ABSTRACT
Background
Vaccine hesitancy was listed as one of the top 10 issues threatening global health in 2019. The objectives of this study were to (a) use an extended protection motivation theory (PMT) with an added trust component to identify predictors of vaccine hesitancy and (b) explore the predictive ability of vaccine hesitancy on vaccination behavior.
Methods
We conducted an online questionnaire from February 9 to April 9, 2021, in China. The target population was Chinese residents aged 18 and over. A total of 14,236 responses were received. Structural equation modeling was used to test the extended PMT model hypotheses.
Results
A total of 10,379 participants were finally included in this study, of whom 52.0% showed hesitancy toward vaccination. 2854 (27.5%) participants reported that they got flu shots in the past year, and 2561 (24.7%) participants were vaccinated against COVID-19. 2857 (27.5%) participants engaged in healthcare occupation. The model explained 85.7% variance of vaccine hesitancy. Self-efficacy was the strongest predictor, negatively associated with vaccine hesitancy (β = −0.584; p < .001). Response efficacy had a negative effect on vaccine hesitancy (β = −0.372; p < .001), while threat appraisal showed a positive effect (β = 0.104; p < .001). Compared with non-health workers, health workers showed more vaccine hesitancy, and response efficacy was the strongest predictor (β = −0.560; p < .001). Vaccine hesitancy had a negative effect on vaccination behavior (β = −0.483; p < .001), and the model explained 23.4% variance of vaccination behavior.
Conclusions
This study demonstrates that the extended PMT model is efficient in explaining vaccine hesitancy. However, the predictive ability of vaccine hesitancy on vaccination behavior is limited.
KEYWORDS: Vaccine hesitancy, protection motivation theory, behavior, adults
1. Introduction
With the development of medical technology, vaccination has become an important method to control diseases and contributed to a dramatic reduction in the prevalence and incidence of vaccine preventable disease (VPD). However, people’s hesitancy to get vaccinated is widespread worldwide,1–4 leading to a decrease in vaccine coverage and an increase in VPD. The Strategic Advisory Group of Experts (SAGE) defined vaccine hesitancy (VH) as “delay in acceptance or refusal of vaccination despite availability of vaccination services.”5 VH was listed as one of the top 10 issues threatening global health in 2019.6
In China, VH is a serious problem that needs attention. In 2013, a hepatitis B vaccine produced by Shenzhen Biokangtai was reported to have caused infant deaths, leading to a decline in parents’ confidence in the vaccines and rejection of vaccination.7 In 2018, the Changsheng vaccine scandal broke out in mainland China, with 252,600 unqualified diphtheria, tetanus, and pertussis combined vaccines reported to be used for child vaccination, undermining public confidence in vaccines.8 Du, Fanxing et al. suggested that 60% of caregivers expressed hesitancy about vaccination. Moreover, recent studies showed that 44.2% of Chinese adults were unwilling to get the COVID-19 vaccine and overall parental acceptance of childhood COVID-19 vaccines was only 50.0%.9,10 Therefore, VH has become an issue to be solved; exploring the influencing factors of VH may be crucial for effective interventions.
Effective behavior prevention intervention needs to be based on the corresponding theoretical basis. Health-related behavior changes theory constructed from the perspective of psycho-social plays an important role in the prediction, prevention and intervention of health behavior.11–13 Protection motivation theory (PMT) is a classical theory extensively used to explain and predict human behaviors.14–16 According to PMT, individual threat appraisal and coping appraisal jointly form the protective motivation and further promote the occurrence of behavior.17,18 Threat appraisal depends on an individual’s cognition about the severity and vulnerability of the negative consequences of the health threatened event. Coping appraisal consists of self-efficacy (cognition of individual’s ability to successfully perform protective behavior), response efficacy (cognition of the effectiveness of the protective behavior) and response cost (barriers to conducting protective behavior).19,20
A previous study concluded that PMT accounted for 62% of the variance in vaccination intention for seasonal influenza, with response efficacy being the strongest predictor.21 More recently, Xiao Q et al reported that the PMT model explained 26.6% of the variance in the vaccine willingness, and response efficacy, self-efficacy, and response cost were significantly correlated with willingness.9 Additionally, SAGE concluded that VH is influenced by factors such as confidence (do not trust vaccine or provider), complacency (do not perceive a need for a vaccine, do not value vaccination), and convenience (access to vaccines).22 The utility in interpreting VH is almost consistent between PMT and the standard 3 C model, with confidence and convenience reflecting coping appraisal and complacency reflecting threat appraisal.21 Consequently, PMT may be a rational theory to explain the VH.
However, inconsistencies exist in the different contexts of the relationship between PMT composition and vaccine intention. Camerini A-L et al reported that only response efficacy showed to be related to parents’ intention to MMR vaccination among central PMT concepts.23 Recent research showed that only the perceived severity of PMT was associated with motivation to have a vaccination against COVID-19.24 Furthermore, according to PMT, the intention is the best predictor of behavior. As for VH, although we generally agree that is an important reason for the reduced vaccine coverage, the predictive ability of VH on actual vaccine uptake remains unclear. Some studies even suggest that VH may not be directly related to vaccine uptake. For example, Freed et al. research showed that despite parents showing some degree of concern, the vast majority of them accept all vaccines for their children on schedule and are less likely to have ever refused a vaccine.25 In addition, in previous studies, PMT was mostly focused on the explanation of vaccination intention, but few studies on vaccination behavior. Moreover, PMT is substantially consistent with the standard 3 C model of vaccine hesitancy. Still, the confidence component is defined as “trust in the vaccines or the system that delivers them,”26 whereas PMT lacks the consideration of trust in providers. Thus, we attempted to develop an extended PMT model with a trust component to examine VH and vaccination behavior prediction.
