Abstract
Purpose
There is a paucity of literature examining the trajectory of meaningful clinical improvement after distal radius fracture (DRF) fixation. We sought to answer the following questions: (1) When do patients meet the minimum clinically important difference (MCID) in the Quick–Disabilities in Arm, Shoulder, and Hand questionnaire (QuickDASH) score change after DRF fixation? (2) What gains in terms of number of MCIDs achieved (as measured by QuickDASH) do patients make as they recover from DRF fixation? (3) What patient and injury factors are characteristic of patients who meet or do not meet the average recovery trajectory?
Methods
We performed a retrospective review of an institutional database of DRF patients treated with operative fixation. The change in QuickDASH scores from before surgery to approximate follow-up intervals of 0 to 2 months, 3 to 6 months, and a minimum of 9 of 12 months was assessed, in which a delta of 14 reflected the MCID. The change in QuickDASH score from before surgery to each follow-up interval was divided by 14 to determine the number of MCIDs, representing appreciable clinical improvement. Patient characteristics were compared between those who did and did not reach average levels of clinical improvement.
Results
The study included 173 patients. Mean QuickDASH score before surgery was 74 (SD, 19; range, 0–100). After surgery, this improved to 50 (SD, 24; range, 0–100) by 0 to 2 months, 22 (SD, 22; range, 0–98) by 3 to 6 months, and 9.8 (SD, 15; range, 0–75) by a minimum of 9 to 12 months. Overall, 96% of patients reached the MCID by 1 year. Mean cumulative number of MCIDs achieved (ie, number of 14-point decreases in QuickDASH score) at each interval was 1.57, 3.64, and 4.43, respectively. Assuming 4.43 represents maximum average improvement at 1 year, patients achieved 35% (1.57 of 4.43) of recovery from 0 to 2 months after surgery and 82% (3.64 of 4.43) of recovery by 3 to 6 months after surgery. There appeared to be no difference in terms of age, sex, or body mass index with respect to these findings.
Conclusions
Overall, 96% of patients undergoing DRF fixation will achieve one QuickDASH MCID by 1 year after surgery. Patients achieved over 80% of total expected functional improvement by 3 to 6 months after surgery, which appeared to be irrespective of age, sex, or body mass index.
Type of study/level of evidence
Therapeutic IV.
Key words: Distal radius fracture, Minimum clinically important difference, Patient-reported outcome measures, QuickDASH
Patient-reported outcome measures (PROMs) are frequently used tools in clinical care and research across orthopedic surgery. Specifically within hand surgery, PROMs have been used to quantify surgical outcomes, including in distal radius fracture (DRF) fixation.1, 2, 3, 4, 5, 6 One commonly used PROM in hand surgery is the Quick–Disabilities of the Arm, Shoulder, and Hand questionnaire (QuickDASH), an instrument considered to be a reliable and valid measure of upper-extremity function in this patient population.7,8 Several previous investigations have helped establish the trajectory of recovery using an interval assessment of QuickDASH and Patient-Related Wrist Evaluation scores.9, 10, 11 Despite the increased use of PROMs, it remains challenging to describe how changes in functional outcome scores are reflected in the patient clinical experience.
The minimum clinically important difference (MCID) is a method proposed to understand how a change in QuickDASH score may be experienced clinically. The MCID of a given PROM is the change in score that results in a patient who experiences a clinically relevant improvement (or decline) in symptoms.12, 13, 14 In the case of QuickDASH, a commonly used value is 14.13 Although several prior investigations identified patient and surgical factors that affect QuickDASH scores after DRF fixation,10,15, 16, 17, 18, 19 there are limited data on the timing of when patients achieve a change reflective of the MCID. Furthermore, there is a paucity of literature using the MCID to evaluate the level of functional recovery for patients after surgical fixation of DRFs.
