ABSTRACT
Background
In the general population with coronavirus disease 2019 (COVID-19), obesity is associated with an increased risk of mortality. Given the typically observed obesity paradox among patients on kidney function replacement therapy (KFRT), especially dialysis patients, we examined the association of obesity with mortality among dialysis patients or living with a kidney transplant with COVID-19.
Methods
Data from the European Renal Association COVID-19 Database (ERACODA) were used. KFRT patients diagnosed with COVID-19 between 1 February 2020 and 31 January 2021 were included. The association of Quetelet's body mass index (BMI) (kg/m2), divided into: <18.5 (lean), 18.5–24.9 (normal weight), 25–29.9 (overweight), 30–34.9 (obese I) and ≥35 (obese II/III), with 3-month mortality was investigated using Cox proportional-hazards regression analyses.
Results
In 3160 patients on KFRT (mean age: 65 years, male: 61%), 99 patients were lean, 1151 normal weight (reference), 1160 overweight, 525 obese I and 225 obese II/III. During follow-up of 3 months, 28, 20, 21, 23 and 27% of patients died in these categories, respectively. In the fully adjusted model, the hazard ratios (HRs) for 3-month mortality were 1.65 [95% confidence interval (CI): 1.10, 2.47], 1 (ref.), 1.07 (95% CI: 0.89, 1.28), 1.17 (95% CI: 0.93, 1.46) and 1.71 (95% CI: 1.27, 2.30), respectively. Results were similar among dialysis patients (N = 2343) and among those living with a kidney transplant (N = 817) (Pinteraction = 0.99), but differed by sex (Pinteraction = 0.019). In males, the HRs for the association of aforementioned BMI categories with 3-month mortality were 2.07 (95% CI: 1.22, 3.52), 1 (ref.), 0.97 (95% CI: 0.78. 1.21), 0.99 (95% CI: 0.74, 1.33) and 1.22 (95% CI: 0.78, 1.91), respectively, and in females corresponding HRs were 1.34 (95% CI: 0.70, 2.57), 1 (ref.), 1.31 (95% CI: 0.94, 1.85), 1.54 (95% CI: 1.05, 2.26) and 2.49 (95% CI: 1.62, 3.84), respectively.
Conclusion
In KFRT patients with COVID-19, on dialysis or a kidney transplant, obesity is associated with an increased risk of mortality at 3 months. This is in contrast to the obesity paradox generally observed in dialysis patients. Additional studies are required to corroborate the sex difference in the association of obesity with mortality.
Keywords: COVID-19, kidney failure, mortality, obesity paradox, reverse epidemiology
INTRODUCTION
Obesity is a well-established risk factor for mortality in the general population, such that Quetelet's body mass index (BMI) over 30 kg/m² is associated with a sharp increase in the risk of mortality [1]. However, the relationship between obesity and mortality has not been observed consistently across all population subgroups. Among patients on kidney function replacement therapy (KFRT), especially dialysis patients, obesity is reported to be associated with better survival, a phenomenon known as the ‘obesity paradox’ [2].
Early in the coronavirus disease 2019 (COVID-19) pandemic, obesity was identified as a key risk factor for severe complications including death among the general population with COVID-19 [3]. To our knowledge, there has not been a comprehensive study to investigate the association of obesity with the risk of mortality among patients on KFRT with COVID-19, and consequently, it is unclear whether the ‘obesity paradox’ holds true also among patients on KFRT with COVID-19 infection [4].
Given the high COVID-19 case-fatality rate among patients on KFRT [5] and thereby the need to understand risk factors for severe COVID-19, we aimed to investigate the relationship of obesity with mortality and other major disease-related outcomes among patients on KFRT with COVID-19 using data from the European Renal Association COVID-19 Database (ERACODA), the largest European database of patients on KFRT with COVID-19, which prospectively collected detailed information on patient and disease characteristics.
MATERIALS AND METHODS
Study design and participants
The ERACODA database was established in March 2020 and currently involves the cooperation of approximately 220 physicians representing over 140 centers in 33 countries, mostly in Europe. Data were collected on adult (≥18 years) patients with kidney failure, either on dialysis or living with a functioning kidney allograft, who were diagnosed with COVID-19 based on a positive result on a real-time polymerase chain reaction assay or rapid antigen test of nasal and/or pharyngeal swab specimens and/or compatible findings on CT scan or chest X-ray. Data were voluntarily reported from outpatients and hospitalized patients by physicians responsible for their care [6].
The ERACODA database is hosted at the University Medical Center Groningen, the Netherlands. Data are recorded using REDCap software (Research Electronic Data Capture, Vanderbilt University Medical Center, Nashville, TN, USA) for data collection [7]. Patient information is stored pseudonymized. The study was approved by the Institutional Review Board of the University Medical Center Groningen, the Netherlands. Because of the observational, non-interventional nature, the institutional review board deemed the collection and analysis of data exempt from ethics review regarding the Medical Research Involving Human Subjects Act (WMO).
Data collection
Detailed information was collected on the patient (age, sex, ethnicity, height, weight, frailty, comorbidities, hospitalization and medication use) and COVID-19-related characteristics (symptoms, vital signs and laboratory test results) at presentation. Frailty was assessed using the Clinical Frailty Score developed by Rockwood et al. [8]. BMI was calculated by dividing body weight by the square of height, expressed in kg/m2, and used to assess obesity categorized as per World Health Organization (WHO) classification i.e. <18.5 (underweight), 18.5–24.9 (normal), 25–29.9 (overweight), 30–34.9 (obesity Class I) and ≥35 kg/m2 (obesity Class II/III) [9]. Obesity classes II and III were merged to allow sufficient patients in this category.
The primary outcome of this study was vital status at 3 months after COVID-19 diagnosis and the secondary outcomes were hospitalization, Intensive Care Unit (ICU) admission and, in-hospital mortality. All patients who presented between 1 February 2020 and 31 January 2021 and for whom information on BMI, type of KFRT, date of presentation and 3-month vital status was available, were included in the analysis (Supplementary data, Figure S1).
Statistical analysis
Baseline characteristics are presented for the total population, and by categories of BMI. Characteristics were compared between groups using ANOVA for continuous variables (Kruskal–Wallis test for non-normally distributed data) and Pearson chi-squared statistics for categorical variables.
For the association of BMI (18.5–24.9 kg/m2 as reference) with primary and secondary outcomes, hazard ratios (HRs) with corresponding 95% confidence intervals (CIs), were estimated for the total population and dialysis patients and those living with kidney transplants separately using Cox proportional-hazards regression analyses. To account for potential confounders, multiple models were constructed in a stepwise manner. Model 1 was unadjusted. In Model 2 we adjusted for age (continuous) and sex (male/female) and in Model 3 additionally for type of KFRT (except when analyzing dialysis patients and those living with kidney transplants separately). Model 4 was additionally adjusted for factors known to be associated with COVID-19 outcomes, i.e. smoking (never, current, former), hypertension (no/yes), diabetes (no/yes), coronary artery disease (no/yes), heart failure (no/yes) and chronic lung disease (no/yes). Finally, in Model 5, we further adjusted for clinical frailty score (continuous). Heterogeneity in the association of BMI and mortality in dialysis patients and those living with kidney transplants was investigated by testing the interaction between type of KFRT (dialysis/kidney transplant) and BMI in a fully adjusted model. The proportional-hazards assumption was investigated by comparing the fully adjusted model with and without the interaction of log(time) with individual covariates. Kaplan–Meier curves were plotted to show cumulative 3-month survival by BMI categories.
Several additional analyses were performed to assess the robustness of our findings. First, the association between BMI and mortality was investigated across key subgroups including age (<65/≥65 years), sex (female/male), clinical frailty score (<4/≥4), the reason for COVID-19 screening (symptoms-based screening/positive COVID-19 contact or routine screening), hypertension (no/yes) and diabetes mellitus (no/yes). Heterogeneity of associations between aforementioned subgroups was investigated by testing the interaction between a subgroup and BMI in Model 5. Second, to allow modeling of any nonlinear association between BMI and mortality, we explored the association between BMI (continuous) and 3-month mortality using restricted cubic splines. We prespecified the use of three knots to ensure enough flexibility to the model while also not making the model oversensitive to small fluctuations. Third, to investigate the association of BMI with mortality during the earlier phase of the disease, the association was investigated for 28-day mortality instead of 3-month mortality. Finally, to account for missing values for BMI, we imputed missing values using multiple imputations by chained equations and repeated our analyses. In total, 10 imputed datasets were created with 100 iterations. Estimated coefficients and corresponding standard errors across imputed datasets were pooled as per Rubin’s Rules [10].
All analyses were performed using Stata version 14.0 (College Station, TX, USA). A 2-sided value of ˂0.05 indicated statistical significance.
RESULTS
Baseline characteristics
A total of 3160 patients were analyzed, of which 3% were underweight, 36% normal weight, 37% overweight, 17% obesity class I and 7% obesity class II/III (Table 1). When compared with normal weight, the higher obesity categories were characterized by lower age, more women and higher frailty. Hypertension and diabetes were more prevalent in the obesity categories compared with the normal weight category. Also, the prevalence of cough, shortness of breath and myalgia/arthralgia was higher in the obesity categories compared with the normal weight category, as was the level of C-reactive protein (CRP). Dialysis patients on average were older and had a higher comorbidity burden than those living with a kidney transplant. However, the mean BMI, the prevalence of obesity and the trends in the distribution of patient demographics, comorbidities and disease characteristics across BMI categories in dialysis patients and transplant recipients were similar to trends in the total population (Supplementary data, Tables S1 and S2).
