Abstract
Objective: To investigate factors influencing psychological distress and the effect of stepwise psychological care on the quality of life in patients undergoing chemotherapy after breast cancer surgery. Methods: A retrospective study was conducted on 96 patients undergoing chemotherapy after breast cancer surgery. The patients were evenly divided into a routine care group (control group) and a stepwise psychological care group (observation group) according to the care method. The correlation between the psychological distress and the Self-Rating Anxiety Scale (SAS) score was investigated. The impact of care intervention on the psychological distress, SAS score, and the quality of life of patients before and after intervention were explored. Relevant factors that affect the psychological distress of patients undergoing chemotherapy after breast cancer surgery were also investigated. Results: A univariate analysis showed that age, residence, monthly income, education level, medical insurance status, occupation, surgery method, and anxiety score all contributed to the degree of psychological distress in patients with breast cancer mastectomy (all P<0.05). A multivariate regression analysis demonstrated that young age, low monthly income, no medical insurance, mastectomy, and high SAS score were risk factors for the psychological distress of patients who underwent mastectomy (all P<0.05). The psychological distress was positively correlated with anxiety scores of patients undergoing chemotherapy after breast cancer surgery (r=0.249, P=0.005). Both psychological distress and anxiety scores of the observation group after stepwise psychological care were significantly lower than those before treatment and those of the control group (both P<0.05). After treatment, both groups of patients showed better scores in additional concerning items, social/family well-being, functional well-being, physical well-being, emotional well-being, and overall quality of life than before treatment (all P<0.05). Of note, the observation group demonstrated better quality of life than that of the control group. Conclusion: Age, low monthly income, radical mastectomy, and no medical insurance prior to undergoing chemotherapy after breast cancer surgery are independent factors that affect psychological distress. The distress was positively correlated with anxiety. Thus, stepwise psychological care may alleviate patients’ psychological distress and anxiety.
Keywords: Breast cancer, mastectomy, chemotherapy, psychological distress, stepwise psychological care, anxiety, influencing factors
Introduction
Breast cancer is one of the most common cancers in women. The morbidity of breast cancer is as high as 11.4%, resulting in a death rate of 6.7% [1-3]. Studies have shown that the incidence of breast cancer is increasing year by year including in younger women [4]. Currently, mastectomy is a conventional treatment method for prolonging the survival of breast cancer patients, and postoperative adjuvant chemotherapy is an important strategy to control the disease progression and prevent postoperative relapse [5,6]. A previous study reported that patients with cancer were under tremendous psychological stress, and long-term stress can easily lead to depression, anxiety, or even suicidal tendencies in patients [7]. As a secondary sex characteristic, changes in the shape of breasts caused by surgery have a psychological impact on patients [8]. Hair loss and adverse effects during postoperative chemotherapy also have an adverse effect on patients’ mental health [9,10]. The incidence of mental illness in breast cancer patients was reported to be 10%-20%, and the incidence was much higher in breast cancer patients with mastectomy [11]. Therefore, psychological problems of breast cancer patients are attracting more attention.
The distress thermometer (DT) is an evaluation and screening tool that reflects the degree of psychological distress of patients [12]. A study revealed that psychological distress was positively correlated with patients’ anxiety [12]. Stepwise psychological care is a systematic psychological therapy that plays important roles in alleviating distress, regulating patients’ emotions, and making patients adapt to clinical treatment [13]. The care model has been widely used among cancer patients in recent years. At present, studies have reported that the psychological distress of patients undergoing chemotherapy after breast cancer surgery is correlated with their age, non-breast-conserving surgery, and clinical stage. However, so far no research has been conducted to study the effect of stepwise care on the psychological distress of patients undergoing chemotherapy after breast cancer surgery [14]. This study aimed to investigate influencing factors of the psychological distress and explore the effect of stepwise psychological care on the psychological distress and anxiety of patients after breast cancer surgery.
Materials and methods
General information
A retrospective study was conducted on 96 patients undergoing breast cancer mastectomy in the breast surgery department of Affiliated Hospital of Guangdong Medical University from January 2018 to December 2020. Patients were divided into a routine care group (control group) and a stepwise psychological care group (observation group), with 48 patients in each group. The patients had an age of 26-72 years old and an average age of 48.6±9.9 years old. All participants signed an informed consent form. This study was approved by the Ethics Committee of Affiliated Hospital of Guangdong Medical University.