In this study, we aimed to 1) use an extended protection motivation theory (PMT) with an added trust component to identify predictors of VH and 2) examine the predictive ability of VH on vaccination behavior. Moreover, healthcare workers (HCWs) are a key focus group for vaccination; their attitudes influence patients’ vaccination decisions.27,28 Thus, this study further examined whether there are differences influences between HCWs and the general population. Accordingly, we proposed the following hypotheses:
H1: a) Perceived severity, b) perceived vulnerability, c) self-efficacy, d) response efficacy, and e) trust negatively affect VH. f) Response cost has a positive effect on VH.
H2: VH negatively affects vaccine uptake.
Based on these hypotheses, the theoretical model is depicted in Figure 1.
Figure 1.
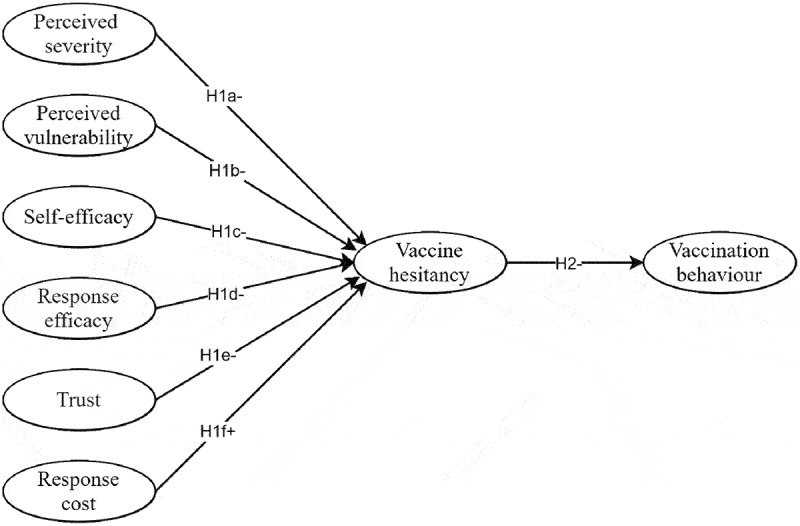
Hypothesis model.
2. Materials and methods
2.1. Participants and procedure
We conducted a cross-sectional online survey from February 9 to April 9, 2021, via the website Wenjuanxing, a widely used electronic questionnaire survey platform in China. The research team disseminated the survey link through social network platforms of OpenICQ, WeChat, Sina Weibo to their respective online communities and encouraged family members, friends, and voluntary participants to forward it to more people. The Ethics Committee of Wuxi Center for Disease Control and Prevention (2020No10) approved this study. The target population of the survey was Chinese residents aged 18 and over. Each participant obtained informed consent before completing the questionnaire online. Participants received a CNY 1.5 reward (equivalent to $0.23) upon survey completion, and a mobile phone number can only be used to complete the questionnaire once.
2.2. Measures
We developed a questionnaire consisting of four parts: socio-demographic characteristics, PMT measures, vaccine hesitancy and vaccination behavior. After we developed a preliminary questionnaire, 20 students and five professors of the Southeast University were invited to perform a pilot test. Adjustments were made in some items to ensure clarity, readability and logicality. The reliability and validity analysis results of the pilot test are shown in Supplementary 2 Table S1 and Table S2. Measurement items were referenced and modified from existing literature.21,29 The final questionnaire measures are shown in Table 1 and the full questionnaire is shown in Supplementary 1.
Table 1.
Questionnaire measures
| Measures | Items | Response scale |
|---|---|---|
| Perceived severity | PS1. Diseases can seriously affect health and cannot be resisted by natural immunity alone. | Strongly disagree (1) to strongly agree (5) |
| PS2. My body can fight off disease even if I get it, so there is no need for vaccination. | Strongly disagree (1) to strongly agree (5) | |
| Perceived vulnerability | PV1. Without vaccinations, I am vulnerable to diseases. | Strongly disagree (1) to strongly agree (5) |
| PV2. I don’t think it’s necessary to get vaccinated because the disease risk is low. | Strongly disagree (1) to strongly agree (5) | |
| Self-efficacy | SE1. I’d be able to get vaccines if I wanted to. | Strongly disagree (1) to strongly agree (5) |
| SE2. I can afford vaccines. | Strongly disagree (1) to strongly agree (5) | |
| Response efficacy | RE1. I think vaccines are safe. | Strongly disagree (1) to strongly agree (5) |
| RE2. I think vaccines are effective. | Strongly disagree (1) to strongly agree (5) | |
| RE3. I think it’s good for my health to get vaccinated. | Strongly disagree (1) to strongly agree (5) | |
| Response cost | RC1. I think the vaccination clinic service is poor. | Strongly disagree (1) to strongly agree (5) |
| RC2. I think it’s convenient and takes a short time to get the vaccination. | Strongly disagree (1) to strongly agree (5) | |
| Trust | T1. I think the management process of vaccines is reliable and trustworthy. | Strongly disagree (1) to strongly agree (5) |
| T2. The information about vaccines I receive from nurses or doctors is reliable and trustworthy. | Strongly disagree (1) to strongly agree (5) | |
| T3. The information about vaccines I receive from the Center for Disease Control is reliable and trustworthy. | Strongly disagree (1) to strongly agree (5) | |
| T4. The information about vaccines I receive from the government is reliable and trustworthy. | Strongly disagree (1) to strongly agree (5) | |
| Vaccine hesitancy | VH1. I’m hesitant (intent to delay or reject) about getting vaccinations. | Strongly disagree (1) to strongly agree (5) |
| VH2. If my family, friends, or doctor suggests I get the vaccine, I usually get it. | Strongly disagree (1) to strongly agree (5) | |
| Vaccination behavior | VB1. Did you get a flu vaccine in the past year? | No (1) or Yes (2) |
| VB2. Did you get a COVID-19 vaccine? | No (1) or Yes (2) |
Socio-demographic characteristics. We collected information on participants’ age, gender, educational background, annual household income, healthcare occupation, and health status.
