Abstract
Background:
Many autistic adults report interpersonal traumas (IPTs) such as physical or sexual assault, which are often associated with posttraumatic stress and dissociation. Factors such as gender might make autistic individuals particularly vulnerable to experiencing IPT and negative posttraumatic symptoms.
Methods:
In this study, 687 self-identified autistic adults completed an online survey on their traumatic experiences and mental health symptoms.
Results:
Seventy-two percent of participants reported experiencing sexual assault, other unwanted or uncomfortable sexual experiences, or physical assault. Forty-four percent of participants met the criteria for posttraumatic stress disorder (PTSD), including 50% of those who had experienced IPT and 28% of those who had not (odds ratio = 2.50; 95% confidence interval 1.74–3.60). IPT was also significantly associated with higher levels of psychoform (p < 0.001) and somatoform (p < 0.001) dissociation. Autistic cisgender women and gender minorities experienced a significantly higher number of traumas (p = 0.004) and were significantly more likely than cisgender men to experience sexual IPT (p < 0.001) and meet the criteria for PTSD (p < 0.001). There were no significant differences between autistic individuals with and without a professional autism spectrum disorder (ASD) diagnosis.
Conclusions:
IPT is associated with potentially severe mental health outcomes for autistic adults. Autistic women and gender minorities may be particularly vulnerable to sexual IPT and adverse outcomes. Increased screening for a history of IPT and posttraumatic symptoms is recommended for all autistic adults regardless of ASD diagnosis status.
Lay summary
Why was this study done?
Many autistic people experience interpersonal traumas (IPTs) such as sexual or physical assault. These can lead to mental health challenges such as posttraumatic stress disorder (PTSD) or dissociation (a disconnection between individuals and aspects of their perceptions or sense of self). We wanted to better understand what might make autistic adults more likely to experience trauma and how it affects them.
What was the purpose of this study?
The purpose was to understand what might make autistic people more at risk of experiencing IPT and PTSD. We also wanted to know if IPT is associated with a higher risk of PTSD or dissociation.
What did the researchers do?
Six hundred eighty-seven autistic adults filled out an online survey about their traumatic experiences, PTSD symptoms, and dissociation symptoms. We analyzed their responses to see how often participants reported experiencing different types of trauma and whether they met the criteria for PTSD and clinical dissociation. We then compared trauma experiences and PTSD rates across genders and those with and without a professional autism spectrum disorder (ASD) diagnosis and compared PTSD rates and dissociation rates across participants who had versus had not experienced IPT.
What were the results of the study?
Seventy-two percent of autistic adults in this study reported having experienced sexual assault, another unwanted sexual experience, or physical assault. Almost half (44%) met the criteria for PTSD. Most participants (93%) also reported high levels of mind-based dissociation, and 32% reported high levels of body-based dissociation (dissociation that causes negative emotions to be experienced as physical problems such as headaches or trouble moving). Participants who had experienced IPT were almost twice as likely to meet the criteria for PTSD and scored higher on both measures of dissociation. Cisgender women and gender minorities were more likely to experience IPT and meet the criteria for PTSD than cisgender men. Participants with and without a professional ASD diagnosis did not differ.
What do these findings add to what was already known?
Most previous research on trauma and PTSD for autistic people was done on children and did not look at IPT specifically or compare people based on their gender or ASD diagnosis. As far as we know, this is the first study on posttraumatic dissociation in autistic adults.
What are potential weaknesses in the study?
The findings of this study may not apply to autistic adults as a whole. People who could have participated may not have been interested in the topic, may not have seen study advertisements and so been unaware of the study, or may not have had the time or energy to participate. Findings might have been different if different groups of autistic people participated more.
How will these findings help autistic adults now or in the future?
If professionals who help autistic people do not talk to them about trauma, traumatized autistic adults may not get the right support. This study could encourage professionals to screen more autistic people, especially women and gender minorities, for trauma.
Keywords: interpersonal trauma, sexual trauma, posttraumatic stress disorder, dissociation, gender differences, autistic adults
Background
Disability is associated with an increased risk of experiencing trauma, including interpersonal trauma (IPT).1–6 IPT, traumatic events in which one individual personally harms another, is a better predictor of posttraumatic stress than non-IPT. IPT includes traumas such as child maltreatment, assault, and intimate partner violence.7,8 Higher rates of IPT have been associated with many disabilities, including neurodevelopmental disability9–12 and intellectual disability.13,14 Autism is also associated with an increased risk of IPT. Studies have found that compared with typically developing children, autistic children face a significantly higher risk of child maltreatment (50.4%–80%)1,10–12,14–17 and bullying (44%–97.8%).1,12,17–22 Victimization often continues into adulthood, and autistic adults report more sexual victimization and bullying than nonautistic adults.23,24
Many factors associated with autism increase vulnerability to IPT. Differences in interpersonal communication can make it harder to form protective relationships and recognize warning signs from perpetrators. Intellectual disability or uneven cognitive profiles are a particular risk for child maltreatment. Other risks include mental health symptoms and difficulties regulating emotions.6,14,17–19,21,24–27 Parental stress, cultural attitudes toward disability, low socioeconomic status, reduced independence, and perception of vulnerability may also increase the risk of trauma.6,14,15,18,28 Even in the absence of a formal autism spectrum disorder (ASD) diagnosis, autistic traits and associated sociocultural factors may increase the risk of experiencing trauma.6,24
Many of these same factors can also worsen posttraumatic outcomes. Risks for maladaptive posttraumatic outcomes include executive dysfunction, difficulties processing emotions, and differences in information processing.24–26,29,30 In addition, autistic individuals may experience many stressors not traditionally considered traumatic, including social confusion, punishment for behaviors that come naturally to the individual, potentially stressful or stigmatizing interventions, intolerable sensory stimuli, and unexpected events.24–26,31,32 One study found that compared with victimized typically developing children, victimized autistic children had significantly more symptoms of posttraumatic stress.21 Another study found that 77% of trauma-exposed autistic youth showed symptoms of posttraumatic stress.33 One study of autistic adults found that 32% of autistic adults compared with 4% of nonautistic adults met the criteria for posttraumatic stress disorder (PTSD).24 Another found that 45% of trauma-exposed autistic adults had current probable PTSD, and 61% were likely to have met the criteria at some point in their life.25 Furthermore, even in nonautistic populations, autistic traits are associated with worse posttraumatic stress.6,24,34 However, not all studies have found higher rates of PTSD in autistic individuals, and it is largely unknown what predisposes some to develop PTSD following trauma.