Table 1.
Baseline demographic and clinical characteristics of patients on kidney function replacement therapy with COVID-19 by Quetelet's body mass index (BMI) categories
| BMI categories | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Total (N = 3160) | Underweight <18.5 (N = 99) | Normal 18.5–24.9 (N = 1151) | Overweight 25–29.9 (N = 1160) | Obesity I 30–34.9 (N = 525) | Obesity II/III ≥35 (N = 225) | P-value |
| Patient characteristics | |||||||
| Male sex, % | 61.1 | 47.5 | 61.2 | 66.9 | 58.1 | 44.0 | <0.001 |
| Age, year | 64.8 | 60.7 | 64.8 | 65.4 | 65.7 | 62.3 | 0.002 |
| BMI, kg/m2 | 26.8 | 17.2 | 22.4 | 27.2 | 32.1 | 39.2 | <0.001 |
| Race | 0.08 | ||||||
| White or Caucasian, % | 84.6 | 77.8 | 85.5 | 83.3 | 85.0 | 88.3 | |
| Non-White, % | 15.4 | 22.2 | 14.5 | 16.7 | 15.0 | 11.7 | |
| Tobacco use | 0.01 | ||||||
| Current, % | 5.8 | 8.1 | 7.5 | 4.4 | 4.6 | 5.8 | |
| Prior, % | 20.9 | 15.2 | 19.4 | 23.5 | 20.8 | 18.7 | |
| Never, % | 41.6 | 42.4 | 42.5 | 40.2 | 44.4 | 37.8 | |
| Unknown, % | 31.7 | 34.3 | 30.7 | 31.9 | 30.3 | 37.8 | |
| Clinical frailty scale, AU | 3.6 | 4.2 | 3.6 | 3.5 | 3.7 | 4.1 | <0.001 |
| Reason for screeninga | 0.04 | ||||||
| Symptoms only, % | 66.9 | 61.4 | 64.3 | 66.2 | 70.7 | 77.4 | |
| Symptoms & COVID + Contact, % | 15.2 | 17.1 | 14.5 | 16.4 | 15.4 | 11,3 | |
| COVID + Contact only, % | 9.6 | 8.6 | 11.8 | 9.0 | 8.1 | 5.1 | |
| Routine, % | 8.3 | 12.9 | 9.4 | 8.4 | 5.9 | 6.2 | |
| Comorbidities | |||||||
| Hypertension, % | 83.6 | 73.7 | 80.5 | 85.7 | 87.6 | 84.0 | <0.001 |
| Diabetes mellitus, % | 40.7 | 19.2 | 30.2 | 42.4 | 56.2 | 59.1 | <0.001 |
| Coronary artery disease, % | 31.4 | 25.3 | 32.1 | 29.8 | 33.7 | 32.9 | 0.30 |
| Heart failure, % | 20.9 | 17.2 | 19.8 | 20.7 | 22.7 | 24.4 | 0.36 |
| Chronic lung disease, % | 11.8 | 15.2 | 10.7 | 11.6 | 12.4 | 16.0 | 0.16 |
| Active malignancy, % | 5.3 | 4.0 | 6.5 | 5.5 | 3.2 | 3.1 | 0.03 |
| Auto-immune disease, % | 4.2 | 9.1 | 4.5 | 3.9 | 3.0 | 4.9 | 0.08 |
| Primary kidney disease | |||||||
| Primary glomerulonephritis, % | 14.5 | 12.1 | 16.7 | 15.7 | 9.5 | 9.8 | <0.001 |
| Pyelonephritis, % | 2.0 | 0.0 | 2.6 | 2.0 | 1.0 | 1.8 | 0.12 |
| Interstitial nephritis, % | 3.0 | 6.1 | 2.8 | 2.6 | 3.4 | 3.6 | 0.33 |
| Hereditary kidney disease, % | 8.6 | 5.1 | 10.8 | 8.4 | 6.5 | 4.9 | 0.003 |
| Congenital diseases, % | 2.2 | 4.0 | 3.1 | 1.4 | 2.1 | 1.8 | 0.06 |
| Vascular diseases, % | 15.9 | 17.2 | 16.5 | 15.8 | 16.8 | 10.3 | 0.19 |
| Sec. glomerular disease, % | 7.9 | 12.1 | 6.9 | 7.8 | 8.6 | 9.8 | 0.24 |
| Diabetic kidney disease, % | 20.4 | 7.1 | 16.1 | 20.6 | 27.7 | 29.9 | <0.001 |
| Other, % | 16.2 | 22.2 | 14.6 | 15.8 | 17.6 | 20.5 | 0.07 |
| Unknown, % | 9.4 | 14.1 | 9.9 | 10.0 | 6.9 | 7.6 | 0.09 |
| Kidney replacement type | 0.07 | ||||||
| Dialysis, % | 74.1 | 82.8 | 75.9 | 72.2 | 72.8 | 74.2 | |
| Transplant, % | 25.8 | 17.2 | 24.1 | 27.8 | 27.2 | 25.8 | |
| Time since transplantationb | 0.01 | ||||||
| <1 year, % | 10.3 | 11.8 | 6.5 | 9.9 | 18.9 | 8.6 | |
| 1–5 years, % | 37.6 | 29.4 | 36.1 | 40.4 | 37.1 | 32.8 | |
| >5 years, % | 51.6 | 58.8 | 57.0 | 49.1 | 44.1 | 56.9 | |
| Medication use | |||||||
| RAAS inhibition use, % | 26.2 | 23.2 | 24.0 | 27.3 | 29.3 | 25.8 | 0.05 |
| Immunosuppressants useb | 0.55 | ||||||
| Triple therapy, % | 62.1 | 52.9 | 59.2 | 63.7 | 61.5 | 70.7 | |
| Dual therapy, % | 35.0 | 41.2 | 38.6 | 33.5 | 32.9 | 29.3 | |
| Mono therapy, % | 2.1 | 5.9 | 1.4 | 2.5 | 2.8 | 0 | |
| Disease-related characteristics | |||||||
| Presenting symptoms | |||||||
| Sore throat, % | 13.5 | 7.2 | 13.2 | 13.8 | 16.3 | 9.6 | 0.002 |
| Cough, % | 52.4 | 42.5 | 50.0 | 51.1 | 60.4 | 56.9 | 0.001 |
| Shortness of breath, % | 35.1 | 34.2 | 33.9 | 33.1 | 37.8 | 45.8 | 0.009 |
| Fever, % | 58.7 | 51.4 | 56.6 | 60.4 | 61.0 | 58.3 | 0.23 |
| Headache, % | 12.4 | 12.0 | 12.2 | 12.7 | 12.2 | 13.3 | 0.37 |
| Nausea or vomiting, % | 11.8 | 12.0 | 12.4 | 10.4 | 13.0 | 12.7 | 0.26 |
| Diarrhea, % | 15.8 | 12.0 | 15.9 | 16.0 | 15.4 | 16.8 | 0.72 |
| Myalgia or arthralgia, % | 23.0 | 16.9 | 23.0 | 22.7 | 23.4 | 26.9 | 0.03 |
| Vital signs | |||||||
| Temperature, °C | 37.4 | 37.3 | 37.4 | 37.5 | 37.4 | 37.6 | 0.18 |
| Respiration rate/min | 19.1 | 19.3 | 18.6 | 19.1 | 19.9 | 20.2 | <0.001 |
| O2 saturation room air, % | 93.9 | 93.2 | 94.3 | 93.9 | 93.8 | 92.9 | 0.08 |
| Systolic BP, mmHg | 135.4 | 128.7 | 135.4 | 134.7 | 137.8 | 135.9 | 0.08 |
| Diastolic BP, mmHg | 74.9 | 76.6 | 74.5 | 75.2 | 75.2 | 73.2 | 0.48 |
| Pulse rate, BPM | 82.7 | 86.2 | 82.0 | 83.1 | 82.8 | 83.6 | 0.27 |
| Laboratory test results | |||||||
| eGFR | 42.8 | 37.8 | 45.6 | 43.3 | 38.4 | 40.1 | 0.61 |
| Lymphocytes, ×1000/µL | 0.8 (0.5, 1.4) | 0.8 (0.5, 1.3) | 0.8 (0.6, 1.3) | 0.9 (0.6, 1.3) | 0.9 (0.6, 1.4) | 0.9 (0.6, 1.5) | 0.62 |
| CRP, mg/L | 28 (7, 82) | 30 (6, 74) | 23 (6, 70) | 28 (7, 84) | 33 (10, 88) | 44 (10, 107) | <0.001 |
Continuous variables are reported as mean ± SD or median (IQR). Groups were compared using one way ANOVA, Kruskal–Wallis test or chi-squared test as appropriate. Obesity is defined as BMI >30 kg/m2.
ACE, angiotensin-converting enzyme; ARB, angiotensin-II receptor blocker; BMI, body mass index; RAAS, renin-angiotensin-aldosterone system; CNI, calcineurin inhibitor; °C, degree Celsius; CRP, C-reactive protein; BP, blood pressure; O2, oxygen; eGFR, estimated glomerular filtration rate.
a664 patients missing information of identification method.
bAmong kidney transplant recipients (n = 817).
