Abstract
Objective
We evaluated the effects of mental health interventions among people hospitalized with COVID-19.
Methods
We conducted a systematic review and searched 9 databases (2 Chinese-language) from December 31, 2019 to June 28, 2021. Eligible randomized controlled trials assessed interventions among hospitalized COVID-19 patients that targeted mental health symptoms. Due to the poor quality of trials, we sought to verify accuracy of trial reports including results.
Results
We identified 47 randomized controlled trials from China (N = 42), Iran (N = 4) and Turkey (N = 1) of which 21 tested the efficacy of psychological interventions, 5 physical and breathing exercises, and 21 a combination of interventions. Trial information could only be verified for 3 trials of psychological interventions (cognitive behavioral, guided imagery, multicomponent online), and these were the only trials with low risk of bias on at least 4 of 7 domains. Results could not be pooled or interpreted with confidence due to the degree of poor reporting and trial quality, the frequency of what were deemed implausibly large effects, and heterogeneity.
Conclusion
Trials of interventions to address mental health in hospitalized COVID-19 patients, collectively, are not of sufficient quality to inform practice. Health care providers should refer to existing expert recommendations and standard hospital-based practices.
Registration: PROSPERO (CRD42020179703); registered on April 17, 2020.
Keywords: COVID-19, Interventions, Mental health, Randomized controlled trials, Systematic review
Abbreviations: ICU, intensive care unit; TIDieR, Template for Intervention Description and Replication; SMD, standardized mean difference; CI, confidence interval
1. Introduction
People infected with COVID-19, including those who have been hospitalized, are at risk for negative mental health outcomes [[1], [2], [3], [4], [5]]. In addition to stressors faced by anybody with a serious medical condition, including the risk of disability and death, people hospitalized due to COVID-19 may be at particular risk of poor mental health outcomes due to (1) limited social contact between healthcare workers and patients, (2) smaller health care worker to patient ratios, (3) families being excluded from intensive care units, (4) limited resources such as beds and mechanical ventilators, (5) long-term health sequelae of COVID-19, and (6) stigma and discrimination associated with being infected [[2], [3], [4], [5]]. Strategies for mental health management for people hospitalized due to COVID-19 are needed to reduce short- and long-term negative mental health outcomes.
Two previous systematic reviews have evaluated the effects of non-pharmacological interventions to reduce psychological distress among intensive care unit (ICU) patients, but both concluded that methodological limitations and risk of bias, small sample sizes, and heterogeneity in populations and approaches limited confidence in results [6,7]. Two systematic reviews [8,9] have sought to evaluate the effects of interventions on mental health among COVID-19 patients. One [8] searched through April 2020 and identified 16 studies but no randomized controlled trials [RCTs]. The other [9] searched for RCTs through July 2020, identified 5 (768 participants), and synthesized results quantitatively; however, low risk of bias ratings were applied to trials with major shortcomings, and results were pooled across highly heterogeneous interventions (muscle relaxation, respiratory rehabilitation, “life intervention”, traditional Chinese nursing, internet-based intervention), which reduced confidence in synthesized results.
We are conducting a series of living systematic reviews [10] of changes in mental health symptoms during COVID-19 and the effects of interventions designed to improve mental health during the pandemic [11,12]. Living systematic reviews are systematic reviews that are updated frequently and provide ongoing access to results as they become available [10]. They are logistically challenging but provide value beyond conventional systematic reviews in situations where (1) important decisions need to be made that merit the resources involved; (2) the certainty in existing evidence is low or very low, posing a barrier to decision-making; and (3) there is likely to be new research evidence emerging that would inform decisions [10].
The objective of the present sub-study was to synthesize evidence from RCTs on the effects of mental health interventions for people hospitalized with COVID-19 infection. Results from trials of interventions for people not quarantined or undergoing treatment due to COVID-19 infection have been reported elsewhere [13].
