Abstract
Dental surgeons regularly provide intravenous dental sedation and oral/transmucosal sedation, which involves cannulation. Cannulation is an essential skill that dental surgeons should be competent to perform, but certain patient groups may be difficult to cannulate. Ultrasound-guided peripheral intravenous cannulation is an evidence-based technique already used in radiology, emergency medicine, and anaesthesia. Ultrasound-guided peripheral intravenous cannulation has been shown to reduce complications and significantly increase the success of cannulation in patients with difficult intravenous access (DIVA); it may also be preferable in certain special care patient groups. The application of ultrasound-guided peripheral intravenous cannulation should be considered for patients with DIVA who require intravenous dental sedation or other common procedures in dental surgery that involve cannulation.
Supplementary Information
Zusatzmaterial online: Zu diesem Beitrag sind unter 10.1038/s41415-022-4133-x für autorisierte Leser zusätzliche Dateien abrufbar.
Key points
Discusses the potential future changes to the provision of dental sedation.
Discusses possible indications and contraindications of USG-PIVC for intravenous dental sedation.
Describes the method of USG-PIVC and current barriers to implementing USG-PIVC for intravenous dental sedation.
Supplementary Information
Zusatzmaterial online: Zu diesem Beitrag sind unter 10.1038/s41415-022-4133-x für autorisierte Leser zusätzliche Dateien abrufbar.
Introduction
Sedation and general anaesthesia are commonly provided as part of dental surgery, particularly with patients who may require special care dentistry. In the UK, the utilisation of sedation has increased since the recommendation that general anaesthesia in dental surgery should be restricted to a hospital setting.1,2
Internationally, there is also a move towards greater emphasis on promoting the safety of pain and anxiety control in dental surgery. The USA have recently recognised 'dental anaesthesiology' as a dental speciality3 and in the UK it is recommended that dedicated sedationists (as opposed to operator-sedationists) provide sedation to more complex special care patients, such as those who are medically compromised, older, physically disabled or emotionally challenging.4 As the numbers of complex patients requiring sedation increases, it is likely that dedicated sedationists will become more common.
While inhalation sedation is an effective method of sedation, its use is often limited to paediatric patients and simple treatments, such as restorations or simple extractions. Intravenous dental sedation provides the advantages of more profound sedation with anterograde amnesia and is more likely to be accepted by adults or special care patients.5 Intravenous dental sedation, however, has more risk involved compared to inhalation sedation, which includes respiratory depression. Furthermore, intravenous dental sedation (and general anaesthesia) has a higher risk of falls, and contemporary pre-operative sedation assessments should consider potential post-falls risk.6 In addition, intravenous dental sedation requires cannulation in order to administer the sedative drug; it is also common practice to place a cannula during oral/transmucosal sedation.
Cannulation carries its own risks, which include: pain, haematoma, extravasation, thrombus, phlebitis and air-embolism and nerve injury.7 Although short-term peripheral venous catheter-related bloodstream infections are unlikely in intravenous dental sedation due to the short duration of treatment, repeated cannulations increase the risk of introduction of infection and, therefore, bacteraemia or sepsis,8 which can be particularly dangerous in systemically compromised special care patients.
Several techniques have been described to try and improve the success of cannulation or promote venodilatation, including: the use of surface anatomy, warmth, inhalation sedation, blood pressure cuffs, near infrared imaging and glyceryl trinitrate patches. Oral/transmucosal sedation has been used with special care patients to aid cooperation for cannulation, but this has the disadvantage of unpredictable response and recovery. Moreover, clinical holding can also be used with special care patients to ameliorate cooperation for cannulation, but this is restricted to certain patient groups and can be associated with adverse outcomes, including musculoskeletal injuries, cardiorespiratory restriction or psychological distress.9
Previous authors have also suggested pre-operative scales10,11 to help predict the difficulty of intravenous access. Despite this, cannulation can still be challenging, with success being reported at 33-69%.12
Successful cannulation can reduce anxiety; improve the patient's experience and quality of sedation; increase future compliance; and prevent delays in treatment/referral and potential complaints.
