Abstract
Acupuncture involves the stimulation of acupoints, which are located at specific sites of the human body, by insertion of fine metal needles, followed by manipulation. Acupuncture has been proven to be an effective treatment in pain relief. Available evidence showed that acupuncture alleviates acute pain in conditions such as postoperative pain, acute back pain, labour pain, primary dysmenorrhea, tension-type headaches and migraines. In addition, acupuncture relieves chronic pain, for example, low back pain (LBP), knee osteoarthritis (KOA), headache, shoulder pain, and neck pain. For other diseases like insomnia, drug addiction and stroke, more high-quality randomized control trials (RCTs) are needed to confirm the efficacy of acupuncture, although there are particular difficulties surrounding adequate blinding and control group designs. Recent biomedical technology unveils the mechanisms of acupuncture. Studies have found that adenosine triphosphate (ATP) and transient receptor potential vanilloid (TRPV) channels are involved in the stimulation of acupuncture at the acupoint area. In the central nervous system (CNS), neurotransmissions including opioids, serotonin, norepinephrine, orexin and endocannabinoid are modulated by acupuncture to induce analgesia. Moreover, acupuncture reduces cyclooxygenase-2 (COX-2) and prostaglandin E2 (PGE2) levels on the peripheral level by acting on the hypothalamic-pituitary-adrenal (HPA) axis, mediating peripheral opioid release. Acupuncture helps to treat insomnia by inhibiting sympathetic activity and down-regulating the HPA axis. Additionally, acupuncture reduces the effects of positive and negative reinforcements by modulating dopamine release in the nucleus accumbens. Recently, i-needles have been developed to allow for the analysis of metagenomics, meta-transcriptomics, and host-microbiome relationships following acupuncture, while skin implantable microsensors or needle-shaped microsensors are feasible for monitoring real-time microenvironmental changes in acupoints and even target organs. These studies may further accelerate the understanding of acupuncture’s action mechanism.
Keywords: Acupuncture, analgesia, neurotransmission, opioids, pain
Introduction
Acupuncture is the process of stimulating acupoints by inserting thin metal needles and manipulating them with manual, electrical, or other forms of stimulation. Acupoints are located throughout the body, with the majority located along 12 bilateral meridians and two midline channels, namely the Du and Ren Meridians [1]. Manual acupuncture (MA) involves lifting and thrusting the needles or rotating them until a sensation of Deqi is achieved, which is described as a sense of soreness, numbness, fullness, or heaviness [2]. Electroacupuncture (EA) was developed in the 1950s where the needles are connected to an electrical stimulator that delivers either high or low-frequency impulses, or a combination of both. Electrical stimulation frequency, voltage, waveform, and duration all contribute to the standardization of EA. Nonetheless, MA is considered the standard of care in the majority of clinical studies [3].
Since the 1970s, acupuncture has risen rapidly and become more and more popular in Western countries [4]. Acupuncture was recommended as a treatment for 43 diseases by the World Health Organisation (WHO) experts in 1979 [5]. In 1998, the National Institutes of Health [3] consensus conference concluded that “promising results have emerged, for example, demonstrating acupuncture’s efficacy in adult postoperative and chemotherapy nausea and vomiting, as well as in postoperative dental pain”. There are additional circumstances, such as addiction, stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia, myofascial pain, osteoarthritis, low back pain, carpal tunnel syndrome, and asthma, in which acupuncture may be beneficial as an adjunct treatment or an acceptable alternative or as part of a comprehensive management program [3]. The WHO Consultation on Acupuncture published a review of 225 clinical trials in 2002, concluding that acupuncture was effective for 28 diseases and beneficial for 63 others [6].
Acupuncture is distinguished by its simplicity, convenience, and low cost in clinical [7,8]. When performed by a properly trained practitioner, it is a relatively safe treatment setting with few adverse effects [8,9]. Standardization of acupoint sites improved the reliability and reproducibility of acupuncture studies, thereby increasing our understanding of how acupuncture works in clinical symptoms or diseases [10]. Acupuncture is used in conjunction with or as an alternative to conventional treatments in Western countries [11]. Researchers begin to elucidate the mechanism of action of acupuncture and develop a modern form of acupuncture as a result of the growing body of evidence. This review discusses the key progress of modern acupuncture and the underlying mechanisms of its clinical applications.
Acupuncture and pain
Acupuncture has been proven to be effective for pain relief (Table 1) [12], in both acute and chronic pain [13].
Table 1.
Efficacy of acupuncture in analgesia confirmed by many RCTs
| Efficacy of acupuncture analgesia on acute and chronic pain | References |
|---|---|
| Acupuncture for acute pain | |
| 1. Postoperative pain | [17] |
| 2. Emergency department and acute trauma setting | [18-21] |
| 3. Acute back pain | [23-26] |
| 4. Labour pain | [27-30] |
| 5. Dysmenorrhea | [35-38] |
| 6. Tension-type headaches and migraine | [42-46] |
| Acupuncture for chronic pain | |
| 1. Chronic low back pain | [52-67] |
| 2. Chronic headache | [42,43,70-77] |
| 3. Osteoarthritis knee pain | [51,79-87] |
| 4. Chronic neck pain | [91-93] |
| 5. Chronic shoulder pain | [96-99] |
Acupuncture for acute pain
Large-scale randomized controlled trials (RCTs) and systematic reviews have been conducted to determine the effect of acupuncture in acute pain conditions [14]. The evidence has focused on the efficacy of acupuncture for acute pain in postoperative pain, emergency department setting, back pain, labor pain, primary dysmenorrhea, tension-type headaches, and migraine.
Postoperative pain
Postoperative pain caused by surgical injury is an important challenge for health care providers [15]. Use of opioid analgesics is the most common treatment for postoperative pain , but is often associated with side effects [16]. Acupuncture is effective for postoperative pain management caused by various surgical procedures, for example, heart, abdominal, orthopedic, gynecological, and obstetric surgery [15]. A systematic review concludes that acupuncture reduces postoperative pain and opioid consumption along with nausea, sedation, pruritus, and urinary retention, when compared with sham controls [17].
Emergency department and acute trauma setting
Patients often visit the emergency department (ED) due to acute pain. Previous studies have examined the efficacy of acupuncture in patients with acute pain in ED setting such as musculoskeletal pain, abdominal pain, and rib fracture [18,19]. These studies have shown that when compared to retrospectively matched controls or sham control, acupuncture produced more effective pain and nausea relief in ED patients associated with musculoskeletal, abdominal pain, and rib fractures. A RCT reveals that acupuncture provides effective and immediate analgesia with better tolerance, compared to the intravenous morphine group in ED patients without adverse effects [20]. Similarly, acupuncture reduced acute pain by 50% faster than IV morphine in acute renal colic patients [21].
Acute back pain
Acute back pain usually lasts for less than 4 weeks, or sometimes not more than 3 months [22]. Acupuncture is one of the most widely used complementary and alternative methods for patients with low back pain (LBP). In 2013, a systematic review indicated that one session of acupuncture was able to reduce acute LBP, in addition to slight improvement of lower back symptoms, when compared with nonsteroidal anti-inflammatory drugs (NSAIDs) [23]. A large well-designed RCT demonstrates the effectiveness of acupuncture on acute LBP [24]. In this study, five sessions of acupuncture alone significantly reduced the pain and analgesic consumption and improved work readiness over conventional treatment, but there was minor variation between verum acupuncture, sham acupuncture, and placebo acupuncture [24]. In another RCT, one session acupuncture with concurrent gentle exercise induced greater analgesia for severely disabling acute LBP over diclofenac [25]. A systemic review published in 2013 demonstrated that acupuncture for acute LBP significantly improved the pain intensity over sham acupuncture or anti-inflammatory medicines, but the clinical significances were in borderline [23]. Acupuncture is also recommended as an optional treatment for acute LBP by the American College of Physicians [26].