2. Method
Our systematic reviews on COVID-19 mental health [11,12] were registered (CRD 42020179703), and a protocol was posted (https://osf.io/96csg/) prior to initiation. Results are posted online as data are extracted (https://www.depressd.ca/research-question-3-intervention). This manuscript adheres to the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement [14].
2.1. Study eligibility
For trials to be included in the present review, all participants had to be enrolled after December 31, 2019, when China first reported on COVID-19 to the World Health Organization [15]. The population was restricted to patients receiving hospital-based care due to COVID-19 infection. Eligible interventions included any intervention described as designed primarily to address mental health symptoms from COVID-19. Trials that tested non-mental health interventions and primarily targeted non-mental health outcomes (e.g., exercise with primary outcome physical activity) were excluded. Eligible comparators included: (1) inactive control conditions (e.g., no treatment, waitlist) and (2) other eligible interventions. Eligible outcomes were defined broadly and included general mental health, mental health quality of life, anxiety symptoms, depression symptoms, stress, loneliness, anger, grief, burnout, and other emotional states. Eligible studies had to be RCTs that included at least 10 participants. There were no restrictions on language or publication format.
We did not include non-randomized studies because such studies are highly prone to bias when intervention and control groups are self-selected or there is no control group. Results from pre-post analyses of non-randomized studies without a control group are not possible to interpret unless there is a precise knowledge of the natural trajectory of symptoms or if one can safely assume that symptoms will not change over time without intervention. Even in normal times, however, this is not the case for mental health trials. Participants often seek mental health services and enrol in trials when they are experiencing high levels of symptoms, and regression to the mean is common [[16], [17], [18], [19], [20]]. Approximately 40% of participants assigned to placebo groups in drug trials or no-treatment groups in psychological intervention trials for major depression, for instance, achieve remission [21]. The Cochrane Collaboration discourages inclusion of evidence from non-randomized studies when conducting trials is feasible and when evidence from non-randomized trials is subject to these kinds of biases [22].
2.2. Search strategy
We searched MEDLINE (Ovid), PsycINFO (Ovid), CINAHL (EBSCO), EMBASE (Ovid), Web of Science Core Collection: Citation Indexes, China National Knowledge Infrastructure, Wanfang, medRxiv (preprints), and Open Science Framework Preprints (preprint server aggregator), using a search strategy designed and built by an experienced health sciences librarian. The China National Knowledge Infrastructure and Wanfang databases were searched using Chinese-language terms based on the English-language strategy. (See Appendix A).
An initial search was conducted from December 31, 2019 to April 13, 2020, then automated searches were set for daily updates. As of December 28, 2020, the automatic daily search updates were converted to weekly updates for feasibility. The present report includes trials from searches conducted up to June 28, 2021. We conducted a pre-submission study review up to searches done on February 14, 2022 to determine if any verified studies had been published since the main search date.
2.3. Selection of eligible studies
Search results were downloaded into the systematic review software DistillerSR (Evidence Partners, Ottawa, Canada) where duplicate references were identified and removed. Two reviewers independently screened titles and abstracts in random order to identify potentially eligible trials. If either reviewer deemed a study potentially eligible then a full-text review was conducted by two reviewers independently. Any disagreements at the full-text level were resolved through discussion and consensus, involving a third reviewer if necessary. An inclusion/exclusion coding guide was developed and pre-tested, and all team members were trained over several sessions. See Appendix B.
2.4. Data extraction
For each included RCT, one reviewer extracted data using a pre-specified standardized form in DistillerSR. A second reviewer validated the extracted data. Reviewers extracted (1) publication characteristics (e.g., first author, publication year, journal, funding source); (2) population characteristics and demographics (e.g., country, study eligibility criteria, number of participants, age, sex or gender, recruitment setting; (3) COVID-19 characteristics (e.g., severity); (4) intervention components, and (5) mental health outcomes. If sufficient information to calculate effect sizes was not provided, we attempted to obtain from authors.