Ultrasound can be used to guide peripheral intravenous cannulation and therefore be applied to intravenous dental sedation. This paper outlines the method for ultrasound-guided peripheral intravenous cannulation (USG-PIVC) and its possible indications, contraindications and current barriers to its implementation in dental surgery.
Ultrasound-guided peripheral intravenous cannulation
Ultrasound is a non-invasive and painless real time special investigation, that can be used to visualise internal organs and blood vessels within the body using high frequency sound waves (greater than 2 MHz). Ultrasound does not use radiation and there are no special pre or post instructions (for cannulation) or side effects, making it suitable for most patients. Ultrasound has many uses in medicine, including in radiology, cardiology, dermatology, gynaecology and emergency medicine. In dental surgery, ultrasound has been used for caries detection, dental and maxillofacial trauma, periapical and periodontal disease, temporomandibular joint disorders and implantology.13
USG-PIVC is a relatively novel technique which has been used in radiology, emergency medicine14 and anaesthesia15 and can be applied to intravenous dental sedation. It has been shown to improve the success of cannulation in patients with difficult intravenous access (DIVA) and reduce the number of attempts required.16,17,18,19 USG-PIVC may also enable dental surgeons to use alternative sites, such as distal to the antecubital fossa or mid-arm basilic or cephalic veins,20 or deeper veins for intravenous dental sedation, therefore reducing the chance of failed cannulations and a delay in treatment. USG-PIVC is increasingly being taught to medical students,21 foundation doctors22 and nurses.23
One study into the success of USG-PIVC in medical students showed that USG-PIVC had a success rate of 100% versus 56% for surface landmark cannulation and required fewer attempts.24 The European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) also recommends USG-PIVC for patients with DIVA.25
Special care dentistry, in particular, involves providing intravenous dental sedation for a range of complex patients who may have DIVA. Musculoskeletal, dermatological, or other systemic pathologies such as Dupuytren's contracture, rheumatoid arthritis, clonus/spasticity of the hands (eg cerebral palsy), and skin cancer may affect cannulation. Drugs or treatment may also complicate cannulation. Bleomycin can cause vein wall hypertrophy26 and radiotherapy can be associated with peripheral venous stenosis.27 Women who have had breast cancer treatment (mastectomy or radiotherapy) with lymph node removal are at higher risk of lymphoedema; therefore, cannulation and blood pressure measurements may be safer on the untreated side.28 In addition, hypercoagulable patients are at higher risk of thromboembolic complications, and repeated cannulations should be avoided.29 USG-PIVC may therefore be more suitable for certain special care patient groups requiring intravenous dental sedation in comparison to other cannulation techniques.
Table 1 shows suggested indications and contraindications for USG-PIVC for intravenous dental sedation.
Table 1.
Suggested indications and contraindications for using USG-PIVC for intravenous dental sedation
| Indications | Contraindications |
|---|---|
|
Non-ultrasound-guided techniques failed on more than two occasions History of difficult cannulation, for example: obese patients; IV drug abusers; those with altered/extraordinary surface anatomy; frail, older patients; arthritic patients; and hypotensive patients Reduce needlestick injuries in hypercoagulable patients,29 such as patients with Factor V Leiden, cancer, myeloproliferative disorders, chronic renal disease and COVID-19 disease Patients with bleeding disorders, for example, haemophilia, Von Willebrand disease, liver disease, and anticoagulated patients Patients with multiple previous cannulations, for example, chemotherapy patients30 Renal patients31 who have regular haemodialysis and an arteriovenous fistula; where cephalic or veins in the antecubital fossa are vital, therefore there is less opportunity to repeat cannulation or there is difficulty with cannulation. The dorsum of the hand may be the safest site for cannulation in this group of patients Patients who have blood-borne diseases (for example, Hepatitis B or HIV) and a history of difficult cannulation or potential difficulty with cannulation by non-ultrasound-guided cannulation to reduce the chance of needlestick injuries Patients with movement disorders (for example, Huntington's disease) where cannulation is difficult (may require dual operator technique [see below] or clinical holding to complete) Patients with rare skin disorders, where minor trauma can be serious, and there is limited skin surface suitable for cannulation or there is fragile vasculature (eg epidermolysis bullosa or Ehlers-Danlos syndrome). Special care (or paediatric)32 patients where cooperation is likely to be limited for multiple cannulation attempts (and USG-PIVC is possible) Needle-phobic patients (that accept cannulation), who may not allow repeated attempts at cannulation |
The same contraindications for other cannulation techniques; for example, inflammation/pathology at site Vein pathology identified on ultrasound, for example, thrombus Untrained in ultrasound or intravenous dental sedation/cannulation |
USG-PIVC is clearly beneficial for dental surgeons involved in the 'sedation specialities' but may also be beneficial for other common procedures that involve cannulation, such as in oral surgery for platelet-rich growth factor extraction or in oral medicine where blood tests are commonly required as part of the diagnostic process. In acute situations, USG-PIVC may be beneficial during medical emergencies in the dental practice, providing the dental surgeon is happy to obtain intravenous access.
