ABSTRACT
Since 2018, Spanish National Immunization Guidelines include vaccination recommendations for adults ≥65 years. To determine whether health-care professionals and the ≥65 years target group value the need for these recommendations, a cross-sectional study was conducted to capture and describe their knowledge, attitudes, beliefs and behaviors about vaccination. Online surveys were administered to representative groups of general practitioners (GPs), primary care nurses and adults ≥65 years from six major cities (and surrounding rural areas) in Spain. Main topics were attitudes and awareness of vaccines, perceptions about vaccination in adults ≥65 years, and impact of the COVID-19 pandemic on vaccination uptake. A total of 286 health-care professionals (185 GPs, 101 nurses) and 400 adults aged ≥65 years participated in the survey. GP and nurse groups agreed strongly about the importance of influenza and pneumococcal vaccination in the target population. Longer patient visit times were identified as a key factor toward promoting vaccination. The ≥65 years sample group, especially those ≥75+ years and/or with chronic diseases, was reasonably positive about the effectiveness and benefits of vaccines. Lower vaccination rates for the pneumococcal than influenza vaccine (29% vs. 80%) in the ≥65 years sample group suggest that efforts are needed to improve pneumococcal vaccine uptake. Aligning with other published works, GPs have a key role in promoting vaccination in the target population. The COVID-19 pandemic appears to have heightened awareness about the importance of vaccination among health-care professionals and adults ≥65 years.
KEYWORDS: Influenza vaccines, pneumococcal vaccines, adult vaccination, attitudes toward vaccination, healthy aging
Introduction
Immunization in older adults is an important component of preventive health-care services that aim to prevent infectious diseases such as influenza and pneumococcal disease (e.g. pneumonia, otitis, sinusitis).1 Adult vaccination has been shown to decrease the morbidity and mortality associated with preventable infectious diseases, and reduce complications and hospitalizations including intensive care unit admissions.2 Although immunization in children is well established in most countries, coverage rates for routine adult vaccinations remain low.3,4
As many of the functional and immunological changes associated with aging are responsible for an increased incidence and severity of infectious diseases in the elderly (≥65 years),5 there is a clear need for targeted preventative measures in this growing sector of the population.6 In 2018, as part of an overall strategy to prevent morbidity and mortality and promote healthy aging,7 the Spanish Ministry of Health’s National Immunization Guidelines included for the first time recommendations for adults aged ≥65 years,8 effectively extending the vaccination schedule ‘for life.’8 Despite this initiative, vaccination coverage rates in Spain for adults ≥65 years remain below the European Union’s target of 75% for the influenza vaccine,9,10 and are even lower for the pneumococcal vaccine.11
Research shows that most adults believe vaccines are important and that a recommendation from their treating healthcare professional is the strongest predictor of adult vaccine uptake.12–16 However, knowledge and attitudes toward adult vaccination among healthcare professionals are heterogeneous and not always optimal, often confusing the patient vaccination decision.17–20 Reasons for suboptimal vaccination uptake by the ≥65 years target group include a fear of adverse effects or associated illness from the vaccine, inconvenience (access, cost), a lack of awareness of the need for vaccination, and a low perception of risk for vaccine-preventable diseases.21,22 Vaccine hesitancy, which refers to the continuum between vaccine acceptance and vaccine refusal, recognizes the importance of the doctor-patient relationship among the many strategies required to address this complex issue.23–26
We conducted a cross-sectional survey study, to our knowledge the first of its kind in Spain or other European country, to evaluate and describe the knowledge, attitudes, beliefs and barriers of healthcare professionals and adults ≥65 years about vaccination for influenza and pneumococcal disease and the potential risks associated with being unvaccinated. Secondary objectives were to evaluate the possible demand by health professionals for training and information in this area; to estimate the amount of time health professionals dedicate to prevention activities; and to assess the impact of the COVID-19 pandemic on engagement with vaccination among healthcare professionals and adults ≥65 years.
Methods
Inclusion/Exclusion criteria
ADult Vaccination drIverS and barriErs (ADVISE) is a cross sectional survey-based study that was conducted from September-December 2020 and involved representative groups of healthcare professionals (general practitioners [GPs] and nurses) and adults aged ≥65 years. GPs and nurses were recruited through a panel of healthcare professionals affiliated with the MSD-approved external vendor, GfK (Growth from Knowledge), a market research and analytics company. Adults ≥65 years were recruited randomly on the streets by the vendor.
Eligible for participation in the survey were: GPs and nurses working at primary care centers in six main cities of Spain (Madrid, Barcelona, Sevilla, Bilbao, Valencia, A Coruña) or surrounding rural areas (<10,000 inhabitants); individuals in the general population ≥65 years of age residing in these same six cities or surrounding rural areas. Excluded were: healthcare professionals in a specialty other than primary care or general practice; nurses employed in settings such as hospitals or intensive care units and those involved with pediatric populations; individuals in the general population ≥65 years of age who had been resident in Spain for less than 5 years.
Survey design
Online surveys were conducted in Spanish language (one per representative group: GPs and nurses; adults ≥65 years). Healthcare professional surveys were performed using computer-assisted web interviewing (CAWI) methodology and a telephone support internet surveying technique in which the interviewer follows a script provided in a website. Questionnaires for GPs and nurses were identical in content (Supplementary File 1). Surveys of adults aged ≥65 years were performed using computer-assisted personal interviewing (CAPI) methodology, a face-to-face data collection method in which the interviewer reads questions displayed on an electronic device and enters the respondent’s answers directly into the computer. This methodology was chosen because internet access for persons aged ≥65 years was considered insufficient to provide an adequate sample of the population. The questionnaire for adults aged ≥65 years is provided in Supplementary File 2. Surveys lasted a maximum of 20 minutes.
