Abstract
Purpose
To define self-reported WALANT use among American Society for Surgery of the Hand (ASSH) members. We aimed to define surgeon and practice demographics relative to WALANT use and identify potential barriers for WALANT implementation.
Methods
An anonymous multiple-choice survey was electronically distributed to all active ASSH members. Incomplete surveys were included in the final analysis. Surgeons were asked to provide reasons for not performing WALANT, which were categorized based on general themes. We compared practice and surgeon demographic information relative to WALANT use.
Results
Of 3,826 ASSH members, 869 responded (23%). A total of 79% of respondents had performed at least one WALANT procedure; 62% currently incorporated WALANT into their practice. Hospital-owned outpatient surgery centers were the most common location for WALANT procedures (31%). Canadian surgeons were more likely to use WALANT, compared with US and international surgeons. Surgeons with fewer years in practice and higher-volume surgeons were more likely to use WALANT. There was no statistically significant association between either practice or income structure and WALANT use. For carpal tunnel release (CTR), 13% did not offer patients WALANT, whereas 43% offered WALANT to all patients. Moreover, 51% of surgeons reported that anesthesia staff was required to be present for WALANT cases at their institution. In determining reasons for not using WALANT, 16% reported that they preferred a tourniquet for visualization. Only 2% had concerns regarding epinephrine use in the hand.
Conclusions
The results of this survey illustrate current WALANT use among ASSH members and defines the demographics of those employing WALANT. Lack of familiarity with WALANT and an acceptance of the use of epinephrine in the hand has increased from prior ASSH surveys. Lack of familiarity with the technique, concerns regarding operating room efficiency, and patient preferences remain considerable barriers to more widespread adoption of WALANT procedures.
Type of study/level of evidence
Economic and Decision Analysis V.
Key words: American Society for Surgery of the Hand, Hand surgery, Survey, WALANT, Wide-awake surgery
As an alternative to general anesthesia or sedation in the operating room, many hand and wrist procedures can be performed with wide-awake local anesthesia no tourniquet (WALANT) techniques.1, 2, 3, 4 Potential benefits of this technique include decreasing complications associated with intravenous sedation and general anesthesia as well as decreased costs.5,6 Although the literature on safety, efficacy, and potential cost-savings has increased, there is little information on how frequently WALANT procedures are being performed.
The purpose of this investigation was to define current self-reported WALANT use among active members of the American Society for Surgery of the Hand (ASSH). We aimed to define surgeon and practice demographics relative to WALANT use and identify potential concerns and barriers for the implementation of WALANT procedures. We hypothesized that WALANT use would be common among ASSH members, particularly for those who had recently completed fellowship.
Materials and Methods
We received institutional review board approval; we also obtained permission from the ASSH and received an e-mail list of all active ASSH members. An anonymous survey was electronically distributed to all full, active ASSH members (both US and international) with a valid e-mail address. The survey contained 24 questions. In accordance with ASSH protocols, the introductory e-mail contained a brief overview of the study and link to complete the survey on-line. A second follow-up e-mail was sent 1 week later containing the same information.
Results were uploaded to an on-line spreadsheet. Incomplete surveys (n = 434), which contained some blank fields, were included in the final analysis. In addition to multiple-choice questions, surgeons were asked to provide reasons for not performing WALANT. These free-text responses were analyzed and categorized based on general themes.
Descriptive statistics were used to define baseline demographics and characteristics for participating surgeons. For survey questions regarding case volume and years in practice, Kruskal-Wallis nonparametric rank test was employed to compare the groups’ WALANT use. For cases in which non-ranked answer choice categories were used, chi-square test was chosen to compare the distributions of answers between groups.
Results
Of the 3,826 surveys distributed to active ASSH members, 869 responded (23%). Table 1 includes baseline demographics of all surgeons who responded to the survey. Eighty percent of respondents were from the United States. Table 2 includes additional information about WALANT use and experience with the technique. A total of 79% of respondents had performed at least one WALANT procedure; 62% currently incorporated WALANT into their practice. Hospital-owned outpatient surgery centers were the most common location for WALANT procedures (31%).
Table 1.