PMT measures. Derived from the extended PMT model, the survey included measures of perceived severity (items PS1, PS2), perceived vulnerability (items PV1, PV2), self-efficacy (items SE1, SE2), response efficacy (items RE1, RE2, RE3), response cost (items RC1, RC2) and trust (items T1, T2, T3, T4). Each item was measured on a 5-point Likert scale with the answer ranging from 1 (“strongly disagree”) to 5 (“strongly agree”). A higher item score indicates a higher level of PMT component, whereas scores of items PS2, PV2 and RC2 were flipped because they were worded reverse.
Vaccine hesitancy. We measured VH using two items (“VH1. I’m hesitant (intent to delay or reject) about getting vaccinations.” and “VH2. If my family, friends, or doctor suggests I get the vaccine, I usually get it.”) with 5-point Likert scale also. Similarly, we flipped the score on reverse item VH2. Higher scores of the two items represented higher intention to VH.
Vaccination behavior. Vaccination behavior was assessed by two items (“VB1. Did you get a flu vaccine in the last year?” and “VB2. Did you get a COVID-19 vaccine?”) with a binary response format where 1 indicates “No” and 2 indicates “Yes.” We chose these two vaccines to represent vaccination behavior because they were more closely related to the individual’s recent vaccination attitude. The flu vaccine is an optional and self-pay non-EPI vaccine in China; meanwhile, it can be obtained every epidemic season. As for the COVID-19 vaccine, COVID-19 is a global pandemic, and whether or not to be vaccinated against the newly developed vaccine is a choice many people face.
2.3. Data analysis
Based on the pilot test, we found that it took at least 40 seconds to complete the questionnaire, so 40 seconds was set as the cutoff value to exclude participants who did not seriously participate in the survey. We defined the completion rate of the complete questionnaire as 80%, so the questionnaire with more than 3 unfilled items were excluded. In addition, logical contradiction questionnaires were excluded in the subsequent analysis.
Descriptive statistics were used to analyze the socio-demographic characteristics of the participants. Additionally, we used the average score of the two items (item VH1 and VH2) to measure the level of VH of the respondents, with a cutoff of 3 points, and 3 points or above were considered VH. Multivariate logistic regression analysis was performed to explore the influence of socio-demographic characteristics to vaccine hesitancy.
We calculated Cronbach’s α to determine the reliability of the measurement model (Supplementary 2 Table S3). We performed confirmatory factor analysis (CFA) to assess the validity of the measurement model and calculated average variance extracted (AVE) and composite reliability (CR) to assess convergent validity (Supplementary 2 Table S3). Cronbach’s α values above 0.70 indicated that the reliability was acceptable, while AVE values above 0.50 and CR values above 0.70 were considered as acceptable validity. Then Pearson correlation analysis was used to examine the associations between studied variables.
Structural equation modeling (SEM) was utilized to verify the research model. Fit indexes including goodness-of-fit index (GFI) >0.90, adjusted goodness-of-fit index (AGFI) >0.90, comparative fit index (CFI) >0.90, parsimony normed fit index (PNFI) >0.50, and root mean square error of approximation (RMSEA) <0.08, which indicated the acceptable model fit.30 Further, we employed the multi-group SEM to analyze the differences between HCWs and non-HCWs. We performed the analysis to compare the measurement weights, structural weights, structural covariance, structural residual, and measurement residual of HCWs and non-HCWs.
Statistical analyses were conducted in SPSS 25 and AMOS 24. The two-side p-value of <0.05 was considered statistically significant.
3. Results
3.1. Socio-demographic characteristics of participants
A total of 14,236 responses were received, and 10,379 were finally included in the study after excluding unqualified questionnaires. The flow chart of questionnaire inclusion is shown in Figure 2. The socio-demographic characteristics of these participants are shown in Table 2. Among these participants, people aged 26–35 make up the largest proportion (n = 4081; 39.3%), and just over half of were women (n = 5564; 53.6%), and almost two-thirds were college-educated (n = 6909; 66.6%), and people earning between 50,000 and 100,000 RMB made up the largest percentage (n = 3591; 34.6%), and 2857 (27.5%) participants engaged in healthcare occupation. 2854 (27.5%) participants reported that they got flu shots in the past year, and 2561 (24.7%) participants were vaccinated against COVID-19.
Figure 2.
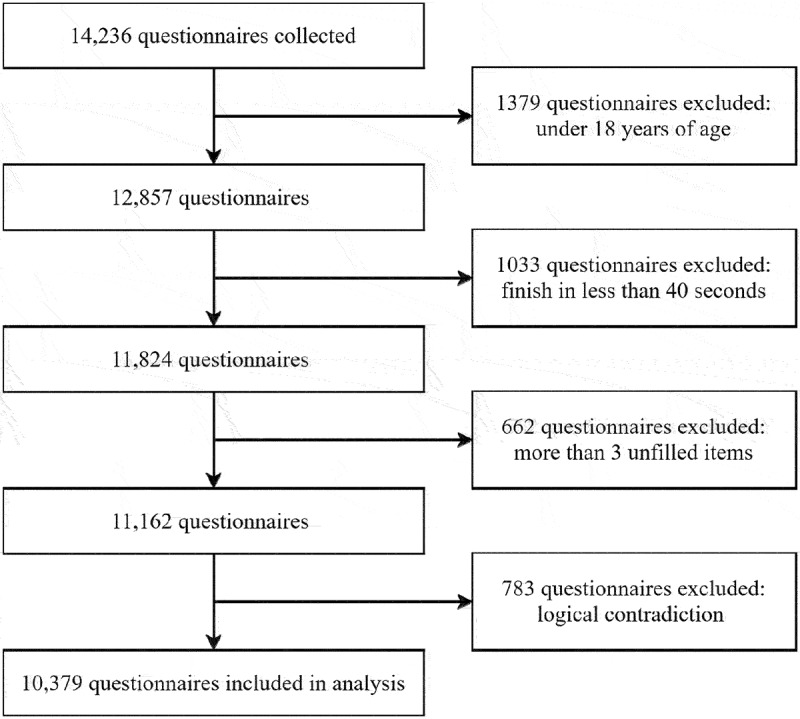
Flow chart of questionnaire inclusion.