The questionnaires were developed by a Scientific Committee coordinated by MSD Spain, based on the literature and adapted to the study objectives. After confirming eligibility for participation, survey questions related mainly to attitudes and awareness of vaccines and of vaccination in adults ≥65 years, and the impact of the COVID-19 pandemic on vaccination. To assure that questions were appropriate and understandable and that the language was interpreted as intended, prior to utilizing the questionnaire in the main study, it was pilot tested by the Scientific Committee integrated by Esther Redondo and Antoni Trilla as scientific leaders; by Manuel Cotarelo and Almudena Jaramillo from MSD primarily; and by a small trusted group of healthcare professionals and adults ≥65 years secondarily. Comments, changes and suggestions were included in the survey during the pilot testing phase.
To ensure that samples were representative of healthcare providers and the general population ≥65 years in Spain, different quotas were established. The estimated total sample size was 680 subjects, which was to involve 180 online interviews with GPs (± 7.3% sampling error with a confidence level of 95%), 100 online interviews with nurses (± 9.8% sampling error with a confidence level of 95%), and 400 face-to-face interviews with members of the general population aged ≥65 years (± 4.9% sampling error with a confidence level of 95%) who were stratified into age groups: 65–74 years and 75+ years. To assure that sample groups of healthcare professionals and adults ≥65 years were representative of Spanish geography, quotas were established by considering the population distribution of persons aged ≥65 years in each of the six cities and corresponding rural areas selected for participation in the study.
Statistical analyses
Two main types of results were obtained from the survey, either the average level of agreement with a statement expressed on a 0–10 scale (x/10) or the percentage of participants who selected a specific response (%).
Independent descriptive analyses were performed for each participating group, and compared for suitable content. For healthcare professionals, data are reported for the group as a whole and per GP and nurse subgroups. For the ≥65 years sample group, data are reported for the group as a whole and per gender, age range (65–74 years and 75+ years), and presence/absence of chronic diseases. No statistical hypotheses tests were conducted given the exploratory nature of the study and descriptive objectives.
Ethical considerations
The study protocol was approved by the Ethical Committee for Clinical Research of the Hospital Clínic de Barcelona. MSD sponsored the study and participated in data and manuscript review, but had no influence with regard to subject participation or data acquisition, handling and analysis. All participants were informed about their legal rights according to Spanish regulations. All participants were informed about MSD’s sponsorship and were required to provide informed consent before answering any survey questions. This consent was reviewed and approved by the Ethical Committee for Clinical Research together with all regulatory aspects of the study.
Results
Characteristics of the representative groups
The representative group of healthcare professionals consisted of 185 GPs and 101 nurses (n = 286). This group was 58% female (n = 166) and 91% (n = 261) of participants had ≥10 years’ clinical experience. The representative group of adults ≥65 years consisted of 400 participants. This group was 59% female, approximately evenly distributed by age (65–74 years: 48%; 75+ years: 52%), and about two-thirds of the sample (68%; n = 271) had chronic diseases, most commonly heart disease/hypertension/high cholesterol. The distribution of representative groups by city (and surrounding rural area) was proportionate (Table 1).
Table 1.
Area of residence for representative groups of healthcare professionals and adults ≥65 years
| Location | GPs (n = 185) | Nurses (n = 101) | Adults ≥65 years (n = 400) |
|---|---|---|---|
| Madrid | 69 (37.3%) | 37 (36.6%) | 151 (37.8%) |
| Barcelona | 48 (25.9%) | 25 (24.8%) | 97 (24.3%) |
| Valencia | 25 (13.5%) | 14 (13.9%) | 54 (13.5%) |
| Vizcaya | 11 (5.9%) | 7 (6.9%) | 27 (6.8%) |
| Sevilla | 17 (9.2%) | 10 (9.9%) | 38 (9.5%) |
| A Coruña | 15 (8.1%) | 8 (7.9%) | 33 (8.3%) |
GPs, general practitioners.
Results are presented according to respective surveys (healthcare professionals and adults ≥65 years) and main topics within the respective surveys.
Healthcare professionals survey results
What is the attitude of healthcare professionals toward vaccines and what is their commitment to vaccination programs?
The majority of representative GPs and nurses (78% and 85%, respectively) reported having received the influenza vaccine within the past year/influenza campaign. A large proportion of GPs (70%) and nurses (74%) reported having never received a pneumococcal vaccine. [Note: Influenza vaccination is recommended for all healthcare professionals in Spain, but there is no specific corresponding recommendation for the pneumococcal vaccine].
The attitudes of participating GPs and nurses toward vaccines in general are shown in Figure 1. There was strong agreement from both groups about the importance of vaccination for public health and about the need to be informed and up to date about vaccination. Relative to GPs, nurses reported being more personally involved with vaccination in terms of recommending and informing patients, had a more favorable perception about the safety and efficacy of vaccines, and were more actively engaged with patients about vaccines. There was less certainty among GP and nurse groups about the equal importance of vaccination for all age groups.
Figure 1.
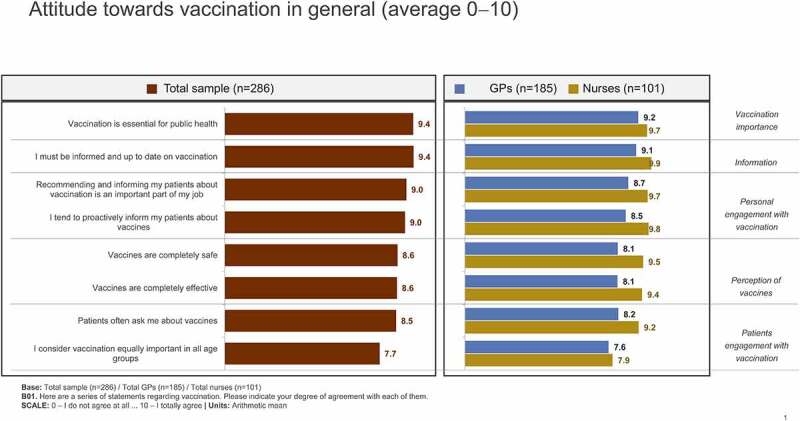
Attitudes of surveyed healthcare professionals toward vaccination in general. Scale: 0 – I do not agree at all … 10 – I totally agree.
