Abstract
Distal radius fractures are among the most common injuries to the upper extremity and have a bimodal distribution in younger male patients and older women. Young men suffer from high-energy injuries and older women from fragility fractures. Approximately 50% of these are intra-articular. Timely and appropriate treatment usually will lead to an acceptable outcome, but loss of congruity of the articular surface remains a difficult problem to manage. We report here on the case of a 16-year-old boy with malunion of the radial articular surface with lack of motion and pain. He was managed by replacing the displaced and damaged segment of the radial articular surface with a vascularized osteochondral graft from the proximal phalanx of the great toe. This matched the shape of this portion of the radius quite well, and he has had improvements in motion and pain in the 10 months since that time. The donor site has not caused him any difficulty to date.
Key words: Die-punch fracture, Distal radius, Reconstruction, Toe transfer, Vascularized cartilage graft
Distal radius fractures are among the most common injuries to the upper extremity.1 They have a bimodal distribution, occurring more frequently in younger men due to high-energy trauma and in older women due to bone fragility. It is estimated that 50% of the distal radius fractures are intra-articular,1 and young adults with these fractures have a high incidence of joint degeneration. Knirk and Jupiter2 noted that the majority of patients developing arthritis had malreduced die-punch fractures. Accurate reduction and fixation of the articular surface has been shown to significantly improve the outcomes in these injuries.3 However, once a malunion of a die-punch fracture has been established management is extremely challenging.4 Options for replacement of damaged joint surfaces have been limited, and results using cartilage grafts have been mixed.5 Here we present here the case of a patient with a delayed presentation and malunion of a distal radius die-punch fracture managed with a vascularized osteochondral graft from the proximal articular surface of the great toe.
Case Report
The patient presented at age 16, approximately 10 months after open reduction and pin fixation of a distal radius fracture caused by falling off a horse. At the time of the initial injury, an attempt at volar plate fixation at an outside facility was aborted because of the severe comminution, and the fracture was simply fixed with Kirschner wires. Figure 1 shows the anteroposterior and lateral views at the time of the initial procedure. The patient was immobilized for approximately 8 weeks, and the wires were removed. He was referred to physical therapy but continued to have ongoing problems, with increasing pain and lack of motion. At 10 months postinjury he was referred to our institution.
Figure 1.
A AP view of the patient’s wrist after open reduction and fixation with Kirschner wires. B Lateral view of the patient’s wrist after open reduction and fixation with Kirschner wires. AP, anteroposterior.
At the time of presentation, he complained of pain and swelling in the right wrist. He had limited active and passive motion, with 20° of flexion and 15° of dorsiflexion, and had pain with any motion in the wrist. His pronation was 60° and supination 75°. Plain radiographs taken at that time showed degenerative changes in the radiocarpal joint, with loss of volar tilt (Fig. 2). Radial inclination on these images was 13°, volar tilt was -12°, and ulnar variance was +3 mm. Further imaging was done with computerized tomographic scans to evaluate the malunion and magnetic resonance imaging (MRI) to evaluate the state of his cartilage (Figs. 3, 4). These images confirmed a large defect in the articular surface of the distal radius, involving part of the lunate and scaphoid fossae, while the cartilage on the carpal bones appeared to be intact. Due to the patient’s age, consideration was given to the possibility of a vascularized osteochondral graft, but on further research, none of the described donor sites appeared to offer the right size6 or concavity7 to reconstruct the involved segment. Comparing x-rays of his great toe and the defect in the distal radius showed that the articular surface of the proximal phalanx at the metatarsophalangeal joint potentially offered such a graft. This option was discussed at length with the patient and his mother, who agreed to undertake an attempt at reconstruction of his wrist with a vascularized graft from the great toe.
Figure 2.
A AP view of the patient’s wrist 10 months postoperatively. B Lateral view of the patient’s wrist 10 months postoperatively. AP, anteroposterior.
Figure 3.
A Representative view of the right wrist on CT scan. B Representative view of the right wrist on CT scan. CT, computerized tomography.
Figure 4.
View of articular surface of radius at exploration. The black line outlines the proximal carpal bones.
