Abstract
Physical activity is beneficial for physical and mental health in the general population. Among autistic people, a range of physical and mental health conditions, particularly depression and anxiety, occur more frequently than in the general population. Physical activity interventions could help improve physical and mental health in autistic adults, but there is a lack of research in the area. The aim of this perspective article is to explore research into physical activity interventions for autistic adults, and identify gaps particularly in need of addressing. This perspective article considers six intervention studies carried out with adults, a pilot study, and seven review studies of adult and child interventions. Studies found significant increases in amount of physical activity undertaken, well-being, interaction, emotion, and regulation. There were decreases in imitative and distress behaviors. However, there were few studies, samples were small, participants all had co-occurring intellectual disability (ID), and measures were heterogeneous with lack of assessment of changes in physical fitness levels. Qualitative exploration was extremely limited. Recommendations are that there should be increased focus on research into physical activity for autistic adults, with input from autistic people to identify enjoyable, accessible activities. There should be particular consideration of longer term, sustainable activities for autistic people both with and without ID. Finally, but of major importance, there should be an increased focus on addressing mental health and anxiety through physical activity.
Keywords: exercise, well-being, running, walking, health
Lay summary
Why is this topic important?
Physical activity is effective at reducing the risk of and managing long-term physical and mental health conditions in the general population. Autistic people's health is poorer on average than the general population, so exercise might be particularly helpful for them, but little is known in this area.
What is the purpose of this article?
The article looks at the existing research on physical activity for autistic people and identifies where research is needed to understand better how physical activity could benefit autistic people's health and well-being.
What is the perspective of the author?
The author is a late-diagnosed autistic woman who worked as a fitness instructor before she completed her studies in psychology. She was awarded a PhD in psychology in 2015, looking at music in exercise, and works as a university researcher and tutor.
What does existing research show?
Research so far has consisted of small studies, and the designs have often been poor. There is a tendency to overlook the well-being of autistic people and to focus on stopping certain behaviors without recognizing why they are happening, or that they may be helpful for autistic people. Studies found that physical activity has many benefits for autistic people, such as increasing well-being, helping with emotional regulation, improving walking gait and balance, and raising activity levels. However, most studies did not look at health and fitness outcomes and were more focused on outcomes that have not been identified as important to autistic people.
What is recommended for future research?
Research needs to focus much more on autistic adults, across a wide age range, as needs and physical characteristics change across the life span. Autistic people need to be involved with the design of the programs that the research is testing, to make sure they are acceptable and appropriate for their needs. At the moment, research has looked at mainly short programs and researchers have not measured fitness. Unless fitness is measured at the outset and end of physical activity programs, we will not know if they are effective at improving fitness. Fitness improvements are lost if physical activity is not continued, so programs need to be continued after the end of a research study if they are effective.
Research on physical activity for autistic adults has only looked at adults who also have intellectual disabilities. Research needs to consider adults without intellectual disabilities, and also consider adults who have other common conditions that are often found alongside autism, for example, epilepsy, and Ehlers–Danlos syndrome. Perhaps most importantly, researchers need to recognize neurodiversity and understand it better, so that they can avoid trying to suppress activities such as stimming, which many autistic people find helpful in managing everyday stresses. Instead, researchers need to avoid treating autism as a disorder that needs to be fixed and focus on the needs and wishes of autistic people.
How will these findings help autistic adults now or in the future?
This article gives clear guidance on a way forward for research. The author hopes that this will lead to good-quality studies focusing on autistic people's priorities, and that the evidence these studies generate will lead to better provision of physical activity facilities and opportunities for autistic people, improving their health and well-being.
