Abstract
Purpose
To determine barriers to implementing an osteoporosis protocol in a community institution following distal radius (DR) fragility fracture to help prevent subsequent fragility fractures.
Methods
This cross-sectional study included elderly patients with DR fractures that occurred between 2016 and 2018. Exclusion criteria were age under 50 years, high-energy mechanism, and inability to follow-up locally. Patients were directed to follow-up with the hospital’s osteoporosis center (OC) or an endocrinologist. Patients were contacted to identify if care was established with the OC and screened for potential barriers in evaluation for bone health. Primary outcomes included the completion of a follow-up visit with an osteoporosis care provider and identification of barriers for patients who did not complete this visit. Secondary outcomes included whether or not patients obtained bone health labs, dual-energy x-ray absorptiometry (DEXA) scans, and/or underwent medical treatment for osteoporosis.
Results
One hundred seventy-five patients met final inclusion criteria and were contacted after discharge. Fifty patients agreed to follow-up with the OC, voicemails were left for 66 patients, only 70 (60.3%) patients actually followed up for bone health analysis. Patients were lost to follow-up due to lack of accessibility (32 patients; death, incorrect phone number, no voicemail, or impaired cognition), and lack of interest (27 patients). Ninety-six (54.9%) patients received appropriate treatment based on bone health labs and/or DEXA scan. Ninety (51.4%) patients had chemical treatment for osteoporosis. Fifty-five patients underwent DEXA scans with equal distribution of patients with normal, osteopenic, and osteoporotic bone. Forty-three (78%) patients who had DEXA scans underwent treatment.
Conclusions
Establishing a protocol for follow-up for bone health assessment following a DR fracture is challenging. Only half of the patients underwent evaluation and management of their bone health. It is imperative to understand the barriers for at-risk patients to provide them with care that will improve their quality of life.
Type of study/level of evidence
Diagnostic III.
Key words: Bone health, Distal radius fracture, Fragility fracture, Osteoporosis, Osteoporosis center
Osteoporosis is the most common metabolic disorder worldwide1 and remains a public health issue that will grow at a rate commensurate with an increasing elderly population. It is estimated that 14 million people are diagnosed with osteoporosis and 47 million with low bone mass.2 The World Health Organization has defined osteoporosis as a bone mineral density of 2.5 standard deviations below the mean in adults aged 20–29 years. It is measured using dual-energy x-ray absorptiometry (DEXA). Osteopenia is defined as a bone mineral density between 1 and 2.5 standard deviations below the mean. A low bone density increases the chance of a fragility fracture caused by a low-energy mechanism. It has been estimated that 35.1 million women and 17.2 million men have either a low bone mass or osteoporosis.3 The morbidity associated with osteoporosis has economic implications resulting in considerable health care resource usage.2 It has been estimated that the yearly cost of osteoporosis in the United States is $19 billion, with the costs expected to increase to $25.3 billion by 2025.4
Osteoporosis is often asymptomatic and frequently manifests as a fracture due to low-energy trauma. Distal radius (DR) fractures are the second most common fracture in the elderly and account for 18% of all fractures in this population.5 One year after experiencing a DR fracture, elderly patients are at a greater risk of vertebral and hip fractures.6 The effects of this disease among the elderly include physical disability, depression, decreased quality of life, and death. Fragility fractures in the elderly necessitate an interdisciplinary approach to ensure adequate follow-up to prevent subsequent fractures. Even with widespread awareness among health care providers, motivating patients to follow-up for bone density assessment or the medical management of any modifiable risk factors that predispose them to further fractures is challenging.
