Abstract
Despite the promising initial anti-tumor efficacy of epidermal growth factor receptor-tyrosine kinase inhibitors (EGFR-TKIs), most advanced non-small-cell lung cancers (NSCLCs) progress eventually due to therapeutic resistance. V-Raf murine sarcoma viral oncogene homolog B1 (BRAF)V600E mutation has been considered as an uncommon mutation that contributes to acquired resistance for EGFR-TKIs. In the presented case, BRAFV600E mutation was detected as an acquired resistance-mediated mutation in a patient treated with osimertinib (a third-generation EGFR-TKI). The presented patient achieved partial regression and ongoing PFS of four months after the co-inhibition of osimertinib plus dabrafenib (BRAF inhibitor) and trametinib (MEK inhibitor). Our case further enriches the clinical evidence of the efficacy of EGFR/BRAF/MEK co-inhibition in patients with an acquired BRAFV600E mutation, consistent with the review of the literature (eight cases). Additionally, our case highlights the important role of sample type, method, and platform of gene detection in patient management, life quality, and prognosis, as well as the understanding of acquired resistance mechanism.
Keywords: NSCLC, targeted therapy, resistance mechanisms, EGFR mutation, BRAFV600E mutation, case report
INTRODUCTION
Lung cancer is the leading cause of cancer-related mortality worldwide, and non-small-cell lung cancer (NSCLC) represents the histological subtype of 85% of lung cancer[1]. Great progress has been made in targeting the driver gene mutation for lung adenocarcinoma, a common subtype of NSCLC. Epidermal growth factor receptor (EGFR) mutations occur in 16% of advanced adenocarcinoma Caucasian patients, and the mutation frequency is as high as 61.1% in Asian females[2,3]. EGFR-tyrosine kinase inhibitors (TKIs) are the most common targeted therapy available for lung adenocarcinoma, including the first-generation inhibitors erlotinib, gefitinib, and icotinib; the second-generation inhibitor afatinib; and the third-generation inhibition osimertinib[4]. Although these therapies show promising initial anti-tumor activities, most advanced NSCLC cases eventually progress due to therapeutic resistance, also known as acquired resistance (AR). The alterations leading to EGFR-TKI resistance are divided into “on-target” resistance (alterations in targeted oncogene, EGFR) and “off-target” resistance (alterations in other downstream and parallel pathways)[5]. For alterations in downstream pathways, MAPK pathway reactivation plays an important role in the AR mechanism of EGFR-mutated lung cancer, including V-Raf murine sarcoma viral oncogene homolog B1 (BRAF)V600E mutation[6].
BRAF mutations are targeting oncogenic drivers, occurring in 3%-8% of lung adenocarcinomas. The common BRAF mutations consists of BRAFV600E (50%), BRAFG467A/V (35%), and BRAFD549G (6%) mutations[7,8]. BRAFV600E mutation induces constitutive BRAF activation in its monomeric form, activating downstream MEK-extracellular regulated protein kinases signaling[9].
BRAFV600E is also considered an uncommon mutation which contributes to AR in approximately 3% of patients receiving second-line osimertinib[10,11]. Although dabrafenib and trametinib have been approved for first-line treatment of metastatic NSCLC patients harboring BRAFV600E mutation, and a pre-clinical study and several case reports have revealed the anti-tumor potential of co-inhibition treatment for post-line treatment after targeted therapy resistance, the efficacy and safety of EGFR/BRAF/MEK co-inhibition for EGFR-mutated NSCLC patients with an acquired BRAFV600E mutation remain to be confirmed[12-19].
Therefore, we report the therapeutic outcome of co-inhibition of EGFR, BRAF, and MEK for a lung adenocarcinoma patient who developed resistance to osimertinib. We also present a literature review of the clinical outcome and safety for EGFR/BRAF/MEK co-inhibition therapy in EGFR-TKI-treated NSCLC patients with acquired BRAFV600E mutation, in order to further enrich the clinical evidence.
