Abstract
We report the case of a 65‐year‐old male patient who presented with chest pain and was found to have a mediastinal paraganglioma between the left atrium and main pulmonary artery. This is the first reported case of a mediastinal paraganglioma resection utilization transection of the main pulmonary artery.
Keywords: cardiac tumor, cardiothoracic surgery, paraganglioma, pulmonary artery transection, tumor resection
Surgical resection is the standard of care for mediastinal paragangliomas. For paragangliomas located between the great vessels, transection of the main pulmonary artery may be utilized to gain optimal exposure and allow for complete resection.
![]()
1. INTRODUCTION
Paragangliomas are extra‐adrenal tumors that arise from autonomic neural ganglia. 1 Paragangliomas of the mediastinum have been reported in a handful of cases and represent just 0.3% of all mediastinal tumors. 2 , 3 Patients with catecholamine‐secreting mediastinal paragangliomas may present with symptoms of hypertension, tachycardia, or diaphoresis. However, the majority of mediastinal paragangliomas are nonfunctional and patients often present with nonspecific symptoms, such as chest pain, back pain, or dyspnea. Given that mediastinal paragangliomas are resistant to radiation and chemotherapy, complete surgical resection is the standard of care. Here, we report the case of a middle mediastinal paraganglioma surgically resected using a median sternotomy and main pulmonary artery transection. Informed consent was obtained, and Institutional Review Board approval was waived for the publication of this report.
2. CASE REPORT
The patient is a 65‐year‐old man with no significant past medical history who presented to the emergency department with symptoms of chest pain that radiated to his back. At the time, a computed tomography angiogram (CTA) of the chest found a 5.7 × 3.6 cm heterogeneous mass interposed between the left atrium and the main pulmonary artery (Figure 1A). The patient was referred to cardiac surgery for further workup of the finding.
FIGURE 1.
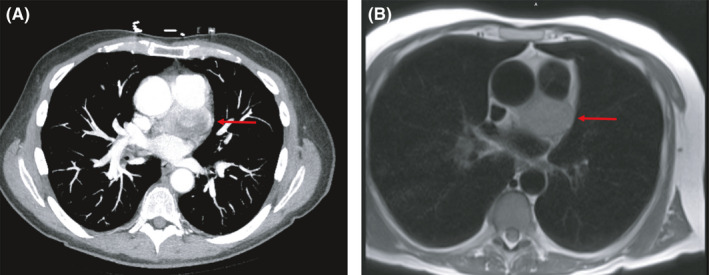
(A) Axial view from a CTA of the chest showing a 5.7 x 3.6 cm heterogeneous mass‐like structure (arrow) interposed between the left atrium and the main pulmonary artery. (B) MRI demonstrating a well‐circumscribed mass (arrow) in the middle mediastinum with area of central hypointensity
The patient underwent a workup that involved cardiac magnetic resonance imaging (MRI, Figure 1B) and positron emission tomography (PET) scans (Figure 2). The lesion was found to be a well‐circumscribed, enhancing mass in the middle mediastinum abutting the aortic root, main pulmonary artery, left superior pulmonary vein, and left atrium. The mass was found to have a central area of hypointensity and nonenhancement, likely representing blood products. The mass was intensely fluorodeoxyglucose (FDG)‐avid, and additional sub‐centimeter mildly hypermetabolic right hilar and prevascular lymph nodes were found. A transthoracic echocardiogram (TTE) revealed narrowing of the pulmonary artery just distal to the pulmonic valve and mild dilation of the aortic root to 4.3 cm.
FIGURE 2.

Sagittal view of a PET scan demonstrating an intensely FDG‐avid soft tissue mass (circled)
The findings of the workup seemed most consistent with a mediastinal mass, but a ruptured sinus of Valsalva aneurysm was also considered. Given the location of the mass with regards to its proximity to the great vessels, a multi‐disciplinary team recommended surgical resection both for diagnosis and treatment. A median sternotomy incision was utilized with institution of cardiopulmonary bypass. Several surgical approaches were considered. However, given the size of the mass and proximity to the left main coronary artery immediately posterior to the main pulmonary artery, it was decided to transect the pulmonary artery for best exposure, complete resection, and to ensure no injury to the left main, left anterior descending (LAD), or left circumflex (LCX) coronary arteries. The 5.5 × 4.0 × 2.5 cm mass was then completely resected away from the main pulmonary artery, the aorta, and the left main coronary artery to the bifurcation of the LCX and LAD arteries (Figure 3). The pulmonary artery was then closed with a running 4–0 Prolene suture.