Currently, there are several protocols in the outpatient setting to help treat osteoporosis; however, there exist barriers to patients undergoing proper workup and interventions based on their clinical risk factors.7 Currently, interventions are often initiated by a primary-care physician or endocrinologist. Supplementation with vitamin D and calcium is often initiated if the patient is aged 50 years or older and has experienced an osteoporosis-related fracture. In addition to these supplements, the physician may prescribe medication for bone loss prevention or bone production stimulation. An osteoporosis center (OC), osteoporosis care service, or a fracture liaison service, with a dedicated individual who helps coordinate providing care between a group of specialists, can help improve patient outcomes.8, 9, 10, 11
Our aim was to establish an institutional protocol whereby patients aged 50 years or older presenting with a DR fracture to our hospital can coordinate their follow-up for bone health analysis at an OC. Our endpoint was to identify barriers to patient follow-up with a health care professional by conducting one-on-one phone interviews, in which it was determined whether the patient followed up for bone health analysis. The bone health analysis data from patients who were able to follow-up were also reviewed, with the ultimate future goal of subsequent fracture risk mitigation and any metabolic abnormality correction. It was hypothesized that barriers to patient care include but are not limited to problems of provider-patient information asymmetry, such as limited understanding of osteoporosis as a disease process and clinical resources available to patients for treatment.
Materials and Methods
This cross-sectional study involving all patients aged 50 years or older who presented with a DR fracture due to a low-energy mechanism to the community hospital emergency department was conducted at a single institution during a 27-month period between March 2016 and June 2018. The screening cohort for this study consisted of a total of 211 patients. Patients who were excluded from the study were those who sustained a DR fracture due to a high-energy mechanism (n = 5), were younger than 50 years when the fracture occurred (n = 23), resided out of state, and could not follow-up locally (n = 8).
Eligible patients were initially examined by an on-call orthopedic resident and educated on the importance of follow-up for bone health analysis because of the risk of subsequent fragility fractures. The patients were discharged with detailed instructions on follow-up with the OC to meet an endocrinologist for vitamin D screening and bone health analysis, and they were provided with the contact information of 1 of 3 local fellowship-trained hand surgeons for routine fracture care follow-up (Appendix 1 is available on the Journal’s Web site at www.jhsgo.org). The patients were also contacted by phone by a hand surgery resident and the OC several weeks after their initial visit. The callers used a script to reinforce the importance of follow-up for bone health analysis (Appendix 2 is available on the Journal’s Web site at www.jhsgo.org). The patients were called again by a hospital-provided translator if English was not their preferred language (n = 4). For patients who had dementia or other cognitive issues and lived with family members or other care providers, a discussion on the importance of bone health screening and follow-up occurred with their family or caretakers. If a voicemail was left, if a voicemail was not set up, or if no contact was made, a second attempt was made by the hand surgery resident and a third attempt by the OC 2–4 weeks following the first attempt. If the patient followed up with 1 of the 3 local fellowship-trained hand surgeons, they were also educated on the importance of following up at the OC.
At the end of the 27 months, patient charts were reviewed for demographic data; calcium and vitamin D levels; parathyroid hormone, thyroid-stimulating hormone, and alkaline phosphatase levels; and DEXA scan results. Laboratory values and DEXA scan results from either 2 years prior to the DR fracture or 2 years after were included. Inpatient and outpatient charts were reviewed in order to determine whether the patients had previously received care for their bone health. The laboratory values were compared with normal ranges established by the local hospital laboratory. The primary outcome included chart records of follow-up or lack of follow-up with an osteoporosis care provider and verbalized barriers to follow-up conducted using the one-on-one phone interview with the patients and their family members or caretakers. Secondary outcomes of interest included whether patients obtained bone health laboratory tests, DEXA scans, and/or medical treatment for osteoporosis. Approval for this study was granted by the hospital’s institutional review board.
Statistical analysis included data presented as mean ± standard deviation for continuous variables and proportions for nominal variables. The chi-square and Fisher exact tests were used for nonparametric data and the Student t test for parametric data, with a level of significance of .05 (P value).