Participating GP and nurse groups agreed strongly about the importance of vaccination in adults ≥65 years (9.3/10 and 9.9/10, respectively) and most reported recommending the influenza (9.5/10 and 9.9/10) and pneumococcal (9.2/10 and 9.8/10) vaccine to this target population. GPs rated themselves somewhat less able than nurses to inform patients about the influenza (8.9/10 and 9.9/10) and pneumococcal (8.6/10 and 9.8/10) vaccines.
What is the attitude of healthcare professionals toward influenza/pneumococcal vaccines specifically?
The attitudes of participating GP and nurse groups toward influenza and pneumococcal vaccination in adults ≥65 years are shown in Figure 2. Both groups agreed strongly about the importance of influenza and pneumococcal vaccination in this target population, and reported proactively informing adults ≥65 years about these vaccines, although less so among GPs for the pneumococcal vaccine. Both groups indicated that interest in vaccines, general informedness about vaccines and their importance, access to sufficient information about vaccines, and awareness of the risk of contracting influenza/pneumococcal disease in adults ≥65 years was greater for the influenza than pneumococcal vaccine.
Figure 2.
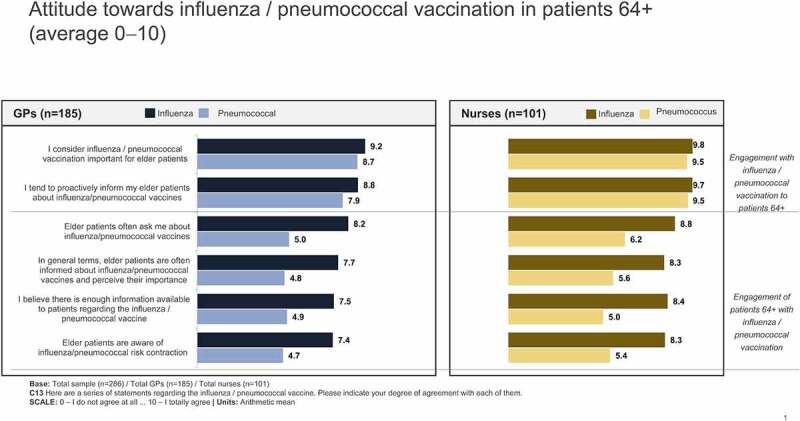
Attitudes of surveyed healthcare professionals toward influenza/pneumococcal vaccination in the ≥65 years target population. Scale: 0 – I do not agree at all … 10 – I totally agree.
How much time do healthcare professionals spend on vaccination? What is needed to further promote vaccination?
Representative GPs reported spending less percentage of their consultation time than nurses on recommending or informing patients about vaccination in general (14% vs. 51%). With regard to specific vaccine type, each group reported spending about twice as much consultation time recommending or informing patients about the influenza vaccine (54% and 65%, respectively) than the pneumococcal vaccine (25% and 30%).
A considerable proportion of representative GPs (62%) and nurses (72%) reported that workload prevents them from dedicating as much time as desirable to preventative tasks such as vaccination. Both groups considered that key measures to further promote vaccination would include having more time to spend with patients per visit (46% of GPs and 38% of nurses selected this response) and having more time to spend informing patients about the benefits of vaccination (33% and 43%), ahead of measures such as increasing the time spent on vaccination training (8% and 8%) or arranging specific consultations with patients about vaccination (11% and 9%).
Representative GP and nurse groups each reported spending an equal amount of time on prevention, recommendation and treatment measures (approximately 1/3 of the time per task) with both the influenza and pneumococcal vaccines. Nearly twice as many nurses as GPs (56% vs. 29%) considered vaccination to be the priority preventive activity in primary care.
Do healthcare professionals consider themselves well informed about vaccines? What are their main sources of information?
There was considerable agreement from participating GPs and nurses about the need to stay informed and up to date with adult vaccination (9.1/10 and 9.9/10, respectively). Both groups, but particularly nurses, considered themselves to be well informed about the influenza (9.2/10 and 10.0) and pneumococcal (8.9/10 and 9.9/10) vaccines in adults ≥65 years. Nurses reported more practical involvement with vaccination schedules than GPs, and GPs rated themselves less informed than nurses about the regional vaccination schedule for adults ≥65 years as, in their view, the information is not easy to obtain.
Representative GP and nurse groups considered it necessary for health professionals to receive more training about vaccination in adults ≥65 years. GPs expressed interest in receiving training through a range of internal and external information sources, whereas nurses expressed a preference to receive training through attendance at congresses, seminars or training activities of scientific societies (Figure 3).
Figure 3.
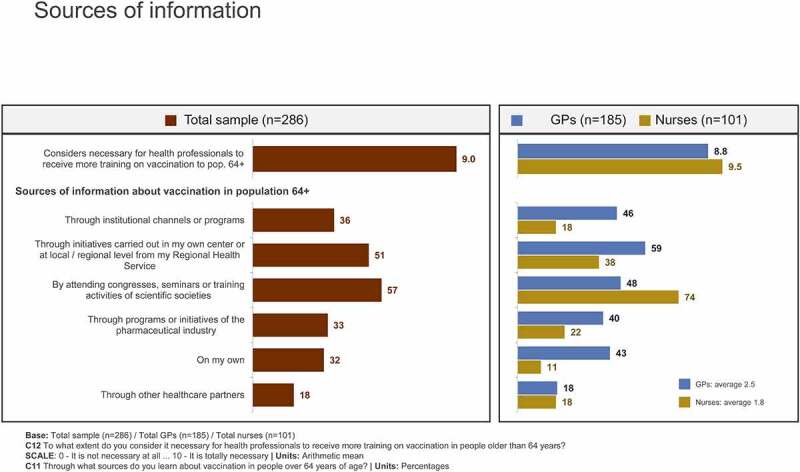
Preferred information sources of surveyed healthcare professionals for additional training about vaccination in the ≥65 years target population. Percent (%) of sample who selected response; multiple answers were possible. Scale: 0 – It is not necessary at all … 10 – It is totally necessary.
