Abstract
Objective
We evaluated exercise interventions for cognitive appraisal of chronic low back pain (cLBP) in an underserved population.
Methods
We conducted a secondary analysis of the Back to Health Trial, showing yoga to be noninferior to physical therapy (PT) for pain and function outcomes among adults with cLBP (n = 320) recruited from primary care clinics with predominantly low-income patients. Participants were randomized to 12 weeks of yoga, PT, or education. Cognitive appraisal was assessed with the Pain Self-Efficacy Questionnaire (PSEQ), Coping Strategies Questionnaire (CSQ), and Fear-Avoidance Beliefs Questionnaire (FABQ). Using multiple imputation and linear regression, we estimated within- and between-group changes in cognitive appraisal at 12 and 52 weeks, with baseline and the education group as references.
Results
Participants (mean age = 46 years) were majority female (64%) and majority Black (57%), and 54% had an annual household income <$30,000. All three groups showed improvements in PSEQ (range 0–60) at 12 weeks (yoga, mean difference [MD] = 7.0, 95% confidence interval [CI]: 4.9, 9.0; PT, MD = 6.9, 95% CI: 4.7 to 9.1; and education, MD = 3.4, 95% CI: 0.54 to 6.3), with yoga and PT improvements being clinically meaningful. At 12 weeks, improvements in catastrophizing (CSQ, range 0–36) were largest in the yoga and PT groups (MD = –3.0, 95% CI: –4.4 to –1.6; MD = –2.7, 95% CI: –4.2 to –1.2, respectively). Changes in FABQ were small. No statistically significant between-group differences were observed on PSEQ, CSQ, or FABQ at either time point. Many of the changes observed at 12 weeks were sustained at 52 weeks.
Conclusion
All three interventions were associated with improvements in self-efficacy and catastrophizing among low-income, racially diverse adults with cLBP.
Trial registration
ClinicalTrials.gov identifier NCT01343927.
Keywords: Back Pain, Chronic Pain, Yoga, Physical Therapy, Self-Efficacy, Coping Skills
Introduction
Chronic low back pain (cLBP) is a leading cause of disability and health care cost in the United States [1, 2]. Low-income and racially diverse adults report greater pain severity, disability, and psychological comorbidities [3, 4]. Evidence suggests that how patients perceive and cope with pain is predictive of cLBP outcomes [5, 6].
We will use the term “cognitive appraisal of pain” to describe three constructs of an individual’s psychological response to pain: self-efficacy, coping strategies (e.g., catastrophizing) and fear avoidance [7, 8]. Low self-efficacy, high catastrophizing, and high fear-avoidance beliefs prospectively predict worse recovery in patients with cLBP [9]. Increasing self-efficacy is associated with improvements in physical function, independent of pain severity [10]. Psychological interventions for pain (e.g., cognitive behavioral therapy) have been shown to work via improvements in cognitive appraisal of pain [11, 12]. Less is known about the effect of exercise-oriented interventions on cognitive appraisal in adults with cLBP.
Yoga and physical therapy (PT) are evidence-based treatments for cLBP that include physical activity as a major component [13, 14]. Previous clinical trials have suggested that yoga improves self-efficacy in adults with cLBP [8, 15, 16], with one study demonstrating increased self-efficacy as a mediator of improved back-related disability [8]. Less is known about the effects of yoga interventions on fear avoidance and catastrophizing among adults with cLBP. PT and exercise therapy can improve catastrophizing and fear avoidance [17–21]. The effect of PT on self-efficacy is less established. A recent systematic review reported that exercise interventions may increase self-efficacy [22], and we are aware of a single retrospective study of PT for cLBP that observed that changes in self-efficacy mediated improvement in back-related disability [23]. We are unaware of any yoga or PT studies that have measured short- and long-term changes in cognitive appraisal of pain among adults with cLBP from low-income and racially diverse populations.
The purpose of our study was to determine whether yoga and PT improve cognitive appraisal of pain among adults with cLBP as compared with an educational intervention. We used data from the Back to Health Study, which randomized 320 adults with cLBP to 12-week yoga, PT, and education interventions [24]. The Back to Health Study found yoga to be noninferior to PT for pain and physical function outcomes [25]. Prior research using this sample found that baseline cognitive appraisal of pain predicted 12-week improvements in physical function [26]. Here, we hypothesized that a 12-week yoga or PT treatment would result in greater improvements in self-efficacy, coping, and fear avoidance than would an educational intervention, both immediately after the intervention and at 1-year follow-up. We also explored whether improvements in cognitive appraisal of pain were associated with short- and long-term improvements in back pain and physical function.
Methods
Study Design
We performed a secondary analysis of the Back to Health Study, a single-blinded randomized controlled trial that compared the effectiveness of yoga, PT, and a back pain education book among 320 low-income adults with cLBP. The methods for the Back to Health Study and previously reported findings are described in detail elsewhere [24, 25]. Participants were recruited from an academic safety net hospital and seven federally qualified community health centers. Adults (ages 18–64 years) were eligible for the trial if they had nonspecific cLBP of ≥12 weeks’ duration and average pain intensity over the prior week of ≥4 (0–10 scale). All subjects provided written informed consent before participation in this study. This research was reviewed and approved by the Boston University Institutional Review Board.
Participants were randomized in a 2:2:1 ratio to yoga classes, one-on-one PT sessions, or an educational book, respectively. The study consisted of a 12-week treatment phase followed by a 40-week maintenance phase, during which the yoga and PT groups were additionally randomized to continue receiving in-person treatment (i.e., yoga drop-in sessions, PT booster sessions) or home practice only. Because clinical outcomes were similar across the drop-in and home practice groups at the end of the maintenance phase [25], we have collapsed the yoga and PT subgroups for our 52-week analysis.
Randomization, study survey administration, and data entry were all conducted by staff blinded to participants’ treatment groups.
Interventions
A manualized yoga for back pain intervention was delivered in small groups by hatha yoga instructors [24]. This approach included 12 weekly 75-minute sessions. These sessions consisted of meditative exercises, breathing sequences, and yoga poses. The 12-week treatment period was divided into four 3-week segments—each segment consisting of 15 to 19 poses, which were tailored to the specific abilities of each participant through modifications. Daily DVD-aided home practice was encouraged.
One-on-one PT was delivered by a physical therapist in either a hospital or a community-based outpatient setting [24]. The physical therapists used a treatment-based classification system to select a program of graded exercises during 15 visits. All participants received instructional materials for home practice and were encouraged to exercise for 30 minutes on days when they did not have a PT appointment.
