ABSTRACT
COVID-19 has caused severe financial, clinical, and sociological consequences besides posing a burden on healthcare. Many nutritional approaches have been employed to manage the deleterious consequences of COVID-19. Among the several micronutrients, vitamin D deprivation has been linked to an increased likelihood of hospitalization of COVID-19 patients. Vitamin D has been reported to be a critical regulator of the renin-angiotensin system, which is used by the SARS-CoV-2 to access the host cell. Vitamin D also modulates the multiple immune system mechanisms to contain the virus, including the curtailment of the viral entry into the host cell. The adequate levels of vitamin D in the host have been associated with the reduced release of proinflammatory cytokines, thus lowering the risk of a cytokine storm; increased levels of anti-inflammatory cytokines and enhanced secretion of natural antimicrobial peptides. It may also be involved in the enhancement of the Th2 immune response and activation of defensive cells such as macrophages. Contrary to these findings, several studies have concluded that there is no direct association between vitamin D concentrations and poor prognosis of the disease. Hence, this paper aims to decipher the immunoregulatory properties of vitamin D and its possible involvement in management of COVID-19.
KEYWORDS: COVID-19, SARS-CoV-2, vitamin D, immunomodulation, therapeutic
1. Introduction
Coronavirus disease 2019 (COVID-19) pandemic has resulted in more than 5.0 million fatalities globally, besides imposing strenuous challenges on health-care facilities and medical infrastructure.1,2 This scenario has instigated widespread panic, worldwide threats and financial losses.3,4 Currently, there are no authorized therapies for the management of COVID-19; hence, non-pharmaceutical interventions such as social distancing, public cleanliness, and facial masks remain the best available approaches for the mitigation of COVID-19. Recent research suggests that certain dietary supplements may be beneficial in COVID-19 patients. Higher-than-recommended daily dosages of nutrients such as vitamins and zinc may have a positive impact, perhaps decreasing the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral load and duration of hospitalization.5,6 These micronutrients have been reported to exhibit immunomodulatory activities and reduce the deleterious consequences of several ailments. On the other hand, imbalances in these nutrients can cause immunological dysfunction and increased vulnerability to pathogenic infections. Vitamin D deficiency has been reported in high-risk categories of COVID-19 patients, including the geriatric population, and might be associated with increased severity and mortality rates among this age group.7
Micronutrient deficiency has been linked to poor clinical outcomes during viral infections. To enhance the immune response and strengthen the defense against infections, malnourished individuals at risk of or diagnosed with COVID-19 may benefit from a daily intake of vitamins and trace elements. Recent research revealed the vitamin D, zinc, and selenium deficits in COVID-19 patients with acute respiratory tract infections. Vitamin D strengthens the physical barrier against viruses and promotes the synthesis of antimicrobial peptides. Moreover, vitamin D might have the potential to mitigate cytokine storms by reducing the secretion of proinflammatory cytokines8 (Figure 1).
Figure 1.
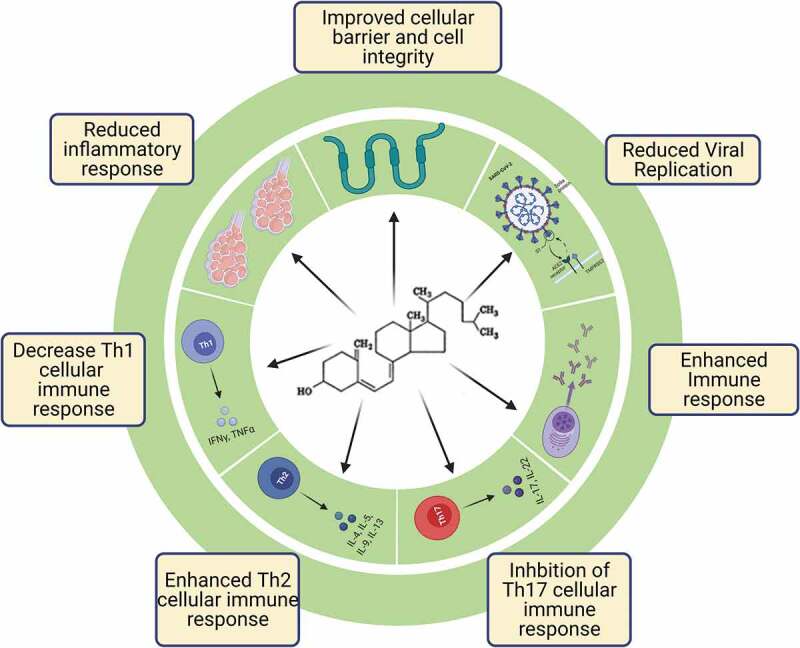
Comprehensive range of functions and benefits of vitamin D in lowering the risk of COVID-19. (The figure was created with BioRender.com).
