Abstract
Noroviruses are the leading cause of foodborne disease in the United States. Foodborne transmission of norovirus is often associated with contamination of food during preparation by an infected food worker. The U.S. Food and Drug Administration’s Food Code provides model food safety regulations for preventing transmission of foodborne disease in restaurants; however, adoption of specific provisions is at the discretion of state and local governments. We analyzed the food service regulations of all 50 states and the District of Columbia (i.e., 51 states) to describe differences in adoption of norovirus-related Food Code provisions into state food service regulations. We then assessed potential correlations between adoption of these regulations and characteristics of foodborne norovirus outbreaks reported to the National Outbreak Reporting System from 2009 through 2014. Of the 51 states assessed, all (100%) required food workers to wash their hands, and 39 (76%) prohibited bare-hand contact with ready-to-eat food. Thirty states (59%) required exclusion of staff with vomiting and diarrhea until 24 h after cessation of symptoms. Provisions requiring a certified food protection manager (CFPM) and a response plan for contamination events (i.e., vomiting) were least commonly adopted; 26 states (51%) required a CFPM, and 8 (16%) required a response plan. Although not statistically significant, states that adopted the provisions prohibiting bare-hand contact (0.45 versus 0.74, P = 0.07), requiring a CFPM (0.38 versus 0.75, P = 0.09), and excluding ill staff for ≥24 h after symptom resolution (0.44 versus 0.73, P = 0.24) each reported fewer foodborne norovirus outbreaks per million person-years than did those states without these provisions. Adoption and compliance with federal recommended food service regulations may decrease the incidence of foodborne norovirus outbreaks.
Keywords: Food service, Norovirus, Prevention, Regulation, Retail food code
Noroviruses are the leading cause of acute gastroenteritis and foodborne disease in the United States (11). From 2009 through 2012, approximately 48% of foodborne disease outbreaks reported to the National Outbreak Reporting System (NORS) that had a single known etiology were caused by noroviruses (15). Symptoms of norovirus infection generally include vomiting and diarrhea; however, infected individuals can be asymptomatic (13). Noroviruses can be spread by ingestion of contaminated food or water, contact with contaminated fomites, direct person-to-person contact, and inhalation and subsequent ingestion of aerosolized vomitus (13, 21). Norovirus can be shed in high quantities by infected individuals, and shedding can occur before, during, and after presentation of symptoms (1). The virus has a low infectious dose (18 to 2,800 viral particles) (2, 24), can withstand freezing temperatures and heating, and is difficult to kill with common disinfectants (13). Therefore, norovirus can spread quickly in food service settings, where a contaminated food item can potentially expose hundreds of people.
Foodborne norovirus outbreaks are typically associated with contamination of food during preparation by an infected food service worker, often involving bare-hand contact with ready-to-eat (RTE) foods or working while ill (3, 11). Among foodborne norovirus outbreaks occurring from 2009 through 2012, infected food workers were implicated as the source of contamination in 70% of outbreaks in which factors contributing to contamination were reported; bare-hand contact was specifically implicated in over half of these outbreaks (15). Of the reported foodborne norovirus outbreaks, 90% involved foods prepared in food service facilities, most commonly in restaurants (15).
The U.S. Food and Drug Administration (FDA) Food Code provides model food safety regulations for preventing transmission of foodborne disease in food service facilities (31). Since 2009, the Food Code has been published every 4 years, based on stakeholder input from the food industry, consumer groups, academia, and government through the Conference for Food Protection (7). Before 2009, the Food Code was revised every 2 years. Updates or revisions to Food Code provisions may be released between published versions in the form of a supplement to the previously published version. Although the Food Code represents current guidelines for food safety, adoption of the Food Code provisions, in whole or in part, is at the discretion of state and local governments; consequently, adoption varies widely among states (30).
Uniform adherence to food service guidelines has significant potential to improve food safety in the United States. Identification of gaps in adherence to these guidelines would allow lawmakers and the food industry to determine appropriate areas for improvement. The primary objective of our study was to assess adoption of specific norovirus-related food service provisions of the 2013 FDA Food Code (31) that were previously identified as important in decreasing transmission of foodborne norovirus (15) and to describe differences in the adoption of these provisions among states. We also evaluated associations between the adoption of select provisions and the rate and characteristics of foodborne norovirus outbreaks reported by each state.
MATERIALS AND METHODS
Food service provisions.
We searched the government Web sites of all 50 states and the District of Columbia (hereinafter referred to as 51 states) to obtain the most recent food code regulations that were in effect as of 31 December 2014. Publicly accessible regulations (Table 1) were downloaded from government Web sites and/or obtained through contact with state public health departments. Regulations were assessed by two independent reviewers for the presence of provisions on hand washing, bare-hand contact with RTE food, exclusion of ill workers, certified food protection manager (CFPM), and a response plan for contamination events, as described in the 2013 FDA Food Code. Descriptions of each provision and the specific criteria used for assessment of state regulations in this analysis are provided in Table 2.
TABLE 1.