CASE REPORT
A 64-year-old female was admitted to the Department of Respiratory and Critical Care Medicine, Shanghai Ruijin Hospital in October 2017 due to the symptoms of cough and sputum. Further hospital examinations found scattered nodules in bilateral lungs, multiple enlarged (right supraclavicular, bilateral axillary, and bilateral inguinal) lymph nodes, and increased carcinoembryonic antigen (CEA) levels. Moreover, lung adenocarcinoma cells were found in biopsies of the lung nodules and right supraclavicular lymph node. After subsequent evaluation, she was diagnosed with lung adenocarcinoma, with the stage cT4N3M1a (tumor nodules in different ipsilateral lobes, supraclavicular node, and contralateral lobes), stage IVA (AJCC 8th edition), and lymphangitis carcinoma of the lung. Additionally, an EGFR exon 19 deletion (E19del) was identified by droplet digital polymerase chain reaction on lymph node biopsy. The whole course of treatment and changes of tumor indicators during the treatment are shown in Figures 1 and 2.
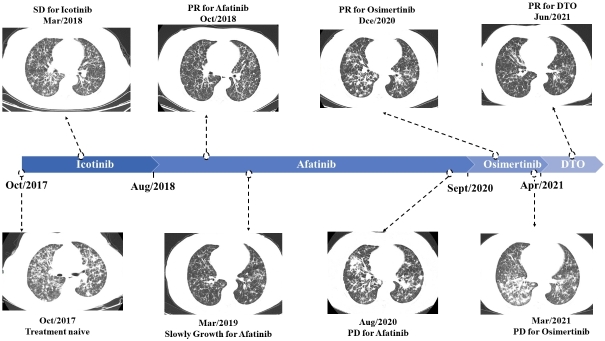
Figure 1.
Radiologic images and timeline of the patient’s clinical course.
Figure 2.
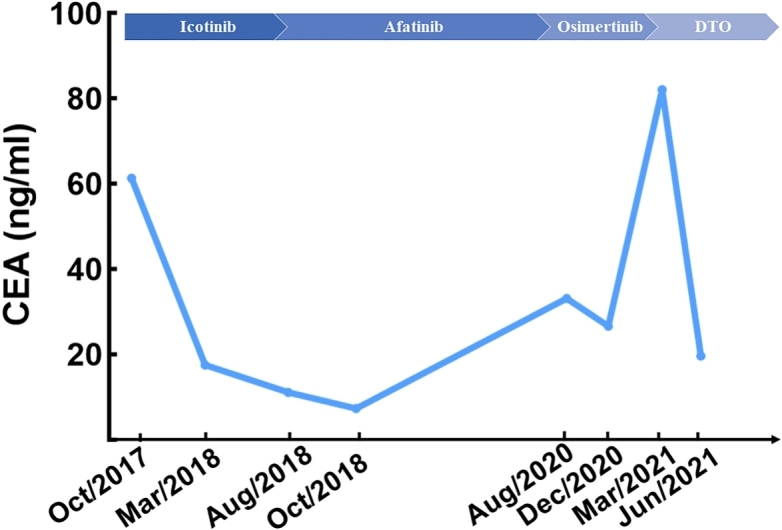
The changes in the carcinoembryonic antigen (CEA) level during the patient’s clinical course.
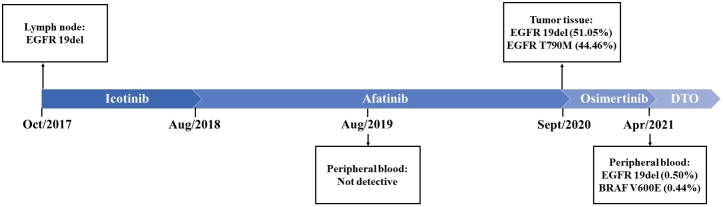
Thus, she had clear indications for the first-generation EGFR-TKIs. Considering her abnormal liver function before hospitalization, we gave her icotinib (BETTA pharmaceutical, China) at a dose of 125 mg t.i.d, which has less hepatotoxicity than erlotinib and gefitinib. The treatment quickly prompted a stable disease based on criteria in Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 and decreased CEA level. Five months later, she was diagnosed with drug-induced abnormal liver function (Grade 3) due to increased glutamine transaminase (ALT), aspartate amino transferase (AST), and bilirubin. Although icotinib was discontinued for one month and symptomatic treatment was given, abnormal liver function appeared again after the rechallenge of icotinib. Thus, afatinib (40 mg q.d) was given in August 2018. The chest computerized tomography (CT) after two months of afatinib showed partial response (PR) based on criteria in RECIST 1.1, with significant regression of scattered nodules in bilateral lungs. However, in January 2019, her disease progressed slowly after a progression-free survival (PFS) of 17 months. Then, a secondary genetic testing was recommended, and she agreed to take a 168-gene panel (Burning Rock Biotech, Guangzhou, China) to test the driver mutation in her peripheral blood in April 2019. The results show that there was no targetable mutation, including E19del, EGFR-T790M, and BRAFV600E [Figure 3].