We sought to answer the following study questions: (1) When do patients meet the MCID in QuickDASH score change after DRF fixation? (2) What gains in terms of the number of MCIDs achieved (as measured by QuickDASH) do patients make as they recover from DRF fixation? and (3) What patient and injury factors are characteristic of patients who meet or do not meet the average recovery trajectory? We hypothesized that the vast majority of patients would meet the MCID after surgery. Furthermore, we suspected that this improvement would be the case irrespective of age, sex, or body mass index (BMI). In addition, we hypothesized that many patients would demonstrate continued improvement in QuickDASH scores consistent with achieving multiple MCIDs over the year after operative intervention, which would suggest continued clinical recovery over time.
Materials and Methods
Our institutional review board approved this study (Protocol 2016P000035).
We performed a retrospective review of an institutional database containing data collected over 5 years for patients presenting to a single, urban, level 1 trauma center with a DRF treated with operative fixation using a volar plate. Standard postoperative protocol begins with immobilization in a removable orthosis with progression to a standardized range of motion (ROM) regimen at 10 days.
We extracted the following patient characteristics from the database: age (years), sex (male or female), insurance status (Medicare, Medicaid, private, workers’ compensation, or other), BMI, hand dominance (right or left), injury side (right or left), injury mechanism (fall from a standing height, fall from a height, motor vehicle collision, or other), and QuickDASH score. Developed based on the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire,20 the QuickDASH is a shorter PROM that is a reliable and valid measure of upper-extremity functional status and symptoms. Specifically with DRFs, the QuickDASH has been shown to demonstrate good concurrent validity and responsiveness compared with the DASH.7
Only patients with a preoperative QuickDASH score as well as at least one follow-up QuickDASH score were included (n = 173). Patients who only had a preoperative QuickDASH score but not one or more follow-up surveys completed were excluded from the study (n = 187). Overall descriptive statistics for the entire patient sample were calculated and reported. The QuickDASH scores were assessed at each follow-up clinic visit, which were grouped into the approximate ranges of 0 to 2 months, 3 to 6 months, and a minimum of 9 to 12 months.
The change in QuickDASH score representative of the MCID, reflective of the smallest clinical improvement or decline appreciated by patients, was defined as 14; it is a commonly used value in the hand surgery literature and was originally described using an anchor-based MCID estimation approach.13 The proportion of patients achieving a change in QuickDASH score reflective of the MCID from before surgery to each follow-up point was determined. In addition, at each follow-up point, the total improvement or decline in QuickDASH scores among all patients was calculated. We subsequently divided this number by 14 to obtain the average number of MCIDs achieved at each follow-up point in the patient sample; this represented the degree of continued clinical improvement by patients. For instance, a decrease in the QuickDASH score of 28 points from the preoperative visit to a follow-up point equates to 2 MCIDs achieved.
Descriptive statistics of the patient characteristics were calculated, reported, and compared for those who did and did not meet the average number of MCIDs achieved at each follow-up point for the overall patient cohort.
Results
We included 173 patients, average age 62 years (SD, 13 years). A notable majority were women (n = 146; 84%). Table 1 lists the demographic details of the sample. A total of 23 patients (13% of 173) had QuickDASH scores calculated at all 4 time points (before surgery and at all approximate follow-up points: 0 to 2 months, 3 to 6 months, and a minimum of 9 to 12 months), whereas the remainder had a preoperative score and at least one follow-up score. Mean QuickDASH score at the preoperative visit was 74 (SD, 19; range, 0–100). This improved to 50 (SD, 24; range, 0–100) by 0 to 2 months, 22 (SD, 22, range, 0–98) by 3 to 6 months, and 9.8 (SD, 15, range, 0–75) by 9 to 12 months (Table 2).
Table 1.