The radius was approached both dorsally and volarly. There was dense scarring of the joint capsule both dorsally and volarly, which was released dorsally and somewhat volarly, preserving the radioscaphocapitate ligament. At exploration of the wrist, he was found to have severe damage to the involved segment of cartilage; however, the cartilage on the carpal bones was preserved (Fig. 4). The volar tilt of the radius was first restored with a transverse dorsal opening wedge osteotomy and volar plate. The defect in the articular surface was excised from the dorsal side, and the proximal half of the proximal phalanx of the great toe was harvested on the dorsal circulation and proper digital branches to the proximal phalanx (Fig. 5).8, 9, 10 The cortical portions of the graft were carefully removed, and the phalanx was squared off to fit the defect (Fig. 6). After assuring appropriate positioning of the graft, it was fixed with screws from the volar plate (Fig. 7). Vascular anastomosis of the dorsalis pedis artery and 2 venae comitans was performed end-to-side to the radial vessels on the volar side of the wrist. The defect at the toe was managed by interpositional arthroplasty using the extensor digitorum brevis and a portion of the extensor hallucis longus placed in the defect, and was pinned for 8 weeks.
Figure 5.
Articular surface of the proximal great toe after harvesting, with the vascular pedicle to the left.
Figure 6.
Graft after removal of cortex and shaping.
Figure 7.
A PA view immediately postoperatively. B Lateral view immediately postoperatively.
His wrist was immobilized for 6 weeks and appeared to have good early healing at this point. After this, he was started on occupational therapy.
He had excellent radiographic healing of the graft, and the last plain films showed some improvement in the joint surface. Radial inclination in these images was unchanged at 13°; however, volar tilt was improved to 11° and ulnar variance remained at approximately +3 mm. He discontinued therapy himself at around 3 months. His pain resolved and he returned to playing baseball. His motion gradually improved, but he continued to have a marked lack of extension while his flexion improved. His pronation and supination returned to nearly normal. At his last follow-up at 10 months, the graft was well incorporated (Fig. 8). His wrist extension was 20° and flexion was 45° (Fig. 9). He denied pain in the wrist. The foot was not bothersome and he was able to run and play sports. We have been unable to contact him since that time for further imaging to evaluate the status of the cartilage.
Figure 8.
A PA view at 10 months. B Lateral view at 10 months.
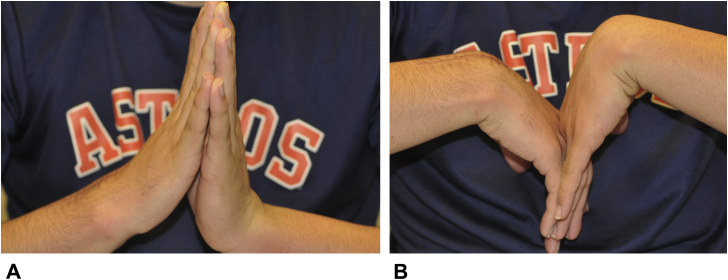
Figure 9.
A Dorsiflexion at 10 months. B Flexion at 10 months.
Discussion
Repair and reconstruction of significant cartilage defects remains a difficult challenge. Younger patients pose particular issues, as salvage procedures and joint replacement are not good options. There are small series that have reported using nonvascularized osseocartilaginous grafts from the rib to replace the cartilage of the distal radius; while early results were encouraging,5,11 this technique has not gained favor. The medial femoral condylar vascularized graft can be harvested with the cartilage of the trochlea of the femur to reconstruct the scaphoid,7 and the results of this procedure have been reasonable.11 The shape of this particular graft is convex, however, and not really applicable to the articular surface of the radius. Del Pinal et al12 have described the anatomy of the base of the third metatarsal as a vascularized osseocartilaginous graft, and reconstructed a portion of the scaphoid fossa with this. Del Pinal et al6 likewise used this graft to reconstruct the sigmoid notch of the radius. This did not appear to offer enough cartilage to adequately reconstruct the defect in this patient.