In the general population, rates of PTSD are higher among females than males, and this is attributable, in part, to women being more likely to experience IPT such as sexual assault.7,24,25,35,36 Some studies have shown increased rates of total or sexual IPT toward disabled women compared with disabled men,2–4 and one study found higher rates of sexual IPT toward neurodevelopmentally disabled women.9 However, there is little research exploring gender, IPT, and PTSD for autistic adults. Two studies found that trauma-exposed autistic females and males are equally likely to develop posttraumatic stress,22,25 and an Israeli study found elevated PTSD symptoms in autistic females but not males.24 Even less is known about the risk for autistic gender minorities despite transgender individuals having a high risk for traumatic events and subsequent posttraumatic stress.37–40
To date, there are no studies on posttraumatic dissociation in autistic individuals. Psychoform (mind-based) dissociation includes experiences such as feeling detached from the world (derealization), feeling disconnected from one's body or emotions (depersonalization), difficulty remembering stressful experiences (dissociative amnesia), uncertainty about who one really is (identity confusion), and internal fragmentation (identity alteration). Somatoform (body-based) dissociation describes emotional stress manifesting as medical symptoms without an underlying medical cause. Mild dissociation can be a normal response to stress, anxiety, or fatigue, but long-term dissociation can severely impact quality of life. Trauma is a major risk factor for all forms of dissociation. Dissociation immediately following a trauma is common and predicts later symptoms of posttraumatic stress.41–46 If left untreated, individuals with posttraumatic dissociation are at a higher risk of revictimization47 and self-injury.41
Depersonalization and derealization have been found to accompany anxiety in 18% of autistic youth.48 In addition, a study found that 7% of autistic individuals meet a screening cutoff for somatization disorder,49 and somatization is higher among autistic compared with typically developing youth.50 Despite findings that dissociation is more prevalent among traumatized individuals in clinical and general populations, it is unknown if the same is true for autistic individuals.
Present study
This study has three aims: (1) to examine whether trauma exposure, particularly IPT exposure, differs according to gender and ASD diagnosis status for autistic adults; (2) to investigate whether PTSD rates differ according to gender and diagnosis status; and (3) to explore if IPT is associated with PTSD and dissociation for autistic adults.
Methods
Participants
The current study includes autistic participants with either a professional or suspected ASD diagnosis to minimize potential biases associated with diagnostic disparities on the basis of race/ethnicity, socioeconomic status, and gender.51–54 Recruitment sites were online communities frequented by autistic adults (autism-centric subreddits, Wrong Planet, and Autism Forums) and organizations that are for, or work in partnership with, autistic adults (the Academic Autism Spectrum Partnership in Research and Education [AASPIRE] and the Autism Self Advocacy Network [ASAN]). Every participant either self-reported a formal ASD diagnosis made by a medical professional or self-reported a suspected ASD diagnosis and scored above a 65 on the Ritvo Autism Asperger Diagnostic Scale—Revised (RAADS-R). The RAADS-R is an autism screener, and 65 is a commonly used cutoff to distinguish between populations with and without autism.55 In addition, each participant completed the Life Events Checklist for DSM-5 (LEC-5) or PTSD Checklist for DSM-5 (PCL-5). The majority of excluded data (347 participants) lacked these measures, and a minority (19 participants) had invalid response patterns (e.g., long stretches of the same response or conflicting responses to items). In total, 1053 individuals consented to participate in the study, and 687 individuals met the inclusion criteria and composed the final sample for the current study.
Table 1 presents participant demographics. A similar number of cisgender men and women participated in the study, and a sizeable minority of participants identified as nonbinary (i.e., their gender did not fit a man/woman binary). The sample is well educated; 47% (n = 319) of participants had postsecondary education. However, 17% (n = 117) were unemployed, and another 15% (n = 100) could not work due to disability. Data collection ran from the beginning of May to the end of August in 2018. Participants did not receive compensation for their participation in the study. The Institutional Review Board of the Georgia Institute of Technology approved this research.
Table 1.
Demographic Information
| Demographic variable | N (%) |
|---|---|
| Age | |
| 18–21 | 194 (28) |
| 22–30 | 255 (38) |
| 31–40 | 153 (22) |
| 41 or older | 84 (12) |
| Race and ethnicity | |
| White | 587 (86) |
| Black | 40 (6) |
| Another racial background | 32 (5) |
| Hispanic | 32 (5) |
| Education | |
| Less than high school | 48 (7) |
| High school diploma or equivalent, no college degree | 318 (46) |
| College degree or technical, vocational, or trade training only | 229 (33) |
| Postgraduate degree | 90 (13) |
| Vocation | |
| Student | 129 (19) |
| Employed | 317 (46) |
| Caregiver | 14 (2) |
| Unemployed | 117 (17) |
| On or seeking disability | 100 (15) |
| Gender | |
| Cisgender men | 230 (35) |
| Cisgender women | 242 (37) |
| Transgender women (male to female) | 13 (2) |
| Transgender men (female to male) | 40 (6) |
| Nonbinary, agender, or other | 127 (19) |
Materials and procedure
Autism: RAADS-R
The RAADS-R is an 80-item questionnaire that contains 64 questions about the traits of ASD as well as 16 reverse scored questions that describe normative behaviors. It asks whether these apply to the individual now and applied to the individual in the past (3 points), only apply to the individual now (2 points), only applied to the individual when they were younger than 16 (1 point), or never applied to the individual (0 points). The RAADS-R has excellent sensitivity (97%) and specificity (100%) when using a cutoff score of 65.55
Dissociation (psychoform): multiscale dissociation inventory
The Multiscale Dissociation Inventory (MDI) is a 30-item questionnaire that asks how often participants experienced psychoform dissociative symptoms over the past month. Responses range from 1 (never) to 5 (very often). The MDI contains six scales that each score a different type of psychoform dissociation, four of which correspond to clinical diagnoses. The MDI has been normed and standardized on 444 trauma-exposed individuals and validated in clinical, community, and university samples.56,57 In this study, Cronbach's alpha was 0.94 (0.77–0.91 for subscales).