State food service regulations
| State | Source | Effective date |
|---|---|---|
| Alabama | Rules of Alabama State Board of Health, Bureau of Environmental Services, chapter 420-3-22 for Food Establishment Sanitation | 4 Apr. 2013 |
| Alaska | 18 AAC 31 Alaska Food Code | 24 June 2012 |
| Arizona | Arizona Administrative Code, Title 9, Health Services, chapter 8: Department of Health Services Food, Recreational and Institutional Sanitation | 14 July 2000 |
| Arkansas | Rules and Regulations Pertaining to Food Establishments | 1 Aug. 2012 |
| California | California Retail Food Code | 1 Jan. 2014 |
| Colorado | Colorado Retail Food Establishment Rules and Regulations | 1 Mar. 2013 |
| Connecticut | 19–13-B42, Sanitation of places dispensing foods or beverages | 3 July 2007 |
| Delaware | State of Delaware Food Code | 11 May 2014 |
| Florida | Florida Administrative Code, chapter 64e-11, Food Hygiene | 1 Jan. 2013 |
| Georgia | Rules of Department of Human Resources Public Health, chapter 290-5-14, Food Service | 12 Sep. 2007 |
| Hawaii | Hawaii Administrative Rules, chapter 11–50, Food Safety Code | 24 Feb. 2014 |
| Idaho | Idaho Food Code | 2 Apr. 2008 |
| Illinois | Illinois Administrative Code, Title 77, Public Health, chapter I, Department of Public Health, subchapter M, Food, Drugs and Cosmetics, part 750, Food Service Sanitation Code | 20 Nov. 2014 |
| Indiana | Retail Food Establishment Sanitation Requirements, Title 410 IAC 7–24 | 13 Nov. 2004 |
| Iowa | Iowa Food Code | 1 Jan. 2014 |
| Kansas | Kansas Food Code 2012 | 1 July 2012 |
| Kentucky | Kentucky Food Code, 902 KAR 45:005 | 1 May 2009 |
| Louisiana | Louisiana Public Health-Sanitary Code, Title 51 | 20 June 2002 |
| Maine | State of Maine Food Code 2013 | 1 Oct. 2013 |
| Maryland | Code of Maryland Regulations, Title 10, Department of Health and Mental Hygiene, Subtitle 15, Food, chapter 03, Food Service Facilities | 7 Dec. 2007 |
| Massachusetts | Massachusetts 105 CMR 590.000, Minimum Sanitation Standards for Food Establishments | 29 Sep. 2000 |
| Michigan | Michigan Food Law and Food Code | 1 Oct. 2012 |
| Minnesota | Minnesota Food Code, Minnesota Rules, chapter 4626 | 3 Oct. 2013 |
| Mississippi | Mississippi Food Regulations | 1 Jan. 1999 |
| Missouri | Missouri Food Code for the Food Establishments of the State of Missouri | 30 Sep. 2013 |
| Montana | Administrative Rules of Montana, Title 37, chapter 110, subchapter 2 | 23 Nov. 2000 |
| Nebraska | Nebraska Food Code | 8 Mar. 2012 |
| Nevada | Nevada Administrative Code, chapter 446, Food Establishments | 18 Dec. 2013 |
| New Hampshire | Chapter He-P 2300, Sanitary Production and Distribution of Food | 12 Oct. 2012 |
| New Jersey | New Jersey Administrative Code, chapter 24, Sanitation in Retail Food Establishments and Food and Beverage Vending Machines | 2 Jan. 2007 |
| New Mexico | New Mexico Administrative Code, chapter 7.6.2 | 12 Aug. 2000 |
| New York | New York State Sanitary Code, part 14 | 8 Jan. 1997 |
| North Carolina | North Carolina Food Code Manual | 1 Sep. 2012 |
| North Dakota | North Dakota Food Code, chapter 33-33-04 | 1 Apr. 2012 |
| Ohio | Ohio Uniform Food Safety Code | 1 Jan. 2014 |
| Oklahoma | Oklahoma Food Code | 1 Nov. 2011 |
| Oregon | Oregon Health Authority Food Sanitation Rules | 4 Sep. 2012 |
| Pennsylvania | Pennsylvania Food Code, chapter 46 | 12 May 2014 |
| Rhode Island | Rhode Island Food Code | 17 Sep. 2012 |
| South Carolina | South Carolina Retail Food Establishments, Regulation 61–25 | 27 June 2014 |
| South Dakota | South Dakota Food Service Code, chapter 44:02:07 | 26 May 1997 |
| Tennessee | Rules of Tennessee Department of Health, Food Service Establishments | 1978 |
| Texas | Texas Food Establishment Rules | 15 Mar. 2006 |
| Utah | Utah Administrative Code, Food Service Sanitation | 10 Sep. 2012 |
| Vermont | Vermont Health Regulations for Food Service Establishments | 1 Dec. 2003 |
| Virginia | Virginia Food Regulations | 1 Jan. 2010 |
| Washington | Washington State Retail Food Code | 1 May 2013 |
| West Virginia | West Virginia Legislative Rule, Title 64, Series 17, Food Establishments | 2 Apr. 2008 |
| Wisconsin | Wisconsin Food Code | 1 Sep. 2013 |
| Wyoming | Wyoming Food Safety Rule | 2012 |
| District of Columbia | District of Columbia Food Code Regulations, Title 25 | 30 Nov. 2012 |
TABLE 2.
Assessment criteria for norovirus-related food service provisions in state regulations
| Provision | 2013 Food Code | Assessment criteria for state regulation |
|---|---|---|
| Hand washing procedure | Food Code details a hand washing procedure for all food workers, including how to wash their hands and for how long, and nine specific instances before or after which employees should wash (Section 2–3). | Any provision requiring hand washing. |
| Prohibition of bare-hand contact | Food Code prohibits bare-hand contact with ready-to-eat (RTE) food, except in certain circumstances, such as when washing vegetables or when a kill step is involved (Section 3–301.11). | Any regulation prohibiting bare-hand contact with RTE foods; states that called for limitation or minimization of bare-hand contact were not considered as explicitly prohibiting contact. |
| Certified food protection manager (CFPM) | Provision requires that each establishment have at least one employee with supervisory or managerial duties who has been certified as a food protection manager by passing a test from an accredited program. Food Code also allows for the presence of a CFPM to fulfill a separate provision, which requires a person in charge to be able to demonstrate knowledge of food safety principles during an inspection or other request (Sections 2–102.12 and 2–102.20). | Provision requiring at least one CFPM per food establishment; states that did not require a CFPM but allowed a certification to fulfill knowledge requirements were not considered as explicitly requiring a CFPM. |
| 24-h ill staff exclusion | Food Code recommends that food workers with diarrhea or vomiting be excluded until 24 h after resolution of symptoms. Exclusion means that affected employees do not report to work at all for the specified time. Food Code provides more stringent exclusion periods for employees with laboratory-confirmed norovirus infections, recommending exclusion for 24 h after symptom resolution and then restriction from certain food handling duties for another 24 h after the exclusion period. However, because laboratory confirmation of norovirus infection is rarely performed in sporadic cases due to lack of widely available routine clinical assays, this provision is often not applicable (Section 2–2). | Provision requiring employees with vomiting or diarrhea to be excluded for at least 24 h after symptom resolution. Provisions requiring medical clearance before returning to work were considered to meet this criterion. Provisions allowing either exclusion or restriction for employees with symptoms or not specifying a length of time for exclusion were not considered to meet this criterion. Because most ill workers will not be specifically diagnosed with laboratory-confirmed norovirus, we used adoption of the general vomiting and diarrhea exclusion period as the primary indicator of adopting ill staff exclusion guidelines and used this provision in our subsequent analyses. To descriptively assess differences in regulations, we also examined other exclusion criteria, including the norovirus-specific indicator. |
| Response plan for contamination events | Provision requires that food establishments have procedures in place for employees to follow during situations in which vomitus or fecal matter is expelled onto surfaces in the establishment. Although Food Code does not recommend specific procedures, it indicates that response plans should include actions that employees should take to prevent transmission of pathogens to other employees and patrons of the establishment (Section 2–501). | Any provision requiring a contamination event response plan. |
Outbreak data.
Data on all foodborne disease outbreaks with a first illness onset date of 1 January 2009 to 31 December 2014 and that listed norovirus as the only epidemiologically suspected or laboratory-confirmed etiology were obtained from NORS on 4 December 2015. NORS is an Internet-based voluntary surveillance system used by local, state, and territorial public health agencies to report to the Centers for Disease Control and Prevention (CDC) all foodborne and waterborne disease outbreaks and enteric disease outbreaks that are spread by person-to-person contact or environmental contamination or have other or unknown modes of transmission (6, 14). Foodborne outbreaks are defined as two or more cases of a similar illness associated with a common exposure in which food is reported as the primary mode of transmission. The following outbreak characteristics were extracted from NORS: outbreak size and duration, implication of food workers as the source of the outbreak, implication of bare-hand contact by an infected worker, and whether an analytic study (i.e., case-control or cohort) was conducted as part of the outbreak investigation.