Labour pain
Labour pain is severe and can be exacerbated when a woman feels tension, anxiety, and fear of the childbirth and birth experience. Many women prefer to give birth in the absence of drugs or surgical methods, thus turning to alternatives for pain management [27]. A Cochrane review published in 2011 indicated that acupuncture and acupressure reduced labor pain, decreased the use of pharmacological management, and improved satisfaction with pain management [27]. EA also reduces labour duration and epidurals’ use [28,29]. In another recent Cochrane review, some RCTs have shown the effectiveness of acupuncture for labour and post-partum pain, namely, reducing acute pain and the use of pharmacological analgesia, and increasing satisfaction with pain relief [30].
Dysmenorrhea
Primary dysmenorrhea is common cramping pain in women during menstruation [31] and it is also found in few women throughout their menstrual years [32]. The symptoms of dysmenorrhea are relieved by NSAIDs and oral contraceptives (OCs) [33]. However, these drugs are not satisfactory. Several complementary and alternative modalities can be used to relieve symptoms of dysmenorrhea, which includes acupuncture [34]. In 2011, a Cochrane review demonstrated the effect of acupuncture and acupoint stimulation on primary dysmenorrhea. This review concluded that acupuncture and acupoint stimulation were more effective in pain reduction than active control NSAIDs, and Chinese herbal medicine reduced pain in primary dysmenorrhea [35]. In 2016, another Cochrane review found that acupuncture is significantly more effective in reducing the pain in primary dysmenorrhea compared with NSAIDs or no acupuncture controls, but it is insignificant when compared to sham or placebo controls [36]. The findings of a network meta-analysis further confirmed that acupuncture and EA are superior to NSAIDs in decreasing the frequency of pain episodes of primary dysmenorrhea [37], and EA is more effective than acupuncture or NSAIDs as reported by another systematic review [38].
Tension-type headaches and migraine
Tension-type headache is a common type of primary headache, and sometimes, it may occur frequently and affect a patient’s quality of life. On the other hand, acute migraine is a repetitive attack of primary headache [39]. Acupuncture is commonly used to treat headaches [40] and is recommended by the European Federation of Neurological Societies as a complimentary optional treatment [41]. In 2016, a Cochrane review suggested that acupuncture produced promising effects on tension-type headaches over standard care, but minimal effect over sham acupuncture [42]. Similarly, acupuncture reduced migraine attacks more than prophylactic drug treatment, and it can be at least as effective or possibly more effective [43]. Subsequent RCT found that EA has a prophylactic effect on migraines [44]. According to the National Clinical Guideline Centre of the UK, 10 sessions of acupuncture are suggested for tension-type headaches and migraines when prophylactic medications are ineffective [45]. In comparison with sham acupuncture, acupuncture effectively reduced pain intensity in acute migraine attacks [46].
Acupuncture on chronic pain
Acupuncture is a valid treatment for chronic pain, including chronic LBP, knee osteoarthritis, chronic headache, shoulder pain, and neck pain [47-51].
Chronic low back pain
In contrast to acute back pain that is caused immediately by the strains or sprains of the soft tissues in the back, chronic back pain develops deliberately by several diseases such as degenerative disc disease, osteoarthritis herniated disc, spinal stenosis, compression fractures or sciatica. Acupuncture for chronic LBP is one of the most commonly used non-pharmacological pain-relieving techniques. Some early systematic reviews reported the use of acupuncture for chronic LBP and concluded its clinical efficacy [52-60]. These findings are consistent with other systemic reviews conducted over different control interventions [61-63]. Acupuncture provided positive outcomes in clinical use for the treatment of chronic LBP compared to the usual care [64]. Furthermore, a systematic review showed that acupuncture may have a positive effect on self-reported pain and functional limitations of nonspecific chronic LBP [63]. In 2015, an overview of sixteen systematic reviews confirmed the efficacy of acupuncture for LBP over conventional treatments, while producing short-term effects on pain relief and functional improvement [65]. Recent systematic reviews also indicated that acupuncture provids pain relief in lumbar disc herniation [66] and average effects on non-specific LBP [67].
Chronic headache
Chronic headaches and migraines occur more frequently than episodic tension-type headaches, which occur at least 15 days every month for at least three months [68,69]. Chronic migraine is less common and belongs to a group of migraine disorders. In 2009, Cochrane reviews found that acupuncture was effective for tension-type headaches [70] and migraines [71]. Earlier systematic reviews claimed the efficacy of acupuncture for recurrent headaches [72] or tension-type and cervicogenic headaches [73]. Similarly, earlier critical review and meta-analysis also indicated that acupuncture reduced the frequency of headaches in the treatment of headache [74,75], and Cochrane review in 2001 demonstrated that acupuncture was more effective than no treatment control or sham control for idiopathic headache [76]. Later, a systematic review concluded that acupuncture was superior to sham control or medication therapy for chronic headaches in terms of headache intensity, frequency, and response rate, which showed at least 33% improvement by assessing headache index, frequency or overall evaluation [77]. Subsequent Cochrane reviews provided the superiority of acupuncture over placebo to prevent frequent chronic tension-type headaches [42] and reduce the frequency of headaches in episodic migraines [43].
Osteoarthritis knee pain
Chronic knee pain is common in those above 50 years of age and it can disturb daily activities [78]. A systematic review indicated short-term improvements in pain associated with peripheral joint osteoarthritis after treatment with acupuncture [79,80], and it also reduced pain intensity, with improvement of quality of life and functional mobility [51]. According to a Cochrane review published in 2018, acupuncture significantly reduced pain associated with osteoarthritis of the hip [81]. Some systematic reviews showed that acupuncture increased the pain threshold in knee osteoarthritis (KOA) when compared to interventions alone, or in combination with other interventions [82-86]. Recent systematic reviews and meta-analyses have also concluded that acupuncture was beneficial for alleviating pain associated with KOA [87].
Chronic neck pain
Chronic neck pain is a major and serious health problem worldwide. It is characterized by activity limitations, dizziness, anxiety, and insomnia [88]. Non-pharmacological treatments have been reported to be effective in reducing neck pain [89]. Acupuncture is one of the accepted treatments for chronic neck pain [90]. An RCT showed that acupuncture treatment relieved neck pain and also improved the quality of sleep, anxiety, depression, and life satisfaction [91]. A Cochrane review in 2006 concluded that acupuncture eased chronic neck pain [92]. Another systematic review also found that individual treatment of acupuncture or EA and conventional medicine for chronic neck pain have similar effects on pain and disability [93]. However, a combination of EA with conventional treatment relieved pain better than acupuncture with conventional treatment.
Chronic shoulder pain
Chronic shoulder pain is the most common type of musculoskeletal pain and has a severe effect on patient’s quality of life [94]. This pain is caused by rotator cuff strain or tear, biceps tendinitis, subacromial bursitis, glenohumeral osteoarthritis, impingement syndrome, and adhesive capsulitis [95]. Acupuncture is clinically safe for the treatment of chronic shoulder pain [96]. An earlier RCT concluded that acupuncture is more effective at reducing the pain intensity in chronic shoulder pain patients than the control group, besides improving the secondary outcome measures, such as quality of life, functional ability, NSAIDs intake, and global satisfaction than the control group [97]. Previous RCTs showed beneficial effects of contralateral acupuncture and trigger-points acupuncture by improving the pain threshold and function in treating chronic shoulder pain [98,99]. Moreover, The German Randomized Acupuncture Trial for chronic shoulder pain (GRASP) found that acupuncture significantly increased the rate of patients with at least 50% reduction from the baseline visual analogue scale [24] for pain at 3 months post-treatment and directly after the end of treatment [96].