Introduction
Background
Physical activity (defined as “bodily movement produced by skeletal muscles that results in energy expenditure”1 p.126) offers health benefits, while inactivity is associated with increased mortality.2 Physical activity and exercise (a subcategory of physical activity, structured to increase or preserve fitness1) decrease the risk of chronic physical conditions3 and assist with their management, including improving symptoms of coronary heart disease and type 2 diabetes,4 lowering risk of depressive illness,5 and having a therapeutic effect on mild to moderate depression,6 although adherence may be difficult for those with depression.6 There is also evidence of improvement in anxiety, insomnia, and stress-related symptoms.7,8
To date, there has been little research into the benefits of physical activity for autistic people, particularly adults. Autistic adults have increased risks of conditions, including depression, anxiety, sleep disorders, obesity, hypertension, stroke, and diabetes,9 suggesting physical activity could be particularly beneficial for this group. Motor co-ordination difficulties are common among autistic people.10 Motor skills improve with exercise in the general population,11 with a single session having a “priming” effect for learning motor skills.12 Improved motor co-ordination can reduce injuries—for example, from falls—again indicating that physical activity may help improve autistic people's health. However, reviews of the literature13–19 show that studies of physical activity and exercise for autistic people focus on children and often have small sample sizes. The use of small samples, and the lack of control groups in many studies, results in a fairly weak body of evidence from which to draw conclusions. Due to heterogeneity of designs and measures, it is rarely feasible to compare studies or collate many outcomes in a meta-analysis. In addition, changes in diagnostic criteria, particularly over the last 30 years, mean that descriptions of participants may be inconsistent; for example, the widely used Diagnostic and Statistical Manual of Mental Disorders (DSM) presents autism and Asperger's syndrome as different diagnoses in its fourth edition,20 while the fifth edition10 subsumes both into a diagnosis of autistic spectrum disorder.
Beyond design weaknesses, there is apparent uncertainty in the field regarding the conceptualization of what a “desirable” outcome is. Throughout both older and newer literatures, autistic traits are most often presented as deficits without considering that autism also confers some advantages.21,22 Sowa and Meulenbroek describe “maladaptive behavioural patterns such as rigidity and stereotypical movements,” to be “suppress[ed] or eliminate[d]” (p.47)13 but fail to acknowledge sensory issues23 that may contribute. “Self-stimulation” or stimming (the preferred term of the autistic community) is an example. It includes verbalizations and actions such as rocking and hand-flapping, which provide a coping mechanism to help regulate overwhelming environments and alleviate the distress they cause, and provides a release for both positive and negative emotion.24 Studies frequently report reductions in stimming while overlooking its purpose, although Lang et al.14 suggest exercise may have a similar effect to stimming, and that autistic people may prefer activities that match preferred stims. Exercise helps reduce cortisol produced in response to stress,25,26 which may also be decreasing stimming. However, the language used in some studies conceptualizes stimming as disruptive, needing to be curtailed to enable learning,27 rather than something that might—along with physical activity—assist learning by helping manage emotions.
The present article was inspired by anecdotal evidence that many autistic people enjoy exercise and find it beneficial for their well-being. Although I conducted a systematic review following PRISMA guidelines, the gaps in the literature were so large that it was more appropriate to present the findings in a perspective piece with recommendations for future research.
Terminology
Physical activity and exercise definitions here are based on a study by Caspersen et al.1 Physical activity interventions tend to be structured and may include exercise; however, the widespread absence of physical fitness measures in studies of autism and exercise suggests no intention to increase/preserve fitness, and thus is inconsistent with the definition. The term “physical activity” is used in preference to the term “exercise” in this perspective article, unless research specifically refers to exercise. Identity-first (“autistic person”) rather than person-first (“person with autism”) terminology is used as this is the preference of the majority of autistic people.28 Studies discussed in this article were sometimes inconsistent with present guidelines on respectful language and conceptualization, and these discrepancies are noted.
Positionality
The author is an autistic postdoctoral researcher specializing in psychology, exercise, and music. She is a fully qualified exercise-to-music instructor, gym instructor, and personal trainer, and worked in the fitness industry for 5 years, during which time she completed her undergraduate psychology degree. She left the industry to focus on full-time postgraduate study in 2011, and received a formal diagnosis of autism in 2017. This information is presented so that readers will recognize that the recommendations herein arise through a combination of interest in effective and enjoyable physical activity, psychology research principles, and an autistic viewpoint.
