ABSTRACT
With the advent of COVID-19 vaccines, countries around the globe are anticipating a way out from the pandemic. Despite being an initiative to contain the COVID-19 virus spreading, the mass vaccination program also raised concerns about its consequences on the lifestyle, attitude, and behavioral pattern of vaccinated people in the post-vaccination period. With this in mind, this study investigated changes in lifestyle, attitude, and behavior among vaccinated people in Bangladesh. A cross-sectional survey was conducted incorporating 1227 COVID-19 vaccinated respondents from eight divisions of Bangladesh. The relative importance index (RII) was used to assess the most compelling lifestyle, attitude, and behavior changes, while binary logistic regression was used to identify factors driving the changes. Findings disclosed that respondents increased the physical contact with non-vaccinated ones and amplified consuming nutritious food after vaccination. The inclination of avoiding distance, handshaking, abandoning sanitizer and mask, visiting crowded places, traveling, and staying outside longer was found to be increased among vaccinated individuals. Surprisingly, about seven out of ten surveyed respondents exhibited a sedentary lifestyle, while 67.37% of respondents showed negative behavioral changes following the vaccination period. A positive attitude was observed in encouraging others to be vaccinated against COVID-19. However, 92% of the respondents positively changed their attitude toward the COVID-19 vaccine after vaccination. Furthermore, the participants’ age, residence, economic status, and educational level influenced lifestyle, attitude, and behavioral changes positively. The study recommends informing citizens about the opacity of vaccinations’ ability to contain infections and encouraging them to continue following COVID-19 protective guidelines.
KEYWORDS: COVID-19 vaccine, lifestyle, attitude, behavior, post-vaccination
Introduction
Like past pandemics, the COVID-19 pandemic is linked with anxiety, fear, and concerns about the everyday activities of the common people.1 The pandemic situation is unique, because individuals were afraid of becoming infected or transferring disease, and governments’ efforts to control the pandemic and stop human transmission of the disease had societal and economic ramifications.2–4 Alongside physical health hazards and economic consequences, the COVID-19 caused severe mental trauma among general populations, healthcare professionals, and children of Bangladesh.5–7
The first verified COVID-19 case was reported in Bangladesh on 8 March 2020. Infection rates appeared to remain low until the end of March, but in April 2020, a sharp increase began, with cases doubling times of 2 days.8,9 The government’s efforts for containing the COVID-19 transmissions include enforcement lockdown, self-isolation, social distancing, borders shutdowns, school and university closure, quarantines, and travel restriction.10–12 Notably, accompanied by plasma therapy, some oral medications have become available to treat COVID-19 infected people, including Remdesivir, Paxlovid, and the latest Molnupiravir.13 However, like other previous epidemics (Dengue, Cholera), scientists believe that mass vaccination programs can substantially alleviate the transmission of viruses and ultimately lead to a normal lifestyle and revitalize the economy.
Like many other countries around the world, Bangladesh started the vaccination program on 7 February 2021 by importing the Oxford/AstraZeneca COVID-19 vaccine (brand name: COVISHIELD), manufactured by the Serum Institute of India and protected by the Oxford-AstraZeneca vaccine patent.14 Unfortunately, the government was forced to halt the first dose of the vaccine campaign on 25 April 2021, a day after India stopped exporting the vaccine due to a record-breaking increase in cases and deaths there. Bangladesh resumed its vaccination program by procuring vaccines from other countries, such as Moderna vaccine from the US and Sinopharm vaccine from China15,16 and planning to inoculate at least 50 million people by the end of 2021.17 To date, Bangladesh has brought about 22.6% of its total population under vaccination, markedly lower than that of India (33%), Sri Lanka (64.1%) and Pakistan (24%).18 Hence, while implementing the vaccination strategy, Bangladesh must keep in mind the necessity to acquire more vaccines in order to meet its immunization targets.
Previous studies indicated that vaccination programs could impact vaccinated individuals’ lifestyle, attitude, and behavior because of the protection they received.19,20 Vaccinated individuals may begin to interact with more people and be exposed to situations where non-vaccinated individuals are more likely to become infected. A recent study found that people who have been vaccinated can harbor viruses in their bodies without showing any symptoms, which can then be spread to others.21 Therefore, despite being immunized, everyone should maintain safety measures, not just for himself/herself, but for people around. It should also be noted that, since a significant pie of the Bangladeshi people are yet to be vaccinated, relaxing and ignoring COVID-19 protocol in their quotidian life may lead to a spike in cases and could cause another wave of the pandemic.22
There are also some studies on the impact of vaccination programs on individual behavior. A longitudinal study of behavior after Lyme disease vaccination in the United States (US) revealed that individuals who were vaccinated were less likely to practice two of five preventive behaviors: Wearing light-colored clothing and using tick repellent.23 In another comparable study conducted in the US stated that vaccinated individuals interacted with more people in larger groups during the 2 days following vaccination than they had prior.24 On the other hand, from various studies, we found the vaccination rollout of a country is challenged in two ways; change in public adherence to the preventive measures of infection disease, i.e., behavioral change and logistic capacity of vaccine delivery.25,26 Besides, a study suspected that mass vaccination programs might result in risky behavior among the general people.27
The above discussion suggests that vaccination may lead to a reduction in public health precautions over the world. Worriedly, neglecting COVID-19 protocol among the vaccinated population of Bangladesh may lead to another catastrophe as it witnessed in the last one and half years. Alongside, this could put other unvaccinated and vulnerable ones at risk of catching the virus, while some may lose their lives, too. Indeed, the fear that the vaccinated population could be super-spreaders raised our attention. Thus, the influence of COVID-19 vaccination programs on immunized individuals must be investigated. Several studies explored the COVID-19 vaccine-taking hesitancy and acceptability among Bangladeshi people.28–31 However, no study investigates the lifestyle, attitude, and behavior changes of vaccinated people in Bangladesh, a third-world nation with a vulnerable healthcare system. This study not just determines the changes in lifestyle, attitude, and behavior in vaccinated people but also attempts to identify the factors responsible for the changes.
This study will enrich the literature on COVID-19 vaccination in several ways. First, this is the first kind of study that examines the impact of the COVID-19 vaccine on the lifestyle and attitude of vaccinated individuals. Second, a study on the change in behavior due to vaccination is also absent in Bangladesh. Third, this study will help policymakers gain firsthand knowledge about the vaccination’s impact on individual lifestyle, attitude, and behavior. Indeed, this will enable them to develop new policies regarding the vaccinated people about their public adherence, changing lifestyle, and attitude.