Training in USG-PIVC
The Royal College of Radiologists (RCR) suggests that clinicians who undertake ultrasound investigations should undergo annual training and have guidance for USG-PIVC, which may be provided by wards, outpatient clinics or general practice surgeries (non-radiologists). This guidance can be used to determine the possible requirements for training of dental surgeons in USG-PIVC (Box 1).33
The RCR suggests the observation of 20 USG-PIVCs, then performing 20 ultrasound scans under supervision, and then finally performing 20 USG-PIVCs under supervision before independent practice.33
Box 1 RCR training guidance for non-radiologists in USG-PIVC .
Knowledge base33
Physics and technology, ultrasound techniques and administration
Sectional and ultrasonic anatomy, including difference between veins and arteries and nerves
Pathology, including thrombus, patency and occlusion
Basic knowledge of Doppler ultrasound.
Technique for intravenous dental sedation using USG-PIVC
Relevant ultrasound anatomy
It is very important that any clinician who performs ultrasound has a sound knowledge of ultrasound anatomy and USG-PIVC, which is not possible to fully cover in this paper. The main structures which need differentiation during cannulation on ultrasound include veins and arteries (see Table 2).34,35
Table 2.
| Characteristic | Veins | Arteries |
|---|---|---|
| Walls | Thin (may also be able to see valves on longitudinal view) | Thick |
| Compressibility with ultrasound probe | Compresses on slight pressure | Less compressible |
| Shape | Oval (transverse view) | Round (transverse view) |
| Echogenicity | Anechoic | Anechoic |
| Pulse | No pulse | Pulse |
| Doppler assessment | Low velocity | High velocity |
Nerves may be distinguished from arteries and veins as they are generally smaller, less compressible, and appear with hyperechoic (fascicles) with internal hypoechoic (epineurium) circles - a 'honeycomb' appearance on ultrasound.36 In addition, nerves are mainly elliptical in shape (but can be round or triangular depending on the position in the nerve path) in transverse view or present as long, slim structures with parallel hypoechoic and hyperechoic lines in longitudinal view.36 Nerves also have no pulse and display no signal on colour Doppler.36
Materials and equipment
See Figures 1 and 2 for materials and equipment, which include:
Standard intravenous dental sedation setup (cannula [22 Birmingham gauge], tourniquet, plasters, syringes, topical anaesthetic, skin disinfectant, cotton wool rolls/buds, intravenous dressing, sterile saline, midazolam, and flumazenil [rescue]).
An ultrasound machine or a wireless ultrasound probe with a smart device.
Linear ultrasound probe (5-8 MHz) and ultrasound gel. Lower frequency curvilinear probes (2-5 MHz) may be more suitable for obese patients due to their deeper veins37
Ultrasound probe/transducer cover.
