Abstract
Background
The purpose of the present study was to systematically review the current treatment strategies for the treatment of Neer type IIB distal clavicle fractures in terms of functional outcome and complication rates and to examine the most appropriate surgical method by comparing all the available surgical techniques and implants.
Methods
We performed a systematic review of the existing literature (2000–2021) in accordance with the PRISMA statement. We searched PubMed, Scopus, Web of Science, Research Gate and Google Scholar using the general terms ‘distal AND clavicle AND fracture’ to capture as many reports as possible. The MINORS tool was used to assess the risk of bias of the nonrandomized studies. We categorized the reported surgical techniques into four main types: open or arthroscopic coracoclavicular (CC) stabilization, locking plate fixation with or without CC augmentation, hook plate fixation and acromioclavicular joint (ACJ) transfixation. We reported findings for two main outcomes: clinical results and complication rates categorized into major and minor.
Results
Our database search yielded a total of 630 records; 34 studies were appropriate for qualitative analysis. There were 790 patients, with a mean age of 40.1 years, a female percentage of 37% and a mean follow-up period of 29.3 months. In total, 132 patients received a hook plate, 252 received a locking plate, 368 received CC stabilization and 41 received transacromial transfixation. All studies were retrospective and had fair MINORS scores. Locking plate, CC stabilization and ACJ transfixation showed similar clinical results but were much better than hook plate fixation; CC augmentation did not significantly improve the outcome of locking plate fixation. The rate of major complications was similar among groups; hook plate and AC joint transfixation had the worst rates of minor complications. Open CC techniques were slightly better than arthroscopic techniques.
Conclusions
The present systematic review for the optimal fixation method for Neer type IIB fractures of the distal clavicle showed similar major complication rates among techniques; the hook plate technique demonstrated inferior clinical results to other techniques. Open CC stabilization and locking plate fixation without CC augmentation seem to be the best available treatment options.
Keywords: Distal clavicle fractures, Neer type IIB, Coracoclavicular stabilization, Hook plate, Locking plate, ACJ transfixation
Introduction
Fractures of the distal end of the clavicle account for 10–30% of all clavicle fractures, are displaced in 50% of cases and, when treated conservatively, can lead to symptomatic malunion or nonunion in 10–44% of cases [1, 2]. Displaced fractures are considered the Neer-Graig subtypes IIA, IIB and V, which usually require operative intervention [3–5]. Cho et al. [6] proposed a modified classification system to include the tiny “extralateral” type (IIC), where both of the CC ligaments are detached from the medial fragment; this type may not be amenable for traditional hardware due to its small size, and other techniques of CC stabilization are needed [7].
To date, there is no optimal surgical technique for managing the unstable types (IIA, IIB, IIC or V) of distal clavicle fractures. Numerous surgical techniques have been described in the literature and consist of three main categories: (a) rigid internal fixation with plates, coracoclavicular screws and Knowles pins; (b) flexible fixation with or without arthroscopic assistance (tension band wiring and CC stabilization with buttons, sutures, anchors, tapes, cables and synthetic grafts, autografts or allografts); and (c) mixed techniques, especially in terms of coracoclavicular augmentation to support a standard locking plate using screws, anchors, buttons or cables [7–18].
In a recent survey [19] among British Elbow and Shoulder Society consultant surgeons, there was considerable heterogeneity in the management of patients with distal clavicle fractures; the most important factor in favour of operative treatment was the degree of displacement (90%), while the most common operative intervention was the locking plate (68%), although there was no clear consensus regarding other fixation methods. According to the authors, the indications for surgery and the optimal fixation method remain uncertain, indicating a clear need for pragmatic multicentre clinical research in this area.
To date, several systematic reviews and meta-analyses [20–28] have shown inconsistent clinical results, time to union and complication rates in favour of one technique to another. For example, Asadollahi and Bucknill (2019) [23], in a systematic review of eleven comparative hook plate studies, including 634 patients, found no significant difference in the functional outcomes and union rates among hook plate fixation, coracoclavicular (CC) stabilization, and locking plate fixation. In contrast, Uittenbogaard et al. (2021) [26], in a systematic review of 59 studies, including 2284 patients, found that hook plates showed lower Constant-Murley scores than coracoclavicular fixation, but there was no significant difference when the hook plate was compared with the locking plate and tension band wire/K-wire groups. An important bias of these studies is the general homogenization of all displaced fractures as Neer type ΙΙ without clarification of the specific subtypes, especially IIA and IIB (IIC). In an effort to increase the current evidence on distal clavicle fractures, we have already published [27] a systematic review on the safety and efficacy of coracoclavicular fixation techniques in Neer type IIB (IIC) fractures. We included 21 studies with 421 patients; the reported clinical results were very good to excellent, and the overall major and minor complication rates were 2.6% and 12.8%, respectively.
Based on all these controversies, the purpose of the present study was to systematically review the current treatment strategies for Neer type IIB (or IIC) distal clavicle fractures in terms of functional outcomes and complication rates and to examine the most appropriate surgical method for this particular type of fracture, comparing all the available surgical techniques and implants.
Material and methods
We performed a systematic review of the existing literature for Neer type IIB (IIC) distal clavicle fractures in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [29].
Inclusion criteria
Our purpose was to identify randomized trials, cohort or case–control studies, comparative studies and case series, evaluating the clinical outcomes and complication rates of Neer type IIB (C) distal clavicle fractures in adult patients. We did not exclude comparative studies of two or more different surgical methods, but we excluded patients with other types of distal clavicle fractures (IIA, V) when presented together with type IIB fractures. Studies were only reviewed if the published manuscript was in the English, French, German or Spanish language; had at least 6 months follow-up evaluation; and provided clinical outcomes with objective clinical scores, complication rates and reoperation rates. We excluded any studies that did not meet the above criteria, studies that reported on fewer than 5 patients and comparative studies of different Neer types that did not separate the outcomes for each type.
Study identification and selection
We searched the PubMed (Medline and PubMed Central), Scopus, Web of Science, Research Gate, Google Scholar, and Cochrane Central Register of Controlled Trials electronic databases to retrieve studies published between January 2000 and November 2021. Our search strategy included a combination of keyword terms, including ‘distal AND clavicle AND fracture’, to capture as many reports as possible using a more general terminology. We also supplemented our search by screening the references of relevant published manuscripts, and we exported all captured studies into a reference manager library (EndNote X9), removing all duplicates. The results were evaluated by two independent reviewers (AP and ZK) at both the title-abstract and full-text levels; any discrepancies were solved during title-abstract screening by including the article by default and during full-text screening by senior author consensus.