Inclusion and exclusion criteria
Inclusion criteria: 1) Patients with breast cancer and TNM staging in accordance with Guideline for Breast Cancer, Chinese Anti-Cancer Association (CACA) [15]. 2) Patients with an age above 18 years-old; 3) Patients who underwent radical mastectomy for breast cancer; 4) Patients who underwent chemotherapy after surgery. Exclusion criteria: 1) Patients with incomplete clinical data; 2) Patients with severe heart, liver, kidney and other diseases; 3) Patients with mental illness or cerebrovascular disease who cannot cooperate; 4) Patients with inconvenient follow-up; 5) Patients with other cancers.
Methods
Collection of general data and relevant information
First, general data of patients were collected in the form of questionnaires, including: the age of the patient, education level, residence, family monthly income, payment method, current marital status, tumor staging, etc.
Randomization of selected patients after the questionnaire survey
Routine care
1) Patients underwent routine chemotherapy after the mastectomy, during which vital signs were checked three-times a day [16]. Any progression of the disease should be reported to the doctor in time; 2) It was assured that the ward was comfortable and tidy; 3) The diet should be carefully prepared according to the specific condition of individuals, avoiding spicy food; 4) Treatment guidance for the administration of chemotherapy drugs was introduced, including the dosage, time, and adverse effects that may occur.
Stepwise psychological care
On the basis of routine care, the observation group was given stepwise psychological care. The researchers collected and analyzed the clinical data and proposed a stepwise psychological care plan according to the psychological characteristics and the cause of disease for patients after breast cancer surgery. Based on the step, course, content, and strategy, the stepwise psychological care consisted of an observation period, guidance period, face-to-face instruction period, and professional intervention period. For the observation period, after admission, routine health education was given to help the patients better understand their ability of daily life and self-care. The patients’ psychological anxiety or depression and psychological distress were observed. They were also informed to contact the doctor and nurse in time in case of any question in order to establish a harmonious nurse-patient relationship. For the guidance period, a WeChat group was established to give the patients instructions for 10-15 minutes every week after their discharge, to understand the needs of patients for out-of-hospital care, and find out major problems and concerns faced by patients. For example, hygiene of the surgical area, rest and exercise, and prevention of postoperative complications, were considered and strategies and plans were provided to solve these concerns. This reduced patients’ anxiety to a large extent, as well as enhanced their abilities of cognition, judgment, choice making, and emotional understanding. For the face-to-face instruction period, the intervention followed the guidelines of US authoritative “Home Care Manual for Cancer”, which included symptom knowledge and management methods. In this period, the nursing staff focused on practical skills and aimed to guide patients to perform functional exercises of the upper limbs on the surgical side in order to promote postoperative blood circulation and chemotherapy. This also helped patients to understand the precautions and to help them maintain a good mood and socialize. The intervention course lasted for 1 hour each time when patients revisited the hospital every week. For the professional intervention period, in case the psychological distress continued or was aggravated after the intervention, the mental health doctors were able to strengthen the intervention, in which one-to-one counseling was adopted to understand the patients’ problems, capture important information, guide patients to have faith in chemotherapy and its efficacy, and talk about the concerns or problems during chemotherapy. If symptoms were severe, patients could be transferred to a psychiatrist for psychotherapy.
Outcome measures
(1) A univariate analysis and a multivariate logistic regression were conducted to analyze the related factors affecting the psychological distress of patients undergoing chemotherapy after breast cancer surgery.
(2) A correlation analysis was applied to study the correlation between the degree of psychological distress and SAS score before care intervention.
(3) The effects of care intervention on patients’ psychological distress and SAS scores were investigated. The distress thermometer (DT) was used to measure patients’ psychological distress level, with a scale of 0-10 (0: no distress and 10: extreme distress, where ≥4 indicated moderate to severe psychological distress, while <4 indicated normal mood fluctuation). Patients’ anxiety was evaluated by using Self-rating Anxiety Scale (SAS), which contained 20 items with 1-4 points per item [12]. The sum of scores indicated the degree of anxiety. (The cut-off value of SAS standard score was 50 points, in which 50-59 points were considered mild anxiety, 60-69 points were moderate anxiety, and 70 points or more were severe anxiety [8].
(4) The quality of life was evaluated before and after treatment by the functional assessment of cancer therapy-breast (FACT-G) [8]. The FACT-G contains 5 domains and 36 items, including functional well-being (7 items), social/family well-being (7 items), physical well-being (7 items), emotional well-being (6 items) and additional concerning items (9 items). Each item was rated on a 5-point scale, and the points in each domain were added to get the total points. Higher points indicated a better quality of life.