Participants randomized to the education group received the Back Pain Helpbook, a comprehensive guide to back pain self-care that describes causes of back pain and multiple methods of managing pain [27]. The book includes a comprehensive exercise and strength training program, lifestyle modifications, and information on the role of emotions in the perception of pain. The role of cognitive appraisal of pain (e.g., fear-avoidance beliefs) is described, as are relevant coping skills (e.g., distraction from pain, reinterpretation of pain) and mind-body practices (breathing and meditation). Readers are encouraged to avoid bed rest and remain active despite symptoms. Participants were mailed summary sheets of key information from chapters at 3, 6, 9, and 12 weeks and received phone calls from study staff encouraging participants to complete their reading assignment.
Measurement
Self-efficacy was measured with the Pain Self-Efficacy Questionnaire (PSEQ) [28]. The PSEQ is a 10-item questionnaire that asks participants to rate on a scale of 0–6 current feelings of confidence in performing activities despite the presence of pain. Total PSEQ scores range from 0 to 60, with larger scores indicating increased pain self-efficacy.
Catastrophizing and cognitive coping were measured with two subscales of the Coping Strategies Questionnaire (CSQ) [29]. The 23-item CSQ consists of statements related to one of four domains: catastrophizing, cognitive coping, reinterpreting, and diversion. Participants were asked to rate their use of pain-related coping behaviors on a seven-point Likert scale (values ranging from 0 to 6). Subscale scores range from 0 to 36. Higher scores represent reliance on that coping domain but do not necessarily mean adaptiveness. For example, higher values of the catastrophizing subscale (CSQ-CAT) score represent greater reliance on catastrophizing, a maladaptive behavior. In contrast, higher CSQ-CC is adaptive and reflects a greater ability to persevere despite pain. We focused on changes in catastrophizing (CSQ-CAT) and cognitive coping (CSQ-CC) because these coping skills have been hypothesized to be strong predictors of functional outcomes in adults with cLBP [18, 30].
Fear-avoidance beliefs were measured with the 16-item Fear-Avoidance Beliefs Questionnaire (FABQ) [31]. Patients rated their agreement with each question on a seven-point Likert scale ranging from 0 (completely disagree) to 6 (completely agree). Higher aggregate scores indicate stronger fear-avoidance beliefs. Two subscales within the FABQ are work (seven-question FABQ-W, scores 0–42), and physical activity (four-question FABQ-PA, scores 0–24). FABQ-W assesses the fear of losing work because of pain, and the FABQ-PA assesses the relationship between physical activity and pain exacerbation.
We measured average pain in the prior week on an 11-point numerical rating scale (where 0 = no pain at all and 10 = the worst possible pain) [32]. Back-specific physical functioning was measured with the modified Roland Morris Disability Questionnaire (RMDQ), a 23-point scale on which a higher score indicated a greater level of disability [33, 34].
Covariates
Baseline sociodemographic factors included age, sex, race (white, nonwhite), ethnicity (Hispanic, non-Hispanic), birthplace (United States, non–United States), primary language (English, non-English), annual income (≤$30,000, >$30,000), level of education (no college degree, college degree or higher), and employment status (employed, unemployed).
Outcomes
For our main analysis, we were interested in the changes of cognitive appraisal subscales over time. All three scales, PSEQ, CSQ, and FABQ, were assessed at baseline, 12, and 52 weeks, and the FABQ was additionally assessed at 6, 26, and 40 weeks. The primary outcome was the change score, or the change in each measure of cognitive appraisal from baseline to 12 weeks. We also assessed change scores from the baseline to 52 weeks. We were interested in comparing both within- and between-group differences.
For our secondary analysis, we defined “responders” as the proportion of participants who achieved at least the minimal clinically important difference (MCID) on each measure by treatment group. We used the established MCIDs for PSEQ, FABQ-W, and FABQ-PA of 5.5, 7, and 4 points, respectively [35, 36]. For CSQ-CC or CSQ-CAT, which do not have an established MCID, we identified those who had at least a 30% improvement and used this in place of the MCID [37].
In additional exploratory analyses, we evaluated the relationships among cognitive appraisal, pain, and function in two ways. First, we assessed the concurrent changes in pain and physical function at 12 and 52 weeks, relative to each cognitive appraisal scale. Second, we compared changes in pain and disability at 12 and 52 weeks between those who had a clinically important improvement in cognitive appraisal and those at 12 weeks who did not.
Analysis
Baseline characteristics were compared across treatment groups with the use of analysis of variance and chi-squared tests for continuous and categorical variables, respectively.
To evaluate within- and between-group changes for each outcome, separate linear regression models were fitted to estimate the change score in relation to each treatment group, with adjustment for baseline sociodemographic characteristics, pain, and back-related disability (RMDQ). We estimated between-group differences in each outcome for yoga and PT relative to the education group. For the purposes of interpreting the magnitude of change, or the effect size, we calculated Cohen’s d score for each scale. Effect sizes were classified as small (d = 0.20–0.49), medium (d = 0.50–0.79), or large (d ≥ 0.80) [38].
Separate logistic regression models were fitted to estimate the odds of having at least the MCID improvement, or “response,” on the PSEQ, CSQ, and FABQ with adjustment for baseline sociodemographic characteristics, pain, and back-related disability (RMDQ). There was no adjustment for multiple testing.
We used linear regression adjusted for sociodemographic characteristics, baseline pain, and disability to determine whether a clinically meaningful improvement in PSEQ, CSQ, or FABQ subscale scores at 12 weeks was associated with a concurrent change in pain or disability over the intervention period (0 to 12 weeks) or a future change over the remaining follow-up period (12 to 52 weeks). We additionally calculated Pearson correlation coefficients between continuous versions of the scales across 1) baseline values, 2) changes during the intervention period (0 to 12 weeks), and 3) intervention period changes with follow-up period (12 to 52 weeks) changes.
To account for missing data, we used 20-fold multiple imputation with fully conditional specification [39, 40]. Sensitivity analyses included the use of data from participants with complete follow-up, specific to each time point and measure of cognitive appraisal. Statistical significance was defined as P < 0.05. All analyses were conducted with SAS software version 9.4 (© 2013 SAS Institute, Inc., Cary, NC, USA).
Results
Baseline Participant Characteristics
All participant characteristics were balanced among groups, except for gender and RMDQ score (Table 1). Most participants (mean age = 46 years, standard deviation [SD] = 10.7) were female (64%), most were Black (57%), and 54% had an annual household income <$30,000.
Table 1.