Acupuncture and insomnia
Acupuncture has long been used to treat insomnia, but the evidence to support its therapeutic effects is not sufficiently robust. Recent systemic reviews and meta-analyses have indicated that acupuncture is of marginal benefit to insomnia [100]. Lacking of high-quality clinical evidence clearly hampers a definitive conclusion in this regard [101,102]. Despite the aforementioned limitation, acupuncture is still widely used to treat insomnia clinically.
Acupuncture and opiate addiction
Acupuncture was first proposed as a means of providing relief from symptoms of opiate withdrawal in 1972 [103]. In 1985, a new auricular acupuncture protocol was developed that was subsequently adopted in many clinical settings in Western countries [104-106]. However, there are only a few RCTs that investigated the use of acupuncture treatment for opiate addiction, and the methodologies used in several clinical trials are of poor quality. In a recent systematic review, only 10 published articles met the inclusion criteria and no definitive conclusions were drawn [107]. More high-quality RCTs are needed to support the use of acupuncture in the treatment of drug addiction.
A recent RCT suggested that acupuncture can reduce the required daily dose of methadone, which is currently prescribed for opiate dependence [108]. This study raises the possibility of acupuncture as an appropriate adjuvant to methadone maintenance therapy in opiate addiction.
Other applications of acupuncture
In various other indications, evidence in support of acupuncture use is even weaker. For example, it remains contentious as to whether acupuncture has beneficial effects in the process of in vitro fertilization (IVF) [109], though traditional Chinese medicine has recorded the use of acupuncture in infertility treatment. IVF process involves several steps where women feel discomfort. A recent systematic review reported the benefits of acupuncture during an IVF process, if performed at a particular time during the process [110]. However, the effects of acupuncture on IVF outcomes remain to be demonstrated. The following suggestions may be considered for future studies: (i) to evaluate the effects of acupuncture on IVF outcomes, primary outcome measures can also include embryo viability, numbers of oocyte retrieval per treatment cycle, semen analysis, implantation rates, besides pregnancy rates; (ii) to examine whether acupuncture can improve the symptoms of discomfort associated with IVF treatment.
Stroke is a leading cause of death or disability worldwide, therefore, the clinical benefits of acupuncture in stroke treatment draw much attention. Although some pieces of evidence were provided [111], the meta-analysis suggests that the efficacy of acupuncture remains to be established with large-scale RCTs [112].
Issues for acupuncture RCTs
The lack of confirmatory data in acupuncture efficacy is partly caused by the difficulty in performing acupuncture RCTs, particularly in terms of adequate blinding and control group designs [113]. Furthermore, acupoint specificity is another special issue in acupuncture RCTs. It is believed that acupuncture at acupoints induces a better therapeutic response than that of a non-acupoint. Liang et al. (2015) listed many RCTs and clinical studies demonstrating that EA or acupuncture at acupoints was associated with significantly greater benefits than those at non-acupoints [114]. As mentioned in these studies, in current acupuncture RCTs, the selection of the sham acupoint was categorized into non-acupoints/sham points, irrelevant acupoints, and trigger points [114].
The use of a trigger point as a sham control must be performed with care. It is well known that a stimulating trigger point can produce significant pain relief [99]. When using trigger points as sham control in pain research, it may render the estimations of acupuncture-related therapeutic effects. Moreover, needle penetration into non-acupoints or irrelevant acupoints can act as nociceptive stimuli, which activate the A delta and/or peripheral C-fibers, causing diffuse noxious inhibitory controls [115]. In RCTs investigating acupuncture analgesia, if the control group design is involving needle penetration into non-acupoints or non-therapeutic acupoints, these procedures can reduce pain in the control subjects. A larger sample size is needed to demonstrate the acupoint specificity, whereby the efficacy of the real acupuncture treatment is superior to that of the non-acupoint or non-therapeutic acupoint control group.
Mechanistic understanding of acupuncture
Neurophysiology might illustrate the mechanism of acupuncture as well. Following the insertion of acupuncture needles, local receptors will first be activated, delivering neural impulses to the spinal cord and brain, which results in the modulation of physiological functions.
The physiological mechanism of acupuncture needling: the involvement in purinergic signaling pathway and TRPV family
The mechanism of acupuncture stimulation on a local acupoint is not yet understood completely. Purinergic signaling is proposed to be involved in the physiological mechanisms from acupuncture needling [116]. This hypothesis suggests that acupuncture needle insertion or electrical stimulation induces the release of adenosine triphosphate (ATP) from keratinocytes and fibroblasts in the skin for binding with purinergic receptors. As ATP rapidly degrades to adenosine, it’s binding to adenosine A1 receptors mediates analgesic effect in acupuncture [117]. In addition to purinergic signaling, degranulation of mast cells in tissues also plays an important role in acupuncture efficacy. Research has revealed a higher density of mast cells at acupoint ST36 as compared with mast cell density at sham acupoints in rats [118]. Acupuncture can cause an increase in degranulation of mast cells, and on the contrary, inhibition of mast degranulation can reduce acupuncture analgesia [118]. The transient receptor potential cation channel subfamily V, member 2 (TRPV2) in mast cells may act as a sensor in response to the mechanical, heat and red laser-light stimulation [119].
In clinical practice, the tip of the acupuncture needle may sometimes penetrate through the skin and deep into the muscle layer. A recent study has indicated that TRPV1 is abundant in muscle and epimysium at acupoint ST36 and it might be a mechanosensitive channel for manual acupuncture in mice [120]. Furthermore, local tissues injured by acupuncture together with immune cells can release proinflammatory factors to stimulate afferent fiber terminals [121]. Anatomical features underlying an acupoint remain unclear. It has been proposed that acupoints are sites that comprise the muscle-spindle-rich, cutaneous-receptor rich, ortendon-organ-rich properties [121].
Acupuncture analgesia
Stimulating different acupoints may cause different physiological modulations. The effects of acupuncture depend on individual status too. As to acupuncture analgesia, the endorphins theory is already a widely accepted explanation [122]. In addition, a recent review article has proposed that acupuncture activates a variety of bioactive chemicals through the spinal and supraspinal mechanisms [123]. These bioactive chemicals include: (i) opioids at the spinal and supraspinal levels, and (ii) serotonin and norepinephrine at the spinal level [124,125]. Recent animal studies have also indicated that some portion of EA analgesia is not blocked by naloxone [126]. An orexin-endocannabinoid pathway in the periaqueductal gray has been indicated [127]. Exploring non-opioid mechanisms of acupuncture may lead to the discovery of a new pharmacological target for the treatment of pain in the future (Figure 1).
Figure 1.