Methods
Study design, sampling, and data collection
A countrywide cross-sectional survey was conducted in Bangladesh between 28 July 2021 to 13 August 2021. We selected the citizens of Bangladesh who had already been vaccinated against COVID-19 before one month of data collection. This is because it can give a better understanding of vaccinated people’s changes in lifestyle, attitude, and behavior. To provide a more substantiated and nationwide image in our research, we included representative participants from each of Bangladesh’s eight divisions. To reveal reliable and robust results, this study used a disproportionate sampling based on the population size of the respective division. Since there is a vast variation in the population size of the eight divisions, proportionate sampling would not adequately represent the overall picture of the country. We used a mixed-method for data collection, i.e., direct interview method and online survey for several reasons such as, (i) It allowed rural participants who do not have adequate internet facilities to participate in the survey; (ii) It allowed a various range of participant with the different socio-economic background; (iii) To collect a nationally representative sample within a limited time frame. However, the direct face-to-face interview was conducted with a physical distance of at least 2 m and maintained COVID-19 protective norms advised by World Health Organization (WHO).32
We estimated the sample size for this survey using a 95% confidence interval and a margin of error of ±3%, assuming that 50% of the respondents had a good lifestyle, attitude, and behavior. According to the latest statistics, the adult population of Bangladesh is 111720699,33 hence this is the population size of our study. The target sample size was determined to be 1068 respondents using the Raosoft (http://www.raosoft.com/samplesize.html) sample size calculator and considering the information mentioned above. When the survey portal and direct interviews were closed, a total of 1243 responses were recorded. Among the recorded sample, sixteen samples were found incomplete, and those were discarded from the final analysis. As a result, this study used a total of 1227 valid samples, which were well above the minimum required sample. Therefore, our sample size met the minimum sample size requirement for this study. Samples were selected based on some criteria. Firstly, it only included the people over eighteen years of age since the Government of Bangladesh had availed vaccination to them at the time of the survey. Secondly, people who have completed taking both doses of an available COVID-19 vaccine at least 30 days prior to the survey. People, who were over eighteen years and did not take any or did not complete the second dose of the COVID-19 vaccine, were excluded from the study sample.
Online data were collected using Google Forms through a self-reported questionnaire following the snowball sampling technique, whereas face-to-face interviews were conducted through personal field visits of data enumerators who are postgraduate and had prior experience of data collection. To collect data through the online portal, a shareable link was developed using Google Forms. It was widely disseminated via social media platforms (e.g., WhatsApp, Facebook, Messenger, Instagram, LinkedIn, etc.) to the participants who filled up requested to forward it to others. In addition, the questionnaire link was sent out through e-mail to the authors’ e-mail list. The goal of the survey was clearly communicated to the respondents, and their consent was obtained prior to the data collection. Prior to data collection, a pilot survey was undertaken on ten vaccinated persons. The questionnaire was revised and finalized for data collection according to the observations of the pilot survey. Data obtained from both online survey and face-to-face interviews were continuously monitored and scrutinized by the researchers for any measurement errors, duplications, or inconsistencies.
Questionnaire development and measures
A well-structured questionnaire was created in both English and Bangla language to perform the data collection. The questionnaire was divided into four sections: (i) socio-demographic information; (ii) changes in lifestyle after vaccination; (iii) changes in attitude after vaccination; and (iv) behavioral changes after taking the COVID-19 vaccine. It took 7–10 minutes to complete the survey. Respondents were asked five questions on their lifestyle changes after being vaccinated, with the options to respond as either increased, decreased, or unchanged. We assigned +1, −1, and 0 for increased, decreased, and unchanged, respectively. The total score of lifestyle change ranged from −5 to +5. The cumulative positive score indicated the improved lifestyle while the minus score denoted the negative lifestyle change. Cronbach alpha was used to assess items’ internal reliability, with a coefficient of 0.72 indicating internal reliability.
The attitudes scores were calculated using the participants’ responses to five statements, while responses were recorded on a five-point Likert scale. The scoring was done in following way i.e., strongly agree = 5, agree = 4, neutral = 3, disagree = 2, strongly disagree = 1. The total attitude scores ranged from 5 to 25, with scores 5 to 15 denoting negative attitudes while 16 to 25 signifying the positive attitudes. The value of the Cronbach alpha coefficient was 0.71, marking internal reliability. Respondents were asked to react to the given 11 statements with a scale of “Increased = +1,” “Unchanged = 0,” or “Decreased = −1” for assessing the behavioral changes. However, a reverse scale was used for negative statements.34 The overall score ranged from −11 to +11. The cumulative positive score means an affirmative change in behavior, whereas a negative value indicates negative change. The value of Cronbach’s alpha coefficient was 0.80, reflecting internal reliability.
Data analysis
This study primarily employed frequencies and percentages in tabular and graphical form to demonstrate the participant’s responses. Each item of participants’ lifestyle, attitudes, and behavioral change after COVID-19 vaccination were examined through the Relative Importance Index (RII).35,36 RII has been useful in various studies to determine the ranking of the different factors from the viewpoints of different groups.37,38 The formula for computing RII is as follows:
| (1) |
where P is the score given to each statement by the participants, n is the number of responses in each Likert, Q is the highest score of the Likert scale, and N is the total number of participants.
Furthermore, a binary logistic regression was used to estimate and depict more understanding of the contributing factors influencing the participant’s lifestyle, attitude, and behavior change following COVID-19 vaccination. The binary logit model is considered the best choice for investigating binary variables since regular linear regression models (whether simple or multiple) are not appropriate for binary responses.39 In this study, explained variables are lifestyle, attitude, and behavior change where the value one was assigned for the respondent who had a positive change (Y = 1) and 0 for otherwise (Y = 0). A p-value of < 0.01, 0.05, and 0.1 was used to demonstrate statistical significance at the 1%, 5%, and 10% levels, respectively. The STATA (StataCorp LLC, Texas, USA) version 15 software was used to analyze the data.
Ethical approval
This study did not require any ethical approval since all human involvements were ensured following local legislation and institutional concern. Besides, all proceeds of this study were conducted as per the Helsinki Declaration principles of the human subject survey.
Results
Socio-demographic characteristics of participants
Table 1 illustrates the personal and clinical characteristics of the studied respondents. Among the respondents, more than half (59.17%) were males, and the rest were females. Nearly half of the participants (48.97%) were under the age of 36, with around a quarter falling into both the middle and old age categories. Approximately half of the participants (49.40%) lived in the urban area, whereas 21% of participants were from rural and the rest (29.6%) were from semi-urban areas. Only 5.87% of respondents had completed their primary school, while over 55% had completed their university degrees. Regarding the monthly family income, more than half of respondents (60.88%) remained in the lower-middle income group, and 30.97% of participants were from the upper-middle income group. Three out of ten respondents had adverse effects after getting vaccinated, whereas the rest did not observe any side effects. The most common side effects were muscle pain (30.22%), fever (28%), headache (20.88%), dizziness (17.33), weakness (15%), and allergic reaction on the skin (1.33%).