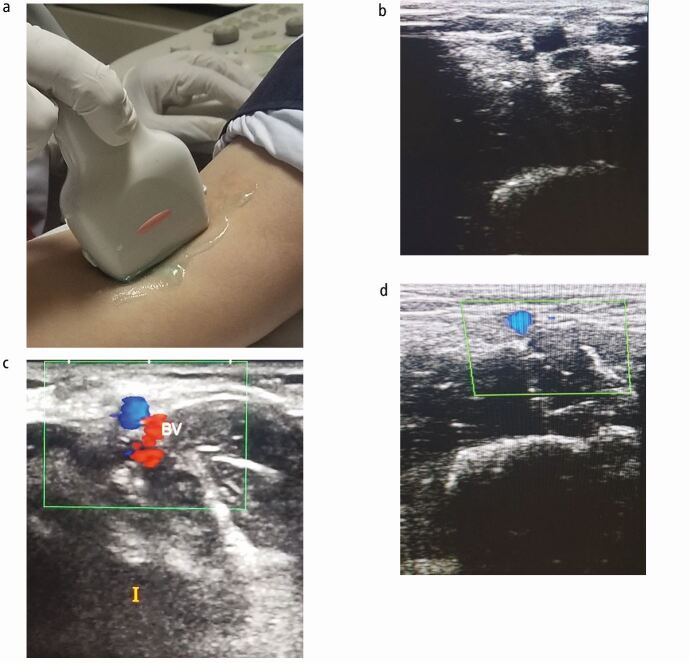
Fig. 1.
Materials and equipment for USG-PIVC. a) Ultrasound machine. b) Standard intravenous sedation setup. c) Linear probe. d) Curvilinear probe (for obese patients)
Fig. 2.
Ultrasound scan of the antecubital fossa to identify basilic vein. a) Ultrasound scan of the antecubital fossa using a linear probe. b) Ultrasound image of the antecubital fossa (transverse view). c, d) Colour Doppler views of the basilic vein in the antecubital fossa (transverse view)
Ultrasound settings
Ultrasound settings are:
Vascular access configuration
Ultrasound B Mode (2D-brightness modulation) and, if available, colour Doppler
Setting at 5-10 MHz linear probe
Depth of 3-4 cm.
Procedure using an ultrasound machine
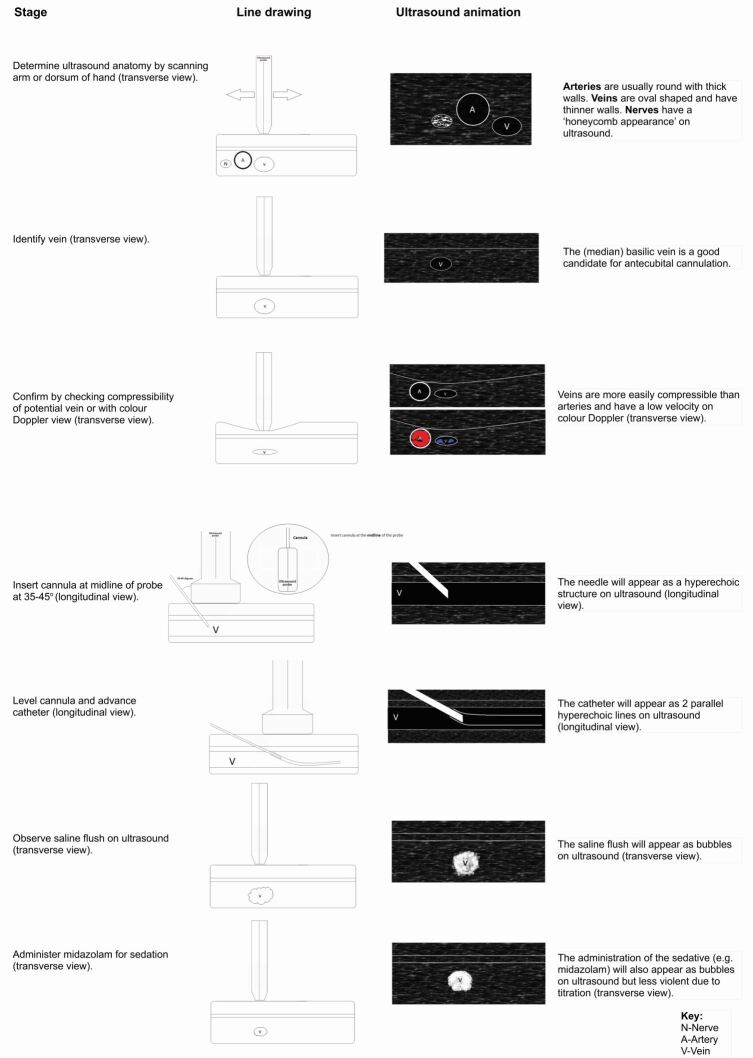
The ultrasound aspects of the procedure were adapted38 (see Figure 3).