Dissociation (somatoform): 20-item somatoform dissociation questionnaire
The 20-item Somatoform Dissociation Questionnaire (SDQ-20) asks participants to select on a scale from 1 (this applies to me NOT AT ALL) to 5 (this applies to me EXTREMELY) how often they experienced somatoform dissociative symptoms within the past year.58 The SDQ-20 has good discriminant validity for dissociative disorders.59 Cronbach's alpha in this study was 0.89.
Trauma history: LEC-5
The LEC-5 contains 17 items that describe potentially traumatic events and asks whether participants have directly experienced or been exposed to each event.60 It is correlated with PTSD symptoms and trauma-specific measures of distress.61
Posttraumatic stress: PCL-5
The PCL-5 contains 20 items and asks participants to rate how much posttraumatic symptoms have bothered them over the past month. Subscales pertain to DSM-5 PTSD criteria B (posttraumatic intrusions), C (avoidance of trauma reminders), D (negative alterations in mood and cognitions), and E (alterations in arousal and reactivity). Responses are on a scale from 0 (not at all) to 4 (extremely).62 It has excellent convergent and discriminant validity among clinical populations and adequate convergent and discriminant validity among nonclinical populations.63 Cronbach's alpha in this study was 0.95 (0.85–0.90 for criterion scales).
Design and procedure
The study consent form advised participants that they should participate only if they were comfortable answering questions pertaining to their mental health symptoms and trauma histories. At any point in time, participants could quit the survey and access a list of crisis hotlines and other mental health resources. The survey, which was on Qualtrics, had no time limit. Immediately following the completion of the survey, a screen debriefed participants and displayed a list of mental health resources.
The primary research questions for the present study are as follows:
-
1.
Does exposure to trauma and IPT differ according to gender and ASD diagnosis status?
-
2.
Do PTSD rates differ according to gender and ASD diagnosis status?
-
3.
Does IPT predict PTSD and dissociation?
The LEC-5 measures exposure to trauma. LEC-5 items include both IPT and non-IPTs and capture the type of exposure. For this study, endorsing having directly experienced physical assault, sexual assault, or other unwanted or uncomfortable sexual experiences constituted a history of IPT. IPT analyses do not separately include assault with a weapon because fewer than five participants endorsed this in the absence of physical or sexual assault. IPT analyses also do not include items that: fewer than 25 participants endorsed directly experiencing (captivity; combat or exposure to a war zone); could not have been directly experienced by the participant as the victim (sudden violent death; serious harm caused to another); or are not interpersonal (e.g., natural disaster; life-threatening illness or injury).
The researchers coded data as meeting criteria for a provisional PTSD diagnosis if, on the PCL-5, participants scored at or above the severity cutoff of 33 and reported a sufficient number and intensity of symptoms from criteria B, C, D, and E. We compared trauma exposure across genders and ASD diagnosis status using analysis of variance (ANOVA) and compared rates of IPT and PTSD using chi-square. We used odds ratios (OR) to compare the risk of PTSD among autistic individuals who had versus had not experienced IPT. We compared levels of psychoform and somatoform dissociation among autistic individuals who had versus had not experienced IPT using ANOVA. Finally, we performed logistic regression to clarify the influence of demographic variables on the relationships between gender, ASD diagnosis status, IPT, and PTSD. For all statistics, the alpha value was 0.05.
Results
Trauma exposure
There was a high level of trauma exposure in this sample (Supplementary Table S1). On average, participants reported exposure to 8.05 types of trauma (SD: 4.12) and direct experiences of 3.54 types (SD: 2.54). Ninety-one percent of the sample reported directly experiencing trauma. Seventy-two percent (n = 482) reported experiencing physical assault (n = 377, 56%), sexual assault (n = 211, 31%), or other unwanted or uncomfortable sexual experiences (n = 366, 54%).
Gender
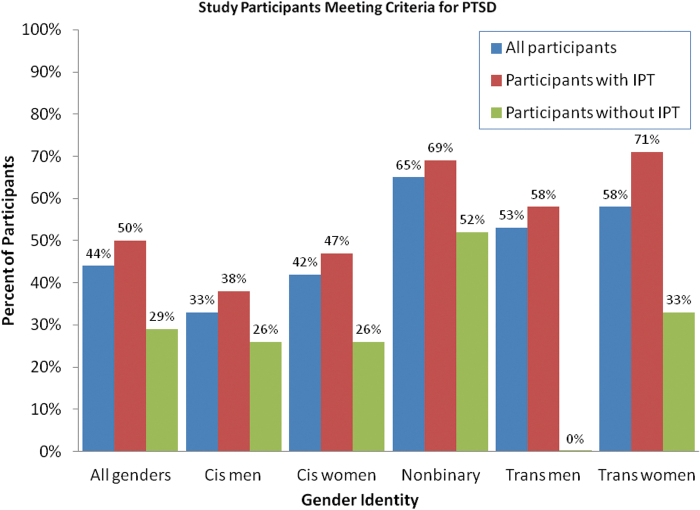
Significant gender differences emerged for the average number of types of trauma experienced (F(4, 636) = 3.87, p = 0.004; Table 2) and exposed to (F(4, 636) = 2.43, p = 0.04). Group differences also emerged for histories of IPT (χ2(4, N = 641) = 27.86, p < 0.001) and meeting criteria for PTSD (χ2(4, N = 643) = 36.54, p < 0.001). Figure 1 displays the differences in PTSD prevalence according to IPT history and gender. Post hoc analyses revealed that the difference in IPT by gender was driven by sexual IPT (χ2(4, N = 641) = 116.89, p < 0.001); physical assault rates did not differ (χ2(4, N = 641) = 0.694, p = 0.952).