Characteristics of 320 participants with chronic lower back pain by treatment group*
| Characteristics† | Overall | Yoga | PT | Education |
|---|---|---|---|---|
| (n = 320) | (n = 127) | (n = 129) | (n = 64) | |
| Sociodemographic measures | ||||
| Age, years | 45.9 ± 10.7 | 46.7 ± 10.2 | 46.0 ± 11.4 | 44.3 ± 10.3 |
| Female, n (%) | 204 (64) | 72 (57) | 90 (70) | 42 (66) |
| Race, Black, n (%) | 183 (57) | 71 (56) | 73 (57) | 39 (61) |
| Ethnicity, Hispanic, n (%) | 43/316 (14) | 20/126 (16) | 17/127 (13) | 6/63 (10) |
| Born in the United States, n (%) | 226/302 (75) | 91/124 (73) | 84/116 (72) | 51/62 (82) |
| English is primary language, n (%) | 268 (84) | 108 (85) | 106 (82) | 54 (84) |
| Annual income ≤$30,000, n (%) | 159/294 (54) | 62/120 (52) | 61/115 (53) | 36/59 (61) |
| College degree or higher, n (%) | 93/317 (29) | 38/125 (30) | 30/128 (23) | 25 (39) |
| Currently employed, n (%) | 143 (45) | 60 (47) | 53 (41) | 30 (47) |
| Clinical measures | ||||
| PSEQ | 37.0 ± 13.8 | 37.3 ± 14.8 | 35.9 ± 13.6 | 38.5 ± 11.8 |
| CSQ-CAT | 13.1 ± 8.2 | 12.8 ± 8.6 | 14.3 ± 8.0 | 11.6 ± 7.7 |
| CSQ-CC | 22.2 ± 8.1 | 22.6 ± 8.0 | 21.9 ± 8.6 | 21.8 ± 7.0 |
| FABQ-W | 15.2 ± 11.9 | 14.2 ± 11.8 | 16.6 ± 11.8 | 14.4 ± 12.2 |
| FABQ-PA | 13.1 ± 6.6 | 13.2 ± 7.0 | 13.3 ± 6.4 | 12.2 ± 6.5 |
| NRS | 7.1 ± 1.4 | 7.1 ± 1.5 | 7.2 ± 1.5 | 7.0 ± 1.4 |
| RMDQ | 14.8 ± 5.3 | 13.9 ± 5.6 | 15.6 ± 5.1 | 15.0 ± 5.0 |
NRS = numerical rating scale for back pain.
All values are mean ± SD unless otherwise specified. Percentages may not sum to 100 because of rounding.
Baseline between-group differences were present for gender (P = 0.02) and RMDQ score (P = 0.03).
The mean score with standard deviation [SD] for the PSEQ was 37.0 ± 13.8, which represents moderate to poor self-efficacy [35]. The CSQ-CAT and CSQ-CC mean and SD scores were 13.1 ± 8.2 and 22.2 ± 8.1, respectively. Mean and SD baseline scores for the FABQ-W and FABQ-PA were 15.2 ± 11.9 and 13.1 ± 6.6, respectively. Mean CSQ and FABQ scores represent moderate catastrophizing scores and mild fear-avoidance beliefs scores.
The pattern of missing data is illustrated in the Supplementary Data. At 12 and 52 weeks, data completion rates were highest in the yoga (98% and 83%, respectively) and education (92% and 86%) groups and lower in the PT group (78% and 68%). The Supplementary Data display baseline demographics among participants with complete data on all outcome measures after 12 weeks of follow-up (n = 283).
Changes in Cognitive Appraisal over Time
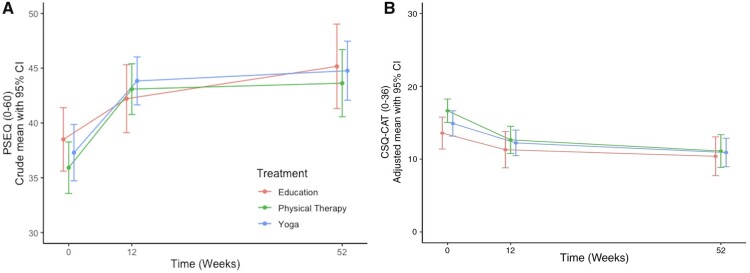
Adjusted short- and long-term changes in cognitive appraisal of pain are presented in Table 2. Pain self-efficacy and catastrophizing scores were plotted over 52 weeks in Figure 1 (Panels A–B).
Table 2.
Adjusted within- and between- group changes in pain self-efficacy, pain coping skills, and fear-avoidance beliefs at 12 and 52 weeks, with missing data imputed
| Within-Group Change from Baseline‡ |
Between-Group Differences‡ |
|||
|---|---|---|---|---|
| Outcome Measure | Mean (95% CI) | Cohen’s d | Mean (95% CI) | Cohen’s d |
| 12-week PSEQ | ||||
| Yoga | 6.98 (4.93 to 9.04) | 0.59† | 3.56 (0 to 7.12) | 0.30* |
| PT | 6.90 (4.70 to 9.09) | 0.54† | 3.47 (−0.12 to 7.07) | 0.28* |
| Education | 3.43 (0.54 to 6.31) | 0.29* | Reference | |
| 52−week PSEQ | ||||
| Yoga | 8.18 (5.74 to 10.63) | 0.58† | 2.16 (−2.11 to 6.42) | 0.15 |
| PT | 7.35 (4.46 to 10.23) | 0.44† | 1.32 (−3.3 to 5.94) | 0.08 |
| Education | 6.03 (2.53 to 9.52) | 0.42† | Reference | |
| 12-week CSQ-CAT | ||||
| Yoga | −2.98 (−4.35 to −1.60) | −0.38* | −1.25 (−3.67 to 1.18) | −0.16 |
| PT | −2.72 (−4.21 to −1.24) | −0.32* | −0.99 (−3.46 to 1.47) | −0.12 |
| Education | −1.73 (−3.70 to 0.24) | −0.22* | Reference | |
| 52-week CSQ-CAT | ||||
| Yoga | −4.46 (−6.16 to −2.77) | −0.46† | −1.65 (−4.43 to 1.14) | −0.17 |
| PT | −4.24 (−6.07 to −2.41) | −0.40* | −1.42 (−4.38 to 1.53) | −0.14 |
| Education | −2.82 (−5.09 to −0.54) | −0.30* | Reference | |
| 12-week CSQ-CC | ||||
| Yoga | 0.65 (−0.84 to 2.13) | 0.08 | −0.02 (−2.62 to 2.59) | 0.00 |
| PT | 0.17 (−1.61 to 1.95) | 0.02 | −0.49 (−3.15 to 2.17) | −0.05 |
| Education | 0.66 (−1.46 to 2.78) | 0.08 | Reference | |
| 52−week CSQ-CC | ||||
| Yoga | −0.25 (−2.15 to 1.66) | −0.02 | −2.41 (−5.83 to 1.01) | −0.22* |
| PT | −0.64 (−2.83 to 1.54) | −0.05 | −2.81 (−6.24 to 0.62) | −0.23* |
| Education | 2.16 (−0.57 to 4.89) | 0.19 | Reference | |
| 12-week FABQ-W | ||||
| Yoga | −1.13 (−3.08 to 0.82) | −0.10 | 0.55 (−2.99 to 4.08) | 0.05 |
| PT | −0.45 (−2.81 to 1.91) | −0.03 | 1.23 (−2.29 to 4.75) | 0.09 |
| Education | −1.68 (−4.61 to 1.25) | −0.14 | Reference | |
| 52-week FABQ-W | ||||
| Yoga | −2.64 (−4.89 to −0.39) | −0.20* | 0.55 (−3.12 to 4.22) | 0.04 |
| PT | −3.67 (−5.97 to −1.36) | −0.28* | −0.48 (−4.14 to 3.18) | −0.04 |
| Education | −3.19 (−6.17 to −0.21) | −0.26* | Reference | |
| 12-week FABQ-PA | ||||
| Yoga | −0.80 (−2.08 to 0.47) | −0.11 | −0.40 (−2.63 to 1.82) | −0.05 |
| PT | −0.13 (−1.60 to 1.35) | −0.01 | 0.27 (−2.05 to 2.59) | 0.03 |
| Education | −0.40 (−2.23 to 1.43) | −0.05 | Reference | |
| 52-week FABQ-PA | ||||
| Yoga | −1.29 (−2.85 to 0.28) | −0.14 | −0.26 (−2.83 to 2.31) | −0.03 |
| PT | −1.75 (−3.78 to 0.28) | −0.15 | −0.73 (−3.61 to 2.15) | −0.07 |
| Education | −1.03 (−3.13 to 1.07) | −0.12 | Reference | |
Cohen’s d values with asterisk (*) indicating small effect size (0.2–0.4) and dagger (†) indicating medium effect size (0.41–0.7).