Studies of Physical Activity for Autistic Adults
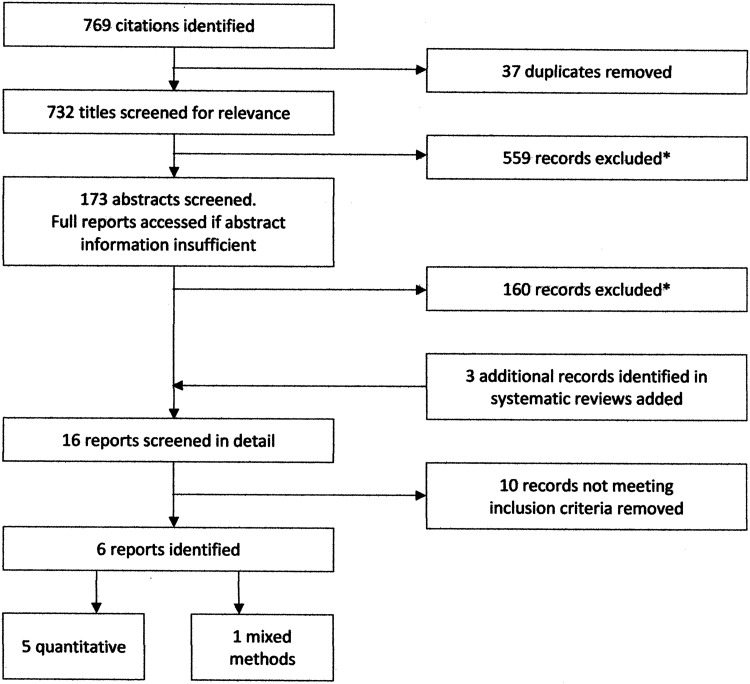
Research into physical activity for autistic adults (defined here as participants of age 18 and older) has received little coverage in review studies. As research literature in autism is growing rapidly, it was not clear whether existing reviews reflected an overall absence of studies of adults or whether there were studies too recently published for inclusion. A systematic review (see Appendix A for full strategy and Figure 1 for search process) found six individual studies29–34 of physical activity for autistic adults, summarized in Table 1. The present search looked for studies that included group comparisons in the case of quantitative research. Of note, I specifically sought out qualitative descriptive studies (using, e.g., interviews or focus groups to gather data), but only found small-scale investigations nested within quantitative studies.
FIG. 1. .
The search process stages. *Reasons for exclusion: no diagnosis (including self-diagnosis) of an autistic spectrum condition; no group comparison; participants younger than 18 years; general advisory articles; intervention not physical activity/exercise related; book reviews; research on nonhumans; conference abstracts without subsequent peer-reviewed publication to date; case study.
Table 1.
Summary of Studies Identified Through Systematic Review
| Authors | Year of publication | Participants | Focus | Findings |
|---|---|---|---|---|
| Elliott et al.29 | 1994 | 6 (within-participant design) | Effects of exercise on behavior | Improvement in “maladaptive and stereotypic behaviors” after vigorous exercise. No significant findings for motor training. |
| García-Villamisar and Dattilo31 | 2010 | 71 Intervention group: 37 Wait-list control: 34 |
Effects of leisure program on quality of life and stress | Statistically significant improvements in stress, quality of life, empowerment-independence and social belonging-community integration. |
| García-Villamisar et al.30 | 2017 | 46 Intervention group: 26 Wait-list control: 18 |
Effects of walking intervention on balance, gait, stress, and well-being | Statistically significant improvements in gait, balance, and personal well-being (not significant for stress). |
| LaLonde et al.34 | 2014 | 5 | Increasing physical activity using goal setting and rewards | Increased with intervention, decreased when intervention was removed, increased again with return to intervention. |
| Mateos-Moreno and Atencia-Doña32 | 2013 | 16 Intervention group: 8 Control: 8 |
Effects of dance/movement and music therapy on behavior | Improvements in interaction, imitation, emotion, instinct, and regulation. No significant findings for attention, perception, association, intention, muscle tone, motility, contact, or communication regulation. |
| Savage et al.33 | 2018 | 3 | Comparison of in-person and technology-delivered praise to increase physical activity | Interventions increased the number of laps. Technology users were able to maintain the increase when the intervention was reduced. |
Across studies, findings were broad; “stereotypical” and “aggressive” behaviors were reduced, interventions to increase activity were successful at least in part, and quality of life for autistic adults improved. Results were largely consistent with previous, child-focused reviews, although some of the measures differed. However, half the studies had very small samples and there were issues with study design.
