Abstract
Volar distal radioulnar joint (DRUJ) dislocation is a rare clinical entity that is commonly missed during initial evaluation. We report a case of a locked volar DRUJ dislocation associated with ulnar artery transection in a 53-year-old patient. He presented to the hospital after sustaining an injury to the right wrist by a heavy machinery object. Clinical evaluation showed contused skin, decreased sensation in the ulnar 2 digits, and an audible radial pulse, assessed using Doppler. Imaging studies revealed a locked volar DRUJ dislocation associated with a nondisplaced fracture of the distal ulna. Open reduction was performed with decompression of the Guyon canal. The ulnar artery was found to be transected and was primarily repaired. After the surgery, the patient showed marked improvement in neurological symptoms and patent ulnar artery flow. This case highlights the importance of meticulous evaluation and presents the heterogeneity of a volar DRUJ dislocation.
Key words: Distal ulna fracture, Neurovascular injury, Ulnar artery transection, Ulnar nerve compression, Volar distal radioulnar joint dislocation
Volar distal radioulnar joint (DRUJ) dislocation is a rare clinical entity. This condition is frequently misdiagnosed in about 50% of cases.1 In 1777, Desault2 reported the first case of isolated volar DRUJ dislocation in cadavers and published it in 1791. In 2017, Alnusif et al3 reported a case of median nerve compression secondary to a volar DRUJ dislocation associated with a distal radius fracture, the symptoms of which resolved after decompression. However, no previous reports have indicated that this clinical condition might be accompanied by an arterial injury. Herein, we describe a case of a locked volar DRUJ dislocation associated with a complete ulnar artery transection injury and an ulnar nerve compression injury. Following the Strengthening the Reporting of Observational Studies in Epidemiology guidelines, we discussed the mechanism of the injury, the importance of thorough clinical and radiological evaluations, and forearm arterial injuries.
Case Report
A healthy 53-year-old man presented to the emergency department after sustaining an injury by a heavy object that fell directly on his right wrist and forearm while his forearm was pronated. The patient complained of immediate pain associated with moderate numbness in the ulnar digits. Clinical examination showed a semisupinated right forearm, with significant wrist swelling, accompanied by the loss of the normal contour of the distal ulnar prominence with contused skin. The patient was able to move his fingers, but his wrist and forearm motions were significantly limited. Sensory and motor assessments of the radial, median, and ulnar nerves revealed a marked decrease in sensation in the volar aspect of the ulnar 2 digits, with significant weakness during abduction and adduction of the fingers. The palpation of the distal radial and ulnar pulses was not possible because of the presence of significant swelling. The color and temperature of the hand were normal. The capillary refill was less than 2 seconds in all fingers. The perfusion of the hand was normal. Using a hand-held Doppler device, the radial pulse was examined and found to be detectable. Pain impeded further assessment.
Radiographs of the wrist demonstrated a complete DRUJ dislocation and an ulnar styloid fracture (Fig. 1). A lateral radiograph of the wrist could not be obtained as a result of pain. Instead, a computed tomography (CT) scan was performed, which showed comminution involving the ulnar head, with an undisplaced fracture extending to the metadisphysis of the ulna and the volar locked dislocation, as evidenced by ulnar impaction on the volar rim of the radius (Fig. 2A–E). Because of the comminution involving the distal ulna as well as the ulnar impaction, closed reduction was not attempted. Additionally, the patient presented with the signs of ulnar nerve compression, therefore he was urgently taken to the operative room for the open reduction of the DRUJ and for ulnar nerve decompression. With the patient in the supine position with an arm board, a tourniquet was applied to the proximal upper arm. An extended volar ulnar approach using the interval between the flexor carpi ulnaris and ulnar neurovascular structures on the ulnar side and the flexor digitorum profundus on the radial side was taken. Upon dissection, the ulnar artery was found to be completely transected, with thrombosed edges on both ends, especially at the proximal end (Fig. 3A). The ulnar nerve was found to be intact, with mild contusions proximal to the wrist crease. The dissection was performed distally, and the Guyon canal was released. Given the patient’s significant swelling, carpal tunnel release was performed as part of the procedure using the same approach to decrease the risk of latent median nerve compression due to edema. The ulnar head was found to be dislocated volarly and buttonholed through the volar capsule and pronator quadratus muscle. The muscles fibers of the ulnar aspect of the pronator quadratus were severely damaged because of the volar DRUJ dislocation. A gentle dissection was performed to free the ulnar head from the soft tissue, which was reduced back to its normal position. The volar capsule was repaired in a standard fashion using Ethibond Excel 2.0 (Ethicon Inc, Somerville, NJ) suture, with the wrist in full supination to reduce the risk of overtightening the volar capsule and limiting future supination. Stability was assessed after the reduction, which indicated that the DRUJ was unstable. A vascular surgeon performed thrombectomy, followed by end-to-end primary anastomosis of the ulnar artery (Fig. 3B). Then, radioulnar transfixation was performed using Kirschner wires with the forearm in full supination. Distal radioulnar joint alignment was checked and confirmed using image intensification. The ulnar styloid fracture was found to be comminuted and undisplaced; therefore, the decision to treat it conservatively without fixation was made. The limb was then splinted in an above-elbow backslab in supination. The procedure was performed by a hand fellowship-trained hand surgeon.