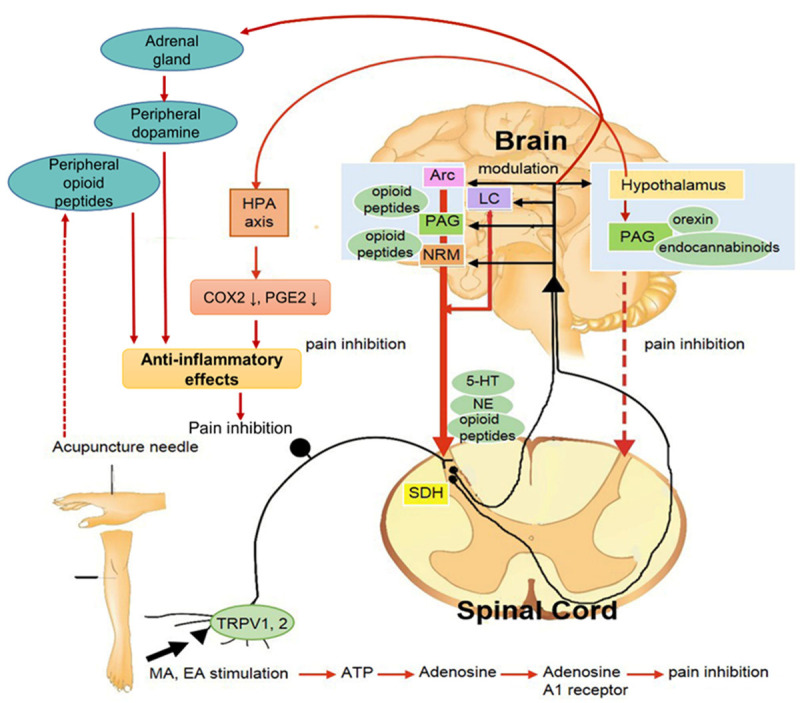
Possible neurophysiologic mechanisms underlying acupuncture analgesia. Abbreviations: Arc, arcuate nucleus; PAG, periaqueductal grey; NRM, nucleus raphe magnus; LC, locus coeruleus; ATP, adenosine triphosphate; TRPV1, transient receptor potential vanilloid 1; 5-HT, 5-hydroxytryptamine (serotonin); NE, norepinephrine; SDH, spinal cord dorsal horn; HPA axis, hypothalamic-pituitary adrenal; COX-2, cyclooxygenase-2; PGE2, prostaglandin E2; MA, manual acupuncture; EA, electroacupuncture; RCTs, randomized controlled trials. The solid line indicates the pathway that has been shown in many studies, while the dotted line represents the pathway yet to be determined.
Anti-inflammatory effects of acupuncture
Acupuncture can also exert anti-inflammatory effects by (i) affecting the hypothalamic-pituitary adrenal (HPA) axis to lower cyclooxygenase-2 (COX-2) and prostaglandin E2 (PGE2) levels and (ii) enhancing the sympathetic nervous system to cause the peripheral release of opioids [123]. Acupuncture stimulates the release of catecholamines from the adrenal gland, acting on peripheral dopamine D1 receptors to produce systemic anti-inflammatory effects [128].
Acupuncture for insomnia
Acupuncture may modulate various neurotransmitters and hormones that assist in the treatment of insomnia [101]. In this case, acupuncture inhibits sympathetic activity and modulates the endocrine system by down-regulating the HPA axis.
Acupuncture for drug addiction
In the treatment of drug addiction, the molecular mechanism of acupuncture involves the modulation of dopamine release in the nucleus accumbens, which reduces the effects of positive and negative reinforcements [129]. A recent study found that EA prevents cocaine relapse by reducing the ΔFosB and GluR2 expression in the nucleus accumbens [130].
Perspective of future acupuncture direction
The mechanistic studies of acupuncture pose numerous challenges. Some researchers assert that the innovative “i-needle” offers enhanced capabilities for exploring the biochemical pathways, using high-input information including miRNA, mRNA, metabolites and 16sr RNA-omic database [131]. They hypothesize that the perfect conjugations of those omics approaches into an i-needle can overcome the above-mentioned limitations of acupuncture needles, and enable the analysis of metagenomics, metatranscriptomics and host-microbiome relationships. However, this type of analysis is limited to collecting information at a particular time point after acupuncture and does not enable easy identification of the biomarkers associated with acupuncture.
Evaluation of the dynamic changes and real-time changes in the acupoints and the target organ is of importance. A combination of needle and microsensor as an acupuncture tool could be used along with the i-needle to investigate the mechanisms of acupuncture. Skin implantable microsensors or needle-shaped microsensors have been recently developed [132]. It has become feasible to measure real-time microenvironmental changes in many acupoints and even target organs. Using these sensors in efficacy studies, such as tests for pain thresholds, will enable us to better define the microenvironmental changes and the efficacy of acupuncture. Their results are expected to provide new insights into the mechanisms of acupuncture.
Limitation of this review
Although we included some useful meta-analyses in the literature [54,55], there are several limitations in this mini review. A meta-analysis of RCTs on acupuncture was not conducted. The specificity of acupoints was not adequately discussed in this review due to a dearth of literature about this field. For example, the ST36 is more useful for treating abdominal pain, whereas the LI4 is more appropriate for treating orofacial pain, while HT7 is, in particular, beneficial for insomnia. The rationale for the acupoints’ specificity has not been thoroughly discussed.
Conclusion
Acupuncture has been proven to be an effective treatment in pain relief with minimal risk. For IVF and some diseases, such as insomnia, opiate addiction and stroke, more high-quality RCTs are needed to confirm the efficacy of acupuncture. Progress in modern biomedical technology will eventually help us to understand the mechanisms of acupuncture.
Acknowledgements
This work was supported by grants from China Medical University, Taichung, Taiwan (CMU109-MF-50). This work was also financially supported by the “Chinese Medicine Research Center, China Medical University” from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project under the Ministry of Education (MOE) in Taiwan. We thank Professor Wen-Hwa Lee for his critical reading and Ms. Katrina PikMunn Tan for her editorial assistance.
Disclosure of conflict of interest
None.
