2001–2002, 2011–2012 and 2013–2015 from 10 US cities (Bronx and Brooklyn, New York; Chicago, Illinois; San Francisco, California; Los Angeles, California; Washington District of Columbia; Atlanta, Georgia; Chapel Hill, North Carolina; Miami, Florida; Jackson, Mississippi and Birmingham, Alabama). Full details of recruitment, retention and demographics have been published previously.8 Eligibility criteria varied with each wave of enrolment mainly to recruit women with earlier HIV disease stage and who had never taken older antiretroviral drugs associated with increased metabolic perturbations during later waves (ie, didanosine and stavudine). Eligible women had documentation of reactive anti-HIV serology and if positive, a confirmatory test or if they were HIV-seronegative had risk factor(s) for HIV exposure. Baseline sociodemographic characteristics and HIV risk factors were similar between HIV-seropositive and HIV-seronegative women. At semi-annual research visits, participants completed a physical examination, provided biological specimens (eg, serum, plasma, peripheral blood mononuclear cells, urine) and completed interviewer-administered questionnaires to obtain information regarding sociodemographics, lifestyle data (eg, substance use, food security, physical activity) and clinical, psychosocial and medication history. Host genetic data and genome-wide association studies are also available in the WIHS, as are markers of immune activation and inflammation and hormone levels.
From December 2013 to December 2018, 1576 of the approximately 2100 active WIHS women were enrolled into the LIVRA ancillary study. Eligibility included age 35–60 years old for women without chronic HCV. All women with chronic HCV infection were eligible for enrolment, regardless of age, as long as they were not currently receiving anti-HCV therapy. Women with positive hepatitis B surface antigen, haemochromatosis, autoimmune hepatitis or primary biliary cholangitis were excluded, as were women who reported using medications associated with steatosis (ie, systemic corticosteroids, amiodarone, methotrexate), signs of decompensated cirrhosis, current cancer or severe renal insufficiency. Women who were pregnant or had an implantable cardiac device were excluded per the VCTE manufacturer (Fibroscan; Echosens, Paris, France).
As part of the study protocol, longitudinal VCTE examinations are performed at 3-year intervals after their baseline measurement unless liver stiffness (LS) values are ≥9.5 kPa, consistent with advanced fibrosis, in which case VCTE are performed annually. Additionally, participants who report HCV treatment after enrolment undergo VCTE every 6 months until 18 months after HCV treatment initiation.
VCTE performance and quality assurance
VCTE reliability is operator-dependent,9 and therefore proper operator training and experience is important, especially in multicentre studies involving multiple operators. VCTE operators at each site were first trained by Echosens to: (1) operate the device, (2) obtain at least 10 measurements that the device deemed as valid per scan and (3) recognise images that the device deemed valid but required manual adjustment of probe placement by the operator due to interference from vessel, breathing or lung, and not being completely in the liver (eg, probe placed too low or needing to switch to the XL probe due to subcutaneous fat interference). Operators at each WIHS site were then certified by Echosens after demonstrating proficiency in scanning three to five volunteers.
A quality assurance (QA) programme was implemented which required operators to complete at least 50 additional training examinations on subjects with a wide range of body types and within the age range of eligible participants. This benchmark was selected because a large multicentre study indicated that at least 50 examinations were needed before an operator was considered proficient to consistently acquire valid scans.10 Each of the first 25 examinations was reviewed by the QA team, which comprised two clinicians and an experienced VCTE operator (table 1). On completion of the review, a written report was provided with the additional option of individualised verbal feedback or an in-person hands-on training and observation. A similar procedure was followed for the next 25 examinations. After completion of 50 training examinations, the final report indicated whether: (1) the operator was certified; (2) additional examinations were needed and/or (3) a site visit for in-person training was warranted. Twenty-nine operators submitted a median of 55 scans (IQR 51, 62) for review before being certified. To maintain certification, operators are required to perform at least 20 examinations per year.
Table 1.
LIVRA study QA programme for VCTE operator training certification
| Exams | Guidelines | Training goals |
| 1–25 |
Subjects: varied body types and ages, discrete subjects Parameter goals to work towards: IQR <30% of median, >60% of measurements deemed valid by device REQUIRED: 10 valid measurements obtained per participant |
|
| Scans are reviewed by QA team and operator receives written feedback report. Check-in call and additional in-person training optional. | ||
| 26–50 |
Subjects: varied body types and ages, discrete subjects Parameters: REQUIRED: IQR <30% of median, >60% of measurements deemed valid by device, 10 valid measurements per participant |
|
| Scans are reviewed by QA team and operator receives written feedback report. Additional examinations and site visit may be required prior to certification. | ||
Maintenance certification:
| ||
QA, quality assurance; VCTE, vibration controlled transient elastography.
