Abstract
Background
Hand hygiene is a fundamental action which is simple, inexpensive and an effective tool in reducing hospital-acquired infections, yet compliance remains low in healthcare settings. In 2014, Changi General Hospital embarked on a pilot project to improve hand hygiene compliance in a pilot ward with the intention to eventually spread a multifaceted set of interventions hospital wide.
Methods
A before and after interventional study of a pilot project. Hand hygiene data collection was through direct observations by auditors using WHO monitoring standards and techniques based on the five-moment model.
Setting
A medical ward in an acute hospital in Singapore.
Results
Overall hand hygiene compliance improved from a median of 53% in 2015 to 80% by end of 2017. Hand hygiene compliance of doctors increased from 43% to 60% (p=0.00), nurses from 62% to 89% (p=0.014) and allied health staff from 67% to 83% (p=0.002).
Conclusions
A multifaceted set of interventions developed by the project team was effective in improving hand hygiene compliance of doctors, nurses and allied health staff.
Keywords: Healthcare quality improvement, Infection control, Patient safety, PDSA
Introduction
Between 5 and 10 per cent of patients admitted to acute care hospitals acquire new infections.1 Patients with hospital-acquired infection (HAI) have two and a half times longer length of stay, which results in almost three times higher hospital costs.2 Cross-infection of patients by healthcare workers with contaminated hands is still a major source of infection.
Proper hand hygiene (HH) is a very useful and simple practice to reduce HAIs. However, the compliance rates are generally low globally, although its importance is increasingly being recognised and the numbers have gradually started to go up in select healthcare systems. A systematic review of 35 studies revealed that HH compliance rates were between 60% and 70%.3
Also, literature has shown that improved HH compliance is associated with decreased healthcare-acquired infections, including serious infections.3 4 An increase in HH adherence by three times was shown to reduce incidence of HAIs by 64%.3
Prior studies have also shown that a multifaceted approach would be important to HH compliance rates.5
In 2014, at Changi General Hospital (CGH), a public teaching hospital with over 1000 beds serving the eastern population of Singapore, a pilot project was started to test out the value of a multifaceted set of HH interventions. If found to be valuable, the final goal was to eventually spread these interventions hospital wide. CGH has close to 800 doctors, 2500 nurses and 600 allied health staff.
Methods
In October 2014, a multidisciplinary improvement team was formed under the sponsorship of hospital management. A doctor and a nurse manager were appointed as team leaders for this project. Members of the team included ward nurses, physiotherapists and a radiographer. An infection prevention and control nurse and facilitators from the quality improvement (QI) department were also involved in the project as subject matter experts. Having a multidisciplinary team was a critical aspect of the team setup as the interventions were meant to target every profession working in a medical ward.
The project aims to increase HH compliance of various professions in the pilot ward by 10%–20% from baseline in 3 years (December 2017).
A medical ward with 44 beds was selected as the pilot site because it already had various QI initiatives in place and the ward team seniors were known to be highly motivated. Also, the ward had high flow of traffic from various groups of healthcare professionals with close to 50 nurses and 100 staff from other profession groups passing through the ward daily.
The project team did a baseline study at the start of the project. HH compliance data of each profession were collected by auditors appointed from the nursing and allied health staff who worked in the same ward. This was done to minimise Hawthorne effect.6 This would also give ownership of the data to the ward staff and they would be able to gather learnings from the experience. Each auditor would be required to go through a training session with infection prevention and control on WHO monitoring standards and techniques based on the five-moment model.7 Auditors were instructed to document moments only if they were able to observe entire portions of work processes relevant to a particular moment. They were also given a minimum number of opportunities to observe to minimise variation in the data. Nurse auditors were to audit doctors and allied health staff while allied health auditors would audit nurses. The identity of the auditors was not revealed to the staff in the ward with the results sent to the project team.
Also, a survey of HH awareness was done via a questionnaire which tested knowledge of the five moments of HH, the types of HH products used in the hospital and trainings attended. Infection prevention and control nurses then conducted educational sessions for staff in the pilot ward to improve their HH knowledge.
Key measures for the project include HH compliance rate as an outcome measure, alcohol hand rub usage as a process measure and Methicillin-resistant Staphylococcus aureus (MRSA) rate to assess the impact of the project in reducing HAIs (table 1). HH compliance rate was selected as the outcome measure as the project was targeted at improving HH compliance in the pilot site. Alcohol hand rub usage would be a useful process measure as improved HH rates would see increased usage of alcohol hand rub usage. MRSA rate was selected as the MRSA rate was an indicator of concern in the pilot ward and had much room for improvement.
