ABSTRACT.
The new Lancet Commission on water, sanitation, and hygiene (WASH) hopes to reimagine and guide global WASH efforts. This comes at a time when unequal living conditions and global disparities in response and recovery have been highlighted by the COVID-19 pandemic and recent large impact trials have delivered mostly disappointing results suggesting the need for radically more effective interventions to improve global public health. We find ourselves at an inflection point in global WASH with an opportunity to build new approaches with potentially more equitable, cost-effective, and scalable solutions. Mobile health (mHealth) technology is an important and innovative tool for WASH advances. Yet, the use of mHealth has not been equally distributed in terms of its benefits nor is its impact guaranteed. In resource-constrained settings, where technology can increase inequalities, special attention should be paid to structural and systemic hierarchies during the development of mHealth programs along with the acknowledgment and understanding of how these systems can reinforce the systematic exclusion of those most vulnerable. The WASH sector needs to adapt to a future that is innovative and inclusive with a commitment to rethinking the resources needed to enhance scope and impact. We highlight urban sanitation in Brazil as a case study to demonstrate that mHealth can support and enhance publicly funded infrastructure and to help reimagine WASH for postpandemic and beyond.
The Lancet announced a new Commission on water, sanitation, and hygiene 1, 2 (WASH) with the goal to reimagine global efforts in WASH and to support the WASH sector to meet current and impending environmental challenges such as climate change and urbanization. They also argue that WASH is a central pillar for gender equality and social and environmental justice. 1 This is prescient as the world has seen how dramatically inadequate and unequal living conditions are across cities, nations, and the globe amid the COVID-19 pandemic. 3, 4
The majority of the world lives in urban settings, 5 where insufficient and unequally distributed resources disproportionately affect the growing low-income population. As a result, one in seven people on earth lives in urban communities often called slums, 5 characterized by a lack of access to basic needs such as water, sanitation, solid waste services, and secure housing. The COVID-19 pandemic exposed the vulnerability of those living in these settings to infectious disease spread, and has exacerbated disproportionate health and economic burdens in these communities. 4 The global health community has an opportunity to innovate away from traditional approaches for WASH that have not addressed systemic inequities 6 and move toward supporting and enhancing cost-effective, scalable, sustainable, and community-derived solutions.
The COVID-19 pandemic highlighted WASH challenges of low-income urban populations where demographic density, poor housing conditions, and lack of access to clean water and adequate sanitation made preventive hygiene and social distancing practices impossible. 4, 7, 8 Urban areas often have greater WASH coverage 9; however, densely populated, poor urban communities experience substantial disparities in distribution, quality, and continuity of these services; often the result of historical and systemic racism and oppression. 10, 11 Often these sanitation systems are not adequate nor safely managed 12 with an estimated > 1.8 billion households in need of fecal sludge management services 13 and most wastewater produced in cities in low- and middle-income countries being untreated before discharge. 14 Poor sanitation puts residents at risk of disproportionate exposure to emerging and reemerging infectious disease which is pertinent with increasing globalization, urbanization, and climate change and the risk extends beyond the boundaries of these communities. 15, 16
Beyond the need for publicly funded infrastructure investments and professionalized WASH service delivery, numerous challenges exist that reduce the potential return on these investments. They include quality and consistency of services, user behavior change, communication between users and service providers, and community participation, which are key to realizing the benefits of WASH. As recently highlighted by mostly disappointing results from large impact trials, there is a need for radically more effective WASH interventions to improve global public health, 17 reflected in calls for “transformative” WASH. 1, 17, 18 For urban sanitation interventions, poor relationships between users and providers, and lack of collective action, stakeholder engagement, and sustained behavior change are all barriers to impactful sanitation solutions. 15, 19 – 22 Collective and individual behavior change is required for urban sanitation solutions to function, be sustainable, and provide the greatest health benefits. 21 Solutions to address barriers to effective urban sanitation interventions also need to be scalable to achieve greater impact.