Assessment of hepatic steatosis and fibrosis
Hepatic steatosis was estimated in dB/m using the VCTE-controlled attenuation parameter (CAP) software and fibrosis was estimated using LS measurements in kPa. Participants were instructed to fast for at least 3 hours prior to VCTE. Operators were instructed to manually switch from the M probe to the XL probe if images suggested subcutaneous fat interference in the measurement range of the probe, that is, >2.5 cm distance from skin to liver capsule.11 All examinations had at least 10 successful measurements. At the time of analyses, examinations were flagged as having abnormal validity if they had an IQR/median LS ratio >30% and/or success rate <60% as per prior published criteria,12 or poor image quality. The QA team manually reviewed scan images and data on all VCTE examinations with LS ≥9.3 kPa, a random selection of 10% of examinations with LS <9.3 kPa and those with CAP <150 dB/m. This latter criterion was established after image review suggested that some scans with very low CAP values, including those with the lower bound CAP value of 100 dB/m, may partly capture data from outside of the liver.
Of the 1576 VCTEs performed, 56 had an IQR/median >30% (3.6%), 129 had a success rate <60% (8.2%) and 49 had poor image quality on review (3.1%). These categories were not mutually exclusive; 193 had at least one of these indices (12%). Due to an early technical error with the VCTE device, CAP values were missing for 33 women. Steatosis was defined by CAP ≥248 dB/m, which was the optimal cut-off for selecting mild or greater steatosis in a meta-analysis including data from 2735 patients with liver biopsies13 and was 83% sensitive and 72% specific in detecting mild or greater steatosis in a subset of our cohort when compared with magnetic resonance spectroscopy-measured liver fat fraction.14 The following fibrosis categories were used: significant fibrosis (LS ≥7.1 kPa), advanced fibrosis (LS ≥9.5 kPa) and cirrhosis (LS ≥12.5 kPa).15
Covariates
Race/Ethnicity was self-reported as white, black or Hispanic (including white and black Hispanic). Menopause stage was determined based on the Stages of Reproductive Ageing Workshop criteria.16 Self-reported alcohol consumption was categorised as: none; light (>0–7 drinks/week); moderate (7–12 drinks/week) or heavy (>12 drinks/week). Additional demographic and behavioural covariates were obtained through self-report. Body mass index was calculated in kg/m2, waist circumference was measured in cm and the homeostatic model assessment of insulin resistance (HOMA-IR) was calculated using 8-hour fasting insulin and glucose values.
HIV and HCV seropositivity were defined by documentation of a reactive HIV enzyme immunoassay and reactive second-generation or third-generation HCV enzyme immunoassay, respectively). At WIHS study entry, women underwent testing for HCV antibody (Ab) with HCV RNA if positive. If negative, HCV Ab testing was repeated at last WIHS study visit. For those who became HCV Ab positive, additional retrospective HCV Ab testing was performed to determine when HCV incidence occurred, and then HCV RNA testing was performed at least 2 years later to determine whether they had spontaneously cleared or had chronic infection. For all chronic infections, HCV RNA testing was performed at later visits to determine which had cleared following treatment. HCV RNA was performed using either the COBAS Amplicor Monitor V.2.0 or the COBAS Taqman assay, as previously described (both from Roche Diagnostics, Branchburg, New Jersey, USA).17 HCV genotyping was conducted on a subset of HCV viraemic women using the NC TRUGENE HCV 5 NC Genotyping Kit (Bayer HealthCare, Tarrytown, New York, USA), as previously described.18
NC Genotyping Kit (Bayer HealthCare, Tarrytown, New York, USA), as previously described.18
Statistical analysis
For the purposes of this analysis, HIV and HCV infection categories were defined by serostatus. We compared participant characteristics by infection category using analysis of variance or Kruskal-Wallis tests for continuous variables and χ2 or Fisher’s exact tests for categorical variables, as appropriate. We used unadjusted and multivariable adjusted linear regression models to examine associations with CAP and LS. LS had a right-skewed distribution and therefore was log-transformed to normalise its distribution, and the regression coefficients and their CIs were exponentiated to calculate percentage differences attributable to each covariate. These analyses were performed for all women with successful VCTEs, and sensitivity analyses were performed excluding the scans with IQR/median >30%, success rate <60%, poor image quality on QA review or any one of these criteria. In linear regression models where there were missing covariate information, we used the full information maximum likelihood approach in the setting of path analysis instead of the multiple imputation approach for its efficiency.19 All analyses were performed using SAS V.9.4 (SAS Institute, Cary, North Carolina, USA).