Table 2.
Trauma Exposure and Posttraumatic Stress Disorder by Gender
| Gender |
M (SD) |
M (SD) |
N (%) |
N (%) |
N (%) |
N (%) |
|---|---|---|---|---|---|---|
| Exposeda | Experiencedb | IPTc | Sexual IPT | Physical assault | PTSD | |
| Cisgender men | 7.54 (4.52) | 3.05 (2.49) | 136 (60) | 61 (27) | 123 (54) | 74 (33) |
| Cisgender women | 8.50 (4.01) | 3.79 (2.55) | 184 (78) | 164 (69) | 135 (57) | 100 (42) |
| Nonbinary | 8.51 (3.75) | 3.87 (2.64) | 97 (76) | 88 (69) | 73 (57) | 81 (65) |
| Trans men | 8.61 (3.49) | 4.12 (2.12) | 37 (90) | 34 (85) | 24 (60) | 22 (54) |
| Trans women | 6.64 (4.37) | 3.27 (2.41) | 8 (73) | 6 (60) | 5 (50) | 5 (58) |
| Group differences | F (4, 636) = 2.43d | F (4, 636) = 3.87e | χ2 (4, N = 641) = 27.86f | χ2 (4, N = 641) = 116.89f | χ2 (4, N = 641) = 0.694 | χ2 (4, N = 643) = 36.54f |
Mean number of LEC-5 traumas experienced, witnessed, learned happened to a close friend or family member, or exposed to as part of a job.
Mean number of LEC-5 traumas directly experienced.
Direct experiences of IPT. Sexual IPT (sexual assault and unwanted or uncomfortable sexual experiences) and physical assault are subtypes of IPT; participants could endorse having directly experienced any combination of these to be counted as having experienced IPT.
p < 0.05.
p < 0.01.
p < 0.001.
IPT, interpersonal trauma; LEC-5, Life Events Checklist for DSM-5; PTSD, posttraumatic stress disorder.
FIG. 1.
Study participants meeting criteria for PTSD. The percent of participants who met the criteria for PTSD is displayed for all participants as well as separated by the gender identity of participants and by participants' history of IPT. The category “all genders” is the average across all gender categories, and the category “all participants” is the average across both participants with and without a history of IPT. It is important to note that participants without a history of IPT may still have a history of noninterpersonal trauma. IPT, interpersonal trauma; PTSD, posttraumatic stress disorder.
ASD diagnosis status
All participants self-reported identifying as autistic, and 453 (66%) reported a prior professional diagnosis of ASD. There were no significant differences between those with and without a diagnosis in regard to the number of trauma types participants directly experienced (F(1,673) = 2.82, p = 0.09) or were exposed to (F(1,673) = 1.341, p = 0.25). In addition, no group differences emerged for history of IPT (χ2(1, N = 674) = 0.648, p = 0.423) nor for meeting criteria for PTSD (χ2(1, N = 677) = 0.012, p = 0.914).
Symptoms associated with IPT
Posttraumatic stress disorder
Forty-four percent of participants (n = 297) met the criteria for PTSD on the PCL-5 (Supplementary Table S2), including 50% (n = 239) of those who experienced IPT and 28% (n = 54) of those who did not. This difference was significant (OR = 2.50; 95% confidence interval 1.74–3.60). Post hoc analysis revealed no difference in PTSD rates between those who had experienced physical assault versus sexual IPT.
Dissociation
Ninety-four percent of participants (n = 643) scored in a clinically relevant range on at least one scale of the MDI, and 83% (n = 570) on a scale that corresponds to a psychoform dissociative disorder (Table 3). In addition, 32% of participants (n = 221) scored above 35 on the SDQ-20. Participants who had experienced IPT reported significantly higher psychoform (F(1, 672) = 38.90, p < 0.001) and somatoform dissociation (F(1, 670) = 33.62, p < 0.001). Post hoc analysis revealed no difference in either psychoform or somatoform dissociation rates between those who had experienced physical assault versus sexual IPT.
Table 3.
Participant Measure Scores and Score Cutoffs
| Measure | Cutoffa | Mean (SD) | N Total | N (%) Above cutoff |
|---|---|---|---|---|
| RAADS-R | 65 | 154.11 (32.39) | 687 | 677 (99) |
| MDI (any subscale)b | 687 | 643 (94) | ||
| Disengagement | 14 | 18.05 (4.13) | 587 (85) | |
| Depersonalizationc | 9 | 12.67 (5.41) | 496 (72) | |
| Derealizationc | 12 | 13.39 (5.31) | 408 (59) | |
| Emotional constriction | 13 | 14.11 (5.84) | 413 (60) | |
| Memory disturbancesc | 11 | 11.91 (5.13) | 362 (53) | |
| Identity disturbancesc | 10 | 8.61 (5.49) | 176 (26) | |
| Clinical subscales,c any | 570 (83) | |||
| SDQ-20 | 35 | 32.60 (11.15) | 685 | 221 (32) |
| PCL-5 (total score) | 33 | 34.23 (20.35) | 677 | 349 (52) |
| PCL-5 (PTSD criteria) | 297 (44) |
Chosen cutoffs are discussed in more detail under Materials and Procedures.
MDI cutoffs are presented as raw scores; all MDI cutoff t-scores are 80 except for identity disturbances, which has a t-score cutoff of 95.
Corresponds to a psychoform dissociation diagnosis.
MDI, Multiscale Dissociation Inventory; PCL-5, PTSD Checklist for DSM-5; RAADS-R, Ritvo Autism Asperger Diagnostic Scale—Revised; SDQ-20, 20-item Somatoform Dissociation Questionnaire.