Association of BMI with 3-month mortality
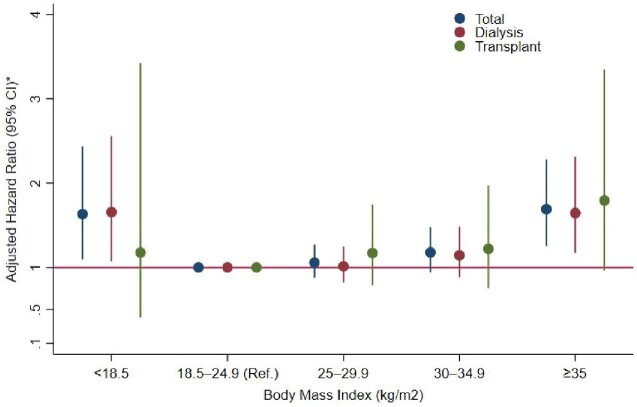
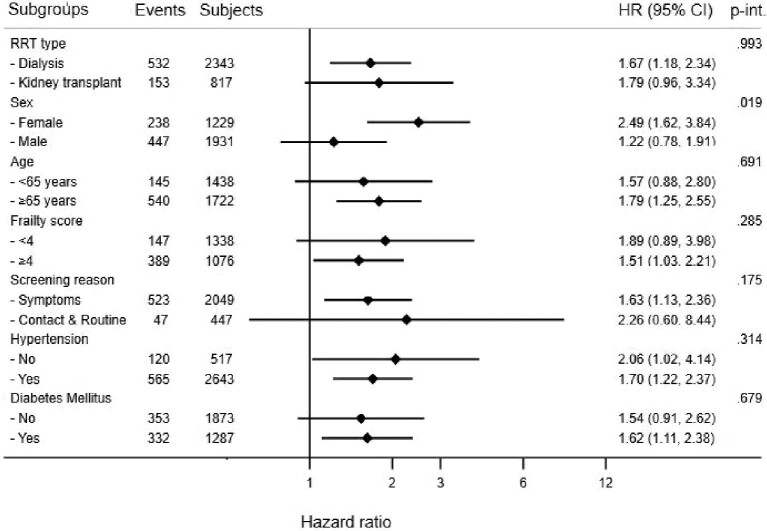
The percentage of patients who experienced 3-month mortality was 28.3, 20.2, 21.0, 23.0 and 26.7% in the underweight, normal weight, overweight, obesity class I and obesity class II/III categories, respectively. The 3-month cumulative survival was lower in underweight and obesity class II/III categories compared with other BMI categories, with similar results among dialysis patients and transplant recipients (Figure 1). Compared with the normal weight category, the HR for the association of 3-month mortality in the fully adjusted model was 1.65 (95% CI: 1.10, 2.47) in underweight, 1.07 (95% CI: 0.89, 1.28) in overweight, 1.17 (95% CI: 0.93, 1.46) in obesity class I and 1.71 (95% CI: 1.27, 2.30) in obesity class II/III categories (Table 2). These HRs were essentially similar in dialysis patients and those living with a kidney transplant (Table 2, Figure 2). There was no interaction between the type of KFRT (dialysis/kidney transplant) and BMI categories (Pinteraction = 0.99 in the fully adjusted model). The models that were used demonstrated no violation of the proportional-hazards assumption (P for the difference in fully adjusted model with and without time-varying covariates = .13 in the total population, .21 in dialysis patients and .62 in transplant recipients).
FIGURE 1:
Kaplan–Meier curves showing cumulative survival (3 months vital status) by Quetelet's body mass index (BMI) categories. (A) Total. (B) Dialysis. (C) Those living with kidney transplant.
Table 2.
Association of Quetelet's body mass index (BMI) with 3 months vital status in total population and by type of kidney function replacement therapy
| BMI categories | |||||
|---|---|---|---|---|---|
| Lean <18.5 | Normal 18.5–24.9 | Overweight 25–29.9 | Obese I 30–34.9 | Obese II/III ≥35 | |
| Total (N = 3160) | (N = 99) | (N = 1151) | (N = 1160) | (N = 525) | (N = 225) |
| Events, n (%) | 28 (28.3) | 232 (20.2) | 244 (21.0) | 121 (23.0) | 60 (26.7) |
| Model 1 | 1.47 (1.00, 2.18) | Ref. | 1.05 (0.88, 1.26) | 1.16 (0.93, 1.44) | 1.40 (1.06, 1.86) |
| Model 2 | 1.82 (1.23, 2.70) | Ref. | 1.06 (0.89, 1.27) | 1.22 (0.98, 1.52) | 1.94 (1.45, 2.59) |
| Model 3 | 1.87 (1.26, 2.77) | Ref. | 1.06 (0.88, 1.26) | 1.20 (0.97, 1.50) | 1.97 (1.47, 2.63) |
| Model 4 | 1.96 (1.32, 2.92) | Ref. | 1.05 (0.87, 1.26) | 1.15 (0.92, 1.45) | 1.88 (1.40, 2.53) |
| Model 5 | 1.65 (1.10, 2.47) | Ref. | 1.07 (0.89, 1.28) | 1.17 (0.93, 1.46) | 1.71 (1.27, 2.30) |
| Dialysis (N = 2343) | (N = 82) | (N = 874) | (N = 838) | (N = 382) | (N = 167) |
| Events, n (%) | 24 (29.3) | 189 (21.6) | 184 (22.0) | 90 (23.6) | 45 (27.0) |
| Model 1 | 1.41 (0.92, 2.15) | Ref. | 1.03 (0.84, 1.26) | 1.10 (0.86, 1.41) | 1.30 (0.94, 1.80) |
| Model 2 | 1.83 (1.19, 2.80) | Ref. | 1.02 (0.83, 1.25) | 1.17 (0.91, 1.51) | 1.87 (1.34, 2.61) |
| Model 4 | 1.94 (1.26, 2.98) | Ref. | 1.02 (0.83, 1.25) | 1.16 (0.89, 1.50) | 1.86 (1.33, 2.61) |
| Model 5 | 1.68 (1.08, 2.61) | Ref. | 1.03 (0.83, 1.26) | 1.13 (0.87, 1.47) | 1.67 (1.18, 2.34) |
| Transplant (N = 817) | (N = 17) | (N = 277) | (N = 322) | (N = 143) | (N = 58) |
| Events, n (%) | 4 (23.5) | 43 (15.5) | 60 (18.6) | 31 (21.7) | 15 (25.9) |
| Model 1 | 1.64 (0.59, 4.56) | Ref. | 1.21 (0.82, 1.78) | 1.44 (0.91, 2.29) | 1.87 (1.04, 3.37) |
| Model 2 | 1.60 (0.57, 4.53) | Ref. | 1.16 (0.79, 1.72) | 1.23 (0.78, 1.95) | 2.07 (1.14, 3.76) |
| Model 4 | 1.54 (0.54, 4.38) | Ref. | 1.11 (0.75, 1.64) | 1.11 (0.69, 1.77) | 1.84 (0.99, 3.41) |
| Model 5 | 1.16 (0.40, 3.39) | Ref. | 1.17 (0.79, 1.74) | 1.22 (0.75, 1.96) | 1.79 (0.96, 3.34) |
Model 1: crude.
Model 2: age, sex.
Model 3: model 2 + type of kidney function replacement therapy (expect when analyzing dialysis patients/kidney transplant recipients separately).
Model 4: model 3 + hypertension, diabetes, coronary artery disease, chronic lung disease, heart failure, smoking.
Model 5: model 4 + frailty.
FIGURE 2:
Association of Quetelet's BMI with 3 months vital status among patients on kidney function replacement therapy with COVID-19 (presented results are from Model 5*). *Model 5: adjusted for age, sex, type of kidney function replacement therapy (except when analyzing dialysis patients/those living with kidney transplant separately), hypertension, diabetes, coronary artery disease, chronic lung disease, heart failure, smoking, frailty.
Association of BMI with hospitalization, ICU admission and in-hospital mortality
The association between BMI and hospitalization rate was not statistically significant in the total study population, nor in dialysis patients or transplant recipients when analyzed separately (Supplementary data, Table S3). The chance to be admitted to an ICU was higher with increasing BMI, with similar results among dialysis patients and transplant recipients (Pinteraction = 0.37) (Supplementary data, Table S4). Results for in-hospital mortality were essentially similar to the results for overall mortality (Supplementary data, Table S5).