Data collection
All relevant data were extracted using piloted forms and exported to a digital spreadsheet (Microsoft® Excel). Data extraction was performed by two independent reviewers. We classified extraction fields into 5 main categories: study methods, demographics, surgical intervention, clinical outcomes and complications. Any discrepancies in the extracted data were resolved by thoroughly evaluating the manuscripts during consensus meetings.
Risk of bias assessment
We did not find any randomized controlled trials (RCTs); thus, the Methodological Index for Non-Randomized Studies (MINORS) was used to assess the risk of bias in nonrandomized studies [30]. For all studies, the first 8 items of this tool included the following: a clearly stated aim; the inclusion of consecutive patients; prospective data collection; endpoints appropriate for the study aim; unbiased assessment of study endpoint; < 5% lost to follow-up; and a prospective calculation of study size. Additional criteria in the case of comparative studies were an adequate control group, contemporary groups, baseline equivalence, and adequate statistical analyses. The items were scored 0 if not reported, 1 when reported but inadequate, and 2 when reported and adequate; the global ideal score was 16 for noncomparative studies and 24 for comparative studies. Methodological quality was categorized a priori as follows: a score of 0–8 or 0–12 was considered poor quality, 9–12 or 13–18 was considered fair quality, and 13–16 or 19–24 was considered excellent quality for noncomparative and comparative studies, respectively.
Data synthesis
We synthesised all studies qualitatively using descriptive statistics where applicable. We categorized the reported surgical techniques into four main types: (a) open or arthroscopic coracoclavicular stabilization (CCS) with buttons, sutures, tapes, wires, cables with or without interfragmentary sutures, tension bands or KWs; (b) locking plate fixation (LPF) with or without CC augmentation with anchors, buttons, CC screws or sutures and/or interfragmentary fixation; (c) hook plate fixation (HPF) and d) AC joint transfixation (ACJTF) using KW or Steinman pins. We reported findings for two main outcomes: (a) clinical results, evaluated by synthesising and summarizing data from objective clinical scores specifically designed for the shoulder (CS: Constant Score, ASES: American Shoulder and Elbow Surgeons Shoulder score, UCLA: University of California at Los Angeles Shoulder Score) and (b) complication rate, categorized into major (peri-implant fracture, implant failure, nonunion, coracoid or acromial fracture, deep infection) and minor (malunion—delayed union, hardware irritation/migration/prominence or breakage, subacromial osteolysis, clavicular erosion, button subsidence, peri-anchor or screw osteolysis, slight loss of reduction, AC joint arthrosis, pain-discomfort, frozen shoulder stiffness, superficial infection and hypertrophic scar-wound breakdown).
Statistical analysis
Primarily, a set of clinical scores was available for meta-analysis among studies. The default clinical score that was used was the Constant score, available in the majority of the studies; otherwise, ASES or UCLA scores were used (with the latter one being converted to the 0–100 scale). The effect size that was meta-analysed was the mean ± SD. In cases where the range (min–max) was available instead of SD, the SD was approximately computed as the range divided by the number 4. Pooling effect sizes were held with the inverse variance method, tau^2 was computed via the Sidik-Jonkman (SJ) estimator and its confidence intervals via the Q-profile method, while Hartung-Knapp adjustment for random effects model was also used. Overall, the random effects model was utilized, and means were considered untransformed (raw). Heterogeneity was quantified with the indices I^2 and tau^2, as well as with the application of Cochran’s Q test. Confidence and prediction intervals were computed at the level of 95%. Finally, the meta-analysis outcome visualization was performed with summary forest plots.
In sequence, a comparison of the meta-analysis outcomes among sets of studies was performed with the use of an analysis of variance (ANOVA) procedure that took into account the generated summary statistics as input. Post hoc pairwise comparisons, where available, were performed using Bonferroni correction. Similarly, proportions of the major and minor complications of the same sets of studies were compared to each other, with the application of Pearson’s chi^2 test of independence. Once more, post hoc pairwise comparisons, where available, were performed using Bonferroni correction. All statistical tests were two-sided, and statistical significance was defined as p < 0.05. Implementation was performed with R, the language for statistical computing, along with the RStudio IDE, both of which are well-known open-source products. More specifically, a set of functions from the base library were used and from the libraries “meta”, “metafor”, “dmetar”, “ggplot2”, and “binom”.
Results
Data extraction
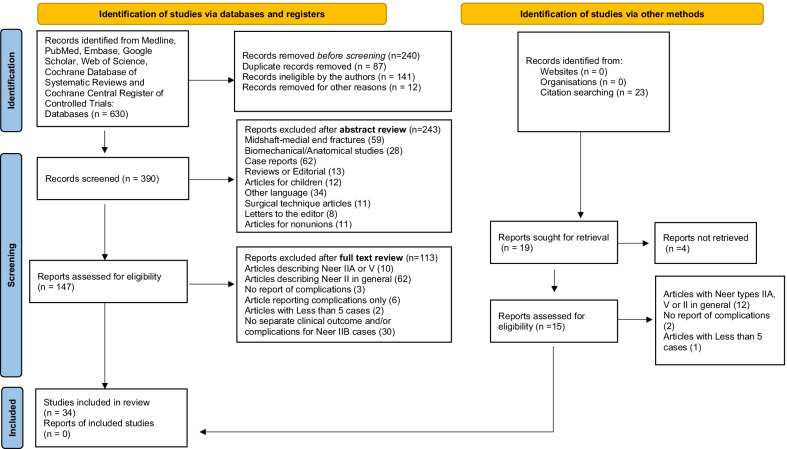
Our database search following duplicate removal yielded a total of 630 records; 240 were removed after title review and 243 after abstract review. We retrieved the full texts of 147 manuscripts to screen them in their entirety; thirty-four studies were deemed appropriate for inclusion in our qualitative synthesis (Table 1). The most common reasons for the exclusion of full-text articles (113) were studies reporting on Neer type II fractures in general (N = 62) or only om IIA and V types (N = 10) and studies without distinct clinical outcomes and/or complication rates among Neer type IIA and IIB fractures (n = 30).