Results
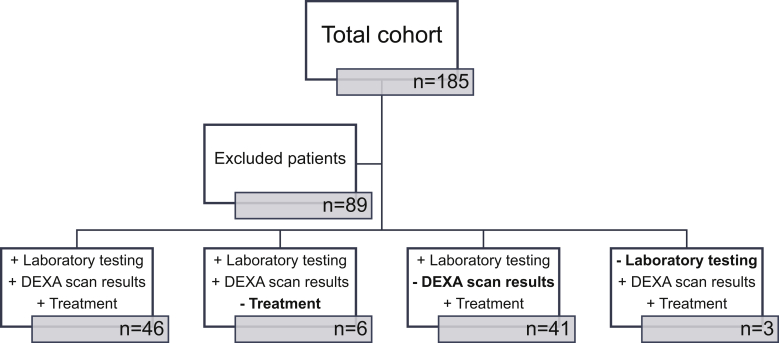
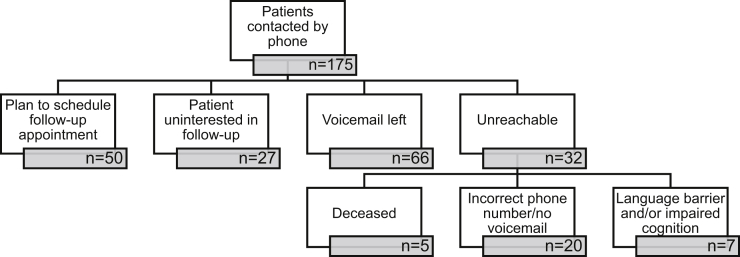
One hundred seventy-five patients were eligible to participate in the study (Fig. 1). The average age of the eligible patients was 71.5 years (range 50–99 years), and 143 (82%) patients were women. All 175 patients were called to reinforce the importance of following up with an OC or a health care professional (Fig. 2). Seventy-seven calls were successfully made to the patients, with 50 patients stating that they would make follow-up appointments with the OC and 27 patients not interested in follow-up. The patient-cited reasons for not pursuing further workup or treatment, as cited on the phone calls, are listed in Table 1. The reasons included not being interested (n = 7), already following up with their own doctor (n = 5), and not wanting any more doctors’ appointments (n = 3). The patients also cited being unable to make follow-up appointments because of living in a nursing home or finances, mobility, time, or transportation issues (n = 8) as reasons for the lack of bone health follow-up. They also stated that they were managing their own supplements (n = 3) or were in denial about their bone health status (n = 1).
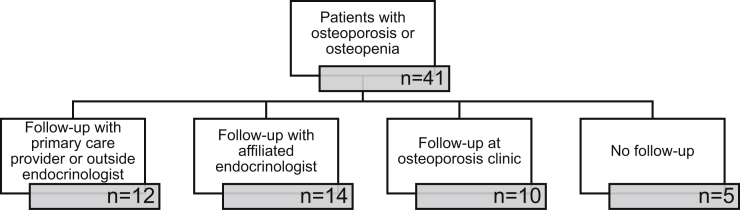
Figure 1.
Study population.
Figure 2.
Phone call results.
Table 1.
Patients’ Reasons for Not Being Interested in Follow-Up
| Not Interested (n) | Reason | |
|---|---|---|
| n = 7 | Not interested | Wanted no further education/discussion |
| n = 5 | Following their own PCP | Did not want more doctors involved |
| n = 4 | Resided in a nursing home | Unsure how to coordinate follow-up |
| n = 3 | Already taking supplements | Did not want any more medications/interventions |
| n = 3 | No more doctors’ appointments | Already burdened with current health care situation |
| n = 1 | No transportation | Unable to make follow-up appointments |
| n = 1 | Financial issues | Cannot afford more medication/appointments |
| n = 1 | Mobility issues | Unable to make follow-up appointments |
| n = 1 | Time issues | Unable to make follow-up appointments |
| n = 1 | Denial | “My bones are already strong” |
PCP, primary-care physician.
Other barriers to follow-up included inability to directly speak to the patients or their family or caregivers, because of which a voicemail was left in 66 cases. Of the 50 patients who stated that they would follow-up and 66 patients for whom a voicemail was left, 70 (60.3%) patients actually followed up for bone health analysis. Of the 32 patients who were unreachable, 5 patients had died, 20 had incorrect phone numbers documented in the chart, and 7 had communication difficulty owing to mental status changes or dementia.