Baseline characteristics
Among the 1576 WIHS women enrolled in LIVRA, 77 had HCV monoinfection, 248 had HIV/HCV coinfection, 868 had HIV infection alone and 383 had neither infection (table 2). About three-quarters were black, and median age was 51 years (IQR 44, 56), with 31% premenopausal, 13% perimenopausal and 56% postmenopausal. Nearly half reported an annual household income of ≤US$12 000, and one-third of the cohort completed less than a high school education. Most women with HIV were taking antiretroviral therapy (ART) and had undetectable HIV RNA. Among the 325 women with HCV seropositivity, 136 were HCV viraemic at the baseline LIVRA visit (42%), 98 had cleared HCV with treatment (30%) and 91 had cleared HCV spontaneously (28%).
Table 2.
Characteristics of the study population by HIV and HCV antibody status
| Median (IQR) or % | HIV−/HCV+ (n=77) |
HIV+/HCV+ (n=248) |
HIV+/HCV− (n=868) |
HIV−/HCV− (n=383) |
P value |
| Sociodemographic | |||||
| Age (years) | 56 (49, 60) | 56 (53, 60) | 49 (43, 54) | 47 (41, 54) | <0.001 |
| Race/Ethnicity | 0.001 | ||||
| Black | 64% | 67% | 76% | 76% | |
| White | 7% | 15% | 9% | 7% | |
| Hispanic | 22% | 17% | 11% | 12% | |
| Other | 7% | 2% | 4% | 5% | |
| Menopause stage | <0.001 | ||||
| Premenopause | 16% | 7% | 33% | 44% | |
| Perimenopause | 13% | 8% | 14% | 14% | |
| Postmenopause | 71% | 85% | 53% | 43% | |
| Household income (US$) | |||||
| <6000 | 29% | 16% | 12% | 19% | <0.001 |
| 6000–12 000 | 44% | 49% | 35% | 26% | |
| 12 001–36 000 | 7% | 13% | 15% | 13% | |
| >36 000 | 9% | 9% | 17% | 23% | |
| Education | |||||
| Less than high school | 43% | 39% | 31% | 32% | 0.02 |
| High school | 35% | 29% | 34% | 28% | |
| More than high school | 22% | 32% | 35% | 41% | |
| Lifestyle | |||||
| Alcohol use | <0.001 | ||||
| None | 51% | 63% | 51% | 42% | |
| Light | 27% | 25% | 40% | 42% | |
| Moderate | 4% | 3% | 3% | 4% | |
| Heavy | 18% | 8% | 6% | 12% | |
| Current smoking | 71% | 54% | 35% | 42% | <0.001 |
| Current marijuana use | 30% | 26% | 20% | 27% | 0.05 |
| Ever injection drug use | 36% | 23% | 1% | 4% | <0.001 |
| Metabolic | |||||
| BMI (kg/m2) | 30 (25, 36) | 28 (23, 32) | 31 (26, 36) | 32 (27, 38) | <0.001 |
| Waist circumference (cm) | 99 (88, 115) | 97 (86, 108) | 99 (89, 111) | 100 (88, 113) | 0.12 |
| HOMA-IR | 3.2 (1.6, 6.8) | 2.48 (1.3, 4.9) | 2.1 (1.3, 3.8) | 1.8 (1.1, 3.3) | <0.001 |
| Liver-related | |||||
| AST (U/L) | 26 (19, 37) | 24 (18, 35) | 19 (15, 23) | 17 (14, 20) | <0.001 |
| ALT (U/L) | 23 (15, 34) | 18 (12, 30) | 15 (12, 21) | 14 (11, 18) | <0.001 |
| HIV-related | |||||
| Undetectable HIV RNA | 69% | 72% | 0.60 | ||
| CD4 current (cells/mm3) | 616 (428, 869) | 656 (435, 870) | 0.35 | ||
| CD4 nadir (cells/mm3) | 215 (107, 320) | 222 (103, 361) | 0.95 | ||
| History of clinical AIDS | 42% | 28% | <0.001 | ||
| Current ART | 89% | 89% | 0.81 | ||
| NNRTI | 30% | 29% | 0.84 | ||
| PI | 26% | 25% | 0.80 | ||
| INSTI | 44% | 48% | 0.22 | ||
| EI | 1.6% | 0.8% | 0.26 |
ALT, alanine aminotransferase; AST, aspartate transaminase; BMI, body mass index; EI, entry inhibitor; HCV, hepatitis C virus; HOMA-IR, homeostatic model assessment of insulin resistance; INSTI, integrase strand transfer inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; PI, protease inhibitor.