Statistical methods
SPSS 17.0 statistical software was used to analyze the data. Continuous variables conforming to a normal distribution and homogeneity of variances were presented as mean ± standard deviation (x̅ ± sd), which were analyzed by independent sample t test between groups and paired sample t test for before and after comparison within groups. Multi-group comparisons were done by one-way analysis of variance (ANOVA) combined with Bonferroni post hoc test. The counted data was analyzed by Pearson Chi-square test. The bivariate correlation was analyzed by Pearson correlation coefficient. Logistic regression analysis was applied to screen for risk factors affecting the psychological distress of patients undergoing chemotherapy after breast cancer surgery. A univariate analysis was conducted to identify variables with between-group differences, and forward stepwise selection (Ward) was used for variable screening. The inclusion level was 0.05 and the exclusion level was 0.1. The odds ratio (OR) was used to represent the risk of increased psychological distress, and the difference was considered statistically significant when P<0.05.
Results
Comparison of general information between the two groups of patients
There were no significant differences in terms of age, address, monthly income, education level, marital status, medical insurance status, tumor stage, occupation, surgery method, psychological distress, and anxiety score between the two groups of patients at the admission (all P>0.05; Table 1).
Table 1.
General information in the two groups of patients
| Category | Observation group (n=48) | Control group (n=48) | χ2/t | P |
|---|---|---|---|---|
| Age (n) | 0.168 | 0.919 | ||
| 18-40 | 12 | 11 | ||
| 41-60 | 25 | 27 | ||
| >61 | 11 | 10 | ||
| Residence (n) | 0.686 | 0.408 | ||
| Urban | 30 | 26 | ||
| Rural | 18 | 22 | ||
| Monthly income (n) | 0.188 | 0.665 | ||
| ≤5000 CNY | 15 | 17 | ||
| >5000 CNY | 33 | 31 | ||
| Education level (n) | 0.784 | 0.853 | ||
| Elementary school and below | 11 | 12 | ||
| Middle and high school | 19 | 15 | ||
| College | 10 | 11 | ||
| College and above | 8 | 10 | ||
| Marital status (n) | 1.126 | 0.771 | ||
| Unmarried | 10 | 13 | ||
| Married | 32 | 27 | ||
| Divorced | 4 | 5 | ||
| Widowed | 2 | 3 | ||
| Medical insurance status (n) | 0.547 | 0.761 | ||
| No insurance | 10 | 13 | ||
| Medical insurance for employees or residents | 32 | 30 | ||
| Commercial insurance | 6 | 5 | ||
| Tumor stage (n) | 0.858 | 0.651 | ||
| I | 6 | 4 | ||
| II | 32 | 36 | ||
| III | 10 | 8 | ||
| Occupation (n) | 0.048 | 0.827 | ||
| Yes | 32 | 33 | ||
| No | 16 | 15 | ||
| Surgery method (n) | 0.194 | 0.660 | ||
| Modified radical mastectomy | 34 | 32 | ||
| Breast-conserving surgery or modified reconstruction | 14 | 16 | ||
| Psychological distress (point) | 4.61±1.86 | 4.49±1.79 | 0.322 | 0.748 |
| SAS score (point) | 54.25±9.54 | 55.27±10.35 | 0.502 | 0.617 |
Note: SAS: self-rating anxiety scale.
Factors influencing psychological distress in patients undergoing chemotherapy after breast cancer surgery
The average score of psychological distress of patients undergoing chemotherapy after breast cancer surgery was 4.57±1.81. A univariate analysis of the psychological distress of these patients showed that age, residence, monthly income, education level, medical insurance status, occupation, surgery method, and anxiety score wereall factors contributing to psychological distress (all P<0.05; Table 2).
Table 2.