Table 1.
Characteristics of selected respondents (N = 1227)
| Personal and clinical characteristics | Level | No. of participants (%) |
|---|---|---|
| Age (years)a | Young (18–36) | 601 (48.97) |
| Middle aged (37–51) | 286 (23.31) | |
| Old aged (>51) | 340 (27.71) | |
| Sex | Male | 726 (59.17) |
| Female | 501 (40.83) | |
| Level of education | Primary | 72 5.87 |
| Secondary | 266 21.68 | |
| Higher secondary | 210 17.11 | |
| Graduate | 524 42.71 | |
| Postgraduate or above | 155 12.63 | |
| Total family income (monthly)b | Low income | 58 (4.73) |
| Lower-middle income | 747 (60.88) | |
| Upper-middle income | 380 (30.97) | |
| High income | 42 (3.42) | |
| Residence area | Urban | 606 (49.40) |
| Rural | 258 (21) | |
| Semi urban | 363 (29.6) | |
| Suffered from any side effect after vaccination? | Yes | 372 (30.32) |
| No | 855 (69.68) | |
| Which side effect did you suffer from?c | Fever | 189 (28.0) |
| Headache | 141 (20.88) | |
| Muscle pain | 204 (30.22) | |
| Dizziness | 117 (17.33) | |
| Weakness | 15 (2.22) | |
| Allergic reaction on the skin | 9 (1.33) |
aAge is categorized according to the National Youth Policy of Bangladesh (2017).
bTotal household income categorized into: Low income (≤$85), Lower middle income ($86 to $336), Upper middle income ($337 to $1040), and High income (≥$1040) according to World Bank income group.
cThe number of respondents answered to the question does not equal total participants who were suffered from side effect due to multiple responses by a participant.
Change in lifestyle of COVID-19 vaccinated people
The responses to five statements were used to assess post-vaccination lifestyle change. The statements were ranked based on the relative importance index (RII) value, and the estimated findings are illustrated in Table 2. Based on the RII value, the vaccinated people’s ‘intention to avoid close contact with non-vaccinated friends and closed one’ ranked first (RII = 0.59). However, the results showed that 71.56% of respondents had decreased their intention, while 9.04% had raised their intention to contact non-vaccinated relatives or friends. The second-ranked statement, ‘consuming nutritious food after vaccination,’ increased and decreased among 61.7% and 16.67% of respondents, respectively. On the other hand, respondents’ ‘sleeping quality after vaccination’ and ‘intention to remain physically active’ got lower importance, ranked fourth and fifth with RII of 0.42 and 0.32, respectively. Thus, despite a significant variation in sleeping patterns, the majority of the respondents’ intentions to be physically active remained basically same as of prior vaccination.
Table 2.
Question regarding the change in lifestyle after being vaccinated (N = 1227)
| Questions | No. of participants (%) |
RII | Rank | ||
|---|---|---|---|---|---|
| Increased | Decreased | Unchanged | |||
| Avoiding close contact with friends and loved ones who aren’t vaccinated? | 111 (9.04) | 878 (71.56) | 228 (18.58) | 0.59 | 1 |
| Consumption of nutritious food after vaccination? | 648 (61.7) | 174 (16.67) | 228 (21.7) | 0.55 | 2 |
| Intention of keeping essentials medication after vaccination? | 240 (19.56) | 252 (20.54) | 735 (59.90) | 0.45 | 3 |
| Sleeping quality after vaccination than previous? | 426 (34.7) | 78 (6.4) | 720 (58.7) | 0.42 | 4 |
| Intention to be physically active after the vaccination? | 39 (3.2) | 54 (4.4) | 1134 (92.4) | 0.32 | 5 |
Change in attitude toward COVID-19 vaccine
Like the lifestyle change, the shift in respondents’ attitudes toward COVID-19 vaccines after vaccination was assessed using five-point Likert scale statements (Table 3). The estimated RII value ranked the statements. Results revealed that the highest RII value, 0.83, was calculated for the statement, ‘after taking the vaccine, I encourage my family members to take the vaccine.’ More than 96% of the respondents agreed with this statement, and more than 81% of the respondents consented positively with ‘vaccination will bring back a normal life.’ After getting vaccinated, more than half of the respondents (55.5%) believed their immunity system improved. Furthermore, 67.3% of respondents believed that the COVID-19 vaccine could protect them from future health threats.
Table 3.
Statements regarding the change in attitudes toward COVID-19 after being vaccinated (N = 1227)
| Statements | No. of participants (%) |
RII | Rank | ||||
|---|---|---|---|---|---|---|---|
| SA | A | N | D | SD | |||
| After taking vaccine, I encourage my other family members and relatives to be vaccinated. | 744 (60.6) | 435 (35.5) | 42 (3.4) | 3 (0.2) | 3 (0.2) | 0.83 | 1 |
| I think that the COVID-19 vaccination will bring the normal life back. | 720 (58.7) | 276 (22.5) | 180 (14.7) | 48 (3.9) | 3 (0.2) | 0.76 | 2 |
| I think that my immunity system is now more improved after vaccination. | 102 (8.3) | 579 (47.2) | 480 (39.1) | 57 (4.6) | 9 (0.7) | 0.66 | 3 |
| I feel confident that the vaccines can prevent myself from being COVID-19 infected. | 216 (17.6) | 633 (51.6) | 312 (25.4) | 63 (5.1) | 3 (0.24) | 0.55 | 4 |
| I think that vaccines can protect myself from future health threat. | 186 (15.2) | 639 (52.1) | 345 (28.1) | 51 (4.2) | 6 (0.5) | 0.43 | 5 |
Note: SA = Strongly agree, A = Agree, N = Neutral, D = Disagree, SD = Strongly disagree.
