ABSTRACT.
Latent Plasmodium vivax parasites in the liver known as hypnozoites activate causing malaria relapses months after the original infection. The putative initiation signal is unknown. Plasmodium falciparum infections appear to trigger P. vivax relapses and initiation of relapse may be triggered by hemolysis or fever. The U.S. Army hospital records from the Korean War (> 500,000 individual records) were used to determine whether there was an association between blood transfusion and vivax malaria relapse. Importantly, blood for transfusion was collected in the United States, so the risk of transmission of malaria parasites was minimal. Blood transfusion (largely for combat trauma) was a risk factor for subsequent vivax malaria (relative risk 2.54, 95% CI 2.15–2.99, P < 0.0001). As expected, blood transfusion was not a risk factor for subsequent dysentery, but transfusion was a risk factor for subsequent hepatitis. Blood transfusion causing an increased heme delivery to the liver and a subsequent redox signal within hepatocytes may partially explain hypnozoite activation leading to relapses of vivax malaria.
Relapsing malarias such as Plasmodium vivax and P. ovale have evolved a survival advantage of delayed relapses that allows them to bridge nontransmission seasons of several months. It is likely that most P. vivax infections in the tropics are actually the result of reactivation of latent hepatic parasites known as hypnozoites and not primary infections from mosquitoes. Therefore, achieving cure in a P. vivax patient involves not only clearing the bloodstream with effective schizonticidal drugs, but also killing residual hypnozoites to prevent relapse. This has proven difficult as latent hypnozoites are metabolically inactive in the liver and thus relatively insusceptible to most antimalarial drugs. The 8-aminoquinolines such as primaquine or tafenoquine are the only class of drugs that reliably prevent relapses, and their mode of action is unknown. Given the difficulties of investigating latent parasites in asymptomatic persons, we sought large historical datasets from the U.S. military that might allow a search for risk factors associated with P. vivax relapse.
Data sets large enough to contain the thousands of P. vivax infections required to see any significant effect are few but records of the U.S. Army in Korea in the 1950s had sufficient scale. 1 Every U.S. soldier hospitalized during the Korean War had a coded punch card prepared for enumeration purposes. These data were used at the time by the U.S. Army Medical Corps for administrative and logistical purposes such as noting how many soldiers were in hospital and how many units of blood had been used. In the 1970s, before these punch cards were destroyed, the data were transferred to computer tape format. We were thus able to obtain a dataset of > 500,000 records from the U.S. National Archives containing within them 7,046 P. vivax infections from 1950 to 1953. 2 Because the records could be linked by a unique identifier (soldier’s serial number) and only P. vivax infections were possible in Korea, individual P. vivax relapses could reliably be identified even though the great majority occurred after return to the United States. Blood transfusions and other diagnoses were recorded in the same data set. Importantly, blood for transfusion was collected in the United States, so the risk of transmission of malaria was minimal. The vast majority of blood transfusions were because of traumatic injuries occurring during combat on the Korean peninsula.