Baseline Demographics and Frequency of WALANT Procedures Among Active ASSH Members Responding to Survey
| Baseline Demographics | n (%) |
|---|---|
| Practice location, n (%) | |
| United States | 692 (80) |
| Canada | 27 (3) |
| International | 146 (17) |
| Did not answer | 4 (<1) |
| Practice type, n (%) | |
| Academic | 137 (16) |
| Private practice with academic appointment | 152 (17) |
| Hospital employed–academic | 97 (11) |
| Hospital employed–nonacademic | 77 (9) |
| Private–group | 303 (35) |
| Private–solo | 60 (7) |
| Government | 26 (3) |
| Other | 13 (2) |
| Years in practice, n (%) | |
| ≤5 | 182 (21) |
| 5–10 | 106 (12) |
| 11–20 | 208 (24) |
| >20 | 369 (43) |
| Income structure, n (%) | |
| Salary without performance incentive | 142 (16) |
| Salary with performance incentive | 221 (25) |
| Relative value unit based | 157 (18) |
| Percentage of billing | 44 (5) |
| Percentage of collection | 214 (25) |
| Other | 90 (10) |
| Did not answer | 1 (<1) |
| Cases/y, n (%) | |
| <200 | 119 (13) |
| 200–500 | 372 (43) |
| >500 | 375 (43) |
| Did not answer | 3 (<1) |
| Completion of hand surgery fellowship, n (%) | 842 (97) |
| Population in practice location, n (%) | |
| Urban | 437 (50) |
| Suburban | 369 (42) |
| Rural | 62 (7) |
| Did not answer | 1 (<1) |
Table 2.
WALANT Characteristics for Surgeons
| Surgeon Characteristics | n (%) |
|---|---|
| Was WALANT part of residency/fellowship training? (n [%]) | |
| Yes | 151 (17) |
| No | 684 (79) |
| Did not answer | 34 (4) |
| Ever performed WALANT, n (%) | |
| Yes | 689 (79) |
| No | 173 (20) |
| Did not answer | 7 (1) |
| Currently performing WALANT (of the 689 who ever did), n (%) | |
| Yes | 538 (62) |
| No | 88 (10) |
| Did not answer | 63 (7) |
| Years performing WALANT (of those 538 currently performing it), n (%) | |
| ≤2 | 144 (27) |
| 3–5 | 195 (36) |
| >5 | 198 (37) |
| Did not answer | 1 (<1) |
| Where is WALANT being performed, n (%) (multiple answers allowed/surgeon) | |
| Outpatient clinic–procedure room | 211 (24) |
| Outpatient surgery center–physician owned | 221 (25) |
| Outpatient surgery center–hospital affiliated | 270 (31) |
| Inpatient hospital | 141 (16) |
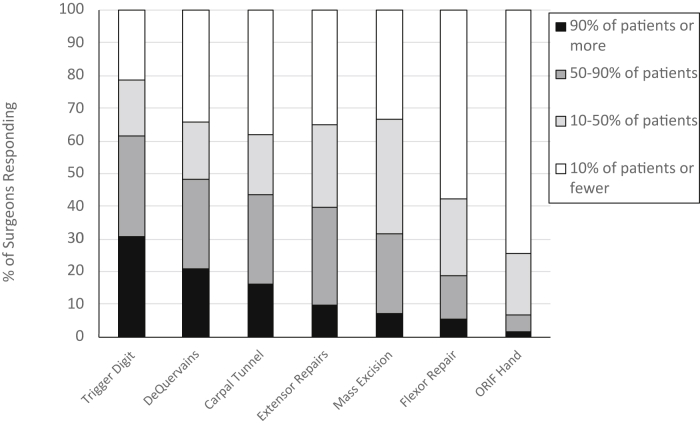
Table 3 outlines the percentage of cases performed using WALANT, categorized by decile. Trigger digit release (TDR) was the most frequently performed procedure; over half of responding surgeons reported that they used WALANT for TDR 90% of the time (Fig. 1).
Table 3.
Surgeons Who Responded That Various Percentages of Procedures Were Performed Using WALANT, by Procedure Type
| Procedure | Respondents, n (%) | Median Response (%) |
|---|---|---|
| Trigger digit release | 535 (62) | 90 |
| Carpal tunnel release | 533 (61) | 50 |
| de Quervain release | 534 (62) | 50 |
| Extensor tendon repair | 531 (61) | 50 |
| Mass excision | 525 (60) | 40 |
| Flexor tenolysis | 520 (60) | 20 |
| Flexor tendon repair | 530 (61) | 10 |
| Trapeziometacarpal arthroplasty | 529 (61) | 0 |
| Distal radius fracture fixation | 526 (61) | 0 |
| Hand fracture fixation | 529 (61) | 0 |
| Dupuytren, single digit | 527 (61) | 0 |
| Dupuytren, two to three digits | 527 (61) | 0 |
| Flexor tendon reconstruction | 523 (60) | 0 |
Figure 1.