Of the 175 patients meeting the inclusion criteria, 33 (18.9%) did not follow-up, and 46 (26.3%) underwent bloodwork but no imaging or treatment, leaving 96 patients (54.9%) eligible for secondary analysis (Fig. 1). We were unable to obtain information regarding why the patients were lost to follow-up despite indicating interest in scheduling an appointment with the OC. The demographics of the patients in the follow-up group versus those in the no follow-up group are listed in Table 2. The mean age of the follow-up group was 74 years versus 68 years in the no follow-up group. There was also a higher percentage of men in the no follow-up group (29.5%) than in the follow-up group (8.3%). There was no difference in sex with regard to the patients who followed up with the OC and no difference in sex between the treatment or no-treatment groups (P = .13 and P = .21, respectively) (Table 3).
Table 2.
Differences Between Follow-Up and No Follow-Up Populations
| Age (y) | Follow-Up | No Follow-Up | P Value | ||
| Mean | SD | Mean | SD | 2.60 × 10−3 | |
| 74.04 | 11.08 | 68.42 | 13.18 | ||
| Sex (female) | Follow-Up | No Follow-Up | P Value | ||
| Count | % | Count | % | 2.90 × 10−4 | |
| 88 | 91.7 | 55 | 70.5 | ||
Table 3.
Differences Between Patients Who Followed Up With OC Versus Those Who Followed Up With a Primary-Care Physician or Outside Endocrinologist
| Variable | Category | No OC |
OC Patient |
P Value | ||
|---|---|---|---|---|---|---|
| Count | % | Count | % | |||
| Sex | F | 68 | 93.2 | 19 | 82.6 | .13 |
| M | 5 | 6.8 | 4 | 17.4 | ||
| Treatment | Treatment | 67 | 91.8 | 19 | 82.6 | .21 |
| No treatment | 6 | 8.2 | 4 | 17.4 | ||
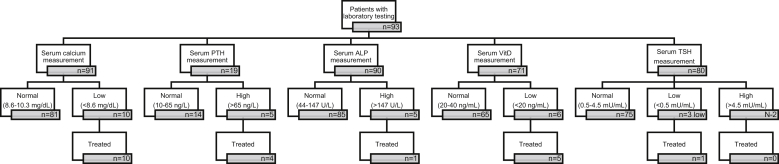
Of the 96 patients (54.9%) who underwent the bone health laboratory tests, DEXA scan, and/or treatment, 23 (24.0%) chose to follow-up either with the OC or endocrinologists affiliated with the OC. The remaining 73 (76.0%) patients followed up with their primary-care physician affiliated with our community hospital. We were unable to determine why the patients chose to follow-up with the OC versus their own primary-care physician. Bone health analysis results via bloodwork were obtained for 93 patients (Fig. 3).
Figure 3.
Laboratory findings.
Ninety (51.4%) patients received documented treatment with medication for their osteoporosis either at the time of enrollment or during the study period. Of the 90 patients who were treated with medication, 77 (85.5%) were on vitamin D and/or calcium supplementation, and the remaining 13 (14.4%) were on a prescribed medication such as bisphosphonate.
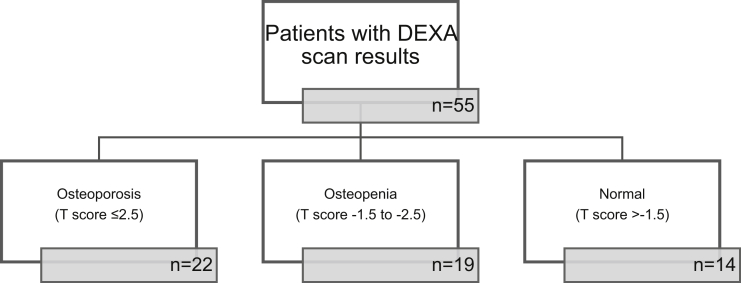
Fifty-five patients underwent DEXA scan, shown in Figure 4. The fractures were equally distributed across normal bone metabolism, osteopenia, and osteoporosis groups (Table 4). Of the 55 patients who underwent DEXA scan, 41 (74.5%) had either osteopenia or osteoporosis. Thirty-six (87.8%) patients received documented treatment, 22 patients were treated with vitamin D and calcium supplementation, 10 were treated with vitamin D and calcium supplementation, and bisphosphonates, and 4 were treated only with bisphosphonates. The follow-up details are shown in Figure 5. Abnormalities in the laboratory values and differences in the treatment between the osteoporosis, osteopenia, and healthy bone metabolism groups did not differ vastly; however, the osteopenia group had a higher percentage of patients with a high alkaline phosphatase level, and the osteoporosis and osteopenia groups were more likely to be treated with bisphosphonate as well as vitamin D and calcium (Tables 5 and 6).