To reduce the risk of infection, it is recommended that people at risk of influenza and COVID-19 should consider taking 10,000 IU/d of vitamin D3 for a few weeks to rapidly raise 25(OH)D concentrations, followed by 5000 IU/d. The goal should be to raise 25(OH)D concentrations above 40–60 ng/mL (100–150 nmol/L).7 Viral infections can be reduced by a number of ways involving vitamin D. One of these ways is the induction of cathelicidins and defensins, which can reduce viral replication rates as well as reduce inflammation that damages the lungs’ lining and causes pneumonia. Another way is raising the levels of anti-inflammatory cytokines.8,9 Although some observational research and clinical trials have found that taking vitamin D supplements can lower the chances of getting influenza, others have not found this to be true.10 Consequently, this review would focus on the different functions of vitamin D and its potential benefits in lowering the risk of COVID-19.
2. Immunomodulatory roles of vitamin D
One of the most well-known roles of vitamin D is to keep the calcium and phosphorus levels balanced in the body and to regulate bone metabolism. The deficiency of vitamin D is associated with increased inflammation and immune system dysregulation in several chronic diseases. Based on such findings, it appears that vitamin D plays a crucial role in regulating immunological function. Previously, it has been reported that the immune cells of both innate and adaptive immune systems, such as monocytes, macrophages, dendritic cells, B and T lymphocytes, express the vitamin D receptor (VDR). In another report, it has been suggested that vitamin D and VDR signaling has an anti-inflammatory impact by increasing the proliferation of regulatory T cells and dendritic cells and decreasing the response of T cells and the release of inflammatory cytokines. Acute respiratory distress syndrome (ARDS) caused by excessive secretion of proinflammatory cytokines may be the primary reason for the rise in death rates,11,12 and vitamin D can be employed to control the excessive release of cytokines.
Previous studies have revealed vitamin D’s immunomodulatory effects, and it has been found to affect the helper T cell responses. Vitamin D has been found to inhibit the Th1 immune responses13 while increasing the Th2 immunological response.14 Th1 cells generate proinflammatory cytokines like IFN-ɣ and TNF-β, whereas Th2 cells produce IL-4, IL-5, IL-10, and IL-13.15 Vitamin D lowers the Th1 cytokines while increasing the Th2 cytokines since it causes a shift from Th1 to Th2 phenotypes.16 The Th1 immune response has been found to be deleterious in the patients with COVID-19; hence, vitamin D can be employed to modulate the immune response and manage the COVID-19 patients.
In addition, several other recent reports have concluded that vitamin D can reduce the excessive release of cytokines in patients with COVID-19.17 The SARS-CoV-2 infection leads to endothelial and alveolar membrane damage, both of which can cause death, and vitamin D has been reported to prevent the endothelial damage by reducing the secretion of cytokines. Critically ill patients with COVID-19 are more likely to have elevated levels of proinflammatory cytokines such as IL-6 compared to those who have mild symptoms.8,18 Serum SARS-CoV-2 nucleic acid detection has been associated with elevated levels of IL-6 in severely sick COVID-19 patients.19 TNF-α, IL-6, IL-1, IL-12, and IFN-β production may be reduced by vitamin D.20–22 (Figure 2). Moreover, the inhibition of nuclear factor-kB (NF-kB) activation has been associated with the anti-inflammatory effects of vitamin D. Previous studies have recorded the interaction of vitamin D receptor with an inhibitor of kB (IkB) kinase beta, which in turn leads to the inhibition of NF-kB activation.22
Figure 2.