Bar graph for each procedure type illustrating what percentage of surgeons reported that the percentage of that procedure is done with WALANT. ORIF, open reduction internal fixation.
Table 4 categorizes respondents into 3 groups: current WALANT users, former WALANT users, and those who had never used WALANT. Canadian surgeons were more likely to be WALANT users compared with those in the United States and international surgeons (P = .003). In addition, surgeons with fewer years in practice were more likely to be current WALANT users compared with those who had been in practice greater than 20 years (P ≤ .001). Higher-volume surgeons were more likely to use WALANT (P = .007), as were surgeons who had used WALANT during residency or fellowship training (P ≤ .001). There was no statistically significant association between either practice or income structure and current WALANT use.
Table 4.
Comparison of Baseline Characteristics of Surgeons Who Reported They Were Currently Using, Formerly Used, or Never Used WALANT
| Surgeon Characteristic | WALANT Use |
P Value | ||
|---|---|---|---|---|
| Currently (n = 538) | Formerly Used (n = 88) | Never Used (n = 173) | ||
| Practice location, n (%) | .003 | |||
| United States | 442 (69) | 70 (11) | 129 (20) | |
| Canada | 20 (87) | 2 (9) | 1 (4) | |
| International | 73 (55) | 16 (12) | 43 (33) | |
| Practice type, n (%) | .11 | |||
| Academic | 92 (71) | 17 (13) | 20 (16) | |
| Private practice with academic appointment | 90 (68) | 15 (11) | 28 (21) | |
| Hospital employed–academic | 56 (60) | 12 (13) | 25 (27) | |
| Hospital employed–nonacademic | 52 (75) | 2 (3) | 15 (22) | |
| Private–group | 196 (68) | 32 (11) | 59 (21) | |
| Private–solo | 26 (52) | 5 (10) | 19 (38) | |
| Government | 19 (76) | 3 (12) | 3 (12) | |
| Other | 7 (54) | 2 (15) | 4 (31) | |
| Years in practice, n (%) | <.001 | |||
| ≤5 | 134 (75) | 19 (11) | 25 (14) | |
| 6–10 | 76 (75) | 8 (8) | 18 (18) | |
| 11–20 | 140 (71) | 16 (8) | 40 (20) | |
| >20 | 188 (58) | 45 (14) | 90 (28) | |
| Income structure, n (%) | .31 | |||
| Salary without performance incentive | 87 (66) | 16 (12) | 29 (22) | |
| Salary with performance incentive | 142 (71) | 23 (11) | 36 (18) | |
| Relative value unit based | 103 (69) | 16 (11) | 30 (20) | |
| Percentage of billing or collection | 161 (69) | 22 (9) | 52 (22) | |
| Other | 44 (54) | 11 (14) | 26 (32) | |
| Cases/y, n (%) | .003 | |||
| <200 | 58 (55) | 19 (18) | 28 (27) | |
| 200–500 | 223 (65) | 32 (9) | 86 (25) | |
| >500 | 254 (73) | 37 (11) | 59 (17) | |
| Completion of hand surgery fellowship, n (%) | .69 | |||
| Yes | 522 (67) | 86 (11) | 166 (21) | |
| No | 16 (64) | 2 (8) | 7 (28) | |
| Was WALANT part of residency/fellowship training? | <.001 | |||
| Yes | 122 (87) | 12 (9) | 6 (4) | |
| No | 397 (63) | 74 (12) | 158 (25) | |
| Population in practice location, n (%) | .60 | |||
| Urban | 265 (66) | 43 (11) | 92 (23) | |
| Suburban | 229 (67) | 38 (11) | 73 (21) | |
| Rural | 44 (75) | 7 (12) | 8 (14) | |
For CTR, 6% of the 480 respondents reported that either they or their institution had a financial gain associated with performing WALANT procedures. However, surgeons who reported financial gains were not more likely to perform WALANT CTR compared with those who reported no gain (P = .11). For TDR, 9% of the 480 respondents reported that either they or their institution had a financial gain associated with performing WALANT TDR. Surgeons reporting financial gain were less likely to perform WALANT TDRs compared with those who reported no financial gain (P = .01).