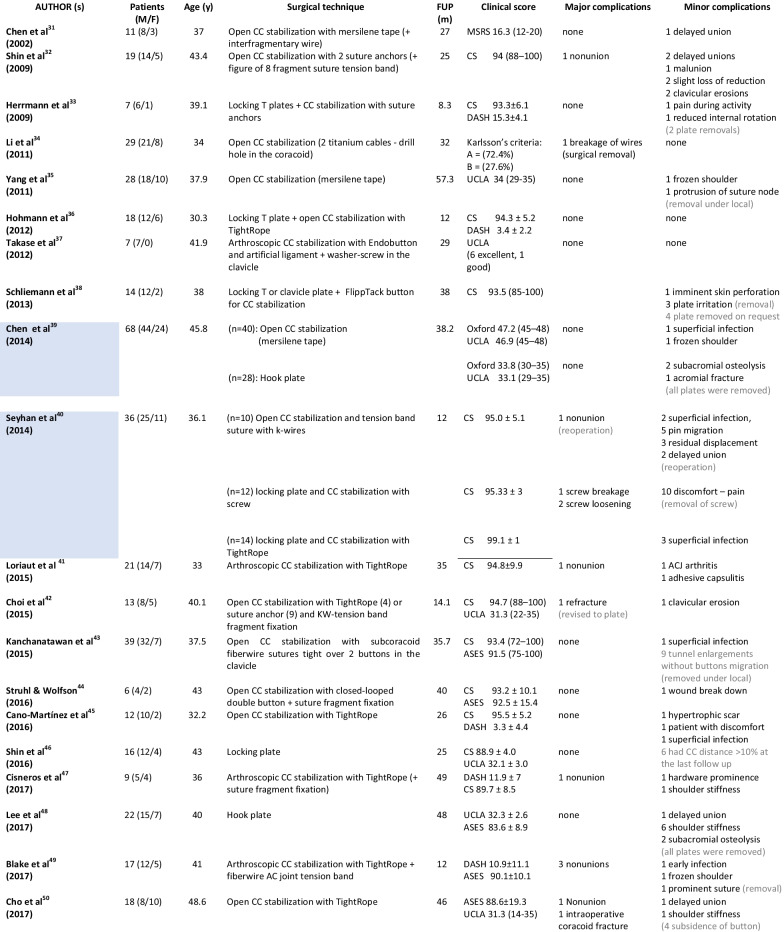
Table 1.
PRISMA work flow and eligibility of the studies
Characteristics of included studies
The total number of retrieved patients with Neer type IIB (IIC) distal clavicle fractures was 790, ranging from 6 to 82 patients. The mean age of the patients was 40.1 years (30.3–49 years), the female percentage was 37%, and the mean follow-up period was 29.3 months (4.6–67 months). The key characteristics of the 34 included studies are summarized in Table 2.
Table 2.
Overall characteristics of the included studies (in light blue are comparative studies)
MSRS, modified shoulder rating scale; FUSSs, Fudan University Shoulder Scores.
In total, 132 (16.7%) patients received a hook plate [39, 48, 57, 58, 60]; 252 (31.8%) received a locking plate [7, 18, 33, 36, 38, 40, 46, 52, 53, 58–62]; 368 (46.4%) received CC stabilization [7, 31, 32, 34, 35, 37, 39–45, 47, 49, 50, 54–56]; and 41 (5.1%) received transacromial transfixation [51]. In the locking plate group, the majority of patients (82%) had additional CC augmentation (CCA) with a) coracoid screws (7.5%); b) CC sutures, cables or anchors (44%); and c) CC buttons (30.5%). In the CC stabilization group, there were 91 arthroscopic procedures (49 with additional ACJ transfixation, 42 without) and 274 open procedures (108 with ACJ transfixation and 166 without). Finally, there were 6 retrospective comparative studies comparing (a) open CC stabilization with tape versus hook plate [39], (b) open CC stabilization + tension band suture + k-wires versus locking plate + CC stabilization with screw versus locking plate + CC stabilization with TightRope [40], (c) locking plate vs. hook plate [58], (d) locking plate versus locking plate + CC stabilization with anchor [59], (e) locking plate + suture CC stabilization + transosseous sutures vs. open CC stabilization with suture loop + transosseous sutures [7] and (f) locking plate + CC stabilization with soft anchor vs. hook plate [60].
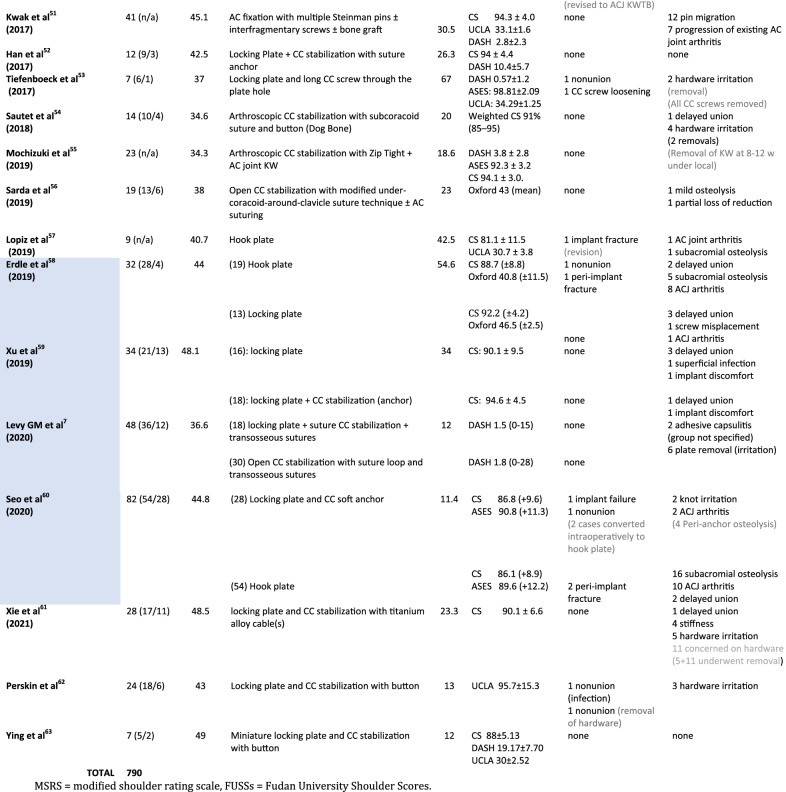
Risk of bias assessment
All studies were retrospective, with the majority of them having a fair MINORS score (Table 3). Only 2/28 noncomparative studies demonstrated an “excellent” score greater than 12 (max = 16). Among the 6 comparative studies, only one had an “excellent” score of 20 (max = 24). Thus, our systematic review had a low level of evidence (IV).
Table 3.