Researchers varied in how they conceptualized the autistic traits and physical activity effects, affecting outcome measures and conclusions drawn. Elliott et al.29 presented “stereotypic behaviors” (stimming) as a barrier to learning (p.566), and noted that their intervention had helped participants enter into employment, but did not consider underpinning mechanisms. García-Villamisar and Dattilo,31 on the contrary, recognized distress behaviors and focused on stress and quality of life in their 2010 study. This work preceded Autistica's collation of autistic people's research priorities,35 but was consistent with it, emphasizing the importance of quality of life, which is lower among autistic people than in the general population.36
Participant feedback on acceptability of interventions was mentioned in two studies.33,34 LaLonde et al.34 noted that participants and teachers liked goal-setting for number of steps achieved by walking, with rewards, while Savage et al.33 described one of their participants engaging particularly enthusiastically with their praise-for-running intervention. However, the same study included a participant who declined to take part on several successive days; the reasons are unclear, but the implication is that the activity was not universally enjoyed, and it would be expected that, as in the wider population, autistic preferences for different physical activities will vary.
Effectiveness of any physical activity program will be compromised if a participant dislikes it and consequently engages less with it. García-Villamisar et al. factored in participant enjoyment with their B-Active2 program30 incorporating physical activity guidance in conjunction with enjoyment and activity choice.31 This consideration for what autistic people might like to do was not generally evident in the studies. A wider understanding of different activity preferences and potential barriers to exercise for this population is needed.
There were some notable weaknesses in the methodologies used. Three of the six studies had fewer than 10 participants, meaning statistical power was insufficient for meaningful group comparisons. Elliott et al.29 aimed to include participants who would particularly enjoy physical activity, which may have biased their results.29 Mateos-Moreno and Atencia-Doña32 measured 15 variables (with some overlap) for a sample of only 16 participants, a ratio likely to lead to type 1 (false positive) errors.37 Only half the studies—Elliott et al.29 and the two García-Villamisar studies30,31—reported randomized allocation to conditions, but did not provide details. Elliott et al.'s reporting29 focused on the best outcomes and appeared somewhat selective.
The varied outcome measures make comparison difficult. Elliott et al.29 and Mateos-Moreno and Atencia-Doña32 emphasized behavior change, while Savage et al.33 and LaLonde et al.34 focused on increasing physical activity. Both studies from García-Villamisar et al.30,31 were concerned with improving quality of life and reducing stress; the more recent study30 also measured gait and balance with a view to reducing risk of falls.
Interventions included running/jogging and walking but varied in delivery and intended purpose. Cardiovascular activity dominated, with some consideration of motor co-ordination, but strength and flexibility were largely overlooked. Progression focused on increasing duration rather than intensity, and, unusually for physical activity studies, fitness measurements were noticeably absent. The only measures evident were gait and balance in García-Villamisar et al.,30 and muscle tone in Mateos-Moreno and Atencia-Doña32 although the latter was part of a clinical scale for evaluating autistic behavior, which used subjective and somewhat offensive criteria such as “bizarre posture”; this may be a translation issue, as the study is Spanish and the scale was published in English by French researchers,38 but nevertheless raises questions regarding appropriate language.
Five of the studies specifically stated that participants had an intellectual disability (ID), while in the sixth study, by LaLonde et al.,34 it was implicit in the limited scope of feedback sought from participants, using simple questions with yes/no answers, compared with much greater detail requested from their teacher. This contrasts with Matson and Shoemaker's39 findings that autism research prioritizes those without ID; in physical activity studies, the opposite appears to be the case. This risks overlooking limitations and barriers to physical activity experienced by those living more independently. Language frequently presented all autistic traits as problematic. In Elliott et al.29 and Mateos-Moreno and Atencia-Doña32 measures focused on behaviors such as stimming, constructed as negative traits by the authors. Stimming is often harmless and may help an autistic person regulate emotion and the effects of the environment.23 Elliott et al.,29 for example, suggest that self-stimulation is “interfering with learning the skills needed to succeed” (p.566) rather than acknowledging it may be helpful when skills are taught in an overstimulating environment. This construction of certain autistic traits as undesirable overlooks their function and underpinning mechanisms, and thus fails to prioritize the well-being of autistic individuals.