Adjusted for age, gender, baseline score on the numerical rating scale for back pain, and RMDQ score.
Figure 1.
Changes in cognitive appraisal of pain over 52 weeks, with missing data imputed. (A) Pain self-efficacy (PSEQ). (B) Catastrophizing (CSQ-CAT).
PSEQ scores improved among all three groups at 12 weeks (yoga, mean difference [MD] = 7.0, 95% confidence interval [CI]: 4.9 to 9.0; PT, MD = 6.9, 95% CI: 4.7 to 9.1; and education, MD = 3.4, 95% CI: 0.5 to 6.3); these improvements remained at 52 weeks. Medium 12-week effect sizes were seen in PSEQ change scores among yoga (0.59) and PT participants (0.54).
At 12 weeks, CSQ-CAT scores were reduced only in the yoga and PT groups (yoga, MD = –3.0, 95% CI: –4.4 to –1.6; PT, MD = –2.7, 95% CI: –4.2 to –1.2). All three treatment groups showed reductions in CSQ-CAT at 52 weeks. No between-group differences in CSQ-CAT or CSC-CC change scores at 12 or 52 weeks were observed. The mean CSQ-CC scores did not change from baseline in any treatment group.
There were no within-group FABQ-W or FABQ-PA changes at 12 weeks. There were no between-group differences at either follow-up time.
Changes in complete case analyses for the PSEQ and CSQ were generally similar in direction and magnitude to those with multiple imputation for missing data (Supplementary Data).
Relationships Among Cognitive Appraisal, Pain, and Function
Table 3 provides the proportion of participants who had clinically meaningful improvements in cognitive appraisal of pain. Clinically meaningful improvement in cognitive appraisal did not differ between treatment groups. For most measures, clinically meaningful improvements in cognitive appraisal were associated with larger post-intervention improvements in pain and physical function (Table 4). For example, those with a clinically meaningful improvement in the PSEQ at the end of the intervention (week 12) experienced an additional 0.80-point improvement in pain and a 2.56-point improvement in disability at week 12, compared with those without a clinical meaningful improvement in the PSEQ. Results were similar with continuous versions of most measures of cognitive appraisal (Supplementary Data).
Table 3.
Adjusted odds ratio of participants reporting a minimal clinically important improvement in pain self-efficacy, pain coping skills, and fear-avoidance beliefs among those with follow-up data at 12 or 52 weeks
| Total | 12 Weeks |
52 Weeks |
|||
|---|---|---|---|---|---|
| Improvement by MCID† or Greater* |
Improvement by MCID† or Greater* |
||||
| Measures | N‡ | n/N (%)‡ | Odds Ratio (95% CI) | n/N (%)‡ | Odds Ratio (95% CI) |
| PSEQ | |||||
| Yoga | 110 | 61/107 (57) | 1.73 (0.89 to 3.37) | 56/90 (62) | 2.14 (1.01 to 4.52) |
| PT | 118 | 50/92 (54) | 1.53 (0.77 to 3.01) | 47/76 (62) | 1.81 (0.84 to 3.88) |
| Education | 60 | 24/55 (44) | Reference | 26/50 (52) | Reference |
| CSQ-CAT§ | |||||
| Yoga | 127 | 58/124 (47) | 1.72 (0.89 to 3.31) | 62/106 (58) | 1.57 (0.79 to 3.14) |
| PT | 129 | 42/100 (42) | 1.43 (0.73 to 2.81) | 44/82 (54) | 1.21 (0.60 to 2.46) |
| Education | 64 | 21/59 (36) | Reference | 28/54 (52) | Reference |
| CSQ-CC§ | |||||
| Yoga | 91 | 24/89 (27) | 1.06 (0.46 to 2.46) | 30/76 (39) | 1.00 (0.45 to 2.24) |
| PT | 92 | 21/70 (30) | 1.24 (0.53 to 2.91) | 20/58 (34) | 0.86 (0.37 to 1.99) |
| Education | 49 | 12/45 (27) | Reference | 14/42 (38) | Reference |
| FABQ-W | |||||
| Yoga | 85 | 29/82 (35) | 0.71 (0.32 to 1.57) | 34/71 (48) | 1.08 (0.47 to 2.51) |
| PT | 94 | 29/71 (41) | 0.84 (0.37 to 1.89) | 27/59 (46) | 0.96 (0.40 to 2.30) |
| Education | 45 | 17/40 (43) | Reference | 17/37 (46) | Reference |
| FABQ-PA | |||||
| Yoga | 113 | 35/111 (32) | 1.34 (0.63 to 2.85) | 28/95 (29) | 0.60 (0.28 to 1.27) |
| PT | 117 | 25/90 (28) | 1.09 (0.50 to 2.39) | 26/73 (33) | 0.70 (0.32 to 1.51) |
| Education | 56 | 14/53 (26) | Reference | 20/48 (42) | Reference |
Adjusted for baseline age, gender, baseline score on the numerical rating scale for back pain, and RMDQ score.