We encountered many trials of unclear origin and funding, of very poor quality, and with effect sizes that exceeded plausibility. Thus, we emailed all included study authors twice (if no response to initial email) and requested that they verified the (1) authenticity of methods and results and (2) accuracy of our extracted outcomes. Authors of Chinese-language studies were contacted in both English and Chinese.
2.5. Assessment of risk of bias
We used the 2011 Cochrane Risk of Bias tool [23], which includes 7 domains that are rated as high risk, low risk, or unclear risk of bias. Two independent reviewers assessed each study independently; disagreements were resolved through discussion and consensus with a third reviewer consulted as necessary.
2.6. Assessment of reporting quality of trials
We used the Template for Intervention Description and Replication (TIDieR) checklist [24] to evaluate intervention reporting adequacy. The checklist is comprised of 12 items that assess reporting of intervention name; rationale for use of the intervention; materials used; intervention provider and background; delivery mode; location and necessary infrastructure; intervention frequency and duration; any tailoring; any modifications; if adherence or fidelity was assessed; and, if assessed, degree to which intervention was delivered as planned. TIDieR was done independently by two reviewers with consensus-based resolution of conflicts, including a third reviewer if necessary.
2.7. Data analysis
We calculated between-groups standardized mean difference (SMD) effect size for each outcome using Hedges' g with 95% confidence interval (CI) when possible. We did not pool results quantitatively in a meta-analysis due to substantial heterogeneity of populations, interventions, and outcomes and because of serious concerns about risk of bias.
2.8. Protocol amendments
Protocol amendments are shown in Appendix C.
3. Results
3.1. Search results
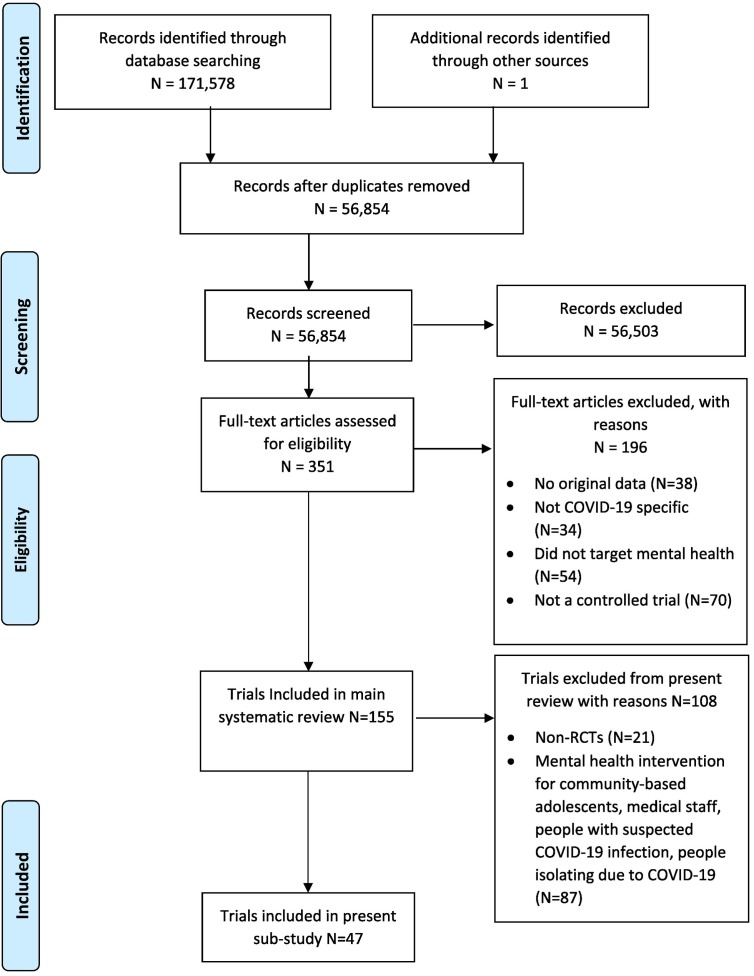
As of June 28, 2021, our search identified 56,854 unique titles and abstracts. Of these, 56,503 were excluded after title and abstract review and 196 at the full-text level, leaving 155 trials, of which 108 were excluded from the present sub-study because they were not RCTs (N = 21) or were not conducted with people infected with COVID-19 (N = 87), resulting in 47 [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71]] included RCTs. See Fig. 1 . Additional searches from the search date to February 14, 2022, did not include any eligible RCTs that were registered prior to enrolling participants, that were verified, or that were low risk of bias on at least 4 of 7 domains.