References
- 1.World Health Organization. WHO standard acupuncture point locations in the Western Pacific Region. World Health Organization. 2008 [Google Scholar]
- 2.Yang XY, Shi GX, Li QQ, Zhang ZH, Xu Q, Liu CZ. Characterization of deqi sensation and acupuncture effect. Evid Based Complement Alternat Med. 2013;2013:319734. doi: 10.1155/2013/319734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NIH consensus conference. Acupuncture. JAMA. 1998;280:1518–1524. [PubMed] [Google Scholar]
- 4.Zhu H. Acupoints initiate the healing process. Med Acupunct. 2014;26:264–270. doi: 10.1089/acu.2014.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bannerman RH. Acupuncture: the WHO view. World Health. 1979;12:27–28. [Google Scholar]
- 6.Zhang X. Acupuncture: review and analysis of controlled clinical trials. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 7.Li Q, Zhao T, Wang X, Qiu C, Zhou B, Wang H, Wang B. Study on potential of meridian acupoints of Traditional Chinese Medicine. J Healthc Eng. 2021;2021:5599272. doi: 10.1155/2021/5599272. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.MacPherson H, Hammerschlag R. Acupuncture and the emerging evidence base: contrived controversy and rational debate. J Acupunct Meridian Stud. 2012;5:141–147. doi: 10.1016/j.jams.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 9.White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ. 2001;323:485–486. doi: 10.1136/bmj.323.7311.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim S. WHO Standard Acupuncture Point Locations. Evid Based Complement Alternat Med. 2010;7:167–168. doi: 10.1093/ecam/nep006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee AD, Hsu ESZ. Mechanisms of acupuncture analgesia. Acupuncture for pain management. Springer; 2014. pp. 73–85. [Google Scholar]
- 12.Department of Health. A literary review of curative effects of Traditional Chinese Medicine. Taipei: Committee on Chinese Medicine and Pharmacy. Executive Yuan; 2008. [Google Scholar]
- 13.Short C, Lynch M. Clinical assessment in adult patients. Clinical Pain Management: A Practical Guide. 2011;51:9. [Google Scholar]
- 14.Schug SA, Palmer GM, Scott DA, Alcock M, Halliwell R, Mott J. Acute pain management: scientific evidence. Australian and New Zealand College of Anaesthetists. 2020 [Google Scholar]
- 15.Sun Y, Gan TJ, Dubose JW, Habib AS. Acupuncture and related techniques for postoperative pain: a systematic review of randomized controlled trials. Br J Anaesth. 2008;101:151–160. doi: 10.1093/bja/aen146. [DOI] [PubMed] [Google Scholar]
- 16.Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, Glaser SE, Vallejo R. Opioid complications and side effects. Pain Physician. 2008;11(Suppl):S105–120. [PubMed] [Google Scholar]
- 17.Wu MS, Chen KH, Chen IF, Huang SK, Tzeng PC, Yeh ML, Lee FP, Lin JG, Chen C. The efficacy of acupuncture in post-operative pain management: a systematic review and meta-analysis. PLoS One. 2016;11:e0150367. doi: 10.1371/journal.pone.0150367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho HY, Chen CW, Li MC, Hsu YP, Kang SC, Liu EH, Lee KH. A novel and effective acupuncture modality as a complementary therapy to acute pain relief in inpatients with rib fractures. Biomed J. 2014;37:147–155. doi: 10.4103/2319-4170.117895. [DOI] [PubMed] [Google Scholar]
- 19.Zhang AL, Parker SJ, Smit de V, Taylor DM, Xue CC. Acupuncture and standard emergency department care for pain and/or nausea and its impact on emergency care delivery: a feasibility study. Acupunct Med. 2014;32:250–256. doi: 10.1136/acupmed-2013-010501. [DOI] [PubMed] [Google Scholar]
- 20.Grissa MH, Baccouche H, Boubaker H, Beltaief K, Bzeouich N, Fredj N, Msolli MA, Boukef R, Bouida W, Nouira S. Acupuncture vs intravenous morphine in the management of acute pain in the ED. Am J Emerg Med. 2016;34:2112–2116. doi: 10.1016/j.ajem.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 21.Beltaief K, Grissa MH, Msolli MA, Bzeouich N, Fredj N, Sakma A, Boubaker H, Bouida W, Boukef R, Nouira S. Acupuncture versus titrated morphine in acute renal colic: a randomized controlled trial. J Pain Res. 2018;11:335–341. doi: 10.2147/JPR.S136299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, Owens DK Clinical Efficacy Assessment Subcommittee of the American College of Physicians, American College of Physicians and American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 23.Lee JH, Choi TY, Lee MS, Lee H, Shin BC, Lee H. Acupuncture for acute low back pain: a systematic review. Clin J Pain. 2013;29:172–185. doi: 10.1097/AJP.0b013e31824909f9. [DOI] [PubMed] [Google Scholar]
- 24.Vas J, Aranda JM, Modesto M, Benitez-Parejo N, Herrera A, Martinez-Barquin DM, Aguilar I, Sanchez-Araujo M, Rivas-Ruiz F. Acupuncture in patients with acute low back pain: a multicentre randomised controlled clinical trial. Pain. 2012;153:1883–1889. doi: 10.1016/j.pain.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 25.Shin JS, Ha IH, Lee J, Choi Y, Kim MR, Park BY, Shin BC, Lee MS. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: a multicenter, randomized, controlled, comparative effectiveness trial. Pain. 2013;154:1030–1037. doi: 10.1016/j.pain.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 26.Qaseem A, Wilt TJ, McLean RM, Forciea MA Clinical Guidelines Committee of the American College of Physicians. Denberg TD, Barry MJ, Boyd C, Chow RD, Fitterman N, Harris RP, Humphrey LL, Vijan S. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 27.Smith CA, Collins CT, Crowther CA, Levett KM. Acupuncture or acupressure for pain management in labour. Cochrane Database Syst Rev. 2011;6:CD009232. doi: 10.1002/14651858.CD009232. [DOI] [PubMed] [Google Scholar]
- 28.Mucuk S, Baser M. Effects of noninvasive electroacupuncture on labour pain and duration. J Clin Nurs. 2014;23:1603–1610. doi: 10.1111/jocn.12256. [DOI] [PubMed] [Google Scholar]
- 29.Vixner L, Schytt E, Stener-Victorin E, Waldenstrom U, Pettersson H, Martensson LB. Acupuncture with manual and electrical stimulation for labour pain: a longitudinal randomised controlled trial. BMC Complement Altern Med. 2014;14:187. doi: 10.1186/1472-6882-14-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith CA, Collins CT, Levett KM, Armour M, Dahlen HG, Tan AL, Mesgarpour B. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020;2:CD009232. doi: 10.1002/14651858.CD009232.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108:428–441. doi: 10.1097/01.AOG.0000230214.26638.0c. [DOI] [PubMed] [Google Scholar]
- 32.Weissman AM, Hartz AJ, Hansen MD, Johnson SR. The natural history of primary dysmenorrhoea: a longitudinal study. BJOG. 2004;111:345–352. doi: 10.1111/j.1471-0528.2004.00090.x. [DOI] [PubMed] [Google Scholar]
- 33.Lefebvre G, Pinsonneault O, Antao V, Black A, Burnett M, Feldman K, Lea R, Robert M SOGC. Primary dysmenorrhea consensus guideline. J Obstet Gynaecol Can. 2005;27:1117–1146. doi: 10.1016/s1701-2163(16)30395-4. [DOI] [PubMed] [Google Scholar]