Behavioral changes of vaccinated people
Along with lifestyle and attitudinal changes, the vaccination against COVID-19 alters the behavioral pattern of the respondents. To elicit responses, eleven behavioral change-related questions were employed, and RII was calculated to find the respondents’ most change-explaining question (Table 4). Results revealed that 78% of participants had decreased their distance maintaining habit after being vaccinated due to their apathetic movements. The second and fourth-ranked questions (RII 0.80 and 0.73) indicated that the frequent visits to crowded places and traveling increased among 73.8% and 75.3% of the respondents, respectively. Alarmingly, the intention of abandoning sanitizers and mask use after vaccination had increased among 78.2% of the respondents, while only 13.4% of the respondents kept the habit unchanged. After being vaccinated, approximately 75% of the participants increased their willingness to stay outside of their homes and shake hands with friends and surroundings. Besides, vaccinated peoples’ intention of spending more time on outside recreational activities increased, concurred by 85.1% of the respondents. Approximately eight out of ten respondents reported that their mental health has improved after vaccination. Although communicating with the medical personnel remained unchanged for the majority of the respondents (80.4%), the intention of expending more on protective measures, i.e., masks, sanitizers, hand rub, etc., decreased for 77% of the respondents. For nonsmoker respondents, the behavior of smoking was least presentative, but for smokers, the smoking habit remains unchanged between prior and post-vaccine periods. Only a few (6.1%) respondents agreed that their intention of smoking after vaccination decreased.
Table 4.
Questions related to change in behavioral pattern after COVID-19 vaccination (N = 1227)
| Questions | No. of participants (%) |
RII | Rank | ||
|---|---|---|---|---|---|
| Increased | Decreased | Unchanged | |||
| Distance avoiding habit in the public place after vaccination? | 957 (78) | 114 (9.3) | 156 (12.7) | 0.84 | 1 |
| Frequency of visit to crowded areas (Market/Shopping mall/public gathering) after vaccination? | 906 (73.8) | 174 (14.2) | 147 (12) | 0.80 | 2 |
| Intention of abandoning sanitizer and mask after vaccination? | 960 (78.2) | 102 (8.3) | 165 (13.4) | 0.76 | 3 |
| Frequency of traveling after the vaccination? | 924 (75.3) | 165 (13.4) | 138 (11.2) | 0.73 | 4 |
| Your mental health after the vaccination? | 968 (78.89) | 66 (5.38) | 193 (15.73) | 0.66 | 5 |
| Intention of handshaking with friends and surroundings after vaccination? | 927 (75.6) | 138 (11.2) | 162 (13.2) | 0.63 | 6 |
| The duration of staying outside of home after vaccination? | 912 (74.3) | 153 (12.5) | 162 (13.2) | 0.57 | 7 |
| Intention of expending more on protective measures i.e., mask, sanitizers, hand rub after vaccination? | 141 (11.5) | 945 (77) | 141 (11.5) | 0.55 | 8 |
| Communication with medical personnel after vaccination? | 54 (4.4) | 186 (15.2) | 987 (80.4) | 0.49 | 9 |
| Intention of spending more on outside recreational activities after the vaccination? | 1044 (85.1) | 48 (3.9) | 135 (11) | 0.42 | 10 |
| Intention of smoking (for smoker only) after vaccination? | 33 (5.1) | 39 (6.1) | 570 (88.2) | 0.35 | 11 |
Level of change in vaccinated people’s lifestyle, attitude, and behavior
Figure 1 depicts the percentage of respondents who had positive and negative changes in their lifestyle, attitude toward the COVID-19 vaccine, and behavior after receiving the vaccine. Among the respondents, 28.85% expressed positive changes in lifestyle, whereas a majority portion of respondents (71.15%) had negative changes. According to the attitude score of surveyed respondents, nine out of ten respondents displayed positive changes in attitude. In the view of behavioral changes of studied respondents, 32.63% exposed positive changes, and 67.37% of participants disclosed negative changes.
Figure 1.
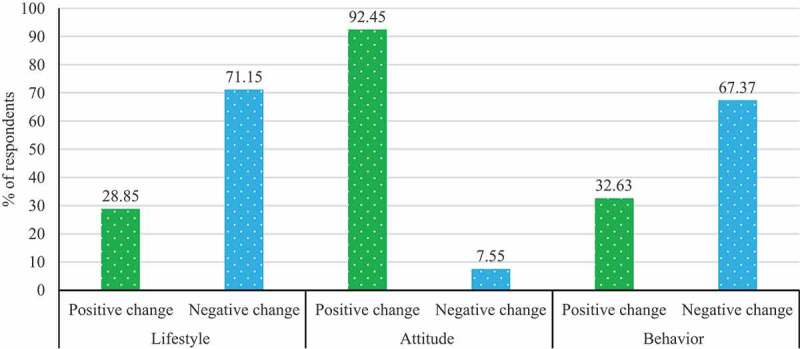
Percentage of respondents having positive and negative changes in lifestyle, attitude toward COVID-19 vaccine, and behavior after being vaccinated (N = 1227).
Factors influencing the lifestyle, attitude, and behavior change of vaccinated people
A binary logistic model was employed to determine the factors that significantly influence vaccinated people’s lifestyle, attitude, and behavior change. As predictor variables, age, sex, residence area (rural, urban or semi-urban), economic class (based on income), formal education level, and any side effects of vaccination were used to explain the focus variable (Table 5). Young respondents (18 to 36 years) were more likely to have a sedentary lifestyle, positive attitudinal change toward vaccines, and risky behavioral changes than older respondents (age > 51 years). The findings revealed that urban dwellers were more likely to undergo positive lifestyle and attitudinal changes than rural individuals. Lower-middle-income people did not show any sign of lifestyle, attitude, and behavior change. On the other hand, the upper-middle-income people were more likely to change their lifestyle and attitude positively after being vaccinated. However, the high-income group illustrated significant positive lifestyle, attitude, and behavior change. People with higher education, such as a bachelor’s degree, are more likely to go through all the positive changes with significant odds. For example, respondents with postgraduation showed higher odds of going through positive behavioral changes than primary-level educated people. Finally, no link was found between the side effect of vaccination and a person’s lifestyle, attitude toward vaccines, and behavior change.
Table 5.