An MCID improvement was defined as 5.5 points on the PSEQ for pain self-efficacy and 7 points on the FABQ-W scale and 4 points on the FABQ-PA scale for work- and physical activity–related fear-avoidance beliefs, respectively.
A 30% improvement in CSQ subscales was used to indicate a clinically important improvement, as an established MCID was not known.
Participants whose baseline scores showed they could not improve by the MCID were removed, i.e., 32 participants (10%) for the PSEQ, 88 participants (27.5%) for the CSQ-CC, 96 (30%) for the FABQ-W, and 34 (11%) for the FABQ-PA. Participants who had missing data at 12 weeks and 52 weeks were removed from each column, respectively.
Table 4.
The association of minimal clinically important improvements in self-efficacy, coping skills, and fear avoidance by 12 weeks with changes in pain and physical function during the treatment phase and follow-up period, with missing data imputed
| Total | Pain, Mean Change (95% CI)* |
RMDQ, Mean Change (95% CI)* |
|||
|---|---|---|---|---|---|
| 12-Week Improvement by MCID† | N‡ | 0 to 12 Weeks | 12 to 52 Weeks | 0 to 12 Weeks | 12 to 52 Weeks |
| PSEQ | |||||
| ≥ MCID | 135/254 | −2.13 (−2.46 to −1.80) | −0.84 (−1.32 to −0.35) | −4.48 (−5.29 to −3.68) | −1.98 (−2.90 to −1.06) |
| < MCID | 119/254 | −1.32 (−1.67 to −0.98) | −0.56 (−1.08 to −0.04) | −1.92 (−2.78 to −1.06) | −0.90 (−1.92 to 0.13) |
| Difference | −0.80 (−1.27 to −0.34) | −0.28 (−0.98 to 0.41) | −2.56 (−3.72 to −1.40) | −1.08 (−2.45 to 0.29) | |
| CSQ-CAT§ | |||||
| ≥ MCID | 121/283 | −2.58 (−2.94 to −2.22) | −0.79 (−1.32 to −0.27) | −5.29 (−6.14 to −4.43) | −1.39 (−2.40 to −0.38) |
| < MCID | 162/283 | −1.18 (−1.49 to −0.87) | −0.77 (−1.27 to −0.27) | −1.81 (−2.53 to −1.08) | −1.45 (−2.33 to −0.57) |
| Difference | −1.40 (−1.86 to −0.93) | −0.03 (−0.72 to 0.67) | −3.48 (−4.56 to −2.40) | 0.06 (−1.20 to 1.32) | |
| CSQ-CC§ | |||||
| ≥ MCID | 57/204 | −1.72 (−2.26 to −1.17) | −1.86 (−2.74 to −0.99) | −3.63 (−4.89 to −2.36) | −2.60 (−4.07 to −1.13) |
| < MCID | 147/204 | −1.77 (−2.04 to −1.49) | −0.48 (−0.89 to −0.08) | −3.13 (−3.81 to −2.45) | −1.11 (−1.87 to −0.34) |
| Difference | 0.05 (−0.55 to 0.65) | −1.38 (−2.34 to −0.42) | −0.50 (−1.91 to 0.92) | −1.49 (−3.10 to 0.11) | |
| FABQ-W | |||||
| ≥ MCID | 75/193 | −2.63 (−3.31 to −1.95) | 0.22 (−1.03 to 1.46) | −4.77 (−6.40 to −3.13) | −0.24 (−2.47 to 1.99) |
| < MCID | 118/193 | −1.31 (−1.75 to −0.88) | −1.18 (−2.03 to −0.32) | −2.68 (−3.74 to −1.63) | −1.86 (−3.57 to −0.15) |
| Difference | −1.32 (−2.13 to −0.51) | 1.39 (−0.12 to 2.90) | −2.08 (−3.97 to −0.19) | 1.62 (−1.19 to 4.44) | |
| FABQ-PA | |||||
| ≥ MCID | 74/254 | −2.22 (−2.74 to −1.7) | −0.70 (−1.49 to 0.09) | −4.74 (−6.05 to −3.43) | −1.53 (−2.99 to −0.07) |
| < MCID | 180/254 | −1.56 (−1.88 to −1.23) | −0.72 (−1.26 to −0.18) | −2.64 (−3.39 to −1.88) | −1.19 (−2.15 to −0.23) |
| Difference | −0.67 (−1.28 to −0.05) | 0.02 (−0.96 to 1.00) | −2.11 (−3.65 to −0.57) | −0.33 (−2.03 to 1.36) | |
Adjusted for baseline age, gender, baseline score on the numerical rating scale for back pain, and RMDQ score.
An MCID improvement was defined as 5.5 points on the PSEQ for pain-self-efficacy and 7 points on the FABQ-W scale and 4 points on the FABQ-PA scale for work- and physical activity–related fear-avoidance beliefs, respectively.
A 30% improvement in CSQ subscales was used to indicate a clinically important improvement, as an established MCID was not known.
Participants whose baseline scores showed they could not improve by the MCID or who had missing data at 12 weeks were removed, i.e., 66 participants (21%) for the PSEQ, 37 participants (12%) for the CSQ-CAT, 116 participants (36%) for the CSQ-CC, 127 (40%) for the FABQ-W, and 66 (21%) for the FABQ-PA.
Discussion
In this randomized trial of cLBP treatments, yoga and PT were not more effective than education at improving cognitive appraisal of pain, as had been originally hypothesized. All three groups experienced improved pain self-efficacy by 12 weeks that was sustained over 52 weeks of follow-up. Improvements in self-efficacy exceeded the threshold for a clinically meaningful improvement in the yoga and PT groups but not in the education group [35]. Similarly, there were significant decreases in catastrophizing at 12 weeks in the yoga and PT groups, and all three groups improved by 52 weeks. In contrast, cognitive coping and fear-avoidance beliefs were unchanged at 12 weeks. Irrespective of treatment, clinically meaningful improvements in self-efficacy, catastrophizing, and fear avoidance were associated with larger 12-week improvements in pain and function.
Few prior prospective studies have evaluated changes in cognitive appraisal of pain after yoga and PT interventions, and we are not aware of any among low-income minority populations with cLBP. Low-income minority populations are disproportionately impacted by back pain and psychological comorbidities [4, 41]. This might explain why our sample reported lower baseline self-efficacy [11, 15, 16] and higher catastrophizing [7, 42] scores than prior studies that either enrolled mostly white, moderate- to high-income participants or did not identify the race or income of participants.