Factors influencing psychological distress in patients undergoing chemotherapy after breast cancer surgery
| Category | Case | Degree of psychological distress (point) | t/F | P |
|---|---|---|---|---|
| Age (Y) | 8.504 | <0.001 | ||
| 18-40 | 23 | 5.61±1.83 | ||
| 41-60 | 52 | 4.54±1.81a | ||
| 61 | 21 | 3.52±1.03aaa,b | ||
| Residence (n) | 2.154 | 0.035 | ||
| Urban | 56 | 4.23±1.60 | ||
| Rural | 40 | 5.05±1.99 | ||
| Monthly income (n) | 2.419 | 0.018 | ||
| ≤5000 CNY | 32 | 5.19±1.97 | ||
| >5000 CNY | 64 | 4.27±1.65 | ||
| Education level (n) | 6.928 | <0.001 | ||
| Elementary school and below | 23 | 5.61±1.81 | ||
| Middle and high school | 34 | 4.62±1.76c | ||
| College | 21 | 4.20±1.94c | ||
| College and above | 18 | 3.63±1.01ccc,d | ||
| Marital status (n) | 0.343 | 0.567 | ||
| Unmarried | 23 | 4.65±1.82 | ||
| Married | 59 | 4.58±1.76 | ||
| Divorced | 9 | 4.49±1.92 | ||
| Widowed | 5 | 4.54±1.78 | ||
| Medical insurance status (n) | 6.459 | 0.002 | ||
| No insurance | 23 | 5.35±1.80 | ||
| Medical insurance for employees or residents | 62 | 4.35±1.80e | ||
| Commercial insurance | 11 | 4.18±1.47e | ||
| Tumor stage (n) | 0.872 | 0.345 | ||
| I | 10 | 4.62±1.82 | ||
| II | 68 | 4.56±1.67 | ||
| III | 18 | 4.76±1.92 | ||
| Occupation (n) | 2.660 | 0.009 | ||
| Yes | 65 | 4.21±1.60 | ||
| No | 31 | 5.20±1.98 | ||
| Surgery method (n) | 2.174 | 0.032 | ||
| Modified radical mastectomy | 66 | 5.12±1.85 | ||
| Breast-conserving surgery or modified reconstruction | 30 | 4.26±1.67 | ||
| SAS score (point) | 2.956 | 0.004 | ||
| <50 | 32 | 4.53±1.74 | ||
| ≥50 | 64 | 5.32±1.97 |
Note: compared with 18-40 years old;
P<0.05;
P<0.001.
Compared with 41-60 years old;
P<0.05.
Compared with elementary school and below;
P<0.05;
P<0.001.
Compared with middle and high school;
P<0.05.
Compared with self-finance;
P<0.05.
SAS: Self-rating Anxiety Scale.
Multivariate logistic regression analysis of risk factors for psychological distress in patients undergoing chemotherapy after breast cancer surgery
A multivariate regression analysis demonstrated that age, monthly income, medical insurance status, surgery method, and SAS score were factors influencing the psychological distress of patients after breast cancer surgery (all P<0.05), among which the OR value of age was less than 1, while OR values of monthly payment, medical insurance status, surgery method, and SAS score were all above 1. Young age, low monthly income, no medical insurance, mastectomy, and high SAS score were risk factors for psychological distress (Tables 3, 4).
Table 3.
Assignment table of independent variables of influencing factors on psychological distress in patients undergoing chemotherapy after breast cancer surgery
| Factor | Independent variable | Value |
|---|---|---|
| Age (Y) | X1 | ≤60=1, >60=0 |
| Residence | X2 | rural=1, urban=0 |
| Monthly income (CNY) | X4 | ≤5000=1, >5000=0 |
| Education level | X5 | high school and below =1, college and above =0 |
| Medical insurance status | X6 | self-finance =1, medical insurance or commercial insurance =0 |
| Occupation | X7 | yes =1, no =0 |
| Surgery method | X8 | modified radical mastectomy =1, breast-conserving surgery or modified reconstruction =0 |
| SAS score (point) | X9 | ≥50=1, <50=0 |
Note: SAS: Self-rating Anxiety Scale.
Table 4.
Multivariate logistic regression analysis of psychological distress in breast cancer patients undergoing chemotherapy
| Factor | β | SE | Wald value | OR value (95% CI) | P |
|---|---|---|---|---|---|
| Age (Y) | 1.819 | 0.802 | 6.632 | 0.157 (0.051-0.624) | 0.025 |
| Residence | 0.813 | 0.815 | 1.063 | 2.269 (0.501-10.269) | 0.312 |
| Monthly income (CNY) | 0.308 | 0.846 | 12.688 | 0.072 (0.036-0.239) | <0.001 |
| Education level | 1.242 | 0.732 | 2.732 | 3.258 (0.802-12.265) | 0.129 |
| Medical insurance status | 1.852 | 0.736 | 5.696 | 5.109 (1.403-21.364) | 0.036 |
| Occupation | 0.196 | 0.732 | 0.068 | 0.842 (0.196-3.539) | 0.785 |
| Surgery method | 1.956 | 0.754 | 5.491 | 5.017 (1.398-19.254) | 0.031 |
| SAS score (point) | 1.983 | 0.843 | 6.892 | 0.178 (0.079-0.689) | 0.006 |
Note: SAS: Self-rating Anxiety Scale.