Figure 1.
Posteroanterior radiograph of the right wrist joint demonstrating a dislocation of the DRUJ.
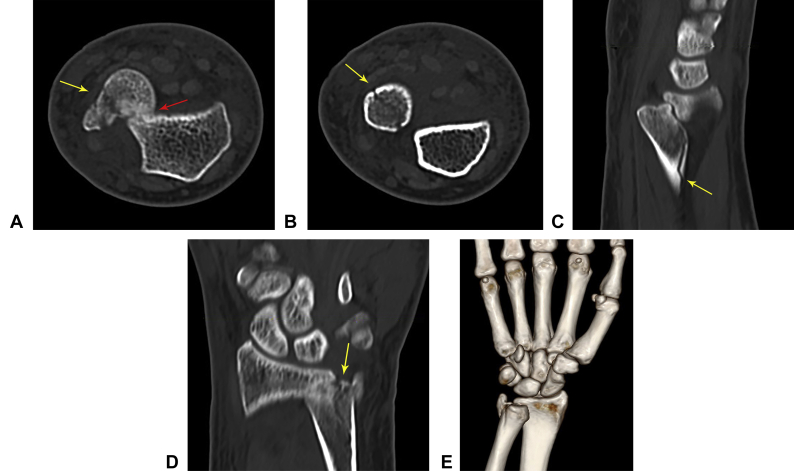
Figure 2.
A Axial CT image demonstrating comminution of the ulnar styloid and head (yellow arrow) as well as the perching of the ulnar head on the volar aspect of the distal radius, indicating a fixed dislocation (red arrow). B Axial CT image demonstrating a nondisplaced fracture extending to the metadiaphyseal region of the distal ulna (yellow arrow). C Sagittal CT image demonstrating a nondisplaced fracture extending to the metadiaphyseal region of the distal ulna (yellow arrow) as well as the locked volar DRUJ dislocation. D Coronal CT image demonstrating significant comminution of the ulnar fovea (yellow arrow). E Three-dimensional reformatted CT image demonstrating a volar DRUJ dislocation.
Figure 3.
A Intraoperative image showing clear ulnar artery transection with thrombosed ends. B Intraoperative image showing a repaired ulnar artery.
After the surgery, the patient showed partial yet significant improvement in neurological symptoms. Physical examination showed a capillary refill of less than 2 seconds, and patent arterial flow distal to the anastomosis was detected using Doppler ultrasound. Unfractionated heparin, 5,000 units subcutaneously, was given to the patient twice a day during his 5-day hospital stay, which was followed by a daily dose of 100 mg of aspirin for a total of 6 weeks after discharge. Postoperative radiographs showed excellent alignment of the DRUJ and an obious distal ulna fracture, which was evident in the preoperative CT scan (Fig. 4A, B). At the 2-week follow-up, the wound showed good healing, and the clips were removed. Neurological examination revealed full recovery of ulnar nerve symptoms. The above-elbow backslab was discontinued at week 4, and a full below-the-elbow cast was applied for 2 more weeks. At the 6-week follow-up visit, the Kirschner wires were removed and physical therapy was prescribed. At 12 weeks after the surgery, clinical examination revealed an improvement in the range of motion of the right wrist and forearm, and strengthening exercises were started.
