ABSTRACT
Background
The coronavirus disease 2019 (COVID-19) pandemic has impacted many aspects of daily life, including dietary intake; however, few studies have reported its impacts on dietary behaviors and food security across multiple countries.
Objectives
We examined self-reported impacts of COVID-19 on food behaviors, food security, and overall diet healthfulness in 5 countries.
Methods
Adults aged 18–100 years (n = 20,554) in Australia, Canada, Mexico, the United Kingdom, and the United States completed an online survey in November and December 2020 as part of the International Food Policy Study, an annual, repeat cross-sectional survey. Survey measures assessed perceived impacts of the COVID-19 pandemic on eating food prepared away from home, having food delivered from a restaurant, and buying groceries online, as well as perceived food security and overall diet healthfulness. Regression models examined associations between each outcome and sociodemographic correlates.
Results
Across all countries, 62% of respondents reported eating less food prepared away from home due to the pandemic, while 11% reported eating more. Some participants reported having less food delivered from a restaurant (35%) and buying fewer groceries online (17%), while other respondents reported more of each (19% and 25%, respectively). An average of 39% reported impacts on their food security, and 27% reported healthful changes to their overall diet. The largest changes for all outcomes were observed in Mexico. Participants who were younger, ethnic minorities, or had lower income adequacy tended to be more likely to report food-related changes in either direction; however, these relationships were often less pronounced among respondents in Mexico.
Conclusions
Respondents reported important changes in how they sourced their food during the pandemic, with trends suggesting shifts towards less food prepared away from home and more healthful diets overall. However, changes in diet and food behaviors occurred in both healthful and less healthful directions, suggesting that dietary responses to the pandemic were highly variable.
Keywords: COVID-19, coronavirus, nutrition, food behaviors, diet, food security, pandemic
Introduction
On 11 March 2020, the WHO declared coronavirus disease 2019 (COVID-19) to be a global pandemic (1). In response, many countries introduced a variety of measures to curb transmission rates and minimize the burden on health-care systems, which fundamentally changed social, work, and daily routines (2).
The nature and severity of COVID-19 public health measures (and the impact of the disease itself) varied across and within countries (2,3). Some of the most common measures implemented included travel bans and border closures, restrictions on social gatherings, temporary closure of schools and nonessential businesses, workplace policies encouraging employees to work from home, and mandatory face coverings in shared public spaces (2,4). Some countries and regions enforced more restrictive measures for select periods of time, such as curfews or stay-at-home orders, while others introduced fewer measures.
COVID-19 lockdowns and restrictions are likely to have impacted a variety of food behaviors, such as eating out compared with preparing meals at home, having food delivered from restaurants, and purchasing groceries from nontraditional sources (e.g., online or from convenience/corner stores) (5). Similarly, COVID-19 infection rates may have impacted food behaviors if individuals opted to avoid public contact out of fear of contracting the virus, regardless of the public health measures in place. Observational evidence to date suggests that self-reported food behaviors shifted in many countries during the COVID-19 pandemic, with most studies reporting increases in more healthful behaviors, such as more frequent cooking, fewer ready-made meals, and fewer fast food or takeout foods (6–15). There is also early evidence that modes and sources of grocery purchasing were impacted by the pandemic. Commercial retail data from many countries have shown that the pandemic accelerated the already growing use of online grocery ordering (16–18); the small number of peer-reviewed, observational studies assessing online grocery ordering during the pandemic suggest similar trends (13,19,20). In addition, stay-at-home orders and hesitancy to visit large or crowded grocery outlets may have increased use of convenience or corner stores as food sources.
Given these potential changes in food behaviors, dietary intake may have shifted for many individuals throughout the COVID-19 pandemic (5). Observational studies conducted thus far suggest that the impacts of COVID-19 were variable, but showed some tendency towards healthful changes (21). For example, 2 cross-sectional studies in the United States found that over half of adults reported dietary changes, with a larger proportion indicating a shift towards a more healthful diet overall, but a substantial proportion indicating less healthful changes (6,7). Similar conclusions were drawn from a web-based cohort of adults in Quebec, Canada, which identified a small increase in diet quality (measured by the Healthy Eating Index 2015) in April and May 2020 relative to before the pandemic (22).
Food security is a key driver of food behaviors and dietary intake, and there is already preliminary evidence suggesting that the COVID-19 pandemic substantially impacted the food security of some populations (23–25). Some evidence suggests that the food security of individuals with lower incomes, those experiencing anxiety or depression, or those who are otherwise socially vulnerable has been disproportionately impacted during the pandemic (23, 25). However, the impact on food security may also have been alleviated in some contexts by pandemic-related financial assistance measures intended to mitigate the economic impact of the pandemic (26). Food security has implications for all food behaviors and overall diet healthfulness, and is important to assess in the context of the financial and social challenges raised by the COVID-19 pandemic.
Although evidence of COVID-19’s impacts on diet-related outcomes is growing, few studies have reported and compared its impacts on food behaviors, food security, or overall diet healthfulness across multiple countries, particularly with sample sizes that allow for international comparisons. Among the small number of studies that provide comparisons across countries, there is evidence that changes in dietary behaviors differed by country, often reflecting the status of the COVID-19 pandemic and/or public health measures at the national level (10,11). For example, online, cross-sectional surveys of adults in Ireland, Great Britain, and the United States found that the European samples reported increases in more healthful food habits during the pandemic, including preparing dinners using fresh ingredients and time spent cooking. These changes, however, were not observed in the United States, where fewer comprehensive COVID-19 restrictions were implemented nationwide (10, 11). Multi-country comparisons are important for assessing how COVID-19 policies and other contextual variables across countries may have differentially impacted food behaviors and dietary intake.
The International Food Policy Study (IFPS) conducts annual, repeat cross-sectional surveys on dietary patterns and policy-relevant behaviors among adults in Australia, Canada, Mexico, the United Kingdom, and the United States. The IFPS provides a unique opportunity to assess self-reported impacts of COVID-19 on dietary behaviors approximately 8 months into the pandemic. Our study aimed to evaluate self-reported impacts of the COVID-19 pandemic on food behaviors, food security, and overall diet healthfulness among adults in 5 countries with varying levels of COVID-19 infection rates and pandemic-related restrictions (see Supplemental Table 1). This study also explored associations between self-reported impacts and correlates of interest, including sociodemographic characteristics and COVID-19 illness status.
Methods
Study design and participants
Data were from the 2020 wave of the IFPS. Data were collected via self-completed, web-based surveys conducted in November and December 2020 with adults aged 18 to 100 years in Australia, Canada, Mexico, the United Kingdom, and the United States. Respondents were recruited through the Nielsen Consumer Insights Global Panel and their partners’ panels. Email invitations with unique survey access links were sent to a random sample of panelists within each country after targeting for demographics; panelists known to be ineligible were not invited. Potential respondents were screened for eligibility and quota requirements based on age and sex. Surveys were conducted in English in Australia and the United Kingdom; Spanish in Mexico; English or French in Canada; and English or Spanish in the United States. Members of the research team who were native in each language reviewed the French and Spanish translations independently. The median survey time was 44 minutes.
Respondents provided consent prior to survey completion. Respondents received remuneration in accordance with their panel's usual incentive structure (e.g., points-based or monetary rewards, chances to win prizes). The study was reviewed by and received ethics clearance through a University of Waterloo Research Ethics Board (ORE# 30,829). A full description of the study methods can be found in the International Food Policy Study: Technical Report – 2020 Survey (Wave 4) (27).