How is the COVID-19 pandemic affecting vaccination? Is it eliciting any kind of reaction from healthcare professionals?
With respect to the COVID-19 pandemic, representative GP and nurse groups reported greater engagement with vaccination by adults ≥65 years, in terms of fielding more enquiries from patients and by patients being better informed. The COVID-19 pandemic appears to have heightened GPs’ personal engagement with vaccination in adults ≥65 years, especially as regards the need to prioritize vaccination as a preventive activity, increase awareness about the importance of vaccination, and receive additional training about vaccination in the target population (Figure 4).
Figure 4.
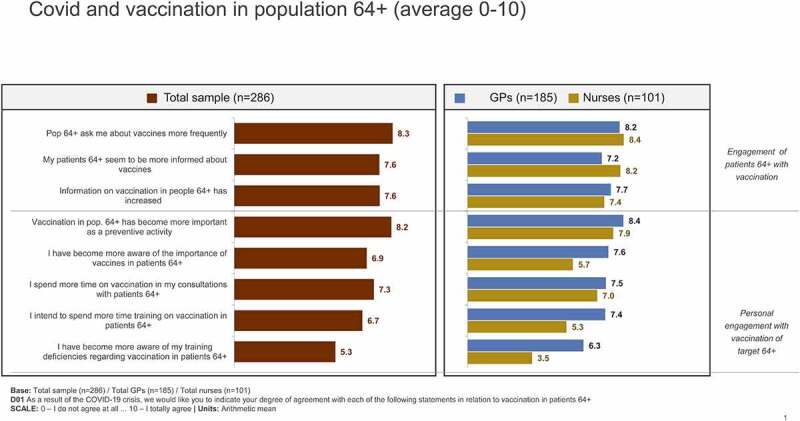
Impact of the COVID-19 pandemic on engagement of surveyed health professionals with vaccination in the ≥65 years target population. Scale: 0 – I do not agree at all … 10 – I totally agree.
Participating GP and especially nurse groups reported being aware of the World Health Organization’s recommendation, in the context of COVID-19, to vaccinate older adults and those with chronic diseases against influenza and pneumococcal disease (8.6/10 and 9.6/10, respectively). Both groups appeared to be reasonably aware that, in the context of COVID-19, the pneumococcal vaccine can prevent bacterial infections and reduce unnecessary use of antibiotics (8.7/10 and 8.3/10).
Adults ≥65 years survey results
How much knowledge does the ≥65 years target group have about vaccines and what is their level of engagement with vaccination programs?
The representative group of adults ≥65 years reported a high level of awareness of the existence of adult vaccines (9.2/10). A third of the group (32%) indicated awareness of their own vaccination schedule, whereas another third (35%) indicated being aware of their own vaccination schedule only when directed by a doctor or nurse.
What is the attitude of the ≥65 years target group toward vaccines in general?
The attitude of the representative ≥65 years target group toward vaccines was reasonably positive, with agreement scores ranging from 7.1/10 to 7.7/10 for a series of statements about the attributes of vaccines. Agreement scores tended higher in the 75+ years and chronic diseases subgroups (Figure 5). The group as a whole expressed reasonable confidence about vaccine efficacy and the importance of vaccination to prevent diseases personally and to protect society. Only about half the group indicated that they usually ask their family doctor or nurse about vaccination, suggesting a considerable level of passivity in their overall approach to vaccination.
Figure 5.
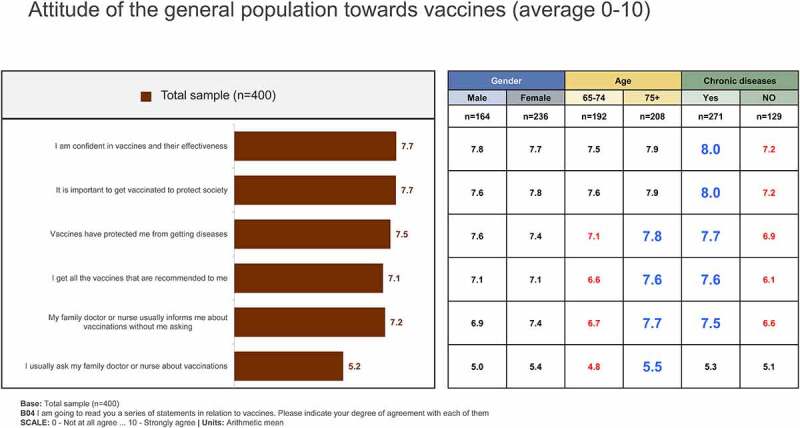
Attitudes of the ≥65 years sample group toward vaccines/vaccinations. Scale: 0 – Not at all agree … 10 – Strongly agree.
What leads the ≥65 years target group to get vaccinated? And to refuse vaccination?
A recommendation by a GP and perception of an age-related risk of acquiring certain diseases were the main drivers of vaccination as reported by the representative ≥65 years sample group, especially in the 75+ years and chronic diseases subgroups. Assuming that no reasons in favor of vaccination were selected among the available choices, 18% of the group indicated that they ‘never get vaccinated’ (Figure 6). Main reasons identified for refusing vaccination were a low perception of risk due to good health, a lack of confidence in the ability of vaccination to protect against diseases, and a general distrust of vaccines and fear of possible associated side effects. Assuming that no reasons to refuse vaccination were selected among the available choices, 71% of the group reported that they ‘always get vaccinated.’
Figure 6.