Figure 4.
A Postoperative posteroanterior radiograph of the right wrist joint demonstrating a well-reduced DRUJ held in place by 2 Kirschner wires and well-aligned fractures of the distal ulna. B Postoperative lateral radiograph of the right wrist joint demonstrating a well-reduced DRUJ.
At the final 10-month follow-up, the patient was pain-free and had returned to work, with no restrictions. His only complaint was an electric-like sensation along the distribution of the dorsal ulnar cutaneous nerve. He did not complain of ulnar-sided wrist pain or clicks. Sensation over the palmar aspect the ulnar 2 digits was normal. Motor examination of the ulnar nerve showed normal adduction and abduction strength for all fingers. Both radial and ulnar pulses were palpable. An assessment of the DRUJ in supination, pronation, and neutral positions revealed a stable joint without any appreciable translation or painful motion. The range of motion (measured using a goniometer) was as follows: the injured versus normal wrist extension and flexion were 45° and 78° versus 65° and 80°, respectively, whereas the injured versus normal forearm pronation and supination were 79° and 80° versus 80° and 83°, respectively. The handgrip strength was measured 4 times on both sides using a handgrip dynamometer. The average handgrip strength on the right was 81% relative to that on the left side, with values of 30 and 37 kg, respectively. The Disabilities of the Arm, Shoulder and Hand score was 4.2/100, whereas the Mayo wrist score was 90/100.4,5 The radiographs revealed an excellent bony union, without arthritic changes, deformity, or instability (Fig. 5A, B).
Figure 5.
A Posteroanterior radiograph of the right wrist joint at 10 months showing healed distal ulna and ulnar styloid fractures as well as a reduced DRUJ without arthrosis. B Lateral radiograph of the right wrist joint at 10 months showing a well-reduced DRUJ.
Discussion
Only sporadic case reports and few case series have described volar DRUJ dislocations and their management. Consequently, the management of volar DRUJ dislocation injuries is controversial, and its outcome is still unclear. Mulford et al6 reviewed the literature and found 22 volar DRUJ case reports, 14 of which were misdiagnosed. It is important to note that there has been no report in the literature indicating that a volar DRUJ dislocation might be associated with an arterial injury or ulnar nerve injury. Therefore, to our knowledge, this is the first report to describe a complete transection injury of the ulnar artery and an ulnar nerve compression injury associated with a locked volar DRUJ dislocation.
The mechanism of the injury in our case is unique, in that it was not a pure rotational injury, as has been reported in the literature.7 Typically, a volar DRUJ dislocation occurs when hypersupination is inflicted on the forearm. Subsequently, the distal ulna becomes volar in relation to the distal radius; hence, it is called a volar DRUJ dislocation. However, in the present case, the patient had suffered a direct blow to the distal ulna in a posterior-to-anterior direction, with significant compression of his forearm between 2 heavy machinery objects. The obliquity of the fracture and the comminution signify the severity of the injury and confirm that the vector of the force was perpendicular to the forearm rather than rotational.
Closed reduction was not attempted in the present case, and the treating surgeon proceeded directly to open reduction for 2 main reasons: the presence of comminution in the distal ulna and the presence of significant perching of the distal ulna on the volar rim of the radius. It is possible that with closed reduction attempts, the fracture would have propagated and become complete, thus converting a relatively simple injury to a more complex one. Garrigues and Aldridge8 described the appearance of perching on a CT image, wherein the impaction of the ulnar head on the distal radius “locked” the injury. Such an appearance has been reported in various injuries; for example, in a locked posterior hip dislocation, the femoral head perches on the rim of the acetabulum, making the dislocation irreducible. A prereduction CT scan is extremely valuable in these cases and can help surgeons select a more appropriate treatment strategy. Of note, the radiographs failed to demonstrate the comminution or the impaction of the distal ulna; therefore, plain radiographs may underestimate the severity of an injury.7
Upper-extremity arterial injuries are extremely rare, accounting for 0.74% of admissions for trauma. Franz et al9 conducted a retrospective study of upper-extremity arterial injuries and found that 73% of them occurred because of a penetrating injury as opposed to 27% that occurred because of blunt trauma. Moreover, an ulnar artery injury occurred in 32.1% of the cases. Arterial injuries of the forearm can have a very subtle presentation because of the presence of excellent collateral circulation. Having a commonly missed injury that is accompanied by a subtle neurovascular injury can pose a diagnostic challenge, and there is a potential to overlook both injuries.10 In the present case, the significant swelling and deformity precluded the physician from assessing arterial pulses; however, the radial artery pulse was detectable using Doppler examination. The peripheral perfusion of the hand, as evidenced by the normal capillary refill, color, temperature, and detectable radial pulse assessed using Doppler examination, led to the conclusion that an arterial injury was very unlikely. However, in retrospect, multiple soft signs, including the proximity of the injury to the ulnar artery, ulnar nerve compression symptoms and signs, and mechanism of the injury (crush injury), could have indicated the possibility of an arterial injury. The diagnosis of serious injuries with a subtle presentation requires a vigilant physician and a thorough clinical evaluation coupled with the appropriate radiological investigations.