Risk of bias assessment of the included studies according to MINORS tool
Comparative studies are in blue
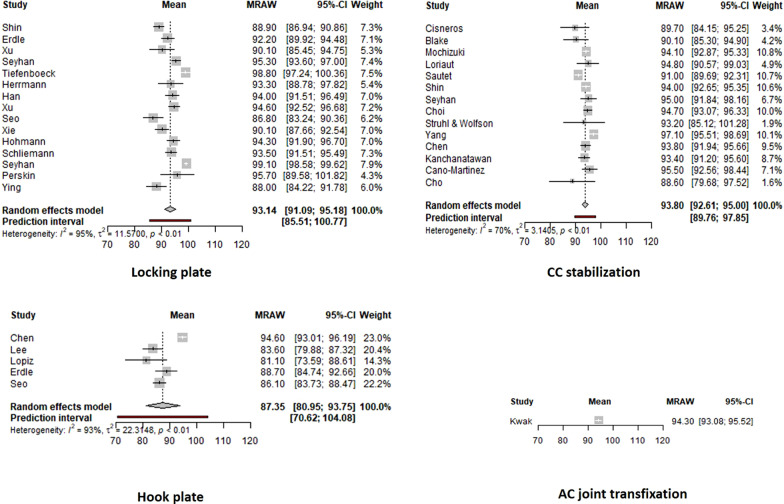
Outcome scores
Clinical results were reported with various clinical scores, including the Constant Score (27 studies), UCLA (13 studies), DASH (12 studies), ASES (8 studies), Oxford score (5 studies), Karlsson’s criteria (1 study) and Modified Shoulder Rating Scale for Clavicle Fractures (1 study). Twenty-three studies (67.7%) utilized more than one score for final clinical evaluation. A meta-analysis was performed that included all studies utilizing the Constant, ASES and UCLA scores (after transformation to a 100-scale). The forest plots of the four main techniques are presented in Fig. 1. Locking plate, CC stabilization and AC joint transfixation showed excellent clinical results in contrast to hook plate, which showed statistically significant lower clinical scores (p = 0.0009). The comparison of locking plate fixation with and without CC augmentation showed no difference (p = 0.3029); similarly, no difference was noticed among the 3 groups of locking plate augmentations (anchors, CC screw, button) [p = 0.7613]. Finally, the comparison between arthroscopic and open CC stabilization techniques showed a statistically important difference in favour of better clinical outcomes for open techniques (p = 0.0416).
Fig. 1.
Forest plots of the overall clinical outcome for the four surgical techniques
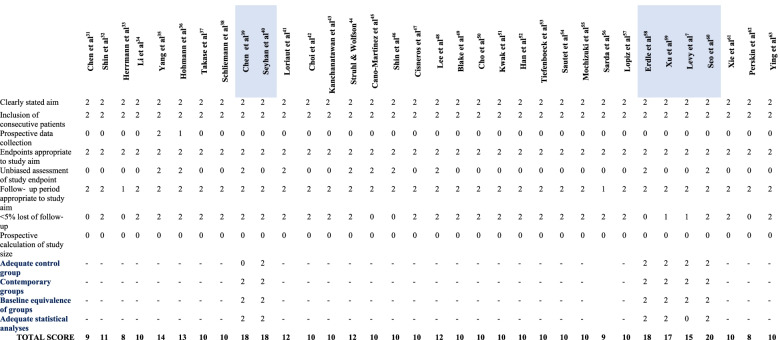
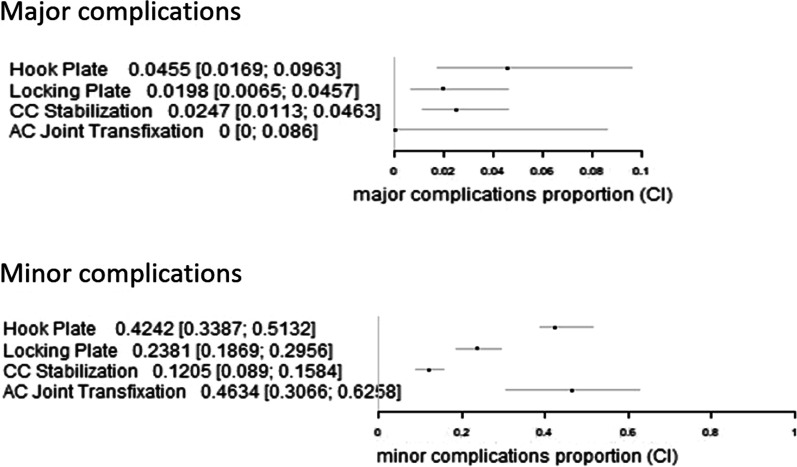
Complications
The overall major complication rate was 4.5% for the hook plate, 1.9% for the locking plate with CC augmentation and 2.4% for the CC stabilization group (Table 4). Interestingly, there were no major complications in the plate fixation without CC augmentation and ACJ transfixation groups. Regarding minor complications, the AC joint transfixation group demonstrated the highest complication rate (46%), followed by the hook plate group (42%), the locking plate group (23.8%) and the CC stabilization group (14.24%). Our meta-analysis did not show any significant difference among the four groups regarding the major complication rate (p = 0.3147). Additionally, there was no difference between the locking plate groups with and without CC augmentation (p = 0.6431) or among the 3 augmentation subgroups (p = 0.6563). Finally, there was no difference between open and arthroscopic CC stabilization techniques (p = 0.3271).
Table 4.
Major and minor complications
| Implant/surgical technique | N = 790 | Major complications | Minor complications | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-union | Implant failure | Peri implant fracture | Deep infection | Coracoid or acromial fracture | Malunion – Delayed union | Hardware irritation, migration breakage, loosening | Subacromial osteolysis | Clavicular erosion | Button subsidence Peri-anchor or screw osteolysis | Slight Loss of reduction | AC joint arthrosis |
Pain /discomfort Frozen shoulder /stiffness |
Superficial infection |
Scar problems, skin irritation wound breakdown |
||
| Hook plate [39, 48, 57, 58, 60] | 132 | 1 | 4 | 1 | 5 | 26 | 19 | 6 | ||||||||
| Locking plate | 252 | |||||||||||||||
| (−) CC augmentation [46, 58, 59] | 45 | 6 | 2 | 6 | 1 | 1 | ||||||||||
| (+) CCA-screw [40, 53] | 19 | 1 | 6 | 10 | ||||||||||||
| (+) CCA-anchor(s), sutures, cables [7, 33, 52, 59–61] | 111 | 1 | 1 | 2 | 8 | 4 | 2 | 8 | ||||||||
| (+) CCA-button [18, 36, 38, 40, 62] | 77 | 2 | 1 | 3 | ||||||||||||
| CC stabilization | 365 | |||||||||||||||
| Arthroscopic (91) | ||||||||||||||||
| (+) ACJ transfixation [47, 49, 55] | 49 | 3 | 1 | 2 | 1 | 1 | ||||||||||
| (−) ACJ transfixation [37, 41, 54] | 42 | 1 | 1 | 4 | 1 | 1 | ||||||||||
| Open (274) | ||||||||||||||||
| (+) ACJ transfixation [7, 31, 32, 40, 42, 44, 56] | 108 | 2 | 1 | 6 | 5 | 4 | 6 | 2 | 1 | |||||||
| (−) ACJ transfixation [34, 35, 39, 43, 45, 50] | 166 | 1 | 1 | 1 | 1 | 1 | 3 | 2 | ||||||||
| AC joint trans-fixation [51] | 41 | 12 | 7 | |||||||||||||
In contrast, there was a significant difference in the rate of minor complications in favour of CC stabilization in contrast to other techniques (p < 0.0001). There was no difference in the rate of minor complications between the plate fixation with and without augmentation groups (p = 0.0646) or between the open and arthroscopic CC stabilization groups (p = 0.8438). The forest plot of the complication rate is presented in Fig. 2.