Recommendations
The studies covered in the previous sections reveal a number of areas on which future research should focus. There is a particular need for a breadth of expertise, and an interdisciplinary approach; expertise in autism and expertise in physical activity are both needed to develop effective programs, which take into account autistic people's needs but are also effective at delivering health and well-being benefits over the longer term. The focus on reducing “problem” traits without recognizing the broader context overlooks the interests of autistic people, as noted by Livingston and Happé:
“The majority of studies into adult outcomes thus far rely heavily on definitions of outcome imposed by neurotypicals to neurotypical standards, and may not necessarily reflect the best outcomes as perceived by autistic individuals themselves” (p.733).40
A recent pilot study41 was published after the review was carried out, and does not meet inclusion criteria due to lack of a control group, but is worthy of note. It features an intervention where adult autistic college students were mentored by nonautistic kinesiology students to develop physical activity programs suited to their preferences in terms of content, dedicated space, and opportunities to interact. This mixed-methods study demonstrates quantitative fitness improvements alongside qualitative evidence of enhanced well-being, and enjoyment of fitness and social aspects of the program. The authors plan a randomized controlled trial, which may provide further evidence in addition to going some way to address the recommendations below.
Based on the results of this systematic review, my recommendations are as follows:
Suitable environments and activities for adults need to be identified, explored, and developed. The vast majority of research studies look at children, and research needs to cover the full life span. In studies of children, participants will have limited autonomy regarding exercise, and activities are likely to arise through school or parental provision. Studies of adults show a similar pattern of structured interventions, provided through day care centers or colleges. This excludes autistic adults with higher levels of independence for whom general community physical activity resources may be challenging to access. In addition, adults have different motor skills and physiques than children, and there are limitations to the generalizability of study results because of this.
Programs need to be developed with likely participant profiles in mind. There was a dearth of input from autistic people and their allies regarding what physical activity they participate in and enjoy, or activities they find inaccessible and the reasons for that. A first step in designing effective interventions is to understand better what enjoyable and practical physical activity looks like for autistic people. Qualitative research would be particularly helpful to identify barriers to physical activity, and also what options are accessible and enjoyable. For intervention studies, it is vital that autistic people are involved at the design stage to help identify appropriate activities. Low fitness levels and obesity may also limit activities; these were issues in Todd et al.'s recent pilot.41 Obesity in particular can cause joint pain and mobility limitations, for example, moving from different exercise positions such as exercises lying on the floor to standing exercises.
There needs to be a move away from trying to “fix” autism, in favor of acceptance and a focus on what is best for autistic people, through increased recognition of the neurodiversity paradigm. This means involving autistic people in developing programs and recognizing what benefits they seek. A shift is needed away from trying to suppress activities such as stimming simply because they are deemed socially unacceptable, and there needs to be a move toward understanding their purpose and identifying what is genuinely helpful for autistic people to achieve good quality of life.
Different aspects of fitness such as strength, cardiovascular function, flexibility, and co-ordination should all be addressed to maximize health benefits, and outcomes relating to fitness, physical health, and mental health should be measured. The interventions featured were short term, and there was little understanding of progression. By addressing this, effective programs can be identified and strong evidence presented to support their wider implementation.
It is important to evaluate longer term programs, and for those participants who adhere to the program, it is important to add variety and increase challenge to ensure progression. Health benefits are quickly lost when regular physical activity stops, and progression soon plateaus if new challenges are not introduced. This may not always be welcome in a population that prefers consistency and routine; again, autistic people should be involved with the design of progressive programs.
Projects need to involve multiple agencies to develop impact and sustainability in the longer term. In addition to a focus on short-term programs in studies, there was little evidence of longer term sustainability or impact. It is important that interventions can be implemented widely if they are effective, and that provision is accessible. Fitness gains are rapidly lost if an individual is not regularly active, so maintaining fitness needs to be considered if full physical and mental health benefits of physical activity are to be enjoyed. Researchers may find that community providers (e.g., local authorities and leisure trusts in the United Kingdom) are able to collaborate in building an evidence base and, furthermore, have an interest and remit to engage hard-to-reach populations and sustain programs.
When developing a research study, careful consideration needs to be given regarding the target population. With the exception of Todd et al.'s recent pilot study,41 all adults in the studies discussed had co-occurring ID. While ID is common in the autism population, the majority of autistic people do not have ID. Many live unsupported in the community and may struggle with a variety of barriers to being physically active, including cost, unpredictability, and sensory issues. Individuals with co-occurring ID certainly need to be included in research studies, but so too do other commonly co-occurring conditions, particularly those such as epilepsy and Ehlers–Danlos syndrome, which may limit certain physical activity and exercise activities.42,43 Again, involvement of autistic people with co-occurring conditions in the design of programs is vital so that their varied needs can be taken into account.