- 34.Shetty GB, Shetty B, Mooventhan A. Efficacy of acupuncture in the management of primary dysmenorrhea: a randomized controlled trial. J Acupunct Meridian Stud. 2018;11:153–158. doi: 10.1016/j.jams.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Smith CA, Zhu X, He L, Song J. Acupuncture for primary dysmenorrhoea. Cochrane Database Syst Rev. 2011:CD007854. doi: 10.1002/14651858.CD007854.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Smith CA, Armour M, Zhu X, Li X, Lu ZY, Song J. Acupuncture for dysmenorrhoea. Cochrane Database Syst Rev. 2016;4:CD007854. doi: 10.1002/14651858.CD007854.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luo F, Huang X, Liu X, Wang L, Xu N. Comparative efficacy and safety of NSAIDs-controlled acupuncture in the treatment of patients with primary dysmenorrhoea: a Bayesian network meta-analysis. J Int Med Res. 2019;47:19–30. doi: 10.1177/0300060518800609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woo HL, Ji HR, Pak YK, Lee H, Heo SJ, Lee JM, Park KS. The efficacy and safety of acupuncture in women with primary dysmenorrhea: a systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11007. doi: 10.1097/MD.0000000000011007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mayans L, Walling A. Acute migraine headache: treatment strategies. Am Fam Physician. 2018;97:243–251. [PubMed] [Google Scholar]
- 40.Coeytaux RR, Befus D. Role of acupuncture in the treatment or prevention of migraine, tension-type headache, or chronic headache disorders. Headache. 2016;56:1238–1240. doi: 10.1111/head.12857. [DOI] [PubMed] [Google Scholar]
- 41.Bendtsen L, Evers S, Linde M, Mitsikostas DD, Sandrini G, Schoenen J EFNS. EFNS guideline on the treatment of tension-type headache-report of an EFNS task force. Eur J Neurol. 2010;17:1318–1325. doi: 10.1111/j.1468-1331.2010.03070.x. [DOI] [PubMed] [Google Scholar]
- 42.Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Shin BC, Vickers A, White AR. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016;4:CD007587. doi: 10.1002/14651858.CD007587.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Vertosick EA, Vickers A, White AR. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;2016:CD001218. doi: 10.1002/14651858.CD001218.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li H, Xu QR. Effect of percutaneous electrical nerve stimulation for the treatment of migraine. Medicine (Baltimore) 2017;96:e8108. doi: 10.1097/MD.0000000000008108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Clinical Guideline Centre (UK) Headaches: diagnosis and management of headaches in young people and adults. London: Royal College of Physicians (UK); 2012. Sep, [PubMed] [Google Scholar]
- 46.Wang LP, Zhang XZ, Guo J, Liu HL, Zhang Y, Liu CZ, Yi JH, Wang LP, Zhao JP, Li SS. Efficacy of acupuncture for acute migraine attack: a multicenter single blinded, randomized controlled trial. Pain Med. 2012;13:623–630. doi: 10.1111/j.1526-4637.2012.01376.x. [DOI] [PubMed] [Google Scholar]
- 47.Lin ML, Huang CT, Lin JG, Tsai SK. A comparison between the pain relief effect of electroacupuncture, regional never block and electroacupuncture plus regional never block in frozen shoulder. Acta Anaesthesiol Sin. 1994;32:237–242. [PubMed] [Google Scholar]
- 48.Lin JG, Chen WL. Review: acupuncture analgesia in clinical trials. Am J Chin Med. 2009;37:1–18. doi: 10.1142/S0192415X09006679. [DOI] [PubMed] [Google Scholar]
- 49.Lu TW, Wei IP, Liu YH, Hsu WC, Wang TM, Chang CF, Lin JG. Immediate effects of acupuncture on gait patterns in patients with knee osteoarthritis. Chin Med J. 2010;123:165–172. [PubMed] [Google Scholar]
- 50.Cohen J. Statistical power analysis for the behavioral sciences. Academic Press; 2013. [Google Scholar]
- 51.Manyanga T, Froese M, Zarychanski R, Abou-Setta A, Friesen C, Tennenhouse M, Shay BL. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med. 2014;14:312. doi: 10.1186/1472-6882-14-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ter Riet G, Kleijnen J, Knipschild P. Acupuncture and neck pain/back pain. Huisarts Wet. 1989;32:223–227. [Google Scholar]
- 53.Ernst E, White AR. Acupuncture for back pain: a meta-analysis of randomized controlled trials. Arch Intern Med. 1998;158:2235–2241. doi: 10.1001/archinte.158.20.2235. [DOI] [PubMed] [Google Scholar]
- 54.Strauss A. Acupuncture and the treatment of chronic low-back pain: a review of the literature. Chiropractic Journal of Australia. 1999;29:112–118. [Google Scholar]
- 55.Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain. 2000;86:119–132. doi: 10.1016/s0304-3959(00)00234-7. [DOI] [PubMed] [Google Scholar]
- 56.Tulder MW VA, Cherkin DC, Berman B, Lao L, Koes BW. Acupuncture for low back pain. Cochrane Database Syst Rev. 2000:CD001351. doi: 10.1002/14651858.CD001351. [DOI] [PubMed] [Google Scholar]
- 57.Henderson H. Acupuncture: evidence for its use in chronic low back pain. Br J Nurs. 2002;11:1395–1403. doi: 10.12968/bjon.2002.11.21.10931. [DOI] [PubMed] [Google Scholar]
- 58.Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain. Ann Intern Med. 2003;138:898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 59.Yuan J, Purepong N, Kerr D, McDonough S. Acupuncture for non-specific low back pain: a systematic review of RCTs. Focus Altern Complement Ther. 2004;9:61–61. [Google Scholar]
- 60.Manheimer E, White A, Berman B, Forys K, Ernst E. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142:651–663. doi: 10.7326/0003-4819-142-8-200504190-00014. [DOI] [PubMed] [Google Scholar]
- 61.Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, Irnich D, Walther HU, Melchart D, Willich SN. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166:450–457. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- 62.Thomas KJ, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell MJ, Roman M, Walters SJ, Nicholl J. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ. 2006;333:623. doi: 10.1136/bmj.38878.907361.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lam M, Galvin R, Curry P. Effectiveness of acupuncture for nonspecific chronic low back pain: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2013;38:2124–2138. doi: 10.1097/01.brs.0000435025.65564.b7. [DOI] [PubMed] [Google Scholar]
- 64.Trigkilidas D. Acupuncture therapy for chronic lower back pain: a systematic review. Ann R Coll Surg Engl. 2010;92:595–598. doi: 10.1308/003588410X12699663904196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu L, Skinner M, McDonough S, Mabire L, Baxter GD. Acupuncture for low back pain: an overview of systematic reviews. Evid Based Complement Alternat Med. 2015;2015:328196. doi: 10.1155/2015/328196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tang S, Mo Z, Zhang R. Acupuncture for lumbar disc herniation: a systematic review and meta-analysis. Acupunct Med. 2018;36:62–70. doi: 10.1136/acupmed-2016-011332. [DOI] [PubMed] [Google Scholar]
- 67.Xiang Y, He JY, Tian HH, Cao BY, Li R. Evidence of efficacy of acupuncture in the management of low back pain: a systematic review and meta-analysis of randomised placebo- or sham-controlled trials. Acupunct Med. 2020;38:15–24. doi: 10.1136/acupmed-2017-011445. [DOI] [PubMed] [Google Scholar]
- 68.Yancey JR, Sheridan R, Koren KG. Chronic daily headache: diagnosis and management. Am Fam Physician. 2014;89:642–648. [PubMed] [Google Scholar]
- 69.Ha H, Gonzalez A. Migraine headache prophylaxis. Am Fam Physician. 2019;99:17–24. [PubMed] [Google Scholar]
- 70.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for tension-type headache. Cochrane Database Syst Rev. 2009;4:CD007587. doi: 10.1002/14651858.CD007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009:CD001218. doi: 10.1002/14651858.CD001218.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Melchart D, Linde K, Fischer P, White A, Allais G, Vickers A, Berman B. Acupuncture for recurrent headaches: a systematic review of randomized controlled trials. Cephalalgia. 1999;19:779–786. doi: 10.1046/j.1468-2982.1999.1909779.x. [DOI] [PubMed] [Google Scholar]