Logistic regression
When controlling for age, racial/ethnic minority status, education, employment, ASD diagnosis status, and gender, only age and gender predicted history of IPT (Table 4). Those older than 21 were more likely to report a history of IPT, as were cisgender women, transgender men, and nonbinary individuals. When controlling for the same variables and IPT history, only IPT history, employment, and gender significantly predicted PTSD. Those who had experienced IPT, those unable to work due to disability, and nonbinary individuals were most likely to meet the criteria for PTSD.
Table 4.
Odds Ratios for Interpersonal Trauma and Posttraumatic Stress Disorder
| Variable | IPT |
PTSD |
|||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 4 | |
| IPT | — | — | — | 2.502a | 2.617a | 2.608a | 2.313a |
| Age | |||||||
| 22–30 | 1.859b | 1.841c | 2.156b | 0.851 | 0.843 | 0.889 | |
| 31–40 | 2.518b | 2.481b | 3.504a | 0.518c | 0.509c | 0.620 | |
| 41–50 | 1.501 | 1.483 | 2.048 | 0.649 | 0.642 | 0.861 | |
| 51+ | 2.104 | 2.012 | 2.912c | 1.196 | 1.139 | 1.457 | |
| Racial minority | 1.551 | 1.538 | 1.454 | 1.344 | 1.334 | 1.316 | |
| Education | |||||||
| Less than HS | 1.138 | 1.137 | 1.250 | 1.062 | 1.063 | 1.164 | |
| College | 0.929 | 0.933 | 0.877 | 0.944 | 0.949 | 0.920 | |
| Postgraduate | 0.869 | 0.869 | 0.799 | 0.800 | 0.798 | 0.877 | |
| Employment | |||||||
| Unemployed | 1.069 | 1.075 | 1.064 | 1.447 | 1.495 | 1.501 | |
| Student | 0.828 | 0.832 | 0.881 | 0.905 | 0.910 | 0.892 | |
| Disability | 1.611 | 1.664 | 1.472 | 2.151b | 2.231b | 2.010c | |
| Other | 2.863 | 2.876 | 2.964 | 0.941 | 0.947 | 0.933 | |
| Diagnosis | 0.876 | 1.028 | 0.867 | 0.946 | |||
| Gender | |||||||
| Cis women | 2.531a | 1.256 | |||||
| Trans men | 9.392a | 1.658 | |||||
| Trans women | 1.826 | 2.204 | |||||
| Nonbinary | 2.574a | 2.814a | |||||
| R 2 | 0.0399 | 0.0406 | 0.0884 | 0.0384 | 0.0803 | 0.0812 | 0.1087 |
Reference groups: individuals with no IPT (PTSD models only); ages 18–21; non-Hispanic White; high school education; employed; professionally diagnosed with an autism spectrum disorder; cisgender men.
p < 0.001.
p < 0.01.
p < 0.05.
HS, high school.
Discussion
Participants reported a high rate of trauma exposure. In addition, a majority of participants reported directly experiencing IPT, a known risk factor for more severe posttraumatic outcomes. Seventy-two percent (n = 482) of participants reported experiencing sexual assault, other unwanted or uncomfortable sexual experiences, or physical assault. Accordingly, participants had a high rate of PTSD; 44% met the criteria for a provisional PTSD diagnosis. The odds of participants meeting the criteria for PTSD were 2.50 higher if they had experienced IPT (adjusted odds: 2.31). In addition, a majority of the sample experienced clinically relevant levels of psychoform and somatoform dissociation, and levels of dissociation were significantly higher for those who had experienced IPT. This study also highlights that gender may be an important risk factor for trauma exposure and negative posttraumatic outcomes for autistic adults. Cisgender women and gender minorities experienced significantly more traumas, especially IPT, and were more likely to meet the criteria for PTSD than cisgender men.
Studies of the general population show that while women experience trauma at rates comparable with men, women are more likely to develop PTSD. Different patterns of IPT explain much of this discrepancy. In particular, gender-based and sexual violence makes PTSD much more likely, and controlling for sexual trauma can level PTSD rates between genders.7,8,35,36 There are many reasons why gendered and sexual violence may have a particularly severe mental health impact, including social stigma, victim blaming, and denial of the trauma by people important to the survivor.35
Sexual violence also often involves betrayal. Traumas that are high in betrayal lead to more severe posttraumatic stress and dissociation.64 Although less often studied in this context, transgender and nonbinary individuals may be particularly vulnerable to high-betrayal traumas. Transgender individuals have an increased risk of experiencing sexual violence, intimate partner violence, and transphobic assault, severely impacting mental health.37–40 In this sample, women and gender minorities were more than twice as likely as cisgender men to report sexual IPT, which may have contributed to their higher PTSD rates.
In contrast, ASD diagnosis status did not predict IPT exposure or PTSD, indicating that individuals who identify as autistic are at risk of IPT and PTSD regardless of if they have been professionally diagnosed with ASD. In addition, logistic regression showed that other than gender, demographic variables contributed little to predicting IPT exposure or PTSD. Individuals older than 21 had higher odds of experiencing IPT compared with those younger than 21, reflecting cumulative opportunities to experience IPT across the life span. Being unable to work due to disability compared with being employed was associated with higher odds of PTSD, although it is unclear how much of this is due to PTSD leading to an inability to work as opposed to employment status influencing PTSD risk.
Future studies
Future studies should further explore the impact of gender and associated risks of exposure to sexual violence for autistic individuals. In particular, the perpetrators and context of this violence are important to understand. Different prevention strategies would be needed if, for example, the most pressing concern was identified as intimate partner violence versus assault attributed to the individuals' gender nonconformity. Participants in this study reported identifying as nonbinary or transgender at a higher rate than is found in studies of the general population, and even cisgender autistic women may feel less identification with their gender and so conform less to female gender roles.65,66 It is important to understand the potential risks and impacts of the intersection of gender-based violence and autism.