Fig. 3.
Stages of intravenous dental sedation using USG-PIVC
Follow universal cross infection procedures:
Obtain consent for USG-PIVC (see online Supplementary Information). Assess the arm or hand for a potential cannulation site; if there is significant pathology, avoid this area and consider referral (if serious pathology is found, eg melanoma) or advise the patient to seek care from a medical professional
Place a tourniquet about 10 cm away from the potential cannulation site
Apply ultrasound gel to the potential cannulation site
Using the ultrasound machine and linear probe, scan the antecubital fossa or dorsum of the hand for potential veins using the ultrasound probe transversely. USG-PIVC is generally used for the cannulation of larger superficial veins found in the antecubital fossa rather than smaller veins often found in the dorsum of the hand
Determine the ultrasound anatomy
Identify veins on ultrasound; wide veins which are not close to arteries or nerves should be used. The median basilic vein is normally good for intravenous access at the antecubital fossa
Rotate the linear probe longitudinally once a suitable vein is found
Remove ultrasound gel from the potential cannulation site and clean site using disinfectant wipe
Prepare cannula and ensure it is bevel up
Insert cannula at the midline of the linear probe at 35-45 degrees to ensure sufficient feedback from ultrasound.34 You should be able to observe the cannula entering the vein (the needle appears as a hyperechoic structure) on the ultrasound machine
You should observe primary flashback. Now, level the cannula and advance a few millimetres into the vein, again observing this on the ultrasound machine
Withdraw the needle for the second flashback and insert the catheter into the vein, observing it on ultrasound (it should appear as two parallel hyperechoic lines)
Release the tourniquet and apply pressure to the vein near the tip of the catheter. Remove the cap from the needle and place the cap at the end of the cannula. Dispose of the needle in the sharps bin
Secure site with intravenous dressing
Rotate the linear probe transversely and flush the catheter with sterile saline. Observe on the ultrasound machine
Administer midazolam or a drug for intravenous dental sedation and check for entry into vein with ultrasound.
A single or dual operator technique may be used, where one operator carries out the ultrasound and the other completes the cannulation.34 Alternatively, ultrasound can be used to identify the vein for cannulation and then this area of the skin is marked and cannulation is performed without any ultrasound guidance.34 Ultrasound could also be utilised at the pre-assessment appointment to more accurately document the favourable veins for cannulation in patients with expected difficulty, as images can be stored or videos kept in patient records for other clinicians to view.
Another technique, known as the 'dynamic needle tip positioning'39 (see Figure 4), can also be used for USG-PIVC. This approach is less technique sensitive, requiring less stability and can be an easier technique for the cannulation of smaller veins.39
Fig. 4.
Dynamic needle tip positioning technique for USG-PIVC
Current barriers to the implementation of USG-PIVC in dental surgery
USG-PIVC has many advantages for dental surgeons; however, at present, there are barriers to its introduction in dental surgery. Due to expense, ultrasound may be more accessible in general or dental hospitals. In addition, equipment requirements, training/continuing professional development (CPD), time, medico-legal implications and patient selection need consideration (see Table 3).
Table 3.
Challenges to implementing ultrasound-guided peripheral intravenous cannulation in dental surgery
| Possible barrier | Comment |
|---|---|
| Cost |
Initial and maintenance (equipment) Extra materials required for example, ultrasound gel CPD training/courses |
| Training |
Annual CPD required (RCR guidance) No current postgraduate courses for dental surgeons Not covered in undergraduate dental training |
| Equipment |
Space requirements (non-portable) Several systems available |
| Time |
Set up may prolong appointment time, however, may be time-saving in comparison to other techniques in difficult patient groups Consider the potential need for USG-PIVC at the pre-assessment appointment to avoid time lost at the treatment appointment |
| Medico-legal |
Should be able to report all findings (including pathology, for example, thrombus or nerve pathology) on ultrasound and refer if necessary May need to make dental indemnity aware |
| Patient acceptance | There may be some difficulty with special care and paediatric patients |
Dental radiologists are well trained in ultrasound and can help in difficult cases, but they can also teach USG-PIVC to help dental surgeons gain competency in this skill. The relevant dental sedation societies should consider providing training in USG-PIVC to increase access for dental surgeons involved in sedation/special care dentistry.