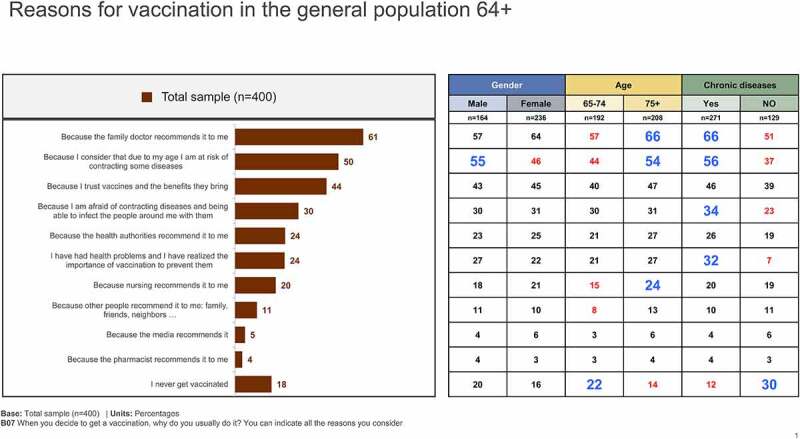
Reasons for getting vaccinated in the ≥65 years sample group. Percent (%) of sample who selected response; multiple answers were possible.
What is the level of awareness and concern about influenza and pneumococcal diseases in the ≥65 years target group?
Almost all participants (~100%) in the ≥65 years sample group reported being aware of influenza. The average level of concern about influenza was 7.2/10 in the overall group, and somewhat greater in the 75+ years (7.5/10) and chronic diseases (7.5/10) subgroups. The seriousness of influenza was rated 7.6/10 overall, more so in the 75+ years (8.0/10) and chronic diseases (7.8/10) subgroups. A smaller proportion (77%) of the ≥65 years sample group reported being aware of pneumococcal disease, whereas levels of concern about pneumococcal diseases (7.8/10 in the overall group; 8.1/10 in the chronic diseases subgroup) and their perceived seriousness (8.6/10 and 8.9/10, respectively) were greater than those for influenza.
Awareness of the influenza vaccine was almost twice that of the pneumococcal vaccine in the representative ≥65 years target group (98% vs. 54%), and was reflected in reported vaccination rates (80% vs. 29%). GPs were identified as the main driver of influenza vaccination (63%), ahead of nurses (16%). Less than a third of the ≥65 years sample group (29%) reported controlling their own influenza vaccination schedule. Among the 118 individuals (29% of the group) who reported having received the pneumococcal vaccine, the main driver was a recommendation by a GP (78%) or nurse (21%); patients’ own initiative to receive the pneumococcal vaccine was low (6%).
Who are the main prescribers of vaccines to the ≥65 years target group?
The representative ≥65 years target group identified primary care centers (influenza: 82%; pneumococcus: 86%), ahead of public hospitals (influenza: 7%; pneumococcus: 7%), or private sector clinics (influenza: 5%; pneumococcus: 4%) as the main vaccination sites. GPs (in particular) and nurses were key figures identified by the group in relation to vaccination, ahead of health authorities/information campaigns, pharmacists and nonprofessional sources such as family, friends or media (Figure 7). Participants aged 75+ years and those with chronic diseases were particularly receptive to receiving vaccine recommendations from professional sources.
Figure 7.
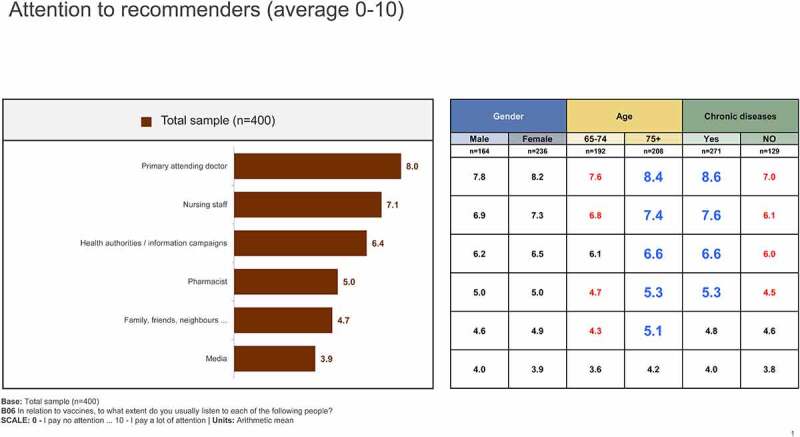
Most relevant recommenders of vaccination in the ≥65 years sample group. Scale: 0 – I pay no attention … 10 – I pay a lot of attention.
Participants’ recall of having received a vaccination recommendation was greater for the influenza than pneumococcal vaccine (80% vs. 33%), possibly reflecting different awareness levels of these vaccines in the target population.
How is the COVID-19 pandemic affecting vaccination? Is it triggering any kind of reaction in the ≥65 years target group?
There was general agreement in the representative ≥65 years target group, especially among those aged 75+ years, that the COVID-19 pandemic has increased their awareness of the role that vaccination plays to protect society (7.8/10) and of the importance of vaccination (7.2/10). Agreement was low (3.3/10) as to whether the COVID-19 pandemic had dissuaded them from getting vaccinated because of having to attend a primary care center.
Discussion
This survey study was undertaken to better understand whether healthcare professionals working in primary care and the target group of adults ≥65 years in Spain value the need for routine influenza and pneumococcal vaccinations. We also explored the impact of vaccination on daily workflow, the need for more education about vaccination, and the impact of the COVID-19 pandemic on vaccination behavior.
A major finding of the healthcare professionals’ survey was the strong belief by participating GPs and nurses about the importance of influenza and pneumococcal vaccination for adults ≥65 years, mirroring the results of other survey studies exploring attitudes of primary care professionals to older adult vaccination.27–30 We found that nurses were generally more comfortable than GPs about vaccination in adults ≥65 years, likely reflecting their greater involvement with vaccination activities in the primary care setting. Both groups indicated an openness to receiving more information about vaccination for the target group. Both groups identified workload burden as the main obstacle to dedicating more time to preventive activities such as vaccination, with longer patient visit times regarded as a key factor to promote vaccination. The COVID-19 pandemic appears to have increased GPs’ sensitivity in particular about the need for vaccination programs in the target population and the need for additional training.