During the COVID-19 pandemic, mobile health (mHealth) technology applications for population health have proliferated ranging from remote health service provision, 23 to health promotion campaigns 24 and to informing COVID-19 disease prevention and control strategies. 25 mHealth can provide a radical shift in how we think, act, and succeed in WASH, as we harness new communication modalities to coordinate action, inform consumers, change behaviors, provide actionable feedback, and problem solve. 26 Worldwide, there are > 5 billion mobile phone users; yet, the application and benefits of mobile technology have not been equally distributed. 27 mHealth applications have the capacity to address social and environmental justice issues. In terms of equity, the technology can gather large amounts of data directly from the underserved populations in need of sustained WASH solutions 28 and enhance the inclusion of vulnerable populations in the participatory construction of these solutions. 29 mHealth strategies have been successfully applied to a wide variety of public health problems 30, 31 including use for WASH-related conditions such as diarrheal disease surveillance, 32 enhancing child health and caregiver attention to WASH conditions, 33 and addressing COVID-19 response in Africa. 34, 35 There is growing evidence that mHealth may improve gender inequality 36 and address urban environmental injustice in many settings. 29, 37, 38
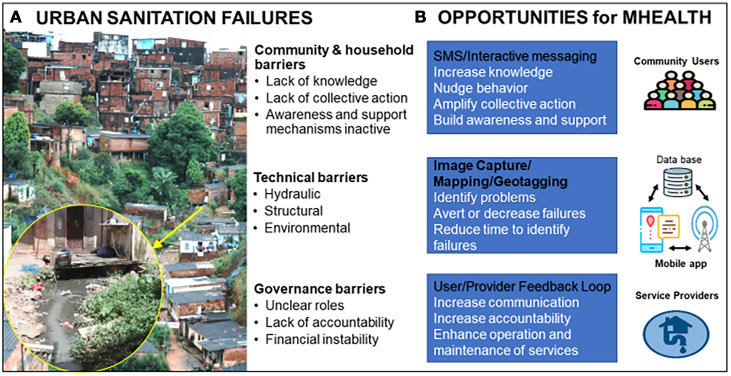
However, evidence is limited about successful integration of mHealth applications and their effectiveness for environmental health interventions—especially in urban communities where this work is critical. 39 – 42 Potential examples of mHealth deployment 43 – 45 to meet urban sanitation challenges are highlighted in Figure 1 and include interactive messages, uploading and geotagging of pictures to report and record the location of environmental issues, and user-provider feedback loops. 26 In many settings, evidence shows that mHealth approaches can be highly cost-effective and scalable. 46, 47 In contrast to technology-based approaches to WASH that disregard the “lived experience of poverty,” 48 mHealth may enable people to document and voice their own experiences and perceptions of the sanitation problems in their communities.
Figure 1.
Overview of urban sanitation challenges and opportunities for mHealth tools. This figure appears in color at www.ajtmh.org.
Yet, none of the potential benefits are guaranteed without focused and intentional mHealth development and delivery. Global challenges for mHealth delivery and implementation include user engagement and sustained use over time. 49 Additionally, in resource-constrained settings, where technology can increase inequalities, be used to oppress, or lead to a reliance on a neoliberal model for provision of privatized services, special attention should be paid to the process and approach for development of mHealth programs and applications along with the acknowledgment and understanding that these systems can reinforce the systematic exclusion of those most vulnerable. 50 – 52 Effective implementation and scalability of new technologies can be severely limited without key stakeholder involvement. Community-engaged and community-empowered approaches are needed to inform user-centered design of new technologies as well as best practices for implementation and broader dissemination. Responsibility and accountability for change, however, does not lie with these stakeholders, but rather with governments. We need to encourage the WASH sector to adapt and commit resources to build thoughtful and inclusive approaches that will lead to a better understanding and enhance the development of mHealth in efforts to support the reimagining of WASH.