Patient Characteristics (n = 173)
| Characteristic | n (%) or Mean (SD) |
|---|---|
| Age, y (n = 169) | 62 (13) |
| BMI (n = 89) | 27 (5) |
| Sex | |
| Male | 27 (16) |
| Female | 146 (84) |
| Hand dominance | |
| Right | 141 (82) |
| Left | 16 (9) |
| Ambidextrous/unknown | 16 (9) |
| Insurance | |
| Medicare | 29 (17) |
| Medicaid | 5 (3) |
| Private | 44 (25) |
| Workers’ compensation | 35 (20) |
| Unknown | 60 (35) |
| Injury side | |
| Right | 81 (47) |
| Left | 92 (53) |
| Injury mechanism | |
| Fall from standing height | 75 (43) |
| Fall from height | 11 (6) |
| Motor vehicle accident | 1 (1) |
| Other | 26 (15) |
| Unknown | 60 (35) |
Table 2.
Average QuickDASH Scores at Each Follow-Up Point
| Postoperative Point | QuickDASH Score (mean [SD] [range]) |
|---|---|
| Before surgery (n = 173) | 74 (19) (0–100) |
| 0–2 mo (n = 82) | 50 (24) (0–100) |
| 3–6 mo (n = 129) | 22 (22) (0–98) |
| ≥6–12 mo (n = 80) | 9.8 (15) (0–75) |
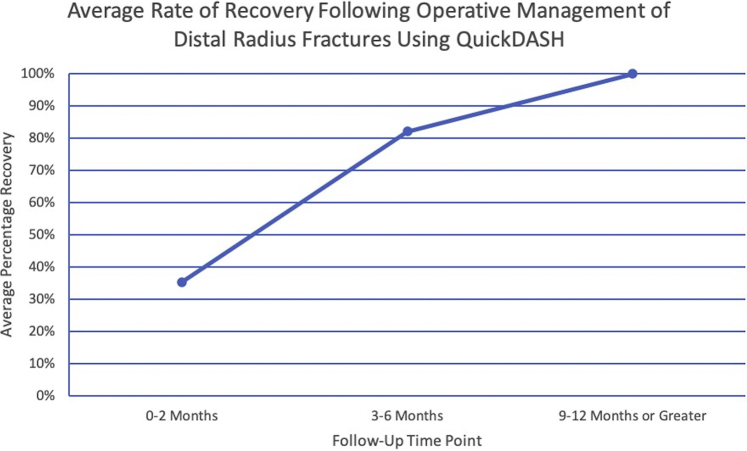
The proportion of patients achieving a change in QuickDASH score at or above the MCID at approximately 0 to 2 months, 3 to 6 months, and a minimum of 9 to 12 months of follow-up was 62%, 88%, and 96%, respectively (Table 3). On average, the number of MCIDs achieved (ie, the number of 14-point decreases in QuickDASH score) at approximately 0 to 2 months, 3 to 6 months, and a minimum of 9 to 12 months of follow-up was 1.57, 3.64, and 4.43, respectively (Table 4). Assuming that 4.43 MCIDs equates to the average maximum improvement by the time of final follow-up (ie, 100%), patients recovered, on average, 35% and 82% of maximum improvement by 0 to 2 and 3 to 6 months after surgery, respectively (Fig. 1).
Table 3.
Proportion of Patients at Each Follow-Up Point Who Achieved MCID
| Postoperative Point | MCID Achieved, n (%) |
|---|---|
| 0–2 mo (n = 82) | 51 (62) |
| 3–6 mo (n = 129) | 113 (88) |
| ≥9–12 mo (n = 80) | 77 (96) |
Table 4.
Average Change in QuickDASH Scores at Each Point
| Postoperative Point | Change in QuickDASH Score (Average [SD] [range]) | Average MCIDs Achieved, n |
|---|---|---|
| 0–2 mo (n = 82) | 22 (28) (–69 to 87) | 1.57 |
| 3–6 mo (n = 129) | 51 (27) (–36 to 94) | 3.64 |
| ≥9–12 mo (n = 80) | 62 (23) (7 to 100) | 4.43 |
Figure 1.
Average rate of recovery after operative management of DRFs using QuickDASH. Assuming that 4.43 MCIDs equates to average maximum improvement by the time of final follow-up (ie, 100%), patients recover, on average, 35% and 82% of maximum improvement by 0 to 2 months and 3 to 6 months, respectively, after surgery.