Fig. 2.
Forest plots of the overall major and minor complication rates
Discussion
The most important findings of the present systematic review on Neer type IIB (IIC) distal clavicle fractures are as follows: (a) the hook plate technique demonstrated lower functional scores in contrast to other techniques; (b) there was no difference in the rate of major complications among the four different techniques; (c) the CC augmentation of a standard locking plate with screws, sutures, cables, anchors or buttons did not improve clinical outcomes and provided a similar major complication rate, and the button augmentation subgroup had better results regarding minor complications; (d) open CC stabilization techniques showed better clinical outcomes than the arthroscopic techniques and same rate of major and minor complications; and (e) the AC joint transfixation technique had excellent early clinical outcomes and no major complications but the highest rate of minor complications (46%), although these results were extracted from only one study [51]. In this particular study, 7/41 (17%) patients had evidence of posttraumatic AC joint arthritis in a mean follow-up period of 30.5 months; this risk must be taken into account when AC transfixation is applied together with the possibility of KW breakage or migration (29%).
Our results are different from those the most recent systematic review by Uittenbogaard et al. (2021) [26] in 2284 patients, which included all Neer type II (IIA and IIB) distal clavicle fractures; according to these authors, the hook plate technique showed lower Constant scores than CC stabilization but no significant differences when the hook plate group was compared with the locking plate and tension band wire/K-wire groups. They also found higher Constant scores in those patients with supplemental CC fixation when locking plates were used, a finding that was not confirmed in our study.
Several other systematic reviews have also shown inconsistent results. Oh et al. [20] performed a systematic review in 365/425 surgically treated patients with Neer type II fractures (2011) before the wide use of locking plate fixation and found a higher complication rate with the use of the hook plate (40.7%) and tension band wiring (20.0%) than with coracoclavicular (4.8%), intramedullary (2.4%) and interfragmentary fixation (6.3%). Stegeman et al. [21] reported a meta-analysis of 21 studies including 350 patients (2013) with type II distal clavicle fractures; union was achieved in 98% of the patients, and the functional outcomes were similar among the treatment modalities (hook plate, different other plates, CC sutures, screws and Knowles pins). In this study, hook plate fixation was associated with an 11-fold increased risk of major complications compared to intramedullary fixation and a 24-fold increased risk compared to suture anchoring. Boonard et al. [22] performed a systematic review and network meta-analysis in 2018; among ten comparative studies (n = 505 patients) and one RCT study (n = 42), the Constant-Murley scores of coracoclavicular fixation were significantly higher than those of hook plate and tension band wiring. Asadollahi and Bucknill (2019) [23], in a systematic review of eleven comparative studies to hook plate fixation, including 634 patients, found no significant difference between the functional outcome and union rate between hook plate fixation, CC stabilization and locking plate fixation. Hook plate fixation resulted in a higher Constant score than tension band wiring (TBW) but was also associated with a higher complication rate than CC stabilization and the locking plate. Vannabouathong et al. [24] reported that in type II distal clavicle fractures, a locking plate with or without CC suturing yielded significantly better outcomes than K-wires with or without tension bands, CC suturing alone, a locking plate with a CC screw, a hook plate, and a sling. In 2021, Malik et al. [26] and Yagnik et al. [28] systematically reviewed the reports of arthroscopic or arthroscopically assisted CC stabilization techniques; despite overall good to excellent shoulder function in both reports, the first one found considerably lower union rates up to 70% and overall complication rates as high as 28.6%, and the second reported union rates in 94.1% of the fractures and overall complication rates of 27.4%, of which 12% were considered major complications, and only 6% required a reoperation for hardware-related complications. Finally, Panagopoulos et al. [27] systematically reviewed the safety and efficacy of CC stabilization techniques (67% open, and 33% arthroscopic) in 2021, particularly in Neer type IIB fractures, and found very good to excellent clinical scores and overall major and minor complication rates of 2.6% and 12.8%, respectively. Major complications were more frequent with arthroscopic-assisted techniques (4.3%) than with open techniques (1.8%).
From all these systematic reviews, it is clear that hook plate fixation is associated with more major complications and worse clinical results and should likely no longer be considered as an ideal implant for Neer type IIB distal clavicle fractures. In our meta-analysis, we found a similar rate of major complications to the other techniques but a significant difference in the rate of minor complications. The other techniques demonstrated similar clinical outcomes, high union rates and lower rates of complications, but we do not yet have a precise answer to whether CC augmentation to a standard locking plate is always necessary or whether arthroscopic CC stabilization with buttons is superior to the classic open technique. Nevertheless, the current trend in the literature is plate fixation with CC augmentation and open or arthroscopic CC stabilization techniques. A critical advantage of arthroscopic-assisted stabilization is the ability to recognize and address any concomitant intra-articular shoulder pathology during diagnostic arthroscopy. A recent study from Marín Fermín et al. [63] revealed a mean of 17.70% concomitant glenohumeral injuries, whereas 84.21% of them required additional surgical management; rotator cuff injuries, labral tears, and biceps pulley lesions were the most common concomitant injuries.