Research into physical activity programs should incorporate mental well-being measures, and consider physical activity broadly as well as specific components (e.g., solitary versus group activities, indoor versus outdoor, varying intensity and duration). Mental health is a major issue for the autistic population. While physical activity and exercise have limited capacity to manage severe depression, it is widely recognized as effective for mild to moderate depression in the general population,5–7 and this may also be the case for autistic people. This is a particularly important area, therefore, for better understanding of what is helpful, but mental well-being was largely overlooked in the literature covered here.
Researchers should consider exploring activities such as exercise-to-music classes (e.g., spinning or aerobics), circuit training, and weight lifting, which have had little coverage in research but lend themselves well to progressive programs as challenge can be increased gradually. The existing research draws connections between physical activity and stimming, suggesting that physical activity may have the same effect as stimming, and that activities similar to preferred stims may be particularly helpful for autistic people's well-being.14 Stimming takes a wide variety of forms, and includes vocalization as well as movement.24 At present, there is little research into stimming beyond Kapp et al.'s recent qualitative study,24 but there is scope to investigate whether physical activity and stimming have similar effects, and whether physical activity may provide a useful emotional release. Existing research covers a small range of physical activity programs, and it is likely that—as with the wider population—autistic people have diverse individual preferences.
Conclusion
Research into physical activity and exercise interventions for autistic adults consists of a few, small studies that, in general, do not focus on autistic people's priorities. There is a need for larger, well-designed intervention studies, with autistic people involved early in the planning stages. Before this can happen, understanding of the population's preferences, motivations, and barriers to activity is needed to inform intervention design and ensure accessibility and enjoyment. The breadth of the population and very varied situations of autistic adults need to be recognized. Overall, there is considerable scope for research into physical activity for autistic adults to help improve mental and physical health outcomes and increase quality of life.
Authorship Confirmation Statement
Rachel Hallett researched the field and wrote the manuscript. The manuscript has been submitted solely to this journal and is not published, in press or submitted elsewhere.
Appendix A
Systematic Review Search Strategy
Spring 2018
Search keywords and word stems:
Autis*
Asperger*
Exercise
Physical Activity
Sport
Fitness
Studies with following keywords and word stems to be excluded in searches:
Child*
Adolesc*
A total of 27 databases were searched
Academic Search Complete
AMED
ASSIA
Biomed Central
BMJ Open
British Nursing Index
CINAHL
Clinical Evidence
Cochrane Library
DOAJ
Emerald Premier
EThOS
IngentaConnect
JSTOR
MEDLINE
NHS Evidence
Periodicals Archive Online
PsycARTICLES
PsycINFO
PubMed
Science Citation Index Expanded
ScienceDirect
Scopus
Social Sciences Citation Index
SPORTDiscus
TRIP
Web of Science
Inclusion Criteria
Some of the language in the inclusion criteria is pathologizing and disorder-focused; this is consistent with the terminology used in many relevant article and so was applied to identify qualifying articles. Criteria included all outcome measures, all languages, and all dates of publication.
Quantitative reports
Random allocation or comparison group designs, including within-participant designs.
Inclusion of pre- and postintervention data.
Qualitative reports
Methods of data collection and analysis reported.
Study reports people's experiences, views, preferences, and beliefs regarding physical activity and exercise.
Includes data from autistic individuals and/or associates of autistic individuals such as family and carers, with clear information regarding the proportion of autistic participants.
Presents views as data, for example, as quotations or descriptions of what participants said, rather than providing the results of analyzing the data (e.g., themes) without support from the data.
Participants
Self-diagnosis/identification as autistic, Aspergian, or having pervasive developmental disorder (PDD).
Criteria for autism spectrum condition or disorder, Asperger's syndrome, and PDD with or without co-occurring conditions.
Ages 18 or older; studies with mixed age groups met criteria if the majority of participants were older than 18 years, or the mean age stated was more than 18.
Interventions
Exercise or physical activity programs with or without other elements (such as education or healthy eating).
Land or water based.
Community, hospital, facility, or home based.
Any physical activity considered, for example, walking, resistance training, and dance.
No stipulations regarding delivery length, frequency, and intensity.
Group or individual programs.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No specific funding was provided for this perspective article or the systematic review underpinning it. It was carried out within the author's paid role as a researcher.