Fig. 1.
PRISMA flow diagram of study selection.
3.2. Characteristic of included trials
Of the 47 included RCTs, 42 were from China [25,[27], [28], [29], [30], [31], [32], [33], [34], [35], [36],[39], [40], [41], [42], [43], [44], [45], [46], [47],[49], [50], [51], [52], [53],[55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71]], 4 from Iran [26,37,38,54], and 1 from Turkey [48]. All were conducted in 2020 or did not report when conducted. One trial was registered prior to initiation but reported outcomes that differed from those registered [34], and 3 were registered retrospectively [31,37,38]. Contact information for trial authors was only included in publications for 21 trials [26,27,29,[31], [32], [33], [34],37,38,43,45,[47], [48], [49], [50],54,56,60,62,69,70], and only 3 of the 21 authors verified their results [31,37,38].
Participants in 46 trials [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53],[55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71]] were hospitalized; in the other trial [54], participants received emergency department care and were sent to home quarantine. Participants in only 4 trials were required to have mental health symptoms as part of inclusion criteria [30,34,43,60]. There were 21 trials [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45]] that tested psychological interventions, 5 [[46], [47], [48], [49], [50]] that tested breathing or physical exercise interventions, and 21 [[51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71]] that tested mixed interventions that combined different forms of psychological, exercise-based, or what were described as humanistic care interventions. Most comparators were standard care [25,28,[30], [31], [32], [33], [34], [35], [36], [37],[39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53],[55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71]], but two trials compared interventions to standard individual psychological care [26,29], one to an online ‘We Chat’ group where doctors answered patients' questions and provided psychotherapy [27], one to offering phone-based counselling [38], and one to COVID-19 education [54]. See Table 1 .
Table 1.
Characteristics of included trials.
| First author Dates Country Registration |
Verified | Setting | Participants | Intervention | Comparator | N Intervention/Comparator Analyzed | Outcome Domain(s) | Mean (SD) Age | % Female |
|---|---|---|---|---|---|---|---|---|---|
|
Psychological Interventions | |||||||||
| Ding [25] NR China NR |
No | Hospital isolation ward | COVID-19 patients with pneumonia | Multifaceted, including COVID-19 related education; relaxation techniques, and encouragement to use electronic devices to connect with family | Routine nursing | 31/31 | Anxiety, Depression | Range: 22–72 | 16 |
| Gharaati [26] 05–06/2020 Iran NR |
No | General hospital | COVID-19 patients | Crisis intervention package including 4 60-min psychotherapy sessions over 4 weeks focusing on empathy, adjustment, responsibility, and spirituality | Standard individual psychotherapy | 14/16 | Anxiety, Depression, Mental Health Function, Stress | Range: 18–65 | 53 |
| Gu [27] 01–02/2020 China NR |
No | Hospital isolation ward | COVID-19 patients able to use a video chat platform | Mindfulness-based stress reduction therapy 2 20–30-min sessions per week for 4 weeks | WeChat group where doctors answer patients' questions, assess their mental health, and provide therapy and health education | 33/30 | Anxiety, Depression | 41 (14) | 46 |
| Guo [28] 02–03/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms | Psychological nursing, including evaluation of psychological status, prevention of negative emotions, and encouragement of family support | Standard nursing | 30/30 | Anxiety, Depression | Intervention median 54 (3) Comparator median 53 (3) | 45 |
| Hui [29] 01–02/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms | 2× per day, 14-day psychological crisis intervention | 2× per day,14-day standard psychological care | 36/36 | Anxiety, Depression | 58 (8) | 46 |