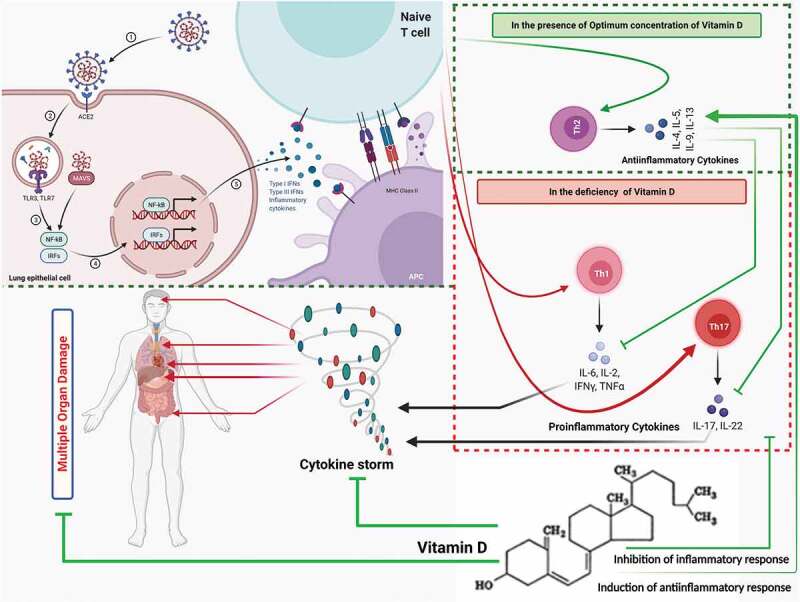
Schematic representation of immunomodulatory actions of Vitamin D. Vitamin D induces the proliferation of Th2 type cells and increases the production of anti-inflammatory cytokines such as IL-4, IL-5, IL-19, and IL-13. Further, anti-inflammatory cytokines inhibit the action of inflammatory cytokines such as IL-6, IL-2, TNF-α, and IFN-ɣ, which help control the excessive release of cytokines, also known as a cytokine storm. Moreover, in the deficiency of vitamin D the hyperactivation of Th1 and Th17 immune response has been postulated, which leads to cytokine storm. (The figure was created with BioRender.com).
Previously, the anti-inflammatory and immunomodulatory capabilities of vitamin D have been utilized in the treatment of type 2 diabetes. To reduce the virulence of SARS-CoV-2 and limit the illness progression, vitamin D has been proposed as an immunomodulation therapeutic approach. Researchers believe that vitamin D’s anti-inflammatory characteristics can help control the cytokine storm in COVID-19.23,24 In addition, recently, it has been concluded that vitamin D is an essential micronutrient that reduces the intensified inflammatory responses by decreasing the proinflammatory cytokines that cause ARDS.25–27
3. Vitamin D in the management of COVID-19
Several clinical studies have been conducted to establish the protective roles of vitamin D in the management of COVID-19. Recently, a study was conducted to check the correlation between vitamin D levels in various Asia Pacific countries and the morbidity and mortality rates of COVID-19. A significant relationship was found between the levels of this vitamin and the number of COVID-19 cases, which inturn indicates the protective role of vitamin D in COVID-19.28 Another study has shown that vitamin D deficiency could be associated with COVID-19 positivity and disease severity.29 An elevated level of this vitamin could decrease COVID-19 positivity, C-reactive protein (CRP) level, and the number of affected lung segments in patients with COVID-19, thereby shortening the duration of hospital stay. A study of six months duration conducted on the children with COVID-19, recorded significantly higher viral loads among patients with low vitamin D levels and lower BMI, which reflects the impact of nutritional status on the immune system.30 An investigation comparing the influence of a single high dose of vitamin D3 (200 000 IU) on the duration of hospital stay of patients with mild to extreme COVID-19 (N = 120) found no clinically significant variations among the groups examined in terms of duration of hospital stay, referral to ICU (intensive care unit), or requirement for artificial ventilation.31 In addition, researchers also suggest that vitamin D enhances the concentration of Angiotensin converting enzyme (ACE) and reduces the Angiotensin converting enzyme 2 (ACE2) expression, which may help to protect against the COVID-19. However, even while it is an intriguing theory, there is no clinical evidence to back it up just yet.32
According to some research, vitamin D supplementation may benefit patients with COVID-19, particularly those with a proven deficiency and other risk factors, including obesity, aging, dark skin tone, and geographical location.33 Researchers also believe that supplementing with 25(OH)D at levels above 50 ng/ml may help reduce the incidence and symptoms of viral diseases like COVID-19, along the lines of its protective effects in several other diseases like cardiovascular disease, diabetes, cancer, respiratory infections, and hypertension.33 COVID-19 infection risk has been found to be associated with the incidence of vitamin D insufficiency in an extensive Israeli observational population research involving 200 communities. Around 52,000 patients were included in this study, possibly the most extensive study to find the association of vitamin D and COVID-19. It has been concluded that there is a significantly strong link between low levels of vitamin D and an increased chance of acquiring COVID-19, with the risk being highest in those with a severe deficit.34 Moreover, several researchers have underlined the need for prophylactic usage of vitamin D in COVID-19 therapy.35,36 Hence, supplementation of vitamin D can be considered as one of the preventive measures to reduce the fatality rates among the risk-possessing population.