The ≥65 years sample group, particularly those aged 75+ years and/or with chronic diseases, was reasonably positive about the effectiveness of vaccines and associated benefit to personal and societal health. However, about one in five respondents indicated that they ‘never get vaccinated,’ more so those aged 65–74 years and/or without chronic diseases. This crude estimate of vaccine refusal rates was verified to some extent by the proportion of participants who reported that they ‘always get vaccinated’ (71%). Confidence in vaccination recommendations from a GP and concerns about an age-related increased risk of contracting infectious diseases were identified by the sample group as the main drivers of vaccination. Vaccine refusers justified their decision based on a low perception of risk (considered themselves healthy), a lack of confidence in vaccine protection, and a fear of adverse events. These results align closely with a recent general population-based survey from Hong Kong which found that high levels of perceived susceptibility to infection (adjusted odds ratio [AOR] 3.6; 95% confidence interval [CI] 2.3–5.7, p < .001) and high levels of perceived benefits of vaccination (AOR 1.7; 95% CI 1.1–2.5; p < .001) were independent factors associated with an intention of older adults to participate in a pneumococcal vaccination program.31 The marked difference in pneumococcal and influenza vaccination rates (29% vs. 80%) in the ≥65 years sample group emphasize the need to increase awareness of the pneumococcal vaccine and the potentially serious consequences of pneumococcal diseases in older adults. Similar to surveyed healthcare professionals, the COVID-19 context appears to have increased awareness of the role and importance of vaccines for public health among participating adults ≥65 years.
A comparison of our work with a sample of cross-sectional studies conducted in other world regions highlights striking similarities, especially as regards the importance of vaccine awareness and the provider-patient relationship in vaccination uptake. In a Canadian survey of adults ≥65 years (n = 863), factors strongly associated with pneumococcal vaccine receipt among responders (58%) were ‘having heard of the vaccine’ (AOR 10.1; 95% CI 4.7–21.7) and ‘being offered the vaccine by a healthcare provider’ (AOR 23.4; 95% CI 13.4–40.7).32 Another Canadian group exploring attitudes toward vaccines found that about 60% of adult participants (n = 4023) reported a willingness to be vaccinated if recommended by their healthcare provider.33 Investigators examining PPV23 vaccine uptake at a family medicine clinic in rural Japan identified significant associations between vaccine receipt and vaccine awareness (odds ratio [OR] 8.5; 95% CI 2.1–35.0), physician’s recommendation for vaccination (OR 8.5; 95% CI 2.8–26.0), and perceived vaccine effectiveness (OR 4.1; 95% CI 1.2–13.9).34 Other Japanese investigators reported that influenza and pneumococcal vaccine uptake among patients ≥65 years was positively associated with patients’ primary care experience.35 Factors influencing vaccination decisions (influenza, pneumococcal, herpes zoster vaccines) among Turkish patients ≥65 years (n = 326) attending family medicine clinics were a recommendation by a physician and being informed about the vaccine by a doctor or nurse.36 A recent systematic review of factors influencing vaccine acceptability among Canadians identified a perceived need or importance of vaccination, protection of self and others, and recommendation by a healthcare provider as influential factors for acceptability of adult vaccines in high-risk groups.37
Taken together, our findings and those of other survey studies suggest that attitudes toward older adult vaccination are largely positive, although with scope for improvement. As the most trusted source of vaccination recommendations, GPs are in a unique position to address systemic barriers to vaccination in primary practice. Allowing for longer patient consult times and further expanding the role of primary care nurses in vaccination activities may facilitate outreach to a greater proportion of the target population. Public health interventions, such as awareness campaigns about the pneumococcal vaccine in particular, are likely to complement primary care strategies to increase vaccine uptake in the ≥65 years target population. An interesting analysis of publicly available data from four ‘benchmark’ countries with high influenza vaccine coverage rates in adults ≥65 years identified 42 key policy and programmatic factors which were clustered into five ‘pillars’ of success for a vaccination program: health authority accountability, facilitated access to vaccination, healthcare professional accountability, awareness of influenza burden and disease severity, and belief in influenza vaccination benefits.38 Although the analysis was specific to influenza vaccination, most components have universal application and can be selected and combined in myriad ways to develop a tailored approach to improving vaccine coverage rates in any given country or jurisdiction.
Limitations
The limitations of the ADVISE study include, most notably, a potential response bias if respondents self-selected for participation based on motivation and/or interest in vaccination. Since the focus of the study was on the ≥65 years target population, no corresponding data were collected about attitudes, beliefs, drivers and barriers toward vaccination in adults 18–64 years. Likewise, because the focus was on vaccination activities among healthcare professionals in primary care, no corresponding data were collected from other specialties which may promote older adult vaccination such as geriatrics, preventive medicine, pneumology, and endocrinology. We acknowledge that sample groups in terms of participant numbers and geographical location may not be wholly representative of other regions of Spain. Although survey questionnaires were pilot tested prior to their use in the main study, it is possible that questions were not the most relevant or appropriate or were not always interpreted correctly. We further acknowledge that responses may have been influenced to some degree by the timing of the survey during the COVID pandemic, which has increased awareness of the importance of vaccination in general, especially among higher-risk groups.
Conclusions
Despite the lower attention that immunization receives in adults compared with children, surveyed primary care professionals were highly aware and strongly positive about the needs and benefits of vaccination in the target population aged ≥65 years. Practice changes that allow for more time per patient visit and undertaking specific training about vaccination in older adults are some measures that primary care providers could consider to improve vaccine uptake and, in turn, contribute to healthy aging. The ≥65 years sample group, particularly those most vulnerable (aged ≥75 years and/or with chronic diseases), were also positive about adult vaccination and its benefits, although more work is needed to lift vaccination coverage rates to recommended levels in this target group. As GP recommendations are the main driver of vaccination in older adults, efforts aimed at enhancing GP engagement with vaccine initiatives may be beneficial. Importantly, stronger efforts are required to increase awareness of the risks associated with pneumococcal disease and of the health benefits of preventing pneumococcal disease through vaccination.
Supplementary Material
Acknowledgments
Editorial assistance was provided by Kerry Dechant, ISMPP CMPP™ on behalf of Content Ed Net (Madrid, Spain), with funding from MSD Spain (Madrid, Spain).