Figure 3.
The mutations detected at different timepoints available from tissue or liquid biopsies.
Despise of our strong recommendation of secondary tissue biopsy, she refused any invasive manipulation and therapeutic regimen adjustment. After the continuation of afatinib until August 2020, the patient was admitted to our hospital due to chest distress, which could not be alleviated by rest. Further examination in August 2020 revealed the significant progression in pulmonary scattered nodules and a newly emerging enhanced brain nodule, combined with severe lymphangitis carcinoma and an increased CEA level. What is worse, she became increasingly dyspneic, along with presenting severe hypoxemia. At this time, she agreed to take ultrasound-guided percutaneous cutting needle biopsy, and E19del combined with EGFR-T790M mutation was identified by next-generation sequencing (NGS) targeting 168 genes [Figure 3]. Subsequently, the patient was treated with osimertinib (80 mg q.d) and achieved a PR in December 2020. Notably, brain MRI scanning showed the enhanced brain nodule was absorptive.
Unfortunately, in March 2021, she experienced disease progression again, along with highly increasing CEA levels and deep chest tightness. The chest scans showed enlargement of lung nodules, especially in the right lower lobe. NGS was performed by the patient’s plasma sample using a 168-gene panel and identified EGFR 19Del and BRAF V600E, but no EGFR T790M was detected [Figure 3]. Therefore, she began to receive osimertinib (80 mg q.d), dabrafenib (150 mg b.i.d), and trametinib (2 mg q.d) in April 2021. Her symptoms were significantly improved, and her CEA level decreased significantly within three weeks. The CT scan also demonstrated regressed lung nodules. All treatment-related adverse events, including rash, decreased appetite, fatigue, and repeated fever (range from 37.5 to 39.0 °C) were tolerable, graded as 1-2 (Common Terminology Criteria for Adverse Events version 5.0, CTCAE v5.0)[20]. The itching rash was distributed mostly in hands and feet, with spontaneous remission. Pyrexia occurred on the sixth day after the co-inhibition therapy. The co-inhibition therapy was discontinued for only two days when the temperature was as high as 39.0 °C. With physical cooling methods and usage of non-steroidal anti-inflammatory drug, pyrexia could be relieved. Notably, the laboratory test, including blood routine examination, etiological examinations, and C-reactive protein, showed no abnormality during her fever. At the last follow-up (September 2021), her disease evaluation remained stable.
DISCUSSION
BRAFV600E mutation is a rare oncogenic driver, occurring in 1.5%-4.0% of lung adenocarcinomas[7]. In a retrospective multicenter study enrolling 65 NSCLC patients harboring BRAF mutation, 54 patients harbored BRAFV600E mutation and 11 had non-V600E mutations, including K601E, G469S, G469V, G469A, G596R, G466R, and T599dup[21]. An international, multicenter, noncomparative, and open-label trial (BRF113928) showed that the overall response rate of dabrafenib plus trametinib was 63% with response durations ≥ 6 months in 64% of responders[22]. Based on these results, in 2017, the Food and Drug Administration approved dabrafenib and trametinib for first-line treatment of metastatic NSCLC patients harboring BRAFV600E mutation. The update of a phase 2 study (NCT01336634) showed promising efficacy of dabrafenib plus trametinib as second-line treatment, with a median PFS of 10.2 months and a median OS of 18.2 months[23]. However, no clinical trial has been conducted to confirm the efficacy of EGFR/BRAF/MEK co-inhibition in patients harboring E19 and BRAFV600E after the therapy of osimertinib.