Table 2.
Socio-demographic characteristics and logistic regression analysis
| Vaccine hesitancy |
||||||
|---|---|---|---|---|---|---|
| Socio-demographic characteristics | n (%) | No (%) | Yes (%) | OR | 95% CI | p-Value |
| Total | 10379 (100.0) | 4981 (48.0) | 5398 (52.0) | |||
| Age (years) | ||||||
| 18–25* | 3152 (30.4) | 1438 (45.6) | 1714 (54.4) | |||
| 26–35 | 4081 (39.3) | 2015 (49.4) | 2066 (50.6) | 0.891 | (0.808, 0.984) | 0.022 |
| 36–45 | 1899 (18.3) | 917 (48.3) | 982 (51.7) | 0.870 | (0.770, 0.982) | 0.024 |
| ≥46 | 1247 (12.0) | 611 (49.0) | 636 (51.0) | 0.729 | (0.632, 0.840) | <0.001 |
| Gender | ||||||
| Man* | 4815 (46.4) | 2448 (50.8) | 2367 (49.2) | |||
| Woman | 5564 (53.6) | 2533 (45.5) | 3031 (54.5) | 1.142 | (1.052, 1.238) | 0.001 |
| Education background | ||||||
| Junior high school or below * | 554 (5.3) | 257 (46.4) | 297 (53.6) | |||
| High school graduate or equivalent | 1566 (15.1) | 779 (49.7) | 787 (50.3) | 0.954 | (0.780, 1.167) | 0.648 |
| College or equivalent | 6909 (66.6) | 3403 (49.3) | 3506 (50.7) | 0.906 | (0.751, 1.092) | 0.299 |
| Postgraduate or above | 1350 (13.0) | 542 (40.1) | 808 (59.9) | 1.212 | (0.975, 1.505) | 0.083 |
| Annual household income (10,000 RMB) | ||||||
| <5* | 1695 (16.3) | 699 (41.2) | 996 (58.8) | |||
| 5–10 | 3591 (34.6) | 1793 (49.9) | 1798 (50.1) | 0.707 | (0.626, 0.799) | <0.001 |
| 11–15 | 2559 (24.7) | 1363 (53.3) | 1196 (46.7) | 0.618 | (0.541, 0.705) | <0.001 |
| ≥16 | 2534 (24.4) | 1126 (44.4) | 1408 (55.6) | 0.781 | (0.680, 0.897) | <0.001 |
| Healthcare occupation | ||||||
| No* | 7522 (72.5) | 3731 (49.6) | 3791 (50.4) | |||
| Yes | 2857 (27.5) | 1250 (43.8) | 1607 (56.2) | 1.734 | (1.569, 1.916) | <0.001 |
| Health status | ||||||
| Very good* | 4862 (46.8) | 2718 (55.9) | 2144 (44.1) | |||
| Good | 4087 (39.4) | 1730 (42.3) | 2357 (57.7) | 1.591 | (1.456, 1.738) | <0.001 |
| Fair | 1332 (12.8) | 495 (37.2) | 837 (62.8) | 1.943 | (1.708, 2.211) | <0.001 |
| Poor | 79 (0.8) | 31 (39.2) | 48 (60.8) | 1.790 | (1.126, 2.845) | 0.014 |
| Very poor | 19 (0.2) | 7 (36.8) | 12 (63.2) | 1.892 | (0.731, 4.899) | 0.189 |
| Did you get a flu vaccination in the last year? | ||||||
| No* | 7525 (72.5) | 3341 (44.4) | 4184 (55.6) | |||
| Yes | 2854 (27.5) | 1640 (57.5) | 1214 (42.5) | 0.745 | (0.670, 0.828) | <0.001 |
| Did you get a COVID-19 vaccination? | ||||||
| No* | 7818 (75.3) | 3466 (44.3) | 4352 (55.7) | |||
| Yes | 2561 (24.7) | 1515 (59.2) | 1046 (40.8) | 0.558 | (0.500, 0.624) | <0.001 |
*Reference variable.
3.2. Vaccine hesitancy of the participants
Measured by items VH1 and VH2, 5398 (52.0%) of them showed hesitancy toward vaccination (3 points or above). The multivariate logistic regression analysis (Table 2) showed that those aged 18–25 were more hesitant than any other age groups. Females were more hesitant compared with males (OR = 1.142; 95%CI: 1.052, 1.238). Participants with low-level income presented more hesitant than other groups. HCWs showed more VH compared with non-HCWs (OR = 1.734; 95%CI: 1.569, 1.916). Participants who reported being in very good health were more positive about the vaccines. In addition, participants who were not vaccinated against influenza or COVID-19 reported more VH compared with those vaccinated.