In general, more research is needed on the rates and risk factors of trauma exposure and the subsequent posttraumatic stress and dissociation in autistic adults. More should be done to understand the impact of trauma-related variables, such as age of onset and chronicity. This could help to shape interventions for trauma-exposed autistic adults by informing clinicians of likely posttraumatic symptoms and experiences, highlighting which autistic individuals are most at risk, and suggesting what variables may lead to worse mental health outcomes following trauma.
Limitations
Relying on online self-report data may lead to different outcomes than if professionals screened and diagnosed participants in person. Participants may also differ from the larger population of autistic adults in key ways. Because participants self-selected into the study, it is possible that autistic adults who experienced trauma were more interested in participating and so were overrepresented. However, this risk is lessened because study advertisements focused on dissociation, not trauma, and welcomed participants with no prior familiarity with the topic. Other studies have found similar rates of trauma and posttraumatic stress in autistic adults when using different strategies of participant recruitment.17,23–25 Autistic adults who agree to participate in research may nonetheless be different from those who do not have the time, energy, or interest, and this may bias study conclusions.
Other differences between study participants and autistic adults who did not participate may be due to the demographics of the online communities chosen for recruitment. Notably, 19% (n = 127) of participants identified as nonbinary, although this finding is not unprecedented. Other studies have found that autistic individuals feel less identification with and less positively toward their gender group, with 22%–27% of women and 8% of men reporting feeling partially or fully distanced from binary genders.65,66 Another important difference is that autistic individuals from minority racial and ethnic groups and autistic adults older than 40 were not well represented in this study. Special efforts may be needed to reach autistic ethnic minorities in particular due to underdiagnosis of these individuals.51,52 The generalizability of this study may also be limited because it oversamples autistic individuals with high literacy and membership in online communities.
Finally, although physical assault, sexual assault, and other unwanted sexual experiences are central to the understanding of IPT, these are not the only types of IPT. Understanding the prevalence and outcomes of other IPT types such as verbal abuse or childhood neglect requires further research. This study was also limited to comparing participants who had experienced IPT with those who had not experienced IPT; this latter group contained both individuals who had and had not experienced non-IPTs. To compare autistic adults with trauma histories with those without, a larger subsample without any trauma exposure is needed.
Implications
This study has important implications for policy designed to protect autistic individuals. If autistic women and gender minorities are at an increased risk of experiencing sexual IPT associated with potentially severe mental health symptoms such as posttraumatic stress and dissociation, implementing adequate preventions and interventions is crucial. In addition, the findings of this study are important for professionals (e.g., doctors, mental health clinicians, and support workers) who work with autistic individuals. Knowing that an autistic individual has experienced trauma can help to ensure that they receive appropriate trauma-informed treatment and support. Increased screening of all autistic adults for a history of trauma, particularly IPT, and resulting PTSD and dissociative symptoms is recommended to best fit services to the needs of autistic individuals and improve posttraumatic outcomes in this vulnerable yet historically underserved population.
Supplementary Material
Authorship Confirmation Statement
K.E.R. conceived of the study, participated in its design, collected the data, performed the statistical analyses, participated in the interpretation of data, and helped to draft the article. C.M.S. participated in the study design, participated in the interpretation of data, and helped to draft the article. J.L.S. participated in the study design and helped to draft the article. All authors read and approved the article before submission. The article has been submitted solely to this journal and is not published, in press, or submitted elsewhere.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Supplementary Material
References
- 1. Baladerian N, Coleman T, Stream J. Abuse of people with disabilities: Victims and their families speak out. 2013. https://ncvc.dspacedirect.org/handle/20.500.11990/998 (accessed July 15, 2019).
- 2. Hughes RB, Lund EM, Gabrielli J, Powers LE, Curry MA. Prevalence of interpersonal violence against community-living adults with disabilities: A literature review. Rehabil Psychol. 2011;56(4):302–319. [DOI] [PubMed] [Google Scholar]
- 3. Mitra M, Mouradian VE, Diamond M. Sexual violence victimization against men with disabilities. Am J Prev Med. 2011;41(5):494–497. [DOI] [PubMed] [Google Scholar]
- 4. Smith DL. Disability, gender and intimate partner violence: Relationships from the behavioral risk factor surveillance system. Sex Disabil. 2008;26(1):15–28. [Google Scholar]
- 5. Cohen MM, Forte T, Du Mont J, Hyman I, Romans S. Adding insult to injury: Intimate partner violence among women and men reporting activity limitations. Ann Epidemiol. 2006;16(8):644–651. [DOI] [PubMed] [Google Scholar]