Binary logistic regression presenting factors influencing the participant’s lifestyle, attitude, and behavior change after COVID-19 vaccination (N = 1227)
| Lifestyle change |
Attitude change |
Behavior change |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Categories | Coef. | AOR | P-value | Coef. | AOR | P-value | Coef. | AOR | P-value |
| Age | Old aged (>51) (Ref) | |||||||||
| Middle aged (37–51) | 0.32 | 1.34 | 0.17 | 0.82 | 1.12 | 0.26 | 0.09 | 1.12 | 0.23 | |
| Young (18–36) | −0.26 | 0.72 | 0.04** | 0.43 | 1.76 | 0.00*** | −0.16 | 0.89 | 0.00*** | |
| Sex | Male (Ref.) | |||||||||
| Female | −0.18 | 0.92 | 0.25 | 0.04 | 1.29 | 0.66 | 0.10 | 1.41 | 0.57 | |
| Residence area | Rural (Ref.) | |||||||||
| Urban | 1.27 | 3.58 | 0.00*** | 1.04 | 2.85 | 0.00*** | 0.21 | 1.23 | 0.18 | |
| Semi-urban | 0.35 | 1.42 | 0.25 | 0.65 | 1.21 | 0.15 | 0.17 | 1.19 | 0.42 | |
| Economic class | Low income (Ref.) | |||||||||
| Lower-middle income | 0.92 | 2.44 | 0.19 | 1.01 | 2.78 | 0.24 | 1.36 | 2.17 | 0.46 | |
| Upper-middle income | 1.67 | 3.78 | 0.07* | 1.91 | 4.21 | 0.03** | 0.92 | 1.79 | 0.21 | |
| High income | 1.92 | 4.19 | 0.00*** | 1.28 | 3.08 | 0.0.8* | 0.02 | 1.28 | 0.06* | |
| Education level | Primary (Ref.) | |||||||||
| Secondary | 0.78 | 1.43 | 0.23 | 1.30 | 1.94 | 0.17 | 0.10 | 1.02 | 0.49 | |
| Higher secondary | 0.89 | 1.67 | 0.11 | 1.89 | 2.38 | 0.08* | 0.78 | 2.31 | 0.05** | |
| Graduate | 1.20 | 3.89 | 0.01** | 0.06 | 1.19 | 0.09* | 1.88 | 4.03 | 0.00*** | |
| Postgraduate | 0.56 | 1.26 | 0.00*** | 0.89 | 2.01 | 0.04** | 2.23 | 5.47 | 0.00*** | |
| Suffering from side effects of vaccination | Yes (Ref.) | |||||||||
| No | −0.89 | 0.81 | 0.62 | 1.23 | 1.08 | 0.74 | −1.36 | 0.75 | 0.36 | |
Note: ***, ** and * indicates significance at 1%, 5% and 10% level, respectively. In binary logistic regression, explained variables are lifestyle change (1 if have positive change, 0 for otherwise), attitude change (1 if have positive change, 0 for otherwise), and behavior change (1 if have positive change, 0 for otherwise). AOR = Adjusted Odds Ratio, Ref. = Reference category, Coef. = Coefficient.
Discussion
Post-vaccination infection surges are one of the most raging risks for any nation. Unfortunately, still adequate amount of research is required to validate whether a COVID-19 vaccine can provide life-long protection against the deadly virus. A recent study showed that the Moderna mRNA-1273 vaccine ensures antibody protection against COVID-19 up-till six months after its second dose.40 Despite the fact that numerous vaccinations have been developed and are being used around the world, the virus continues to spread, owing to its rapid mutations.41 However, vaccinated people’s risky behavior and sedentary lifestyle changes are also responsible for increasing COVID-19 infection rates. Under these circumstances, our study was an effort to explore post-vaccination lifestyle, attitude, and behavior change by incorporating 1227 vaccinated individuals of Bangladesh.
According to the findings, maintaining distance was the most avoided phenomenon among the respondents, as the majority of them claimed that they wanted to expand intimate touch with their friends and loved ones. This is obviously a worrisome revelation, as avoiding intimate contact with friends and family may increase infections, as the majority of recorded cases are considered to be transmitted through family and close friends.42 Hence, allowing close contact may not be that serious for youth but can be lethal for the elder ones of the families because old aged people have a 23-fold higher risk of COVID-19 death and infection than those are middle and young aged.43 Reportedly, an increase in nutritious food intake was observed among more than 60% of the participants. This may roughly represent that people have resorted to consuming more nutritious food to boost their immunity. Intention to keep essential medicines at home, intention to perform physical activity, and sleeping quality was found to be less volatile as the majority of the participants reported no change. However, a notable portion of the respondents claimed that they enjoy more sound sleep following vaccination. Sound sleep is inextricably associated with the psychological state of an individual.44 Since a COVID-19 vaccine is expected to boost people’s confidence in their ability to defend themselves from the deadly virus; thus, it can help them enhance their sleeping quality and reduce their stress levels. Overall, this study found a considerable change in lifestyle after vaccination, with approximately three-quarters of the participants reporting a move to a sedentary lifestyle.
Our study further revealed a positive change in attitudes among vaccinated respondents toward a COVID-19 vaccine as more than 90% of them were found to be optimistic and confident regarding a COVID-19 vaccine. Happily, the majority of the respondents claim that they will convince their family and relatives to take a vaccine as the preponderance of them believed COVID-19 vaccines can bring back a normal life. Similar findings were also observed in the study of Hossain et al.28 Therefore, it is clear that persons who have been vaccinated will play a critical role in persuading others to get vaccinated. This will hasten the vaccination campaign in Bangladesh, resulting in more people being vaccinated and, in turn, limiting the virus’s spread.45,46 However, a sizable portion of the participants were overconfident in their ability to prevent COVID-19 infection and potential health risks after vaccination. It might play a decisive role in deceiving them to adopt a sedentary lifestyle that may put them at risk of getting other health issues, deteriorating their overall well-being.
Moreover, behavioral changes seemed negative among the lion’s share of the sample studied. In particular, the participants largely overlooked distance maintaining habits in public places, whereas visiting crowded places was also reported more frequently. This finding was contradicting the study of Rahamim-Cohen et al.47 demonstrating that less than half the respondents in a sample of Israel continued adhering to social distancing. Besides, a recent report by the World Economic Forum (WEF)48 showed that the majority of the participants were found to follow social distancing following vaccination. It was surprising that roughly three-quarters of the total participants stated an escalation in their visit to crowded places, traveling, time of staying outside, and handshaking with friends and others after being vaccinated. What is more concerning is that nearly 78% of the total participants stopped wearing masks and using sanitizer. Moreover, nearly 85% of the respondents reported expanding their outside recreational activities for a longer period. These findings are way depressing compared to a report from the USA, the UK, Germany, France, Italy, Brazil, Mexico, Japan, and Spain, where more than 75% of participants in the study were willing to maintain social distance and wearing masks even after being vaccinated.48 Moreover, a previous study led by Wright et al.49 showed that some portion of UK adults refused to maintain social distancing, whereas the report of The Guardian50 stated that Israelis are curbing safeguarding practices and behavior following being vaccinated. Previous studies on changes in behavior and health safety measures among US residents after receiving the Lyme disease and influenza vaccines found that respondents were reluctant to maintain health safety precautions and a healthy behavioral pattern.23,24
Nonetheless, the results of our research are really alarming. Indeed, all of these disparaging behavioral patterns may surely contribute to an increase in infections in the following days. Apart from the aforementioned findings, a significant pie (four-fifth) of the selected respondents reported the improvement in mental health. This could be explained by the fact that the COVID-19 vaccination helps to alleviate people’s pandemic-related trauma, hence reducing stress, enhancing confidence, and restoring psychological balance.51 However, a minimal change was witnessed in maintaining contact with health professionals and smoking frequency among the smokers.