3.3. Measurement model
According to the reliability and validity analyses results, standard loadings of item PS1 was −0.022, and Cronbach’s α of perceived severity was −0.042 (Supplementary 2 Table S3). Therefore, item PS1 was deleted. Due to the limited number of items, we combined perceived severity and perceived vulnerability into threat appraisal, with items PS2, PV1 and PV2 as the measurement variables of threat appraisal. Then the reliability and validity were analyzed again. The results satisfied the reliability and validity requirements (Supplementary 2 Table S4). The Pearson correlation analysis results are shown in Supplementary 2 Table S5, and the correlation is significant.
3.4. Structural equation model and testing results
3.4.1. Hypothesis testing results of the research model
The model is illustrated in Figure 3 with a goodness-of-fit results of GFI = 0.920, AGFI = 0.885, CFI = 0.900, PNFI = 0.610, and RMSEA = 0.052. Standardized path coefficients of the model are presented in Table 3. VH significantly affected vaccination behavior (β = −0.483; p < .001), which supported H2. Both self-efficacy (β = −0.584; p < .001) and response efficacy (β = −0.372; p < .001) showed significant negative effects on VH. Thus, H1c and H1d hypotheses were proven. However, we merged perceived severity and perceived vulnerability into threat appraisal, and the coefficients of threat appraisal (β = 0.104; p < .001) indicated a positive effect. So H1a and H1b were not proven. Trust (β = −0.032; p = .693) and response cost (β = −0.030; p = .299) were not statistically significant. Therefore, these results failed to confirm H1e and H1f. Further, the R2 value explained 85.7% of VH variance and 23.4% in vaccination behavior.
Figure 3.
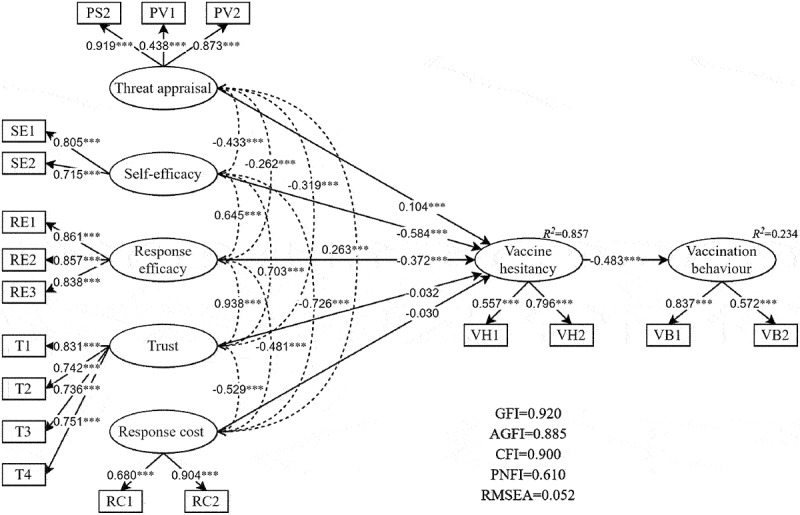
Results of the final research model.
Table 3.
Summary of findings regarding hypotheses
| Path | Stand. Coeff. | S.E. | C.R. | p-Value |
|---|---|---|---|---|
| Threat appraisal →Vaccine hesitancy | 0.104 | 0.005 | 6.477 | *** |
| Self-efficacy →Vaccine hesitancy | −0.584 | 0.025 | −11.975 | *** |
| Response efficacy →Vaccine hesitancy | −0.372 | 0.037 | −4.973 | *** |
| Trust →Vaccine hesitancy | −0.032 | 0.049 | −0.395 | 0.693 |
| Response cost →Vaccine hesitancy | −0.030 | 0.008 | −1.204 | 0.299 |
| Vaccine hesitancy →Vaccination behavior | −0.483 | 0.024 | 16.723 | *** |
Stand. Coeff. = standardized path coefficient; S.E. = Standard error; C.R. = critical ratio; *** p < 0.001.
3.4.2. Subgroup analysis results
Table 4 lists the multi-group analysis results. The standardized path coefficients of the HCWs and non-HCWs groups were consistent with the significant results of the overall SEM model path test done above. In comparison, response efficacy was the strongest predictor of HCWs (β = −0.560; p < .001), while self-efficacy was the strongest predictor of non-HCWs (β = −0.584; p < .001). For the path of vaccine hesitancy to vaccination behavior, vaccine hesitancy showed a higher negative effect of HCWs (β = −0.584; p < .001) than non-HCWs (β = −0.493; p < .001).
Table 4.
Multi-group analysis results of healthcare occupation
| Path | Healthcare workers |
Non-healthcare workers |
||||
|---|---|---|---|---|---|---|
| Stand. Coeff. | S.E. | p-Value | Stand. Coeff. | S.E. | p-Value | |
| Threat appraisal →Vaccine hesitancy | 0.284 | 0.019 | *** | 0.043 | 0.008 | 0.011 |
| Self-efficacy →Vaccine hesitancy | −0.476 | 0.080 | *** | −0.584 | 0.044 | *** |
| Response efficacy →Vaccine hesitancy | −0.560 | 0.136 | *** | −0.268 | 0.081 | 0.001 |
| Trust →Vaccine hesitancy | 0.234 | 0.268 | 0.121 | −0.161 | 0.111 | 0.076 |
| Response cost →Vaccine hesitancy | −0.053 | 0.025 | 0.138 | −0.031 | 0.018 | 0.351 |
| Vaccine hesitancy →Vaccination behavior | −0.584 | 0.015 | *** | −0.493 | 0.009 | *** |
Stand. Coeff. = standardized path coefficient; S.E. = Standard error; *** p < 0.001.