Repair versus ligation of arterial injuries in the forearm with intact distal circulation is a controversial topic. The loss of bone mass, muscular mass, and strength has been reported in patients who have undergone the ligation of a single vessel.10 For this reason, the surgical repair of arterial injuries in the forearm with intact distal circulation is often recommended.10 Thus, one must be prepared for the possibility of a vascular injury and the need for a vascular repair.
In conclusion, the case report here presents unique associated injuries with a locked volar DRUJ dislocation. It highlights the importance of meticulous evaluation and vigilance when treating rare injuries. We strongly recommend that physicians obtain CT scans before a closed reduction is attempted, and that they proceed with a high index of suspicion regarding neurovascular injury when encountering a volar DRUJ dislocation.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Heiple K.G., Freehafer A.A., Van't Hof A. Isolated traumatic dislocation of the distal end of the ulna or distal radio-ulnar joint. J Boint Joint Surg Am. 1962;44(7):1387–1394. [PubMed] [Google Scholar]
- 2.Desault M. Extrait d’un memoire de M. Desault sur la luxation de Pextremite inferieure du cubitus/ chir. 1791;1:78–87. [Google Scholar]
- 3.Alnusif N., Aldebeyan S., Reindl R. Volar distal radioulnar joint dislocation associated with acute median nerve neuropathy and a distal radius fracture. Case Rep Orthop. 2017;2017 doi: 10.1155/2017/5674098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Germann G., Wind G., Harth A. The DASH (Disability of Arm-Shoulder-Hand) Questionnaire–a new instrument for evaluating upper extremity treatment outcome. Handchir Mikrochir Plast Chir. 1999;31(3):149–152. doi: 10.1055/s-1999-13902. [DOI] [PubMed] [Google Scholar]
- 5.Cooney W.P., Bussey R., Dobyns J.H., Linscheid R.L. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;214:136–147. [PubMed] [Google Scholar]
- 6.Mulford J.S., Jansen S., Axelrod T.S. Isolated volar distal radioulnar joint dislocation. J Trauma. 2010;68(1):E23–E25. doi: 10.1097/TA.0b013e3181568db2. [DOI] [PubMed] [Google Scholar]
- 7.Dameron T.B., Jr. Traumatic dislocation of the distal radio-ulnar joint. Clin Orthop Relat Res. 1972;83:55–63. doi: 10.1097/00003086-197203000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Garrigues G.E., Aldridge J.M., III Acute irreducible distal radioulnar joint dislocation: a case report. J Bone Joint Surg Am. 2007;89(7):1594–1597. doi: 10.2106/JBJS.F.01566. [DOI] [PubMed] [Google Scholar]
- 9.Franz R.W., Skytta C.K., Shah K.J., Hartman J.F., Wright M.L. A five-year review of management of upper-extremity arterial injuries at an urban level I trauma center. Ann Vasc Surg. 2012;26(5):655–664. doi: 10.1016/j.avsg.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Lebowitz C., Matzon J.L. Arterial injury in the upper extremity: evaluation, strategies, and anticoagulation management. Hand Clin. 2018;34(1):85–95. doi: 10.1016/j.hcl.2017.09.009. [DOI] [PubMed] [Google Scholar]