- 6. Roberts AL, Koenen KC, Lyall K, Robinson E, Weisskopf MG. Association of autistic traits in adulthood with childhood abuse, interpersonal victimization, and posttraumatic stress. Child Abuse Negl. 2015;45:135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lilly M, Valdez C. Interpersonal trauma and PTSD: The roles of gender and a lifespan perspective in predicting risk. Psychol Trauma. 2011;4(1):140–144. [Google Scholar]
- 8. Breire J, Agee E, Dietrich A. Cumulative trauma and current posttraumatic stress disorder status in general population and inmate samples. Psychol Trauma. 2016;8(4);439–446. [DOI] [PubMed] [Google Scholar]
- 9. Platt L, Powers L, Leotti S, et al. The role of gender in violence experienced by adults with developmental disabilities. J Interpers Violence. 2015;32(1):101–129. [DOI] [PubMed] [Google Scholar]
- 10. Gotby VO, Lichtenstein P, Langstrom N, Pettersson E. Childhood neurodevelopmental disorders and risk of coercive sexual victimization in childhood and adolescence: A population-based prospective twin study. J Child Psychol Psychiatry. 2018;59(9):957–965. [DOI] [PubMed] [Google Scholar]
- 11. Dinkler L, Lundstrom S, Gajwani R, Lichtenstein P, Gillberg C, Minnis H. Maltreatment-associated neurodevelopmental disorders: A co-twin control analysis. J Child Psychol Psychiatry. 2017;58(6):691–701. [DOI] [PubMed] [Google Scholar]
- 12. Hellstrom, L. A systematic review of polyvictimization among children with attention deficit hyperactivity or autism spectrum disorder. Int J Environ Res Public Health. 2019;16(13):2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brendli KR, Broda MD, Brown R. Children with intellectual disability and victimization: A logistic regression analysis. Child Maltreat. 2021. DOI: 10.1177/1077559521994177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McDonnell CG, Boan AD, Bradley CC, Seay KD, Charles JM, Carpenter LA. Child maltreatment in autism spectrum disorder and intellectual disability: Results from a population-based sample. J Child Psychol Psychiatry. 2019;60(5):576–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pfeffer RD. Childhood victimization in a national sample of youth with autism spectrum disorders. J Policy Pract Intellect Disabil. 2016;13(4):311–319. [Google Scholar]
- 16. Mandell DS, Walrath CM, Manteuffel B, Sgro G, Pinto-Martin JA. The prevalence and correlates of abuse among children with autism served in comprehensive community-based mental health settings. Child Abuse Negl. 2005;29(12):1359–1372. [DOI] [PubMed] [Google Scholar]
- 17. Chan KL, Lo CKM, Ip P. Associating disabilities, school environments, and child victimization. Child Abuse Negl. 2018;83:21–30. [DOI] [PubMed] [Google Scholar]
- 18. Weiss JA, Fardella MA. Victimization and perpetration experiences of adults with autism. Front Psychiatry. 2018:9:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schroeder JH, Cappadocia MC, Bebko JM, Pepler DJ, Weiss JA. Shedding light on a pervasive problem: A review of research on bullying experiences among children with autism spectrum disorders. J Autism Dev Disord. 2014;44(7):1520–1534. [DOI] [PubMed] [Google Scholar]
- 20. Maïano C, Normand CL, Salvas MC, Moullec G, Aimé A. Prevalence of school bullying among youth with autism spectrum disorders: A systematic review and meta-analysis. Autism Res. 2016;9(6):601–615. [DOI] [PubMed] [Google Scholar]
- 21. Paul A, Gallot C, Lelouche C, Bouvard MP, Amestoy A. Victimisation in a French population of children and youths with autism spectrum disorder: A case control study. Child Adolesc Psychiatry Ment Health. 2018;12:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rose CA, Simpson CG, Moss A. The bullying dynamic: Prevalence of involvement among a large-scale sample of middle and high school youth with and without disabilities. Psychol Sch. 2015;52(5):515–531. [Google Scholar]
- 23. Brown-Lavoie SM, Viecili MA, Weiss JA. Sexual knowledge and victimization in adults with autism spectrum disorders. J Autism Dev Disord. 2014;44(9):2185–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haruvi-Lamdan N, Horesh D, Zohar S, Kraus M, Golan O. Autism spectrum disorder and post-traumatic stress disorder: An unexplored co-occurrence of conditions. Autism. 2020;24(4):884–898. [DOI] [PubMed] [Google Scholar]
- 25. Rumball F, Happé F, Grey N. Experience of trauma and PTSD symptoms in autistic adults: Risk of PTSD development following DSM-5 and non-DSM-5 traumatic life events. Autism Res. 2020. DOI: 10.1002/aur.2306. [DOI] [PubMed] [Google Scholar]
- 26. Kerns CM, Newschaffer CJ, Berkowitz SJ. Traumatic childhood events and autism spectrum disorder. J Autism Dev Disord. 2015;45(11):3475–3486. [DOI] [PubMed] [Google Scholar]
- 27. Holtmann M, Bölt S, Poustka F. Autism spectrum disorders: Sex differences in autistic behaviour domains and coexisting psychopathology. Dev Med Child Neurol. 2007;49(5):361–366. [DOI] [PubMed] [Google Scholar]
- 28. Hoover DW, Kaufman J. Adverse childhood experiences in children with autism spectrum disorder. Curr Opin Psychiatry. 2018;31(2):128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kinnaird E, Stewart C, Tchanturia K. Investigating alexithymia in autism: A systematic review and meta-analysis. Eur Psychiatry. 2019;55:80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Orejuela-Dávila AI, Cann A, Tedeschi RG. Alexithymia predicts posttraumatic growth and distress after trauma. J Loss Trauma. 2017;22(3):171–182. [Google Scholar]
- 31. Kupferstein H. Evidence of increased PTSD symptoms in autistics exposed to applied behavior analysis. Adv Autism. 2018;4(1):19–29. [Google Scholar]
- 32. Samuel P. Dissociative identity disorder, autism, and a conversation [Blog Post]. 2012. https://blog.donnawilliams.net/2012/06/07/dissociative-identity-disorder-autism-and-a-conversation/#more-4182 (accessed March 5, 2020).