4. Discussion
In this cross-sectional online survey of vaccine hesitancy among Chinese adults, 52.0% of them expressed hesitation about vaccination, which is a high rate of vaccine hesitancy that needs our attention. In this study, we construct an extended PMT model to predict VH and vaccination behavior. VH had a negative association with vaccination behavior, and the model explained 85.7% variance of VH and 23.4% variance of vaccination behavior. While PMT is not a perfect predictor of vaccination behavior, we think this study still provides valuable insights into the prediction of vaccine hesitancy intentions. We found that self-efficacy and response efficacy was negatively affected VH; conversely, threat appraisal showed a positive effect.
The results showed that, as we expected to assume, self-efficacy and response efficacy negatively affected vaccine hesitancy. In previous studies, response efficacy and self-efficacy had significant influences on the willingness to receive the COVID-19 vaccine among a cross-sectional online survey.9 A Switzerland study reported that response efficacy showed to be related to parents’ intention to MMR vaccination among central PMT concepts.23 Similar results have been found in studies in Mainland China and Hong Kong.31,32 Our results provide further support for this relationship. Therefore, future VH interventions should reduce the cost of vaccination and increase confidence in access to vaccination. Meanwhile, increasing the scientific publicity of vaccination lets people understand the role and effect of the vaccine.
Existing research generally suggested that the high level of threat appraisal was associated with stronger intentions and higher uptake of vaccination,21,33,34 yet our study presented an opposite result. We speculate that the positive effect of threat appraisal maybe because we surveyed at the time of the COVID-19 epidemic and introduced the newly developed COVID-19 vaccine to the population. At this point, although our questionnaire was aimed at the attitude of universal vaccines, participants may inevitably be associated with the COVID-19 vaccine. As a result, both threat appraisal and VH increased. This psychology may arise because exposure to images of illness and fear can exacerbate anxiety and lead to maladaptive behavior. Individuals lack the confidence to deal directly with the threat.35,36 Therefore, while publicizing the risk of disease, the government should also popularize scientific countermeasures to avoid excessive anxiety over the condition.
Vaccine hesitancy performed a significant negative effect on vaccination behavior. Meanwhile, threat appraisal, response efficacy, and self-efficacy had indirect effects on vaccination behavior. However, even the extended PMT model could predict only around 20% vaccination behavior. There are two possible reasons for the intention-behavior gap. First, VH is a context-specific phenomenon, varying across time, place and vaccines.22 Different vaccines produce different behavioral outcomes, and people may accept one vaccine but decline another because their decision is based on vaccine-specific features.37 We used flu and COVID vaccines as the measure of vaccination behavior may get one-sided results. Second, vaccination acceptance is a behavior that results from a complex decision-making process, with socio-cultural and political factors also influencing the decision.5 Studies have suggested that descriptive norms (copying others’ behavior) explain significant variance in vaccination behavior.32,38 Therefore, the influence of social descriptive norms can be explored in future studies.
In consistent with some previous studies, HCWs showed more hesitation than non-HCWs.39,40 Many studies have found that HCWs refuse vaccination because of the risk of side effects and lack of confidence in vaccines.41–43 In our study, PMT elements presented different effects between them. Response efficacy was a strong predictor of VH for HCWs, while self-efficacy was the strongest predictor of non-HCWs. These results are probably due to HCWs making decisions based on their medical knowledge about the vaccine’s efficacy; in contrast, the ability of the general population to believe that they can perform vaccination is critical in stimulating motivational, cognitive and affective processes.44
Our study found that the impact of some demographic characteristic factors on VH is also noteworthy. In the present study, age, gender, annual household income and health status were associated with VH. People aged 18 to 25 were more hesitant than any other age group, similarly, previous research has shown that older people show more positive attitudes toward vaccines.45 In line with previous studies, women were more hesitant than men, probably because men are more likely to engage in risky behavior than women.28,46 Participants with low-level income presented more hesitation, the hesitation of these people may be related to trust issues in the health provider.47 Participants who thought they were very healthy showed less hesitation, possibly because people with less confidence in their health are more cautious about making health decisions.
This study has several limitations. First, our survey collected the data via an online questionnaire survey, a convenient sampling approach. Our study sample had disproportionately more HCWs and was only collected in China, which might limit the generalizability of our results. Second, this study was a cross-sectional survey, so the test of intention-behavior relation did not satisfy causal inference. Further longitudinal studies with interventions are needed to determine the ability of intention to predict behavior. Third, data collection was self-reported, which could have a recall bias. Moreover, we performed this survey when the COVID-19 vaccine was beginning to be promoted, and people might be affected by the new vaccine, which could cause potential biases. Finally, due to the limited number of items, we merged perceived severity and perceived vulnerability into threat appraisal. However, the positive effect of threat appraisal on VH cannot prove the effect of perceived severity and perceived vulnerability, and the effects of these constructs must be further clarified.
5. Conclusion
This study demonstrates that the extended PMT model is efficient in explaining vaccine hesitancy. Self-efficacy and response efficacy had negative effects on vaccine hesitancy, while threat appraisal showed a positive effect. Response efficacy was a strong predictor of VH for HCWs, while self-efficacy was the strongest predictor of non-HCWs. Vaccine hesitancy had a significant negative effect on vaccination behavior. However, the model’s predictive ability for vaccination behavior is limited, which needs further exploration in the future.
Supplementary Material
Funding Statement
Supported by the Wuxi City Technology Development Fund (N20191007); Postgraduate Research & Practice Innovation Program of Jiangsu Province (KYCX20_0153); the Fundamental Research Funds for the Central Universities (3225002102D); Public Health Research Center of Jiangnan University (JUPH201845). The funder/sponsor did not participate in the work.