Analysis.
NORS data were cleaned and analyzed using SAS 9.3 (SAS Institute, Cary, NC) and R (20, 23). State-specific population-based reporting rates (i.e., the number of NORS reports per population in each state during the 6-year reporting period) of foodborne norovirus outbreaks were calculated using 2014 state population estimates from the U.S. Census Bureau (26), under the assumption that each state’s population did not change significantly from 2009 through 2014. Reporting rates were presented in person-time, which combines the number of persons at risk (i.e., number of people in each state) and the study period (i.e., 6-year reporting period) and standardized to 1 million persons per year. NORS data were then merged with the data from our assessment of state regulations.
For the analysis, continuous variables (i.e., outbreak size and duration) were dichotomized using the median. An outbreak was defined as large when the estimated number of primary cases was 12 or more persons and small when the estimated number of primary cases was less than 12. An outbreak was considered to be of long duration when the dates of illness onset spanned three or more days and of short duration when dates of illness onset spanned less than 3 days.
We were unable to assess associations with the provision on hand washing because all states had adopted some form of this provision. We also did not assess associations with the provision requiring a contamination response plan because few states had adopted this provision. We used the Wilcoxon rank-sum test to independently compare the outbreak reporting rates of states with and without the specified provisions and used multivariate linear regression to simultaneously assess associations between outbreak reporting rate and adoption of these provisions. We used multivariate logistic regression models to assess associations between adoption of each specific provision and the outbreak characteristics extracted from NORS, controlling for reporting rate and adoption of other provisions. We also controlled for whether a cohort or case-control study was conducted, as an indication of investigation intensity. Statistical significance was determined by the 95% confidence interval (CI) for all analyses.
RESULTS
Food service provisions.
Of the 51 states assessed, all adopted at least one of the five norovirus-related food service provisions in their respective food codes. A majority (33 states, 65%) adopted three or fewer provisions (Fig. 1). Thirteen states (25%) adopted four provisions, and five states (10%) adopted all five of the selected provisions.
FIGURE 1.
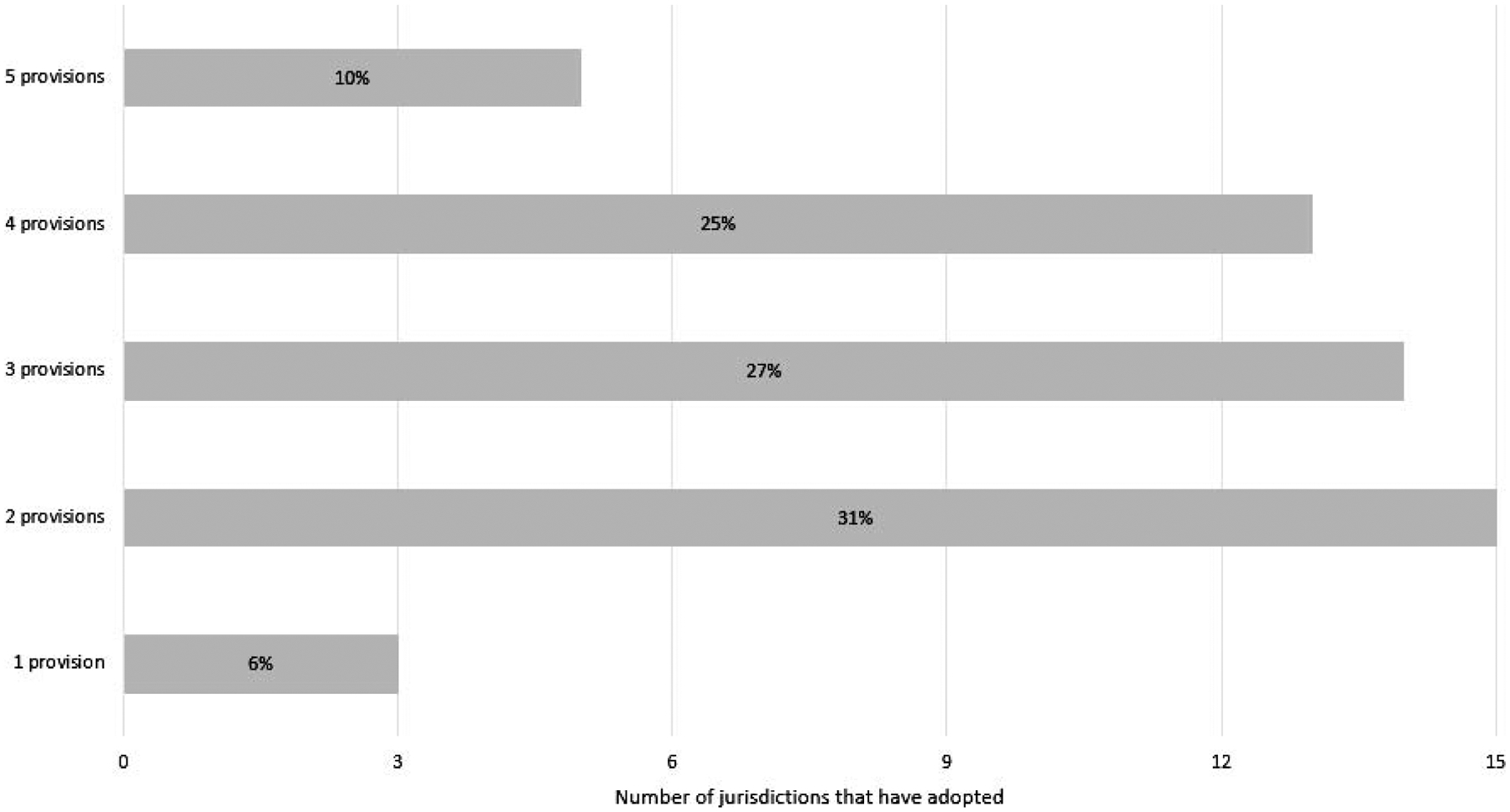
Adoption of selected food service provisions (described in Table 2); n = 51 states (50 states plus District of Columbia).
Hand hygiene provisions, specifically requiring hand washing and prohibiting bare-hand contact, were most widely adopted (Fig. 2). All states had provisions requiring hand washing, and 39 (76%) prohibited bare-hand contact with RTE food; an additional 8 states (16%) did not completely prohibit bare-hand contact but called for limitation or minimization of bare-hand contact with RTE food. Although all states included some type of provision regarding hand washing, not all components outlined in the Food Code were adopted by all states. The Food Code describes nine situations in which a food worker should wash his or her hands (Table 3). All states adopted the subprovision requiring hand washing after using the restrooms, but other subprovisions were not as widely adopted. The subprovision requiring food workers to wash their hands “before donning gloves to initiate a task that involves working with food” was least commonly included in state food codes, with only 40 states (78%) including this subprovision in their respective food codes.