Such tools may have the greatest potential for achieving impact in settings with high smartphone access and data connectivity and persistent sanitation problems typical of transitional economies where inequality is extreme. Brazil, a setting where 86% of the population is considered urban and most of the population has access to cell phones, offers an opportunity for learning and leading in how integration of communication technologies into WASH service delivery can enhance collective action and problem solving. Although 90% of Brazil is reported to have access to basic sanitation, only 48% of the total population is connected to a networked sewer and approximately 58% of the urban population. 53 Dramatic regional, municipal, and community-level disparities exist in access to a range of health and infrastructure services increasing health disparities, which are the result of historic, multi-dimensional, socioeconomic, and racial inequalities. 54 – 57 In densely populated informal and semi-formal urban communities of Brazil (often called favela communities), access to networked sewers is unevenly distributed and inadequate, which can result in environmental deficiencies such as flooding, contact with open sewers, and is associated with disease spread. 58, 59 Despite these challenges, Brazil is a leader in the development of cost-effective, simplified water and sanitation systems for densely populated urban settings called condominial water and sewerage systems. 60 In Salvador, Bahia, Brazil, the installation of >1,000 km of condominial sewer network pipes 60 resulted in city-wide health impacts including reduced intestinal parasites 61 and childhood diarrhea. 62 Yet, barriers for sustained success and expansion of the networked sewers remain in Brazil and they include community and household challenges, technical barriers, as well as challenges with governance. 63 These challenges also result from limited community participation and difficulty in adopting the behaviors and practices required for such systems. 60 Tackling urban sanitation challenges in densely populated communities through user-centered design of mHealth programs has not been a large focus but may have the potential to improve engagement, functioning, and sustainability of such systems. Furthermore, community-derived mHealth solutions to enhance urban sanitation for networked sewer systems can be adapted, expanded, and transferred to other situations that face barriers common in many urban sanitation settings.
Early evidence from building and piloting mHealth tools has demonstrated the potential for anytime and anywhere access to service, often overcoming barriers for those that are underserved. The application of mHealth tools in densely populated urban communities and the widespread use of cell phones among Brazilians in low-income communities may enable successful mHealth approaches in Brazil. Integrated communication technologies to drive improved WASH services in urban settings are largely untapped but given the need to maintain high-quality services to deliver value for money and protect public health, we foresee a future where the strengths of human connectivity and critical infrastructure can create the resilient systems of the future.
References
- 1. Amebelu A. et al., 2021. The Lancet Commission on water, sanitation and hygiene, and health. The Lancet. Available at: 10.1016/S0140-6736(21)02005-5. [DOI] [PubMed]
- 2. Lancet WASH Commission. Available at: https://wash-commission.com/. Accessed September 21, 2021.
- 3. Jensen N Kelly AH Avendano M , 2021. The COVID-19 pandemic underscores the need for an equity-focused global health agenda. Humanities and Social Sciences Communications 8: 15. [Google Scholar]
- 4. Corburn J et al. 2020. Slum health: arresting COVID-19 and improving well-being in urban informal settlements. J Urban Health 97: 348–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. 2019 Sustainable Development Goals Statistics. Available at: https://unstats.un.org/sdgs/report/2019/goal-11/. Accessed August 8, 2020.
- 6. Deshpande A et al., 2020 Mapping geographical inequalities in access to drinking water and sanitation facilities in low-income and middle-income countries, 2000– 17. Lancet Glob Health 8: e1162–e1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ahmad K Erqou S Shah N Nazir U Morrison AR Choudhary G Wu W-C , 2020. Association of poor housing conditions with COVID-19 incidence and mortality across US counties. PLoS One 15: e0241327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Donde OO Atoni E Muia AW Yillia PT , 2021. COVID-19 pandemic: water, sanitation and hygiene (WASH) as a critical control measure remains a major challenge in low-income countries. Water Res 191: 116793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. UNICEF/WHO, 2019. Progress on Household Drinking Water, Sanitation and Hygiene 2000--2017. Special focus on inequalities. New York, NY: United Nations Children’s Fund (UNICEF) and World Health Organization.