Additional analyses
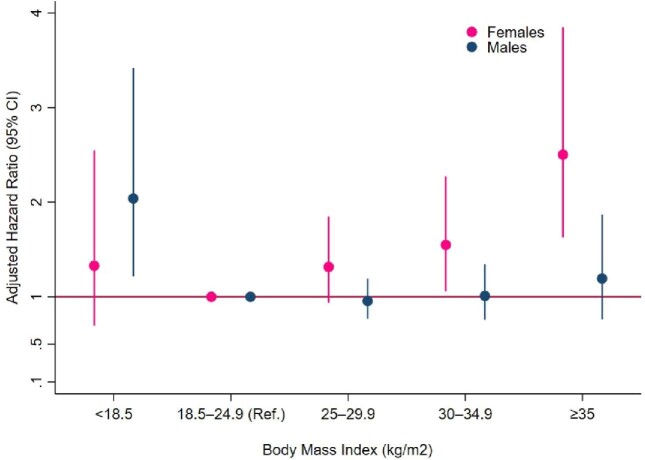
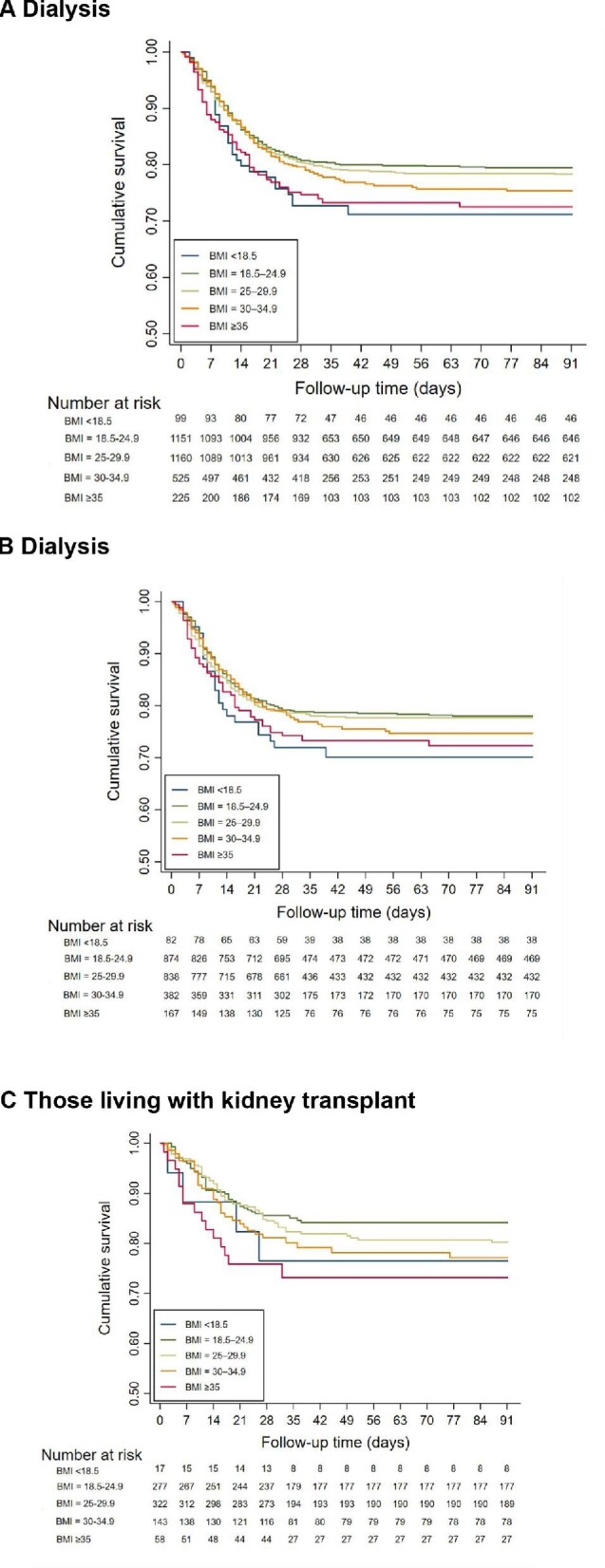
The association between obesity class II/III (versus normal weight) and 3-month mortality was consistent across all examined subgroups except for sex (Figure 3). In general, Kaplan-Meier-curves demonstrated the lowest cumulative survival in the underweight category among men and in the obese class II/III category in women (Supplementary data, Figure S2). Obesity class II/III was significantly associated with 3-month mortality among females but not in males (Pinteraction = 0.019 in the fully adjusted model) (Figures 3 and 4, Table 3). The association between BMI (continuous) and mortality indicated a consistent increase in the risk of mortality in patients with BMI >28 kg/m2 (Supplementary data, Figure S3). Among men, the risk appeared to increase from BMI >28 kg/m2 and in women from BMI >25 kg/m2 (Supplementary data, Figure S3). No interaction was observed between BMI and sex for the risk of ICU admission (Pinteraction = 0.44) (Supplementary data, Table S5). Results for 28-day mortality were essentially similar to the results for 3-month mortality (Supplementary data, Tables S7 and S8). A total of 640 patients (18.1%) had missing information on BMI, who were predominantly Caucasian males and were less likely to have comorbidities compared with those having information on BMI (Supplementary data, Table S9). Results after imputing missing values corroborated our overall findings (Supplementary data, Table S10).
FIGURE 3:
Association of Quetelet's BMI (≥35 kg/m2 versus 18.5–24.9 kg/m2) with 3 months vital status across subgroups. RRT, renal replacement therapy/kidney function replacement therapy; p-int., P for interaction.
FIGURE 4:
Association of Quetelet's BMI with 3 months vital status by sex (presented results are from Model 5*). *Model 5: adjusted for age, sex, type of kidney function replacement therapy (expect when analyzing dialysis patients/those living with kidney transplant separately), hypertension, diabetes, coronary artery disease, chronic lung disease, heart failure, smoking, frailty.
Table 3.
Association of Quetelet's body mass index (BMI) with 3 months vital status in males and females
| BMI categories | |||||
|---|---|---|---|---|---|
| Lean <18.5 | Normal 18.5–24.9 | Overweight 25–29.9 | Obese I 30–34.9 | Obese II/III ≥35 | |
| Females (N = 1229) | (N = 52) | (N = 447) | (N = 384) | (N = 220) | (N = 126) |
| Events, n (%) | 11 (21.1) | 66 (14.8) | 74 (19.3) | 51 (23.2) | 36 (28.6) |
| Model 1 | 1.48 (0.78, 2.81) | Ref. | 1.33 (0.96, 1.86) | 1.62 (1.12, 2.33) | 2.11 (1.40, 3.16) |
| Model 2 | 1.61 (0.85, 3.05) | Ref. | 1.37 (0.98, 1.91) | 1.67 (1.16, 2.40) | 2.70 (1.78, 4.08) |
| Model 3 | 1.60 (0.84, 3.03) | Ref. | 1.34 (0.96, 1.87) | 1.63 (1.13, 2.35) | 2.73 (1.80, 4.13) |
| Model 4 | 1.57 (0.82, 2.99) | Ref. | 1.33 (0.95, 1.87) | 1.51 (1.03, 2.22) | 2.70 (1.76, 4.13) |
| Model 5 | 1.34 (0.70, 2.57) | Ref. | 1.31 (0.94, 1.85) | 1.54 (1.05, 2.26) | 2.49 (1.62, 3.84) |
| Males (N = 1931) | (N = 47) | (N = 704) | (N = 776) | (N = 305) | (N = 99) |
| Events, n (%) | 17 (36.2) | 166 (23.6) | 170 (21.9) | 70 (22.9) | 24 (24.2) |
| Model 1 | 1.66 (1.01, 2.73) | Ref. | 0.93 (0.75, 1.15) | 0.97 (0.74, 1.29) | 1.06 (0.69, 1.63) |
| Model 2 | 2.21 (1.34, 3.64) | Ref. | 0.95 (0.77, 1.18) | 1.02 (0.77, 1.35) | 1.45 (0.94, 2.23) |
| Model 3 | 2.29 (1.39, 3.77) | Ref. | 0.95 (0.76, 1.17) | 1.02 (0.77, 1.35) | 1.47 (0.95, 2.26) |
| Model 4 | 2.44 (1.47, 4.05) | Ref. | 0.94 (0.75, 1.17) | 0.99 (0.75, 1.32) | 1.38 (0.88, 2.14) |
| Model 5 | 2.07 (1.22, 3.52) | Ref. | 0.97 (0.78, 1.21) | 0.99 (0.74, 1.33) | 1.22 (0.78, 1.91) |
Model 1: crude.
Model 2: age.
Model 3: model 2 + type of kidney function replacement therapy.
Model 4: model 3 + hypertension, diabetes, coronary artery disease, chronic lung disease, heart failure, smoking.
Model 5: model 4 + frailty.
DISCUSSION
In this large cohort of patients on KFRT with COVID-19, we showed an independent association between obesity and increased risk of mortality. This association was consistent among dialysis patients and those living with a kidney transplant. Interestingly, the association was different among males and females, such that the risk of mortality associated with obesity versus normal weight was higher in females compared with males.
Several previous studies have reported an association between obesity and increased risk of COVID-19-related complications including mortality in the general population with COVID-19 [11–20]. To our knowledge, the present study is the first to report comprehensively on the obesity–mortality relationship among patients on KFRT with COVID-19. In our study, compared with the WHO-defined category of normal weight, obesity class II/III was associated with an increased risk of mortality. Of note, when the association between BMI and mortality was investigated on a continuous scale, the risk of mortality appeared to increase from a BMI over approximately 28 kg/m2. An increased mortality risk above a BMI of approximately 28 kg/m2 has also been observed in a meta-analysis of 28 studies (N = 112 682) among the general population with COVID-19 [21] and in a large study (N ∼6.9 million) investigating the association between BMI and COVID-19-related complications in the general population [22]. These studies in the general population also reported increased mortality risk at low BMI as in our study. Consequently, the results observed in our study are in line with the previous studies in the general population, but in contrast to the often observed ‘obesity paradox’ among patients on KFRT. Especially obese dialysis patients are at lower long-term non-COVID-19 mortality risk when compared with dialysis patients with normal weight [2]. The reversal of the ‘obesity paradox’ among patients on KFRT with COVID-19 could be related to several factors. First, the influence of obesity on mortality may differ in acute versus chronic diseases. Patients on KFRT that are in poor physical condition due to an underlying illness often lose weight. Thus, obesity may reflect the absence of debilitating disorders and therefore contribute to better long-term outcomes of chronic conditions, such as cardiovascular diseases [23]. However, COVID-19 is an acute viral illness and causes rapid clinical outcomes. Therefore, the survival advantage associated with obesity among patients on KFRT may not be seen when these patients suffer from COVID-19, as this occurs especially in the long term. Second, intubation, positioning and movement may be difficult among seriously ill patients with obesity which may complicate patients’ recovery from COVID-19 [24].