- 73.Vernon H, McDermaid CS, Hagino C. Systematic review of randomized clinical trials of complementary/alternative therapies in the treatment of tension-type and cervicogenic headache. Complement Ther Med. 1999;7:142–155. doi: 10.1016/s0965-2299(99)80122-8. [DOI] [PubMed] [Google Scholar]
- 74.Manias P, Tagaris G, Karageorgiou K. Acupuncture in headache: a critical review. Clin J Pain. 2000;16:334–339. doi: 10.1097/00002508-200012000-00010. [DOI] [PubMed] [Google Scholar]
- 75.Davis MA, Kononowech RW, Rolin SA, Spierings EL. Acupuncture for tension-type headache: a meta-analysis of randomized, controlled trials. J Pain. 2008;9:667–677. doi: 10.1016/j.jpain.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 76.Melchart D, Linde K, Fischer P, Berman B, White A, Vickers A, Allais G. Acupuncture for idiopathic headache. Cochrane Database Syst Rev. 2001:CD001218. doi: 10.1002/14651858.CD001218. [DOI] [PubMed] [Google Scholar]
- 77.Sun Y, Gan TJ. Acupuncture for the management of chronic headache: a systematic review. Anesth Analg. 2008;107:2038–2047. doi: 10.1213/ane.0b013e318187c76a. [DOI] [PubMed] [Google Scholar]
- 78.White A, Foster NE, Cummings M, Barlas P. Acupuncture treatment for chronic knee pain: a systematic review. Rheumatology (Oxford) 2007;46:384–390. doi: 10.1093/rheumatology/kel413. [DOI] [PubMed] [Google Scholar]
- 79.Kwon YD, Pittler MH, Ernst E. Acupuncture for peripheral joint osteoarthritis: a systematic review and meta-analysis. Rheumatology (Oxford) 2006;45:1331–1337. doi: 10.1093/rheumatology/kel207. [DOI] [PubMed] [Google Scholar]
- 80.Manheimer E, Cheng K, Linde K, Lao L, Yoo J, Wieland S, van der Windt DA, Berman BM, Bouter LM. Acupuncture for peripheral joint osteoarthritis. Cochrane Database Syst Rev. 2010:CD001977. doi: 10.1002/14651858.CD001977.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Manheimer E, Cheng K, Wieland LS, Shen X, Lao L, Guo M, Berman BM. Acupuncture for hip osteoarthritis. Cochrane Database Syst Rev. 2018;5:CD013010. doi: 10.1002/14651858.CD013010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lin X, Huang K, Zhu G, Huang Z, Qin A, Fan S. The effects of acupuncture on chronic knee pain due to osteoarthritis: a meta-analysis. J Bone Joint Surg Am. 2016;98:1578–1585. doi: 10.2106/JBJS.15.00620. [DOI] [PubMed] [Google Scholar]
- 83.Chen N, Wang J, Mucelli A, Zhang X, Wang C. Electro-acupuncture is beneficial for knee osteoarthritis: the evidence from meta-analysis of randomized controlled trials. Am J Chin Med. 2017;45:965–985. doi: 10.1142/S0192415X17500513. [DOI] [PubMed] [Google Scholar]
- 84.Zhang Q, Yue J, Golianu B, Sun Z, Lu Y. Updated systematic review and meta-analysis of acupuncture for chronic knee pain. Acupunct Med. 2017;35:392–403. doi: 10.1136/acupmed-2016-011306. [DOI] [PubMed] [Google Scholar]
- 85.Li S, Xie P, Liang Z, Huang W, Huang Z, Ou J, Lin Z, Chai S. Efficacy comparison of five different acupuncture methods on pain, stiffness, and function in osteoarthritis of the knee: a network meta-analysis. Evid Based Complement Alternat Med. 2018;2018:1638904. doi: 10.1155/2018/1638904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sun N, Tu JF, Lin LL, Li YT, Yang JW, Shi GX, Lao LX, Liu CZ. Correlation between acupuncture dose and effectiveness in the treatment of knee osteoarthritis: a systematic review. Acupunct Med. 2019;37:261–267. doi: 10.1136/acupmed-2017-011608. [DOI] [PubMed] [Google Scholar]
- 87.Li J, Li YX, Luo LJ, Ye J, Zhong DL, Xiao QW, Zheng H, Geng CM, Jin RJ, Liang FR. The effectiveness and safety of acupuncture for knee osteoarthritis: an overview of systematic reviews. Medicine (Baltimore) 2019;98:e16301. doi: 10.1097/MD.0000000000016301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sun YQ, Zheng S, Yu J, Yan K, Tian W. Effect of total disc replacement on atypical symptoms associated with cervical spondylosis. Eur Spine J. 2013;22:1553–1557. doi: 10.1007/s00586-013-2785-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Plastaras CT, Schran S, Kim N, Sorosky S, Darr D, Chen MS, Lansky R. Complementary and alternative treatment for neck pain: chiropractic, acupuncture, TENS, massage, yoga, Tai Chi, and Feldenkrais. Phys Med Rehabil Clin N Am. 2011;22:521–537. doi: 10.1016/j.pmr.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 90.Sahin N, Ozcan E, Sezen K, Karatas O, Issever H. Efficacy of acupunture in patients with chronic neck pain-a randomised, sham controlled trial. Acupunct Electrother Res. 2010;35:17–27. doi: 10.3727/036012910803860959. [DOI] [PubMed] [Google Scholar]
- 91.He D, Hostmark AT, Veiersted KB, Medbo JI. Effect of intensive acupuncture on pain-related social and psychological variables for women with chronic neck and shoulder pain--an RCT with six month and three year follow up. Acupunct Med. 2005;23:52–61. doi: 10.1136/aim.23.2.52. [DOI] [PubMed] [Google Scholar]
- 92.Trinh K, Graham N, Irnich D, Cameron ID, Forget M. Acupuncture for neck disorders. Cochrane Database Syst Rev. 2016:CD004870. doi: 10.1002/14651858.CD004870.pub4. [DOI] [PubMed] [Google Scholar]
- 93.Seo SY, Lee KB, Shin JS, Lee J, Kim MR, Ha IH, Ko Y, Lee YJ. Effectiveness of acupuncture and electroacupuncture for chronic neck pain: a systematic review and meta-analysis. Am J Chin Med. 2017;45:1573–1595. doi: 10.1142/S0192415X17500859. [DOI] [PubMed] [Google Scholar]
- 94.Herin F, Vezina M, Thaon I, Soulat JM, Paris C ESTEV group. Predictors of chronic shoulder pain after 5 years in a working population. Pain. 2012;153:2253–2259. doi: 10.1016/j.pain.2012.07.024. [DOI] [PubMed] [Google Scholar]
- 95.Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: epidemiology, pathophysiology, and diagnosis. Am J Orthop. 2005;34:5–9. [PubMed] [Google Scholar]
- 96.Molsberger AF, Schneider T, Gotthardt H, Drabik A. German randomized acupuncture trial for chronic shoulder pain (GRASP)-a pragmatic, controlled, patient-blinded, multi-centre trial in an outpatient care environment. Pain. 2010;151:146–154. doi: 10.1016/j.pain.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 97.Guerra de Hoyos JA, Martín MDCA, Leon EBYB, Lopez MV, López TM, Morilla FAV, Moreno MJG. Randomised trial of long term effect of acupuncture for shoulder pain. Pain. 2004;112:289–298. doi: 10.1016/j.pain.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 98.Itoh K, Saito S, Sahara S, Naitoh Y, Imai K, Kitakoji H. Randomized trial of trigger point acupuncture treatment for chronic shoulder pain: a preliminary study. J Acupunct Meridian Stud. 2014;7:59–64. doi: 10.1016/j.jams.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 99.Wang KF, Zhang LJ, Lu F, Lu YH, Yang CH. Can Ashi points stimulation have specific effects on shoulder pain? A systematic review of randomized controlled trials. Chin J Integr Med. 2016;22:467–472. doi: 10.1007/s11655-015-2107-4. [DOI] [PubMed] [Google Scholar]
- 100.Liu C, Xi H, Wu W, Wang X, Qin S, Zhao Y, Zheng S, Wan Q, Xu L. Placebo effect of acupuncture on insomnia: a systematic review and meta-analysis. Ann Palliat Med. 2020;9:19–29. doi: 10.21037/apm.2019.11.15. [DOI] [PubMed] [Google Scholar]
- 101.Yeung WF, Chung KF, Tjen-A-Looi S, Longhurst J, Lao L. Acupuncture as a potential treatment for insomnia. Science. 2015;350:S84–S85. [Google Scholar]