- 10. Tanana H, Combs J, Hoss A, 2021. Water is life: law, systemic racism, and water security in Indian country. Health Security. Available at: http://doi.org/10.1089/hs.2021.0034. [DOI] [PubMed] [Google Scholar]
- 11. Van de Lande L , 2013. Eliminating Discrimination and Inqualities in Access to Water and Sanitation. Geneva, Switzerland: UN Water.
- 12. Berendes D et al. 2017. The influence of household- and community-level sanitation and fecal sludge management on urban fecal contamination in households and drains and enteric infection in children. Am J Trop Med Hyg 96: 1404–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Berendes DM Sumner TA Brown JM , 2017. Safely managed sanitation for all means fecal sludge management for at least 1.8 billion people in low and middle income countries. Environ Sci Technol 51: 3074–3083. [DOI] [PubMed] [Google Scholar]
- 14. Jones ER van Vliet MTH Qadir M Bierkens MFP , 2021. Country-level and gridded estimates of wastewater production, collection, treatment and reuse. Earth Syst Sci Data 13: 237–254. [Google Scholar]
- 15. Kresch EP Lipscomb M Schechter L , 2020. Externalities and spillovers from sanitation and waste management in urban and rural neighborhoods. Applied Economic Perspectives and Policy 42: 395–420. [Google Scholar]
- 16. Thoradeniya T Jayasinghe S , 2021. COVID-19 and future pandemics: a global systems approach and relevance to SDGs. Global Health 17: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cumming O et al. 2019. The implications of three major new trials for the effect of water, sanitation and hygiene on childhood diarrhea and stunting: a consensus statement. BMC Med 17: 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Workman CL Cairns MR de Los Reyes FL 3rd Verbyla ME , 2021. Global water, sanitation, and hygiene approaches: anthropological contributions and future directions for engineering. Environ Eng Sci 38: 402–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McGranahan G , 2015. Realizing the right to sanitation in deprived urban communities: meeting the challenges of collective action, coproduction, affordability, and housing tenure. World Dev 68: 242–253. [Google Scholar]
- 20. Shiras T Cumming O Brown J Muneme B Nala R Dreibelbis R , 2018. Shared sanitation management and the role of social capital: findings from an urban sanitation intervention in Maputo, Mozambique. Int J Environ Res Public Health 15: 2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McGranahan G, Mitlin D, Diana , 2016. Learning from sustained success: how community-driven initiatives to improve urban sanitation can meet the challenges. World Dev 87: 307–317. [Google Scholar]
- 22. Ramos da Silva S Heller L de Campos Valadares J Cairncross S , 2010. Relationship (or its lack) between population and a water and sanitation service: a study of users’ perception in Vitoria (ES) Brazil. J Water Health 8: 764–778. [DOI] [PubMed] [Google Scholar]
- 23. Adans-Dester CP et al. 2020. Can mHealth technology help mitigate the effects of the COVID-19 pandemic? IEEE Open Journal of Engineering in Medicine and Biology 1: 243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Choudhury A Asan O Choudhury MM , 2021. Mobile health technology to improve maternal health awareness in tribal populations: mobile for mothers. J Am Med Inform Assoc 28: 2467–2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Loh P-S , 2020. Flipping the perspective in contract tracing. arXiv:2010.03806v2 [cs.CY].
- 26. Thomas E Brown J , 2021. Using feedback to improve accountability in global environmental health and engineering. Environ Sci Technol 55: 90–99. [DOI] [PubMed] [Google Scholar]
- 27. 2019 Smartphone Ownership Is Growing Rapidly Around the World, but Not Always Equally. Available at: https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/. Accessed April 19, 2020.
- 28. Hutchings M Dev A Palaniappan M Srinivasan V Ramanathan N Taylor J Ross N Luu P Oakland, CA: Pacific Institute, 115. [Google Scholar]
- 29. Phillips D , 2019. Sewage, Zika virus – and the team in Brazil mapping disease hotspots. The Guardian.