4. Conclusions and Future Perspectives
While the so-called COVID-19 pandemic grips the entire world, the lack of viable medicines necessitates intense study into drug repurposing. Notwithstanding the scarcity of reliable drug candidates against COVID-19, a strong link between vitamin D deficiency and severe viral infections, including COVID-19, suggests that a simple remedy could be helpful in the management of COVID-19. Furthermore, vitamin D’s possible involvement in regulating the immunological response to viral infections has bolstered its relevance in the present pandemic scenario. Considering the earlier work in the domain, there is a compelling case for investigating whether vitamin D can help prevent COVID-19. Along this line, several studies have established the protective roles of vitamin D in the management of patients with COVID-19, atleast in reducing the time of hospitalization and mortality rates. However, there is still inadequate data to substantiate a link between vitamin D levels, severity, and death associated with COVID-19. To address this question, randomized controlled trials and large-scale cohort studies are required. Experimental models should be applied in future research to deduce if vitamin D can inhibit viral replication, suppress proinflammatory cytokines, or have other impacts on SARS-CoV-2 pathogenesis. Extensive epidemiological studies may also be conducted to see if the vitamin D levels are linked to the chances of becoming infected with SARS-CoV-2 and the severity of accompanying illness.
Acknowledgments
All the authors acknowledge and thank their respective universities and institutes.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Authors’ contributions
MD did the ideation, conceptualization, data curation, writing original draft, reviewing and editing. PR executed the conceptualization, writing original draft, reviewing and editing. OPC did the reviewing and editing. All authors critically reviewed and approved the final version of the manuscript.
Ethical approval
This article does not require any human/ animal subjects to acquire such approval.
References
- 1.Rabaan AA, Al-Ahmed SH, Al Mutair A, Alhumaid S, Sule A, Tirupathi R, Fawzy M, Muhammad J, Khan A, Hasan A, et al. Immunopathogenesis and immunobiology of SARS-CoV-2. Infez Med. 2021;29:167–5. [PubMed] [Google Scholar]
- 2.Tareq AM, Emran TB, Dhama K, Dhawan M, Tallei TE.. Impact of SARS-CoV-2 delta variant (B.1.617.2) in surging second wave of COVID-19 and efficacy of vaccines in tackling the ongoing pandemic. Hum Vaccin Immunother. 2021:1–2. doi: 10.1080/21645515.2021.1963601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sreepadmanabh M, Sahu AK, Chande A. COVID-19: advances in diagnostic tools, treatment strategies, and vaccine development. J Biosci. 2020;45(1):148. doi: 10.1007/s12038-020-00114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dhawan M, Parmar M, Sharun K, Tiwari R, Bilal M, Dhama K. Medicinal and therapeutic potential of withanolides from Withania somnifera against COVID-19. J Appl Pharm Sci. 2021;11:006–013. [Google Scholar]
- 5.Shakoor H, Feehan J, Al Dhaheri AS, Ali HI, Platat C, Ismail LC, Apostolopoulos V, Stojanovska L. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: could they help against COVID-19? Maturitas. 2021;143:1–9. doi: 10.1016/j.maturitas.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients. 2020;12(1):236. doi: 10.3390/nu12010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JF, Bhattoa HP. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bae M, Kim H. Mini-review on the roles of vitamin C, vitamin D, and selenium in the immune system against COVID-19. Molecules. 