Table 1.
Operational definitions for measures
| Measure | Numerator | Denominator | Calculation |
| Hand hygiene compliance rate | Number of hand hygiene actions performed (ie, hand washing with soap and water or rubbing hands with alcohol-based hand sanitiser). Hand hygiene action is only valid once with every hand hygiene opportunity. | Number of hand hygiene opportunities observed | Hand hygiene compliance (%)=number of hand hygiene actions performed/ number of hand hygiene opportunities observed x 100 |
| Alcohol hand rub usage | Not applicable | Not applicable | Usage of alcohol hand rub in litres |
| Methicillin-resistant Staphylococcus aureus (MRSA) rate | Number of MRSA positive patients on exit | Number of patients screened | MRSA rate=number of MRSA positive patients on exit/number of patients screened |
Interventions
A comprehensive education on HH was conducted for targeted groups of staff. For every intervention tested, briefing was conducted to all the stakeholders. Surveys and direct observations were conducted to provide timely feedback to the team.
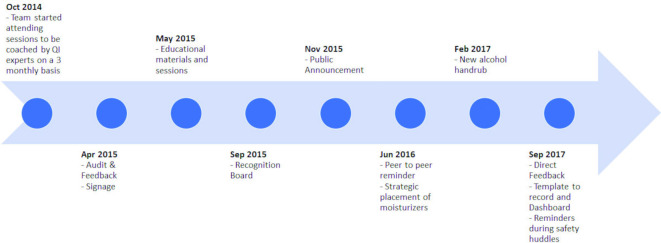
The interventions can largely be divided into three phases. The timeline of interventions is found in figure 1.
Figure 1.
Timeline of interventions.
Phase 1 (October 2014 to August 2015), the project focused mainly on education and an audit-feedback process (box 1). Education included coaching sessions for the team by experts from Institute of Healthcare Improvement (IHI), briefings by the infection control nurses and placement of posters and signs. Audits were conducted by the appointed auditors (described before) and the results were feedback to the respective departments.
Box 1. List of interventions.
Interventions introduced during the project.
Phase 1
Educational activities.
Audit and feedback.
Phase 2
Recognition board.
Public announcement.
Peer to peer reminder.
Change of alcohol hand rub.
Strategic placement of handrubs and moisturisers.
Step sequence labels for Personal Protective Equipment.
Phase 3
Direct feedback.
Template to record and dashboard.
Reminders during safety huddles/dept meetings/roll call.
The project moved onto phase 2 (September 2015 to August 2017), which relied on incentives and social pressure with the interventions mainly focused on positive reinforcement and culture building (box 1). A ‘recognition board’ was placed at the ward entrance to recognise doctors, nurses and allied health staff who performed well in HH for the month. The Public Announcement system was used in the in-patient wards to remind the staff daily about HH from 7:30 am to 10:00 am (every 30 min using different voices). The nursing staff and allied health staff had ‘peer to peer reminder’ sticker on staff badges to increase awareness and for reminding each other. We addressed barriers to proper HH such as change to a new alcohol hand rub (since the existing one cause dry hands) and identification of the best locations in the wards to place the hand rub and moisturisers. We also placed step-sequence labels to facilitate use of alcohol hand rub in the correct sequence before donning Personal Protective Equipment.
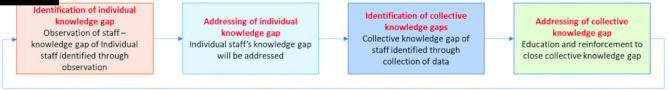
Based on the learnings from the earlier phases, the project then moved onto phase 3 (September 2017 onwards) (box 1). Nursing leaders in the ward were trained in HH auditing. During the daily clinical work, they were asked to record the compliance of all staff working in the ward and coach them just before they were about to miss an opportunity for HH. We called this ‘direct feedback’ and felt this would prevent unnecessary harm to patients. This would enable staff to associate their HH practice with their work processes and address individual knowledge gaps. Positive feedback was also given when good compliance was seen. The direct feedback process was given to doctors, nurses and allied health staff with a visual template used to record down timings, activities and moments where HH opportunities were missed. Staff from different professions were encouraged to remind each other about their HH practice in the spirit of learning and teamwork. To encourage self-reporting and speaking up for the purpose of learning, the team integrated HH as a component of ‘short safety huddles’ and monthly sessions. During the short safety huddles between shift changeover, staff would be encouraged to discuss or share anything about HH for 5 min.