Patients at or above the average 1.57 MCIDs at the approximate 0- to 2-month follow-up appeared to have private insurance more often than did those who did not achieve this average MCID change (48% vs 15%). All other patient characteristics appeared similar between subgroups (Table 5). Patients at or above the average 3.64 MCIDs at the 3- to 6-month follow-up had characteristics similar to those of patients who were below 3.64 MCIDs (Table 6). Patients at or above the average 4.43 MCIDs at the minimum 9- to 12-month follow-up appeared to report the injury mechanism as a fall from a standing height more often than did those who did not achieve this average MCID change (59% vs 35%). All other patient characteristics appeared similar between subgroups (Table 7).
Table 5.
Patient Characteristics of Those Above and Below Average MCID Change (0–2 Months After Surgery) (n = 82)∗
| Characteristic | >1.57 MCIDs (n = 42) | <1.57 MCIDs (n = 40) |
|---|---|---|
| Age | 58 (13) | 64 (11) |
| BMI | 28 (5) | 26 (5) |
| Sex | ||
| Male | 7 (17) | 8 (20) |
| Female | 35 (83) | 32 (80) |
| Insurance | ||
| Medicare | 3 (7) | 11 (28) |
| Medicaid | 2 (5) | 1 (2) |
| Private | 20 (48) | 6 (15) |
| Workers’ compensation | 6 (14) | 9 (2) |
| Unknown | 11 (26) | 13 (33) |
| Injury mechanism | ||
| Fall from standing height | 18 (43) | 18 (45) |
| Fall from height | 4 (9) | 3 (7) |
| Motor vehicle accident | 1 (2) | 0 |
| Other | 8 (19) | 6 (15) |
| Unknown | 11 (26) | 13 (33) |
Data represent n (%) or mean (SD).
Table 6.
Patient Characteristics of Those Above and Below Average MCID Change (3–6 Months After Surgery) (n = 129)∗
| Characteristic | >3.64 MCIDs (n = 75) | <3.64 MCIDs (n = 54) |
|---|---|---|
| Age | 61 (13) | 66 (10) |
| BMI | 27 (5) | 27 (5) |
| Sex | ||
| Male | 11 (15) | 8 (15) |
| Female | 64 (85) | 46 (85) |
| Insurance | ||
| Medicare | 12 (16) | 13 (24) |
| Medicaid | 2 (3) | 1 (2) |
| Private | 22 (29) | 10 (19) |
| Workers’ compensation | 17 (23) | 9 (17) |
| Unknown | 22 (29) | 21 (39) |
| Injury mechanism | ||
| Fall from standing height | 35 (47) | 24 (44) |
| Fall from height | 5 (7) | 3 (6) |
| Motor vehicle accident | 1 (1) | 0 |
| Other | 12 (16) | 3 (6) |
| Unknown | 22 (29) | 21 (39) |
Data represent n (%) or mean (SD).
Table 7.
Patient Characteristics of Those Above and Below Average MCID Change (≥9–12 Months After Surgery) (n = 80)∗
| Characteristic | >4.43 MCIDs (n = 48) | <4.43 MCIDs (n = 32) |
|---|---|---|
| Age | 60 (15) | 61 (12) |
| BMI | 28 (4) | 26 (4) |
| Sex | ||
| Male | 5 (10) | 5 (16) |
| Female | 43 (90) | 27 (84) |
| Insurance | ||
| Medicare | 7 (15) | 10 (31) |
| Medicaid | 1 (2) | 0 (–) |
| Private | 13 (27) | 12 (38) |
| Workers’ compensation | 11 (23) | 4 (13) |
| Unknown | 16 (33) | 6 (19) |
| Injury mechanism | ||
| Fall from standing height | 17 (35) | 19 (59) |
| Fall from height | 5 (10) | 5 (16) |
| Motor vehicle accident | 1 (2) | 0 |
| Other | 9 (19) | 2 (6) |
| Unknown | 16 (33) | 6 (19) |
Data represent n (%) or mean (SD).