Correlation between psychological distress and anxiety score
The anxiety score of patients undergoing chemotherapy after breast cancer surgery was 54.96±9.61, and the degree of psychological distress was positively correlated with the anxiety score (r=0.249, P=0.005; Figure 1).
Figure 1.
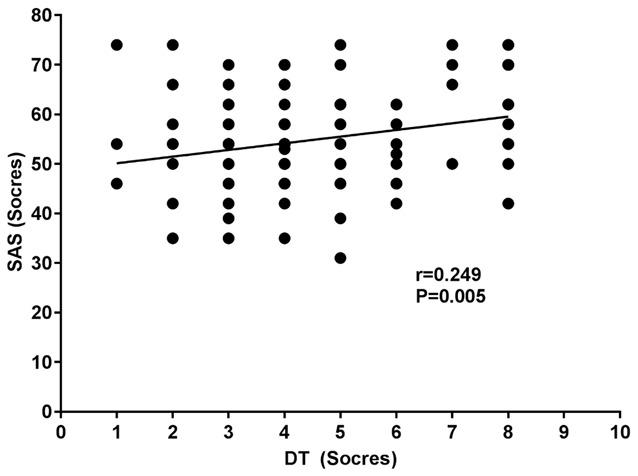
Study of correlation between psychological distress and anxiety score. SAS: Self-rating Anxiety Scale; DT: Distress Thermometer.
Comparison of the degree of psychological distress and anxiety scores between the two groups of patients after care intervention
The degree of psychological distress and anxiety scores of the observation group after treatment were significantly lower than those before treatment and significantly lower than those of the control group (all P<0.05; Table 5).
Table 5.
Degree of psychological distress and anxiety score in the two groups of patients after care intervention
| Category | Observation group | Control group | t | P | Observation group | Control group | t | P |
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before treatment | Before treatment | After treatment | After treatment | |||||
| Degree of psychological distress (point) | 4.61±1.86 | 4.49±1.79 | 0.322 | 0.748 | 3.26±1.52*** | 4.02±1.62 | 2.730 | 0.020 |
| SAS score (point) | 54.25±9.54 | 55.27±10.35 | 0.502 | 0.617 | 48.74±9.01*** | 53.78±10.21 | 2.564 | 0.012 |
Note: Compared to before treatment within the same group;
P<0.001.
Comparison of the quality of life between two groups of patients before and after treatment
Before treatment, there were no significant differences regarding additional items of concern, social/family well-being, functional well-being, physical well-being, emotional well-being, aor overall quality of life between the two groups of patients (all P>0.05). After treatment, both groups of patients demonstrated better scores in additional items of concern, social/family well-being, functional well-being, physical well-being, emotional well-being, and overall quality of life than those before treatment (all P<0.05; Table 6). Of note, the observation group showed better quality of life scales than those of the control group.
Table 6.
Comparison of the quality of life between two groups of patients before and after treatment
| Category | Observation group | Control group | t | P | Observation group | Control group | t | P |
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before treatment | Before treatment | After treatment | After treatment | |||||
| Additional concerning items | 13.82±2.73 | 14.02±2.92 | 0.346 | 0.730 | 18.62±3.22* | 15.92±3.72* | 3.802 | <0.001 |
| Social/family well-being | 11.27±2.65 | 11.87±2.78 | 1.082 | 0.282 | 17.21±3.52* | 13.92±3.31* | 4.717 | <0.001 |
| Functional well-being | 12.82±2.78 | 13.23±2.68 | 0.736 | 0.484 | 16.23±2.83* | 14.04±2.92* | 3.731 | <0.001 |
| Physical well-being | 13.72±2.48 | 13.82±2.61 | 0.192 | 0.848 | 17.62±3.21* | 15.92±3.28* | 2.566 | 0.012 |
| Emotional well-being | 12.23±2.57 | 12.63±2.61 | 0.767 | 0.451 | 17.26±3.35* | 15.32±3.54* | 2.578 | 0.007 |
| Overall quality of life | 63.92±7.92 | 64.23±7.62 | 0.195 | 0.845 | 86.19±12.92 | 75.09±11.72 | 4.409 | <0.001 |
Note: Compared to before treatment within the same group;
P<0.005.
Discussion
Breast cancer is the most common malignancy in women, of which the incidence is increasing year by year with a trend to affect younger women [15]. Surgery is an effective method for the treatment of breast cancer. Postoperative chemotherapy can effectively prevent recurrence and metastasis, so it can control progression and prolong the life of patients [18,19]. After the mastectomy, due to the changes in breast shape and the occurrence of adverse effects after chemotherapy, there may be a negative impact on the psychology of patients. If the negative emotion cannot be well alleviated, this will easily cause psychological disorders in patients. Therefore, how to effectively resolve negative emotions and increase psychological endurance for patients undergoing chemotherapy after breast cancer surgery has become a new topic of clinical research [20,21].