Survey measures
Self-report survey measures examined perceived impacts of COVID-19 on food purchasing and consumption behaviors, food security, and changes in overall diet healthfulness. Measures using 5-point Likert scales were used to assess participants’ perceived impacts of the COVID-19 pandemic on their frequency of eating food prepared away from home, having food delivered from a restaurant, buying groceries online, and buying groceries from convenience/corner stores. Response options included “I [eat/have/buy] a lot less …,” “I [eat/have/buy] a little less …,” “no difference,” “I [eat/have/buy] a little more …,” and “I [eat/have/buy] a lot more …,” with additional wording corresponding to each food behavior. Perceived COVID-19-related impacts on food security were assessed using the question “has the COVID-19 pandemic affected whether your household has had enough food to eat?,” with response options not at all, a little, and a lot. The reported healthfulness of participants’ overall diets compared to before the COVID-19 pandemic was assessed using a 5-point Likert-scale measure (“a lot less healthy” to “a lot more healthy”).
It was hypothesized that being infected with and experiencing symptoms of COVID-19 may have an impact on individuals’ food behaviors and overall diet; therefore, COVID-19 illness status was assessed by asking “have you had COVID-19?,” with response options “no,” “yes–confirmed by test,” “I believe I had COVID-19, but was not tested,” and “don't know.”
Participant age, sex, ethnicity, education level, BMI, and perceived income adequacy were collected using measures drawn from population-level surveys within each country (28–33). BMI levels were calculated and categorized into underweight, normal weight, overweight, and obesity using the WHO thresholds (34). Ethnicity measures were recoded as minority or majority and education measures as low, medium, or high, to allow for comparisons across countries.
“Don't know” and “refuse to answer” were available as response options for all survey questions. The full survey measures are available on the IFPS project website (27).
Data analysis
A total of 30,131 adults completed the survey. Respondents were excluded for the following reasons: region was missing, ineligible, or had an inadequate sample size (i.e., Canadian territories); invalid response to a data quality question; survey completion time under 15 minutes; and/or invalid responses to at least 3 of 21 open-ended measures (n = 8378). For the analysis in this paper, a further 1199 participants were excluded for missing data (“refuse to answer” for all COVID-19-related variables and/or “refuse to answer” or “don't know” for all sociodemographic characteristic variables).
Data were weighted with poststratification sample weights constructed using a raking algorithm, with population estimates from the census in each country based on age group, sex, region, ethnicity (except in Canada), and education (except in Mexico). Estimates reported are weighted unless otherwise specified. Analyses were conducted using SAS statistical software (SAS Institute Inc.).
Descriptive statistics examined the weighted percentages of participants, stratified by country, who reported changes in the frequency of eating food prepared away from home, having food delivered from a restaurant, buying groceries online, buying groceries from a convenience/corner store, perceived food security, and overall healthfulness of their diet compared to before the COVID-19 pandemic.
Multinomial logistic regression models were used to evaluate between-country differences and potential associations between the dependent variables and covariates of interest. All regression models incorporated poststratification sample weights and included the following covariates: country, age, sex, ethnicity, education level, BMI, income adequacy, COVID-19 illness status, and perceived COVID-19 impacts on food security (except for the models assessing food security as the dependent variable). To assess potential country differences in the relationship between the dependent variables and covariates of interest, additional models with country × covariate interactions were run. A significance level of P < 0.01 was used to account for multiple comparisons.
Results
A total of 20,554 respondents were included in the final analytic sample (Australia, n = 4115; Canada, n = 4067; Mexico, n = 3961; United Kingdom, n = 4058; United States, n = 4354). Table 1 presents the characteristics of the weighted sample, by country. Distributions of age, sex, ethnicity (except in Canada), and education groups (except in Mexico) correspond to the poststratification sample weights applied to each country. Across the entire sample, 29% were classified as having overweight and 21% as having obesity. The majority of respondents reported high perceived income adequacy. Overall, 3.4% reported that they had contracted COVID-19 (confirmed by a test); an additional 5.4% believed they had COVID-19, but were not tested.
Table 1.
Weighted characteristics of respondents in the International Food Policy Study 20201
| Characteristic | Total sample N = 20,554 | Australia n = 4115 | Canada n = 4067 | Mexico n = 3961 | United Kingdom n = 4058 | United States n = 4354 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | (n) | % | (n) | % | (n) | % | (n) | % | (n) | % | (n) | |
| Age | ||||||||||||
| 18–29 years | 20.9 | (4287) | 20.5 | (842) | 18.5 | (753) | 27.4 | (1085) | 18.3 | (742) | 19.9 | (865) |
| 30–44 years | 26.2 | (5387) | 26.8 | (1102) | 24.9 | (1013) | 30.7 | (1217) | 24.2 | (981) | 24.7 | (1075) |
| 45–59 years | 26.1 | (5361) | 24.2 | (996) | 24.9 | (1013) | 30.5 | (1210) | 25.9 | (1049) | 25.1 | (1093) |
| ≥60 years | 26.9 | (5520) | 28.6 | (1175) | 31.7 | (1289) | 11.3 | (449) | 31.7 | (1286) | 30.3 | (1321) |
| Sex | ||||||||||||
| Male | 48.9 | (10,056) | 49.1 | (2021) | 49.6 | (2015) | 48.5 | (1919) | 48.8 | (1980) | 48.7 | (2120) |
| Female | 51.1 | (10,498) | 50.9 | (2093) | 50.4 | (2052) | 51.5 | (2041) | 51.2 | (2078) | 51.3 | (2234) |
| Ethnicity2 | ||||||||||||
| Majority group | 77.2 | (15,863) | 74.0 | (3045) | 78.7 | (3199) | 81.1 | (3212) | 89.2 | (3620) | 64.0 | (2787) |
| Minority group | 22.8 | (4691) | 26.0 | (1069) | 21.3 | (868) | 18.9 | (749) | 10.8 | (438) | 36.0 | (1567) |
| Education level3 | ||||||||||||
| Low | 42.7 | (8786) | 41.8 | (1721) | 41.7 | (1696) | 22.5 | (890) | 52.0 | (2111) | 54.4 | (2369) |
| Medium | 21.8 | (4487) | 32.3 | (1331) | 33.7 | (1370) | 13.5 | (534) | 19.7 | (799) | 10.4 | (453) |
| High | 35.4 | (7281) | 25.8 | (1063) | 24.6 | (1001) | 64.0 | (2537) | 28.3 | (1148) | 35.2 | (1532) |
| BMI | ||||||||||||
| Underweight (<18.5 kg/m2) | 2.6 | (540) | 3.5 | (145) | 3.1 | (125) | 1.5 | (58) | 2.9 | (117) | 2.2 | (95) |
| Normal weight (18.5–24.9 kg/m2) | 35.2 | (7226) | 33.3 | (1371) | 35.3 | (1436) | 37.7 | (1492) | 35.8 | (1451) | 33.9 | (1477) |
| Overweight (25.0–29.9 kg/m2) | 28.7 | (5903) | 27.7 | (1140) | 27.2 | (1106) | 32.4 | (1283) | 27.1 | (1099) | 29.3 | (1275) |
| Obesity (≥30 kg/m2) | 21.0 | (4325) | 22.8 | (938) | 22.8 | (926) | 15.6 | (618) | 18.1 | (733) | 25.5 | (1110) |
| Missing | 12.4 | (2559) | 12.7 | (521) | 11.6 | (473) | 12.9 | (510) | 16.2 | (658) | 9.1 | (397) |
| Income adequacy4 | ||||||||||||
| Low | 29.3 | (6031) | 20.7 | (850) | 24.7 | (1005) | 50.6 | (2003) | 20.3 | (823) | 31.0 | (1351) |
| High | 70.7 | (14,523) | 79.3 | (3264) | 75.3 | (3062) | 49.4 | (1958) | 79.7 | (3235) | 69.0 | (3003) |
| COVID-19 illness status | ||||||||||||
| No/don't know | 91.3 | (18,758) | 96.3 | (3962) | 95.4 | (3879) | 86.7 | (3435) | 89.3 | (3623) | 88.6 | (3859) |
| Yes–confirmed by test | 3.4 | (690) | 1.8 | (74) | 1.3 | (53) | 5.2 | (204) | 3.6 | (145) | 4.9 | (213) |
| I believe I had COVID-19, but was not tested | 5.4 | (1106) | 1.9 | (79) | 3.3 | (136) | 8.1 | (321) | 7.1 | (290) | 6.5 | (281) |
Abbreviations: COVID-19, coronavirus disease 2019.