Discussion
Patient-reported outcome measures such as QuickDASH allow hand surgeons to monitor patients’ functional improvement or decline after a given treatment. Overall, we found that 62%, 88%, and 96% patients achieved a change in QuickDASH score consistent with meeting or exceeding the MCID at the approximate follow-up points of 0 to 2 months, 3 to 6 months, and a minimum of 9 to 12 months after surgery, respectively. Furthermore, patients improved, on average 1.57, 3.64, and 4.43 MCIDs (ie, the number of 14-point decreases in the QuickDASH score) at each of these respective time points. Ultimately, we found that patients recovered, on average, 35% and 82% of maximum by 0 to 2 months and 3 to 6 months after surgery, respectively, which suggested that the trajectory of recovery may be nonlinear. A more robust understanding of the time line and trajectory of patient functional gains after surgical fixation of DRF, as established in this study, can help surgeons set patient expectations better and identify patients who are not progressing as anticipated.
To date, a number of studies have examined functional improvement after operative management of DRFs. In one study, Phadnis and colleagues3 published a retrospective review of 183 patients with DRFs who were observed for a mean of 30 months after internal fixation. The authors found the median DASH score for all patients to be 2.3 and the median Mayo Wrist Score to be 90. They considered 74% of these patients to have achieved excellent outcomes. In addition, Rozental and Blazar2 evaluated 41 patients with dorsally displaced DRFs treated with volar plate fixation. Patients were observed for an average of 17 months; mean DASH score at final follow-up was 14. However, patients were not evaluated for changes in DASH scores to note the rate of improvement. Saving et al6 also performed a randomized control trial of elderly patients with DRFs and evaluated functional outcomes in both the volar plating group and nonsurgical group. At 3 months, the operative group had a median DASH score of 14.4 compared with the nonsurgical group’s median DASH score of 29.2. At 12 months, the operative group’s median DASH score improved to 8.3. Other prospective studies found similar results.1,5 However, none of these studies obtained preoperative PROMs; thus, prior research was unable to determine when patient PROM score changes met MCID.
Monitoring postoperative recovery over time is also vital to understanding the full clinical picture. In an effort to compare early ROM protocols with standard of care postoperative use of an orthosis, Quadlbauer and colleagues4 documented QuickDASH scores at routine postoperative follow-up visits. In the early ROM group (n = 15), QuickDASH scores were 31, 11, 4.8, and 5.9 at 6 weeks, 3 months, 6 months, and 1 year, respectively. Our investigation found a similar trajectory of improvement, although with slightly higher final mean QuickDASH scores (ie, 9.8). Overall, in our study, mean change in QuickDASH score from before surgery to final follow-up (ie, minimum of 9 to 12 months after surgery) was 62 points, representing 4.43 MCIDs.
In our investigation, we also sought to understand better the patient factors that are characteristic of achieving (or not) expected functional recovery for patients after fixation for a DRF. Roh and colleagues19 evaluated a cohort of 122 patients with DRFs treated with volar plating and noted that high-energy mechanisms were associated with an initial delay in functional recovery. However, the mechanism of injury did not seem to have an impact on the current patient sample in the early postoperative recovery period. In addition, Roh et al found that age was another factor associated with low Michigan Hand Questionnaire scores at 12 months after surgery. Our descriptive analysis did not appear to show that age affected clinical outcomes in the current patient sample. Another patient factor previously evaluated in the literature is obesity. Interestingly, Hall and colleagues17 noted that although obese patients may have slightly higher QuickDASH scores, the difference between patient groups was not enough to meet MCID. Similarly, we found that BMI did not appear to be a recovery factor.