This study shows that breast cancer patients have a high degree of psychological distress, which is a combination of the psychological problems that may exist in cancer patients according to the National Cancer Institute of the United States, and is defined as cancer-related psychological distress [22]. In this study, BC patients who received chemotherapy after surgery were selected, since psychological problems were more prominent in the early stage of disease diagnosis and treatment. Studies have found that the higher the degree of psychological distress, the more serious the psychological problems of the patients during the treatment of breast cancer, which makes them more likely to develop mental illness [23,24]. There are many factors that affect the degree of psychological distress, and patients with different diseases experience psychological distress in different ways [25,26].
In this study, we analyzed factors affecting the psychological distress of breast cancer patients and demonstrated that age, monthly income, surgery method, and medical insurance status were independent factors that impact the psychological distress of patients undergoing chemotherapy after breast cancer surgery. A study reported that young cancer patients were more prone to have anxiety, depression and suicidal tendency [27]. With age and life experience increasing, the psychological endurance of older patients is also higher than that of young patients. A study revealed that the average age of the psychological distress group was 6 years younger than that of the distress-free group [28]. A previous study demonstrated that young patients with breast cancer were more affected by fatigue and distress due to the greater functional degeneration [29]. The monthly income and medical insurance status are problems encountered by patients in the course of treatment. Because the treatment cost is still a high, patients with low monthly income or without medical insurance are facing huge economic pressure, which undoubtedly have an impact on patients’ psychology [30]. In terms of surgery methods, studies have shown that patients undergoing breast-conserving surgery have lower psychological distress than those undergoing radical mastectomy, which may be due to the psychological distress caused by weakened femininity, impaired sexual life, and depression after mastectomy [31]. Another study revealed that surgery options and adverse effects of chemotherapy can affect the psychological distress of patients, which is consistent with our findings [32]. This may be due to the fact that breast-conserving surgery does not impact patients much regarding the physical appearance, which enables them quickly to return to normal life and to experience low degree of psychological distress.
A study on the psychological distress of patients with a new diagnosis of breast cancer and another one on psychological distress of patients with first-time chemotherapy exhibited psychological scores of (4.47±2.29) and (4.92±2.23), respectively [33,34]. An overseas study reported a psychological distress score of (3.95±2.57) in breast cancer patients [35]. The score by overseas study is slightly lower than that of the domestic study, which may result from the fact that their patients had been diagnosed within 5 years and already had a certain understanding of the disease. Studies have demonstrated that reducing patients’ psychological distress can help to ameliorate their negative emotions, which makes them to cope with the treatment with a positive attitude. Studies have also shown that psychological distress is positively correlated with patients’ anxiety, and the elimination of psychological distress was associated with the removal of negative emotions [12,36]. Our data are in line with previous results that the degree of psychological distress is positively correlated with the anxiety score. Further use of stepwise care intervention has found that this method is beneficial to the elimination of patients’ psychological distress and anxiety. Studies have revealed that the stepwise care is a new type of nursing model that increases the intensity of gradual intervention [37]. A domestic study reported that for patients with gynecological malignant tumors, stepwise psychological care can effectively ameliorate the psychological distress and improve patients’ quality of life [38]. Our study suggests that stepwise psychological care can alleviate patients’ psychological distress and anxiety.
The sample size in this study was small, thus, a multi-center research would be needed to expand the sample size in the future. Additionally, the factors that affect patients’ psychological distress and the therapeutic value of stepwise psychological care also warrant future investigation.
In summary, young age, low monthly income, radical mastectomy, and no medical insurance are independent factors that affect the psychological distress of patients undergoing chemotherapy after breast cancer surgery. The use of stepwise psychological care can reduce patients’ psychological distress and anxiety.