- 30. Marcolino MS Oliveira JAQ D’Agostino M Ribeiro AL Alkmim MBM Novillo-Ortiz D , 2018. The Impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth 6: e23–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alghamdi M Gashgari H Househ M , 2015. A systematic review of mobile health technology use in developing countries. Stud Health Technol Inform 213: 223–226. [PubMed] [Google Scholar]
- 32. Carstensen LS Tamason CC Sultana R Tulsiani SM Phelps MD Gurley ES Jensen PKM , 2019. The cholera phone: diarrheal disease surveillance by mobile phone in Bangladesh. Am J Trop Med Hyg 100: 510–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Biswas SK et al. 2021. Formative research for the design of a baby water, sanitation, and hygiene mobile health program in Bangladesh (CHoBI7 mobile health program). Am J Trop Med Hyg 104: 357–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nachega JB Leisegang R Kallay O Mills EJ Zumla A Lester RT , 2020. Mobile health technology for enhancing the COVID-19 response in Africa: a potential game changer? Am J Trop Med Hyg 103: 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Logie CH et al. 2021. Kukaa Salama (Staying Safe): study protocol for a pre/post-trial of an interactive mHealth intervention for increasing COVID-19 prevention practices with urban refugee youth in Kampala, Uganda. BMJ Open 11: e055530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jennings L Gagliardi L , 2013. Influence of mhealth interventions on gender relations in developing countries: a systematic literature review. Int J Equity Health 12: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jelks NO Smith-Perry DJ Fuller CH Stauber C , 2020. Participatory research in Northwest Atlanta’s Proctor Creek Watershed: using photovoice to explore environmental health risks at the water’s edge. Health Place 66: 102444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jelks NO, Hawthorne TL, Dai D, Fuller CH, Stauber C, 2018. Mapping the hidden hazards: community-led spatial data collection of street-level environmental stressors in a degraded, urban watershed. Int J Environ Res Public Health 15: 825. 10.3390/ijerph15040825. [DOI] [PMC free article] [PubMed]
- 39. Loo A et al. 2019. Development and field testing of low-cost, quantal microbial assays with volunteer reporting as scalable means of drinking water safety estimation. J Appl Microbiol 126: 1944–1954. [DOI] [PubMed] [Google Scholar]
- 40. George CM. et al. , 2020. Effects of a water, sanitation and hygiene mobile health program on diarrhea and child growth in Bangladesh: a cluster-randomized controlled trial of the CHoBI7 mobile health program. Clin Infect Dis 73. [DOI] [PMC free article] [PubMed]
- 41. Markle L Maganani A Katooka O Tiwari A Osbert N Larsen DA Winters B , 2017. A mobile platform enables unprecedented sanitation uptake in Zambia. PLoS Negl Trop Dis 11: e0005131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zohura F et al. 2020. Effect of a water, sanitation and hygiene program on handwashing with soap among household members of diarrhoea patients in healthcare facilities in Bangladesh: a cluster-randomised controlled trial of the CHoBI7 mobile health program. Trop Med Int Health 25: 1008–1015. [DOI] [PubMed] [Google Scholar]
- 43. Dugas M Gao GG Agarwal R , 2020. Unpacking mHealth interventions: a systematic review of behavior change techniques used in randomized controlled trials assessing mHealth effectiveness. Digit Health 6. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7036494/pdf/10.1177_2055207620905411.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Agarwal A, Chaudhuri U, Chaudhuri S, Seetharaman G, 2014. Detection of potential mosquito breeding sites based on community sourced geotagged images. Proc. SPIE 9089, Geospatial InfoFusion and Video Analytics IV, and Motion Imagery for ISR and Situational Awareness II, 90890M, July 3, 2014. Available at: 10.1117/12.2058121. [DOI] [Google Scholar]
- 45. Donaire-Gonzalez D Valentín A de Nazelle A Ambros A Carrasco-Turigas G Seto E Jerrett M Nieuwenhuijsen MJ , 2016. Benefits of mobile phone technology for personal environmental monitoring. JMIR Mhealth Uhealth 4: e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.WHO Global Observatory for eHealth,2011. mHealth: New Horizons for Health through Mobile Technologies: Second Global Survey on eHealth. Geneva, Switzerland: World Health Organization. Available at: https://apps.who.int/iris/handle/10665/44607.