Patient and public involvement
Participants of the LIVRA study were not involved in the development of the study question or the liver disease outcomes. However, the national community advisory board of the WIHS (now MWCCS) approved the study of liver disease progression using VCTE as a high scientific priority.
Findings to date
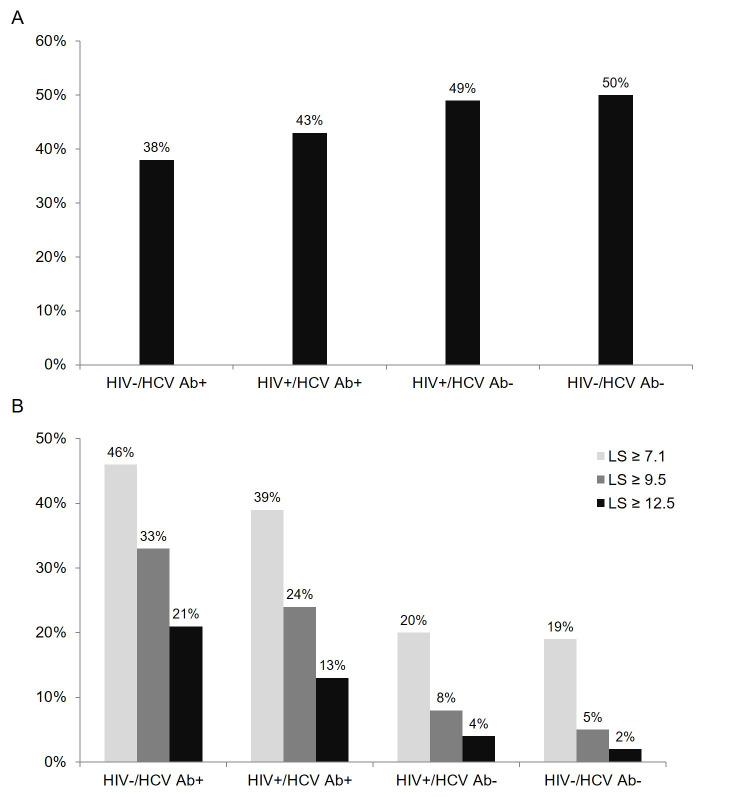
At baseline, women with neither HIV nor HCV had higher median CAP values than women with HCV monoinfection (247 dB/m (IQR 204, 281) vs 232 dB/m (IQR 191, 285)), and women with HIV monoinfection had higher values than women with HIV/HCV coinfection (246 dB/m (IQR 208, 290) vs 237 dB/m (IQR 200, 272)). Similarly, the prevalence of hepatic steatosis based on CAP ≥248 dB/m was highest in women with neither infection (50%), followed by those with HIV monoinfection (49%), HIV/HCV coinfection (43%) and HCV monoinfection (38%) (figure 1A). The overall prevalence of steatosis was 48%, which is slightly higher than the 43% prevalence observed among women in the 2017–2018 National Health and Nutrition Examination Survey study,20 which used a CAP cut-off of 263 dB/m, and higher than the 39% reported in a retrospective study of 1511 PLWH from Canada and Italy, which used the same 248 dB/m CAP cut-off as our study.21 The latter study included mostly white men, whereas our study included mostly black women, a group that has traditionally been found to have lower risk of hepatic steatosis.
Figure 1.
(A) Prevalence of VCTE-estimated hepatic steatosis (CAP ≥248 dB/m) by HIV and HCV antibody status. (B) Prevalence of VCTE-estimated significant fibrosis (LS ≥7.1 kPa), advanced fibrosis (LS ≥9.5 kPa) and cirrhosis (LS ≥12.5 kPa), as estimated by VCTE-measured liver stiffness, by HIV and HCV antibody status. Ab, antibody; CAP, controlled attenuation parameter; HCV, hepatitis C virus; LS, liver stiffness; VCTE, vibration controlled transient elastography.