Point of care ultrasound (POCUS)/wireless ultrasound probes that work with your smartphone or tablet are now available and cheaper, smaller, and more practical,40 which will help to improve the accessibility of ultrasound for healthcare professionals. Pocket ultrasound probes that use web-based operation and internet connectivity should allow for remote learning and assessment of competency.41 They are also easier to disinfect post-COVID dental practice.42 POCUS disadvantages include reduced image quality and working time, inability to use Doppler view, and a higher risk of losing the ultrasound probe.41
Most recently, robotics in combination with ultrasound imaging has been developed to produce hand-held automated venepuncture devices that exclude the need for human involvement in cannulation,43 but this is unlikely to become clinically practicable or financially viable in medicine or dental surgery for some time.
Conclusions
USG-PIVC provides both a significant advantage for patients requiring intravenous dental sedation and an evidence-based approach to cannulation, potentially avoiding the need to repeat cannulation. It can also be used to confirm entry of sedative drugs into veins and therefore prevent complications. In addition, it may also be more beneficial for certain special care patients.USG-PIVC should be considered as part of the pre-assessment/case conference for special care patients or patients with DIVA who require intravenous dental sedation. USG-PIVC can also help in the management of patients requiring oral surgery and oral medicine.
Portable devices may make ultrasound more accessible to general dental surgeons and the community dental services in the future, instead of being restricted to dental and general hospitals. Dental students should be exposed to the advantages of USG-PIVC during their undergraduate training in special care dentistry and opportunities should become available for dental surgeons to learn this skill after graduation.
Supplementary Information
Ethics declaration
The author declares no conflict of interest.
References
- 1.Central Health Services Council, Standing Dental Advisory Committee, Poswillo D E. General anaesthesia, sedation and resuscitation in dentistry: report of an expert working party. London: Department of Health, 1990.
- 2.Whittle J G. The provision of primary care dental general anaesthesia and sedation in the north west region of England, 1996-1999. Br Dent J 2000; 189: 500-502. [DOI] [PubMed]
- 3.Kramer K J. Specialty Recognition for Dental Anesthesiology. Anesth Prog 2019;66: 59-60. [DOI] [PMC free article] [PubMed]
- 4.Intercollegiate Advisory Committee for Sedation in Dentistry. Standards for Conscious Sedation in the Provision of Dental Care (V1.1): Report of the Intercollegiate Advisory Committee for Sedation in Dentistry. 2020. Available at https://www.rcseng.ac.uk/-/media/files/rcs/fds/publications/standardsforconscioussedationand-accreditation/dentalsedationreportv112020.pdf (accessed November 2021).
- 5.Manley M C, Skelly A M, Hamilton A G. Dental treatment for people with challenging behaviour: general anaesthesia or sedation? Br Dent J 2000; 188:358-360. [DOI] [PubMed]
- 6.Khan I. Falls: considerations for the dental surgeon. Br Dent J 2020; 228: 509-514. [DOI] [PubMed]
- 7.Ford C. Cannulation in adults. Br J Nurs 2019; 28:838-841. [DOI] [PubMed]
- 8.South Eastern Sydney Local Health District. Peripheral Intravenous Cannulation (PIVC) Insertion, Care and Removal (Adults). 2021. Available at https://www.seslhd.health.nsw.gov.au/sites/default/files/documents/SESLHDPR%20577%20Peripheral%20Intravenous%20Cannulation%20%28PIVC%29%20Insertion%2C%20Care%20and%20Removal%20%28Adults%29.pdf (accessed November 2021).