| Jiang [30] 02–03/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms and anxiety or depression | Psychological care, including mindfulness therapy, health education, communication with patients, positive movies and soft songs | Standard nursing | 43/43 | Anxiety, Depression | NR | NR |
| Li J. [31] 02–03/2020 China ISRCTN68675756 |
Yes | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms with no previously diagnosed depression, current psychiatric medication, prior cognitive dysfunction or major stressful event | 30-min CBT in the morning daily for 4 weeks | Routine nursing | 47/46 | Anxiety, Depression, Stress | 48 (12) | 65 |
| Liu Ying [32] 03/2020-NR China NR |
No | General hospital | Patients hospitalized with mild COVID-19 infection | Group psychological intervention delivered via WeChat group and pulmonary rehabilitation exercises including five-tone breathing and Baduanjin exercises 30 min a day for 4 weeks | Standard COVID-19 treatment | 70/70 | Anxiety | <25 | 59 |
| Liu Yiwei [33] NR China NR |
No | Hospital isolation ward | Patients aged 18–60 with mild COVID-19 infection; no cognitive dysfunction, mental or psychiatric disorder; no severe underlying diseases | 90–120 min daily art therapy for 10 days | Standard nursing | 25/25 | Anxiety, Depression, Mental Health Function | 44 (9) | 42 |
| Liu Z [34]. NR China ChiCTR2000030084 |
No | General hospital isolation ward | Patients with mild or common type COVID-19, mild to moderate depressive or anxiety symptoms (HAMD17 or HAMA ≥7, HAMD <24, HAMA <21), no psychiatric diagnosis in last 6 months, no psychotic symptoms, no high risk of suicide, no organic mental disorders, no substance abuse or dependence, no current treatment for mental health problems | Self-directed computerized cognitive behavioral therapy (cCBT) 10 min per day for 1 week | Treatment as usual including periodic psychological assessment, general psychological support, and discussion of overall well-being and disease activity. | 126/126 | Anxiety, Depression | 43 (13) | 40 |
| Pan H. [35] 01–03/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with severe COVID-19 symptoms | Routine care plus non-specific psychological interventions tailored to patient presentation: (1) for panic, assign more experienced nursing staff; (2) for dysphoria, emphasize being patient and sympathetic; (3) for depression: analyze origin of pessimistic mood and target communication | Routine care | 30/30 | Anxiety, Depression, Mental Health Function | NR | 45 |
| Pan R. [36] 01–04/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms | Psychological nursing, including building comfortable environment, stabilizing mood, educating patients about COVID-19 knowledge, and alleviating negative affect | Standard nursing | 16/16 | Anxiety, Depression | 53 (6) | 44 |
| Parizad [37] NR Iran IRCT20131112015390N5 |
Yes | General Hospital | COVID-19 patients with an oxygen saturation > 90%, no severe visual or auditory disorders, no mental disorders | 25 min guided imagery sessions 2× per day for 5 consecutive days | Routine care | 55/55 | Anxiety | 40 (12) | 44 |
| Shaygan [38] NR Iran IRCT20201001048893N1 |
Yes | General hospital | Mild to severely infected COVID-19 patients with no previous experience of quarantine and no history of psychiatric disorders or taking psychiatric medications. | Online multifaceted multimedia psycho-educational intervention, 1 60-min module per day for 14 days | Offer to receive telephone-based counselling if needed | 26/22 | Mental Health Function, Stress | 37 (12) | 44 |
| Shi Q. [39] 01–03/2020 China NR |
No | COVID-19 hospital isolation ward | People hospitalized with mild COVID-19 symptoms | Daily psychoeducation focused on emotional regulation; psychological assessment of patients on the 1st, 7th and 14th day after admission; daily traditional Chinese medicine emotional therapy and corresponding diet therapy | Standard nursing care | 30/30 | Anxiety, Depression | 34 (3) | 48 |
| Shi Y. [40] 01–04/2020 China NR |
No | General hospital intensive care unit | Hospitalized in intensive care with COVID-19 infection; have no pre-existing mental disorders, insomnia, or severe comorbidity | Psychological care, including COVID-19 information and relaxation support | Standard care | 30/30 | Anxiety | 52 (10) | 45 |