FIGURE 3.
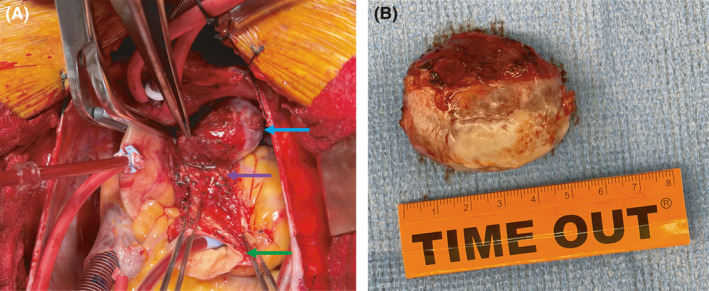
(A) Intraoperative photo showing exposed mass (blue arrow) after transection of the main pulmonary artery. The green arrow points at the transected pulmonary artery proximally with pump suction to keep the field clear. The purple arrow points at the left main coronary artery. (B) Intraoperative photo showing the 5.5 × 4.0 × 2.5 cm mass at time of removal
The patient did well post‐operatively and was discharged on post‐operative Day 3. Final pathology confirmed the diagnosis of a mediastinal paraganglioma that was positive for S100, synaptophysin, and SDHB and negative for AE1/AE3 (Figure 4).
FIGURE 4.
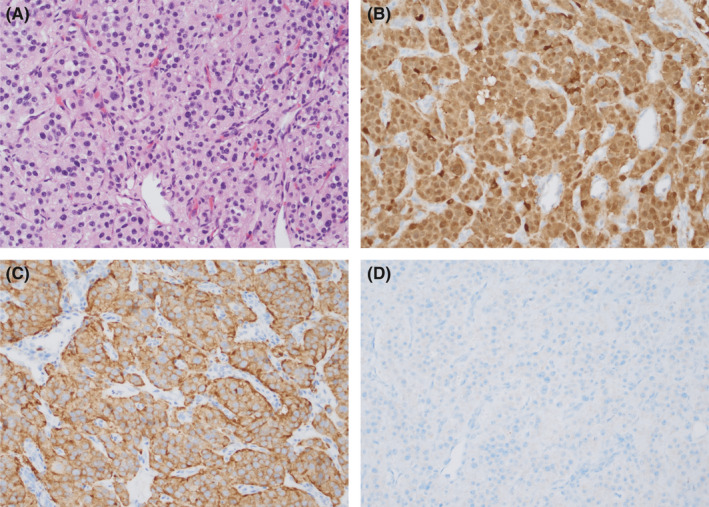
Pathology findings. (A) Hematoxylin and eosin stain. (B) Tumor positive for S100. (C) Tumor positive for synaptophysin. (D) Tumor negative for AE1/AE3
3. DISCUSSION
Paragangliomas are neuroendocrine tumors that arise from extra‐adrenal chromaffin cells. 1 Rarely, paragangliomas can occur in the mediastinum as slow‐growing, highly vascular tumors, often located near the great vessels. 4 With just 150 cases reported in the literature, mediastinal paragangliomas are extremely rare and account for <0.3% of all mediastinal masses. 2 , 3 , 5 Paragangliomas can arise from paravertebral aortosympathetic paraganglia in the posterior mediastinum or from aortopulmonary paraganglia of the anterior and middle mediastinum, as was seen in this case. 6 , 7 , 8 Rare case reports have also described paragangliomas occurring in the subclavian paraganglia of the superior mediastinum. 9
Some mediastinal paragangliomas are functional and can secrete catecholamines into circulation. In these cases, patients can present with symptoms related to catecholamine hypersecretion, such as hypertension, headache, diaphoresis, or tachycardia, and diagnoses can be made based on urine or plasma biochemical markers. 10 , 11 However, the majority of mediastinal paragangliomas are nonfunctional, which can present asymptomatically or with symptoms due to mass effect of the tumor, such as cough, dyspnea, chest pain, or back pain, as was the case with our patient. 10 , 12 Most mediastinal paragangliomas are found incidentally through imaging. Contrast‐enhanced computed tomography (CT) scans frequently reveal a heterogeneous mass with peripheral enhancement correlating with high vascularity and central latency representing tumor necrosis. On MRI, mediastinal paragangliomas are typically isointense or hypointense on T1‐weighted images and hyperintense on T2‐weighted images. 13
Mediastinal paragangliomas are resistant to radiation and chemotherapy. 4 Therefore, complete surgical resection is the standard of care. A retrospective review of cases reported in the literature found that the mean survival time with complete resection is 10.5 years, compared with 6.0 years in cases of incomplete resection. 4 However, complete resection is often difficult due to the close association of these tumors with the cardiac chambers and great vessels. Perioperative morbidity and mortality are typically associated with intraoperative bleeding, due to the high vascularity of these tumors, and catecholamine hypersecretion in cases of functional paragangliomas. To address these complications, some cases report using preoperative embolization to reduce intraoperative bleeding, 14 , 15 and others report utilizing α‐adrenergic blockade to prevent intraoperative catecholamine crisis. 16 Tumor recurrence following resection is common, with past studies demonstrating local recurrences in 55.7% of cases and metastatic spread in 26.6% of cases. 4 After resection, close follow‐up of patients for evidence of recurrence and metastasis is essential.