References
- 1. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organisation. Global Recommendations on Physical Activity for Health. Geneva; 2010. http://apps.who.int/iris/bitstream/handle/10665/44399/9789241599979_eng.pdf;jsessionid=45DDEAFDDD3A9CA543A43F987BE6DB6B?sequence=1 (accessed July 22, 2019). [Google Scholar]
- 3. Chakravarthy MV, Joyner MJ, Booth FW. An obligation for primary care physicians to prescribe physical activity to sedentary patients to reduce the risk of chronic health conditions. Mayo Clin Proc. 2002;77(2):165–173. [DOI] [PubMed] [Google Scholar]
- 4. Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity—a systematic review of longitudinal studies. BMC Public Health. 2013;13(813):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stanton R, Happell B, Reaburn P. The mental health benefits of regular physical activity, and its role in preventing future depressive illness. Nurs Res Rev. 2014;4:45–53. [Google Scholar]
- 6. Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: Meta-analysis and systematic review. Scand J Med Sci Sport. 2014;24:259–272. [DOI] [PubMed] [Google Scholar]
- 7. Stubbs B, Vancampfort D, Rosenbaum S, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: A meta-analysis. Psychiatry Res. 2017;249:102–108. [DOI] [PubMed] [Google Scholar]
- 8. Passos GS, Poyares D, Santana MG, et al. Effects of moderate aerobic exercise training on chronic primary insomnia. Sleep Med. 2011;12(10):1018–1027. [DOI] [PubMed] [Google Scholar]
- 9. Croen LA, Zerbo O, Qian Y, et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814–823. [DOI] [PubMed] [Google Scholar]
- 10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders V (DSM-V). Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 11. Roig M, Skriver K, Lundbye-jensen J, Kiens B, Nielsen JB. A single bout of exercise improves motor memory. PLoS One. 2012;7(9):e44594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Statton MA, Encarnacion M, Celnik P, Bastian AJ. A single bout of moderate aerobic exercise improves motor skill acquisition. PLoS One. 2015;10:e0141393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sowa M, Meulenbroek R. Effects of physical exercise on autism spectrum disorders: A meta-analysis. Res Autism Spectr Disord. 2012;6(1):46–57. [Google Scholar]
- 14. Lang R, Koegel LK, Ashbaugh K, Regester A, Ence W, Smith W. Research in autism spectrum disorders physical exercise and individuals with autism spectrum disorders: A systematic review. Res Autism Spectr Disord. 2010;4(4):565–576. [Google Scholar]
- 15. Jones RA, Downing K, Rinehart NJ, et al. Physical activity, sedentary behavior and their correlates in children with autism spectrum disorder: A systematic review. PLoS One. 2017;12(2):e0172482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Healy S, Nacario A, Braithwaite RE, Hopper C. The effect of physical activity interventions on youth with autism spectrum disorder: A meta-analysis. Autism Res. 2018;11(6):818–833. [DOI] [PubMed] [Google Scholar]
- 17. Young S, Furgal K. Exercise effects in individuals with autism spectrum disorder: A short exercise effects in individuals with autism spectrum disorder: A short review. Autism Open Access. 2016;6(3):180. [Google Scholar]
- 18. Sam K-L, Chow B-C, Tong K-K. Effectiveness of exercise-based interventions for children with autism: A systematic review and meta-analysis. Int J Learn Teach. 2015;1(2):98–103. [Google Scholar]
- 19. Tan BWZ, Pooley JA, Speelman CP. A meta-analytic review of the efficacy of physical exercise interventions on cognition in individuals with autism spectrum disorder and ADHD. J Autism Dev Disord. 2016;46(9):3126–3143. [DOI] [PubMed] [Google Scholar]
- 20. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV). Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 21. Mottron L, Dawson M, Soulières I, Hubert B, Burack J. Enhanced perceptual functioning in autism: An update, and eight principles of autistic perception. J Autism Dev Disord. 2006;36(1):27–43. [DOI] [PubMed] [Google Scholar]
- 22. Samson F, Mottron L, Soulières I, Zeffiro TA. Enhanced visual functioning in autism: An ALE meta-analysis. Hum Brain Mapp. 2012;33(7):1553–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bogdashina O. Sensory Perceptual Issues in Autism and Asperger Syndrome. Second edition. London: Jessica Kingsley Publishers; 2016. [Google Scholar]