FIGURE 2.
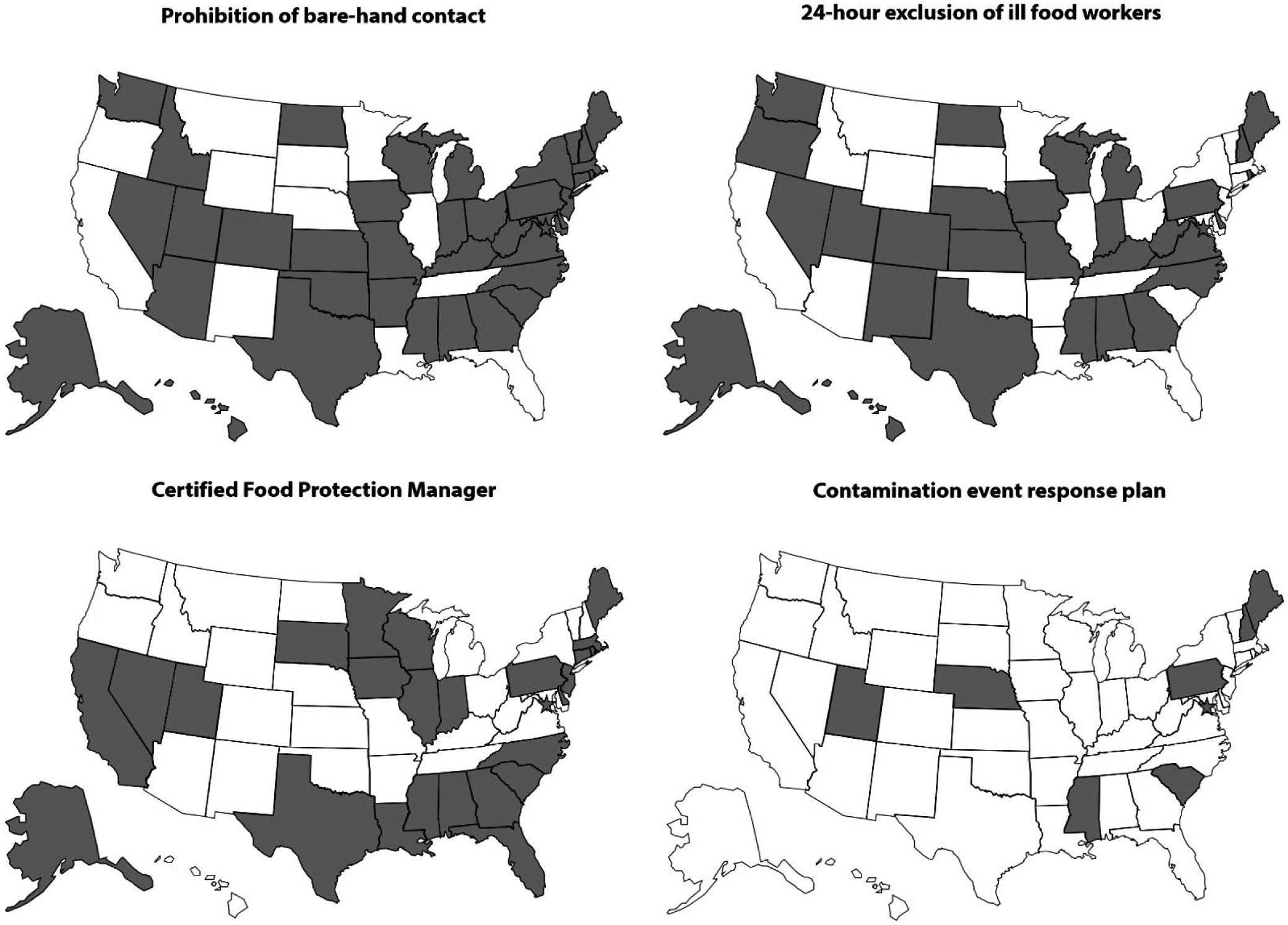
Adoption of selected food service provisions by state.
TABLE 3.
Adoption of specific hand washing provisions; n = 51 states (50 states plus District of Columbia)
| When to wash | No. (%) of states that have adopted |
|---|---|
| After using the restroom | 51 (100) |
| After coughing, sneezing, using a handkerchief or disposable tissue, using tobacco, eating, or drinking | 50 (98) |
| During food preparation, as often as necessary to remove soil and contamination and to prevent cross-contamination when changing tasks | 51 (100) |
| When switching between working with raw food and working with ready-to-eat food | 48 (94) |
| After engaging in other activities that contaminate the hands | 47 (92) |
| After touching bare human body parts other than clean hands and clean exposed portions of arms | 46 (90) |
| After caring for or handling service animals or aquatic animals | 46 (90) |
| After handling soiled equipment or utensils | 45 (88) |
| Before donning gloves to initiate a task that involves working with food | 40 (78) |
Wide variation was observed in the adoption of ill staff exclusion policies. Overall, all but one of the 51 states assessed (98%) included some type of provision requiring exclusion or restriction of employees that were ill with vomiting and diarrhea; however, guidelines for the postsymptomatic period differed among states. Thirty states (59%) required employees to be excluded until 24 h after cessation of vomiting and diarrhea, as described in the 2013 FDA Food Code (Fig. 2). Two states (6%) did not explicitly require a 24-h exclusion period but required at a minimum restriction of employees from food handling activities until 24 h after symptoms have resolved (Fig. 3). Restriction allows ill workers to report to work but restricts them from certain food handling activities that may contribute to illness transmission. Seven states (14%) required exclusion or restriction while employees are experiencing vomiting or diarrhea but allowed employees to return to duties when these symptoms ceased. An additional 11 states (22%) required exclusion or restriction while employees are experiencing vomiting or diarrhea but did not specify a length of time for exclusion or restriction. Thirty states (59%) included an additional norovirus-specific exclusion period in their respective food codes, requiring exclusion of those with a lab-confirmed norovirus diagnosis until 24 h after cessation of symptoms then restriction for another 24 h (Fig. 3).
FIGURE 3.