To our knowledge, the clinical outcome of EGFR/BRAF/MEK co-targeted therapy has been reported for eight cases. We summarize the clinical characteristics, therapeutic outcome, and toxicities in Table 1. Including our own case, ORR was 55.5% with PFS ≥ 6 months in 66.7% of these nine patients. Eight patients (88.9%) experienced adverse effects (AE), including pyrexia (5/9), nausea (2/9), paronychia (2/9), rash (2/9), fatigue (2/9), decreased appetite (2/9), vomiting (1/9), diarrhea (1/9), dysgeusia (1/9), pneumonitis (1/9), and increased creatine kinase (1/9). Most of these AE were evaluated as low grade, and only a few of them led to dose adjustment and co-inhibition therapy discontinuation. The study characterized the incidence, patterns, and management of pyrexia in patients receiving dabrafenib plus trametinib in clinical trials, concluding that pyrexia is the most common adverse event (61.3%) associated with dabrafenib plus trametinib. The incidence of pyrexia was highest early in treatment, decreased with time on treatment, and was manageable with dose interruption[24]. Pyrexia in the case occurred early in treatment, which was not associated with infectious inflammation. As shown in Table 1, patients (55.6%) with pyrexia tended to have a longer PFS (mean PFS: 8.4 months, 4.7-13.4 months) compared to patients without pyrexia (mean PFS: 4.2 months, 1.5-7.4 months). Although the association between pyrexia and clinical outcome is still unclear, there was a trend towards prolonged PFS in patients with pyrexia in our case and reported cases. Undoubtedly, the association between pyrexia and clinical outcome should be explored using larger sample sizes in future prospective clinical trials.
Table 1.
Overview of literature for osimertinib-induced BRAFV600 mutation with the reported efficacy and treatment toxicities
| Author | Cases | Baseline EGFR mutation | Previous treatment | Mutaion profile at resistance to osimertinib | Treatment | Initial dose | Dose adjustment | Best overall response | Progression free time | Adverse effect (Grade) |
| Huang et al.[13] | 65 Male |
EGFR 19del | Gefitinib → osimertinib | EGFR 19del/T790M, BRAF V600E | D+T+O† | D: 150 mg bid T: 1 mg qd O: 80 mg qd |
Not need | SD | > 7.4 months‡ | Diarrhea (G1), aronychia (G1) |
| Solassol et al.[15] | 68 Female |
EGFR 19del | Chemo → Afatinib → chemo → ICI → osimertinib → chemo + anti-VEGF | EGFR 19del/T790M, BRAF V600E | D+T/O§ | D: 150 mg bid T: 2 mg qd O: 80 mg qd |
Not need | SD | 6 months | NR |
| Ding et al.[19] | 63 Male |
EGFR 19del | Gefitinib → osimertinib | EGFR 19del/T790M, BRAF V600E | D+T+O | D: 150 mg bid T: 2 mg qd O: 80 mg qd |
Not need | SD | 9 months | Pyrexia (G1-2) Aronychia (G1-2) |
| Zhou et al.[16] | 69 Male |
EGFR L858R | Post-operative recurrence, gefitinib→ chemo → osimertinib → chemo | EGFR L858R/T790M, BRAF V600E | D+T+O | D: 150 mg bid T: 2 mg qd O: 80 mg qd |
Not need | PR | > 2 months | Rash (G2), decreased appetite (G2) |
| Meng et al.[17] | P1: 56 Female P2: 66 Male |
P1: EGFR 19del P2: EGFR 19del |
P1: Gefitinib → osimertinib P2: Afatinib → osimertinib |
P1: EGFR E19del, BRAF V600E P2: EGFR 19del/T790M, BRAF V600E |
P1: D+T+OP2: D+T+O | P1/P2: D: 150 mg bid T: 2 mg qd O: 80 mg qd |
P1: discontiuation P2: D: 50 mg bid T: 0.5 mg qd O: 80 mg qd |
/ PR |
P1: 6 weeks P2: 13.4 months |
P1: Pneumonitis P2: Pyrexia (G2), nausea,vomiting |
| Ribeiro et al.[18] | 50 Male |
EGFR 19del | Erlotinib → osimertinib + SBRT → chemo + ICI → chemo | EGFR 19del/T790M, BRAF V600E, PIK3CA mutation | D+T+O | D: 75 mg bid T: 1 mg qd O: 80 mg qd |
D: 150 mg bid T: 2 mg qd O: 80 mg qd (Not succeed) |
PR | 8 months | Pyrexia, dysgueusia, nausea (G1) Fatigue (G1 → G2) |
| Mauclet et al.[14] | 60 Female |
EGFR 19del | Chemo + WBRT → ICI → erlotinib → osimertinib | EGFR E19del/T790M, BRAF V600E | D+T+O | D: 150 mg bid T: 2 mg qd O: 80 mg qd |
D: 75 mg bid T: 1 mg qd O: 40 mg qd |
PR |
7 months | Increased creatine kinase (G3) Prexia (G2) |
| This paper | EGFR 19del | Icotinib → afatinib → osimertinib | EFGR 19del, BRAF V600E | D+T+O | D: 150 mg bid T: 2 mg qd O: 80 mg qd |
Not need | PR | > 4.7 months | Pyrexia (G2), rash (G1), fatigue (G1), nausea (G1), decreased appetite (G1) |
D + T + O: dabrafenib and trametinib plus osimertinib; ‡>: treatment ongoing; §D/T and O treatments were alternated every month. Chemo: Chemotherapy; ICI: immune checkpoint inhibitor; PR: partial response; SD: stable disease; PD: progressive disease; SBRT: stereotactic body radiotherapy; WBRT: whole brain radiotherapy; NR: not reported.