Surgical approaches for mediastinal paragangliomas typically involve a median sternotomy or thoracotomy. 10 For patients with posterior mediastinal paragangliomas, thoracoscopic surgery may be performed. 17 , 18 In our case, a median sternotomy was utilized because the mass was located between the pulmonary trunk and the aorta. Even so, the tumor was anatomically difficult to access and required transection of the main pulmonary artery. With this approach, optimal exposure was attained, and a macroscopically complete resection was performed. To the best of our knowledge, this is the first report of a mediastinal paraganglioma resection utilizing pulmonary artery transection.
Due to the rarity of these tumors, diagnostic and treatment guidelines come only from case reports. Given that surgical resection is the standard of care, it is important to define surgical approaches that allow for optimal exposure and complete resection. Our case is the first to highlight a unique surgical approach involving transection of the main pulmonary artery for complete resection of a middle mediastinal paraganglioma.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Alice L Zhou, Meghan E Halub, Benjamin L Shou, and Ahmet Kilic contributed to report design, drafting of the article, critical revision of the article, and approval of the article. Mira Lotfalla performed pathological examination of the tumor sample and contributed to drafting of the article, critical revision of the article, and approval of the article.
ETHICAL APPROVAL
Institutional Review Board approval was waived for this report.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGEMENTS
None.
Zhou AL, Halub ME, Lotfalla M, Shou BL, Kilic A. Pulmonary artery transection for resection of a middle mediastinal paraganglioma. Clin Case Rep. 2022;10:e05600. doi: 10.1002/ccr3.5600
Funding information
No funding was provided for this work.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Gunawardane PTK, Grossman A. Phaeochromocytoma and paraganglioma. In: Islam MdS, ed. Hypertension: From Basic Research to Clinical Practice. Advances in experimental medicine and biology. Springer International Publishing; 2017: 239‐259. doi: 10.1007/5584_2016_76 [DOI] [PubMed] [Google Scholar]
- 2. Drucker E, McLoud T, Dedrick C, Hilgenberg A, Geller S, Shepard J. Mediastinal paraganglioma: radiologic evaluation of an unusual vascular tumor. Am J Roentgenol. 1987;148(3):521‐522. doi: 10.2214/ajr.148.3.521 [DOI] [PubMed] [Google Scholar]
- 3. Wychulis AR, Payne WS, Clagett OT, Woolner LB. Surgical treatment of mediastinal tumors. The Journal of Thoracic and Cardiovascular Surgery. 1971;62(3):379‐392. doi: 10.1016/S0022-5223(19)42048-5 [DOI] [PubMed] [Google Scholar]