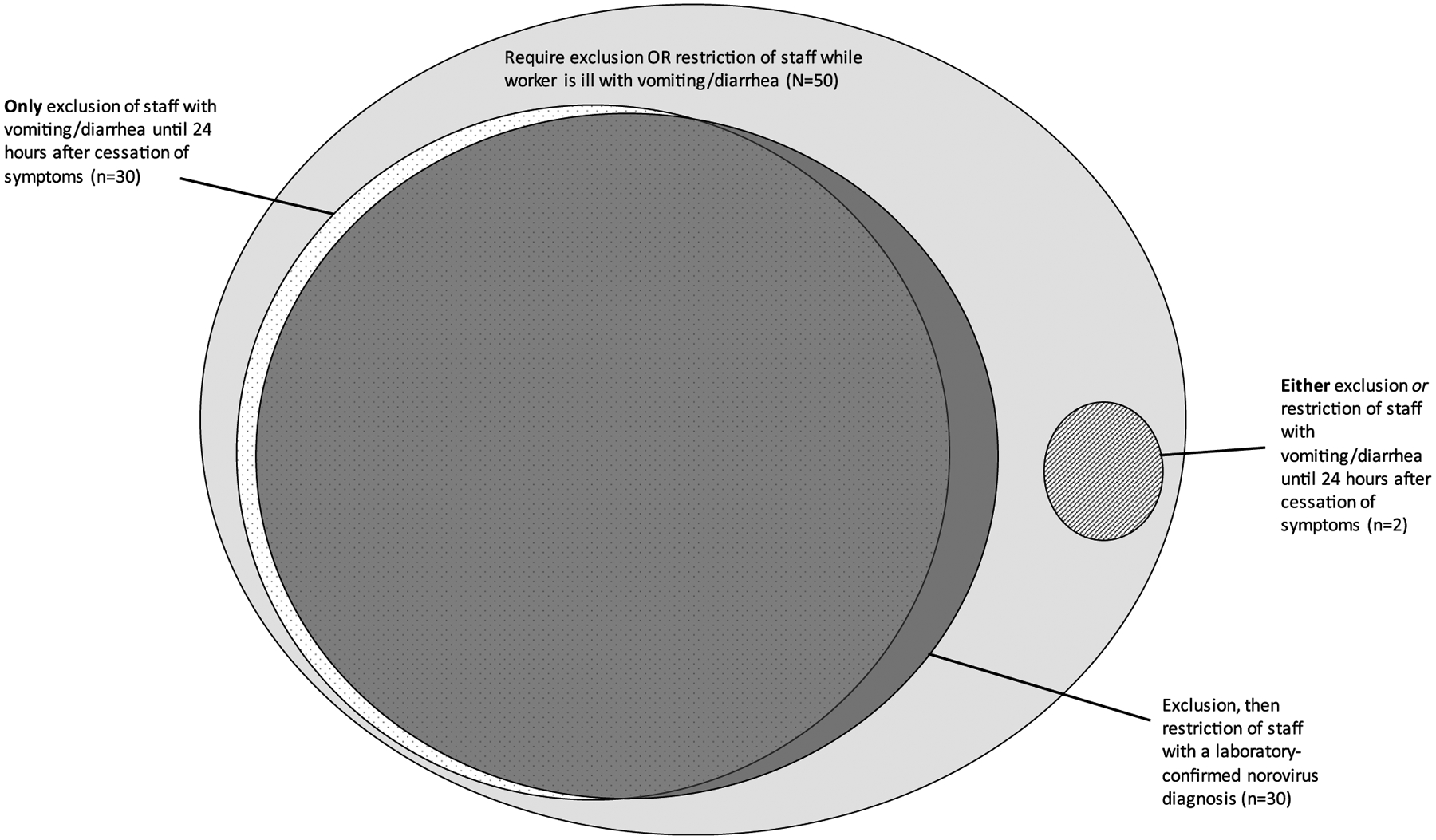
Adoption of specific ill staff exclusion requirements.
The least commonly adopted provisions were those requiring food establishments to have at least one CFPM and to have a plan in place for responding to contamination events (Fig. 2); only 26 states (51%) included the requirement for a CFPM in their food codes, and only 8 states (16%) required a contamination event response plan.
Associations with outbreak characteristics.
In total, 1,475 suspected or confirmed foodborne norovirus infection outbreaks that were reported to NORS occurred between 1 January 2009 and 31 December 2014. Individual states reported 0 to 173 (median, 10) foodborne norovirus outbreaks during the 6-year period, with a median reporting rate of 0.47 outbreaks per million person-years (range, 0.00 to 5.25 outbreaks per million person-years). Three states did not report any foodborne norovirus outbreaks in the 6-year period; therefore, these states were not included in our analysis of associations with outbreak reporting rates or characteristics. Although not statistically significant, states that adopted the provisions prohibiting bare-hand contact (0.45 versus 0.74, P = 0.07), requiring a CFPM (0.38 versus 0.75, P = 0.09), and excluding ill staff for ≥24 h after symptom resolution (0.44 versus 0.73, P = 0.24) each reported fewer outbreaks per million person-years than did those states that did not adopt these provisions (Fig. 4). When analyzed in a multivariate model, controlling for the adoption of 24-h ill staff exclusion and the requirement for a CFPM, states that prohibited bare-hand contact had a significantly lower reporting rate (P < 0.0001) than did states without the provision.
FIGURE 4.