- 24. Kapp SK, Steward R, Crane L, et al. ‘People should be allowed to do what they like’: Autistic adults' views and experiences of stimming. Autism. 2019. [Epub ahead of print]; DOI: 10.1177/1362361319829628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hillier A, Murphy D, Ferrara C. A pilot study: Short-term reduction in salivary cortisol following low level physical exercise and relaxation among adolescents and young adults on the autism spectrum. Stress Heal. 2011;27(5):395–402. [Google Scholar]
- 26. Zschucke E, Renneberg B, Dimeo F, Wüstenberg T, Ströhle A. The stress-buffering effect of acute exercise: Evidence for HPA axis negative feedback. Psychoneuroendocrinology. 2015;51:414–425. [DOI] [PubMed] [Google Scholar]
- 27. Celiberti DA, Bobo HE, Kelly KS, Harris SL, Handleman JS. The differential and temporal effects of antecedent exercise on the self-stimulatory behavior of a child with autism. Res Dev Disabil. 1997;18(2):139–150. [DOI] [PubMed] [Google Scholar]
- 28. Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016;20(4):442–462. [DOI] [PubMed] [Google Scholar]
- 29. Elliott RO, Dobbin AR, Rose GD, Soper HV. Vigorous, aerobic exercise versus general motor training activities: Effects on maladaptive and sterotypic behaviors of adults with both autism and mental retardation. J Autism Dev Disord. 1994;24(5):565–576. [DOI] [PubMed] [Google Scholar]
- 30. García-Villamisar D, Dattilo J, Muela C. Effects of B-active2 on balance, gait, stress, and well-being of adults with autism spectrum disorders and intellectual disability: A controlled trial. Adapt Phys Act Q. 2017;34(2):125–140. [DOI] [PubMed] [Google Scholar]
- 31. García-Villamisar DA, Dattilo J. Effects of a leisure programme on quality of life and stress of individuals with ASD. J Intellect Disabil Res. 2010;54(7):611–619. [DOI] [PubMed] [Google Scholar]
- 32. Mateos-Moreno D, Atencia-Doña L. Effect of a combined dance/movement and music therapy on young adults diagnosed with severe autism. Arts Psychother. 2013;40(5):465–472. [Google Scholar]
- 33. Savage MN, Taber-Doughty T, Brodhead MT, Bouck EC. Increasing physical activity for adults with autism spectrum disorder: Comparing in-person and technology delivered praise. Res Dev Disabil. 2018;73:115–125. [DOI] [PubMed] [Google Scholar]
- 34. LaLonde KB, MacNeill BR, Eversole LW, Ragotzy SP, Poling A. Increasing physical activity in young adults with autism spectrum disorders. Res Autism Spectr Disord. 2014;8(12):1679–1684. [Google Scholar]
- 35. Autistica. Your research priorities. London; undated. https://www.autistica.org.uk/our-research/your-research-priorities (accessed July 22, 2019). [Google Scholar]
- 36. Van Heijst BFC, Geurts HM. Quality of life in autism across the lifespan: A meta-analysis. Autism. 2015;19(2):158–167. [DOI] [PubMed] [Google Scholar]
- 37. VanVoorhis C, Morgan B. Understanding power and rules of thumb for determining sample sizes. Tutor Quant Methods Psychol. 2007;3(2):43–50. [Google Scholar]
- 38. Barthelemy C, Roux S, Adrien JL, et al. Validation of the revised behavior summarized evaluation scale. J Autism Dev Disord. 1997;27(2):139–153. [DOI] [PubMed] [Google Scholar]
- 39. Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil. 2009;30(6):1107–1114. [DOI] [PubMed] [Google Scholar]
- 40. Livingston LA, Happé F. Conceptualising compensation in neurodevelopmental disorders: Reflections from autism spectrum disorder. Neurosci Biobehav Rev. 2017;80:729–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Todd T, Miodrag N, Bougher SC, Zambom AZ, Al TET. A peer mentored physical activity intervention: An emerging practice for autistic college students. Autism Adulthood. 2019. [Epub ahead of print]; DOI: 10.1089/aut.2018.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rombaut L, Malfait F, Cools A, de Paepe A, Calders P. Musculoskeletal complaints, physical activity and health-related quality of life among patients with the Ehlers-Danlos syndrome hypermobility type. Disabil Rehabil. 2010;32(16):1339–1345. [DOI] [PubMed] [Google Scholar]
- 43. Pimentel J, Tojal R, Morgado J. Epilepsy and physical exercise. Seizure. 2015;25:87–94. [DOI] [PubMed] [Google Scholar]