Figure 4.
DEXA scan results.
Table 4.
Fractures Occurring Across Different Bone Densities
| Category | Osteopenia |
Osteoporosis |
Healthy |
P Value | |||
|---|---|---|---|---|---|---|---|
| Count | % | Count | % | Count | % | ||
| Observed | 19 | 34.5 | 22 | 40.0 | 14 | 25.5 | .41 |
| Expectation | 18.33 | 33.3 | 18.33 | 33.3 | 18.33 | 33.3 | |
Figure 5.
Follow-up of patients with abnormal DEXA scan results.
Table 5.
Treatment for Patients With Different DEXA Scan Results
| Treatment | Osteoporosis | Osteopenia | Healthy |
|---|---|---|---|
| No treatment | 3 (13.6%) | 4 (28.6%) | 5 (26.3%) |
| Vitamin D | 7 (31.8%) | 3 (21.4%) | 7 (36.8%) |
| Calcium | 1 (4.5%) | 0 (0.0%) | 2 (10.5%) |
| Vitamin D and calcium | 3 (13.6%) | 5 (35.7%) | 4 (21.1%) |
| Vitamin D and bisphosphonate | 1 (4.5%) | 2 (14.2%) | 0 (0.0%) |
| Vitamin D, bisphosphonate, and calcium | 2 (9.0%) | 0 (0.0%) | 0 (0.0%) |
| Bisphosphonate | 4 (18.2%) | 0 (0.0%) | 0 (0.0%) |
| Denosumab | 1 (4.5%) | 0 (0.0%) | 1 (5.26%) |
| Total | 22 | 14 | 19 |
Table 6.
Laboratory Value Abnormalities Among Different DEXA Results
| Osteoporosis | Osteopenia | Healthy | |
|---|---|---|---|
| Low vitamin D level | 1 (4.5%) | 2 (7.1%) | 0 (0.0%) |
| High TSH level | 1 (4.5%) | 0 (0.0%) | 0 (0.0%) |
| Low TSH level | 0 (0.0%) | 2 (7.1%) | 1 (5.3%) |
| High alkaline phosphatase level | 0 (0.0%) | 4 (28.6%) | 1 (5.3%) |
| High PTH level | 1 (4.5%) | 2 (7.1%) | 1 (5.3%) |
| Low calcium level | 3 (13.6%) | 1 (14.3%) | 2 (10.5%) |
| None | 16 (72.7%) | 3 (21.4%) | 14 (73.7%) |
| Total | 22 | 14 | 19 |
PTH, parathyroid hormone; TSH, thyroid-stimulating hormone.
Discussion
Establishing a protocol to encourage and facilitate patient follow-up with an OC or endocrinologist to evaluate bone health after a fragility fracture has proved to be a challenge despite the increased focus on this condition among providers of orthopedic care and in patient literature. Of the 175 patients who presented to the emergency department with a low-energy DR fracture, only 54.9% underwent a complete bone health evaluation, and only 51.4% of those who followed up with a health care provider were treated with medication.