Consistent with our original hypothesis and prior research [8, 15, 16, 43], we found clinically meaningful improvements [35] in pain self-efficacy among those receiving yoga and PT interventions. The magnitude of improvement in self-efficacy after our 12-week interventions were comparable to changes after 8 weeks of cognitive behavioral therapy or mindfulness-based stress reduction observed in another large randomized controlled trial of adults with cLBP [11].
Our findings suggest that yoga, PT, and pain-related education may be helpful for reducing catastrophizing. Our findings were similar to those of a prior randomized controlled trial of cLBP interventions, which found modest improvements in catastrophizing with three active interventions (PT-supervised exercise, cognitive behavioral therapy, combined exercise and cognitive behavioral therapy) but not with a waitlist control [18]. Another randomized controlled trial examining the postoperative care of adults undergoing surgery for cervical radiculopathy observed improvements in catastrophizing among the intervention and control groups (structured PT that included a behavioral approach and standard postoperative care, respectively) [42]. Recent research has called into question the construct validity of pain catastrophizing measures, including the CSQ-CAT, and suggests that they mainly assess pain-related worrying and distress [44]. These, to us, are constructs that overlap with and are related to catastrophizing. Prior research has also shown that higher pain-related worry and distress are more likely among those with low socioeconomic status [45]. When viewed together, our findings of reduced catastrophizing in an underserved population are consistent with this prior literature, and had we measured worry and distress, we would likely have seen a decrease in those constructs, as well.
We did not observe changes in fear-avoidance beliefs at 12 weeks. This finding is in contrast to a study by George et al. (2003) [46] in which participants had baseline FABQ scores similar to those of our participants, but which found that fear-avoidance–based PT, delivered similarly to our PT intervention, did lead to a significant decrease in FABQ scores at 6 months. Our study population, however, differs from the population of this prior study, as we recruited predominantly low-income participants. Additionally, in our study, 20% of participants had a score of 2 out of 42 potential points on the FABQ-W scale, indicating very little room for improvement. Prior research has shown that the FABQ has poor responsiveness, particularly when baseline levels are low, thus predisposing to a floor effect; this could have been the case in our study and might explain the difference in our results from prior research [47, 48]. Despite this, baseline FABQ-PA scores were high, with room to improve, but did not improve. This was surprising, given the reduction in catastrophizing we observed and previous research suggesting that catastrophizing precedes fear-avoidance behavior [49]. Additionally, the relationships among pain, catastrophizing, and fear might be more nuanced, and factors not measured in our study could be important, such as a history of trauma, perceived racism, and neighborhood safety [50, 51]. These factors might impact participation in group- or community-based interventions, but not necessarily home practice, and this should be considered in future research.
Although improvements in self-efficacy and catastrophizing were observed, the yoga and PT interventions were not superior to education, as had been hypothesized. Conceivably, these improvements could represent regression toward the mean rather than a treatment effect. Another possibility, described by Burns et. al. (2020), lies in a general shared mechanism model, whereby pain-related cognitive measures all change similarly in response to psychosocial treatment approaches [52]. We have observed small to modest improvements in other general psychological outcomes (e.g., perceived stress, sleep quality, symptoms of depression) in this sample, which may also support a more general shared mechanism model of cLBP treatment [8, 53–55]. Each of our interventions has overlapping components that may similarly affect cognitive appraisal and psychological health. They all provided participants with physical postures or exercises that challenged their perceived ability to move despite pain. The yoga and PT interventions included additional components (e.g., graded exercise, social support, and modeling) that could have explained the larger magnitude of effect observed in these groups than in the educational control group [56]. Yoga participants were additionally taught body and breath awareness skills that involved giving attention to physiological cues (e.g., breathing, heart rate, transient pain) without reacting negatively [57]. PT participants additionally received a tailored one-on-one treatment program with the goal of reducing pain, as well as consistent encouragement from their physical therapists.
Our finding that individuals with a clinically meaningful improvement in cognitive appraisal demonstrated a concurrent greater magnitude of change in pain and disability during the 12-week treatment phase was consistent with our initial hypothesis. This finding was consistent across all measures of cognitive appraisal, except improvements in cognitive coping, which were instead associated with improvements during the follow-up period. We previously published an analysis of responders [26] using this sample that showed that lower work-related fear-avoidance beliefs and higher pain self-efficacy at baseline were significant predictors of improvement in disability at 12 weeks independent of treatment group. When viewed together, our research suggests that when cognitive appraisal of pain is optimized (i.e., baseline high levels of self-efficacy or positive changes in self-efficacy), opportunity arises for meaningful clinical outcomes of improvements in pain and disability.
The major strength of this study is that it was a large, randomized comparison of three credible cLBP treatments in a predominantly low-income minority population with 12 months of follow-up. Prior studies have analyzed yoga and PT separately; our study adds evidence that psychological- and exercise-oriented interventions share potential mechanisms of pain improvement, such as improved self-efficacy.
This study’s primary limitation is that it is a secondary analysis of a study for which the main outcomes were pain and disability, rather than cognitive appraisal of pain. A proportion of individuals had adequate baseline cognitive appraisal skills—i.e., scores that did not allow for a clinically meaningful improvement in cognitive appraisal measures. Missing data and differential loss to follow-up in the PT group may have biased our results. We used multiple imputation analyses to address loss of data. Additionally, because measures were collected at the same time, we could not perform mediation analyses to formally assess whether changes in cognitive appraisal preceded improvements in pain and disability. Next, a limitation of our education intervention is that back pain educational materials have evolved over time to become both tailored to individual needs and augmented with technological advances, neither of which is reflected in our study [58, 59]. Finally, in some of our analyses, we identified individuals who had a clinically meaningful improvement in cognitive appraisal measures. Although these cutpoints were selected on the basis of established MCIDs when possible [35, 36], we acknowledge that these thresholds might not be widely used and should be interpreted with caution.
In conclusion, the present study provides evidence supporting the use of relatively low-cost nonpharmacological approaches (yoga, PT, and back pain education) to improve cognitive appraisal of pain. Improvements in cognitive appraisal of pain, mainly pain self-efficacy and catastrophizing, were associated with larger improvements in pain and back-related physical function.
Authors’ Contributions
Ms. Marshall, Mr. Tseng, and Drs. Gerlovin, Saper, and Roseen had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Ms. Marshall and Drs. Saper and Roseen contributed to study concept and design. Ms. Marshall, Mr. Tseng, and Drs. Joyce, Gerlovin, Yeh, Sherman, Saper, and Roseen contributed to the acquisition, analysis, or interpretation of data. Ms. Marshall and Dr. Roseen drafted the manuscript. Ms. Marshall, Mr. Tseng, and Drs. Joyce, Gerlovin, Yeh, Sherman, Saper, and Roseen contributed to critical revision of the manuscript for important intellectual content. Ms. Marshall, Mr. Tseng, and Drs. Gerlovin and Roseen contributed to statistical analysis. Ms. Marshall, Mr. Tseng, and Drs. Saper and Roseen provided administrative, technical, or material support. Drs. Saper and Roseen provided study supervision.