Since the COVID-19 pandemic has sparked discrimination against persons from specific socio-economic backgrounds,52 the vaccination can alter people’s lifestyles, attitudes, and behaviors based on their socio-economic status. Therefore, we explored determinants of changes in lifestyle, attitude toward vaccine, and behavior. As discernable, young people showed a greater likelihood to adopt a sedentary lifestyle and risky behavioral patterns after being vaccinated. This finding is consistent with the study of Rahamim-Cohen et al.47 where they found younger people are more reluctant to health safety measures and health-friendly behavior. Alongside, a study led by SPI-B53 indicated that in the UK, people aged 18–24 are more reticent to maintain protective measures following vaccination. Furthermore, when compared to young people, elderly adults have a stronger desire to protect themselves even after being vaccinated.27 However, youth were likely to develop a more positive attitude toward the COVID-19 vaccine following being vaccinated. Since the COVID-19 vaccine is an emerging subject in the modern world and as young individuals are more exposed to information,54 they can better understand the essence of a potential vaccine to be a vital tool to confront this pandemic. Also, youth are less circumscribed to prejudices than older ones55 as they are more likely to follow the ways of science.
Interestingly, results revealed that respondents from urban areas have higher odds of shifting to a healthy lifestyle and are more likely to be optimistic about the vaccines following vaccination. Since most urban populations tend to be more educated in Bangladesh,56 they might be more cautious about their health. Also, the majority of the urban residents are believed to be void of prejudices,57 and they can accept anything after their own judgment. A plethora of scientific studies and academic reports are gradually disclosing the efficacy and significance of a COVID-19 vaccine as potential protection against the deadly virus. As urban people are more exposed to information sources and the internet,58 they get to know the benefits and efficacy of a vaccine more compared to rural and suburban residents, end subsequently they can change their lifestyle.
Further, upper-middle income and high-income people hold a greater likelihood of following a healthy lifestyle while possessing a more positive attitude toward a COVID-19 vaccine after being vaccinated. Besides, individuals with high income also seem to have positive behavior after being vaccinated. This could be ascribed to the fact that people of higher income levels are more concerned about their health and safety.59 Moreover, as income increases, the standard of living also upgrades,60 which, eventually improves one’s perception of health and well-being. However, it’s not surprising that people with greater education levels (e.g., graduation and postgraduation) are more likely to lead a healthy life and have more trust in the vaccine following the vaccination. Furthermore, people with a greater level of secondary, graduate, or postgraduate education are more likely to change their behavior patterns positively. Education is, without question, one of the most important factors of health awareness that influences one’s behavior and lifestyle in response to any disease.
Our study paves the way to further research avenues as it is circumscribed with certain limitations. This study did not consider the physiological data of the respondents and only focused on their socio-economic factors in evaluating the changes in lifestyle, attitude, and behavioral patterns. A large portion of the respondents participated in the self-administered survey on the internet and social media, whereas face-to-face interviews could have engaged a more diversified range of respondents with versatile socio-economic characteristics. Since we conducted a quick survey-based study, a countrywide study may reveal more actual circumstances. Despite of these limitations, our study will help authorities understand people’s lifestyle and behavioral change and address possible public health concerns following COVID-19 vaccination.
Conclusion
COVID-19 vaccines come forward to evacuate the global population from the turmoil of life threats, economic distress, and painstaking consequences. Vaccination aims to provide short-term safety while breaking the infection chain through prevention measures is more life-saving. Although being vaccinated may increase one’s confidence in health safety measures and protection apart from boosting immunity, for ensuring long-term safety, the growing defiance among vaccinated people toward preventive activities immediately needs to be controlled. If the current attitude persists and the sedentary lifestyle of the Bangladeshi people continues, catastrophe is not far beyond as the COVID virus is highly mutant.25 Thus, an explicit peril may emerge even after continuous vaccine inoculation in Bangladesh. Therefore, changing the general population’s behavior is not an easy task when they assume to be protected. However, the country’s health authority may arrange mass campaigns to ensure that every vaccine recipient understands that vaccine may not provide adequate protection for at least the first 21 days61 and are susceptible to spread the infection get infected from others. Specifically, general awareness needs to be created by any means.
Acknowledgments
The authors are grateful to the participants of this study for sharing their information.
Funding Statement
The authors declare that this study has received no external funding to conduct the research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V.. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. Get rights and content. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO.. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit Ther Res. 2012;36(3):210–9. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- 3.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–93. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blakey SM, Abramowitz JS. Psychological predictors of health anxiety in response to the Zika Virus. J Clin Psychol Med Set. 2017;24(3):270–78. doi: 10.1007/s10880-017-9514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Das R, Hasan MR, Daria S, Islam MR. Impact of COVID-19 pandemic on mental health among general Bangladeshi population: a cross-sectional study. BMJ Open. 2021;11(4):e045727. doi: 10.1136/bmjopen-2020-045727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Islam MR, Qusar MS, Islam MS. Mental health of children amid COVID-19 pandemic in Bangladesh: an exploratory observation. Asia-pacific J Public Health. 2021;33(4):469–70. doi: 10.1177/2F10105395211004371. [DOI] [PubMed] [Google Scholar]
- 7.Repon MAU, Pakhe SA, Quaiyum S, Das R, Daria S, Islam MR. Effect of COVID-19 pandemic on mental health among Bangladeshi healthcare professionals: a cross-sectional study. Sci Prog. 2021;104(2):1–18. doi: 10.1177/2F00368504211026409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO . COVID-19 situation report no.: 11, 2020; 2020. [accessed 2021 July 20]. https://www.who.int/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who-ban-covid-19-sitrep-11.pdf?sfvrsn.
- 9.Dhaka Tribune . 20-fold rise in COVID-19 cases in Bangladesh since 1 April, 2020; 2020. [accessed 2021 July 20]. https://www.dhakatribune.com/health/coronavirus/2020/04/14/20-fold-rise-of-covid-19-cases-in-bangladesh-since-april-1.