Table 5 illustrates potential barriers to performing WALANT cases. A total of 41% of respondents reported that greater than 90% of patients chose a WALANT procedure when it was offered as an option. For CTR, 13% did not offer patients WALANT, whereas 43% offered WALANT to all patients. Moreover, 51% of surgeons reported that an anesthesia staff member was required to be present for WALANT cases at their institution. Table 6 provides categorized responses for reasons why surgeons elected not to use WALANT. Sixteen percent reported that they preferred a tourniquet or had concerns regarding visualization with WALANT. Only 2% of respondents had concerns regarding epinephrine use in the hand.
Table 5.
Potential Barriers to Performing WALANT
| Response to Question | Surgeons Responding, n (%) |
|---|---|
| Surgeons who reported percentage of patients offered WALANT who elect to undergo it (532 surgeons responded [61%]): | |
| 0% of patients | 4 (1) |
| 1% to 50% of patients | 91 (17) |
| 50% to 90% patients | 217 (41) |
| ≥90% of patients | 220 (41) |
| Surgeons offering WALANT to CTR, n (%) (533 surgeons responded [61%]): | |
| I offer WALANT to all. | 231 (43) |
| I offer WALANT to patients who can tolerate being awake. | 151 (28) |
| I only offer WALANT to patients who request no anesthesia. | 80 (15) |
| I do not offer WALANT. | 71 (13) |
| Surgeons offering WALANT to trigger digit release patients, n (%) (529 surgeons responded [61%]): | |
| I offer WALANT to all. | 328 (62) |
| I offer WALANT to patients who can tolerate being awake. | 120 (23) |
| I only offer WALANT to patients who request no anesthesia. | 46 (9) |
| I do not offer WALANT. | 35 (7) |
| Is anesthesia team member required to be present for WALANT case? (N [%]) [517 surgeons (59%) responding] | |
| Yes | 233 (45) |
| No | 265 (51) |
| Not sure | 19 (4) |
Table 6.
Categorized Responses From ASSH Members for Not Performing WALANT Procedures (n = 266)∗
| Categorized Response | n (%) |
|---|---|
| Prefer tourniquet/visualization issues | 37 (16) |
| Satisfied with current techniques | 37 (16) |
| Unfamiliar with WALANT/lack of training | 33 (14) |
| Efficiency | 33 (14) |
| Patient preferences | 28 (12) |
| Administrative barriers | 28 (12) |
| Anesthesia concerns | 21 (9) |
| Other/unclear reason | 20 (9) |
| Outside scope of practice | 13 (6) |
| Financial concerns | 5 (2) |
| Use of epinephrine | 4 (2) |
| Concerns regarding WALANT effectiveness | 3 (1) |
| Sterility | 1 (0) |
| Impact on training residents/fellows | 1 (0) |
Data are presented as n (%).
Discussion
Currently, 62% of respondents (which included 23% of active ASSH members) perform WALANT procedures. Our results suggest that current WALANT users tend to be younger, higher-volume, North American surgeons. The most frequently performed WALANT procedures are TDR, followed by CTR, de Quervain release, and extensor tendon repair. A 2014 survey study of ASSH members by Munns and Awan7 reported that 8% of surgeons were using WALANT for CTR. We report that 16% of ASSH member respondents are performing 100% of CTRs with WALANT and 43% are offering WALANT for CTRs. These data indicate that WALANT use for CTR is increasing for ASSH members.
Although WALANT use is increasing for CTR, widespread adoption of WALANT for surgeries of longer duration and complexity, including flexor tendon repairs, appears to be slower. In a 2016 ASSH survey study of zone II flexor tendon repairs conducted by Gibson et al,8 the authors noted that only 20% of respondents had ever performed this procedure using WALANT; 11% employed it for all flexor tendon repairs. In comparison, we report that 52% of respondents performed 10% or more of flexor tendon repairs using WALANT, and only 5% performed all flexor tendons repairs with WALANT. Trapeziometacarpal arthroplasty, distal radius fracture fixation, and hand fracture fixation are infrequently performed using WALANT.