Funding Statement
The ADVISE study was sponsored and funded by MSD Spain [VEAP ID: 9022.
Disclosure statement
Antoni Trilla has received fees as consultor or/and speaker from GlaxoSmithKline, MSD and Roche. Esther Redondo has received fees as consultant/advisor or/and speaker, as well as grants to assist with conferences or courses by GlaxoSmithKline, MSD, Pfizer, and Sanofi Pasteur MSD. Almudena Jaramillo López-Herce, and Manuel Cotarelo Suárez are employees of MSD Spain. Ignacio L.B. Munguira was in a Scholarship Program with MSD Spain.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2021.2025007
References
- 1.Centers for Disease Control and Prevention (CDC) . Adult vaccination. What vaccines are recommended for you. 2019. Nov 21. [accessed 2021 Jun 2]. https://www.cdc.gov/vaccines/adults/rec-vac/index.html.
- 2.Arriola C, Garg S, Anderson EJ, Ryan PA, George A, Zansky SM, Bennett N, Reingold A, Bargsten M, Miller L, et al. Influenza vaccination modifies disease severity among community-dwelling adults hospitalized with influenza. Clin Infect Dis. 2017;65(8):1289–10. doi: 10.1093/cid/cix468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams WW, Lu P, O’Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, et al. Surveillance of vaccination coverage among adult populations — United States, 2015. MMWR Surveill Summ. 2017;66(No. SS–11):1–28. doi: 10.15585/mmwr.ss6611a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter P, Fryhofer SA, Szilagyi PG.. Vaccination of adults in general medical practice. Mayo Clin Proc. 2020;95(1):169–83. doi: 10.1016/j.mayocp.2019.02.024. [DOI] [PubMed] [Google Scholar]
- 5.Htwe TH, Mushtaq A, Robinson SB, Rosher RB, Khardori N. Infection in the elderly. Infect Disease Clin North Am. 2007;21(3):711–43. doi: 10.1016/j.idc.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Eurostat . Ageing Europe. Looking at the lives of older people in the EU. 2019 ed. Luxembourg: Publications Office of the European Union; 2019. [accessed 2021 Jun 2]. https://ec.europa.eu/eurostat/statistics-explained/index.php/Ageing_Europe_-_looking_at_the_lives_of_older_people_in_the_EU. [Google Scholar]
- 7.Esposito S, Principi N, Rezza G, Bonanni P, Gavazzi G, Beyer I, Sulzner M, Celentano LP, Prymula R, Rappagliosi A, et al. Vaccination of 50+ adults to promote healthy ageing in Europe: the way forward. Vaccine. 2018;36(39):5819–24. doi: 10.1016/j.vaccine.2018.08.041. [DOI] [PubMed] [Google Scholar]
- 8.Ministerio de Sanidad, Consumo y Bienestar Social, Gobierno de España. [accessed 2021. Jun 2]. https://www.mscbs.gob.es/estadEstudios/estadisticas/inforRecopilaciones/barometro/home.htm.
- 9.European Centre for Disease Prevention and Control . Seasonal influenza vaccination and antiviral use in EU/EEA Member States – overview of vaccine recommendations for 2017–2018 and vaccination coverage rates for 2015–2016 and 2016–2017 influenza seasons. Stockholm: ECDC; 2018. [accessed 2021 Sept 2]. https://www.ecdc.europa.eu/sites/default/files/documents/seasonal-influenza-antiviral-use-2018.pdf. [Google Scholar]
- 10.OECD.org . Influenza vaccination rates. Total, % of population aged 65+, 2019 or latest available. [accessed 2021. Jun 2]. https://data.oecd.org/healthcare/influenza-vaccination-rates.htm.
- 11.Ochoa-Gondar O, Vila-Córcoles Á, de Diego C, Satué E, Vila-Rovira A, Aragón M. Vacunación antineumocócica en adultos de Cataluña: coberturas y grado de adecuación a distintas guías de recomendaciones [Antipneumococcal vaccination in Catalonian adults: vaccine coverages and adequacy to distinct guideline recommendations]. Aten Primaria. 2018;50(9):553–59. Spanish. doi: 10.1016/j.aprim.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ames HM, Glenton C, Lewin S. Parents’ and informal caregivers’ views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database Syst Rev. 2017;2(2):CD011787. doi: 10.1002/14651858.CD011787.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stefanoff P, Mamelund SE, Robinson M, Netterlid E, Tuells J, Bergsaker MA, Heijbel H, Yarwood J. Tracking parental attitudes on vaccination across European countries: the Vaccine Safety, Attitudes, Training and Communication Project (VACSATC). Vaccine. 2010;28(35):5731–37. doi: 10.1016/j.vaccine.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 14.European Centre for Disease Prevention and Control . Communication on immunization, vaccine-preventable diseases. [accessed 2021. Sept 2]. https://www.ecdc.europa.eu/en/immunisation-vaccines/communication-on-immunisation.
- 15.Simone B, Carrillo-Santisteve P, Lopalco PL. Healthcare workers role in keeping MMR vaccination uptake high in Europe: a review of evidence. Euro Surveill. 2012;17(26):20206. doi: 10.2807/ese.17.26.20206-en. [DOI] [PubMed] [Google Scholar]
- 16.European Commission . State of health in the EU: companion report 2019. [accessed 2021. May 26]. https://www.digitalhealthnews.eu/download/publications/6014-state-of-health-in-the-eu-companion-report-2019.