- 10.Hoque MN, Hannan A, Imran S, Alam MA, Matubber B, Saha SM. Anxiety and its determinants among undergraduate students during E-learning in Bangladesh amid Covid-19. J Affect Disord Rep. 2021;6:100241. doi: 10.1016/j.jadr.2021.100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mannan DKA, Farhana KM. The COVID-19 pandemic: challenges and reality of quarantine, isolation and social distancing for the returnee migrants in Bangladesh. Int J Migr Res Dev. 2020;6(1). [Google Scholar]
- 12.Kamruzzaman M, Sakib SN. Bangladesh imposes total lockdown over COVID-19. Anadolu Agency; 2020. [accessed 2020 June 5]. https://www.aa.com.tr/en/asia-pacific/bangladesh-imposes-total-lockdown-over-covid-19/1778272.
- 13.Harvard Health Publishing . Treatments for COVID-19; 2021. [accessed 2021 December 5]. https://www.health.harvard.edu/diseases-and-conditions/treatments-for-covid-19.
- 14.Business Standard . Bangladesh approves getting 30 mn doses of Covishield vaccine from India; 2021. [accessed 2021 July 23]. https://www.business-standard.com/article/current-affairs/bangladesh-approves-getting-30-mn-doses-of-covishield-vaccine-from-india-121010800256_1.html.
- 15.Anadolu Agency . Bangladesh resumes mass registration for COVID-19 vaccination; 2021. [accessed 2021 September 15]. https://www.aa.com.tr/en/asia-pacific/bangladesh-resumes-mass-registration-for-covid-19-vaccination/2297662.
- 16.The Daily Star . Bangladesh running out of vaccine; 2021. [accessed 2021 July 19]. https://www.thedailystar.net/editorial/news/bangladesh-running-out-vaccines-2082081.
- 17.Dhaka Tribune . Bangladesh plans to inoculate 50 million people within this year; 2021. [accessed 2021 July 25]. https://www.dhakatribune.com/health/coronavirus/2021/07/03/50-million-people-to-be-inoculated-within-2021.
- 18.Our World in Data . Coronavirus (COVID-19) vaccinations; 2021. [accessed 2021 December 4]. https://ourworldindata.org/covid-vaccinations?country=OWID_WRL.
- 19.Wilde GJ. The theory of risk homeostasis: implications for safety and health. Risk Analysis. 1982;2(4):209–25. doi: 10.1111/j.1539-6924.1982.tb01384.x. [DOI] [Google Scholar]
- 20.Hedlund J. Risky business: safety regulations, risk compensation, and individual behavior. Inj Prev. 2000;6(2):82–89. doi: 10.1136/ip.6.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burmpus N. What’s safe after your Covid-19 Vaccine? 2021. [accessed 2021 July 24].https://www.hopkinsmedicine.org/health/conditions-anddiseases/coronavirus/whats-safe-after-your-covid19-vaccine.
- 22.Daria S, Islam MR. The second wave of COVID-19 pandemic in Bangladesh: an urgent call to save lives. Asia-pacific J Public Health. 2021;33(5):665–66. doi: 10.1177/2F10105395211021686. [DOI] [PubMed] [Google Scholar]
- 23.Brewer NT, Cuite CL, Herrington JE, Weinstein ND. Risk compensation and vaccination: can getting vaccinated cause people to engage in risky behaviors? Ann Behav Med. 2007;34(1):95–99. doi: 10.1007/BF02879925. [DOI] [PubMed] [Google Scholar]
- 24.Reiber C, Shattuck EC, Fiore S, Alperin P, Davis V, Moore J. Change in human social behavior in response to a common vaccine. Ann Epidemiol. 2010;20(10):729–33. doi: 10.1016/j.annepidem.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Wise J. Covid-19: new coronavirus variant is identified in UK. BMJ. 2020;371:m4857. doi: 10.1136/bmj.m4857. [DOI] [PubMed] [Google Scholar]
- 26.Majeed A, Molokhia M. Vaccinating the UK against covid-19. BMJ. 2020;371:m4654. doi: 10.1136/bmj.m4654. [DOI] [PubMed] [Google Scholar]
- 27.Day M. Covid-19: stronger warnings are needed to curb socialising after vaccination, say doctors and behavioural scientists. BMJ. 2021;372:n783. doi: 10.1136/bmj.n783. [DOI] [PubMed] [Google Scholar]
- 28.Hossain ME, Rana MJ, Islam MS, Khan MA, Chakrobortty S, Ema NS, Bekun FV. COVID-19 vaccine-taking hesitancy among Bangladeshi people: knowledge, perceptions and attitude perspective. Hum Vaccin Immunother. 2021. doi: 10.1080/21645515.2021.1968215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ali M, Hossain A. What is the extent of COVID-19 vaccine hesitancy in Bangladesh?: a cross-sectional rapid national survey. BMJ Open. 2021;11(8):e050303. doi: 10.1136/bmjopen-2021-050303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalam MA, Davis TP, Shano S, Uddin N, Islam MA, Kanwagi R, Islam A, Hassan MM, Larson HJ. Exploring the behavioral determinants of COVID-19 vaccine acceptance among an urban population in Bangladesh: implications for behavior change interventions. PLoS One. 2021;16(8):e0256496. doi: 10.1371/journal.pone.0256496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haque MMA, Rahman ML, Hossian M, Matin KF, Nabi MH, Saha S, Hasan M, Manna RM, Barsha SY, Hasan SMR, et al. Acceptance of COVID-19 vaccine and its determinants: evidence from a large sample study in Bangladesh. Heliyon. 2021;7(6):e07376. doi: 10.1016/j.heliyon.2021.e07376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WHO . COVID-19 transmission and protective measures. World Health Organization; 2021. [accessed 2021 September 11]. https://www.who.int/westernpacific/emergencies/covid-19/information/transmission-protective-measures.
- 33.Bangladesh Election Commission . Election Commission Secretariat; 2021. [Accessed 2021 September 6]. http://www.ecs.gov.bd/?lang=en.