Ethnicity categories as per census questions asked in each country: 1) in Australia, majority indicates the participant only speaks English at home and minority indicates the participant speaks a language besides English at home; 2) in Canada, the United Kingdom, and the United States, majority indicates the participant is White race and minority indicates the participant is of other ethnicity; and 3) in Mexico, majority indicates the participant is nonindigenous and minority indicates they are indigenous.
Participants were asked, “what is the highest level of formal education that you have completed?” Responses were categorized as low (completed secondary school or less), medium (some postsecondary qualifications), or high (university degree or higher) according to country-specific criteria.
Participants were asked, “thinking about your total monthly income, how difficult or easy is it for you to make ends meet?” Response options were very easy, easy, and neither easy nor difficult, which were all categorized as high income adequacy, and difficult and very difficult, which were categorized as low income adequacy.
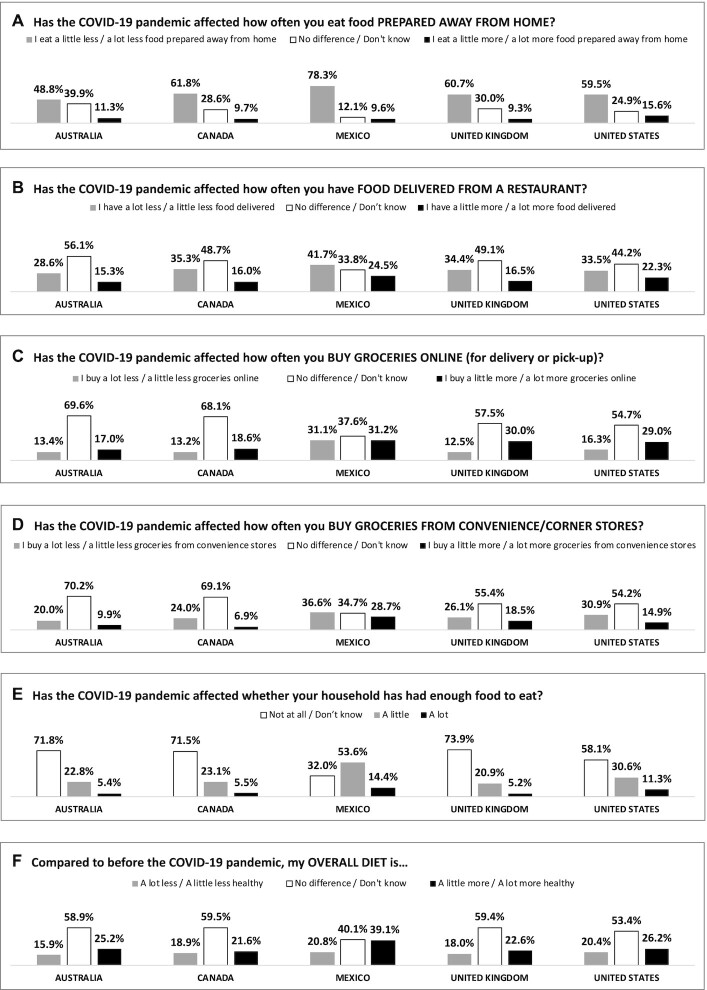
Self-reported impacts of COVID-19 on food behaviors and overall diet
Figure 1 shows the proportions of respondents who indicated the COVID-19 pandemic impacted their food behaviors, food security, and overall diet. Out of the 6 measures, eating food prepared away from home was reported to have changed the most: across all countries, the greatest proportion of participants reported that they ate a little less or a lot less food prepared away from home, ranging from about half of respondents in Australia to over three-quarters in Mexico (Figure 1A). In contrast, only 9%–16% of respondents reported eating more food prepared away from home. For the remaining measures, the majority of respondents in most countries indicated no changes. When asked about having food delivered from a restaurant, 29%–42% of respondents reported less deliveries, and 15%–25% reported more (Figure 1B). Across all countries, 17%–31% of respondents reported that the pandemic led them to purchase more groceries online, while 13%–31% bought fewer groceries online (Figure 1C). In terms of purchasing groceries from convenience/corner stores, 20%–37% of respondents reported buying less and 7%–29% reported buying more (Figure 1D).
Figure 1.
Weighted, unadjusted percentages of participants’ reported impacts of the COVID-19 pandemic on (A) eating food prepared away from home, (B) having food delivered from a restaurant, (C) buying groceries online, (D) buying groceries from convenience/corner stores, (E) food security, and (F) overall diet healthfulness in November to December 2020, from the International Food Policy Study (N = 20,554). Abbreviations: COVID-19, coronavirus disease 2019.
Approximately one-quarter of respondents in Australia, Canada, and the United Kingdom reported that the pandemic affected their food security a little or a lot, with higher proportions in the United States (approximately 40%) and Mexico (nearly 70%; Figure 1E).
Most respondents reported no difference in their overall diet compared to before the pandemic. Among those who did report a difference, a greater proportion indicated that their diet was more healthy compared to less healthy (Figure 1F).
Weighted proportions across all response options for each of the 6 measures are available in Supplemental Table 2.
Between-country differences
Results from regression models (Table 2; Supplemental Table 3) and patterns in Figure 1 demonstrate several differences across countries. Australian respondents were significantly less likely than respondents in the other countries to report changes in eating food prepared away from home (in either direction) and buying groceries less often from convenience stores (compared with no difference). Respondents from Mexico tended to be more likely to report changes in food behaviors than respondents in the other countries, but were significantly more likely to report that the pandemic affected their food security (i.e., having enough food to eat) a little or a lot. Similarly, US respondents were more likely than respondents in Australia, Canada, and the United Kingdom to report COVID-19-related impacts on their food security. Mexican respondents were more likely than those in all other countries to report that their overall diet was more healthy compared to before COVID-19. Participants’ reported changes in having food delivered from a restaurant showed the fewest differences between countries across all 6 outcomes.
Table 2.