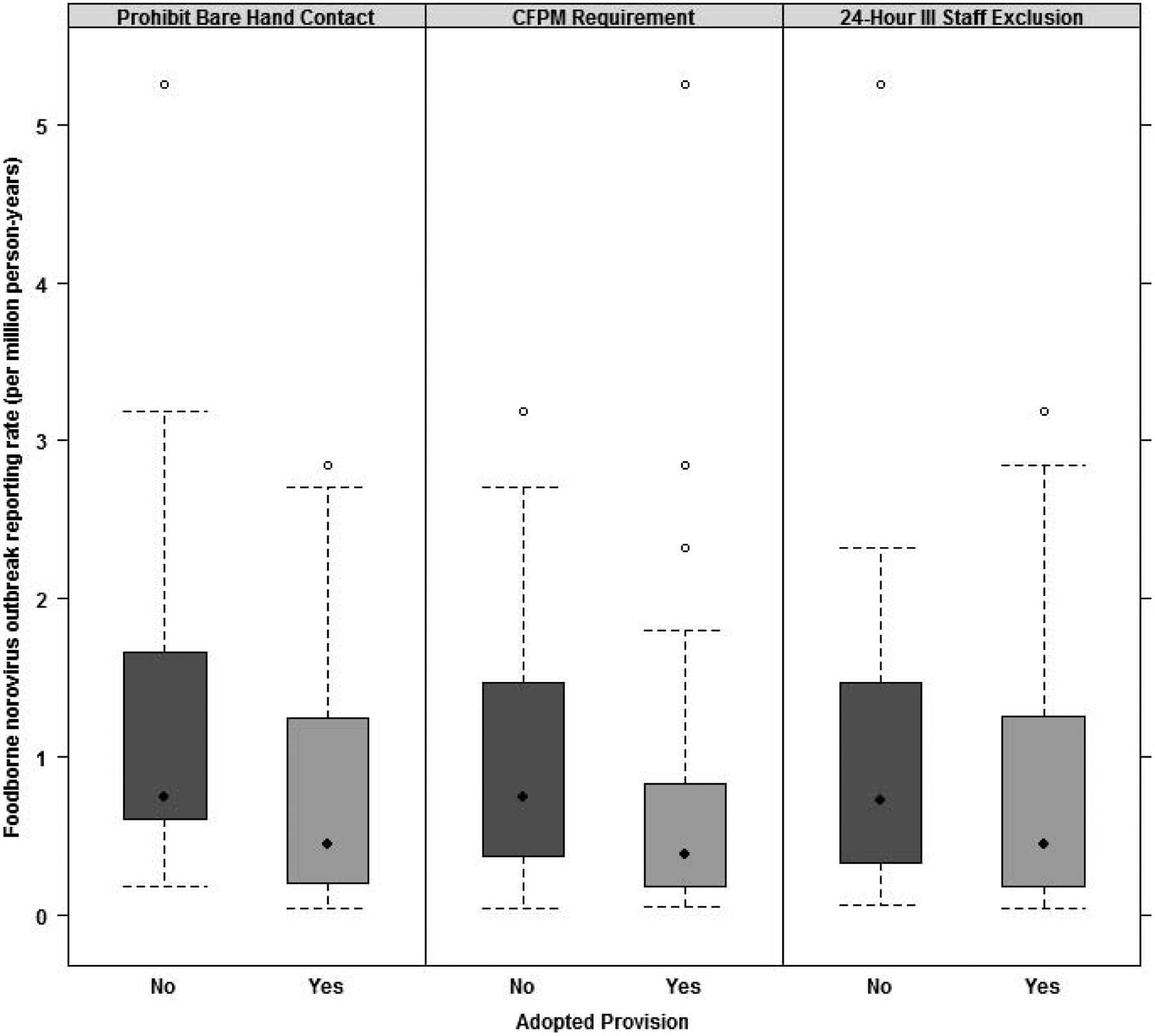
Outbreak reporting rates among 48 states with and without selected food service provisions (three states with no reported outbreaks from 2009 through 2014 were excluded). Solid diamonds denote the median foodborne norovirus outbreak reporting rate among states that did or did not adopt the specified provision; tails indicate the range of reporting rates; open circles indicate outliers.
Controlling for reporting rate, adoption of other provisions, and type of investigation conducted, we found significant associations between certain provisions and specific outbreak characteristics (Table 4). States that adopted the provision requiring a CFPM were 1.7 times (95% CI, 1.3, 2.1) more likely to implicate a food worker as the source of a reported outbreak that were those states without the provision. States that adopted the 24-h ill staff exclusion provision were 0.5 times (0.4, 0.6) more likely to have a smaller outbreaks, 0.7 times (0.5, 0.9) more likely to have shorter outbreaks, and 1.7 (1.0, 2.9) times more likely to implicate bare-hand contact by a food worker suspected to be infectious than were states without the provision.
TABLE 4.
Associations between presence of selected provisions and reported outbreak characteristics in 48 statesa
| Adjusted odds ratio (95% confidence interval)b | |||
|---|---|---|---|
| Comparator | Certified food protection manager | Prohibition of bare-hand contact | 24-h ill staff exclusion |
| Outbreak characteristic | |||
| Smallc | 1.0 (0.8, 1.2) | 1.1 (0.8, 1.4) | 0.5 (0.4, 0.6) |
| Short durationd | 1.2 (0.9, 1.6) | 1.0 (0.7, 1.3) | 0.7 (0.5, 0.9) |
| Implication of food workers | |||
| Food worker as source of reported outbreak | 1.7 (1.3, 2.1) | 1.5 (1.1, 2.0) | 1.1 (0.9, 1.5) |
| Bare-hand contact by a food worker suspected to be infectious | 2.5 (1.5, 4.2) | 1.4 (0.9, 2.4) | 1.7 (1.0, 2.9) |
Comparison was between states with and those without the specified provision. Three states with no reported outbreaks from 2009 through 2014 were excluded from this analysis.
Adjusted for adoption of other two provisions, reporting rate, and whether the state conducted an analytic investigation (case-control or cohort study).
Small outbreak defined as <12 estimated primary cases; large outbreak defined as ≥12 estimated primary cases.
Short duration defined as <3 days between date of onset of first and last illness; long duration defined as ≥3 days between date of onset of first and last illness.
DISCUSSION
In this assessment of state food codes, we found that provisions related to hand hygiene were the most widely adopted. Although some requirement for hand washing was adopted by all states, we found variation in adoption of subprovisions that specify times at which food workers should wash their hands. The least commonly adopted of these subprovisions was the requirement to wash hands before donning gloves. Adoption of hand hygiene provisions is crucial to food safety; poor hand hygiene has been cited as a key factor in the transmission of foodborne disease. A systematic review of 81 foodborne disease outbreaks attributed to food contaminated by food workers revealed that nearly all outbreaks were associated with poor hand hygiene, such as improper hand washing and bare-hand contact with food (22). When used properly, gloves can decrease pathogen transmission between food items and the hands of food workers (19). However, gloves are not always used appropriately, which should include changing gloves when necessary and washing hands before and after glove use. In an observational study of over 300 food workers, appropriate hand washing was less likely when gloves were worn (10).
The provisions regarding ill staff exclusion differed considerably among the states assessed. About 60% of states assessed adopted the 2013 Food Code requirement of exclusion of workers with diarrhea or vomiting until 24 h after symptom resolution. The same number of states included the norovirus-specific exclusion period in their codes, requiring that employees with a laboratory-confirmed diagnosis be excluded for 24 h after cessation of symptoms and then restricted for another 24 h after exclusion. Although all but one state required exclusion or restriction of ill food workers while symptomatic, compliance and enforcement may be lacking. In a survey of over 400 restaurant workers, nearly 60% reported working while ill in the previous year, and 20% had worked while ill with vomiting and diarrhea specifically (4). Nearly half of those who worked while ill indicated that their managers, to whom the responsibility of ill staff exclusion belongs, were not aware of their illness (4). This finding suggests that effective enforcement of the recommended regulations requires proper education of food handlers to foster appreciation of the health hazards of working while ill and the importance of reporting illnesses.
The timing of addition of provisions to the Food Code may affect the inclusion of these provisions in state regulations, because there may be a considerable lag between addition of provisions to the Food Code and state adoption due to state rule-making processes. The two least commonly adopted provisions included in this assessment were those requiring a CFPM and a contamination event response plan. These provisions were also the most recent ones incorporated into the Food Code; the provisions were added in 2011 as a supplement to the 2009 FDA Food Code (29) and were subsequently included in the 2013 Food Code. In contrast, the more commonly adopted provision requiring exclusion of ill staff until 24 h after symptoms was added to the Food Code in 2005 (28). Although a CFPM was not explicitly required in previous versions of the Food Code, previous versions allowed for this certification to fulfill the requirement that a person in charge demonstrate knowledge of food safety. Unlike the provision requiring a CFPM, the contamination response plan provision was not mentioned in previous versions of the Food Code. This provision is important for norovirus infection prevention because public vomiting events have been recognized as a cause of outbreaks (18, 32), and without proper cleaning the virus can persist on food preparation surfaces such as stainless steel and ceramic for up to 42 days (17).