Compared with the results from other studies conducted at institutions where similar fracture liaison services have been established, our results demonstrate similar rates of follow-up. Eekman et al have reported a compliance of 50.6% among elderly patients with a recent fracture who were asked to follow-up with a fracture liaison service.10 Rozental et al found that in patients aged 50 years or older who experienced a DR fracture, only 8.3% were evaluated for osteoporosis, of which only 27.5% received treatment.12 Similar to other reports, we also demonstrated a disparity in age that was statistically significant between those who followed up and those who did not. Gillespie et al found disparities in osteoporosis screening and found that only 21.2% of women aged 50–64 years underwent analysis, with a subsequent treatment rate of 2%; 26.5% of women aged 65–79 years were evaluated, with a treatment rate of 3.3%; and only 12.8% of women aged 80 years or older were screened, with a treatment rate of 3%.13 Freedman et al also found a low follow-up rate in women above 55 years of age with a DR fracture, with only 2.8% of them undergoing DEXA scans and 22.9% receiving treatment with medication.14 An interesting future area of investigation involves an evaluation of the possible reasons for this disparity in age and sex.
We also found a slight disparity in terms of sex between the follow-up and no follow-up groups, with more men and younger patients in the no follow-up group. Osteoporosis is more common in postmenopausal women, who have a higher fracture risk than men.15 In general, men experience fewer fragility fractures; however, the secondary fracture risk is the same in both sexes, and prevention is equally important for both men and women.11 Cawthon believes this may be due in part to the screening and treatment being less cost-effective for men under the age of 80 years than for women aged 65 years or older. In general, men are less likely to receive treatment after a fracture.15 This may also stem from the fact that general knowledge about osteoporosis in older men is lacking because most studies have included only postmenopausal women. This finding focuses on the parts of the population that still need to be studied.
Despite each patient receiving clear follow-up instructions and additional phone calls, it was still difficult to engage patients in a discussion about the importance of further bone testing. Twenty-seven patients did not want further follow-up, citing concerns about additional appointments and medication. Some patients had financial burdens, whereas others had issues with mobility and transportation. Several patients had been previously screened or had already received treatment from an outside provider. Some patients resided in a nursing home, assisted living facility, or with other family members, which made coordination difficult. Patients with mental status changes and dementia were difficult to educate regarding their risks and the importance of bone health. Even patients who seemed interested in undergoing further evaluation had a low follow-up rate, most likely because of the silent nature of osteoporosis and the impression that fragility fractures are not perceived as life-threatening.7,11
Improvements in the treatment protocol for DR fracture could include providing patients with a patient care navigator to help ensure that the information that the patient receives is in the correct language and/or at the appropriate level of education. Additionally, literature that patients can relate to on a personal level may improve their understanding of the future implications of fragility fractures. Another possible improvement, as has been suggested in prior studies, is to create an open-access fracture registry and database to help monitor and improve the care given to patients with fragility fractures.8 Helping patients overcome social and financial barriers with the addition of social workers and services can also help patients who feel burdened while simultaneously helping patients in this at-risk population prevent future falls with the help of education and exercise programs.
The limitations of this study include its small sample size and a poor follow-up rate of less than 70%. This may be because the community hospital is a level-2 trauma center in a small city setting. Some patients (18.9%) did not undergo local follow-up, and 26.3% of the patients underwent only laboratory tests. Despite attempts to reach out to every patient, only 54.5% of the patients underwent further evaluation and treatment. Furthermore, there were difficulties in obtaining DEXA scan results and laboratory data from some patients because not all local general practitioners and endocrinologists were on the same electronic medical record system used by the main hospital. There were also issues with the timeline of when the patients were prescribed medication, which resulted from the electronic medical record system. Therefore, it is possible that more patients underwent bone health analysis and treatment, but we did not have access to their health records. It is also possible that some patients may have died or were otherwise unreachable, preventing them from being able to follow-up. This may change how our data are interpreted because they might not represent the total population; however, several previous studies have cited similar percentages of follow-up data.10,12, 13, 14 Treatment can also be difficult because of patient noncompliance. It was commonly noted during discussions with the patients that they were not interested in increasing the frequency of their doctors’ appointments or number of prescribed medications.