One of the strengths of our study is that it constitutes the first systematic review in the literature that analyses only Neer type IIB fractures of the distal clavicle. We included 34 reports with 790 patients, one of the largest populations even reported, and we were able to show that almost 80% of the cases were treated either with a locking plate (simple or augmented) or CC stabilization (open or arthroscopic). This shows a clear trend in the literature over the last 10 years towards the abandonment of the hook plate and AC joint transfixation techniques. On the other hand, our study has several limitations: (a) the discrepancies in the data available from the included studies and mainly the heterogeneity of fracture patterns as most of the studies did not subclassify the type II (A and B) (it is of major importance that > 100 studies were excluded from this review for that reason); (b) the low level of evidence of the included studies, as there were no randomized comparative or prospective studies; (c) discrepancies also existed in reported outcome measures, as follow-up was obtained at various time points and the evaluation was made with different and sometimes not shoulder-specific scores (DASH) (which, for example, can underestimate the incidence of AC joint arthritis in the long term); and d) the number of the included patients in these studies was relatively low.
Conclusions
Our systematic review and meta-analysis of the best available surgical technique for the treatment of Neer type IIB (IIC) distal clavicle fractures showed great heterogeneity among studies, a low level of evidence, inconsistent classification methods, and a lack of appropriate outcome evaluation and reporting of complications. While hook plate fixation seems to demonstrate inferior clinical results with a high rate of minor complications, locking plate fixation with or without cortical button augmentation and open CC stabilization showed the best results. More prospective comparative studies are needed to increase the existing level of evidence; such studies must include a large number of patients with proper subclassification of different Neer types, incidence of AC joint arthritis and detailed reports of major and minor complications.
Acknowledgements
Not applicable.
Abbreviations
- MINORS
Methodological Index for Non-Randomized Studies
- CC
Coracoclavicular
- ACJ
Acromioclavicular joint
- TBW
Tension band wiring
- RCTs
Randomized controlled trials
- CCs
Coracoclavicular Stabilization
- KW
Kirshner wire
- LPF
Locking Plate Fixation
- HPF
Hook Plate Fixation
- ACJTF
AC joint trans-fixation
- CS
Constant Score
- ASES
American Shoulder and Elbow Surgeons Shoulder score
- UCLA
University of California at Los Angeles Shoulder Score
Author contributions
AP searched, analyzed, designed and wrote the manuscript. KS did the literature search. IT did the literature search. JL made the statistical analysis. AK reviewed the manuscripts and assessed the eligibility. VA reviewed the manuscripts and assessed the eligibility. ZK helped in writing and final interpretation of the manuscript. All authors read and approved the final manuscript.
Funding
There was no funding during the design of the study and collection, analysis, interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication.
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Andreas Panagopoulos, Email: andpan21@gmail.com.
Konstantina Solou, Email: k.solou@gmail.com.
Irini Tatani, Email: irinitatani@gmail.com.
Ioannis K. Triantafyllopoulos, Email: sportdoc@otenet.gr
John Lakoumentas, Email: john.lakoo@gmail.com.
Antonis Kouzelis, Email: akouzelis@yahoo.gr.
Vasileios Athanasiou, Email: vassathanasiou@yahoo.com.
Zinon T. Kokkalis, Email: drkokkalis@gmail.com
References
- 1.Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord. 2017;18(1):82. doi: 10.1186/s12891-017-1444-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee R, Waterman B, Padalecki J, Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19(7):392–401. doi: 10.5435/00124635-201107000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 4.Craig EV. Fractures of the clavicle. In: Rockwood CA, Green DP, editors. Fractures in adults. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 1216–1217. [Google Scholar]
- 5.Sambandam B, Gupta R, Kumar S, Maini L. Fracture of distal end clavicle: a review. J Clin Orthop Trauma. 2014;5(2):65–73. doi: 10.1016/j.jcot.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho CH, Kim BS, Kim DH, Choi CH, Dan J, Lee H. Distal clavicle fractures: a new classification system. Orthop Traumatol Surg Res. 2018;104(8):1231–1235. doi: 10.1016/j.otsr.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Levy GM, Pinto NE, Woods BJ, Hermans D, Duckworth DG. Operative management of an extra-lateral distal clavicle fracture pattern: a study of 48 patients and a proposed update to the modified Neer classification. J Shoulder Elbow Surg. 2020 doi: 10.1016/j.jse.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Tan H-L, Zhao J-K, Qian C, Shi Y, Zhou Q. Clinical results of treatment using a clavicular hook plate versus a T-plate in Neer type II distal clavicle fractures. Orthopedics. 2012;35(8):e1191–e1197. doi: 10.3928/01477447-20120725-18. [DOI] [PubMed] [Google Scholar]
- 9.Hsu KH, Tzeng YH, Chang MC, Chiang CC. Comparing the coracoclavicular loop technique with a hook plate for the treatment of distal clavicle fractures. J Shoulder Elbow Surg. 2018;27(2):224–230. doi: 10.1016/j.jse.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 10.Kaipel M, Majewski M, Regazzoni P. Double-plate fixation in lateral clavicle fractures-a new strategy. J Trauma. 2010;69(4):896–900. doi: 10.1097/TA.0b013e3181bedf28. [DOI] [PubMed] [Google Scholar]
- 11.Furuhata R, Takahashi M, Matsumura N, Morioka H. Osteosynthesis using the anatomical plate with grasping arms for unstable distal clavicle fractures: a technical trick and clinical experience. J Orthop Trauma. 2021;35(7):e263–e267. doi: 10.1097/BOT.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 12.Jou IM, Chiang EP, Lin CJ, Lin CL, Wang PH, Su WR. Treatment of unstable distal clavicle fractures with Knowles pin. J Shoulder Elbow Surg. 2011;20(3):414–419. doi: 10.1016/j.jse.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 13.Esenyel CZ, Ceylan HH, Ayanoğlu S, Kebudi A, Adanir O, Bülbül M. Treatment of Neer Type 2 fractures of the distal clavicle with coracoclavicular screw. Acta Orthop Traumatol Turc. 2011;45(5):291–296. doi: 10.3944/AOTT.2011.2464. [DOI] [PubMed] [Google Scholar]