On multivariable analysis, greater waist circumference (a marker of visceral obesity) and greater HOMA-IR were significantly associated with higher CAP values (table 3). Our findings are consistent with other studies that have demonstrated visceral adiposity and insulin resistance to be key mediators in the pathogenesis of fatty liver disease.22 23 However, HIV infection was not associated with CAP, suggesting that the clinical phenotype of fatty liver disease in PLWH is predominantly caused by metabolic dysregulation that appears to be independent of HIV infection. By contrast, HCV seropositivity was associated with significantly lower CAP values in analyses adjusted for alcohol use, smoking status and menopause stage. This is consistent with our prior finding that non-genotype 3 HCV infection was associated with significantly lower magnetic resonance spectroscopy-measured liver fat fraction among 356 men and women with or without HIV and HCV.24 Further research on the potential mechanisms underlying this observation as well as the impact of HCV clearance on fatty liver disease are warranted.
Table 3.
Independent associations of clinical and demographic characteristics with CAP and LS*
| CAP difference (dB/m) (95% CI)† | P value | LS % change (95% CI)‡ |
P value | |
| Infection status (ref=HIV−/HCV−) | ||||
| HIV+/HCV− | 1.1 (−5.3 to 7.5) | 0.74 | 4.4% (−1.1% to 10.3%) | 0.12 |
| HIV+/HCV+ | −9.2 (−18.2 to –0.3) | 0.04 | 33.4% (23.5% to 44.1%) | <0.001 |
| HIV−/HCV+ | −10.4 (−23.8 to 3.1) | 0.13 | 43.2% (27.8% to 60.4%) | <0.001 |
| Age (per 10 years) | 2.4 (−2.0 to 6.9) | 0.29 | 4.4% (0.4% to 8.4%) | 0.03 |
| Race/Ethnicity (ref=white non-Hispanic) | ||||
| Black | −6.1 (−14.2 to 2.1) | 0.14 | 2.8% (−4.0% to 10.1%) | 0.43 |
| Hispanic | −3.1 (−12.6 to 6.4) | 0.52 | 3.1% (−5.0% to 11.7%) | 0.47 |
| Other | 2.9 (−8.2 to 14.0) | 0.61 | 2.5% (−6.7% to 12.7%) | 0.60 |
| Waist circumference (per 10 cm) | 17.8 (16.2 to 19.4) | <0.001 | 5.0% (3.3% to 6.6%) | <0.001 |
| HOMA-IR (per doubling) | 1.2 (0.8 to 1.6) | <0.001 | 0.3% (−0.1% to 0.7%) | 0.11 |
| CAP (per 10 dB/m) | 0.6% (0.1% to 1.0%) | 0.01 |
*All variables shown in the table are included in a single multiple linear regression model (one model for CAP and one for LS). Also adjusted for alcohol use, smoking status and menopause stage (parameter estimates not shown).
†N=1543.
‡N=1576.
CAP, controlled attenuation parameter; HCV, hepatitis C virus; HOMA-IR, homeostatic model assessment of insulin resistance; LS, liver stiffness.
As expected, women with HCV had higher median LS values compared with women without HCV, with the highest LS observed among those with HCV monoinfection (6.9 kPa (IQR 5.0, 10.7)), followed by those with HIV/HCV coinfection (6.2 kPa (IQR 4.6, 9.1)), HIV monoinfection (5.0 kPa (IQR 3.9, 6.7)) and those with neither infection (4.9 kPa (IQR 3.9, 6.2)). Prevalence of significant fibrosis (LS ≥7.1 kPa), advanced fibrosis (LS ≥9.5 kPa) and cirrhosis (LS ≥12.5 kPa) was also higher among women with HCV compared with those without HCV (figure 1B). In multivariable analysis, HIV/HCV coinfection, HCV monoinfection, older age, greater waist circumference and greater CAP values were each independently associated with higher LS (table 3). These findings have important implications for women as visceral adiposity and metabolic abnormalities increase during the menopausal transition, independent of chronologic age.25 Oestrogen depletion occurs during the late phase of perimenopause and is associated with increased levels of inflammatory cytokines26 and mucosal barrier dysfunctions.27 These changes may result in increased gut microbial translocation and inflammation,28 factors that have also been linked with steatosis and fibrosis.29 30 Studies are underway evaluating the impact of ovarian follicular reserve on steatosis and fibrosis among LIVRA participants.