In conclusion, establishing a protocol for patients to follow-up for bone health assessment following a DR fracture is challenging. Only 54.5% of the patients who sustained a DR fracture were evaluated and managed for their bone health. We found several barriers for patients to follow-up for bone health analysis in the community setting. Some barriers involve the lack of understanding among patients regarding the health impact of fragility fractures. Other barriers are resource-driven, such as access to transportation and worries about finances or living in a nursing home. The other additional barriers are patient perceptions of already feeling burdened with other medical conditions and taking too many medications. It is important to educate elderly patients regarding the importance of detecting metabolic and bone density abnormalities using bloodwork and DEXA scans to characterize and mitigate their risk of future osteoporotic fractures.
Acknowledgments
The authors thank Dr Thomas E. Wasser, PhD, MEd, CIM, for his help with statistical analysis and review and Samantha Quinlan for helping with patient outreach at the osteoporosis center at Stamford Hospital. The authors would also like to thank the Office of Research of Stamford Hospital for their assistance with this research. Additionally, the authors would like to thank Dr Alexander Kossar and Dr Ashlyn Morse for editing the manuscript.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Supplementary Data
References
- 1.US Department of Health and Human Services . US Department of Health and Human Services, Office of the Surgeon General; 2004. Bone Health and Osteoporosis: A Report of the Surgeon General. [Google Scholar]
- 2.National Osteoporosis Foundation . National Osteoporosis Foundation; 2002. America’s Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. [Google Scholar]
- 3.Colón-Emeric C.S., Saag K.G. Osteoporotic fractures in older adults. Best Pract Res Clin Rheumatol. 2006;20(4):695–706. doi: 10.1016/j.berh.2006.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Osteoporosis Foundation Osteoporosis Fast Facts. https://cdn.nof.org/wp-content/uploads/2015/12/Osteoporosis-Fast-Facts.pdf Accessed October 27, 2020.
- 5.Nellans K.W., Kowalski E., Chung K.C. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cuddihy M.T., Gabriel S.E., Crowson C.S., et al. Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int. 1999;9(6):469–475. doi: 10.1007/s001980050172. [DOI] [PubMed] [Google Scholar]
- 7.Vondracek S.F., Minne P., McDermott M.T. Clinical challenges in the management of osteoporosis. Clin Interv Aging. 2008;3(2):315–329. doi: 10.2147/cia.s2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganda K., Puech M., Chen J.S., et al. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int. 2013;24(2):393–406. doi: 10.1007/s00198-012-2090-y. [DOI] [PubMed] [Google Scholar]
- 9.Marsh D., Akesson K., Beaton D.E., et al. Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int. 2011;22(7):2051–2065. doi: 10.1007/s00198-011-1642-x. [DOI] [PubMed] [Google Scholar]
- 10.Eekman D.A., van Helden S.H., Huisman A.M., et al. Optimizing fracture prevention: the fracture liaison service, an observational study. Osteoporos Int. 2014;25(2):701–709. doi: 10.1007/s00198-013-2481-8. [DOI] [PubMed] [Google Scholar]
- 11.Lems W.F., Raterman H.G. Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskel Dis. 2017;9(12):299–316. doi: 10.1177/1759720X17732562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rozental T.D., Makhni E.C., Day C.S., et al. Improving evaluation and treatment for osteoporosis following distal radial fractures: a prospective randomized intervention. J Bone Joint Surg Am. 2008;90(5):953–961. doi: 10.2106/JBJS.G.01121. [DOI] [PubMed] [Google Scholar]
- 13.Gillespie C.W., Morin P.E. Trends and disparities in osteoporosis screening among women in the United States, 2008-2014. Am J Med. 2017;130(3):306–316. doi: 10.1016/j.amjmed.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 14.Freedman K.B., Kaplan F.S., Bilker W.B., et al. Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg Am. 2000;82(8):1063–1070. doi: 10.2106/00004623-200008000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Cawthon P.M. Gender differences in osteoporosis and fractures. Clin Orthop Relat Res. 2011;469(7):1900–1905. doi: 10.1007/s11999-011-1780-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.