Results from multinomial logistic regression models assessing self-reported impacts of the COVID-19 pandemic on food behaviors, food security, and overall diet healthfulness among respondents of the International Food Policy Study (N = 20,554)1
| Has the COVID-19 pandemic affected how often you eat food prepared away from home? | Has the COVID-19 pandemic affected how often you have food delivered from a restaurant? | Has the COVID-19 pandemic affected how often you buy groceries online (for delivery or pick-up)? | Has the COVID-19 pandemic affected how often you buy groceries from convenience/corner stores? | Has the COVID-19 pandemic affected whether your household has had enough food to eat? | Compared to before the COVID-19 pandemic, my overall diet is … | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I eat a lot less/a little less2 | I eat a little more/a lot more2 | I have a lot less/a little less2 | I have a little more/a lot more2 | I buy a lot less/a little less2 | I buy a little more/a lot more2 | I buy a lot less/a little less2 | I buy a little more/a lot more2 | A little3 | A lot3 | A lot less healthy/A little less healthy4 | A little more healthy/A lot more healthy4 | |
| AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | AOR(99% CI) | |
| Country5 | ||||||||||||
| Australia | 0.28 (0.24–0.34)6 | 0.64 (0.49–0.84)6 | 0.64 (0.54–0.76)6 | 0.62 (0.51–0.76)6 | 0.35 (0.29–0.43)6 | 0.44 (0.36–0.52)6 | 0.41 (0.34–0.49)6 | 0.28 (0.22–0.34)6 | 0.27 (0.23–0.32)6 | 0.25 (0.19–0.33)* | 1.03 (0.84–1.26) | 0.64 (0.54–0.76)6 |
| Canada | 0.51 (0.42–0.63)6 | 0.85 (0.63–1.13) | 0.94 (0.79–1.12) | 0.84 (0.68–1.04) | 0.37 (0.30–0.46)6 | 0.51 (0.42–0.61)6 | 0.51 (0.42–0.61)6 | 0.21 (0.17–0.27)6 | 0.27 (0.22–0.32)6 | 0.24 (0.18–0.33)6 | 1.20 (0.98–1.47) | 0.56 (0.47–0.67)6 |
| Mexico | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| United Kingdom | 0.52 (0.43–0.63)6 | 0.83 (0.63–1.09) | 0.96 (0.81–1.14) | 0.89 (0.73–1.09) | 0.45 (0.36–0.55)6 | 1.03 (0.87–1.21) | 0.78 (0.65–0.93)6 | 0.82 (0.68–1.00) | 0.25 (0.21–0.29)6 | 0.23 (0.18–0.31)6 | 1.24 (1.02–1.52)6 | 0.62 (0.52–0.73)6 |
| United States | 0.49 (0.40–0.59)6 | 1.28 (0.98–1.67) | 0.81 (0.69–0.97)6 | 1.10 (0.91–1.35) | 0.43 (0.35–0.52)6 | 0.90 (0.76–1.06) | 0.70 (0.59–0.83)6 | 0.46 (0.38–0.57)6 | 0.41 (0.35–0.49)6 | 0.59 (0.46–0.76)6 | 1.14 (0.94–1.39) | 0.65 (0.55–0.77)6 |
| Age | ||||||||||||
| 18–29 years | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| 30–44 years | 0.86 (0.73–1.01) | 0.60 (0.49–0.74)6 | 0.98 (0.85–1.13) | 0.71 (0.60–0.83)6 | 0.96 (0.81–1.14) | 1.12 (0.97–1.29) | 1.05 (0.90–1.21) | 0.84 (0.71–0.99)6 | 0.78 (0.67–0.90)6 | 0.99 (0.79–1.24) | 0.81 (0.69–0.95)6 | 0.89 (0.77–1.03) |
| 45–59 years | 0.85 (0.72–1.00)6 | 0.33 (0.26–0.42)6 | 0.86 (0.74–0.99)6 | 0.37 (0.31–0.44)6 | 0.83 (0.69–0.99)6 | 0.71 (0.61–0.83)6 | 0.88 (0.75–1.02) | 0.55 (0.46–0.66)6 | 0.45 (0.38–0.52)6 | 0.50 (0.39–0.64)6 | 0.62 (0.52–0.73)6 | 0.80 (0.69–0.93)6 |
| ≥60 years | 0.91 (0.78–1.08) | 0.25 (0.19–0.32)6 | 0.71 (0.61–0.83)6 | 0.21 (0.17–0.26)6 | 0.82 (0.67–1.00) | 0.66 (0.56–0.77)6 | 0.86 (0.73–1.01) | 0.40 (0.32–0.50)6 | 0.22 (0.19–0.26)6 | 0.20 (0.14–0.28)6 | 0.46 (0.38–0.55)6 | 0.70 (0.59–0.82)6 |
| Sex | ||||||||||||
| Female | 1.32 (1.19–1.45)6 | 1.03 (0.88–1.20) | 1.14 (1.03–1.25)6 | 0.98 (0.87–1.11) | 0.97 (0.86–1.10) | 1.25 (1.13–1.38)6 | 1.04 (0.94–1.15) | 1.01 (0.89–1.15) | 0.95 (0.85–1.06) | 0.91 (0.76–1.08) | 1.54 (1.37–1.73)6 | 1.20 (1.09–1.33)6 |
| Male | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| Ethnicity7 | ||||||||||||
| Majority group | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| Minority group | 1.38 (1.19–1.59)6 | 1.36 (1.13–1.65)6 | 1.39 (1.22–1.58)6 | 1.29 (1.10–1.50)6 | 1.65 (1.41–1.92)6 | 1.08 (0.94–1.23) | 1.45 (1.27–1.65)6 | 1.59 (1.35–1.87)6 | 1.58 (1.38–1.80)6 | 1.68 (1.36–2.07)6 | 1.04 (0.89–1.21) | 1.27 (1.12–1.45)6 |
| Education level8 | ||||||||||||
| Low | 0.56 (0.50–0.63)6 | 0.50 (0.42–0.60)6 | 0.79 (0.71–0.89)6 | 0.55 (0.48–0.64)6 | 0.94 (0.81–1.09) | 0.55 (0.49–0.62)6 | 0.76 (0.67–0.86)6 | 0.67 (0.58–0.78)6 | 1.02 (0.90–1.16) | 1.12 (0.91–1.38) | 0.75 (0.65–0.86)6 | 0.55 (0.48–0.62)6 |
| Medium | 0.74 (0.66–0.85)6 | 0.69 (0.57–0.84)6 | 0.87 (0.77–0.99)6 | 0.70 (0.60–0.81)6 | 0.88 (0.74–1.04) | 0.73 (0.64–0.83)6 | 0.87 (0.77–1.00)6 | 0.75 (0.64–0.89)6 | 1.03 (0.90–1.19) | 1.28 (1.02–1.60)6 | 0.90 (0.78–1.05) | 0.73 (0.64–0.83)6 |
| High | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| BMI | ||||||||||||
| Underweight (<18.5 kg/m2) | 0.85 (0.62–1.18) | 0.70 (0.44–1.11) | 0.90 (0.66–1.22) | 1.00 (0.72–1.41) | 1.31 (0.92–1.86) | 1.06 (0.78–1.45) | 1.08 (0.79–1.48) | 1.36 (0.95–1.96) | 1.05 (0.77–1.45) | 1.59 (0.98–2.57)6 | 1.15 (0.82–1.61) | 0.82 (0.59–1.13) |
| Normal weight (18.5–24.9 kg/m2) | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| Overweight (25.0–29.9 kg/m2) | 1.04 (0.92–1.18) | 1.17 (0.97–1.42) | 1.07 (0.95–1.21) | 1.04 (0.90–1.21) | 1.02 (0.87–1.19) | 0.93 (0.82–1.06) | 0.97 (0.85–1.10) | 0.98 (0.83–1.14) | 0.86 (0.75–0.98)6 | 0.79 (0.63–1.00) | 1.50 (1.29–1.75)6 | 1.10 (0.97–1.25) |
| Obesity (≥30 kg/m2) | 1.04 (0.91–1.20) | 1.286 (1.03–1.58) | 1.08 (0.95–1.24) | 1.08 (0.92–1.28) | 1.03 (0.86–1.23) | 0.95 (0.82–1.10) | 1.07 (0.93–1.24) | 1.03 (0.86–1.24) | 0.88 (0.76–1.03) | 0.78 (0.61–1.00)6 | 2.01 (1.71–2.37)6 | 1.15 (1.00–1.33) |
| Missing | 0.70 (0.59–0.82)6 | 0.80 (0.63–1.03) | 0.93 (0.79–1.10) | 0.79 (0.65–0.96)6 | 1.06 (0.87–1.29) | 0.77 (0.65–0.92)6 | 0.90 (0.76–1.07) | 0.85 (0.69–1.05) | 1.25 (1.05–1.49)6 | 1.59 (1.22–2.06)6 | 1.06 (0.87–1.29) | 0.74 (0.62–0.88)6 |
| Income adequacy9 | ||||||||||||
| High | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| Low | 1.16 (1.02–1.32)6 | 0.92 (0.76–1.12) | 1.16 (1.03–1.31)6 | 0.96 (0.83–1.11) | 1.10 (0.95–1.27) | 0.81 (0.71–0.92)6 | 1.15 (1.01–1.30)6 | 0.97 (0.83–1.13) | 4.63 (4.09–5.23)6 | 8.75 (7.31–10.49)6 | 2.08 (1.82–2.37)6 | 0.95 (0.83–1.08) |
| COVID-19 illness status | ||||||||||||
| No | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] |
| Yes–confirmed by test | 1.58 (1.11–2.24)6 | 1.71 (1.12–2.62)6 | 1.71 (1.28–2.27)6 | 1.64 (1.19–2.25)6 | 2.65 (1.96–3.58)6 | 1.59 (1.20–2.11)6 | 2.05 (1.55–2.71)6 | 1.83 (1.34–2.49)6 | 1.91 (1.42–2.58)6 | 2.91 (1.93–4.38)6 | 1.83 (1.32–2.53)6 | 1.94 (1.47–2.56)6 |
| I believe I had COVID-19, but was not tested | 1.10 (0.86–1.42) | 1.19 (0.85–1.65) | 1.20 (0.97–1.49) | 1.29 (1.00–1.67) | 1.20 (0.92–1.56) | 1.13 (0.91–1.41) | 1.17 (0.94–1.46) | 1.36 (1.05–1.76)6 | 2.07 (1.67–2.58)6 | 2.48 (1.79–3.43)6 | 1.20 (0.93–1.56) | 1.23 (0.99–1.54) |
| COVID-19 impacts on food security | ||||||||||||
| A little | 1.80 (1.57–2.06)6 | 2.37 (1.96–2.87)6 | 1.96 (1.74–2.22)6 | 1.80 (1.56–2.08)6 | 2.69 (2.32–3.12)6 | 1.82 (1.61–2.07)6 | 2.38 (2.10–2.69)6 | 2.92 (2.50–3.41)6 | — | — | 2.00 (1.73–2.30)6 | 1.44 (1.27–1.63)6 |
| A lot | 1.78 (1.40–2.27)6 | 2.91 (2.16–3.92)6 | 2.50 (2.03–3.07)6 | 2.34 (1.85–2.96)6 | 3.68 (2.92–4.63)6 | 2.70 (2.20–3.32)6 | 3.09 (2.51–3.81)6 | 4.69 (3.71–5.93)6 | — | — | 3.48 (2.81–4.33)6 | 2.45 (1.98–3.04)6 |
| Not at all/don't know | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | [ref] | — | — | [ref] | [ref] |
Abbreviations: AOR, adjusted odds ratio; COVID-19, coronavirus disease 2019.