Immunotherapy and chemotherapy are suggested options after the failure of EGFR-TKI treatment according to the National Comprehensive Cancer Network Guidelines for Non-Small Cell Lung Cancer (2021). However, for BRAFV600E mutated patients, a previous study showed limited efficacy for chemotherapy, with a first-line objective response rate (ORR) of 23% and second-line ORR of only 9%[25]. As for immunotherapy, research has revealed that ORR with immune checkpoint inhibitors (ICIs) was 24% in BRAF mutation patients, although BRAF mutation NSCLC was associated with high levels of PD-L1 expression[26]. In JTO Clinical and Research Reports, Zhang et al.[27] reported that BRAFV600E mutation was associated with worse clinical outcome for ICIs (median OS, BRAFV600E vs. non-V600E: 5 months vs. 14 months, P = 0.017). Compared with chemotherapy and immunotherapy, better clinical outcomes have been observed in patients treated by anti-BRAF with or without anti-MEK therapy[21,28]. Taken together, it is worth considering EGFR/BRAF/MEK co-inhibition as second-line treatment options for EGFR-mutated NSCLC patients with BRAFV600E mutation.
With the development of genetic tests, great advances have been made in targeted therapy for lung cancer. The accurate identification of predictive genetic alterations is important for patient management, life quality, and prognosis, as well as the understanding of AR mechanism to different therapies[4]. The case is a typical long-term treatment management guided by multiple genetic tests. At the time when cancer cells of our patient developed afatinib resistance, an EGFR T790M was identified by NGS on lung biopsy but without targeting driver mutation found in her peripheral blood NGS test. This result might be due to the higher sensitivity in the genetic test derived from tumor tissues. However, she suffered a rapid disease progression with a very short duration of response. It is reported that, despite the high sensitivity, tissue genetic analysis has difficulty representing the whole driver gene mutation profile because of spatial heterogeneity. The reason for the fast progression for osimertinib in our case might be the existence of other undetected resistance mechanisms. The principal manifestation of this patient’s progressive disease was lymphangitis carcinoma of the lung, which increased the difficulty of tumor tissue biopsy. Liquid biopsy may be better than tissue analysis, as it has the potential to represent tumor heterogeneity and clonal diversification[29]. Several studies emphasized the guiding role of monitoring the dramatic change of the driving mutation by circulating free DNA test[30,31]. Therefore, liquid (peripheral blood and pleural effusion) biopsy and tissue genetic analysis complement each other, and the reasonable choice of detection sample type, method, and platform plays an important role in the accuracy of precision medicine, especially in patients suffering drug resistance. Additionally, a study indicated that serum CEA determinations are a feasible, noninvasive option for monitoring and prognosis[32]. Similar to the previous result, in our case, the change of serum CEA also remained consistent with anti-tumor response.
In conclusion, a strong and fast response to osimertinib plus dabrafenib and trametinib was observed in this case of resistance in a patient with BRAFV600E mediated AR under osimertinib therapy, which has lasted for more than four months. Our case further enriches the clinical evidence of the efficacy of EGFR/BRAF/MEK co-inhibition in patients with an acquired BRAFV600E mutation, consistent with the review of the literature (eight cases). Additionally, our case highlights the important role of sample type, method, and platform of gene detection in patient management, life quality, and prognosis, as well as the understanding of acquired resistance mechanism.
DECLARATIONS
Authors’ contributions
Contributed to conception, design, interpretation of data, drafted and critically revised the manuscript: Gao B, Xiang Y
Contributed to acquisition of data, analysis of data, and drafted the manuscript: Zeng R, Luo L, Sun X, Bao Z, Du W, Dai R, Tang W
Availability of data and materials
Not applicable.