- 9.British Society for Disability and Oral Health. Guidelines for 'Clinical Holding' Skills for Dental Services for people unable to comply with routine oral healthcare. 2009. Available at: https://www.bsdh.org/documents/BSDH_Clinical_Holding_Guideline_Jan_2010.pdf (accessed December 2021).
- 10.van Loon F H J, van Hooff L W E, de Boer H D et al. The modified A-DIVA scale as a predictive tool for prospective identification of adult patients at risk of a difficult intravenous access: a multicentre validation study. J Clin Med 2019; DOI: 10.3390/jcm8020144. [DOI] [PMC free article] [PubMed]
- 11.Civetta G, Cortesi S, Mancardi M et al. EA-DIVA score (Enhanced Adult DIVA score): A new scale to predict difficult preoperative venous cannulation in adult surgical patients. J Vasc Access 2019; 20: 281-289. [DOI] [PubMed]
- 12.Cooke M, Ullman A J, Ray-Barruel G, Wallis M, Corley A, Rickard C M. Not" just" an intravenous line: Consumer perspectives on peripheral intravenous cannulation (PIVC). An international cross-sectional survey of 25 countries. PloS One 2018; DOI: 10.1371/journal.pone.0193436. [DOI] [PMC free article] [PubMed]
- 13.Marotti J, Heger S, Tinschert J et al. Recent advances of ultrasound imaging in dentistry - a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 115: 819-832. [DOI] [PubMed]
- 14.Reardon R, Heegaard B, Plummer D, Clinton J, Cook T, Tayal V. 2006. Ultrasound is a necessary skill for emergency physicians. Acad Emerg Med 2006; 13: 334-336. [DOI] [PubMed]
- 15.Munshey F, Parra D A, McDonnell C, Matava C. Ultrasound-guided techniques for peripheral intravenous placement in children with difficult venous access. Paediatr Anaesth 2020; 30: 108-115. [DOI] [PubMed]
- 16.Egan G, Healy D, O'Neill H, Clarke-Moloney M, Grace P A, Walsh S R. Ultrasound guidance for difficult peripheral venous access: systematic review and meta-analysis. Emerg Med J 2013; 30: 521-526. [DOI] [PubMed]
- 17.Liu Y T, Alsaawi A, Bjornsson H M. Ultrasound-guided peripheral venous access: a systematic review of randomized-controlled trials. Eur J Emerg Med 2014; 21: 18-23. [DOI] [PubMed]
- 18.Stolz L A, Stolz U, Howe C, Farrell I J, Adhikari S. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. J Vasc Access 2015; 16: 321-326. [DOI] [PubMed]
- 19.Costantino T G, Parikh A K, Satz W A, Fojtik J P. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med2005; 46: 456-461. [DOI] [PubMed]
- 20.Sandhu N P S, Sidhu D S. Mid-arm approach to basilic and cephalic vein cannulation using ultrasound guidance. Br J Anaesth 2004; 93: 292-294. [DOI] [PubMed]
- 21.Armson A M, Moynihan R, Stafford N, Jacobs C. Ultrasound-guided cannulation for medical students. Clin Teach 2021; 18: 295-300. [DOI] [PubMed]
- 22.Blair J A. Ultrasound guided peripheral venous cannulation: A useful skill for foundation doctors? J Intens Care Soc 2021; DOI: 10.1177/17511437211003500. [DOI] [PMC free article] [PubMed]
- 23.Stuckey C, Curtis M P. Development of a nurse-led ultrasound-guided peripheral intravenous programme. J Vasc Nurs 2019; 37: 246-249. [DOI] [PubMed]
- 24.Vitto M J, Myers M, Vitto C M, Evans D P. Perceived difficulty and success rate of standard versus ultrasound-guided peripheral intravenous cannulation in a novice study group: A randomized crossover trial. J Ultrasound Med 2016; 35: 895-898. [DOI] [PubMed]
- 25.Jenssen C, Brkljacic B, Hocke M et al. EFSUMB guidelines on interventional ultrasound (INVUS), Part VI - Ultrasoundguided vascular interventions. Ultraschall Med 2016; 37: 473-476. [DOI] [PubMed]
- 26.Joint Formulary Committee. BNF 82 (British National Formulary): September 2021 - March 2022. London: Pharmaceutical Press, 2021.