Participants reporting that they [eat/have/buy] “a lot less/a little less” or “a little more/a lot more” compared with “no difference/don't know.”
Participants reporting that the COVID-19 pandemic affected whether their household had enough food to eat by “a little” or “a lot” compared with “not at all/don't know.”
Participants reporting that their overall diet is “a lot less healthy/a little less healthy” or “a little more healthy/a lot more healthy” compared to before the COVID-19 pandemic, compared with “no difference/don't know.”
Full cross-country comparisons are provided in Supplemental Table 3.
P < 0.01.
Ethnicity categories as per census questions asked in each country: 1) in Australia, majority indicates the participant only speaks English at home and minority indicates the participant speaks a language besides English at home; 2) in Canada, the United Kingdom, and the United States, majority indicates the participant is White race and minority indicates the participant is of other ethnicity; and 3) in Mexico, majority indicates the participant is nonindigenous and minority indicates they are indigenous.
Participants were asked, “what is the highest level of formal education that you have completed?” Responses were categorized as low (completed secondary school or less), medium (some postsecondary qualifications), or high (university degree or higher) according to country-specific criteria.
Participants were asked, “thinking about your total monthly income, how difficult or easy is it for you to make ends meet?” Response options were very easy, easy, and neither easy nor difficult, which were all categorized as high income adequacy, and difficult and very difficult, which were categorized as low income adequacy.
Sociodemographic characteristics and self-reported impacts of COVID-19
Self-reported impacts of the pandemic also differed across sociodemographic characteristics. As Table 2 indicates, respondents who reported that they had a confirmed case of COVID-19 were more likely to report changes in all of the food behaviors and overall diet healthfulness, in either direction. Both respondents with confirmed and unconfirmed COVID-19 were more likely to report that COVID-19 had an impact on their food security.
Across the demographic variables, older participants tended to be less likely to report changes in food behaviors, overall diet healthfulness, and food security compared to participants aged 18 to 29 years. Female respondents were more likely than males to report eating less food prepared away from home, having less food delivered from a restaurant, buying more groceries online, and changes to the overall healthfulness of their diet (in either direction).
Respondents who reported that COVID-19 impacted their food security a little or a lot were more likely to report changes in all of the food behaviors and overall diet healthfulness, in either direction (i.e., more or less). Respondents with low income adequacy were more likely to report eating less food away from home, having less food delivered from a restaurant, buying fewer groceries from convenience stores, and having a less healthy diet compared to before the COVID-19 pandemic. They were also less likely to report buying more groceries online, and more likely to report that the pandemic had impacted their food security.
Respondents of a minority ethnicity were more likely than those from a majority ethnicity to report changes in either direction for eating food prepared away from home, having food delivered from a restaurant, buying groceries from convenience/corner stores, and buying fewer groceries online. Ethnic minority respondents were also more likely to report that COVID-19 impacted their food security a little and a lot, and were more likely to report that their diet was more healthful than before the pandemic.
Respondents with low and medium education levels tended to be less likely to report changes in food behaviors or overall diet healthfulness (in either direction). No association was observed between education level and perceived food security.
Respondents with BMIs corresponding to obesity were more likely to report eating more food prepared away from home and that their diet was less healthy than before the pandemic and less likely to report buying more groceries online compared to respondents with BMIs corresponding to normal weight. Respondents with BMIs corresponding to overweight and obesity were less likely than those with normal weight to report that the pandemic impacted their food security a little or a lot, respectively.
Between-country differences in sociodemographic effects
Statistically significant interactions between country and the covariates of interest were observed for eating food prepared away from home (country × age, country × ethnicity), having food delivered from a restaurant (country × age, country × sex, country × ethnicity, country × food security), buying groceries online (country × ethnicity, country × education, country × income adequacy, country × COVID-19 illness status), buying groceries from convenience stores (country × age, country × sex, country × COVID-19 illness status, country × food security), food security (country × age, country × education, country × income adequacy, country × COVID-19 illness status), and overall diet healthfulness (country × age, country × food security). Some notable interaction results are highlighted in the following paragraphs. Illustrations of all significant interactions are provided in Supplemental Figure 1.
Many of the significant interactions were a result of differences in the magnitude, rather than direction, of covariate-outcome relationships across countries. For example, a significant interaction between country × age for eating food prepared away from home indicated that the inverse relationship between age and eating more food prepared away from home during the pandemic was weaker in Mexico than it was in the other countries. Similarly, the relationship between income adequacy and reporting that COVID-19 impacted food security a little was present in all countries, but less pronounced among Mexican respondents.
In comparison, some interactions revealed contrasting results across countries. For example, in the United States, female respondents were less likely than males to report having more food delivered from a restaurant during the COVID-19 pandemic, while minimal differences by sex were observed in the other countries. Mexican respondents who reported that the pandemic impacted their food security a lot were less likely than those who reported no impacts to have more food delivered during the pandemic, while the opposite was observed in the other countries. Further, in Mexico, respondents with high income adequacy were more likely to buy more groceries online than before the pandemic, but there were minimal differences by income adequacy in the other countries.
Discussion
Our findings indicate that approximately 8 months into the pandemic, many respondents reported changes in food consumption and purchasing behaviors, overall diet, and food security; however, the impact was highly variable, sometimes with inverse relationships across countries and demographic groups.