- 4. Lamy AL, Fradet GJ, Luoma A, Nelems B. Anterior and middle mediastinum paraganglioma: complete resection is the treatment of choice. The Annals of Thoracic Surgery. 1994;57(1):249‐252. doi: 10.1016/0003-4975(94)90419-7 [DOI] [PubMed] [Google Scholar]
- 5. Buchanan SN, Radecki KM, Chambers LW. Mediastinal paraganglioma. Ann Thorac Surg. 2017;103(5):e413‐e414. doi: 10.1016/j.athoracsur.2016.10.031 [DOI] [PubMed] [Google Scholar]
- 6. Nguyen DM, Gonzalez JN, Villamizar NR. Surgical management of mediastinal paraganglioma: all hands on deck! J Card Surg. 2020;35(8):2047‐2049. doi: 10.1111/jocs.14746 [DOI] [PubMed] [Google Scholar]
- 7. Rahi MS, Gunasekaran K, Amoah K, Rudolph D. Paraganglioma of the middle mediastinum. Respir Med Case Rep. 2020;31:101211. doi: 10.1016/j.rmcr.2020.101211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Suster S, Moran CA. Neuroendocrine neoplasms of the mediastinum. Pathol Patterns Rev. 2001;115(suppl_1):S17‐S27. doi: 10.1309/L38W-8P9X-X142-3N78 [DOI] [PubMed] [Google Scholar]
- 9. Takahashi R, Kawabe H, Koide N, et al. Superior mediastinal paraganglioma initially suspected of being a mediastinal thyroid goiter. Auris Nasus Larynx. 2020. doi: 10.1016/j.anl.2020.11.001. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 10. Brown ML, Zayas GE, Abel MD, Young WF, Schaff HV. Mediastinal paragangliomas: the mayo clinic experience. Ann Thorac Surg. 2008;86(3):946‐951. doi: 10.1016/j.athoracsur.2008.04.105 [DOI] [PubMed] [Google Scholar]
- 11. Lenders JWM, Pacak K, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: which test is best? JAMA. 2002;287(11):1427‐1434. doi: 10.1001/jama.287.11.1427 [DOI] [PubMed] [Google Scholar]
- 12. Takashima Y, Kamitani T, Kawanami S, et al. Mediastinal paraganglioma. Jpn J Radiol. 2015;33(7):433‐436. doi: 10.1007/s11604-015-0436-z [DOI] [PubMed] [Google Scholar]
- 13. Hamilton BH, Francis IR, Gross BH, et al. Intrapericardial paragangliomas (pheochromocytomas): imaging features. Am J Roentgenol. 1997;168(1):109‐113. doi: 10.2214/ajr.168.1.8976931 [DOI] [PubMed] [Google Scholar]
- 14. Matsumoto J, Nakajima J, Takeuchi E, Fukami T, Nawata K, Takamoto S‐I. Successful perioperative management of a middle mediastinal paraganglioma. J Thorac Cardiovasc Surg. 2006;132(3):705‐706. doi: 10.1016/j.jtcvs.2006.02.061 [DOI] [PubMed] [Google Scholar]
- 15. Rakovich G, Ferraro P, Therasse E, Duranceau A. Preoperative embolization in the management of a mediastinal paraganglioma. Ann Thorac Surg. 2001;72(2):601‐603. doi: 10.1016/S0003-4975(00)02293-1 [DOI] [PubMed] [Google Scholar]
- 16. Yang Z, Shi Q, Bao F. A case of an unexpected posterior mediastinal functional paraganglioma: case report and literature review. BMC Anesthesiol. 2020;20(1):109. doi: 10.1186/s12871-020-01026-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lin MW, Chang YL, Lee YC, Huang PM. Non‐functional paraganglioma of the posterior mediastinum. Interact Cardiovasc Thorac Surg. 2009;9(3):540‐542. doi: 10.1510/icvts.2009.206169 [DOI] [PubMed] [Google Scholar]
- 18. Shidei H, Maeda H, Isaka T, et al. Mediastinal paraganglioma successfully resected by robot‐assisted thoracoscopic surgery with en bloc chest wall resection: a case report. BMC Surg. 2020;20(1):45. doi: 10.1186/s12893-020-00701-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