Supplementary Data
Supplementary Data may be found online at http://painmedicine.oxfordjournals.org.
Supplementary Material
Funding sources: The Back to Health Study (R01-AT005956) was funded by the National Center for Complementary and Integrative Health (NCCIH). Funding from NCCIH also supported the work of Drs. Yeh (K24-AT009465) and Roseen (K23-AT010487). Mr. Tseng’s work was supported with funding from the Boston University Undergraduate Research Opportunities Program.
Conflicts of interest: The authors have no financial or other relationships that would constitute a conflict of interest.
Prior presentation: This work was presented, in part, at the Integrative Medicine Network Forum at Harvard Medical School on November 6, 2020.
References
- 1. Mokdad AH, Ballestros K, Echko M, et al. ; US Burden of Disease Collaborators. The state of US Health, 1990-2016: Burden of diseases, injuries, and risk factors among US States. JAMA 2018;319(14):1444–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dieleman JL, Cao J, Chapin A, et al. US Health Care spending by payer and health condition, 1996-2016. JAMA 2020;323(9):863–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson KO, Green CR, Payne R.. Racial and ethnic disparities in pain: Causes and consequences of unequal care. J Pain 2009;10(12):1187–204. [DOI] [PubMed] [Google Scholar]
- 4. Tait RC, Chibnall JT, Andresen EM, Hadler NM.. Management of occupational back injuries: Differences among African Americans and Caucasians. Pain 2004;112(3):389–96. [DOI] [PubMed] [Google Scholar]
- 5. Lee H, Hubscher M, Moseley GL, et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain 2015;156(6):988–97. [DOI] [PubMed] [Google Scholar]
- 6. Pincus T, Burton AK, Vogel S, Field AP.. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976) 2002;27(5):E109–20. [DOI] [PubMed] [Google Scholar]
- 7. Hall AM, Kamper SJ, Emsley R, Maher CG.. Does pain-catastrophising mediate the effect of tai chi on treatment outcomes for people with low back pain? Complement Ther Med 2016;25:61–6. [DOI] [PubMed] [Google Scholar]
- 8. Sherman KJ, Wellman RD, Cook AJ, Cherkin DC, Ceballos RM.. Mediators of yoga and stretching for chronic low back pain. Evid Based Complement Alternat Med 2013;2013:130818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wertli MM, Rasmussen-Barr E, Weiser S, Bachmann LM, Brunner F.. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: A systematic review. Spine J 2014;14(5):816–36.e4. [DOI] [PubMed] [Google Scholar]
- 10. Karasawa Y, Yamada K, Iseki M, et al. Association between change in self-efficacy and reduction in disability among patients with chronic pain. PLoS One 2019;14(4):e0215404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Turner JA, Anderson ML, Balderson BH, et al. Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: Similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain 2016;157(11):2434–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nicholas MK, Asghari A, Blyth FM, et al. Self-management intervention for chronic pain in older adults: A randomised controlled trial. Pain 2013;154(6):824–35. [DOI] [PubMed] [Google Scholar]
- 13. Hayden JA, Wilson MN, Stewart S, et al. Exercise treatment effect modifiers in persistent low back pain: An individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med 2020;54(21):1277–8. [DOI] [PubMed] [Google Scholar]
- 14. Anheyer D, Haller H, Lauche R, Dobos G, Cramer H.. Yoga for treating low back pain: A systematic review and meta-analysis. Pain 2021; doi: 10.1097/j.pain.0000000000002416. [DOI] [PubMed] [Google Scholar]
- 15. Cox H, Tilbrook H, Aplin J, et al. A randomised controlled trial of yoga for the treatment of chronic low back pain: Results of a pilot study. Complement Ther Clin Pract 2010;16(4):187–93. [DOI] [PubMed] [Google Scholar]
- 16. Tilbrook HE, Cox H, Hewitt CE, et al. Yoga for chronic low back pain: A randomized trial. Ann Intern Med 2011;155(9):569–78. [DOI] [PubMed] [Google Scholar]
- 17. Woby SR, Watson PJ, Roach NK, Urmston M.. Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of control, predictive of changes in chronic low back pain and disability? Eur J Pain 2004;8(3):201–10. [DOI] [PubMed] [Google Scholar]
- 18. Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA.. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain 2006;7(4):261–71. [DOI] [PubMed] [Google Scholar]
- 19. Fritz JM, Magel JS, McFadden M, et al. Early physical therapy vs usual care in patients with recent-onset low back pain: A randomized clinical trial. JAMA 2015;314(14):1459–67. [DOI] [PubMed] [Google Scholar]
- 20. Leonhardt C, Kuss K, Becker A, et al. Graded exposure for chronic low back pain in older adults: A pilot study. J Geriatr Phys Ther 2017;40(1):51–9. [DOI] [PubMed] [Google Scholar]
- 21. Martinez-Calderon J, Flores-Cortes M, Morales-Asencio JM, Luque-Suarez A.. Conservative interventions reduce fear in individuals with chronic low back pain: A systematic review. Arch Phys Med Rehabil 2020;101(2):329–58. [DOI] [PubMed] [Google Scholar]
- 22. Martinez-Calderon J, Flores-Cortes M, Morales-Asencio JM, Fernandez-Sanchez M, Luque-Suarez A.. Which Interventions enhance pain self-efficacy in people with chronic musculoskeletal pain? A systematic review with meta-analysis of randomized controlled trials, including over 12 000 participants. J Orthop Sports Phys Ther 2020;50(8):418–30. [DOI] [PubMed] [Google Scholar]
- 23. Riley SP, Bialosky J, Coronado RA.. Are changes in fear-avoidance beliefs and self-efficacy mediators of discharge function and pain in patients with acute and chronic low back pain? J Orthop Sports Phys Ther 2020;50(6):301–29. [DOI] [PubMed] [Google Scholar]
- 24. Saper RB, Sherman KJ, Delitto A, et al. Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: Study protocol for a randomized controlled trial. Trials 2014;15:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Saper RB, Lemaster C, Delitto A, et al. Yoga, physical therapy, or education for chronic low back pain: A randomized noninferiority trial. Ann Intern Med 2017;167(2):85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Roseen EJ, Gerlovin H, Felson DT, et al. Which chronic low back pain patients respond favorably to yoga, physical therapy, and a self-care book? Responder analyses from a randomized controlled trial. Pain Med 2021;22(1):165–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moore JL, Von Korff M, Gonzalez VM, Laurent DD.. The Back Pain Helpbook. New York: Perseus Books; 1999. [Google Scholar]