The largest impacts observed were for reductions in eating food prepared away from home. These results reflect those reported in other early COVID-19 studies from Canada, the United States, and the United Kingdom, which have found that individuals reported more time spent cooking, making more meals from scratch, and eating fewer ready-made or takeout meals (8,10,11, 14,15). Similar trends were observed across all countries, but differences in magnitude were apparent: over three-quarters of Mexican respondents reported eating less food prepared away from home, compared to less than half of respondents in Australia. It is difficult to identify the source of these cross-country differences; however, cultural differences may have played a role. In Mexico, it was very common to go out for lunch at restaurants or fondas prior to the pandemic (as opposed to bringing a lunch from home, as is more common in the United States and Canada). Therefore, as more employees began to work from home, a major source of food prepared away from home disappeared. It also may be that in Australia, where COVID-19 lockdowns were more localized, impacts on food behaviors were less pronounced over the broader population compared to other countries. Although the Australian state of Victoria had just emerged from a strict lockdown period prior to our data collection, the remainder of Australia had been predominantly living as usual, with very few COVID-19 cases and minimal to no restrictions (35). Overall, the reported reductions in eating food prepared away from home may be a positive outcome of the increased time spent at home during the pandemic, as greater consumption of meals prepared outside the home has been associated with poorer diet quality and weight gain (36). Whether these reductions in eating out are offset by increases in other less healthful food behaviors remains to be seen, as does the extent to which these changes will persist in the long run.
A smaller but still meaningful proportion of respondents reported changes in their frequency of having food delivered from a restaurant, buying groceries online, and buying groceries from a convenience store. More than one-third of respondents in Canada, Mexico, the United Kingdom, and the United States had less food delivered from a restaurant, and close to that many reported buying more groceries online in Mexico, the United Kingdom, and the United States. Over a quarter of all Mexican, UK, and US respondents bought fewer groceries from convenience stores. However, despite these general trends, a notable proportion of respondents also reported changes in the opposite direction, suggesting differential impacts of COVID-19 on individuals. Changes in food delivery and grocery behaviors were again largest in Mexico, which may be partly explained by the COVID-19 restrictions in place at the time of data collection: nationwide school closures were in place in Mexico (as opposed to more varied regional restrictions in other countries), which would have had far-reaching implications on employment and the day-to-day schedules of households with children (37). Another explanation may be the lower income levels of the Mexican population overall, and therefore the larger proportion of individuals vulnerable to the financial and social shifts of the pandemic. Alternatively, the disproportionate percentage of highly educated individuals in our Mexican sample may have played a role, given that higher income groups in Mexico are more likely than lower income groups to use online grocery ordering (38).
There is limited comparable evidence thus far on restaurant food delivery and grocery sources during the pandemic in the regions analyzed in this study; however, 1 study of adults in European countries, including the United Kingdom, reported increases in online grocery shopping during the pandemic, similar to the results observed in this study (13). Similarly, results from a study assessing sales at a Dutch online supermarket found that online grocery sales increased substantially overall at the onset of COVID-19, and fluctuated throughout the pandemic in tandem with local hospital admission rates (20). Sales data reported by industry sources also suggest that the growth of both restaurant food delivery and online grocery ordering accelerated substantially during the pandemic (16–18,39–42). If use of these online food sources continues to grow after the pandemic, it will be important to monitor whether and how restaurants and retailers incorporate novel marketing strategies into the online shopping experience, and whether the healthfulness of online grocery and meal purchases differ from those of traditional in-store purchases.
In line with some estimates, over a quarter of respondents in all countries experienced at least some impacts on their household's food security as a result of the pandemic. The proportion of respondents affected by the pandemic was highest in Mexico, where the COVID-19 pandemic was associated with reductions in food security among households with children (43). The overall evidence thus far suggests that the pandemic had significant impacts on food security in many populations, particularly among those who are more socially vulnerable (23,25,43). However, there has been evidence of government safety nets mitigating the pandemic's impacts on rates of food insecurity (26), and our results reflect this to some extent: income supports were made available early in the pandemic in Australia, Canada, the United Kingdom, and the United States, but were not available in Mexico until October 2020 (see Supplemental Table 1), where the proportion of respondents reporting food security impacts was highest.
In terms of overall diet healthfulness, about 40%–60% of respondents across all countries reported changes in their diet compared to before the COVID-19 pandemic. A slight trend towards healthful changes was apparent in all countries, but a notable proportion reported less healthful changes as well. The bidirectional nature of these results suggests that the impacts of COVID-19 on dietary intake have been highly variable, and these results to some extent mirror the evidence available thus far on COVID-19 dietary patterns. A study assessing self-reported dietary changes among adults in Los Angeles Country in July 2020 reported results similar to those observed in the current study: 28% reported eating more healthful food and 25% reported eating less healthful food since the beginning of the pandemic (7). A similar study of adults from the United States in October 2020 found that among the three-quarters of respondents who reported their household's eating habits had changed, 64% and 19% reported more healthful and less healthful eating habits, respectively (6). Values from the latter study suggest greater increases in overall diet healthfulness than those observed among US respondents in this study; however, this may be explained by the previous study's focus on changes in eating habits across the respondent's entire household (6).
This study also provided a preliminary look at potential associations between COVID-19-related dietary changes and sociodemographic characteristics. Country-by-covariate interactions confirmed that the relationships between individual characteristics and COVID-19-related dietary outcomes were not always consistent across countries. There were strong relationships between income-related variables (income adequacy and COVID-19 impacts on food security) and changes in food behaviors and overall diet, with results suggesting that respondents of lower socioeconomic status were more likely to have their food behaviors and overall diet impacted by the pandemic. In particular, respondents with low income adequacy were far more likely than those with higher income adequacy to report that COVID-19 has impacted whether their household has had enough food to eat, and more likely to indicate that their diet is less healthful than before the pandemic. However, in Mexico, lower-income respondents were sometimes less likely to report increased frequency of food behaviors like purchasing groceries online, which may be due to limited access to online grocery ordering among lower income groups in Mexico, whose internet access is more likely to be limited to a mobile phone (38).
Associations also suggested that older respondents were less likely to report changes in food behaviors, overall diet, and food security, and female participants were more likely to report some healthier shifts in food behaviors in response to the pandemic, such as less eating food prepared away from home and less food delivered from a restaurant. It is possible that the more stable income provided by pensions among older adults in most countries in this study may have partially mitigated the financial-related impacts of COVID-19 on their food behaviors relative to younger people. Interaction results, however, indicated that the age-outcome relationships were often less pronounced in Mexico. Respondents reporting a minority ethnicity were more likely than those of majority ethnicities to report healthful changes in their overall diet, while respondents with higher BMI values were more likely to report a less healthful diet since the COVID-19 pandemic compared to those classified as having a normal BMI. Previous studies have reported similar associations with sociodemographic characteristics: a study among Los Angeles County adults found that non-Hispanic Black and Hispanic/Latino respondents were more likely than non-Hispanic Whites to report healthful dietary changes following COVID-19, while respondents who were younger or had BMIs corresponding to obesity were more likely to report less healthful changes (7). In a survey among adults living in England, young adults and those from minority ethnic groups reported greater impacts of COVID-19 on their purchasing decisions of more healthful foods (9).
In addition to sociodemographic variables, the current study also observed associations between study outcomes and COVID-19 illness status. Respondents who had contracted COVID-19 (confirmed by test) were more likely than those who had not to report changes in all examined food behaviors and overall diet (in both directions); again, this relationship was often less pronounced among Mexican respondents. Further research will be required to identify the characteristics of individuals who made healthful and less healthful changes in response to the COVID-19 pandemic.