Disclosure of conflict of interest
None.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;60:277–300. [Google Scholar]
- 3.Desantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Sauer AG, Jemal A, Siegel RL. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 4.Dora L, Agrawal S, Panda R, Abraham A. Optimal breast cancer classification using GaussNewton representation based algorithm. Expert Syst Appl. 2017;85:134–145. [Google Scholar]
- 5.Chen Y, Hao Y, Huang Y, Wu W, Liu X, Li Y, Gou M, Qian Z. An injectable, near-infrared light-responsive click cross-linked azobenzene hydrogel for breast cancer chemotherapy. J Biomed Nanotechnol. 2019;15:1923–1936. doi: 10.1166/jbn.2019.2821. [DOI] [PubMed] [Google Scholar]
- 6.Xu AJ, DeSelm CJ, Ho AY, Gillespie EF, Braunstein LZ, Khan AJ, McCormick B, Powell SN, Cahlon O. Overall survival of breast cancer patients with locoregional failures involving internal mammary nodes. Adv Radiat Oncol. 2019;4:447–452. doi: 10.1016/j.adro.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bobevski I, Kissane DW, Vehling S, McKenzie DP, Glaesmer H, Mehnert A. Latent class analysis differentiation of adjustment disorder and demoralization, more severe depressive and anxiety disorders, and somatic symptoms in patients with cancer. Psychooncology. 2018;27:2623–2630. doi: 10.1002/pon.4761. [DOI] [PubMed] [Google Scholar]
- 8.Henry BJ. Quality of life and resilience: exploring a fly fishing intervention for breast cancer survivors. Clin J Oncol Nurs. 2017;21:e9–e14. doi: 10.1188/17.CJON.E9-E14. [DOI] [PubMed] [Google Scholar]
- 9.Zhang C, Shi D, Yang P. BNP as a potential biomarker for cardiac damage of breast cancer after radiotherapy: a meta-analysis. Medicine (Baltimore) 2019;98:e16507. doi: 10.1097/MD.0000000000016507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quyyumi FF, Wright JD, Accordino MK, Buono D, Law CW, Hillyer GC, Neugut AI, Hershman DL. Factors associated with multidisciplinary consultations in patients with early stage breast cancer. Cancer Invest. 2019;37:233–241. doi: 10.1080/07357907.2019.1624766. [DOI] [PubMed] [Google Scholar]
- 11.Lam WW, Yoon SW, Sze WK, Ng AW, Soong I, Kwong A, Suen D, Tsang J, Yeo W, Wong KY, Fielding R. Comparing the meanings of living with advanced breast cancer between women resilient to distress and women with persistent distress: a qualitative study. Psychooncology. 2017;26:255–261. doi: 10.1002/pon.4116. [DOI] [PubMed] [Google Scholar]
- 12.Liu F, Huang J, Zhang L, Fan F, Chen J, Xia K, Liu Z. Screening for distress in patients with primary brain tumor using distress thermometer: a systematic review and meta-analysis. BMC Cancer. 2018;18:124. doi: 10.1186/s12885-018-3990-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Straten A, Hill J, Richards DA, Cuijpers P. Stepped care treatment delivery for depression: a systematic review and meta-analysis. Psychol Med. 2015;45:231–246. doi: 10.1017/S0033291714000701. [DOI] [PubMed] [Google Scholar]
- 14.Li LL, Li XM, Han DF, Li JY, Zhao WQ, Zhang MY. A longitudinal study on the locus of psychological distress and its influencing factors in patients with breast cancer. Chin J Nurs. 2020;55:22–28. [Google Scholar]
- 15.Wan G, Cao F, Wang X, Sun X. Bevacizumab added to neoadjuvant chemotherapy in Her2-negative non-metastatic breast cancer. J Cancer. 2019;10:416–417. doi: 10.7150/jca.29461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zainal NZ, Booth S, Huppert FA. The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: a meta-analysis. Psychooncology. 2013;22:1457–1465. doi: 10.1002/pon.3171. [DOI] [PubMed] [Google Scholar]
- 17.Zhan YN, Wang BQ, Tian J, Liu J, Feng X, Guo Y, Jia Y, Guo R. Effect of ladder psychological nursing on anxiety, depression and quality of life in patients with head and neck cancer. J Nur Sci. 2019;34:6–9. [Google Scholar]