- 28. Nicholas MK. The pain self-efficacy questionnaire: Taking pain into account. Eur J Pain 2007;11(2):153–63. [DOI] [PubMed] [Google Scholar]
- 29. Harland NJ, Georgieff K.. Development of the Coping Strategies Questionnaire 24, a clinically utilitarian version of the Coping Strategies Questionnaire. Rehabil Psychol 2003;48(4):296–300. [Google Scholar]
- 30. Harland N, Ryan CG.. The value of pain coping constructs in subcategorising back pain patients according to risk of poor outcome. Biomed Res Int 2013;2013:898573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Waddell G, Newton M, Henderson I, Somerville D, Main CJ.. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 1993;52(2):157–68. [DOI] [PubMed] [Google Scholar]
- 32. Korff Jensen VM, Karoly MP.. Assessing global pain severity by self-report in clinical and health services research. Spine (Phila Pa 1976) 2000;25(24):3140–51. [DOI] [PubMed] [Google Scholar]
- 33. Patrick DL, Deyo RA, Atlas SJ, et al. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976) 1995;20(17):1899–908; discussion 909. [DOI] [PubMed] [Google Scholar]
- 34. Kent P, Grotle M, Dunn KM, Albert HB, Lauridsen HH.. Rasch analysis of the 23-item version of the Roland Morris Disability Questionnaire. J Rehabil Med 2015;47(4):356–64. [DOI] [PubMed] [Google Scholar]
- 35. Chiarotto A, Vanti C, Cedraschi C, et al. Responsiveness and minimal important change of the pain self-efficacy questionnaire and short forms in patients with chronic low back pain. J Pain 2016;17(6):707–18. [DOI] [PubMed] [Google Scholar]
- 36. Monticone M, Frigau L, Vernon H, et al. Reliability, responsiveness and minimal clinically important difference of the two Fear Avoidance and Beliefs Questionnaire scales in Italian subjects with chronic low back pain undergoing multidisciplinary rehabilitation. Eur J Phys Rehabil Med 2020;56(5):600–6. [DOI] [PubMed] [Google Scholar]
- 37. Kovacs FM, Abraira V, Moix J, et al. Fear avoidance beliefs and low back pain: “Practical reviews” from expert panel discussions versus comprehensive systematic reviews. Spine J 2012;12(2):174–5; author reply 5. [DOI] [PubMed] [Google Scholar]
- 38. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic; 1988. [Google Scholar]
- 39. van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res 2007;16(3):219–42. [DOI] [PubMed] [Google Scholar]
- 40. Rubin DB. Inference and missing data. Biometrika 1976;63(3):581–92. [Google Scholar]
- 41. Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Med 2003;4(3):277–94. [DOI] [PubMed] [Google Scholar]
- 42. Wibault J, Oberg B, Dedering A, et al. Neck-related physical function, self-efficacy, and coping strategies in patients with cervical radiculopathy: A randomized clinical trial of postoperative physiotherapy. J Manipulative Physiol Ther 2017;40(5):330–9. [DOI] [PubMed] [Google Scholar]
- 43. Frost H, Moffett JAK, Moser JS, Fairbank JCT.. Randomised controlled trial for evaluation of fitness programme for patients with chronic low back pain. BMJ 1995;310(6973):151–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Crombez G, De Paepe AL, Veirman E, et al. Let's talk about pain catastrophizing measures: An item content analysis. PeerJ 2020;8:e8643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dany L, Roussel P, Laguette V, Lagouanelle-Simeoni MC, Apostolidis T.. Time perspective, socioeconomic status, and psychological distress in chronic pain patients. Psychol Health Med 2016;21(3):295–308. [DOI] [PubMed] [Google Scholar]
- 46. George SZ, , FritzJM, , BialoskyJE, , Donald DA.. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine 2003;28(23):2551–60. [DOI] [PubMed] [Google Scholar]
- 47. Grotle M, Brox JI, Vollestad NK.. Reliability, validity and responsiveness of the fear-avoidance beliefs questionnaire: Methodological aspects of the Norwegian version. J Rehabil Med 2006;38(6):346–53. [DOI] [PubMed] [Google Scholar]
- 48. Chaory K, Fayad F, Rannou F, et al. Validation of the French version of the Fear Avoidance Belief Questionnaire. Spine (Phila Pa 1976) 2004;29(8):908–13. [DOI] [PubMed] [Google Scholar]
- 49. Vlaeyen JW, Linton SJ.. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000;85(3):317–32. [DOI] [PubMed] [Google Scholar]
- 50. Wideman TH, Asmundson GG, Smeets RJ, et al. Rethinking the fear avoidance model: Toward a multidimensional framework of pain-related disability. Pain 2013;154(11):2262–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Meints SM, Edwards RR.. Evaluating psychosocial contributions to chronic pain outcomes. Prog Neuropsychopharmacol Biol Psychiatry 2018;87(Pt B):168–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Burns JW, Van Dyke BP, Newman AK, Morais CA, Thorn BE.. Cognitive behavioral therapy (CBT) and pain education for people with chronic pain: Tests of treatment mechanisms. J Consult Clin Psychol 2020;88(11):1008–18. [DOI] [PubMed] [Google Scholar]
- 53. Berlowitz J, Hall DL, Joyce C, et al. Changes in perceived stress after yoga, physical therapy, and education interventions for chronic low back pain: A secondary analysis of a randomized controlled trial. Pain Med 2020;21(10):2529–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Joyce C, Roseen EJ, Keysor JJ, et al. Can yoga or physical therapy for chronic low back pain improve depression and anxiety among adults from a racially diverse, low-income community? A secondary analysis of a randomized controlled trial. Arch Phys Med Rehabil 2021;102(6):1049–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Roseen EJ, Gerlovin H, Femia A, et al. Yoga, physical therapy, and back pain education for sleep quality in low-income racially diverse adults with chronic low back pain: A secondary analysis of a randomized controlled trial. J Gen Intern Med 2020;35(1):167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 57. Keosaian JE, Lemaster CM, Dresner D, et al. “We're all in this together”: A qualitative study of predominantly low income minority participants in a yoga trial for chronic low back pain. Complement Ther Med 2016;24:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sandal LF, Bach K, Overas CK, et al. Effectiveness of app-delivered, tailored self-management support for adults with lower back pain-related disability: A selfBACK randomized clinical trial. JAMA Intern Med 2021;181(10):1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Traeger AC, Lee H, Hubscher M, et al. Effect of intensive patient education vs placebo patient education on outcomes in patients with acute low back pain: A randomized clinical trial. JAMA Neurol 2019;76(2):161–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.