Strengths and limitations
This study is among the first to examine COVID-19-related changes in food behaviors and food security across multiple countries. The large sample sizes and consistent methods across countries provide valuable insights into these outcomes across countries and sociodemographic groups. This study is, however, subject to limitations common to survey research. Respondents were recruited using nonprobability-based sampling; therefore, the findings do not provide nationally representative estimates. For example, although the data were weighted by age group, sex, region, ethnicity (except in Canada), and education level (except in Mexico), the Mexico sample had notably higher levels of education and lower levels of overweight and obesity compared to national benchmark estimates. In other countries, estimates of overweight and obesity in the study sample were similar or somewhat lower than national benchmarks. Further, the study relied on self-reported changes in behaviors, which are important and valuable indicators of change in the absence of pre- and postpandemic data; however, the responses assessed in the current study may be subject to social desirability bias or recall bias. Given that our study queried respondents’ food behaviors in the present tense, our results are also limited to the time of data collection (November–December 2020), meaning that behavioral changes that occurred earlier in the pandemic may not have been captured. Future research should assess changes in behaviors and health status using data from before, during, and after the pandemic, where possible. Lastly, the analyses in this paper did not consider subnational differences. There were likely strong regional differences in the way the pandemic was experienced, particularly in countries where COVID-19 restrictions were largely under state or provincial control, including Canada, the United States, and Australia. For example, exploratory analyses within Australia indicated much higher prevalences of changes in food behaviors and food security among respondents in the state of Victoria—where a strict 4-month lockdown period (July–October 2020) had just been lifted prior to our data collection (44)—compared to other Australian respondents (data not shown). Therefore, a full examination of the impact of COVID-19 on dietary patterns will require a closer examination of subnational trends at the regional level.
Conclusions
The data reported here provide empirical evidence from 5 countries on significant shifts in food behaviors, food security, and overall diet during the COVID-19 pandemic. Approximately 8 months into the pandemic, the largest change reported was a decrease in eating food prepared away from home, but shifts towards ordering less food from restaurants, buying more groceries online, and buying fewer groceries from corner stores were also observed. Many respondents reported impacts on their household's food security, as well as some shifts towards a more healthful diet overall. However, changes in both directions were observed for all outcomes, suggesting that the response to COVID-19 was highly variable. Reported changes for all outcomes tended to be largest in Mexico, where national COVID-19-related policies and other contextual factors may have played a role. Across all 5 countries, individuals with characteristics corresponding to a lower socioeconomic status, as well as those experiencing food security effects from the pandemic, were more likely to report shifts in their dietary patterns, suggesting that COVID-19 response plans should include a focus on these populations. In light of the results observed in this study, decision-makers should consider how existing or future food policies (e.g., national dietary guidance, food labeling, marketing restrictions) could be leveraged to encourage healthful dietary changes and discourage less healthful changes in the contexts of current or future pandemics. Perhaps more importantly, social safety nets that guarantee income among citizens will be critical to help to build resilience of populations to the economic shocks and subsequent impacts on food security resulting from pandemics. Longitudinal research is needed to evaluate whether the observed changes persist after the pandemic, and there is a need for research and policy to catch up with the rapid change in food purchasing practices, particularly in the digital market.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—DH, LV, and CMW: were major contributors to the conception and design of the study; CMW: supervised data collection; RBA: analyzed the data and performed the statistical analyses; RBA, LV, and DH: were major contributors in drafting the manuscript; LV, AJC, SG, AJ, GS, CMW, MW, and DH: contributed to interpreting the data and substantively revising the manuscript; RBA: had primary responsibility for the final content; and all authors: read and approved the final manuscript.
Notes
This supplement was supported by funding from a Project Grant from the Canadian Institutes of Health Research (PJT-162167). The views expressed herein are solely the responsibility of the authors and do not necessarily represent the official views of the Canadian Institutes for Health Research or other sources of funding. Funding for the International Food Policy Study was provided by a Canadian Institutes of Health Research (CIHR) Project Grant (PJT-162167), with additional support from Health Canada, the Public Health Agency of Canada (PHAC), and a CIHR-PHAC Applied Public Health Chair (DH). MW is supported with funding for a research programme in the MRC Epidemiology Unit, University of Cambridge, UK (MRC grant number: MC/UU/00006/7).
Author disclosures: DH has served as a paid expert witness on behalf of public health authorities in the legal challenge to San Francisco’s health warning ordinance for sugar-sweetened beverages. All other authors report no conflicts of interest.
Supplemental Tables 1–3 and Supplemental Figure 1 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Contributor Information
Rachel B Acton, School of Public Health Sciences, University of Waterloo, Waterloo, Canada.
Lana Vanderlee, École de Nutrition, Centre Nutrition, santé et société (Centre NUTRISS), and Institut sur la nutrition et les aliments fonctionnels (INAF), Université Laval, Québec, Canada.
Adrian J Cameron, Global Obesity Centre, Institute for Health Transformation, Deakin University, Geelong, Australia.
Samantha Goodman, School of Public Health Sciences, University of Waterloo, Waterloo, Canada.
Alejandra Jáuregui, Centre for Health and Nutrition Research, National Institute of Public Health, Cuernavaca, Mexico.
Gary Sacks, Global Obesity Centre, Institute for Health Transformation, Deakin University, Geelong, Australia.
Christine M White, School of Public Health Sciences, University of Waterloo, Waterloo, Canada.
Martin White, Medical Research Council Epidemiology Unit, University of Cambridge, Cambridge, United Kingdom.
David Hammond, School of Public Health Sciences, University of Waterloo, Waterloo, Canada.
References
- 1. WHO . Listings of WHO's response to COVID-19. [Internet]. Geneva (Switzerland): WHO; 2020. Available from: https://www.who.int/news/item/29-06-2020-covidtimeline. [Google Scholar]
- 2. Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, Macdonald B, Giattino C, Appel C, Roser M. OurWorldInData.org—policy responses to the coronavirus pandemic. [Internet]. Oxford: Oxford University Press; 2020. Available from: https://ourworldindata.org/coronavirus. [Google Scholar]
- 3. Center for Systems Science and Engineering (CSSE) at Johns Hopkins University . COVID-19 data explorer—daily new confirmed COVID-19 cases per million people. [Internet]. Oxford: Oxford University Press; 2021. Available from: https://ourworldindata.org/explorers/coronavirus-data-explorer?zoomToSelection=true&time=2020-11-19.2020-12-23&facet=none&pickerSort=asc&pickerMetric=location&Metric=Confirmed+cases&Interval=7-day+rolling+average&Relative+to+Population=true&Color+by+test+positivity=false&country=USA∼GBR∼CAN∼MEX∼AUS. [Google Scholar]