In the monthly sessions initially facilitated by infection prevention and control nurses, staff would be given the opportunity to share openly about missed HH opportunities within work processes for the purpose of learning and ask questions about HH. In later stages, appointed HH champions was asked to lead the sessions and they could seek guidance from infection prevention and control nurses whenever necessary. Nursing leaders would also take the opportunity to share about the collective knowledge gaps observed, discuss about new initiatives and educate their staff during such monthly sessions.
To address collective knowledge gaps and weak areas, the project team learnt that the following sequence of steps could serve as a guide to leaders. The first step was to highlight the activities where missed opportunities often take place during roll calls. The second step was to create educational materials of these activities. The third step was to place relevant educational materials at strategic locations or on equipment where such activities take place. The fourth step was to highlight key steps in the process for such activities where HH was commonly missed out. The fifth step was to place labels to remind staff of the steps within processes where HH was commonly missed out. With each step, it gets more targeted and specific to highlight the weak areas.
Results
Baseline audit results showed poor overall HH compliance (54%) among the profession groups. The individual compliance rates of doctors, nurses, allied health staff were 43%, 62% and 67%, respectively.
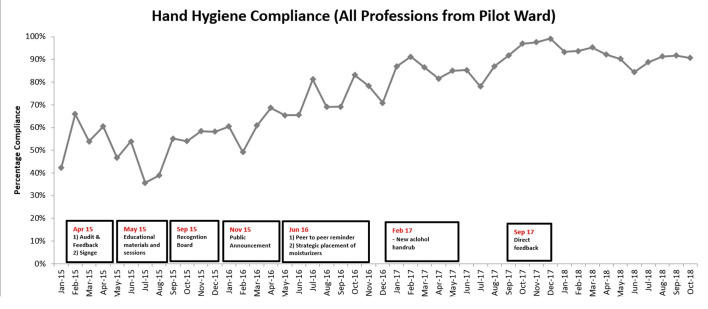
A Mann-Whitney test was used to determine the statistical significance of the results before and after the interventions. At the 3-year completion of the project, overall HH compliance improved from a median of 53% in 2015 to 80% by end of 2017, an increase of 26% (figure 2). Compliance of doctors increased from 43% to 60% (p=0.00). HH compliance of nurses increased from 62% to 89% (p=0.014). HH compliance of allied health staff increased from 67% to 83% (p=0.002) (table 2).
Figure 2.
Run chart of HH compliance. HH, hand hygiene.
Table 2.
HH compliance before and after intervention
| Profession | Total opportunities before |
Total opportunities after |
HH compliance: before (%) | HH compliance: after (%) | Percentage difference (%) | P value |
| Doctors (pilot unit only) |
1704 | 812 | 43 | 60 | 17 | 0.00 |
| Nurses (pilot unit only) |
304 | 749 | 62 | 89 | 27 | 0.014 |
| Allied health (pilot unit only) |
729 | 1012 | 67 | 83 | 16 | 0.002 |
HH, hand hygiene.
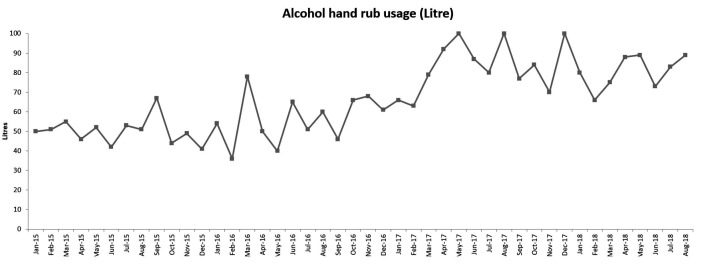
Alcohol hand rub usage increased from a median of 51 L in 2015 to 80 L by end of 2017 (figure 3).
Figure 3.
Run chart of alcohol usage.
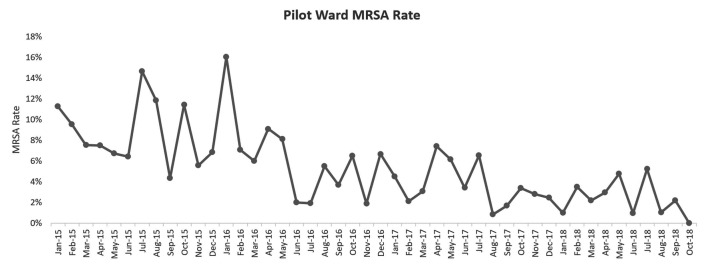
MRSA rate decreased from a median of 8% in 2015 to 3% by end of 2017 (figure 4). These results are congruent with findings from the literature that HH compliance has a negative correlation with healthcare-acquired infections including decrease in serious infections.3 4
Figure 4.