In analysis restricted to women living with HIV, HIV-related factors such as CD4 count, HIV RNA and ART regimen, were not significantly associated with CAP or LS on cross-sectional analysis. However, the potential impact of ART class, including integrase strand transfer inhibitors, on incident steatosis and fibrosis will be an important area of research within the cohort prospectively. Finally, a notable finding was that the factors associated with steatosis and fibrosis were similar after excluding VCTE examinations with IQR/median >30%, success rate <60%, poor image quality or any of these three criteria (online supplemental tables 1 and 2). In the setting of a large multicentre epidemiological study, these findings provide assurance about the rigour of our data collection approach. In clinical practice, currently accepted VCTE validity criteria should be adhered to.
bmjopen-2021-055706supp001.pdf (99.9KB, pdf)
Strengths and limitations
To our knowledge, this is the most comprehensive cohort study evaluating liver disease among US women using VCTE and the largest study of VCTE in women living with HIV. However, our cohort has limitations. First, there are demographic differences by HIV and HCV serostatus, and thus unmeasured confounders may remain despite adjustment for multiple variables. Second, we rely on VCTE to assess liver disease, rather than liver biopsy. However, liver biopsy is infeasible in large cohorts such as ours. Finally, our findings may not be generalisable to men, but our VCTE protocol is currently being implemented in men enrolled in the newly integrated MWCCS allowing us to address sex differences.
A major strength of the LIVRA study is that it is conducted in a large, nationally representative cohort of women living with HIV in the USA,31 where racial and ethnic minorities, people living below the poverty line and those with less than a high school education are at higher risk for liver disease.32 Second, LIVRA has detailed longitudinal HIV and HCV data allowing the study of liver steatosis and fibrosis trajectories in women with active HCV viraemia, spontaneous HCV clearance and treated HCV clearance. Third, the inclusion of women with and without HIV and HCV infections will allow us to evaluate the association of viral factors with liver disease using seronegative controls. Finally, due to our rigorous QA programme, a low proportion of VTCE scans were invalid based on traditional criteria for unreliability and excluding these scans did not impact our results. With longitudinal assessments, the LIVRA study will enable evaluation of hepatic steatosis and fibrosis progression in women and support investigation of mechanistic pathways and potentially modifiable risk factors for liver disease in high-risk women.
Collaboration
The datasets generated and analysed during the current study are not publicly available but are available from the principal investigator of the LIVRA study on reasonable request and on approval by the Executive Committee of the MACS-WIHS Combined Cohort Study. Please see https://statepi.jhsph.edu/mwccs/work-with-us/ for further information on how to work with our cohort.
Supplementary Material
Footnotes
Contributors: PCT and YM contributed the original concept and design of the study. PCT, AA, MF, ALF, ETG, DK-P, MHK, IO, MP and AS were involved in data collection and sample management. YM, JP and PCT performed data analysis and all authors interpreted the data interpretation. JP drafted the manuscript. PCT is responsible for the overall content as guarantor. All authors have critically revised this article and approved the final version to be published.
Funding: Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS), now the MACS/WIHS Combined Cohort Study (MWCCS). MWCCS (Principal Investigators): Atlanta CRS ((IO, AS and Gina Wingood), U01-HL146241; Baltimore CRS (Todd Brown and Joseph Margolick), U01-HL146201; Bronx CRS (Kathryn Anastos and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01- HL146202; Data Analysis and Coordination Center (Gypsyamber D’Souza, Stephen Gange and Elizabeth Golub), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Chicago-Northwestern CRS (Steven Wolinsky), U01-HL146240; Northern California CRS (Bradley Aouizerat, JP and Phyllis Tien), U01-HL146242; Los Angeles CRS (Roger Detels and Matthew Mimiaga), U01-HL146333; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, MF and Deborah Jones), U01-HL146203; Pittsburgh CRS (Jeremy Martinson and Charles Rinaldo), U01-HL146208; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom and DK-P), U01-HL146192; UNC CRS (Adaora Adimora), U01-HL146194. The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD), National Institute on Aging (NIA), National Institute of Dental & Craniofacial Research (NIDCR), National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Neurological Disorders and Stroke (NINDS), National Institute of Mental Health (NIMH), National Institute on Drug Abuse (NIDA), National Institute of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute on Minority Health and Health Disparities (NIMHD) and in coordination and alignment with the research priorities of the National Institutes of Health, Office of AIDS Research (OAR). MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR003098 (JHU ICTR), UL1-TR001881 (UCLA CTSI), P30-AI-050409 (Atlanta CFAR), P30-AI-073961 (Miami CFAR), P30-AI-050410 (UNC CFAR), P30-AI-027767 (UAB CFAR) and P30-MH-116867 (Miami CHARM). The study was also supported by the National Institute of Allergy and Infectious Diseases (K24 AI 108516 (PCT)), the National Institute of Diabetes and Digestive and Kidney Diseases (5R01DK109823 (PCT)) and an American College of Gastroenterology Junior Faculty Development Award (JP).