- 47. Iribarren SJ Cato K Falzon L Stone PW , 2017. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One 12: e0170581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ray I Smith KR , 2021. Towards safe drinking water and clean cooking for all. Lancet Glob Health 9: e361–e365. [DOI] [PubMed] [Google Scholar]
- 49. Trude ACB et al., 2021. A WhatsApp-Based Intervention to Improve Maternal Social Support and Maternal--Child Health in Southern Brazil: The Text-Message Intervention to Enhance Social Support (TIES) Feasibility Study. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. Available at: 10.1177/00469580211048701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hope K Gina G Zonayed M Shelby LG Julia H Carolin Elizabeth G Philip Y Roger WM Iris R Joseph A Mark EM Rami M Impacts of Information Technology on Patient Care and Empowerment. Hershey, PA: IGI Global, 322–342. [Google Scholar]
- 51. Nemer D , 2018. Wired mobile phones: the case of community technology centers in favelas of Brazil. Inf Technol Dev 24: 461–481. [Google Scholar]
- 52. de Souza e Silva A Sutko DM Salis FA de Souza e Silva C , 2011. Mobile phone appropriation in the favelas of Rio de Janeiro, Brazil. New Media Soc 13: 411–426. [Google Scholar]
- 53. von Sperling M, 2016. Urban wastewater treatment in Brazil. Available at: https://publications.iadb.org/publications/english/document/Urban-Wastewater-Treatment-in-Brazil.pdf.
- 54. Bortz M Kano M Ramroth H Barcellos C Weaver SR Rothenberg R Magalhaes M , 2015. Disaggregating health inequalities within Rio de Janeiro, Brazil, 2002–2010, by applying an urban health inequality index. Cad Saude Publica 31 (Suppl 1): 107–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Snyder RE Jaimes G Riley LW Faerstein E Corburn J , 2014. A comparison of social and spatial determinants of health between formal and informal settlements in a large metropolitan setting in Brazil. J Urban Health 91: 432–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nassif Pires L, Carvalho LBd, Lederman Rawet E, 2021. Multi-dimensional inequality and COVID-19 in Brazil. Invest Econ 80: 33–58. [Google Scholar]
- 57. Raupp L Fávaro TR Cunha GM Santos RV , 2017. Sanitation and racial inequality conditions in urban Brazil: an analysis focused on the indigenous population based on the 2010 Population Census. Rev Bras Epidemiol 20: 1–15. [DOI] [PubMed] [Google Scholar]
- 58. Hagan JE et al. 2016. Spatiotemporal determinants of urban leptospirosis transmission: four-year prospective cohort study of slum residents in Brazil. PLoS Negl Trop Dis 10: e0004275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Reis RB et al. 2008. Impact of environment and social gradient on Leptospira infection in urban slums. PLoS Negl Trop Dis 2: e228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Melo JC, 2005. The Experience of Condominial Water and Sewerage Systems in Brazil: Case Studies from Brasilia, Salvador and Parauapebas. Lima, Peru: World Bank, Water and Sanitation Program.
- 61. Barreto ML et al. 2010. Impact of a citywide sanitation program in northeast Brazil on intestinal parasites infection in young children. Environ Health Perspect 118: 1637–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Barreto ML et al. 2007. Effect of city-wide sanitation programme on reduction in rate of childhood diarrhoea in northeast Brazil: assessment by two cohort studies. Lancet 370: 1622–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kennedy-Walker R Mehta N Thomas S Gambrill M , 2020. Connecting the Unconnected: Approaches for Getting Households to Connect to Sewerage Networks. Washington, DC: World Bank. [Google Scholar]