The provisions requiring hand washing and prohibiting bare-hand contact with RTE food, which were the two most commonly adopted provisions, were included in Food Code versions as early as 1997 (previous versions of the Food Code were not available on the Internet for analysis). However, the least commonly adopted hand washing subprovision, requiring food workers to wash their hands before donning gloves, was added to the Food Code in 2001 (27). These comparisons revealed that although the year that the provision was incorporated into the Food Code may impact the uptake of these provisions into state food service regulations, other factors may influence state adoption of a provision.
Because the ultimate goal of food safety regulations is to decrease foodborne disease, we sought to explore potential associations between adoption of specific provisions and the frequency and characteristics of reported outbreaks. When we compared the outbreak reporting rates of states, we found that those states that adopted the specified provisions (requirement of a CFPM, prohibition of bare-hand contact with RTE foods, and 24-h exclusion of ill food workers) had lower median outbreak reporting rates than did those states that did not adopt these provisions, although these associations did not reach statistical significance. Controlling for adoption of the 24-h ill staff exclusion provision and the requirement for a CFPM, we found that adoption of the provision prohibiting bare-hand contact was significantly associated with decreased outbreak reporting rate. These findings suggest that adoption of these specific food service provisions may have an impact on reducing the rates of reported norovirus outbreaks.
States that adopted the requirement for a CFPM were significantly more likely than those without this requirement to implicate an ill food worker as the source of a reported outbreak. Because the responsibilities of a CFPM include ensuring that food workers are observing proper food safety protocols (31), including reporting of worker illness, this finding suggests that the presence of a CFPM is helpful for identifying workers who are in violation of the protocols by working while ill. In previous studies, the presence of a CFPM has had a protective effect on foodborne disease outbreaks, including those specifically caused by norovirus, and the identification of critical violations during restaurant inspections (5, 16).
We also found that states that had adopted the 24-h ill staff exclusion provision were significantly less likely to have outbreaks of a smaller size and shorter duration. This association may reflect the preferential reduction of shorter, smaller outbreaks caused by the relatively brief exposure period from ill food workers as opposed to outbreaks with more protracted periods of exposure, such as those involving foods contaminated during production or processing. Our analyses also indicated that states with the 24-h exclusion provision were significantly more likely to implicate bare-hand contact by an infectious food worker. However, these same states were not significantly associated with implication of ill food workers. Because outbreaks in which bare-hand contact by an infectious food worker was implicated are a subset of those in which an infectious food worker was implicated, this association may be spurious. However, one potential explanation is that those states that are excluding ill food workers are also more actively evaluating the activities of individuals in the kitchen to determine whether those individuals should be excluded and therefore identifying critical violations such as bare-hand contact with food. Another possibility is that the 24-h exclusion period may not be long enough to prevent transmission from a postsymptomatic infected food worker; although individuals infected with norovirus may have symptoms for only 1 to 3 days, they may shed the virus for an average of 4 weeks after infection (1). Therefore, these findings may indicate outbreaks in which ill food workers were excluded in accordance with the regulations but were still shedding infectious virus when they returned to work, suggesting that the 24-h postsymptomatic exclusion period for vomiting and diarrhea may not be sufficient because most norovirus infections are not diagnosed (9, 12, 25). This issue was further reinforced at the 2016 Conference for Food Protection (8), where the Conference voted to increase the postsymptomatic exclusion period for vomiting and diarrhea to 48 h in the 2017 Food Code to align with the postsymptomatic exclusion period for individuals actually diagnosed with norovirus infection.
Although the findings in this study are generally consistent with the notion that adoption of food safety provisions is associated with decreased incidence and improved management of foodborne outbreaks, some associations, such as that observed between the adoption of the 24-h ill staff exclusion and implication of bare-hand contact by an infectious food worker, were contradictory to other observed associations. This discrepancy suggests that the presence of other potential confounders, including variable compliance with these provisions and various reporting biases, may have resulted in spurious associations, and these results should be interpreted with caution. Because NORS is a passive surveillance system, reporting rates may not reflect the true number of outbreaks that occur in a particular state. Although all outbreaks are notifiable events and state health departments are strongly encouraged to report outbreaks to NORS, competing priorities and limited resources may restrict the number of outbreaks that are investigated and reported. These issues are likely reflected in the 100-fold difference in foodborne norovirus outbreak reporting rates between the highest and lowest reporting states (15). Additional food safety provisions may also be adopted at municipal levels that exceed the requirements adopted at the state level, and some restaurants, such as larger chains, may have their own policies that are more stringent than those stipulated by the state food service regulations. Promulgation of regulations or policies on any level does not guarantee compliance by employees or enforcement by management. Finally, our data were collected from outbreaks that occurred during 2009 through 2014, and many of these outbreaks predated adoption of provisions first introduced in the 2011 Food Code supplement (29). However, we analyzed the most recent regulations adopted as of September 2014, because regulations are subject to change at any point and changes do not necessarily follow a calendar year schedule. Therefore, a state’s food code may have changed several times during the time period of outbreak analysis, creating difficulties in determining the presence or absence of provisions in place during a specific outbreak.
Despite these limitations, to our knowledge, this study is the first analysis of adoption of specific food service provisions related to norovirus with an attempt to assess potential correlations between adoption of these provisions and reports of outbreaks. The results of this analysis highlight gaps in state adoption of key food service provisions for prevention of norovirus transmission in food service settings and reemphasize the importance of adopting the most recently recommended food service provisions as these are updated in accordance with the latest science. These results also highlight the difficulties of conducting an ecological analysis including numerous unobservable confounders. Improved reporting of foodborne norovirus outbreaks may provide more opportunities for the identification of effective prevention and control measures. Further research is needed to examine barriers to state adoption of recommended provisions, as well as municipal and restaurant implementation of and compliance with state regulations to better elucidate associations with foodborne transmission of norovirus and opportunities for prevention.