| Wang M. [41] NR China NR |
No | University hospital | Patients hospitalized with severe COVID-19, no recent major life events, no malignant tumor, no prior psychiatric disorder or anti-depressant use | Standard nursing plus daily 20–30 min psychological intervention including empathic listening, transposition thinking, information organizing, and feedback exchanging | Standard nursing | 20/20 | Anxiety, Depression | 46 (7) | 45 |
| Wang Y. [42] 02–03/2020 China NR |
No | COVID-19 treatment hospital | Hospitalized COVID-19 patients | Routine nursing plus multifaceted psychological intervention, including providing patients and their families with COVID-19 information, teaching patients relaxation and psychological regulation techniques for 14 days | Routine nursing | 39/39 | Anxiety, Depression | 57 (4) | 47 |
| Wei [43] 02/2020 China NR |
No | University hospital | COVID-19 patients with PHQ-9 or GAD-7 of ≥5 and < 15, at least a junior middle school level of education, no suicidal ideation, and no antipsychotic use. | Self-help multifaceted internet-based intervention including mindfulness techniques, relaxation training, “refuge” skills, and butterfly hug method with instructions to do 50 min daily for 2 weeks | Daily supportive care | 26/22 | Anxiety, Depression | 45 (12) | 38 |
| Zhang A. [44] NR China NR |
No | General hospital | Patients with mild and ordinary COVID-19, no cognitive disorders. | Routine treatment plus traditional Chinese medicine prescription for pneumonia and shared decision-making psychological counselling | Routine treatment | 106/100 | Anxiety | 36 (5) | 42 |
| Zhu L [45] NR China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms and no psychiatric disorder | Standard nursing plus 5–6 15–30 min individualized daily acceptance and commitment therapy (ACT) sessions | Standard nursing | 46/46 | Anxiety, Depression | Intervention 65 (NR) Comparator 67 (NR) | 45 |
|
Physical/Breathing Exercise Interventions | |||||||||
| Chen X. [46] 02–03/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms | 3-week Baduanjin exercise, 10 times per week, 2 times per day | Standard care | 14/15 | Anxiety, Depression | 69 (11) | 55 |
| Liu K. [47] 01–02/2020 China NR |
No | Hospital Isolation ward | Patients with confirmed COVID-19 | Progressive muscle relaxation and deep breathing 20–30 min per day for 5 consecutive days | Standard care | 25/26 | Anxiety | 50 (13) | 45 |
| Özlü [48] 05–08/2020 Turkey NR |
No | General hospital COVID-19 clinic |
Adult COVID-19 patients receiving treatment | 20–30 min progressive muscle relaxation exercises delivered on TV via CD twice a day for 5 days | Routine care | 33/34 | Anxiety | 35 (12) | 45 |
| Zhang Y. [49] 02–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms | Multifaceted, including Fitness Qigong group training 3 days a week, twice a day in 60 min sessions; Chinese medicine and nursing from 4 pm–5 pm daily; ear acupoint bean-pressing: 10–15 times a day for 3–5 min | Routine nursing | 14/14 | Anxiety, Depression | 50 (4) | 39 |
| Zhu [50] 02–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms | One-on-one health education for 9 days including medication guidance and monitoring vital signs plus breathing exercises twice daily | Standard nursing | 40/40 | Anxiety, Depression | 36 (12) | 43 |
|
Mixed Interventions | |||||||||
| Cai [51] NR China NR |
No | COVID-19 hospital | Mildly infected or ordinary type COVID-19 patients with no severe underlying diseases | Multifaceted intervention, including COVID-19 education, psychological intervention targeted at alleviating patients' negative emotions; nutrition guidance; and exercise | Standard nursing | 30/30 | Anxiety, Depression | 43 (12) | 45 |
| Cao [52] 01–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Severely infected COVID-19 patients not on ventilators aged 41–79 | Humanistic nursing including nutrition plan, individualized pulmonary recovery plan, and attending to patients' emotions | Standard care | 68/68 | Anxiety, Depression | 60 (12) | 29 |