- 33. Mehtar M, Mukaddes NM. Posttraumatic stress disorder in individuals with diagnosis of autistic spectrum disorders. Res Autism Spectr Disord. 2011;5(1):539–546. [Google Scholar]
- 34. Haruvi-Lamdan N, Lebendiger S, Golan O, Horesh D. Are PTSD and autistic traits related? An examination among typically developing Israeli adults. Compr Psychiatry. 2019;89:22–27. [DOI] [PubMed] [Google Scholar]
- 35. Silove D, Baker JR, Mohsin M, et al. The contribution of gender-based violence and network trauma to gender differences in post-traumatic stress disorder. PLoS One. 2017;12(2):e0171879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Guina J, Nahhas RW, Kawalec K, Farnsworth S. Are gender differences in DSM-5 PTSD symptomatology explained by sexual trauma? J Interpers Violence. 2019;34(21–22):4713–4740. [DOI] [PubMed] [Google Scholar]
- 37. Shipherd JC, Maguen S, Skidmore WC, Abramovitz SM. Potentially traumatic events in a transgender sample: Frequency and associated symptoms. Traumatology. 2011;17(2):56–67. [Google Scholar]
- 38. Reisner SL, Hughto JMW, Gamarel KE, Keuroghlian AS, Mizock L, Pachankis JE. Discriminatory experiences associated with posttraumatic stress disorder symptoms among transgender adults. J Couns Psychol. 2016;63(5):509–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Valentine SE, Peitzmeier SM, King DS, et al. Disparities in exposure to intimate partner violence among transgender/gender nonconforming and sexual minority primary care patients. LGBT Health. 2017;4(4):260–267. [DOI] [PubMed] [Google Scholar]
- 40. James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- 41. Rossi R, Longo L, Flore D, et al. Dissociation in stress-related disorders and self-harm: A review of the literature and a systematic review of mediation models. Giornale Italiano di Psicopatologia. 2019;25(3):162–171. [Google Scholar]
- 42. Cardeña E. The domain of dissociation. In: Lynn SJ, Rhue JW, eds. Dissociation: Clinical and Theoretical Perspectives. New York, NY: The Guilford Press;1994:15–31. [Google Scholar]
- 43. Holmes EA, Brown RJ, Manselld W, et al. Are there two qualitatively distinct forms of dissociation? A review and some clinical implications. Clin Psychol Rev. 2005;25(1):1–23. [DOI] [PubMed] [Google Scholar]
- 44. Spiegel D, Loewenstein RJ, Lewis-Fernández R, et al. Dissociative disorders in DSM-5. Depress Anxiety. 2011;28(9):824–852. [DOI] [PubMed] [Google Scholar]
- 45. Steinberg M. Advances in the clinical assessment of dissociation: the SCID-D-R. Bull Menninger Clin. 2000;64(2):146–163. [PubMed] [Google Scholar]
- 46. Van der Hart O, Nijenhuis ERS, Steele K. The Haunted Self: Structural Dissociation and the Treatment of Chronic Traumatization. New York: WW Norton; 2006. [Google Scholar]
- 47. Bockers E, Roepke S, Michael L, Renneberg B, Knaevelsrud C. Risk recognition, attachment anxiety, self-efficacy, and state dissociation predict revictimization. PLoS One. 2014;19(9):e108206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Storch EA, Wood JJ, Ehrenreich-May J, et al. Convergent and discriminant validity and reliability of the pediatric anxiety rating scale in youth with autism spectrum disorders. J Autism Dev Disord. 2012;42(11):2374–2382. [DOI] [PubMed] [Google Scholar]
- 49. Sukhodolsky DG, Scahill L, Gadow KD, et al. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. J Abnorm Child Psychol. 2008;36(1):117–128. [DOI] [PubMed] [Google Scholar]
- 50. Mahan S, Matson JL. Children and adolescents with autism spectrum disorders compared to typically developing controls on the Behavioral Assessment System for Children, Second Edition (BASC-2). Res Autism Spectr Disord. 2011;5(1):119–125. [Google Scholar]
- 51. Jo H, Schieve LA, Rice CE, et al. Age at autism spectrum disorder (ASD) diagnosis by race, ethnicity, and primary household language among children with special health care needs, United States, 2009–2010. Matern Child Health J. 2015;19(8):1687–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Durkin MS, Maenner MJ, Meaney FJ, et al. Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a U.S. cross-sectional study. PLoS One. 2010;5(7):e11551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Loomes R, Hull L, Mandy WPL. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(6):466–474. [DOI] [PubMed] [Google Scholar]
- 54. Russell G, Steer C, Golding J. Social and demographic factors that influence the diagnosis of autistic spectrum disorders. Soc Psychiatry Psychiatr Epidemiol. 2011;46(12):1283–1293. [DOI] [PubMed] [Google Scholar]
- 55. Ritvo RA, Ritvo ER, Guthrie D, et al. The Ritvo Autism Asperger Diagnostic Scale-Revised (RAADS-R): A scale to assist the diagnosis of autism spectrum disorder in adults: An international validation study. J Autism Dev Disord. 2011;41(8):1076–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Briere J. Multiscale Dissociation Inventory Professional Manual. Odessa, FL: Psychological Assessment Resources; 2002. [Google Scholar]
- 57. Briere J, Weathers FW, Runtz M. Is dissociation a multidimensional construct? Data from the multiscale dissociation inventory. J Trauma Stress. 2005;18(3):221–231. [DOI] [PubMed] [Google Scholar]
- 58. Nijenhuis ERS, Spinhoven P, Van Dyck R, Van der Hart O, Vanderlinden J. The development and the psychometric characteristics of the somatoform dissociation questionnaire (SDQ 20). J Nerv Ment Dis. 1996;184(11):688–694. [DOI] [PubMed] [Google Scholar]
- 59. Nijenhuis ERS. The scoring and interpretation of the SDQ-20 and SDQ-5. Activitas Nervosa Superior. 2010;52(1):24–28. [Google Scholar]
- 60. Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Life Events Checklist for DSM-5 (LEC-5). 2013. Instrument available from the National Center for PTSD at www.ptsd.va.gov (accessed October 21, 2020).
- 61. Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341. [DOI] [PubMed] [Google Scholar]
- 62. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5). 2013. Instrument available from the National Center for PTSD at www.ptsd.va.gov (accessed October 21, 2020).
- 63. Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. [DOI] [PubMed] [Google Scholar]
- 64. Martin CG, Cromer LD, DePrince AP, Freyd JJ. The role of cumulative trauma, betrayal, and appraisals in understanding trauma symptomatology. Psychol Trauma. 2013;52(2):110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Dewinter J, Graaf HD, Begeer S. Sexual orientation, gender identity, and romantic relationships in adolescents and adults with autism spectrum disorder. J Autism Dev Disord. 2017;47:2927–2934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Cooper K, Smith LGE, Russell AJ. Gender identity in autism: Sex differences in social affiliation with gender groups. J Autism Dev Disord. 2018;48:3995–4006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.