The vascular supply to and anatomy of the great toe have been widely studied and are consistent.9,13 Transfer of the joints and/or portions of the toe have been used in hand and digital reconstruction for many years.8 Based on this knowledge, we designed a vascularized osteochondral graft from the proximal phalanx of the great toe to reconstruct a relatively large defect in the distal radius articular surface. The dissection of the bone flap is straightforward, and the cartilage obtained fit the concavity of the radial articular surface well.8
The patient did well in the short term, with decreased pain and improved motion. Unfortunately, dorsiflexion did not improve a great deal; we feel this was due to the intense scarring present from the initial injury, along with the inability to completely release the volar side of the wrist. Our follow-up was unfortunately short, and we have not had the opportunity to evaluate the status of the cartilage via MRI. The donor site could well pose more problems as time goes on. We feel that this procedure presents another option for the management of significant cartilage loss in the distal radius, particularly in younger patients. Fortunately, this is an unusual problem, but we will certainly perform this procedure again if a similar problem arises in the future.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
References
- 1.Nellans K.W., Kowalski E., Chung K.C. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knirk J.L., Jupiter J.B. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68(5):647–659. [PubMed] [Google Scholar]
- 3.Trumble T.E., Culp R.W., Hanel D.P., Geissler W.B., Berger R.A. Intra-articular fractures of the distal aspect of the radius. Instr Course Lect. 1999;48:465–480. [PubMed] [Google Scholar]
- 4.Prommersberger K.J., Ring D., González del Pino J., Capomassi M., Slullitel M., Jupiter J.B. Corrective osteotomy for intra-articular malunion of the distal part of the radius. Surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1 Pt 2):202–211. doi: 10.2106/JBJS.F.00145. [DOI] [PubMed] [Google Scholar]
- 5.Obert L., Loisel F., Kielwasser H., Rochet S., Lepage D. The chondrocostal graft to treat articular distal radius malunion. Hand Surg Rehabil. 2016;35S:S112–S114. doi: 10.1016/j.hansur.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 6.del Piñal F., Klausmeyer M., Moraleda E., et al. Vascularized graft from the metatarsal base for reconstructing major osteochondral distal radius defects. J Hand Surg Am. 2013;38(10):1883–1895. doi: 10.1016/j.jhsa.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 7.Bürger H.K., Windhofer C., Gaggl A.J., Higgins J.P. Vascularized medial femoral trochlea osteochondral flap reconstruction of advanced Kienbock disease. J Hand Surg Am. 2014;39(7):1313–1322. doi: 10.1016/j.jhsa.2014.03.040. [DOI] [PubMed] [Google Scholar]
- 8.del Piñal F., García-Bernal F.J., Delgado J., Sanmartín M., Regalado J., Cagigal L. Vascularized bone blocks from the toe phalanx to solve complex intercalated defects in the fingers. J Hand Surg Am. 2006;31(7):1075–1082. doi: 10.1016/j.jhsa.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 9.Chen S.H., Wei F.C., Chen H.C. Vascularized toe joint transplantation. Hand Clin. 1999;15(4):613–627. [PubMed] [Google Scholar]
- 10.del Piñal F., García-Bernal F.J., Delgado J., Sanmartín M., Regalado J. Results of osteotomy, open reduction, and internal fixation for late-presenting malunited intra-articular fractures of the base of the middle phalanx. J Hand Surg Am. 2005;30(5):1039.e1–1039.e14. doi: 10.1016/j.jhsa.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Pet M.A., Higgins J.P. Long-term outcomes of vascularized trochlear flaps for scaphoid proximal pole reconstruction. Hand Clin. 2019;35(3):345–352. doi: 10.1016/j.hcl.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 12.del Piñal F., García-Bernal F.J., Delgado J., Sanmartín M., Regalado J. Reconstruction of the distal radius facet by a free vascularized osteochondral autograft: anatomic study and report of a patient. J Hand Surg Am. 2005;30(6):1200–1210. doi: 10.1016/j.jhsa.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Foucher G., Sammut D., Citron N. Free vascularized toe-joint transfer in hand reconstruction: a series of 25 patients. J Reconstr Microsurg. 1990;6(3):201–207. doi: 10.1055/s-2007-1006819. [DOI] [PubMed] [Google Scholar]