Men and women exhibited a difference in the BMI–mortality relationship in our study. Previously, a large study (N = 502 493) in subjects from the general population with COVID-19, and another study in hospitalized COVID-19 patients, showed similar results regarding COVID-19-related mortality [25, 26]. Also, these studies indicated an increase in mortality with increasing obesity in women, but not in men. The exact reason for the observed difference in the BMI–mortality relationship between men and women is not fully clear to us, though it may be related to sex differences in the anatomy of the lungs and abdominal cavity [27, 28] which may cause difficulty in breathing in presence of obesity [1]. It may also be that in a population like ours, ‘normal weight’ among men is in part a consequence of increased comorbidity burden in men who would have been (slightly) obese if not suffering from comorbidity. Accordingly, when the association between BMI (continuous) and the risk of mortality was investigated for both sexes separately, in men the risk of mortality did not appear to be lowest among those with BMI in the ‘normal weight’ range as is the case in women. To our knowledge, such a difference in the association of BMI with mortality has not been observed in the general population with COVID-19.
Of note, in our study, the absolute COVID-19 mortality rate in obese men and women was similar, whereas the absolute COVID-19 mortality rate in the normal-weight category was almost two-fold higher in men compared with women. This questions whether the sex difference in our results should be interpreted as excess relative mortality in obese women when compared with obese men, or more as a higher absolute mortality rate in normal-weight men when compared with normal-weight women. Putting more emphasis on this latter finding is supported by the fact that there are far more people with normal weight in our cohort (N = 1160) than with obesity class II/III (N = 225). Future studies are required to better understand the reasons for the observed sex difference in the BMI–mortality relationship in our study.
The most important strength of our study is that it reports on a large dataset with detailed information on patients’ demographics, comorbidities, reasons for COVID-19 testing, disease characteristics including symptoms and laboratory test results. This allowed accounting for known confounders in the BMI–mortality relationship and examination of results across key clinical subgroups, thereby allowing a comprehensive assessment of the BMI–mortality relationship among patients on KFRT with COVID-19. However, this study also has limitations. First, patients who presented with COVID-19 may not be representative of the overall population of KFRT patients with COVID-19 which may limit the generalizability of our findings. However, it is worth noting that case-fatality rates observed in our study are comparable to those reported in other studies from patients on KFRT with COVID-19 [4, 29–33]. Second, a significant proportion of patients (18.1%) had missing information on BMI. These patients were predominantly Caucasian males and were less likely to have comorbidities than patients in the cohort with information on BMI (Supplementary data, Table S7). In a sensitivity analysis that included these patients after multiple imputations, we found no difference in the observed associations compared with our main findings. Third, because BMI is associated with disease severity and patients with severe symptoms were more likely to be tested for COVID-19, especially early in the COVID-19 pandemic, there may be a possibility of collider bias [34]. Importantly, we had information on the reason for COVID-19 testing. No heterogeneity was observed in the association between obesity and mortality when patients who were identified through routine screening and those who were identified because of symptoms were analyzed separately, suggesting that this type of bias has no major role.
CONCLUSION
In conclusion, this study shows that among patients on KFRT with COVID-19, dialysis patients as well as transplant recipients, obesity is associated with an increased risk of mortality. This is in contrast to the obesity paradox generally observed in dialysis patients. The association of obesity with COVID-19 mortality may be different in men and women, which requires further study, including investigation of potential reasons for this difference.
Supplementary Material
ACKNOWLEDGEMENTS
We thank all people that entered information in the ERACODA database for their participation and especially all healthcare workers that have taken care of the included COVID-19 patients.
APPENDIX
ERACODA collaborators
The ERACODA collaboration is an initiative to study prognosis and risk factors for mortality due to COVID-19 in patients with a kidney transplant or on dialysis that is endorsed by the European Renal Association (ERA). ERACODA is an acronym for European Renal Association COVID-19 Database. The organizational structure contains a Working Group assisted by a Management Team and an Advisory Board.
The ERACODA Working Group members: Franssen CFM, Gansevoort RT (coordinator), Hemmelder MH, Hilbrands LB and Jager KJ.
The ERACODA Management Team members: Duivenvoorden R, Noordzij M and Vart P.
The ERACODA Advisory Board members: Abramowicz D, Basile C, Covic A, Crespo M, Massy ZA, Mitra S, Petridou E, Sanchez JE and White C.
Names and affiliations of collaborative authors
Albert Schweitzer Hospital, Dordrecht, the Netherlands
- Jeroen B. van der Net, M.D., Ph.D.
Ambroise Pare Hospital, APHP Paris-Saclay University, Boulogne Billancourt, France
- Marie Essig, M.D., Ph.D.
Amphia Hospital, Breda, the Netherlands
- Peggy W.G. du Buf-Vereijken, M.D., Ph.D.
- Betty van Ginneken
- Nanda Maas
Amsterdam UMC, Amsterdam, the Netherlands
- Brigit C. van Jaarsveld, M.D, Ph.D.
- Frederike J. Bemelman, M.D, Ph.D.
- Farah Klingenberg-Salahova, M.D.
- Frederiek Heenan-Vos, M.D., Ph.D.
- Marc G. Vervloet, M.D., Ph.D.
- Azam Nurmohamed, M.D., Ph.D.
- Liffert Vogt, M.D., Ph.D.
Antwerp University Hospital, Antwerp, Belgium
- Daniel Abramowicz, M.D., Ph.D
- Sabine Verhofstede
Avicennes Military Hospital, Faculty of Medicine, Cadi Ayyad University, Marrakech Morocco
- Omar Maoujoud, M.D., Ph.D.
AZ Delta, Roeselare, Belgium
-Thomas Malfait, M.D.
B. Braun Avitum, Litomerice, Czech Republic
- Jana Fialova, M.D.
Bellvitge University Hospital, Hospitalet de Llobregat, Barcelona, Spain
- Edoardo Melilli, M.D., Ph.D.
- Alexandre Favà, M.D.
- Josep M. Cruzado, M.D., Ph.D.
- Nuria Montero Perez, M.D., Ph.D.
Bernhoven Hospital, Uden, the Netherlands
- Joy Lips, M.D.
Bravis Hospital, Roosendaal/Bergen op Zoom, the Netherlands
- Harmen Krepel, M.D., Ph.D.
Cantonal Hospital Zenica, Bosnia and Herzegovina
- Harun Adilovic, M.D.
‘Carol Davila’ University of Medicine and Pharmacy, Bucharest, Romania/Emergency Clinical Hospital ‘Sf. Ioan’
- Daniela Radulescu, M.D., Ph.D.
Catharina Hospital, Eindhoven, the Netherlands
- Maaike Hengst, M.Sc.
Central Clinical Hospital of the Ministry of Interior, Warsaw, Poland
- Andrzej Rydzewski, M.D., Ph.D.
Centre Hospitalier du Nord, Luxembourg
- Philippe Braconnier, M.D.
- Daniel Weis, M.D.
Centre of Postgraduate Medical Education, Poland
- Ryszard Gellert, M.D., Ph.D.
Centrodial, São João da Madeira, Portugal
-João Oliveira, M.D., Ph.D
Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal
- Daniela G. Alferes, M.D.
City Hospital n.a. S.P. Botkin, Moscow, Russia
- Elena V. Zakharova, M.D., Ph.D.
City Hospital Zürich, Switzerland
- Patrice Max Ambuehl, M.D., Ph.D.
- Andrea Walker
Claude Galien Hospital Ramsay santé, Quincy-sous-Sénart, France
- Fanny Lepeytre, M.D.
- Clémentine Rabaté, M.D.
- Guy Rostoker, M.D., Ph.D.
Clínica de Hemodiálise de Felgueiras, Felgueiras, Portugal
- Sofia Marques, M.D.
Clinical Centre of Vojvodina, Novi Sad, Serbia
- Tijana Azasevac, M.D.
- Gordana Strazmester Majstorovic, M.D.
CWZ Nijmegen, Nijmegen, the Netherlands
- Marc ten Dam, M.D.
DaVita Geilenkirchen, Geilenkirchen, Germany
- Thilo Krüger, M.D., Ph.D.
DaVita, Wrocław, Poland
- Szymon Brzosko, M.D., Ph.D
1st Department of Internal Medicine, Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
- Vassilios Liakopoulos, M.D., Ph.D.
Deventer Ziekenhuis, Deventer, the Netherlands
- Adriaan L. Zanen, M.D.
Dianet Dialysis Center, Utrecht, the Netherlands
- Susan J.J. Logtenberg, M.D., Ph.D.
Dialysis Center Bochum, Bochum, Germany
- Lutz Fricke, M.D., Ph.D.
Dnipro State Medical University, Dnipro, Ukraine
- Olexandr Kuryata, M.D., Ph.D.
Elyse Klinieken voor Nierzorg, Kerkrade, the Netherlands
- Jeroen J.P. Slebe, M.D.
Epidemiology Department- High Institute of Public Health- Alexandria University, Egypt
- Samar Abd ElHafeez, M.D., DrPH
Erasme Hospital, Brussels, Belgium
- Delphine Kemlin
Erasmus MC Transplant Institute, Department of Internal Medicine, University Medical Center Rotterdam, Rotterdam, the Netherlands
- Jacqueline van de Wetering, M.D., Ph.D.
- Marlies E.J. Reinders, M.D., Ph.D.
- Dennis A. Hesselink, M.D., Ph.D.
- J. Kal- van Gestel, M.Sc.