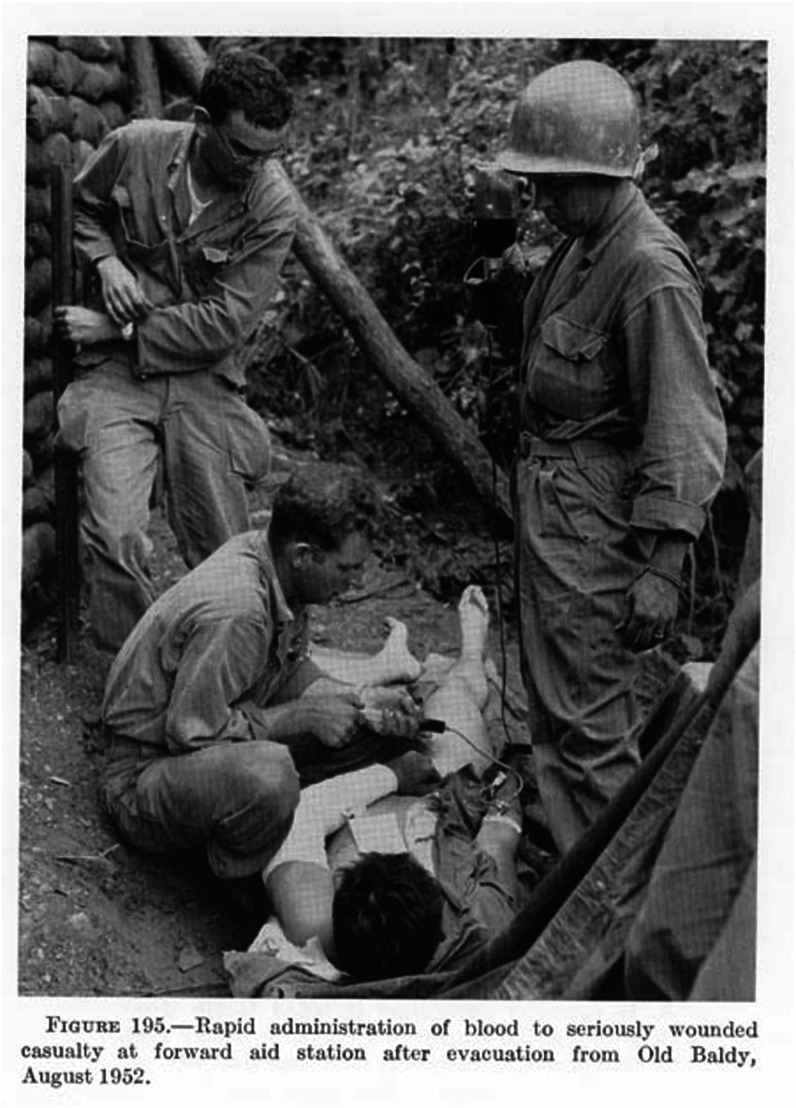
Our working hypothesis was that malaria relapses were triggered through increased heme metabolism in the liver from accelerated removal of older erythrocytes in the transfusion, which then resulted in hepatocyte apoptosis. Triggering by nonspecific immune stimulation because of other blood components such as leukocytes may have also contributed to relapse. The resulting relative risk of P. vivax relapse in U.S. soldiers following blood transfusion, compared with the risk with no prior transfusion are shown in Table 1 (relative risk 2.54, 95% CI 2.15–2.99, P < 0.0001). Blood transfusion was an important risk factor for malaria relapse, which could not have been primarily because of transmission from infected blood, as the blood units were all obtained from donors living in the United States, where malaria was no longer transmitted. Blood was transported from United States to Korea and not supplied from soldiers outside the United States. Dysentery, as another febrile infectious disease similar to malaria, was used for comparison. Hepatitis, as an alternative comparison diagnosis, was justified by the transfusions all occurring before the understanding of the source of post-transfusion hepatitis (no screening of blood for hepatitis viruses) and indicates that the records used could detect true infectious disease associations due to blood transfusions. Limiting records to infantry soldiers (the majority of all combat troops) was used to concentrate risk factors knowing that the vast majority of malaria exposures were in infantry units deployed in rural areas of Korea. See Figure 1 showing U.S. Army infantry in Korea and the field method of delivering a blood transfusion.
Table 1.
Relative risk of relapsing vivax malaria in U.S. Army soldiers from Korea 1950–1952 following receiving a prior blood transfusion, the vast majority of which were for combat injuries.
| Prevalence of vivax malaria | Relative risk of vivax malaria (95% CI) | P value | |
|---|---|---|---|
| Blood transfusion | No blood transfusion | ||
| 142/4,372 (3.2%) | 6,904/539,368 (1.2%) | 2.54 (2.15, 2.99) | < 0.0001 |
| Prevalence of dysentery | Relative risk of dysentery (95% CI) | – | |
| Blood transfusion | No blood transfusion | ||
| 8/4,372 (0.2%) | 1.189/539,368 (0.2%) | 0.83 (0.41, 1.66) | 0.60 |
| Prevalence of hepatitis | Relative risk of hepatitis (95% CI) | – | |
| Blood transfusion | No blood transfusion | ||
| 80/4,372 (1.8%) | 6,186/539,368 (1.1%) | 1.60 (1.28, 1.99) | < 0.0001 |
| Prevalence of vivax malaria (infantry only 1950–1951) | Relative risk of vivax malaria (95% CI) | – | |
| Blood transfusion | No blood transfusion | ||
| 78/1,556 (5.0%) | 1,995/125,763 (1.6%) | 3.16 (2.53, 3.94) | < 0.0001 |
Dysentery, another infectious disease predominately seen in summer, is presented as a negative comparison and hepatitis is used as a positive comparison as this pre-dated the ability to screen blood for hepatitis viruses. Infantry soldiers were more exposed to both malaria and combat injuries and serve as a sensitivity test.