- 18.Gao J, Deng F, Jia W. Inhibition of indoleamine 2,3-dioxygenase enhances the therapeutic efficacy of immunogenic chemotherapeutics in breast cancer. J Breast Cancer. 2019;22:196–209. doi: 10.4048/jbc.2019.22.e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cai G, Cao L, Kirova YM, Feng Y, Chen JY. Prospective results of concurrent radiation therapy and weekly paclitaxel as salvage therapy for unresectable locoregionally recurrent breast cancer. Radiat Oncol. 2019;14:115. doi: 10.1186/s13014-019-1321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Truong C, Gallo J, Roter D, Joo J. The role of self-disclosure by peer mentors: using personal narratives in depression care. Patient Educ Couns. 2019;102:1273–1279. doi: 10.1016/j.pec.2019.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu PH, Chen SW, Huang WT, Chang SC, Hsu MC. Effects of a psychoeducational intervention in patients with breast cancer undergoing chemotherapy. J Nurs Res. 2018;26:266–279. doi: 10.1097/jnr.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology-dis tress management (version 3.2019) National Comprehensive Cancer Network. 2019 doi: 10.6004/jnccn.2019.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pérez S, Conchado A, Andreu Y, Galdón MJ, Cardeña E, Ibáñez E, Durá E. Acute stress trajectories 1 year after a breast cancer diagnosis. Support Care Cancer. 2016;24:1671–1678. doi: 10.1007/s00520-015-2960-x. [DOI] [PubMed] [Google Scholar]
- 24.Goyal NG, Levine BJ, Van Zee KJ, Naftalis E, Avis NE. Trajectories of quality of life following breast cancer diagnosis. Breast Cancer Res Treat. 2018;169:163–173. doi: 10.1007/s10549-018-4677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Wang K, Yin Y, Li Y, Li S. Relationships between family resilience, breast cancer survivors’ individual resilience, and caregiver burden: a cross-sectional study. Int J Nurs Stud. 2018;88:79–84. doi: 10.1016/j.ijnurstu.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 26.Finck C, Barradas S, Zenger M, Hinz A. Quality of life in breast cancer patients: associations with optimism and social support. Int J Clin Health Psychol. 2018;18:27–34. doi: 10.1016/j.ijchp.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie J, Ding S, He S, Duan Y, Yi K, Zhou J. A prevalence study of psychosocial distress in adolescents and young adults with cancer. Cancer Nurs. 2017;40:217–223. doi: 10.1097/NCC.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 28.Robbeson C, Hugenholtz-Wamsteker W, Meeus M, Devoogdt N, Nijs J, De Groef A. Screening of physical distress in breast cancer survivors: concurrent validity of the distress thermometer and problem list. Eur J Cancer Care (Engl) 2019;28:e12880. doi: 10.1111/ecc.12880. [DOI] [PubMed] [Google Scholar]
- 29.Bruce J, Thornton AJ, Powell R, Johnston M, Wells M, Heys SD, Thompson AM, Smith CW, Chambers AW, Scott NW Recovery Study Group. Psychological, surgical, and sociodemographic predictors of pain outcomes after breast cancer surgery: a population-based cohort study. Pain. 2014;155:232–243. doi: 10.1016/j.pain.2013.09.028. [DOI] [PubMed] [Google Scholar]
- 30.Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14:1165–1174. doi: 10.1016/S1470-2045(13)70442-X. [DOI] [PubMed] [Google Scholar]
- 31.Rowland JH, Desmond KA, Meyerowitz BE, Belin TR, Wyatt GE, Ganz PA. Role of breast reconstructive surgery in physical and emotional outcomes among breast cancer survivors. J Natl Cancer Inst. 2000;92:1422–1429. doi: 10.1093/jnci/92.17.1422. [DOI] [PubMed] [Google Scholar]
- 32.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 33.Li AZ, Xia HN, Dong MF, Huang HZ. Analysis of psychological pain in newly diagnosed breast cancer patients and impact factors. Hospital Management Theory. 2018;35:29–32. [Google Scholar]
- 34.Li C, Yang MY, Duan WJ, Huang L, Yang XF. Current status of psychological distress and related factors before first chemotherapy in breast cancer patients. J Kunming Med Univ. 2018;39:33–38. [Google Scholar]
- 35.Mcfarland DC, Shaffer KM, Tiersten A. Prevalence of physical problems detected by the distressthermometer and problem list in patients with breast cancer. Psychooncology. 2018;27:1394–1403. doi: 10.1002/pon.4631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agarwal J, Powers K, Pappas L, Buchmann L, Anderson L, Gauchay L, Rich A. Correlates of elevated distress thermometer scores in breast cancer patients. Support Care Cancer. 2013;21:2125–2136. doi: 10.1007/s00520-013-1773-z. [DOI] [PubMed] [Google Scholar]
- 37.Seekles W, van Straten A, Beekman A, van Marwijk H, Cuijpers P. Stepped care treatment for depression and anxiety in primary care. A randomized controlled trial. Trials. 2011;12:171. doi: 10.1186/1745-6215-12-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ouyang C, Chou CH, Ye S. Effect of ladder psychological nursing on psychological pain and quality of life of patients with gynecological malignant tumor. J Nurs Rehabil. 2020;19:57–61. [Google Scholar]