Author contributions
M.L., H.J., and Q.W. designed the study. M.L., L.Y. and Yue.H. performed data collection. M. L., T.C. and Ying.H. performed data analysis. H.J., M.L., N.S. and Y.Y. interpreted the results. All authors critically revised the manuscript for important intellectual content.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethics approval and consent to participate
The protocol was approved by the Ethics Committee of Wuxi Center for Disease Control and Prevention (2020No10). Online informed consent was obtained from all subjects involved in the study.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2026136
References
- 1.Lutz C, Fink R, Cloud A, Stevenson J, Kim D, Fiebelkorn AJV.. Factors associated with perceptions of influenza vaccine safety and effectiveness among adults, United States, 2017-2018. Vaccine. 2020;38(6):1393–9. doi: 10.1016/j.vaccine.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Simms KT, Hanley SJB, Smith MA, Keane A, Canfell K. Impact of HPV vaccine hesitancy on cervical cancer in Japan: a modelling study. Lancet Public Health. 2020;5(4):E223–E34. doi: 10.1016/S2468-2667(20)30010-4. [DOI] [PubMed] [Google Scholar]
- 3.Schellenberg N, Crizzle A. Vaccine hesitancy among parents of preschoolers in Canada: a systematic literature review. Can J Public Health. 2020;111(4):562–84. doi: 10.17269/s41997-020-00390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rey D, Fressard L, Cortaredona S, Bocquier A, Gautier A, Peretti-Watel P, Verger P. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk-benefit balance. Eurosurveillance. 2018;23(17):30–39. doi: 10.2807/1560-7917.Es.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–64. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization . 2019. Ten threats to global health in 2019. https://www.who.int/newsroom/feature-stories/ten-threats-toglobal-health-in-2019 (accessed 18 June, 2020).
- 7.Yu W, Liu D, Zheng J, Liu Y, An Z, Rodewald L, Zhang G, Su Q, Li K, Xu D, et al. Loss of confidence in vaccines following media reports of infant deaths after hepatitis B vaccination in China. Int J Epidemiol. 2016;45(2):441–49. doi: 10.1093/ije/dyv349. [DOI] [PubMed] [Google Scholar]
- 8.Zhou M, Qu S, Zhao L, Kong N, Campy KS, Wang S. Trust collapse caused by the Changsheng vaccine crisis in China. Vaccine. 2019;37(26):3419–25. doi: 10.1016/j.vaccine.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 9.Xiao Q, Liu X, Wang R, Mao Y, Chen H, Li X, Liu X, Dai J, Gao J, Fu H, et al. Predictors of willingness to receive the COVID-19 vaccine after emergency use authorization: the role of coping appraisal. Vaccines. 2021;9(9):967. doi: 10.3390/vaccines9090967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.K A, Lu X, Wang J, Hu L, Li B, Lu Y. Association between adult vaccine hesitancy and parental acceptance of childhood COVID-19 vaccines: a web-based survey in a northwestern region in China. Vaccines. 2021;9(10):1088. doi: 10.3390/vaccines9101088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers RW. Protection motivation theory of fear appeals and attitude-change. J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 12.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 13.Rosenstock IM, Strecher VJ, Becker MH. Social-learning theory and the health belief model. Health Educ Q. 1988;15(2):175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 14.Roozbahani N, Kaviani A-H, Khorsandi M. Path analysis of skin cancer preventive behavior among the rural women based on protection motivation theory. Bmc Womens Health. 2020;20. doi: 10.1186/s12905-020-0889-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lahiri A, Jha SS, Chakraborty A, Dobe M, Dey A. Role of threat and coping appraisal in protection motivation for adoption of preventive behavior during COVID-19 pandemic. Front Public Health. 2021;9. doi: 10.3389/fpubh.2021.678566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun Y, Wang N, Guo X, Peng Z. Understanding the acceptance of mobile health services: a comparison and integration of alternative models. J Electron Commerce Res. 2013;14:183–200. [Google Scholar]
- 17.Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132(2):249–68. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 18.Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav. 2000;27(5):591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- 19.Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behavior: a meta-analytic review of protection motivation theory. J Appl Soc Psychol. 2000;30(1):106–43. doi: 10.1111/j.1559-1816.2000.tb02308.x. [DOI] [Google Scholar]
- 20.Zhang X, Liu S, Wang L, Zhang Y, Wang J. Mobile health service adoption in China integration of theory of planned behavior, protection motivation theory and personal health differences. Online Inf Rev. 2019;44(1):1–23. doi: 10.1108/OIR-11-2016-0339. [DOI] [Google Scholar]
- 21.Ling M, Kothe EJ, Mullan BA. Predicting intention to receive a seasonal influenza vaccination using protection motivation theory. Soc Sci Med. 2019;233:87–92. doi: 10.1016/j.socscimed.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Bedford H, Attwell K, Danchin M, Marshall H, Corben P, Leask J. Vaccine hesitancy, refusal and access barriers: the need for clarity in terminology. Vaccine. 2018;36(44):6556–58. doi: 10.1016/j.vaccine.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Camerini A-L, Diviani N, Fadda M, Schulz PJ. Using protection motivation theory to predict intention to adhere to official MMR vaccination recommendations in Switzerland. SSM Popul Health. 2019;7:100321. doi: 10.1016/j.ssmph.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang P-W, Ahorsu DK, Lin C-Y, Chen IH, Yen C-F, Kuo Y-J, Griffiths MD, Pakpour AH. Motivation to have COVID-19 vaccination explained using an extended protection motivation theory among university students in China: the role of information sources. Vaccines. 