Figure 1.
A wounded U.S. Army soldier is shown receiving an emergency blood transfusion during the Korean War in August 1953. 1 Photo from US Army historical section in the public domain: http://history.amedd.army.mil/booksdocs/wwii/blood/ch20fig195.jpg
As previously stated, true transfusion malaria (parasites in the donor blood causing infection in the recipient) cannot explain these findings as blood units were obtained from healthy donors in the United States and then shipped to Korea. The United States had no indigenous malaria transmission by 1951 which is why the thousands of imported cases from Korea were so concerning to public health authorities. 3 Although the number of other possible confirmatory transfusion malaria studies are very limited, one small series of post-transfusion malaria from pre-elimination 1960s Yugoslavia noted Plasmodium vivax cases all showed up at least a month after receiving blood. This delay is suggestive of reactivation or relapse rather than gradual increase from an exogenous inoculum where even very low parasitemias from injected blood break through into symptomatic infection within a matter of a few weeks at most. 4
Splenectomy has also been shown to often be followed by vivax and falciparum malaria infections. 5 The actual cause is uncertain as several factors could be operating including blood transfusions, which are often necessary because of blood loss in those requiring surgical splenectomy following trauma. Other possible contributing factors to P. vivax relapses following splenectomy include traumatic injury and loss of reticuloendothelial phagocytes in the spleen for immune surveillance. Although severe traumatic injury following land mine injury has been associated with malaria in Cambodia, the vast majority were due to P. falciparum recrudescence and not P. vivax relapse indicating that severe trauma per se may not be the critical factor for P. vivax relapses. 6, 7
There are several limitations to this report. The data used were collected for administrative or logistical purposes not research. Only limited information could be registered onto the then standard 102 column card format. Because only one record per hospitalization was prepared it is not possible to estimate the interval between blood transfusion and P. vivax relapse as the lengths of hospitalizations varied greatly. Transfusion was not recognized in the early 1950s as a risk for malaria relapse by the military medical officers caring for soldiers during the Korean War. Some of the associated malaria risk may have occurred due to evacuated soldiers not continuing their antimalarial prophylaxis of weekly chloroquine although there were policies to do so after leaving Korea. Once primaquine (15 mg daily for 14 days) was added to chloroquine given to U.S. soldiers on troopships returning to the United States from about 1952, P. vivax relapses from Korea in the United States largely disappeared demonstrating that the malaria episodes were true relapses from activated hypnozoites. 3, 8
Korean War blood transfusion records suggest that the mechanism that triggers malaria relapse by hypnozoite activation may include increased heme delivery to the hepatocyte. Such a hypothesis could make evolutionary sense if increased heme was a reflection of hemolysis because of a new Plasmodium infection, which would also be indicative of recent vector mosquito activity and indicate a favorable time to reinfect the bloodstream to find a new host. 9 Fever is another suggested relapse initiation factor and both fever and heme combined increase redox stress within the hepatocyte leading to apoptosis. 10 As hepatocyte apoptosis is an existential threat to the hypnozoite, it is possible that P. vivax relapse is conditional on cellular initiation of apoptosis, which the parasite then co-opts for its own purposes. Markers of hepatocyte damage such as transaminase elevation occurring after both natural and controlled human malaria infections even with very low parasitemias suggest that hepatocyte dysfunction may trigger relapse. 9, 11
The 8-aminoquinolines (primaquine and from 2018 tafenoquine) are the only current drugs to prevent relapsing malaria but their mechanism of action is not well understood. 12 The 8-aminoquinolines that are not redox active (nonhemolytic) are also not effective in preventing relapse as extensive work over decades have shown. 13 Given the very limited number of anti-relapse drugs, a better understanding of their mechanism especially as it pertains to hemolysis could provide opportunities to choose better companion medications that enhance relapse prevention rather than the reverse. This was recently described when artemisinin combination therapy (dihydro-artemisinin + piperaquine) was unsuccessfully used with tafenoquine during the INSPECTOR trial in Indonesia (J Kevin Baird, unpublished communication). Increases in redox activity produced by methylene blue have been shown to enhance 8-aminoquinoline efficacy against Chesson strain P. vivax relapses in unpublished studies done in the late 1940s by the National Institutes of Health. 14 This suggests that drug combinations that enhance 8-aminoquinoline redox activity inside the hepatocyte are an important focus for further investigation and may be analogous to blood transfusions increasing heme delivery to hepatocytes. Although difficult, more research into the biology of hypnozoite activation is needed both from historical epidemiology as in this report as well as more modern laboratory means to better understand how to prevent vivax malaria relapses. 15 Malaria elimination efforts, particularly in Latin America and Asia, would be greatly enhanced by improved means to stop P. vivax relapses, which are the majority of all cases once a country approaches disease elimination. 16 A simple inexpensive means to kill hypnozoites and thus stop P. vivax relapses would be of great benefit to malaria elimination efforts not-withstanding the need to balance the use of redox active drugs against hemolysis in the setting of glucose-6-phosphate dehydrogenase deficiency.