- 34.Suárez Álvarez J, Pedrosa I, Lozano LM, García Cueto E, Cuesta Izquierdo M, Muñiz Fernández J. Using reversed items in Likert scales: a questionable practice. Psicothema. 2018;30(2):149–58. doi: 10.7334/psicothema2018.33. [DOI] [PubMed] [Google Scholar]
- 35.Badu E, Owusu‐Manu DG, Edwards DJ, Adesi M, Lichtenstein S. Rural infrastructure development in the Volta region of Ghana: barriers and interventions. J Financ Manage Property Constr. 2013;18(2):142–59. doi: 10.1108/JFMPC-11-2012-0040. [DOI] [Google Scholar]
- 36.Kumar B, Pinky SD, Nurudden AM. Knowledge, attitude and practices towards COVID-19 guidelines among students in Bangladesh. Soc Sci Human Open. 2021;4:100194. doi: 10.1016/j.ssaho.2021.100194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muhwezi L, Acai J, Otim G. An assessment of the factors causing delays on building construction projects in Uganda. Int J Constr Eng Manage. 2014;3:13–23. [Google Scholar]
- 38.Rouhanizadeh B, Kermanshachi S. Barriers to an effective post-recovery process: a comparative analysis of the Public’s and experts’ perspectives. Int J Dis Risk Reduc. 2021;57:102181. doi: 10.1016/j.ijdrr.2021.102181. [DOI] [Google Scholar]
- 39.Fritz M, Berger PD. Chapter 11 - will anybody buy? Logistic regression. In: Fritz M, Berger PD, editors. Improving the user experience through practical data analytics, Morgan Kaufmann. 2015. p. 271–304. doi: 10.1016/B978-0-12-800635-1.00011-2. [DOI] [Google Scholar]
- 40.Doria-Rose N, Suthar MS, Makowski M, O’Connell S, McDermott AB, Flach B, Ledgerwood JE, Mascola JR, Graham BS, Lin BC, et al. Antibody persistence through 6 months after the second dose of mRNA-1273 vaccine for Covid-19. NEJM. 2021;384(23):2259–61. doi: 10.1056/NEJMc2103916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rahman FI, Ether SA, Islam MR. The “Delta Plus” COVID-19 variant has evolved to become the next potential variant of concern: mutation history and measures of prevention. J Basic Clin Physiol Pharmacol. 2021. doi: 10.1515/jbcpp-2021-0251. [DOI] [PubMed] [Google Scholar]
- 42.Los Angeles Daily News (LADS) . Studies say you are more likely to get Coronavirus from friends than strangers; 2020. [accessed 2021 September 11]. https://www.dailynews.com/2020/05/15/coronavirus-who-gave-you-covid-19-its-not-who-you-think/.
- 43.Mueller AL, McNamara MS, Sinclair DA. Why does COVID-19 disproportionately affect older people? Aging (Albany NY). 2020;12(10):9959. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly: ensuring sleep to promote a healthy brain and mind. J Psychosom Res. 2004;56(5):465–77. doi: 10.1016/j.jpsychores.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 45.Global Alliance for Vaccines and Immunization (GAVI) . Mounting evidence suggests COVID vaccines do reduce transmission. How does it work? 2021. [accessed 2021 September 10]. https://www.gavi.org/vaccineswork/mounting-evidence-suggests-covid-vaccines-do-reduce-transmission-how-does-work.
- 46.Rella SA, Kulikova YA, Dermitzakis ET, Kondrashov FA. Rates of SARS-CoV-2 transmission and vaccination impact the fate of vaccine-resistant strains. Sci Rep. 2021;11(1):1–10. doi: 10.1038/s41598-021-95025-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rahamim-Cohen D, Gazit S, Perez G, Nada B, Moshe SB, Mizrahi-Reuveni M, et al. Survey of behaviour attitudes towards preventive measures following COVID-19 vaccination. medRxiv. 2021. doi: 10.1101/2021.04.12.21255304. [DOI] [Google Scholar]
- 48.World Economic Forum (WEF) . How will behavior change after vaccination? New survey reveals post-pandemic trends; 2021. [accessed 2021 July 21]. https://www.weforum.org/agenda/2021/07/ipsos-behaviour-change-covid-vaccine/.
- 49.Wright L, Steptoe A, Mak HW, Fancourt D. Do people reduce compliance with COVID-19 guidelines following vaccination? A longitudinal analysis of matched UK adults. J Epidemiol Community Health. 2021:jech-2021-217179. doi: 10.1136/jech-2021-217179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.The Guardian . People are less likely to adhere to Covid rules after vaccination, expert says; 2020. [accessed 2021 July 25]. https://amp.theguardian.com/society/2021/feb/27/people-less-likely-adhere-covid-rules-after-vaccination.
- 51.Perez-Arce F, Angrisani M, Bennett D, Darling J, Kapteyn A, Thomas K. COVID-19 vaccines and mental distress. PloS One. 2021;16(9):e0256406. doi: 10.1371/journal.pone.0256406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Islam MR, Hossain MJ. Social stigma and suicide in Bangladesh: the Covid-19 has worsened the situation. Chronic Stress. 2020:5. doi: 10.1177/24705470211035602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.SPI-B . Possible impact of the COVID-19 vaccination programme on adherence to rules and guidance about personal protective behaviours aimed at preventing spread of the virus; 2021. [accessed 2021 September 5]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/950723/s0978-spi-b-possible-impact-covid-19-vaccination-programme-adherence-to-rules-guidance.pdf.
- 54.ReachOut Autralia . Technology and teenager; 2020. [accessed 2021 September 4]. https://parents.au.reachout.com/skills-to-build/wellbeing/technology-and-teenagers.
- 55.Ye B, Gao J, Fu H, Chen H, Dong W, Gu M. How does ageism influence frailty? A preliminary study using a structural equation model. BMC Geriatr. 2020;20(1):1–11. doi: 10.1186/s12877-020-01749-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Islam MR, Mia A. The role of education for rural population transformation in Bangladesh. Int J Work-Integr Learn. 2007;8:1. [Google Scholar]
- 57.Preeti HS, Naz S. Superstitious beliefs and happiness: a correlation study of young adults. Int J Econ Res. 2018;14:583–94. [Google Scholar]
- 58.Miller C, Purcell K, Mitchell A, Rosensteil T. How people get local news and information in different communities. Pew Research Center; 2012. [accessed 2021 September 13]. https://www.pewresearch.org/internet/2012/09/26/how-people-get-local-news-and-information-in-different-communities/.
- 59.Woolf HS, Aron L, Dubay L, Simon MS, Zimmerman E, Luk KX. How are income and wealth linked to health and longevity. Urban Institute; 2015. [accessed 2021 July 28]. https://www.urban.org/sites/default/files/publication/49116/2000178-How-are-Income-and-Wealth-Linked-to-Health-and-Longevity.pdf.
- 60.Ponthieux S, Meurs D. Gender inequality. In: Handbook of income distribution. Vol. 2. Elsevier; 2015. p. 981–1146. doi: 10.1016/B978-0-444-59428-0.00013-8. [DOI] [Google Scholar]
- 61.Rubin GJ, Brainard J, Hunter P, Michie S. Are people letting down their guard too soon after covid-19 vaccination? BMJ. 2021. https://ueaeprints.uea.ac.uk/id/eprint/79519. [Google Scholar]