Type of insurance has also been reported to influence functional recovery. The association between workers’ compensation and poor outcomes with slower recovery after orthopedic surgery, including hand surgery, has been well-studied.15,16,21 In a group of patients with humeral shaft fractures, with a mix of surgical and nonsurgical treatment, those with private insurance were more likely to achieve higher Short Form–12 scores at final follow-up.22 In our study, patients with private insurance appeared to achieve greater clinical improvement at initial follow-up at a rate greater than those without private insurance. The reason for this is not entirely clear, but it may be a surrogate for socioeconomic status or improved access to initial postoperative care. Importantly, however, this difference was no longer present at final follow-up, which suggests that most patients do well after operative treatment of DRF independent of insurance type or socioeconomic status. Nonetheless, further research is warranted on this topic.
To our knowledge, the current study is the first to examine when patients undergoing surgical fixation for DRFs achieve clinically relevant improvement in functional symptoms using the change in QuickDASH scores and the concept of MCID at routine follow-up points. At a minimum of 9 to 12 months after surgery, nearly all patients (96%) recognized a clinically appreciable positive improvement in symptoms from surgery. Furthermore, our evaluation of patient factors suggested that appreciable clinical improvement was independent of age, sex, or BMI.
An important consideration in reviewing our findings is that a single MCID represents only a minimum level of clinically relevant change. Alternatively, identifying optimal (rather than minimal) improvement or multiples of this minimum improvement has been introduced by several authors in the spine, arthroplasty, and hip preservation literature. This idea is termed the substantial clinical benefit (SCB).23, 24, 25 Generally, these studies used an anchor-based approach coupled with receiver operating characteristic curves to pinpoint a threshold for SCB after surgery. The substantial clinical benefit has yet to be defined in the hand surgery literature for DRFs. However, one could easily see the benefit of understanding SCB when providing guidance to a patient upon postoperative recovery. Our investigation introduces a step toward this end by characterizing the achievement of multiple MCIDs and providing an average trajectory of improvement over the course of recovery after DRF fixation. Using the achievement of only one MCID to represent clinical success with respect to a given PROM (eg, DASH or QuickDASH) likely underestimates true patient improvement after surgical fixation of DRFs and provides little insight into the time line of reaching optimal postoperative clinical improvement. Our hope is that the findings of this study will help guide potential discussions with patients regarding the expected amount of symptom improvement and the time line of such improvement after DRF fixation.
There are several limitations to our study. First, we chose to perform the analysis using one commonly used hand and upper-extremity PROM (ie, QuickDASH) and based on one accepted MCID value in the literature. Similar studies using other frequently used PROMs (eg, Patient-Reported Outcomes Measurement Information System or Patient-Related Wrist Evaluation) are warranted. In addition, the MCID cutoff used in this study has not been widely replicated or validated beyond a few studies, and this estimate was not derived from a cohort of surgical patients. The most appropriate way to determine MCID continues to be debated; the 2 most common approaches are the distribution-based and anchor-based methods. Thus, it is possible that a different methodology might have yielded a different MCID, which might have changed the results (but not the methodology) of our study. Furthermore, whereas MCID estimates may indeed vary between individuals, it remains the best tool established to date for clinicians to quantify clinically meaningful symptom change in a patient’s recovery. Second, our study was limited by small numbers and high rates of clinical success; thus, we were not well-powered to perform bivariate and regression analyses. Therefore, we are able to report descriptive differences between patient subgroups but cannot comment on whether they are significantly different from a statistical perspective. This makes it difficult to make definitive conclusions about patient or injury characteristics, although the descriptive trends