Financial support and sponsorship
This work was supported by the Shanghai Municipal Key Clinical Specialty (shslczdzk02202), and the National Natural Science Foundation of China (81672271).
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Copyright
© The Author(s) 2021.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Rosell R, Moran T, Queralt C, et al. Spanish Lung Cancer Group. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361:958–67. doi: 10.1056/NEJMoa0904554. [DOI] [PubMed] [Google Scholar]
- 3.Shi Y, Au JS, Thongprasert S, et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER) J Thorac Oncol. 2014;9:154–62. doi: 10.1097/JTO.0000000000000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Recondo G, Facchinetti F, Olaussen KA, Besse B, Friboulet L. Making the first move in EGFR-driven or ALK-driven NSCLC: first-generation or next-generation TKI? Nat Rev Clin Oncol. 2018;15:694–708. doi: 10.1038/s41571-018-0081-4. [DOI] [PubMed] [Google Scholar]
- 5.Rotow J, Bivona TG. Understanding and targeting resistance mechanisms in NSCLC. Nat Rev Cancer. 2017;17:637–58. doi: 10.1038/nrc.2017.84. [DOI] [PubMed] [Google Scholar]
- 6.Ohashi K, Sequist LV, Arcila ME, et al. Lung cancers with acquired resistance to EGFR inhibitors occasionally harbor BRAF gene mutations but lack mutations in KRAS, NRAS, or MEK1. Proc Natl Acad Sci U S A. 2012;109:E2127–33. doi: 10.1073/pnas.1203530109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417:949–54. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 8.Subbiah V, Baik C, Kirkwood JM. Clinical development of BRAF plus MEK inhibitor combinations. Trends Cancer. 2020;6:797–810. doi: 10.1016/j.trecan.2020.05.009. [DOI] [PubMed] [Google Scholar]
- 9.Yao Z, Torres NM, Tao A, et al. BRAF mutants evade ERK-dependent feedback by different mechanisms that determine their sensitivity to pharmacologic inhibition. Cancer Cell. 2015;28:370–83. doi: 10.1016/j.ccell.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oxnard GR, Hu Y, Mileham KF, et al. Assessment of resistance mechanisms and clinical implications in patients with EGFR T790M-positive lung cancer and acquired resistance to osimertinib. JAMA Oncol. 2018;4:1527–34. doi: 10.1001/jamaoncol.2018.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leonetti A, Sharma S, Minari R, Perego P, Giovannetti E, Tiseo M. Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer. Br J Cancer. 2019;121:725–37. doi: 10.1038/s41416-019-0573-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho CC, Liao WY, Lin CA, Shih JY, Yu CJ, Yang JC. Acquired BRAF V600E mutation as resistant mechanism after treatment with osimertinib. J Thorac Oncol. 2017;12:567–72. doi: 10.1016/j.jtho.2016.11.2231. [DOI] [PubMed] [Google Scholar]
- 13.Huang Y, Gan J, Guo K, Deng Y, Fang W. Acquired BRAF V600E mutation mediated resistance to osimertinib and responded to osimertinib, dabrafenib, and trametinib combination therapy. J Thorac Oncol. 2019;14:e236–7. doi: 10.1016/j.jtho.2019.05.040. [DOI] [PubMed] [Google Scholar]
- 14.Mauclet C, Collard P, Ghaye B, Hoton D, Nana FA. Tumor response to EGFR/BRAF/MEK co-inhibition in a patient with EGFR mutated lung adenocarcinoma developing a BRAFV600 mutation as an acquired resistance mechanism. Lung Cancer. 2021;159:42–4. doi: 10.1016/j.lungcan.2021.06.025. [DOI] [PubMed] [Google Scholar]
- 15.Solassol J, Vendrell JA, Senal R, Audran P, Leenhardt F, Quantin X. Challenging BRAF/EGFR co-inhibition in NSCLC using sequential liquid biopsies. Lung Cancer. 2019;133:45–7. doi: 10.1016/j.lungcan.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Zhou F, Zhao W, Chen X, Zhang J, Zhou C. Response to the combination of dabrafenib, trametinib and osimertinib in a patient with EGFR-mutant NSCLC harboring an acquired BRAFV600E mutation. Lung Cancer. 2020;139:219–20. doi: 10.1016/j.lungcan.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Meng P, Koopman B, Kok K, et al. Combined osimertinib, dabrafenib and trametinib treatment for advanced non-small-cell lung cancer patients with an osimertinib-induced BRAF V600E mutation. Lung Cancer. 2020;146:358–61. doi: 10.1016/j.lungcan.2020.05.036. [DOI] [PubMed] [Google Scholar]