ACKNOWLEDGMENTS
We recognize and remember the service and sacrifice of all U.S. soldiers who served during the Korean War 1950–1954. Robert Commons is thanked for his analysis of World-Wide Antimalarial Resistance Network (WWARN) data of Plasmodium vivax treatment. We also thank many unnamed historians, medical librarians, and archivists who have unselfishly provided data and ideas for this article.
References
- 1. Kendrick DB Heaton LD Medical Department United States Army in World War II. Washington, DC: US Government Printing Office. [Google Scholar]
- 2. US Army , 2016. Hospital Admission Cards Korean War. Washington, DC: US National Archives. [Google Scholar]
- 3. Zottig VE Shanks GD , 2021. Historical perspective: the evolution of post-exposure prophylaxis for vivax malaria since the Korean War. MSMR 28: 8–10. [PubMed] [Google Scholar]
- 4. Lepes T , 1965. Induced malaria in Yugoslavia transmitted accidentally by blood transfusion. Bull World Health Organ 33: 856. [PMC free article] [PubMed] [Google Scholar]
- 5. Hossain MS et al. 2020. The risk of Plasmodium vivax parasitaemia after P. falciparum malaria: an individual patient data meta-analysis from the WorldWide Antimalarial Resistance Network. PLoS Med 17: e1003393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sundet M Heger T Husum H , 2004. Post‐injury malaria: a risk factor for wound infection and protracted recovery. Trop Med Int Health 9: 238–242. [DOI] [PubMed] [Google Scholar]
- 7. Shanks GD , 2015. Historical review: does stress provoke Plasmodium falciparum recrudescence? Trans R Soc Trop Med Hyg 109: 360–365. [DOI] [PubMed] [Google Scholar]
- 8. Archambeault CP , 1954. Mass antimalarial therapy in veterans returning from Korea. J Am Med Assoc 154: 1411–1415. [DOI] [PubMed] [Google Scholar]
- 9. Gozzelino R et al. 2012. Metabolic adaptation to tissue iron overload confers tolerance to malaria. Cell Host Microbe 12: 693–704. [DOI] [PubMed] [Google Scholar]
- 10. White NJ , 2011. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar J 10: 1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chughlay MF et al. 2020. Liver enzyme elevations in Plasmodium falciparum volunteer infection studies: findings and recommendations. Am J Trop Med Hyg 103: 378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lacerda MV et al. 2019. Single-dose tafenoquine to prevent relapse of Plasmodium vivax malaria. N Engl J Med 380: 215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Myint HY Berman J Walker L Pybus B Melendez V Baird JK Ohrt C , 2011. Improving the therapeutic index of 8-aminoquinolines by the use of drug combinations: review of the literature and proposal for future investigations. Am J Trop Med Hyg 85: 1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alving A Eichelburger L Arnold J Edgcomb J , 1949. The Clinical Testing of Antimalarial Drugs at Statesville Penitentiary. Chicago, IL: Rush University. [Google Scholar]
- 15. Olliaro PL Barnwell JW Barry A Mendis K Mueller I Reeder JC Shanks GD Snounou G Wongsrichanalai C , 2016. Implications of Plasmodium vivax biology for control, elimination, and research. Am J Trop Med Hyg 95 (Suppl 6): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Feachem RG et al. 2019. Malaria eradication within a generation: ambitious, achievable, and necessary. Lancet 394: 1056–1112. [DOI] [PubMed] [Google Scholar]