still appear to be present. In addition, there were too few patients with poor outcomes to determine which characteristics are associated with not reaching MCID at different postoperative follow-up points. Nonetheless, we believe that our study lays the framework for future work in this area. Third, preoperative QuickDASH scores may be variable depending on individual injury tolerance, expectations for management, and overall resiliency. This may lead to 2 patients with similar fractures having widely variable preoperative QuickDASH scores. However, by using preoperative QuickDASH scores and evaluating the change in score at each follow-up, we were still able to estimate the trajectory of recovery using this PROM. Specifically, evaluating clinical progress in terms of MCID may help neutralize these patient factors and provide clinicians and patients with an understanding of average symptom improvement. Future investigation with a larger patient sample that allows for more advanced statistical analyses with appropriate power may help characterize these findings further. Also, although there is a standard postoperative immobilization protocol among surgeons at our institution, this was a retrospective study without the ability to control this definitively. However, deviations from the discussed protocol are unusual. In addition, as with many studies, we were limited by the use of an institutional database. Specifically, we were hindered by missing data, especially among a number of sociodemographic factors. Furthermore, our database does not specifically track complications or operative time, a potential surrogate for case complexity. It also does not include radiographic fracture parameters. Collecting this additional information would provide greater granularity to our analyses, but we believe these additional data points are unlikely to have changed our core findings, because the study included a broad range of patients, fracture types, and fracture morphologies. Nonetheless, future work is warranted to evaluate and compare recovery trajectories across a wide range of patient subgroups. Finally, our study was limited from bias resulting from inconsistent patient follow-up, because not all patients had a follow-up visit in every analyzed time interval. However, in this case, our findings may actually underestimate the true improvement rate and trajectory, because one might suspect that patients who are doing well would be less likely to return for follow-up visits. This is important for readers to consider when using our findings in shared clinical decision-making discussions before surgery.
The data reported here describe the rate of clinically relevant improvement in patient functional outcomes after surgical treatment of DRFs. Overall, we found that on average, patients will achieve over 35% and over 82% of clinically appreciable improvement by approximately 0 to 2 months and 3 to 6 months after surgery, respectively, and that this seems to be consistent across age, sex, and BMI. Further prospective investigation is warranted to characterize the nature of this improvement better for different patient populations to counsel all patients appropriately on their expected recovery after surgery.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received by the authors related directly or indirectly to the subject of this article.
References
- 1.Jupiter J.B., Marent-Huber M. Operative management of distal radial fractures with 2.4-millimeter locking plates a multicenter prospective case series. J Bone Jointt Surg Am. 2009;91(1):55–65. doi: 10.2106/JBJS.G.01498. [DOI] [PubMed] [Google Scholar]
- 2.Rozental T.D., Blazar P.E. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006;31(3):359–365. doi: 10.1016/j.jhsa.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Phadnis J., Trompeter A., Gallagher K., Bradshaw L., Elliott D.S., Newman K.J. Mid-term functional outcome after the internal fixation of distal radius fractures. J Orthop Surg Res. 2012;7(1):4. doi: 10.1186/1749-799X-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quadlbauer S., Pezzei C., Jurkowitsch J., et al. Early rehabilitation of distal radius fractures stabilized by volar locking plate: a prospective randomized pilot study. J Wrist Surg. 2016;06(2):102–112. doi: 10.1055/s-0036-1587317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez-Mendez D., Lizaur-Utrilla A., de-Juan-Herrero J. Intra-articular distal radius fractures in elderly patients: a randomized prospective study of casting versus volar plating. J Hand Surg Eur Vol. 2018;43(2):142–147. doi: 10.1177/1753193417727139. [DOI] [PubMed] [Google Scholar]