Run chart of MRSA rate. MRSA, Methicillin-resistant Staphylococcus aureus.
Discussion
Previous studies have shown that a multifaceted approach is critical for HH improvement. The WHO recommends a strategy with key components such as system change, training/education, evaluation & feedback, reminders in the workplace and institutional safety climate.8
Boyce also suggested that strategies to improve adherence to HH practices should be both multifaceted and multidisciplinary.9 Huis reviewed 41 controlled studies and results showed that the effectiveness of strategies increased for the studies that addressed five determinants of behaviour change as compared with studies addressing one determinant of behaviour change.10 In another study, Grol concluded that multimodal interventions have pronounced effects on practice and outcomes.11
The initial setup of a multidisciplinary pilot project team endorsed by the management was critical to the success of this project. Members of different profession were key in communicating the new initiatives to their profession group and gather buy-in. By being in the project team, they were familiar with the rationale for those interventions and how key principles behind those interventions could be adapted into the context of the work processes of their respective profession groups.
Our team referenced and incorporated suitable best practices suggested in other studies and embarked on a multifaceted set of interventions. However, we also recognised that our organisation has its own unique challenges and key principles from best practices around the world would have to be adapted to make them work in our own organisational context.
The project team was invited to attend sessions that had experts from IHI and other local healthcare QI teams working on similar projects share about the Model for Improvement,12 conducting plan-do-study-act rapid testing cycles and other QI tools. These learnings from sessions held every 3 months provided guidance for the study team.
The project realised that leaders and supervisors have strong influence on behaviour of staff. We felt that getting them to ‘own’ the problem and empowering them to coach their staff greatly helped in improving HH compliance. Their involvement also enables demonstration of visible support by leaders and supervisors, which in the long term would help build a HH culture, where staff could remind each other regardless of profession and rank.
Studies have shown that audit-feedback processes are widely used and can be effective to improve professional practice.13 The Joint Commission, the Centers for Disease Control and Prevention and the WHO have strongly advocated for facilities to monitor HH compliance and provide the information back to frontline staff, so that they can improve adherence to recommended practice.14 A study by Naikoba established that for feedback of performance, if not repeated regularly, this effect would not be maintained over long periods.15 The team learnt the importance of maximising the use of the audit results and observations during huddles and monthly sessions for both individual learning and group learning. Immediate feedback after missed HH opportunities would also help address individual knowledge gaps. Giving of positive feedback was also important to encourage staff who were already having good HH practice to continue to do so.
Having observations in place in the ward enabled leaders to create a cycle of HH learning (figure 5), which addressed individual and collective knowledge gaps immediately. We believe that this learning cycle potentially ensures high levels of HH compliance amidst changes such as staff turnover or evolving best practices.
Figure 5.
Cycle of HH learning. HH, hand hygiene.
Besides looking at the areas for improvement from observations and audit results, the team learnt the importance of celebrating the good HH practice of staff through having a recognition board. The recognition board was well received and staff were appreciative when they received a small token of appreciation for their good HH practice. The recognition board was a visible representation of the importance placed by the leaders on HH. It helped to strengthen belief in the importance of HH among staff and appeal to both their intrinsic and extrinsic motivations for good practice.
For effective education of staff, information about five moments of HH had to be made relatable to the different profession groups and shared in the appropriate platform within profession groups. For example, the five moments were made relatable to the allied health staff through examples of their work situations. This was regularly shared and reinforced during monthly department meetings with sharing of the HH compliance rate. The whole department was educated as allied health staff in the ward can vary or change depending on the manpower coverage.
There were a few obstacles faced during the 3-year project. The HH auditors were not able to get protected time to conduct HH audits. This limited the number of audits done per month per profession, which could have led to greater variation in the data. Audit fatigue was also an issue, which led to the need to change auditors periodically. There was also a drop in number of observations and diminished learning over time.
Conclusions
A multifaceted set of interventions successfully improved HH compliance of doctors, nurses and allied health staff in the pilot ward.
To ensure sustainability of interventions, we worked on getting the interventions to be incorporated into daily work processes.
Ward supervisors were asked to give feedback as part of everyday coaching of their junior staff. Closing of gaps in HH practice was to be part of supervisor’s role to own the issue of maintaining high HH standards.