| Cha [53] 01–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms | Systematic nursing, including psychological nursing to alleviate patients' negative emotions; rehabilitation training to enhance immune system; increasing ward rounds to monitor changes in patients' symptoms; and nutrition guidance | Routine nursing | 50/50 | Anxiety, Depression | 45 (6) | 48 |
| Chakeri [54] NR Iran NR |
No | Emergency department | People given a definitive diagnosis of COVID-19 and prescribed home quarantine, medication, and continued treatment at home | Information about COVID-19 symptoms and methods of preventing transmission plus tele-nursing counselling for 3 weeks every other day | Information about COVID-19 symptoms and methods of preventing transmission | 50/50 | Anxiety | 43 (9) | NR |
| Chen Y. [55] NR China NR |
No | COVID-19 treatment hospital | Patients with mild COVID-19 symptoms | Standard nursing plus humanized nursing (psychological care; health education; relaxation training therapy) | Standard nursing | 40/40 | Anxiety | NR | NR |
| Deng [56] NR China NR |
No | COVID-19 treatment hospital isolation ward | Mild to moderate COVID-19 infected patients with no other underlying diseases | Standard psychological nursing plus personalized psychological nursing and peer-support group including online psychological counselling 4× over 2 weeks | Standard psychological nursing including education about COVID-19 | 30/30 | Anxiety, Depression | NR | 45 |
| Dong [57] 02–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms | Routine nursing plus humanistic care, including sanitary improvement of the ward; educating patients on COVID-19; and using verbal encouragement to decrease patients' anxiety and loneliness; encouraging them to communicate with their families via telephone and video | Routine nursing | 46/46 | Anxiety, Mental Health Function | 42 (8) | 45 |
| Fan [58] 01–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms | Systematic nursing, including psychological nursing to alleviate patients' negative emotions; rehabilitation training to enhance immune system; increasing ward rounds to monitor changes in patients' symptoms; and nutrition guidance | Routine nursing | 50/50 | Anxiety, Depression | 45 (6) | 48 |
| Huang [59] NR China NR |
No | Traditional Chinese hospital | Patients hospitalized with COVID-19 infection | Health education and psychological nursing during and after treatment focusing on eliminating patients' negative affect | Standard nursing | 37/36 | Anxiety, Depression | 56 (NR) | 53 |
| Li Lan [60] NR China NR |
No | COVID-19 hospital | Adult patients of light or ordinary type COVID-19, with a score of HAMD ≥8 or SAS ≥50, no severe somatic diseases | Five Elements Music therapy, Six Words Formula therapy (breathing exercise) and psychological nursing twice daily for 2 weeks; practicing Six Words Formula therapy while listening to music | Routine psychological nursing focusing on encouraging patients to express their emotions, educating on COVID-19, facilitating family support, and performing abdominal breathing | 30/30 | Anxiety, Depression | 45 (14) | 48 |
| Li Li [61] 01–04/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with mild COVID-19 symptoms | High quality nursing including psychological and dietary intervention | Standard care | 58/57 | Anxiety, Depression, Mental Health Function | 54 (3) | 47 |
| Liu Q. [62] NR China NR |
No | COVID-19 treatment hospital isolation ward | COVID-19 patients with blood oxygen saturation > 93% and breathing rate less than 24/min; with no psychiatric disorder or other comorbidity | Standard nursing plus psychological nursing and humanistic nursing focusing on monitoring and stabilizing patients' affect and helping them accept their negative emotions | Standard nursing | 22/22 | Anxiety, Depression | 49 (3) | 52 |
| Liu R. [63] 02–03/2020 China NR |
No | COVID-19 treatment hospital | Patients with mild COVID-19 symptoms | Individualized psychotherapy plus group music therapy and physical exercise over 4 weeks | Standard care | 75/75 | Anxiety, Depression | 52 (7) | 59 |
| Lu [64] 01–05/2020 China NR |