- 6.Saving J., Wahlgren S., Olsson K., et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly. J Bone Joint Surg Am. 2019;101(11):961–969. doi: 10.2106/JBJS.18.00768. [DOI] [PubMed] [Google Scholar]
- 7.Tsang P., Walton D., Grewal R., MacDermid J. Validation of the QuickDASH and DASH in patients with distal radius fractures through agreement analysis. Arch Phys Med Rehabil. 2017;98(6) doi: 10.1016/j.apmr.2016.11.023. 1217.e1–1222.e1. [DOI] [PubMed] [Google Scholar]
- 8.Beaton D.E., Wright J.G., Katz J.N., et al. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 9.MacDermid J.C., Turgeon T., Richards R.S., Beadle M., Roth J.H. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Lozano-Calderón S.A., Souer S., Mudgal C., Jupiter J.B., Ring D. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008;90(6):1297–1304. doi: 10.2106/JBJS.G.01368. [DOI] [PubMed] [Google Scholar]
- 11.Souer J.S., Buijze G., Ring D. A prospective randomized controlled trial comparing occupational therapy with independent exercises after volar plate fixation of a fracture of the distal part of the radius. J Bone Joint Surg Am. 2011;93(19):1761–1766. doi: 10.2106/JBJS.J.01452. [DOI] [PubMed] [Google Scholar]
- 12.Franchignoni F., Vercelli S., Giordano A., Sartorio F., Bravini E., Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (quickDASH) J Orthop Sports Phys Ther. 2014;44(1):30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 13.Sorensen A.A., Howard D., Tan W.H., Ketchersid J., Calfee R.P. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38(4):641–649. doi: 10.1016/j.jhsa.2012.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernstein D.N., Nwachukwu B.U., Bozic K.J. Value-based health care: moving beyond “minimum clinically important difference” to a tiered system of evaluating successful clinical outcomes. Clin Orthop Relat Res. 2019;477(5):945–947. doi: 10.1097/CORR.0000000000000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Day C.S., Alexander M., Lal S., et al. Effects of workers’ compensation on the diagnosis and surgical treatment of patients with hand and wrist disorders. J Bone Joint Surg Am. 2010;92(13):2294–2299. doi: 10.2106/JBJS.I.00158. [DOI] [PubMed] [Google Scholar]
- 16.MacDermid J.C., Roth J.H., McMurtry R. Predictors of time lost from work following a distal radius fracture. J Occup Rehabil. 2007;17(1):47–62. doi: 10.1007/s10926-007-9069-0. [DOI] [PubMed] [Google Scholar]
- 17.Hall M.J., Ostergaard P.J., Dowlatshahi A.S., Harper C.M., Earp B.E., Rozental T.D. The impact of obesity and smoking on outcomes after volar plate fixation of distal radius fractures. J Hand Surg Am. 2019;44(12):1037–1049. doi: 10.1016/j.jhsa.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 18.Souer J.S., Lozano-Calderon S.A., Ring D. Predictors of wrist function and health status after operative treatment of fractures of the distal radius. J Hand Surg Am. 2008;33(2):157.e1–157.e8. doi: 10.1016/j.jhsa.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Roh Y.H., Lee B.K., Noh J.H., Oh J.H., Gong H.S., Baek G.H. Factors delaying recovery after volar plate fixation of distal radius fractures. J Hand Surg Am. 2014;39(8):1465–1470. doi: 10.1016/j.jhsa.2014.04.033. [DOI] [PubMed] [Google Scholar]
- 20.Hudak P.L., Amadio P.C., Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and hand) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 21.Fujihara Y., Shauver M.J., Lark M.E., Zhong L., Chung K.C. The effect of workers’ compensation on outcome measurement methods after upper extremity surgery: a systematic review and meta-analysis. Plast Reconstr Surg. 2017;139(4):923–933. doi: 10.1097/PRS.0000000000003154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shields E., Sundem L., Childs S., et al. Factors predicting patient-reported functional outcome scores after humeral shaft fractures. Injury. 2015;46(4):693–698. doi: 10.1016/j.injury.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 23.Glassman S.D., Copay A.G., Berven S.H., Polly D.W., Subach B.R., Carreon L.Y. Defining substantial clinical benefit following lumbar spine arthrodesis. J Bone Joint Surg Am. 2008;90(9):1839–1847. doi: 10.2106/JBJS.G.01095. [DOI] [PubMed] [Google Scholar]
- 24.Lyman S., Lee Y.Y., McLawhorn A.S., Islam W., MacLean C.H. What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? Clin Orthop Relat Res. 2018;476(12):2432–2441. doi: 10.1097/CORR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nwachukwu B.U., Chang B., Fields K., et al. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(6):1297–1303. doi: 10.1177/0363546516687541. [DOI] [PubMed] [Google Scholar]