2021;9(4):380. doi: 10.3390/vaccines9040380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125(4):654–59. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 26.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 27.Rong H, Lai X, Ma X, Hou Z, Li S, Jing R, Zhang H, Peng Z, Feng L, Fang H, et al. Seasonal influenza vaccination and recommendation: the difference between general practitioners and public health workers in China. Vaccines. 2020;8(2):265. doi: 10.3390/vaccines8020265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Q, Xiu S, Zhao S, Wang J, Han Y, Dong S, Huang J, Cui T, Yang L, Shi N, et al. Vaccine hesitancy: COVID-19 and influenza vaccine willingness among parents in Wuxi, China—a cross-sectional study. Vaccines. 2021;9(4):342. doi: 10.3390/vaccines9040342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quinn SC, Jamison AM, An J, Hancock GR, Freimuth VS. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: results of a national survey of White and African American adults. Vaccine. 2019;37(9):1168–73. doi: 10.1016/j.vaccine.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 30.Browne MW, Cudeck R. Testing structural equation models. In: Bollen, KA, and Long, JS. Alternative ways of assessing model fit. Beverly Hills, CA: Sage. 1993:136–62. [Google Scholar]
- 31.Wang Q, Yue N, Zheng M, Wang D, Duan C, Yu X, Zhang X, Bao C, Jin H. Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: a meta-analysis. Vaccine. 2018;36(48):7262–69. doi: 10.1016/j.vaccine.2018.10.045. [DOI] [PubMed] [Google Scholar]
- 32.Wang LD-L, Lam WWT, Fielding R. Determinants of human papillomavirus vaccination uptake among adolescent girls: a theory-based longitudinal study among Hong Kong Chinese parents. Prev Med. 2017;102:24–30. doi: 10.1016/j.ypmed.2017.06.021. [DOI] [PubMed] [Google Scholar]
- 33.Durando P, Alicino C, Dini G, Barberis I, Bagnasco AM, Iudici R, Zanini M, Martini M, Toletone A, Paganino C, et al. Determinants of adherence to seasonal influenza vaccination among healthcare workers from an Italian region: results from a cross-sectional study. BMJ Open. 2016;6(5):e010779. doi: 10.1136/bmjopen-2015-010779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29(38):6472–84. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 35.Rippetoe PA, Rogers RW. Effects of components of protection-motivation theory on adaptive and maladaptive coping with a health threat. J Pers Soc Psychol. 1987;52(3):596–604. doi: 10.1037/0022-3514.52.3.596. [DOI] [PubMed] [Google Scholar]
- 36.Wang P-W, Ahorsu DK, Lin C-Y, Chen I-H, Yen C-F, Kuo Y-J, Griffiths MD, Pakpour AH. Motivation to have COVID-19 vaccination explained using an extended protection motivation theory among university students in China: the role of information sources. Vaccines. 2021;9(4):380. doi: 10.3390/vaccines9040380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. Plos Curr. 2015;7:ecurrents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289. doi: 10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liao Q, Cowling BJ, Lam WWT, Fielding R. Factors affecting intention to receive and self-reported receipt of 2009 pandemic (H1N1) vaccine in Hong Kong: a longitudinal study. Plos One. 2011;6(3):e17713 doi: 10.1371/journal.pone.0017713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ditekemena JD, Nkamba DM, Mutwadi A, Mavoko HM, Siewe Fodjo JN, Luhata C, Obimpeh M, Van Hees S, Nachega JB, Colebunders R, et al. COVID-19 vaccine acceptance in the Democratic Republic of Congo: a cross-sectional survey. Vaccines. 2021;9(2):153. doi: 10.3390/vaccines9020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hak E, Schönbeck Y, Melker HD, Essen GAV, Sanders EAM. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine. 2005;23:3103–07. [DOI] [PubMed] [Google Scholar]
- 41.Karafillakis E, Dinca I, Apfel F, Cecconi S, Wűrz A, Takacs J, Suk J, Celentano LP, Kramarz P, Larson HJ, et al. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine. 2016;34(41):5013–20. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 42.Barrière J, Vanjak D, Kriegel I, Otto J, Peyrade F, Estève M, Chamorey E. Acceptance of the 2009 A(H1N1) influenza vaccine among hospital workers in two French cancer centers. Vaccine. 2010;28(43):7030–34. doi: 10.1016/j.vaccine.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 43.Di Martino G, Di Giovanni P, Di Girolamo A, Scampoli P, Cedrone F, D’Addezio M, Meo F, Romano F, Di Sciascio MB, Staniscia T, et al. Knowledge and attitude towards vaccination among healthcare workers: a multicenter cross-sectional study in a Southern Italian Region. Vaccines. 2020;8(2):248. doi: 10.3390/vaccines8020248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Floyd DL, Prentice-Dunn S, Rogers RW. A meta-analysis of research on protection motivation theory. J Appl Soc Psychol. 2000;30(2):407–29. doi: 10.1111/j.1559-1816.2000.tb02323.x. [DOI] [Google Scholar]
- 45.K A, Lu X, Wang J, Hu L, Li B, Lu Y. Association between adult vaccine hesitancy and parental acceptance of childhood COVID-19 vaccines: a web-based survey in a northwestern region in China. Vaccines. 2021;9(10). doi: 10.3390/vaccines9101088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ren J, Wagner AL, Zheng A, Sun X, Boulton ML, Huang Z, Zikmund-Fisher BJ. The demographics of vaccine hesitancy in Shanghai, China. Plos One. 2018;13(12):e0209117. doi: 10.1371/journal.pone.0209117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu AC, Wisler-Sher DJ, Griswold K, Colson E, Shapiro ED, Holmboe ES, Benin AL. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern Child Health J. 2008;12(6):766–73. doi: 10.1007/s10995-007-0302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