- 14.Robinson CM, Akhtar MA, Jenkins PJ, Sharpe T, Ray A, Olabi B. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br. 2010;92(6):811–816. doi: 10.1302/0301-620X.92B6.23558. [DOI] [PubMed] [Google Scholar]
- 15.Rose MT, Noyes MP, Denard PJ. Arthroscopy-assisted treatment of displaced distal clavicle fractures utilizing curved buttons and suture tape with a single coracoclavicular tunnel. Tech Hand Up Extrem Surg. 2018;22(3):94–98. doi: 10.1097/BTH.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 16.Badhe SP, Lawrence TM, Clark DI. Tension band suturing for the treatment of displaced type 2 lateral end clavicle fractures. Arch Orthop Trauma Surg. 2007;127(1):25–28. doi: 10.1007/s00402-006-0197-3. [DOI] [PubMed] [Google Scholar]
- 17.Vikas V, Bhatia N, Jalan D, Prakash J, Singh J, Khare S. Clinical Outcome of Neer type II lateral end clavicle fractures with coracoclavicular ligament disruption treated with pre-contoured locking plate and endobutton. Cureus. 2021;13(1):e12585. doi: 10.7759/cureus.12585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perskin CR, Tejwani NC, Jazrawi LM, Leucht P, Egol KA. Clinical outcomes of a combined osteoligamentous reconstruction technique of Neer Type IIB distal clavicle fractures. J Orthop. 2021;25:134–139. doi: 10.1016/j.jor.2021.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma V, Modi A, Armstrong A, Pandey R, Sharma D, Singh H. The management of distal clavicle fractures—a survey of UK shoulder and elbow surgeons. Cureus. 2021;13(8):e17305. doi: 10.7759/cureus.17305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131(4):525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- 21.Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84(2):184–190. doi: 10.3109/17453674.2013.786637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boonard M, Sumanont S, Arirachakaran A, et al. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(6):1065–1078. doi: 10.1007/s00590-018-2187-x. [DOI] [PubMed] [Google Scholar]
- 23.Asadollahi S, Bucknill A. Hook plate fixation for acute unstable distal clavicle fracture: a systematic review and meta-analysis. J Orthop Trauma. 2019;33(8):417–422. doi: 10.1097/BOT.0000000000001481. [DOI] [PubMed] [Google Scholar]
- 24.Vannabouathong C, Chiu J, Patel R, et al. An evaluation of treatment options for medial, midshaft, and distal clavicle fractures: a systematic review and meta-analysis. JSES Int. 2020;4(2):256–271. doi: 10.1016/j.jseint.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malik SS, Tahir M, Malik S, Kwapisz A, Jordan RW. Arthroscopically assisted coraco-clavicular ligament reconstruction in treatment of acute displaced distal clavicle fractures provides good to excellent shoulder function despite low union rates and high complication rates: a systematic review. Arthroscopy. 2021;S0749–8063(21):00672–681. doi: 10.1016/j.arthro.2021.06.034. [DOI] [PubMed] [Google Scholar]
- 26.Uittenbogaard SJ, van Es LJM, den Haan C, van Deurzen DFP, van den Bekerom MPJ. Outcomes, union rate, and complications after operative and nonoperative treatments of neer type II distal clavicle fractures: a systematic review and meta-analysis of 2284 patients. Am J Sports Med. 2021 doi: 10.1177/03635465211053336. [DOI] [PubMed] [Google Scholar]
- 27.Panagopoulos A, Solou K, Nicolaides M, Triantafyllopoulos IK, Kouzelis A, Kokkalis ZT. Coracoclavicular fixation techniques for Neer IIb and ‘extra-lateral’ fractures of the distal clavicle: a systematic review. JSES Rev Rep Tech. 2021 doi: 10.1016/j.xrrt.2021.06.007. [DOI] [Google Scholar]
- 28.Yagnik GP, Seiler JR, Vargas LA, Saxena A, Narvel RI, Hassan R. Outcomes of arthroscopic fixation of unstable distal clavicle fractures: a systematic review. Orthop J Sports Med. 2021;9(5):23259671211001773. doi: 10.1177/23259671211001773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 31.Chen CH, Chen WJ, Shih CH. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52(1):72–78. doi: 10.1097/00005373-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 32.Shin S-J, Roh KJ, Kim JO, Sohn H-S. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40(12):1308–1312. doi: 10.1016/j.injury.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 33.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40(3):236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 34.Li Y, Shi S, Ou-Yang YP, Liu TL. Minimally invasive treatment for Neer IIb distal clavicle fractures with titanium cable. J Trauma. 2011;71(2):E37–E40. doi: 10.1097/TA.0b013e318213f5a6. [DOI] [PubMed] [Google Scholar]
- 35.Yang SW, Lin LC, Chang SJ, Kuo SM, Hwang LC. Treatment of acute unstable distal clavicle fractures with single coracoclavicular suture fixation. Orthopedics. 2011;34(6):172. doi: 10.3928/01477447-20110427-10. [DOI] [PubMed] [Google Scholar]
- 36.Hohmann E, Hansen T, Tetsworth K. Treatment of Neer type II fractures of the lateral clavicle using distal radius locking plates combined with TightRope augmentation of the coraco-clavicular ligaments. Arch Orthop Trauma Surg. 2012;132(10):1415–1421. doi: 10.1007/s00402-012-1570-z. [DOI] [PubMed] [Google Scholar]
- 37.Takase K, Kono R, Yamamoto K. Arthroscopic stabilization for Neer type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132(3):399–403. doi: 10.1007/s00402-011-1455-6. [DOI] [PubMed] [Google Scholar]
- 38.Schliemann B, Roßlenbroich SB, Schneider KN, Petersen W, Raschke MJ, Weimann A. Surgical treatment of vertically unstable lateral clavicle fractures (Neer 2b) with locked plate fixation and coracoclavicular ligament reconstruction. Arch Orthop Trauma Surg. 2013;133(7):935–939. doi: 10.1007/s00402-013-1737-2. [DOI] [PubMed] [Google Scholar]
- 39.Chen CY, Yang SW, Lin KY, et al. Comparison of single coracoclavicular suture fixation and hook plate for the treatment of acute unstable distal clavicle fractures. J Orthop Surg Res. 2014;9:42. doi: 10.1186/1749-799X-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seyhan M, Kocaoglu B, Kiyak G, Gereli A, Turkmen M. Anatomic locking plate and coracoclavicular stabilization with suture endo-button technique is superior in the treatment of Neer Type II distal clavicle fractures. Eur J Orthop Surg Traumatol. 2015;25(5):827–832. doi: 10.1007/s00590-015-1617-2. [DOI] [PubMed] [Google Scholar]