- 17.European Centre for Disease Prevention and Control . Communication on immunisation – building trust. Stockholm: ECDC; 2012. [accessed 2021 Sept 2]. https://www.ecdc.europa.eu/sites/default/files/media/en/publications/Publications/TER-Immunisation-and-trust.pdf. [Google Scholar]
- 18.Peretti-Watel P, Raude J, Sagaon-Teyssier L, Constant A, Verger P, Beck F. Attitudes toward vaccination and the H1N1 vaccine: poor people’s unfounded fears or legitimate concerns of the elite? Soc Sci Med. 2014;109:10–18. doi: 10.1016/j.socscimed.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 19.Esteban-Vasallo MD, López de Andrés A, Bayón M, Aréjula JL, Jiménez-García R. Adequacy of information provided by healthcare professionals on vaccines: results of a population survey in Spain. Patient Educ Couns. 2018;101(7):1240–47. doi: 10.1016/j.pec.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Glenton C, Carlsen B, Lewin S, Wennekes MD, Winje BA, Eilers R. Healthcare workers’ perceptions and experiences of communicating with people over 50 years of age about vaccination: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2021;7:CD013706. doi: 10.1002/14651858.CD013706.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Portero de La Cruz S, Cebrino J. Trends, coverage and influencing determinants of influenza vaccination in the elderly: a population-based national survey in Spain (2006-2017). Vaccines (Basel). 2020;8(2):327. doi: 10.3390/vaccines8020327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doherty M, Schmidt-Ott R, Santos JI, Stanberry LR, Hofstetter AM, Rosenthal SL, Cunningham AL. Vaccination of special populations: protecting the vulnerable. Vaccine. 2016;34(52):6681–90. doi: 10.1016/j.vaccine.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 23.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 24.Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF Joint Reporting Form data-2015-2017. Vaccine. 2018;36(26):3861–67. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dudley MZ, Privor-Dumm L, Dubé È, MacDonald NE. Words matter: vaccine hesitancy, vaccine demand, vaccine confidence, herd immunity and mandatory vaccination. Vaccine. 2020;38(4):709–11. doi: 10.1016/j.vaccine.2019.11.056. [DOI] [PubMed] [Google Scholar]
- 26.Braun C, O’Leary ST. Recent advances in addressing vaccine hesitancy. Curr Opin Pediatr. 2020;32(4):601–09. doi: 10.1097/MOP.0000000000000929. [DOI] [PubMed] [Google Scholar]
- 27.Pavia M, Foresta MR, Carbone V, Angelillo IF. Influenza and pneumococcal immunization in the elderly: knowledge, attitudes, and practices among general practitioners in Italy. Public Health. 2003;117(3):202–07. doi: 10.1016/s0033-3506(03)00066-0. [DOI] [PubMed] [Google Scholar]
- 28.Romani MH, Musharrafieh UM, Lakkis NA, Hamadeh GN. Family physicians beliefs and attitudes regarding adult pneumococcal and influenza immunization in Lebanon. Fam Pract. 2011;28(6):632–37. doi: 10.1093/fampra/cmr038. [DOI] [PubMed] [Google Scholar]
- 29.Hurley LP, Bridges CB, Harpaz R, Allison MA, O’ Leary ST, Crane LA, Brtnikova M, Stokley S, Beaty BL, Jimenez-Zambrano A. Physician attitudes toward adult vaccines and other preventive practices, United States, 2012. Public Health Rep. 2016;131(2):320–30. doi: 10.1177/003335491613100216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vezzosi L, Riccò M, Agozzino E, Odone A, Signorelli C. Knowledge, attitudes, and practices of General Practitioners from the Province of Parma (Northern Italy) towards vaccinations in adults ≥65 year-old. Acta Biomed. 2019;90(9–S):71–75. doi: 10.23750/abm.v90i9-S.8704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang J, Bai Y, Ding H, Wang B, Ngai CH, Kwok KO, Wong ELY, Wong MCS, Yeoh E-K. Acceptance of pneumococcal vaccination in older adults: a general population-based survey. Vaccine. 2021;39(47):6883–93. doi: 10.1016/j.vaccine.2021.10.024. [DOI] [PubMed] [Google Scholar]
- 32.Schneeberg A, Bettinger JA, McNeil S, Ward BJ, Dionne M, Cooper C, Coleman B, Loeb M, Rubinstein E, McElhaney J. Knowledge, attitudes, beliefs and behaviours of older adults about pneumococcal immunization, a Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) investigation. BMC Public Health. 2014;14(1):442. doi: 10.1186/1471-2458-14-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MacDougall DM, Halperin BA, MacKinnon-Cameron D, Li L, McNeil SA, Langley JM, Halperin SA. The challenge of vaccinating adults: attitudes and beliefs of the Canadian public and healthcare providers. BMJ Open. 2015;5(9):e009062. doi: 10.1136/bmjopen-2015-009062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higuchi M, Narumoto K, Goto T, Inoue M. Correlation between family physician’s direct advice and pneumococcal vaccination intention and behavior among the elderly in Japan: a cross-sectional study. BMC Fam Pract. 2018;19(1):153. doi: 10.1186/s12875-018-0841-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaneko M, Aoki T, Goto R, Ozone S, Haruta J. Better patient experience is associated with better vaccine uptake in older adults: multicentered cross-sectional study. J Gen Intern Med. 2020;35(12):3485–91. doi: 10.1007/s11606-020-06187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kizmaz M, Kumtepe Kurt B, Çetin Kargin N, Döner E. Influenza, pneumococcal and herpes zoster vaccination rates among patients over 65 years of age, related factors, and their knowledge and attitudes. Aging Clin Exp Res. 2020;32(11):2383–91. doi: 10.1007/s40520-019-01423-z. [DOI] [PubMed] [Google Scholar]
- 37.Gates A, Gates M, Rahman S, Guitard S, MacGregor T, Pillay J, Ismail SJ, Tunis MC, Young K, Hardy K. A systematic review of factors that influence the acceptability of vaccines among Canadians. Vaccine. 2021;39(2):222–36. doi: 10.1016/j.vaccine.2020.10.038. [DOI] [PubMed] [Google Scholar]
- 38.Kassianos G, Banerjee A, Baron-Papillon F, Hampson AW, McElhaney JE, McGeer A, Rigoine de Fougerolles T, Rothholz M, Seale H, Tan LJ, et al. Key policy and programmatic factors to improve influenza vaccination rates based on the experience from four high-performing countries. Drugs Context. 2021;10:2020-9-5. doi: 10.7573/dic.2020-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