ACKNOWLEDGMENTS
This research was supported in part by appointments to the Research Participation Program at the Centers for Disease Control and Prevention (A.K. and K.S.) administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the CDC. This work was also supported in part by Agriculture and Food Research Initiative Competitive Grant 2011-68003-30395 from the U.S. Department of Agriculture, National Institute of Food and Agriculture. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
REFERENCES
- 1.Atmar RL, Opekun AR, Gilger MA, Estes MK, Crawford SE, Neill FH, and Graham DY. 2008. Norwalk virus shedding after experimental human infection. Emerg. Infect. Dis 14:1553–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atmar RL, Opekun AR, Gilger MA, Estes MK, Crawford SE, Neill FH, Ramani S, Hill H, Ferreira J, and Graham DY. 2013. Determination of the human infectious dose-50% for Norwalk virus. J. Infect. Dis 209:1016–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrabeig I, Rovira A, Buesa J, Bartolomé R, Pintó R, Prellezo H, and Domínguez À. 2010. Foodborne norovirus outbreak: the role of an asymptomatic food handler. BMC Infect. Dis 10:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carpenter L, Green AL, Norton DM, Frick R, Tobin-D’Angelo M, Reimann DW, Blade H, Nicholas DC, Egan JS, and Everstine K. 2013. Food worker experiences with and beliefs about working while ill. J. Food Prot 76:2146–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cates SC, Muth MK, Karns SA, Penne MA, Stone CN, Harrison JE, and Radke VJ. 2009. Certified kitchen managers: do they improve restaurant inspection outcomes? J. Food Prot 72:384–391. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. 2015. The National Outbreak Reporting System Available at: http://www.cdc.gov/NORS/. Accessed 6 August 2015.
- 7.Conference for Food Protection. 2015. Home page Available at: http://www.foodprotect.org/. Accessed 8 June 2015.
- 8.Conference for Food Protection. 2016. Council III issue recommendations Conference for Food Protection biennial meeting, Boise, ID. Available at: http://www.foodprotect.org/media/biennialmeeting/merged-issues-for-council-iii-for-printing-v2.pdf. Accessed 13 June 2016. [Google Scholar]
- 9.Franck KT, Lisby M, Fonager J, Schultz AC, Böttiger B, Villif A, Absalonsen H, and Ethelberg S. 2015. Sources of calicivirus contamination in foodborne outbreaks in Denmark, 2005–2011—the role of the asymptomatic food handler. J. Infect. Dis 211:563–570. [DOI] [PubMed] [Google Scholar]
- 10.Green LR, Radke V, Mason R, Bushnell L, Reimann DW, Mack JC, Motsinger MD, Stigger T, and Selman CA. 2007. Factors related to food worker hand hygiene practices. J. Food Prot 70:661–666. [DOI] [PubMed] [Google Scholar]
- 11.Hall AJ, Eisenbart VG, Etingüe AL, Gould LH, Lopman BA, and Parashar UD. 2012. Epidemiology of foodborne norovirus outbreaks, United States, 2001–2008. Emerg. Infect. Dis 18:1566–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall AJ, Rosenthal M, Gregoricus N, Greene SA, Ferguson J, Henao OL, Vinjé J, Lopman BA, Parashar UD, and Widdowson M-A. 2011. Incidence of acute gastroenteritis and role of norovirus, Georgia, USA, 2004–2005. Emerg. Infect. Dis 17:1381–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall AJ, Vinjé J, Lopman B, Park GW, Yen C, Gregoricus N, and Parashar U. 2011. Updated norovirus outbreak management and disease prevention guidelines U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta. [Google Scholar]
- 14.Hall AJ, Wikswo ME, Manikonda K, Roberts VA, Yoder JS, and Gould LH. 2013. Acute gastroenteritis surveillance through the National Outbreak Reporting System, United States. Emerg. Infect. Dis 19:1305–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall AJ, Wikswo ME, Pringle K, Gould H, and Parashar UD. 2014. Vital signs: foodborne norovirus outbreaks—United States, 2009–2012. Morb. Mortal. Wkly. Rep 63:491–495. [PMC free article] [PubMed] [Google Scholar]
- 16.Hedberg CW, Smith SJ, Kirkland E, Radke V, Jones TF, Selman CA, and Group E-NW. 2006. Systematic environmental evaluations to identify food safety differences between outbreak and nonoutbreak restaurants. J. Food Prot 69:2697–2702. [DOI] [PubMed] [Google Scholar]
- 17.Liu P, Chien Y-W, Papafragkou E, Hsiao H-M, Jaykus L-A, and Moe C. 2009. Persistence of human noroviruses on food preparation surfaces and human hands. Food Environ Virol 1:141–147. [Google Scholar]
- 18.Marks P, Vipond I, Regan F, Wedgwood K, Fey R, and Caul E. 2003. A school outbreak of Norwalk-like virus: evidence for airborne transmission. Epidemiol. Infect 131:727–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montville R, Chen Y, and Schaffner DW. 2001. Glove barriers to bacterial cross-contamination between hands to food. J. Food Prot 64:845–849. [DOI] [PubMed] [Google Scholar]
- 20.R Core Team. 2014. R: a language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- 21.Repp KK, and Keene WE. 2012. A point-source norovirus outbreak caused by exposure to fomites. J. Infect. Dis 205:1639–1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ross M, and Guzewich J. 1999. Evaluation of risks related to microbiological contamination of ready-to-eat food by food preparation workers and the effectiveness of interventions to minimize those risks. White paper U.S. Food and Drug Administration, Center for Food Safety and Applied Nutrition, College Park, MD. [Google Scholar]
- 23.Sarkar D 2008. Lattice: multivariate data visualization with R Springer, New York. [Google Scholar]
- 24.Teunis PF, Moe CL, Liu P, E Miller S, Lindesmith L, Baric RS, Le Pendu J, and Calderon RL. 2008. Norwalk virus: how infectious is it? J. Med. Virol 80:1468–1476. [DOI] [PubMed] [Google Scholar]
- 25.Thornley C, Hewitt J, Perumal L, Van Gessel S, Wong J, David S, Rapana J, Li S, Marshall J, and Greening G. 2013. Multiple outbreaks of a novel norovirus GII.4 linked to an infected postsymptomatic food handler. Epidemiol. Infect 141:1585–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Census Bureau. 2014. Annual estimates of the resident populations: April 1, 2010 to July 1, 2014 U.S. Census Bureau, Washington, DC. [Google Scholar]
- 27.U.S. Food and Drug Administration. 2001. Food Code 2001 U.S. Food and Drug Administration, College Park, MD. [Google Scholar]
- 28.U.S. Food and Drug Administration. 2005. Food Code 2005 U.S. Food and Drug Administration, College Park, MD. [Google Scholar]
- 29.U.S. Food and Drug Administration. 2011. Supplement to the 2009 Food Code U.S. Food and Drug Administration, College Park, MD. [Google Scholar]
- 30.U.S. Food and Drug Administration. 2013. Real progress in Food Code adoption U.S. Food and Drug Administration, College Park, MD. [Google Scholar]
- 31.U.S. Food and Drug Administration. 2013. Food Code 2013 U.S. Food and Drug Administration, College Park, MD. [Google Scholar]
- 32.Wikswo ME, Cortes J, Hall AJ, Vaughan G, Howard C, Gregoricus N, and Cramer EH. 2011. Disease transmission and passenger behaviors during a high morbidity norovirus outbreak on a cruise ship, January 2009. Clin. Infect. Dis 52:1116–1122. [DOI] [PubMed] [Google Scholar]