Faculty of Medicine in Pilsen, Charles University, Pilsen, Czech Republic
- Jaromir Eiselt
- Lukas Kielberger
Faculty of Medicine-Alexandria University, Alexandria, Egypt
- Hala S. El-Wakil, M.D., Ph.D.
Freeman Hospital, Newcastle upon Tyne, United Kingdom
-Ian Logan, M.D.
Fundació Puigvert, Barcelona, Spain
- Cristina Canal, M.D., Ph.D.
- Carme Facundo, M.D., Ph.D.
Fundación Jiménez Díaz, Madrid, Spain
- Ana M. Ramos, M.D., Ph.D.
Gdansk Medical University, Gdansk, Poland
- Alicja Debska-Slizien, M.D., Ph.D.
Gelre Hospital, Apeldoorn, the Netherlands
- Nicoline M.H. Veldhuizen, M.D.
General hospital of Athens ‘G. Gennimatas’, Athens, Greece
- Eirini Tigka
General Hospital of Serres, Serres, Greece
- Maria Anna Polyzou Konsta, M.D.
General University Hospital of Alexandroupolis, Alexandroupolis, Greece
- Stylianos Panagoutsos
Grande Ospedale Metropolitano and CNR, Reggio Calabria, Italy
- Francesca Mallamaci, M.D.
- Adele Postorino, M.D.
- Francesco Cambareri, M.D.
Grigore T Popa University of Medicine and Pharmacy, Iasi, Romania/Dr Ci Parhon Hospital, Iasi, Romania
- Irina Matceac, M.D.
- Adrian Covic, M.D., Ph.D.
Haaglanden Medisch Centrum, the Hague, the Netherlands
- J.H.M Groeneveld, M.D.
- Jolanda Jousma
Haga Hospital, the Hague, the Netherlands
- Marjolijn van Buren, M.D., Ph.D.
Hospital Clínic de Barcelona, Barcelona, Spain
- Fritz Diekmann, M.D., Ph.D.
- Federico Oppenheimer, M.D., Ph.D.
- Miquel Blasco, M.D.
Hospital Curry Cabral—Central Lisbon University Hospital Center, Lisbon, Portugal
- Tiago Assis Pereira, M.D.
Hospital das Clinicas, Universidade Federal de Minas Gerais, Brazil
- Augusto Cesar S. Santos Jr, M.D., Ph.D.
Hospital del Mar, Barcelona, Spain
- Carlos Arias-Cabrales, M.D., Ph.D.
- Marta Crespo, M.D., Ph.D.
- Laura Llinàs-Mallol, MSc., Ph.D.
- Anna Buxeda, M.D.
- Carla Burballa Tàrrega, M.D., Ph.D.
- Dolores Redondo-Pachon, M.D., Ph.D.
- Maria Dolores Arenas Jimenez, M.D.
- Alberto Mendoza-Valderrey, Ph.D.
Hospital de Santa Cruz, Centro Hospitalar de Lisboa Ocidental, Lisbon
- Ana Cristina Martins
- Catarina Mateus
- Goncalo Alvila
- Ivo Laranjinha, M.D.
Hospital Gelderse Vallei, Ede, the Netherlands
- Julia M. Hofstra, M.D., Ph.D.
- Machiel A. Siezenga, M.D., Ph.D.
Hospital General of Alicante, Alicante, Spain
- Antonio Franco
Hospital General Universitario Gregorio Marañón, Madrid, Spain
- David Arroyo, M.D., Ph.D.
- Sandra Castellano, M.D.
Hospital Obispo Polanco, Salud Aragón, Spain
- Sagrario Balda Manzanos, M.D., Ph.D.
Hospital Universitario Ramón y Cajal, Madrid, Spain
- R. Haridian Sosa Barrios, M.Sc.
Imelda Hospital, Bonheiden, Belgium
- Wim Lemahieu, M.D., Ph.D.
Isala, Zwolle, the Netherlands
- Karlijn Bartelet, M.D.
Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey
- Ahmet Burak Dirim, M.D.
- Erol Demir, M.D.
- Mehmet Sukru Sever, M.D.
- Aydin Turkmen, M.D.
- Seda Şafak, M.D.
Jeroen Bosch Ziekenhuis, Den Bosch, the Netherlands
- Daan A.M.J. Hollander, M.D., Ph.D.
Klinikum Aschaffenburg-Alzenau, Aschaffenburg, Germany
- Stefan Büttner, M.D.
Leiden University Medical Center, Leiden, the Netherlands
- Soufian Meziyerh, M.D.
- Danny van der Helm, Ph.D.
- Marko Mallat, Ph.D.
- Hanneke Bouwsma, M.D.
Lister Hospital, Stevenage, United Kingdom
- Sivakumar Sridharan, Ph.D.
Lithuanian University of Health Sciences, Lithuania
- Kristina Petruliene, M.D., Ph.D.
Luzerner Kantonsspital, Luzern, Switzerland
- Sharon-Rose Maloney, M.D.
Maasstad Ziekenhuis, Rotterdam, the Netherlands
- Iris Verberk, M.D., Ph.D.
Maastricht University Medical Center, Maastricht, the Netherlands
- Frank M. van der Sande, M.D., Ph.D.
- Maarten H.L Christiaans, M.D., Ph.D.
- Marc H. Hemmelder, M.D., Ph.D.
Manipal Hospital, Manipal, India
- Mohan Kumar N.
Marche Nord Hospital, Pesaro, Italy
- Marina Di Luca, M.D., Ph.D.
Marmara University School of Medicine, Istanbul, Turkey
- Serhan Z. Tuğlular, M.D.
Martini Ziekenhuis, Groningen, the Netherlands
- Andrea B. Kramer, M.D., Ph.D.
Maxima Medisch Centrum, Veldhoven, the Netherlands
- Charles Beerenhout, M.D., Ph.D.
Meander Medisch Centrum, Amersfoort, the Netherlands
- Peter T. Luik, M.D., Ph.D.
Medical University Innsbruck, Innsbruck, Austria
- Julia Kerschbaum, M.D. (Austrian Dialysis and Transplant Registry)
- Martin Tiefenthaler, M.D.
Medical University of Vienna, Vienna, Austria
- Bruno Watschinger, M.D.
Medisch Centrum Leeuwarden, Leeuwarden, the Netherlands
- Aaltje Y. Adema, M.D., Ph.D.
Moscow Regional Research and Clinical Institute, Moscow, Russia
- Vadim A. Stepanov, M.D., Ph.D.
- Alexey B. Zulkarnaev, M.D., Ph.D
Necmettin Erbakan University Meram School of Medicine, Konya, Turkey
- Kultigin Turkmen, M.D.
Nephrology Unit, Department of Medicine and Surgery, University of Parma, Parma, Italy
- Ilaria Gandolfini, M.D.
- Umberto Maggiore, M.D.
Nierenzentrum Reutlingen-Tübingen, Reutlingen, Germany
- Anselm Fliedner, M.D.
Norwegian Renal Registry, Oslo University Hospital, Rikshospitalet, Olso, Norway
- Anders Åsberg, Ph.D.
- Geir Mjoen, Ph.D.
Okinawa Chubu Hospital, Japan
- Hitoshi Miyasato
OLVG, Amsterdam, the Netherlands
- Carola W.H. de Fijter, M.D., Ph.D.
Ospedale S. Maurizio Bolzano, Bolzano, Italy
- Nicola Mongera, M.D.
Padua University Hospital, Padua, Italy
- Stefano Pini, M.D.
Radboud University Medical Center, Nijmegen, the Netherlands
- Consuelo de Biase, M.D.
- Angele Kerckhoffs, M.D., Ph.D.
- Anne Els van de Logt, M.D.
- Rutger Maas, M.D., Ph.D.
- Raphaël Duivenvoorden, M.D., Ph.D.
Regional Clinical Hospital, Yaroslavl, Russia
- Olga Lebedeva, M.D.
Regional Hospital of Malaga, Malaga, Spain
- Veronica Lopez, M.D., Ph.D.
Rijnstate Hospital, Arnhem, the Netherlands
- Louis J.M. Reichert, M.D., Ph.D.
- Jacobien Verhave, M.D., Ph.D.
RUDN University, Russia
- Denis Titov
Saint-Petersburg State University Hospital, Saint-Petersburg, Russia
- Ekaterina V. Parshina, M.D.
San Marco Hospital, University of Catania, Catania, Italy
- Luca Zanoli, M.D., Ph.D.
- Carmelita Marcantoni, M.D.
Saxenburgh Medisch Centrum, Hardenberg, the Netherlands
-Gijs van Kempen, M.D.
Sint Antonius Ziekenhuis, Nieuwegein, the Netherlands
- Liesbeth E.A. van Gils-Verrij, M.D.
Southern Health and Social Care Trust, Newry, Northern Ireland
- John C. Harty, M.D.
Spaarne Gasthuis, Haarlem, the Netherlands
- Marleen Meurs, M.D.
SPWSZ Hospital, Szczecinie, Poland
- Marek Myslak
St. Anna University Hospital, Ferrara, Italy
- Yuri Battaglia, M.D., Ph.D.
St. Bassiano Hospital, Bassano del Grappo, Italy
- Paolo Lentini, M.D., Ph.D.
Streekziekenhuis Koningin Beatrix, Winterswijk, the Netherlands
- Edwin den Deurwaarder, M.D.
Swedish Renal Registry, Jönköping, Sweden
-Maria Stendahl, M.D., Ph.D.
Tehran University of Medical Sciences, Tehran, Iran
- Hormat Rahimzadeh, M.D.