- 4. Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, Massaro JM, D'Agostino RB, White M. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020;370:m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Parekh N, Deierlein AL. Health behaviours during the coronavirus disease 2019 pandemic: implications for obesity. Public Health Nutr. 2020;23:3121–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cosgrove K, Wharton C. Predictors of COVID-19-related perceived improvements in dietary health: results from a US cross-sectional study. Nutrients. 2021;13:2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Miller S, Bruine de Bruin W, Livings M, Wilson J, Weber K, Frazzini A, Babboni M, de la Haye K. Self-reported dietary changes among L.A. county adults during the COVID-19 pandemic. Appetite. 2021;166:105586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carroll N, Sadowski A, Laila A, Hruska V, Nixon M, Ma DWL, Haines J, on behalf of the Guelph Family Health Study. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12:2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ogundijo DA, Tas AA, Onarinde BA. Exploring the impact of COVID-19 pandemic on eating and purchasing behaviours of people living in England. Nutrients. 2021;13:1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murphy B, Benson T, McCloat A, Mooney E, Elliott C, Dean M, Lavelle F. Changes in consumers’ food practices during the COVID-19 lockdown, implications for diet quality and the food system: a cross-continental comparison. Nutrients. 2020;13:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Benson T, Murphy B, McCloat A, Mooney E, Dean M, Lavelle F. From the pandemic to the pan: the impact of COVID19 on parental inclusion of children in cooking activities–A cross-continental survey. Public Health Nutr. 2021;1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ammar A, Brach M, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, Bouaziz B, Bentlage E, How D, Ahmed Met al. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Skotnicka M, Karwowska K, Kłobukowski F, Wasilewska E, Małgorzewicz S. Dietary habits before and during the COVID-19 epidemic in selected European countries. Nutrients. 2021;13:1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bakaloudi D, Jeyakumar D, Jayawardena R, Chourdakis M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: a systematic review of the evidence. Clin Nutr. [accessed 2022 Feb 14]. doi:10.1016/j.clnu.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Flanagan EW, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity. 2021;29:438–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Blázquez A. Coronavirus: grocery delivery & pickup sales U.S. [Internet]. Hamburg (Germany): Statista; 2021. Available from: https://www.statista.com/statistics/1120211/coronavirus-grocery-delivery-pickup-sales-us/. [Google Scholar]
- 17. Bedford E. Past-week online grocery service usage Canada 2016–2020. [Internet]. Hamburg (Germany): Statista; 2020. Available from: https://www.statista.com/statistics/1175029/past-week-online-grocery-service-usage-canada/. [Google Scholar]
- 18. Hinton T. Australia: monthly online food retail revenue 2020. [Internet]. Hamburg (Germany): Statista; 2021. Available from: https://www.statista.com/statistics/1186876/australia-monthly-online-food-retail-revenue/. [Google Scholar]
- 19. Grashuis J, Skevas T, Segovia MS. Grocery shopping preferences during the COVID-19 pandemic. Sustainability. 2020;12:5369. [Google Scholar]
- 20. Baarsma B, Groenewegen J. COVID-19 and the demand for online grocery shopping: empirical evidence from the Netherlands. Economist (Leiden). [Accessed 2022 Feb 14]. doi:10.1007/s10645-021-09389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dono J, Ettridge K, Wakefield M, Pettigrew S, Coveney J, Roder D, Durkin S, Wittert G, Martin J, Miller C. Intentions to reduce sugar-sweetened beverage consumption: the importance of perceived susceptibility to health risks. Public Health Nutr. 2021;24(17):5663–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lamarche B, Brassard D, Lapointe A, Laramée C, Kearney M, Côté M, Bélanger-Gravel A, Desroches S, Lemieux S, Plante C. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: results from NutriQuébec. Am J Clin Nutr. 2021;113:984–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Picchioni F, Goulao L, Roberfroid D. The impact of COVID-19 on diet quality, food security and nutrition in low and middle income countries: a systematic review of the evidence. Clin Nutr. [accessed 2022 Feb 14]. doi:10.1016/j.clnu.2021.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fitzpatrick KM, Harris C, Drawve G, Willis DE. Assessing food insecurity among US adults during the COVID-19 pandemic. J Hunger Environ Nutr. 2020;16:1–18. [Google Scholar]
- 25. Wolfson JA, Leung CW. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. 2020;12:1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. USDA Economic Research Service . Household food security in the United States in 2020. Economic Research Report No. (ERR-298). [Internet]. Washington (DC): U.S. Department of Agriculture; 2021. Available from: https://www.ers.usda.gov/publications/pub-details/?pubid=102075. [Google Scholar]
- 27. Hammond D, White CM, Rynard VL, Vanderlee L. International food policy study: technical report—2020 survey (Wave 4). [Internet]. Waterloo (Canada): International Food Policy Study; 2021. Available from: http://www.foodpolicystudy.com/methods. [Google Scholar]
- 28. Australia Bureau of Statistics . Census of population and housing. [Internet]. Canberra (Australia): Australian Bureau of Statistics; 2016. Available from: https://www.abs.gov.au/websitedbs/censushome.nsf/home/2016. [Google Scholar]
- 29. Australia Bureau of Statistics . Australian Health Survey: users’ guide, 2011–13. [Internet]. Canberra (Australia): Australian Bureau of Statistics; 2013. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4363.0.55.001main+features12011-13 [Google Scholar]
- 30. Public Health England . National diet and nutrition survey. [Internet]. London: Public Health England; 2016. Available from: https://www.gov.uk/government/collections/national-diet-and-nutrition-survey [Google Scholar]
- 31. Statistics Canada . Canadian Community Health Survey—annual component (CCHS). [Internet]. Ottawa (Canada): Statistics Canada; 2020. Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 32. Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey. [Internet]. Washington (DC): U.S. Department of Health & Human Services; 2021. Available from: https://www.cdc.gov/nchs/nhanes/index.htm. [Google Scholar]
- 33. Centers for Disease Control and Prevention . Behavioral risk factor surveillance system. [Internet]. Washington (DC): U.S. Department of Health & Human Services; 2016. Available from: https://www.cdc.gov/brfss/index.html. [Google Scholar]
- 34. WHO . Body mass index—BMI. [Internet]. Geneva (Switzerland): WHO; 2020. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. [Google Scholar]
- 35. The New York Times . Tracking coronavirus in Australia: latest map and case count. [Internet]. New York (NY): The New York Times; 2021. Available from: https://www.nytimes.com/interactive/2021/world/australia-covid-cases.html. [Google Scholar]
- 36. Wellard-Cole L, Davies A, Allman-Farinelli M. Contribution of foods prepared away from home to intakes of energy and nutrients of public health concern in adults: a systematic review. Crit Rev Food Sci Nutr. [accessed 2022 Feb 14]. doi:10.1080/10408398.2021.1887075. [DOI] [PubMed] [Google Scholar]
- 37. UNICEF . COVID-19 and school closures: one year of education disruption. [Internet]. UNICEF; 2021. Available from: https://data.unicef.org/resources/one-year-of-covid-19-and-school-closures/. [Google Scholar]
- 38. Mendoza J. Online grocery shopping in Mexico—statistics & facts. [Internet]. Hamburg (Germany): Statista; 2021. Available from: https://www.statista.com/topics/7819/online-grocery-shopping-in-mexico/. [Google Scholar]
- 39. Blumtritt C. Number of users forecast for the online food delivery market in United States from 2017 to 2024. [Internet]. Hamburg (Germany): Statista; 2021. Available from: https://www.statista.com/forecasts/891084/online-food-delivery-users-by-segment-in-united-states. [Google Scholar]
- 40. eMarketer Editors . Food delivery orders in Canada increased substantially amid the pandemic. [Internet]. New York: eMarketer; 2021. Available from: https://www.emarketer.com/content/food-delivery-orders-canada-increased-substantially-amid-pandemic. [Google Scholar]
- 41. Roy Morgan Research . Meal delivery services Uber Eats, Menulog, Deliveroo and DoorDash experienced rapid growth during 2020—a year of lockdowns & work from home. [Internet]. Melbourne (Australia): Roy Morgan; 2021. Available from: http://www.roymorgan.com/findings/8713-food-delivery-services-may-2021-202105280627. [Google Scholar]
- 42. Statista Research Department . Online food delivery revenue in Mexico 2017–2024. [Internet]. Hamburg (Germany): Statista; 2021. Available from: https://www.statista.com/forecasts/1220827/revenue-online-food-delivery-mexico. [Google Scholar]
- 43. Gaitán-Rossi P, Vilar-Compte M, Teruel G, Pérez-Escamilla R. Food insecurity measurement and prevalence estimates during the COVID-19 pandemic in a repeated cross-sectional survey in Mexico. Public Health Nutr. 2021;24:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Parliament of Victoria Public Accounts and Estimates Committee . Inquiry into the Victorian government's response to the COVID-19 pandemic. [Internet]. Melbourne (Australia): Parliament of Victoria; 2021. Available from: https://www.parliament.vic.gov.au/file_uploads/PAEC_59-08_Vic_Gov_response_to_COVID-19_pandemic_YKNbjt2Y.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.