- 41.Loriaut P, Moreau P-E, Dallaudière B, Pélissier A, Vu HD, Massin P, et al. Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device. Knee Surgery Sport Traumatol Arthrosc. 2015;23(5):1429–1433. doi: 10.1007/s00167-013-2772-9. [DOI] [PubMed] [Google Scholar]
- 42.Choi S, Kim S-R, Kang H, Kim D, Park Y-G. Modified tension band fixation and coracoclavicular stabilisation for unstable distal clavicle fracture. Injury. 2015;46(2):259–264. doi: 10.1016/j.injury.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 43.Kanchanatawan W, Wongthongsalee P. Management of acute unstable distal clavicle fracture with a modified coracoclavicular stabilization technique using a bidirectional coracoclavicular loop system. Eur J Orthop Surg Traumatol. 2016;26(2):139–143. doi: 10.1007/s00590-015-1723-1. [DOI] [PubMed] [Google Scholar]
- 44.Struhl S, Wolfson TS. Closed-loop double endobutton technique for repair of unstable distal clavicle fractures. Orthop J Sport Med. 2016;4(7):2325967116657810–2325967116657810. doi: 10.1177/2325967116657810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cano-Martínez JA, Nicolás-Serrano G, Andrés-Grau J, Bento-Gerard J. Treatment of distal-third clavicular fractures (Neer type ii-b) with a triple button device. Rev Esp Cir Ortop Traumatol. 2016;60(6):378–386. doi: 10.1016/j.recot.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 46.Shin S-J, Ko Y-W, Lee J, Park M-G. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elb Surg. 2016;25(6):942–948. doi: 10.1016/j.jse.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 47.Cisneros LN, Reiriz JS. Management of unstable distal third clavicle fractures: clinical and radiological outcomes of the arthroscopy-assisted conoid ligament reconstruction and fracture cerclage with sutures. Eur J Orthop Surg Traumatol. 2017;27(3):373–380. doi: 10.1007/s00590-017-1925-9. [DOI] [PubMed] [Google Scholar]
- 48.Lee W, Choi C-H, Choi Y-R, Lim K-H, Chun Y-M. Clavicle hook plate fixation for distal-third clavicle fracture (Neer type II): comparison of clinical and radiologic outcomes between Neer types IIA and IIB. J Shoulder Elb Surg. 2017;26(7):1210–1215. doi: 10.1016/j.jse.2016.11.046. [DOI] [PubMed] [Google Scholar]
- 49.Blake MH, Lu MT, Shulman BS, Glaser DL, Huffman GR. Arthroscopic cortical button stabilization of isolated acute neer type II fractures of the distal clavicle. Orthopedics. 2017;40(6):e1050–e1054. doi: 10.3928/01477447-20170925-06. [DOI] [PubMed] [Google Scholar]
- 50.Cho C-H, Jung J-H, Kim B-S. Coracoclavicular stabilization using a suture button device for Neer type IIB lateral clavicle fractures. J Shoulder Elb Surg. 2017;26(5):804–808. doi: 10.1016/j.jse.2016.09.048. [DOI] [PubMed] [Google Scholar]
- 51.Kwak SH, Lee YH, Kim DW, Kim MB, Choi HS, Baek GH. Treatment of unstable distal clavicle fractures with multiple steinmann pins-a modification of neer's method: a series of 56 consecutive cases. J Orthop Trauma. 2017;31(9):472–478. doi: 10.1097/BOT.0000000000000850. [DOI] [PubMed] [Google Scholar]
- 52.Han L, Hu Y, Quan R, Fang W, Jin B, Huang L. Treatment of neer IIb distal clavicle fractures using anatomical locked plate fixation with coracoclavicular ligament augmentation. J Hand Surg Am. 2017;42(12):1036.e1–1036.e6. doi: 10.1016/j.jhsa.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 53.Tiefenboeck TM, Boesmueller S, Binder H, et al. Displaced Neer Type IIB distal-third clavicle fractures-Long-term clinical outcome after plate fixation and additional screw augmentation for coracoclavicular instability. BMC Musculoskelet Disord. 2017;18(1):30. doi: 10.1186/s12891-017-1398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sautet P, Galland A, Airaudi S, Argenson JN, Gravier R. Arthroscopy-assisted fixation of fracture of the distal part of the clavicle by subcoracoid suture and clavicle button. Orthop Traumatol Surg Res. 2018;104(8):1237–1240. doi: 10.1016/j.otsr.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 55.Mochizuki Y, Kaneko T, Kawahara K, Toyoda S, Ikegami H, Musha Y. Outcome of arthroscopy-assisted treatment for distal clavicle fractures. Arch Orthop Trauma Surg. 2019;139(10):1393–1398. doi: 10.1007/s00402-019-03219-2. [DOI] [PubMed] [Google Scholar]
- 56.Sarda P. Lateral clavicle fractures with coracoclavicular ligament disruption (Neer’s Type IIB): review of literature and a new technique for all-suture fixation. Indian J Orthop. 2019;53(3):465–471. doi: 10.4103/ortho.IJOrtho_485_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lopiz Y, Checa P, García-Fernández C, Valle J, Vega ML, Marco F. Complications with the clavicle hook plate after fixation of Neer type II clavicle fractures. Int Orthop. 2019;43(7):1701–1708. doi: 10.1007/s00264-018-4108-3. [DOI] [PubMed] [Google Scholar]
- 58.Erdle B, Izadpanah K, Jaeger M, Jensen P, Konstantinidis L, Zwingmann J, et al. Comparative analysis of locking plate versus hook plate osteosynthesis of Neer type IIB lateral clavicle fractures. Arch Orthop Trauma Surg. 2017;137(5):651–662. doi: 10.1007/s00402-017-2645-7. [DOI] [PubMed] [Google Scholar]
- 59.Xu H, Chen WJ, Zhi XC, et al. Comparison of the efficacy of a distal clavicular locking plate with and without a suture anchor in the treatment of Neer IIb distal clavicle fractures. BMC Musculoskelet Disord. 2019;20:503. doi: 10.1186/s12891-019-2892-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seo JB, Kwak KY, Yoo JS. Comparative analysis of a locking plate with an all-suture anchor versus hook plate fixation of Neer IIb distal clavicle fractures. J Orthop Surg (Hong Kong) 2020;28(3):2309499020962260. doi: 10.1177/2309499020962260. [DOI] [PubMed] [Google Scholar]
- 61.Xie Z, Song M, Zhou J, Yin G, Lin H. Precontoured locking compression plate with titanium alloy cable system: in treatment of neer type IIb distal clavicle fracture. Orthop Surg. 2021;13(2):451–457. doi: 10.1111/os.12893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ying H, Wang J, Sun Y, Dai K, Yu C, Yang F. Treatment of unstable distal clavicle fractures (Neer type IIb): a modified system using a miniature locking plate with a single button. J Int Med Res. 2021;49(6):3000605211022505. doi: 10.1177/03000605211022505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Marín Fermín T, Migliorini F, Papakostas E, et al. Concomitant glenohumeral injuries in patients with distal clavicle fractures undergoing arthroscopic-assisted surgery: a systematic review. J Orthop Surg Res. 2022;17(1):31. doi: 10.1186/s13018-022-02919-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.