Tergooi MC, Hilversum, the Netherlands
- Marcel Schouten, M.D., Ph.D.
Third Faculty of Medicine, Charles University, and Faculty Hospital Kralovske Vinohrady, Prague, Czech Republic
- Ivan Rychlik, M.D., Ph.D
Toledo University Hospital, Toledo, Spain
- Carlos J. Cabezas-Reina, M.D.
- Ana Maria Roca, M.D.
Treant/Scheper Ziekenhuis, Emmen, the Netherlands
- Ferdau Nauta, M.D., Ph.D.
Turgut Ozal Medical Center, Malatya, Turkey
- İdris Sahin, M.D.
Université Catholique de Louvain, Cliniques Universitaires St Luc, Brussels, Belgium
- Eric Goffin, M.D.
- Nada Kanaan, M.D.
- Laura Labriola, M.D.
- Arnaud Devresse, M.D., Ph.D.
University Clinical Hospital of Santiago de Compostela, Santiago de Compostela, Spain
- Anabel Diaz-Mareque, M.D.
University Clinical Hospital of Valladolid, Valladolid, Spain
- Armando Coca, M.D., Ph.D.
Universitary Hospital of Guadalajara, Guadalajara, Spain
- Gabriel de Arriba, M.D., Ph.D.
University Hospital Leuven, Leuven, Belgium
- Björn K.I. Meijers, M.D., Ph.D.
- Maarten Naesens, M.D., Ph.D.
- Dirk Kuypers, M.D., Ph.D.
- Bruno Desschans
University Hospital Brussels, Brussels, Belgium
- Annelies Tonnerlier
- Karl M. Wissing
University Hospital Martin and Jessenius Faculty of Medicine Comenius University, Martin, Slovakia
- Ivana Dedinska, M.D., Ph.D.
University Hospital Medical Center Verona, Verona, Italy
- Giuseppina Pessolano, M.D.
University Hospitals of Coventry and Warwickshire NHS Trust, Coventry, United Kingdom
- Shafi Malik, M.D.
University Hospital of Ioannina, Ioannina, Greece
- Evangelia Dounousi, M.D., Ph.D.
University Hospital of Patras, Patras, Greece
- Evangelos Papachristou, M.D., Ph.D.
University Medical Center Groningen, Groningen, the Netherlands
- Stefan P. Berger, M.D., Ph.D.
- Esther Meijer, M.D., Ph.D.
- Jan Stephan F. Sanders, M.D., Ph.D.
- Casper F.M. Franssen, M.D., Ph.D.
- Akin Özyilmaz, M.D., Ph.D. (Dialysis Center Groningen)
University Medical Center Ljubljana, Ljubljana, Slovenia
- Jadranka Buturović Ponikvar, M.D., Ph.D.
- Andreja Marn Pernat, M.D.
- Damjan Kovac, M.D., Ph.D.
- Miha Arnol, M.D., Ph.D
University Medical Centre Maribor, Maribor, Slovenia
-Robert Ekart, M.D., Ph.D.
University Medical Center Utrecht, Utrecht, the Netherlands
- Alferso C. Abrahams, M.D., Ph.D.
- Arjan D. van Zuilen, M.D., Ph.D.
- Sabine C.A. Meijvis, M.D., Ph.D.
- Helma Dolmans
University of Genoa, Genoa, Italy
- Pasquale Esposito, M.D., Ph.D.
University of Liège, Liège, Belgium
- Jean-Marie Krzesinski, M.D., Ph.D.
- Jean Damacène Barahira, MPH
University of Milan, Milan, Italy
- Maurizio Gallieni, M.D.
University of Navarra Clinic, Pamplona, Spain
- Paloma Leticia Martin-Moreno
University of Piemonte Orientale, Novara, Italy
- Gabriele Guglielmetti, M.D.
Valais Hospital, Sion & Lausanne University Hospital, Lausanne, Switzerland
- Gabriella Guzzo, M.D.
Vall d'Hebron University Hospital, Barcelona, Spain
- Nestor Toapanta, M.D.
- Maria Jose Soler, M.D., PhD
VieCuri Medical Centre, Venlo, the Netherlands
- Antinus J. Luik, M.D., Ph.D.
- Willi H.M. van Kuijk, M.D., Ph.D.
- Lonneke W.H. Stikkelbroeck, M.D.
- Marc M.H. Hermans, M.D., Ph.D.
Vilnius University, Vilnius, Lithuania
- Laurynas Rimsevicius, M.D., Ph.D.
Vimercate Hospital, Vimercate, Italy
- Marco Righetti, M.D.
Zuyderland Medical Center, Geleen and Heerlen, the Netherlands
- Nicole Heitink-ter Braak, M.D.
Contributor Information
Ekamol Tantisattamo, Harold Simmons Center for Kidney Disease Research and Epidemiology, Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine School of Medicine, Orange, CA, USA.
Celine Imhof, Department of Internal Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Kitty J Jager, ERA Registry, Department of Medical Informatics, Amsterdam University Medical Center, Amsterdam Public Health Research Institute, Amsterdam, The Netherlands.
Luuk B Hilbrands, Department of Nephrology, Radboud University Medical Center, Nijmegen, The Netherlands.
Rebecca Guidotti, Institute of Nephrology, City Hospital Waid and Triemli, Zurich, Switzerland.
Mahmud Islam, Zonguldak Ataturk state hospital, Zonguldak, Turkey.
Dajana Katicic, Croatian Society of Nephrology, Dialysis and Transplantation, Croatia.
Constantijn Konings, Catharina Ziekenhuis, Eindhoven, The Netherlands.
Femke M Molenaar, University Medical Center Utrecht, Utrecht, The Netherlands.
Ionut Nistor, Faculty of Medicine, University of Medicine and Pharmacy, Grigore T.Popa, Iași, Romania.
Marlies Noordzij, Department of Internal Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
María Luisa Rodríguez Ferrero, Department of Nephrology, Hospital General Universitario Gregorio Marañon, Madrid, Spain.
Martine A M Verhoeven, Franciscus Gashuis & Vlietalnd, Schiedam, The Netherlands.
Aiko P J de Vries, Leiden University Medical Center, Leiden, The Netherlands.
Kamyar Kalantar-Zadeh, Harold Simmons Center for Kidney Disease Research and Epidemiology, Division of Nephrology, Hypertension and Kidney Transplantation, Department of Medicine, University of California Irvine School of Medicine, Orange, CA, USA.
Ron T Gansevoort, Department of Internal Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Priya Vart, Department of Internal Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
ERACODA collaborators:
Jeroen B van der Net, Marie Essig, Peggy W G du Buf-Vereijken, Betty van Ginneken, Nanda Maas, Brigit C van Jaarsveld, Frederike J Bemelman, Farah Klingenberg-Salahova, Frederiek Heenan-Vos, Marc G Vervloet, Azam Nurmohamed, Liffert Vogt, Daniel Abramowicz, Sabine Verhofstede, Omar Maoujoud, Thomas Malfait, Jana Fialova, Edoardo Melilli, Alexandre Favà, Josep M Cruzado, Nuria Montero Perez, Joy Lips, Harmen Krepel, Harun Adilovic, Daniela Radulescu, Maaike Hengst, Andrzej Rydzewski, Philippe Braconnier, Daniel Weis, Ryszard Gellert, João Oliveira, Daniela G Alferes, Elena V Zakharova, Patrice Max Ambuehl, Andrea Walker, Fanny Lepeytre, Clémentine Rabaté, Guy Rostoker, Sofia Marques, Tijana Azasevac, Gordana Strazmester Majstorovic, Marc ten Dam, Thilo Krüger, Szymon Brzosko, Vassilios Liakopoulos, Adriaan L Zanen, Susan J J Logtenberg, Lutz Fricke, Olexandr Kuryata, Jeroen J P Slebe, Samar Abd ElHafeez, Delphine Kemlin, Jacqueline van de Wetering, Marlies E J Reinders, Dennis A Hesselink, J Kal-van Gestel, Jaromir Eiselt, Lukas Kielberger, Hala S El-Wakil, Ian Logan, Cristina Canal, Carme Facundo, Ana M Ramos, Alicja Debska-Slizien, Nicoline M H Veldhuizen, Eirini Tigka, Maria Anna Polyzou Konsta, Stylianos Panagoutsos, Francesca Mallamaci, Adele Postorino, Francesco Cambareri, Irina Matceac, Adrian Covic, J H M Groeneveld, Jolanda Jousma, Marjolijn van Buren, Fritz Diekmann, Federico Oppenheimer, Miquel Blasco, Tiago Assis Pereira, Augusto Cesar S Santos, Jr, Carlos Arias-Cabrales, Marta Crespo, Laura Llinàs-Mallol, Anna Buxeda, Carla Burballa Tàrrega, Dolores Redondo-Pachon, Maria Dolores Arenas Jimenez, Alberto Mendoza-Valderrey, Ana Cristina Martins, Catarina Mateus, Goncalo Alvila, Ivo Laranjinha, Julia M Hofstra, Machiel A Siezenga, Antonio Franco, David Arroyo, Sandra Castellano, Sagrario Balda Manzanos, R Haridian Sosa Barrios, Wim Lemahieu, Karlijn Bartelet, Ahmet Burak Dirim, Erol Demir, Mehmet Sukru Sever, Aydin Turkmen, Seda Şafak, Daan A M J Hollander, Stefan Büttner, Soufian Meziyerh, Danny van der Helm, Marko Mallat, Hanneke Bouwsma, Sivakumar Sridharan, Kristina Petruliene, Sharon-Rose Maloney, Iris Verberk, Frank M van der Sande, Maarten H L Christiaans, Marc H Hemmelder, Mohan Kumar N, Marina Di Luca, Serhan Z Tuğlular, Martini Ziekenhuis, Andrea B Kramer, Charles Beerenhout, Peter T Luik, Julia Kerschbaum, Martin Tiefenthaler, Bruno Watschinger, Aaltje Y Adema, Vadim A Stepanov, Alexey B Zulkarnaev, Kultigin Turkmen, Ilaria Gandolfini, Umberto Maggiore, Anselm Fliedner, Anders Åsberg, Geir Mjoen, Hitoshi Miyasato, Carola W H de Fijter, Nicola Mongera, Stefano Pini, Consuelo de Biase, Angele Kerckhoffs, Anne Els van de Logt, Rutger Maas, Raphaël Duivenvoorden, Olga Lebedeva, Veronica Lopez, Louis J M Reichert, Jacobien Verhave, Denis Titov, Ekaterina V Parshina, Luca Zanoli, Carmelita Marcantoni, Gijs van Kempen, Liesbeth E A van Gils-Verrij, John C Harty, Marleen Meurs, Marek Myslak, Yuri Battaglia, Paolo Lentini, Edwin den Deurwaarder, Maria Stendahl, Hormat Rahimzadeh, Marcel Schouten, Ivan Rychlik, Carlos J Cabezas-Reina, Ana Maria Roca, Ferdau Nauta, İdris Sahin, Eric Goffin, Nada Kanaan, Laura Labriola, Arnaud Devresse, Anabel Diaz-Mareque, Armando Coca, Gabriel de Arriba, Björn K I Meijers, Maarten Naesens, Dirk Kuypers, Bruno Desschans, Annelies Tonnerlier, Karl M Wissing, Ivana Dedinska, Giuseppina Pessolano, Shafi Malik, Evangelia Dounousi, Evangelos Papachristou, Stefan P Berger, Esther Meijer, Jan Stephan F Sanders, Casper F M Franssen, Akin Özyilmaz, Jadranka Buturović Ponikvar, Andreja Marn Pernat, Damjan Kovac, Miha Arnol, Robert Ekart, Alferso C Abrahams, Arjan D van Zuilen, Sabine C A Meijvis, Helma Dolmans, Pasquale Esposito, Jean-Marie Krzesinski, Jean Damacène Barahira, Maurizio Gallieni, Paloma Leticia Martin-Moreno, Gabriele Guglielmetti, Gabriella Guzzo, Nestor Toapanta, Maria Jose Soler, Antinus J Luik, Willi H M van Kuijk, Lonneke W H Stikkelbroeck, Marc M H Hermans, Laurynas Rimsevicius, Marco Righetti, and Nicole Heitink-ter Braak