We set up two taskforces (medical and surgical) consisting of doctors, nurses, allied health and operation staff. The taskforces would have oversight of HH standards in the medical and surgical wards and also bring in new ideas for further improvement.
The learnings formed a basis for the project team to develop a comprehensive set of interventions to be employed institution wide. Following this project, the hospital has ‘spread’ these interventions to all the inpatient areas.
We hope that our study will contribute to the body of knowledge of HH improvement strategies.
Footnotes
Contributors: All authors listed in this manuscript contributed to the design and implementation of this quality improvement initiative. As a multi-disciplinary team, each author made unique contributions, providing understanding in their area of work and shedding insights that may not be known to other team members. VP as the main author is responsible for the overall content of this article. VP and AP provided their invaluable leadership to the initiative, driving change in the pilot ward in addition to providing insights about clinical processes of doctors and nurses respectively. MA and FMA contributed their understanding of the operational challenges of nurses in the pilot ward and engaged their nursing colleagues. KKP, AS and SHT as allied health professionals communicated to their colleagues and adapted changes to work in their domain. LJ contributed subject matter expertise in infection prevention and control which included hand hygiene and trained hand hygiene auditors. WBA and AC facilitated the project and guided the team to test changes systematically using quality improvement methodologies as quality improvement specialists.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Burke JP. Infection control - a problem for patient safety. N Engl J Med 2003;348:651–6. 10.1056/NEJMhpr020557 [DOI] [PubMed] [Google Scholar]
- 2.Plowman R, Graves N, Griffin MA, et al. The rate and cost of hospital-acquired infections occurring in patients admitted to selected specialties of a district general Hospital in England and the National burden imposed. J Hosp Infect 2001;47:198–209. 10.1053/jhin.2000.0881 [DOI] [PubMed] [Google Scholar]
- 3.Mouajou V, Adams K, DeLisle G, et al. Hand hygiene compliance in the prevention of hospital-acquired infections: a systematic review. J Hosp Infect 2022;119:33–48. 10.1016/j.jhin.2021.09.016 [DOI] [PubMed] [Google Scholar]
- 4.Yeung WK, Tam WSW, Wong TW, Tze WW. Clustered randomized controlled trial of a hand hygiene intervention involving pocket-sized containers of alcohol-based hand rub for the control of infections in long-term care facilities. Infect Control Hosp Epidemiol 2011;32:67–76. 10.1086/657636 [DOI] [PubMed] [Google Scholar]
- 5.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. The Lancet 2000;356:1307–12. 10.1016/S0140-6736(00)02814-2 [DOI] [PubMed] [Google Scholar]
- 6.Haas JP, Larson EL. Measurement of compliance with hand hygiene. J Hosp Infect 2007;66:6–14. 10.1016/j.jhin.2006.11.013 [DOI] [PubMed] [Google Scholar]
- 7.WHO . WHO guidelines on hand hygiene in health care 2009.
- 8.WHO . A guide to the implementation of the WHO multimodal hand hygiene improvement strategy 2009.
- 9.Boyce JM, Pittet D, Healthcare Infection Control Practices Advisory Committee, et al. Guideline for hand hygiene in health-care settings. Recommendations of the healthcare infection control practices Advisory Committee and hipac/shea/apic/idsa hand hygiene task force. Am J Infect Control 2002;30:S1–46. 10.1067/mic.2002.130391 [DOI] [PubMed] [Google Scholar]
- 10.Huis A, van Achterberg T, de Bruin M, et al. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implement Sci 2012;7:92. 10.1186/1748-5908-7-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet 2003;362:1225–30. 10.1016/S0140-6736(03)14546-1 [DOI] [PubMed] [Google Scholar]
- 12. Langley, Moen R, Nolan KM. The improvement guide: a practical approach to enhancing organizational performance. 2nd edn, 2009. [Google Scholar]
- 13.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012.;12:CD000259. 2012 Jun. 10.1002/14651858.CD000259.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conway LJ, Riley L, Saiman L. Implementation and impact of an automated group monitoring and feedback system to promote hand hygiene among health care personnel. Jt Comm J Qual Patient Saf 20142014;40:408–17. 10.1016/S1553-7250(14)40053-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naikoba S, Hayward A. The effectiveness of interventions aimed at increasing handwashing in healthcare workers - a systematic review. J Hosp Infect 2001;47:173–80. 10.1053/jhin.2000.0882 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information.