- 27.Franklin W J, Strickman N E, Hall R J. Stent deployment for peripheral venous stenosis as a result of radiation therapy. Catheter Cardiovasc Interv 2003; 59: 60-62. [DOI] [PubMed]
- 28.Jakes A D, Twelves C. Breast cancer-related lymphoedema and venepuncture: a review and evidence-based recommendations. Breast Cancer Res Treat 2015; 154: 455-461. [DOI] [PubMed]
- 29.Thorn C, Nickels L C. Ultrasound-Guided Peripheral Intravenous Access. In Ganti L (ed) Atlas of Emergency Medicine Procedures. pp 13-15. New York: Springer, 2016.
- 30.Gallieni M, Pittiruti M, Biffi R. Vascular access in oncology patients. CA Cancer J Clin 2008; 58: 323-346. [DOI] [PubMed]
- 31.Eves J, Cai P, Latham R et al. A randomised clinical trial of ultrasound guided cannulation of difficult fistulae for dialysis access. J Vasc Access 2021; 22: 635-641. [DOI] [PubMed]
- 32.Vinograd A M, Chen A E, Woodford A L et al. Ultrasonographic guidance to improve first-attempt success in children with predicted difficult intravenous access in the emergency department: a randomized controlled trial. Ann Emerg Med 2019; 74: 19-27. [DOI] [PubMed]
- 33.The Royal College of Radiologists. Focused ultrasound training standards. 2012. Available at https://www.rcr.ac.uk/system/files/publication/field_publication_files/BFCR%2812%2918_focused_training.pdf (accessed June 2021).
- 34.McLoughlin R. Ultrasound: Skills of Ultrasound-guided Vascular Access. 2021. Available from https://www.rcemlearning.org/modules/ultrasound-skills-of-ultrasound-guided-vascular-access/ (accessed March 2022).
- 35.Blanco P. Ultrasound-guided peripheral venous cannulation in critically ill patients: a practical guideline. Ultrasound J 2019; DOI: 10.1186/s13089-019-0144-5. [DOI] [PMC free article] [PubMed]
- 36.Im Suk J, Walker F O, Cartwright M S. Ultrasonography of peripheral nerves. Curr Neurol Neurosci Rep 2013; DOI: 10.1007/s11910-012-0328-x. [DOI] [PMC free article] [PubMed]
- 37.Blessing M. Ultrasound Probe Selection, Knobology and Optimization of Image Quality. In Li J, Ming-Der Chow R, Vadivelu N, Kaye A D (eds) Ultrasound Fundamentals: An Evidence-Based Guide for Medical Practitioners. pp 17-24. Switzerland: Springer Nature, 2021.
- 38.Interanest. Peripheral venous cannulation. 2018. Available at https://www.interanest.org/ (accessed June 2021).
- 39.Clemmesen L, Knudsen L, Sloth E, Bendtsen T. Dynamic needle tip positioning-ultrasound guidance for peripheral vascular access. A randomized, controlled and blinded study in phantoms performed by ultrasound novices. Ultraschall Med 2012; DOI: 10.1055/s-0032-1312824. [DOI] [PubMed]
- 40.Forsyth J M, Shalan, A, Thompson A R. Venous access made easy. 2nd ed. London: Taylor & Francis, 2019.
- 41.Baribeau Y, Sharkey A, Chaudhary O et al. Hand-held point of care ultrasound probes-the new generation of POCUS. J Cardiothoracic Vasc Anaesth 2020; 34: 3139-3145. [DOI] [PMC free article] [PubMed]
- 42.Gibson L E, Bittner E A, Chang M G. Handheld ultrasound devices: An emerging technology to reduce viral spread during the Covid-19 pandemic. Am J Infect Control 2020; 48: 968-969. [DOI] [PMC free article] [PubMed]
- 43.Leipheimer J M, Balter M L, Chen A I et al. First-in-human evaluation of a hand-held automated venipuncture device for rapid venous blood draws. Technology (Singap World Sci) 2019; 7: 98-107. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.