Disclaimer: The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH).
Competing interests: AA has received consulting fees from Merck, Viiv Healthcare and Gilead Sciences; Merck and Gilead Sciences have provided her institution with funding for her research. JCP has received consulting fees from Theratechnologies; Gilead Sciences and Merck have provided her institution with funding for her research. PCT: Merck has provided her institution with funding for her research; Gilead and Lilly have also provided her institution with funding for her to conduct industry-sponsored clinical trials. MHK reports consulting for Sanofi. All other authors have no conflicts of interest to report.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. The MACS or WIHS Public Use Data Set (PDS) is available to investigators. To submit a request form to gain access to the PDS visit https://airtable.com/shrVDP51W5J2qcNeT. MWCCS PDS will be available in 2022
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
Ethics approval
The study was approved by the Institutional Review Boards (IRB) of all participating sites and all participants provided written informed consent to undergo longitudinal VCTE exam during the WIHS study visit. Each participating institution’s IRB has been formally designated to review and monitor biomedical research involving human subjects, with the primary responsibility being the protection of subjects from undue risk and from deprivation of personal rights and dignity, which are the touchstones of ethical research.
References
- 1.Smith CJ, Ryom L, Weber R, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet 2014;384:241–8. 10.1016/S0140-6736(14)60604-8 [DOI] [PubMed] [Google Scholar]
- 2.Bhala N, Angulo P, van der Poorten D, et al. The natural history of nonalcoholic fatty liver disease with advanced fibrosis or cirrhosis: an international collaborative study. Hepatology 2011;54:1208–16. 10.1002/hep.24491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005;41:1313–21. 10.1002/hep.20701 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Global health Observatory (GHO) data: number of women living with HIV. Geneva: World Health Organization, 2017. [Google Scholar]
- 5.Centers for Disease Control and Prevention . Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report 2019;24(No. 1), 2019. Available: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Accessed 31 Oct 2019].
- 6.Balakrishnan M, Patel P, Dunn-Valadez S, et al. Women have a lower risk of nonalcoholic fatty liver disease but a higher risk of progression vs men: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2021;19:61-71.e15. 10.1016/j.cgh.2020.04.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D'Souza G, Bhondoekhan F, Benning L, et al. Characteristics of the MACS/WIHS combined cohort study: opportunities for research on aging with HIV in the longest us observational study of HIV. Am J Epidemiol 2021;190:1457 10.1093/aje/kwab050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adimora AA, Ramirez C, Benning L, et al. Cohort profile: the women's Interagency HIV study (WIHS). Int J Epidemiol 2018;47:393–4. 10.1093/ije/dyy021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castéra L, Foucher J, Bernard P-H, et al. Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology 2010;51:NA–835. 10.1002/hep.23425 [DOI] [PubMed] [Google Scholar]
- 10.Kettaneh A, Marcellin P, Douvin C, et al. Features associated with success rate and performance of FibroScan measurements for the diagnosis of cirrhosis in HCV patients: a prospective study of 935 patients. J Hepatol 2007;46:628–34. 10.1016/j.jhep.2006.11.010 [DOI] [PubMed] [Google Scholar]
- 11.de Lédinghen V, Vergniol J, Foucher J, et al. Feasibility of liver transient elastography with FibroScan using a new probe for obese patients. Liver Int 2010;30:1043–8. 10.1111/j.1478-3231.2010.02258.x [DOI] [PubMed] [Google Scholar]
- 12.Gaia S, Carenzi S, Barilli AL, et al. Reliability of transient elastography for the detection of fibrosis in non-alcoholic fatty liver disease and chronic viral hepatitis. J Hepatol 2011;54:64–71. 10.1016/j.jhep.2010.06.022 [DOI] [PubMed] [Google Scholar]
- 13.Karlas T, Petroff D, Sasso M, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol 2017;66:1022–30. 10.1016/j.jhep.2016.12.022 [DOI] [PubMed] [Google Scholar]
- 14.Duarte M, Price J, Ma Y. Characteristics of non-invasive surrogates of hepatic steatosis among persons living with HIV. AASLD 2020. [Google Scholar]