2020;25(22):5346. doi: 10.3390/molecules25225346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hastie CE, Mackay DF, Ho F, Celis-Morales CA, Katikireddi SV, Niedzwiedz CL, Jani BD, Welsh P, Mair FS, Gray SR, et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr. 2020;14(4):561–65. doi: 10.1016/j.dsx.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skrajnowska D, Brumer M, Kankowska S, Matysek M, Miazio N, Bobrowska-Korczak B. Covid 19: diet composition and health. Nutrients. 2021;13(9):2980. doi: 10.3390/nu13092980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabaan AA, Al-Ahmed SH, Muhammad J, Khan A, Sule AA, Tirupathi R, Mutair AA, Alhumaid S, Al-Omari A, Dhawan M, et al. Role of inflammatory cytokines in COVID-19 patients: a review on molecular mechanisms, immune functions, immunopathology and immunomodulatory drugs to counter cytokine storm. Vaccines (Basel). 2021;9(5):436. doi: 10.3390/vaccines9050436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammad Zadeh N, Mashinchi Asl NS, Forouharnejad K, Ghadimi K, Parsa S, Mohammadi S, Omidi A. Mechanism and adverse effects of COVID-19 drugs: a basic review. Int J Physiol Pathophysiol Pharmacol. 2021;13:102–09. [PMC free article] [PubMed] [Google Scholar]
- 13.Lemire JM, Archer DC, Beck L, Spiegelberg HL. Immunosuppressive actions of 1,25-dihydroxyvitamin D3: preferential inhibition of Th1 functions. J Nutr. 1995;125(6 Suppl):1704S–1708S. doi: 10.1093/jn/125.suppl_6.1704S. [DOI] [PubMed] [Google Scholar]
- 14.Boonstra A, Barrat FJ, Crain C, Heath VL, Savelkoul HF, O’Garra A. 1alpha,25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T cells to enhance the development of Th2 cells. J Immunol. 2001;167(9):4974–80. doi: 10.4049/jimmunol.167.9.4974. [DOI] [PubMed] [Google Scholar]
- 15.Kaiko GE, Horvat JC, Beagley KW, Hansbro PM. Immunological decision-making: how does the immune system decide to mount a helper T-cell response? Immunol. 2008;123(3):326–38. doi: 10.1111/j.1365-2567.2007.02719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sloka S, Silva C, Wang J, Yong VW. Predominance of Th2 polarization by vitamin D through a STAT6-dependent mechanism. J Neuroinflammation. 2011;8:56. doi: 10.1186/1742-2094-8-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang Y, Liu J, Zhang D, Xu Z, Ji J, Wen C. Cytokine Storm in COVID-19: the Current Evidence and Treatment Strategies. Front Immunol. 2020;11:1708. doi: 10.3389/fimmu.2020.01708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu F, Zhu Y, Zhang J, Li Y, Peng Z. Intravenous high-dose vitamin C for the treatment of severe COVID-19: study protocol for a multicentre randomised controlled trial. BMJ Open. 2020;10(7):e039519. doi: 10.1136/bmjopen-2020-039519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen X, Zhao B, Qu Y, Chen Y, Xiong J, Feng Y, Men D, Huang Q, Liu Y, Yang B, et al. Detectable serum severe acute respiratory syndrome coronavirus 2 viral load (RNAemia) is closely correlated with drastically elevated interleukin 6 level in critically ill patients with coronavirus disease 2019. Clin Infect Dis. 2020;71(8):1937–42. doi: 10.1093/cid/ciaa449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khare D, Godbole NM, Pawar SD, Mohan V, Pandey G, Gupta S, Kumar D, Dhole TN, Godbole MM. Calcitriol [1, 25[OH]2 D3] pre- and post-treatment suppresses inflammatory response to influenza A (H1N1) infection in human lung A549 epithelial cells. Eur J Nutr. 2013;52(4):1405–15. doi: 10.1007/s00394-012-0449-7. [DOI] [PubMed] [Google Scholar]