- 18.Ribeiro MFSA, Knebel FH, Bettoni F, et al. Impressive response to dabrafenib, trametinib, and osimertinib in a metastatic EGFR-mutant/BRAF V600E lung adenocarcinoma patient. NPJ Precis Oncol. 2021;5:5. doi: 10.1038/s41698-021-00149-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ding H, Zhuang Z, Xie J, Huang H, Tao Z, Liu Z. Durable clinical response of advanced lung adenocarcinoma harboring EGFR-19del/T790M/BRAFV600E mutations after treating with osimertinib and dabrafenib plus trametinib: a case report. Onco Targets Ther. 2020;13:7933–9. doi: 10.2147/OTT.S240775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. US Department of Health and Human Services. Common Terminology criteria for adverse events. Version 5.0. Published November 27, 2017. (2020). [Google Scholar]
- 21.Mu Y, Yang K, Hao X, et al. Clinical characteristics and treatment outcomes of 65 patients with BRAF-mutated non-small cell lung cancer. Front Oncol. 2020;10:603. doi: 10.3389/fonc.2020.00603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Planchard D, Besse B, Groen HJM, et al. Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol. 2016;17:984–93. doi: 10.1016/s1470-2045(16)30146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Planchard D, Besse B, Groen HJM, et al. Phase 2 study of dabrafenib plus trametinib in patients with BRAF V600E-mutant metastatic NSCLC: updated 5-year survival rates and genomic analysis. J Thorac Oncol. 2021;S1556-0864(21)02403 doi: 10.1016/j.jtho.2021.08.011. [DOI] [PubMed] [Google Scholar]
- 24.Schadendorf D, Robert C, Dummer R, et al. Pyrexia in patients treated with dabrafenib plus trametinib across clinical trials in BRAF-mutant cancers. Eur J Cancer. 2021;153:234–41. doi: 10.1016/j.ejca.2021.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Barlesi F, Mazieres J, Merlio J, et al. Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT) Lancet. 2016;387:1415–26. doi: 10.1016/S0140-6736(16)00004-0. [DOI] [PubMed] [Google Scholar]
- 26.Dudnik E, Peled N, Nechushtan H, et al. Israel Lung Cancer Group. BRAF mutant lung cancer: programmed death ligand 1 expression, tumor mutational burden, microsatellite instability status, and response to immune check-point inhibitors. J Thorac Oncol. 2018;13:1128–37. doi: 10.1016/j.jtho.2018.04.024. [DOI] [PubMed] [Google Scholar]
- 27.Zhang C, Zhang C, Lin J, Li Z, Wang H. Patients with BRAF-mutant NSCLC may not benefit from immune checkpoint inhibitors: a population-based study. JTO Clin Res Rep. 2020;1:100006. doi: 10.1016/j.jtocrr.2020.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mazieres J, Drilon A, Lusque A, et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann Oncol. 2019;30:1321–8. doi: 10.1093/annonc/mdz167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jóri B, Schatz S, Kaller L, et al. Comparison of resistance spectra after first and second line osimertinib treatment detected by liquid biopsy. Cancers (Basel) 2021;13:2861. doi: 10.3390/cancers13122861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nichols D, Boyle TA, Noyes D, et al. Evaluation of combined anti-PD-1 immunotherapy and radiation therapy in a preclinical mouse model of pneumonitis and fibrosis. J Thorac Dis. 2018;10:6254–60. doi: 10.21037/jtd.2018.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Miranda FS, Barauna VG, Dos Santos L, Costa G, Vassallo PF, Campos LCG. Properties and application of cell-free DNA as a clinical biomarker. Int J Mol Sci. 2021;22:9110. doi: 10.3390/ijms22179110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arrieta O, Varela-Santoyo E, Cardona AF, et al. Association of carcinoembryonic antigen reduction with progression-free and overall survival improvement in advanced non-small-cell lung cancer. Clin Lung Cancer. 2021;22:510–22. doi: 10.1016/j.cllc.2021.03.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.