- 15.Singh S, Muir AJ, Dieterich DT, et al. American gastroenterological association Institute technical review on the role of elastography in chronic liver diseases. Gastroenterology 2017;152:1544–77. 10.1053/j.gastro.2017.03.016 [DOI] [PubMed] [Google Scholar]
- 16.Harlow SD, Gass M, Hall JE, et al. Executive summary of the stages of reproductive aging workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab 2012;97:1159–68. 10.1210/jc.2011-3362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Harthi L, Voris J, Du W, et al. Evaluating the impact of hepatitis C virus (HCV) on highly active antiretroviral therapy-mediated immune responses in HCV/HIV-coinfected women: role of HCV on expression of primed/memory T cells. J Infect Dis 2006;193:1202–10. 10.1086/500843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Laskus T, Wilkinson J, Karim R, et al. Hepatitis C virus quasispecies in HIV-infected women: role of injecting drug use and highly active antiretroviral therapy (HAART). Hepatology 2007;46:359–70. 10.1002/hep.21715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allison PD. Handling missing data by maximum likelihood. SAS Global Forum 2012:312–2012. [Google Scholar]
- 20.Kim D, Cholankeril G, Loomba R. Prevalence of fatty liver disease and fibrosis detected by FibroScan in adults in the United States, 2017-2018. Clin Gastroenterol Hepatol 2020. [DOI] [PubMed] [Google Scholar]
- 21.Cervo A, Milic J, Mazzola G. Prevalence, predictors and severity of lean non-alcoholic fatty liver disease in HIV-infected patients. Clin Infect Dis 2020. [DOI] [PubMed] [Google Scholar]
- 22.van der Poorten D, Milner K-L, Hui J, et al. Visceral fat: a key mediator of steatohepatitis in metabolic liver disease. Hepatology 2008;48:449–57. 10.1002/hep.22350 [DOI] [PubMed] [Google Scholar]
- 23.Marchesini G, Brizi M, Morselli-Labate AM, et al. Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med 1999;107:450–5. 10.1016/S0002-9343(99)00271-5 [DOI] [PubMed] [Google Scholar]
- 24.Price JC, Ma Y, Scherzer R, et al. Human immunodeficiency virus-infected and uninfected adults with non-genotype 3 hepatitis C virus have less hepatic steatosis than adults with neither infection. Hepatology 2017;65:853–63. 10.1002/hep.28968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sowers M, Zheng H, Tomey K, et al. Changes in body composition in women over six years at midlife: ovarian and chronological aging. J Clin Endocrinol Metab 2007;92:895–901. 10.1210/jc.2006-1393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pfeilschifter J, Köditz R, Pfohl M, et al. Changes in proinflammatory cytokine activity after menopause. Endocr Rev 2002;23:90–119. 10.1210/edrv.23.1.0456 [DOI] [PubMed] [Google Scholar]
- 27.Grishina I, Fenton A, Sankaran-Walters S. Gender differences, aging and hormonal status in mucosal injury and repair. Aging Dis 2014;5:160–9. 10.14336/AD.2014.0500160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sankaran-Walters S, Macal M, Grishina I, et al. Sex differences matter in the gut: effect on mucosal immune activation and inflammation. Biol Sex Differ 2013;4:10. 10.1186/2042-6410-4-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harte AL, da Silva NF, Creely SJ, et al. Elevated endotoxin levels in non-alcoholic fatty liver disease. J Inflamm 2010;7:15. 10.1186/1476-9255-7-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang SQ, Lin HZ, Lane MD, et al. Obesity increases sensitivity to endotoxin liver injury: implications for the pathogenesis of steatohepatitis. Proc Natl Acad Sci U S A 1997;94:2557–62. 10.1073/pnas.94.6.2557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D'Souza G, Bhondoekhan F, Benning L. Characteristics of the MACS-WIHS combined cohort study: opportunities for research on aging with HIV in the longest us observational study of HIV. Am J Epidemiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scaglione S, Kliethermes S, Cao G, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol 2015;49:690–6. 10.1097/MCG.0000000000000208 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055706supp001.pdf (99.9KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. The MACS or WIHS Public Use Data Set (PDS) is available to investigators. To submit a request form to gain access to the PDS visit https://airtable.com/shrVDP51W5J2qcNeT. MWCCS PDS will be available in 2022