- 21.Sharifi A, Vahedi H, Nedjat S, Rafiei H, Hosseinzadeh-Attar MJ. Effect of single-dose injection of vitamin D on immune cytokines in ulcerative colitis patients: a randomized placebo-controlled trial. APMIS. 2019;127(10):681–87. doi: 10.1111/apm.12982. [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, Zhang J, Ge X, Du J, Deb DK, Li YC. Vitamin D receptor inhibits nuclear factor κB activation by interacting with IκB kinase β protein. J Biol Chem. 2013;288(27):19450–58. doi: 10.1074/jbc.M113.467670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pinheiro MM, Fabbri A, Infante M. Cytokine storm modulation in COVID-19: a proposed role for vitamin D and DPP-4 inhibitor combination therapy (VIDPP-4i). Immunotherapy. 2021;13(9):753–65. doi: 10.2217/imt-2020-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients. Aging Clin Exp Res. 2020;32(10):2141–58. doi: 10.1007/s40520-020-01677-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tarazona-Santabalbina FJ, Cuadra L, Cancio JM, Carbonell FR, Garrote JMP, Casas-Herrero A, Martínez-Velilla N, Serra-Rexach A, Formiga F. VitaminD supplementation for the prevention and treatment of COVID-19: a position statement from the Spanish society of geriatrics and gerontology. Rev Esp Geriatr Gerontol. 2021;56(3):177–82. doi: 10.1016/j.regg.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. The possible role of Vitamin D in suppressing cytokine storm and associated mortality in COVID-19 patients. medRxiv. 2020. doi: 10.1101/2020.04.08.20058578. [DOI] [Google Scholar]
- 27.Xu Y, Baylink DJ, Chen CS, Reeves ME, Xiao J, Lacy C, Lau E, Cao H. The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19. J Transl Med. 2020;18(1):322. doi: 10.1186/s12967-020-02488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yadav D, Birdi A, Tomo S, Charan J, Bhardwaj P, Sharma P. Association of vitamin D status with COVID-19 infection and mortality in the Asia Pacific region: a cross-sectional study. Indian J Clin Biochem. 2021;36(4):492–97. doi: 10.1007/s12291-020-00950-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Demir M, Demir F, Aygun H. Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. J Med Virol. 2021;93(5):2992–99. doi: 10.1002/jmv.26832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Isoldi S, Mallardo S, Marcellino A, Bloise S, Dilillo A, Iorfida D, Testa A, Del Giudice E, Martucci V, Sanseviero M, et al. The comprehensive clinic, laboratory, and instrumental evaluation of children with COVID-19: a 6-months prospective study. J Med Virol. 2021;93(5):3122–32. doi: 10.1002/jmv.26871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murai IH, Fernandes AL, Sales LP, Pinto AJ, Goessler KF, Duran CSC, Silva CBR, Franco AS, Macedo MB, Dalmolin HHH, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19. JAMA-J Am Med Assoc. 2021;325:1053. doi: 10.1001/jama.2020.26848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA. Perspective: vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J Intern Med. 2021;289(1):97–115. doi: 10.1111/joim.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grant WB, Al Anouti F, Moukayed M. Targeted 25-hydroxyvitamin D concentration measurements and vitamin D3 supplementation can have important patient and public health benefits. Eur J Clin Nutr. 2020;74(3):366–76. doi: 10.1038/s41430-020-0564-0. [DOI] [PubMed] [Google Scholar]
- 34.Israel A, Cicurel AA, Feldhamer I, Dror Y, Giveon SM, Gillis D, Strich D, Lavie G. The link between vitamin D deficiency and Covid-19 in a large population. medRxiv. 2020. doi: 10.1101/2020.09.04.20188268. [DOI] [Google Scholar]
- 35.Wimalawansa SJ. Global epidemic of coronavirus-Covid-19: what can we do to minimize risks. European J Biomed Pharm Sci. 2020;7:432–38. [Google Scholar]
- 36.Kumar R, Rathi H, Haq A, Wimalawansa SJ, Sharma A. Putative roles of vitamin D in modulating immune response and immunopathology associated with COVID-19. Virus Res. 2021;292:198235. doi: 10.1016/j.virusres.2020.198235. [DOI] [PMC free article] [PubMed] [Google Scholar]