DATA AVAILABILITY STATEMENT
Collaborators that entered data in ERACODA remain the owner of these data. The database can therefore not be disclosed to any third party without the prior written consent of all data providers. Research proposals can be submitted to the Working Group via COVID.19.KRT@umcg.nl. If deemed of interest and methodological sound by the Working Group and Advisory Board, the analyses needed for the proposal will be carried out by the Management Team.
FUNDING
ERACODA received unrestricted research grants from the ERA, the Dutch Kidney Foundation, Baxter and Sandoz.
CONFLICT OF INTEREST STATEMENT
E.T., C.I., L.B.H., R.G., M.I., D.K., C.K., F.M.M., I.N., M.L.R.-F., M.A.M.V. and A.P.J.D.V., have no conflict of interest to disclose. K.J.K. received funding from the ERA. M.N., R.T.G., and P.V. receive grants from Dutch Kidney Foundation, European Renal Association, Sandoz and Baxter as well as received unrestricted research grants for ERACODA; payments were made to the institution.
AUTHORS’ CONTRIBUTIONS
All authors contributed to data collection, study design, data analysis, interpretation and drafting of this article.
REFERENCES
- 1. Global BMI Mortality Collaboration , Di Angelantonio E, Bhupathiraju Set al.Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016; 388: 776–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kalantar-Zadeh K, Block G, Humphreys MHet al. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 2003; 63: 793–808 [DOI] [PubMed] [Google Scholar]
- 3. Williamson EJ, Walker AJ, Bhaskaran Ket al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hilbrands LB, Duivenvoorden R, Vart Pet al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration. Nephrol Dial Transplant 2020; 35: 1973–1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gansevoort RT, Hilbrands LB. CKD is a key risk factor for COVID-19 mortality. Nat Rev Nephrol 2020; 16: 705–706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Noordzij M, Duivenvoorden R, Pena MJet al. ERACODA: the European database collecting clinical information of patients on kidney replacement therapy with COVID-19. Nephrol Dial Transplant 2020; 35: 2023–2025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Harris PA, Taylor R, Minor BLet al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95: 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rockwood K, Song X, MacKnight Cet al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization . Body mass index - BMI. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (18 January 2022, date last accessed) [Google Scholar]
- 10. Little R, Rubin D. Statistical analysis with missing data. 1st ed.New York, NY: John Wiley, 1987 [Google Scholar]
- 11. Kwok S, Adam S, Ho JHet al. Obesity: a critical risk factor in the COVID-19 pandemic. Clin Obes 2020; 10: e12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation 2020; 142: 4–6 [DOI] [PubMed] [Google Scholar]
- 13. Hamer M, Gale CR, Kivimaki Met al. Overweight, obesity, and risk of hospitalization for COVID-19: a community-based cohort study of adults in the United Kingdom. Proc Natl Acad Sci USA 2020; 117: 21011–21013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cottini M, Lombardi C, Berti Aet al. Obesity is a major risk factor for hospitalization in community-managed COVID-19 pneumonia. Mayo Clin Proc 2021; 96: 921–931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Simonnet A, Chetboun M, Poissy Jet al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 2020; 28: 1195–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lighter J, Phillips M, Hochman Set al. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission. Clin Infect Dis 2020; 71: 896–897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Petrilli CM, Jones SA, Yang Jet al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 2020; 369: m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang Y, Lu Y, Huang YMet al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metabolism 2020; 113: 154378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Smati S, Tramunt B, Wargny Met al. Relationship between obesity and severe COVID-19 outcomes in patients with type 2 diabetes: Results from the CORONADO Study. Diabetes Obes Metab 2021; 23: 391–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Luo XM, Jiaerken YM, Shen ZMet al. Obese COVID-19 patients show more severe pneumonia lesions on CT chest imaging. Diabetes Obes Metab 2021; 23: 290–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Huang HK, Bukhari K, Peng CCet al. The J-shaped relationship between body mass index and mortality in patients with COVID-19: a dose-response meta-analysis. Diabetes Obes Metab 2021; 23: 1701–1709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gao M, Piernas C, Astbury NMet al. Associations between body-mass index and COVID-19 severity in 6.9 million people in England: a prospective, community-based, cohort study. Lancet Diabetes Endocrinol 2021; 9: 350–359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Boban M, Bulj N, Kolacevic Zeljkovic Met al. Nutritional considerations of cardiovascular diseases and treatments. Nutr Metab Insights 2019; 12: 1178638819833705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hodgson LE, Murphy PB, Hart N. Respiratory management of the obese patient undergoing surgery. J Thorac Dis 2015; 7: 943–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Peters SAE, MacMahon S, Woodward M. Obesity as a risk factor for COVID-19 mortality in women and men in the UK biobank: comparisons with influenza/pneumonia and coronary heart disease. Diabetes Obes Metab 2021; 23: 258–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Naaraayan A, Nimkar A, Pant Set al. Sex disparity in the effect of obesity in hospitalized COVID-19 patients: A retrospective cohort study from the New York City Metropolitan Area. Cureus 2021; 13: e15235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dominelli PB, Ripoll JG, Cross TJet al. Sex differences in large conducting airway anatomy. J Appl Physiol (1985) 2018; 125: 960–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dominelli PB, Render JN, Molgat-Seon Yet al. Oxygen cost of exercise hyperpnoea is greater in women compared with men. J Physiol 2015; 593: 1965–1979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bell S, Campbell J, McDonald Jet al. COVID-19 in patients undergoing chronic kidney replacement therapy and kidney transplant recipients in Scotland: findings and experience from the Scottish renal registry. BMC Nephrol 2020; 21: 419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jager KJ, Kramer A, Chesnaye NCet al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int 2020; 98: 1540–1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. De Meester J, De Bacquer D, Naesens Met al. Incidence, characteristics, and outcome of COVID-19 in adults on kidney replacement therapy: A regionwide registry study. J Am Soc Nephrol 2021; 32: 385–396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Goffin E, Candellier A, Vart Pet al. COVID-19-related mortality in kidney transplant and haemodialysis patients: a comparative, prospective registry-based study. Nephrol Dial Transplant 2021; 36: 2094–2105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nopsopon T, Kittrakulrat J, Takkavatakarn Ket al. Covid-19 in end-stage renal disease patients with renal replacement therapies: a systematic review and meta-analysis. PLoS Negl Trop Dis 2021; 15: e0009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Griffith GJ, Morris TT, Tudball MJet al. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat Commun 2020; 11: 5749. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Collaborators that entered data in ERACODA remain the owner of these data. The database can therefore not be disclosed to any third party without the prior written consent of all data providers. Research proposals can be submitted to the Working Group via COVID.19.KRT@umcg.nl. If deemed of interest and methodological sound by the Working Group and Advisory Board, the analyses needed for the proposal will be carried out by the Management Team.