- 102.Cheuk DK, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia. Cochrane Database Syst Rev. 2012:CD005472. doi: 10.1002/14651858.CD005472.pub2. [DOI] [PubMed] [Google Scholar]
- 103.Cui CL, Wu LZ, Luo F, Han JS. Acupuncture for the treatment of drug addiction. Sheng Li Ke Xue Jin Zhan. 2008;39:325–330. [PubMed] [Google Scholar]
- 104.Stuyt EB, Voyles CA. The national acupuncture detoxification association protocol, auricular acupuncture to support patients with substance abuse and behavioral health disorders: current perspectives. Subst Abuse Rehabil. 2016;7:169–180. doi: 10.2147/SAR.S99161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grant S, Kandrack R, Motala A, Shanman R, Booth M, Miles J, Sorbero M, Hempel S. Acupuncture for substance use disorders: a systematic review and meta-analysis. Drug Alcohol Depend. 2016;163:1–15. doi: 10.1016/j.drugalcdep.2016.02.034. [DOI] [PubMed] [Google Scholar]
- 106.McLellan AT, Grossman DS, Blaine JD, Haverkos HW. Acupuncture treatment for drug abuse: a technical review. J Subst Abuse Treat. 1993;10:569–576. doi: 10.1016/0740-5472(93)90061-6. [DOI] [PubMed] [Google Scholar]
- 107.Lin JG, Chan YY, Chen YH. Acupuncture for the treatment of opiate addiction. Evid Based Complement Alternat Med. 2012;2012:739045. doi: 10.1155/2012/739045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chan YY, Lo WY, Li TC, Shen LJ, Yang SN, Chen YH, Lin JG. Clinical efficacy of acupuncture as an adjunct to methadone treatment services for heroin addicts: a randomized controlled trial. Am J Chin Med. 2014;42:569–586. doi: 10.1142/S0192415X14500372. [DOI] [PubMed] [Google Scholar]
- 109.Jiang DZJ, Wang FF, Ye YH, Zhang R, Qu F. To make Traditional Chinese medicine and in vitro fertilization a good partner. Science. 2015 In press. [Google Scholar]
- 110.Hullender Rubin LE. Point of influence: what is the role of acupuncture in in vitro fertilization outcomes? Med Acupunct. 2019;31:329–333. doi: 10.1089/acu.2019.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shih CC, Liao CC, Sun MF, Su YC, Wen CP, Morisky DE, Sung FC, Hsu CY, Lin JG. A retrospective cohort study comparing stroke recurrence rate in ischemic stroke patients with and without acupuncture treatment. Medicine (Baltimore) 2015;94:e1572. doi: 10.1097/MD.0000000000001572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wu P, Mills E, Moher D, Seely D. Acupuncture in poststroke rehabilitation: a systematic review and meta-analysis of randomized trials. Stroke. 2010;41:e171–9. doi: 10.1161/STROKEAHA.109.573576. [DOI] [PubMed] [Google Scholar]
- 113.Lin JG, Chen CH, Huang YC, Chen YH. How to design the control group in randomized controlled trials of acupuncture? Evid Based Complement Alternat Med. 2012;2012:875284. doi: 10.1155/2012/875284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Liang FZL, Zeng F, Li Y, Wu X, Ren Y, Wu Q, Zheng H, Yang J, Yang M. Exploring acupoint specificity: progress in clinical and mechanistic studies in China. Science. 2015 In press. [Google Scholar]
- 115.Villanueva L, Le Bars D. The activation of bulbo-spinal controls by peripheral nociceptive inputs: diffuse noxious inhibitory controls. Biol Res. 1995;28:113–125. [PubMed] [Google Scholar]
- 116.He JR, Yu SG, Tang Y, Illes P. Purinergic signaling as a basis of acupuncture-induced analgesia. Purinergic Signal. 2020;16:297–304. doi: 10.1007/s11302-020-09708-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tang Y, Yin HY, Liu J, Rubini P, Illes P. P2X receptors and acupuncture analgesia. Brain Res Bull. 2019;151:144–152. doi: 10.1016/j.brainresbull.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 118.Zhang D, Ding G, Shen X, Yao W, Zhang Z, Zhang Y, Lin J, Gu Q. Role of mast cells in acupuncture effect: a pilot study. Explore (NY) 2008;4:170–177. doi: 10.1016/j.explore.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 119.Zhang D, Spielmann A, Wang L, Ding G, Huang F, Gu Q, Schwarz W. Mast-cell degranulation induced by physical stimuli involves the activation of transient-receptor-potential channel TRPV2. Physiol Res. 2012;61:113–124. doi: 10.33549/physiolres.932053. [DOI] [PubMed] [Google Scholar]
- 120.Wu SY, Chen WH, Hsieh CL, Lin YW. Abundant expression and functional participation of TRPV1 at Zusanli acupoint (ST36) in mice: mechanosensitive TRPV1 as an “acupuncture-responding channel”. BMC Complement Altern Med. 2014;14:96. doi: 10.1186/1472-6882-14-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang ZJ, Wang XM, McAlonan GM. Neural acupuncture unit: a new concept for interpreting effects and mechanisms of acupuncture. Evid Based Complement Alternat Med. 2012:429412. doi: 10.1155/2012/429412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26:17–22. doi: 10.1016/s0166-2236(02)00006-1. [DOI] [PubMed] [Google Scholar]
- 123.Zhang R, Lao L, Ren K, Berman BM. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120:482–503. doi: 10.1097/ALN.0000000000000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chang FC, Tsai HY, Yu MC, Yi PL, Lin JG. The central serotonergic system mediates the analgesic effect of electroacupuncture on ZUSANLI (ST36) acupoints. J Biomed Sci. 2004;11:179–185. doi: 10.1007/BF02256561. [DOI] [PubMed] [Google Scholar]
- 125.Kim SK, Park JH, Bae SJ, Kim JH, Hwang BG, Min BI, Park DS, Na HS. Effects of electroacupuncture on cold allodynia in a rat model of neuropathic pain: mediation by spinal adrenergic and serotonergic receptors. Exp Neurol. 2005;195:430–436. doi: 10.1016/j.expneurol.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 126.Huang C, Wang Y, Han JS, Wan Y. Characteristics of electroacupuncture-induced analgesia in mice: variation with strain, frequency, intensity and opioid involvement. Brain Res. 2002;945:20–25. doi: 10.1016/s0006-8993(02)02503-9. [DOI] [PubMed] [Google Scholar]
- 127.Chen YH, Lee HJ, Lee MT, Wu YT, Lee YH, Hwang LL, Hung MS, Zimmer A, Mackie K, Chiou LC. Median nerve stimulation induces analgesia via orexin-initiated endocannabinoid disinhibition in the periaqueductal gray. Proc Natl Acad Sci U S A. 2018;115:E10720–E10729. doi: 10.1073/pnas.1807991115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Torres-Rosas R, Yehia G, Pena G, Mishra P, del Rocio Thompson-Bonilla M, Moreno-Eutimio MA, Arriaga-Pizano LA, Isibasi A, Ulloa L. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20:291–295. doi: 10.1038/nm.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Motlagh FE, Ibrahim F, Rashid RA, Seghatoleslam T, Habil H. Acupuncture therapy for drug addiction. Chin Med. 2016;11:16. doi: 10.1186/s13020-016-0088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nguyen ATM, Quach TVB, Kotha P, Chien SY, MacDonald IJ, Lane HY, Tu CH, Lin JG, Chen YH. Electroacupuncture prevents cocaine-induced conditioned place preference reinstatement and attenuates DeltaFosB and GluR2 expression. Sci Rep. 2021;11:13694. doi: 10.1038/s41598-021-93014-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nardini C, Carrara S, Liu Y, Devescovi V, Lu Y, Zhou X. i-Needle: detecting the biological mechanisms of acupuncture. Science. 2014;346:S21–S22. [Google Scholar]
- 132.Tang L, Du D, Yang F, Liang Z, Ning Y, Wang H, Zhang GJ. Preparation of graphene-modified acupuncture needle and its application in detecting neurotransmitters. Sci Rep. 2015;5:11627. doi: 10.1038/srep11627. [DOI] [PMC free article] [PubMed] [Google Scholar]