This survey emphasizes some substantial institutional barriers to WALANT implementation. There have been a number of investigations analyzing WALANT-associated cost-savings. Rhee et al5 reported 70% to 85% cost-savings for the Military Healthcare System with a procedure room–based WALANT program. Eliminating preoperative testing, anesthesia fees, and facility fees from operating rooms can contribute to lower costs associated with WALANT in a procedure room. Kazmers et al6 reported on total direct costs for open CTR performed with either sedation or local anesthesia only in operating rooms and procedure rooms. For open CTR performed with local anesthetic only, performing the procedure in an operating room compared with a procedure room resulted in a 6.3-fold increase in total direct costs.6
Respondents were asked whether there was any personal or institutional financial gain associated with WALANT use. Potentially, by eliminating operating room and anesthesia fees, surgeons or institutions could contract with insurance companies to increase professional fees for these office-based WALANT procedures. Less than 10% of respondents reported financial gain associated with performing WALANT procedures, and those surgeons were not more likely to use WALANT compared with other surgeons. More detailed survey analyses in the future may be required to better understand the financial implications of WALANT procedures. Respondents to our survey reported that only 24% of WALANT cases were being performed in a procedure room. Kazmers et al6 also reported an 11-fold increase in total direct costs for open CTR performed in an operating room with monitored anesthesia care sedation compared with procedure room CTR with local anesthesia, in part owing to anesthesia and hospital payments. We report that 45% of respondents stated that anesthesia staff was required to be present for WALANT cases at their facility. Anesthesia staffing requirements, particularly for WALANT cases performed in an operating room, appear to be a major current barrier to maximizing potential cost-savings associated with WALANT.
There were several limitations of this study. A lower response rate may be prone to selection bias. It is possible that ASSH members who did not perform WALANT may have been less likely to respond to the survey. With only 23% of members responding, there was some inherent response bias and the results may not be representative of all ASSH members. Our longer survey may have contributed to some respondents choosing not to answer all questions owing to question fatigue. However, a shorter survey would not have allowed for a detailed analysis of current WALANT trends. Surgeons self-reported reasons why patients chose WALANT compared with other forms of anesthesia, and this was subject to recall bias. We chose to limit the scope of this investigation to WALANT procedures and did not solicit information regarding the use of local anesthesia with a tourniquet for shorter cases.
The results of this survey illustrate current WALANT use among ASSH members and define the demographics of those using WALANT. Surgeon familiarity with WALANT and an acceptance of the use of epinephrine in the hand have increased. Lack of familiarity with the technique, concerns regarding operating room efficiency, and patient preferences remain considerable barriers to more widespread adoption of WALANT procedures.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received by the authors related directly or indirectly to the subject of this article.
References
- 1.Lalonde D.H. Wide-awake flexor tendon repair. Plast Reconstr Surg. 2009;123(2):623–625. doi: 10.1097/PRS.0b013e318195664c. [DOI] [PubMed] [Google Scholar]
- 2.Lalonde D.H. Wide-awake extensor indicis proprius to extensor pollicis longus tendon transfer. J Hand Surg Am. 2014;39(11):2297–2299. doi: 10.1016/j.jhsa.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Hagert E., Lalonde D.H. Wide-awake wrist arthroscopy and open TFCC repair. J Wrist Surg. 2012;1(1):55–60. doi: 10.1055/s-0032-1312045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson R., Higgins A., Conrad J., Bell M., Lalonde D. The wide-awake approach to Dupuytren’s disease: fasciectomy under local anesthetic with epinephrine. Hand (N Y) 2010;5(2):117–124. doi: 10.1007/s11552-009-9239-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rhee P.C., Fischer M.M., Rhee L.S., McMillan H., Johnson A.E. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42(3):139–147. doi: 10.1016/j.jhsa.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 6.Kazmers N.H., Presson A.P., Xu Y., Howenstein A., Tyser A.R. Cost implications of varying the surgical technique, surgical setting, and anesthesia type for carpal tunnel release surgery. J Hand Surg Am. 2018;43(11):971–977. doi: 10.1016/j.jhsa.2018.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Munns J.J., Awan H.M. Trends in carpal tunnel surgery: an online survey of members of the American Society for Surgery of the Hand. J Hand Surg Am. 2015;40(4):767–771. doi: 10.1016/j.jhsa.2014.12.046. [DOI] [PubMed] [Google Scholar]
- 8.Gibson P.D., Sobol G.L., Ahmed I.H. Zone II flexor tendon repairs in the United States: trends in current management. J Hand Surg Am. 2017;42(2):99–108. doi: 10.1016/j.jhsa.2016.11.022. [DOI] [PubMed] [Google Scholar]