No | General Hospital | Hospitalized COVID-19 patients | quality care including monitoring vital signs every 30 min; psychological care focusing on decreasing patients' negative affect and increasing treatment compliance; high-protein-high-energy liquid diets with no more than 200 ml per day; and close monitoring of signs of fever | Routine care | 60/60 | Anxiety, Depression, Mental Health Function | 55 (4) | 48 |
| Ma [65] 02–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Patients with COVID-19 symptoms | Standard nursing plus improving ward environment and individualized humanistic intervention focusing on alleviating patients' negative affect | Standard care | 130/130 | Depression | 64 (NR) | 42 |
| Nie [66] 02–03/2020 China NR |
No | COVID-19 treatment hospital isolation ward | Severely infected COVID-19 patients | Humanistic care including paying attention to negative emotions, providing proper diet, educating on COVID-19 and protecting patients' privacy for 4 weeks | Standard intensive care | 15/15 | Anxiety | 36 (6) | 43 |
| Xu [67] 02–04/2020 China NR |
No | General Hospital | Patients with mild symptoms of COVID-19 | Routine nursing plus humanistic care focusing on improving patients' negative emotions, providing a comfortable ward environment, psychological care targeting patients' needs, and spiritual support through reminding patients of their families | Routine nursing | 40/40 | Anxiety, Depression | 60 (7) | 43 |
| Yang [68] NR China NR |
No | COVID-19 hospital | Patients with mild COVID-19 infection, no severe cardiac, hepatic, or renal functional diseases, and no severe neurological diseases | Traditional Chinese medicine syndrome differentiation nursing methods lasting for 1 month and acupoint massage, lasting 2 min per acupoint 2–3 times daily | Routine nursing | 44/44 | Anxiety, Depression | 49 (0) | 33 |
| Zhang Y. [69] 01–02/2020 China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 symptoms with no serious complications | Personalized guidance including watching educational videos and discussing effective plans every other day; 30–60 min per session, 1 session every two days for 10 days | Standard nursing | 12/12 | Anxiety | 46 (3) | 46 |
| Zheng C. [70] NR China NR |
No | COVID-19 hospital | Patients with no history of psychiatric disorder or severe cognitive disorder | Traditional health education plus “Atlas Menu” health education including presenting knowledge about what patients would encounter during their hospital stay in a menu-like pattern with images for patients' study on their own | Traditional health education at different stages of hospitalization including psychological nursing and safety risk-related information delivered once every 3–5 days | 56/56 | Anxiety, Depression | 59 (6) | 54 |
| Zheng Y. [71] NR China NR |
No | COVID-19 hospital isolation ward | Patients with mild COVID-19 infection, no mental disorder history, recent trauma, or psychiatric disorder. | Humanistic care based on Traditional Chinese Medicine, including cognitive intervention aimed at helping patients build correct cognitions about COVID-19, behavioral intervention aimed at instructing patients on exercises, music intervention to calm patients, and auricular massage intervention 3–5 times per day, 30s per session | Routine care | 30/30 | Anxiety, Depression | 63 (4) | 52 |
3.3. Psychological interventions
The number of participants in 21 psychological intervention trials [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45]] ranged from 14 to 126 (mean = 83.7; standard deviation [SD] = 58.7; median = 60). The percentage of female participants ranged from 16% to 65%, and mean age ranged from 34 to 66 years. There were 11 trials that tested a psychological therapy [26,27,[29], [30], [31],33,34,37,39,44,45] (acceptance and commitment therapy, cognitive behavioral therapy, mindfulness therapy, mixed approach); 4 that tested multifaceted interventions with components that included psychoeducation, stress management and relaxation techniques with an online component [25,32,38,43]; and 6 that tested psychological nursing with relaxation and empathic listening components [28,35,36,[40], [41], [42]].
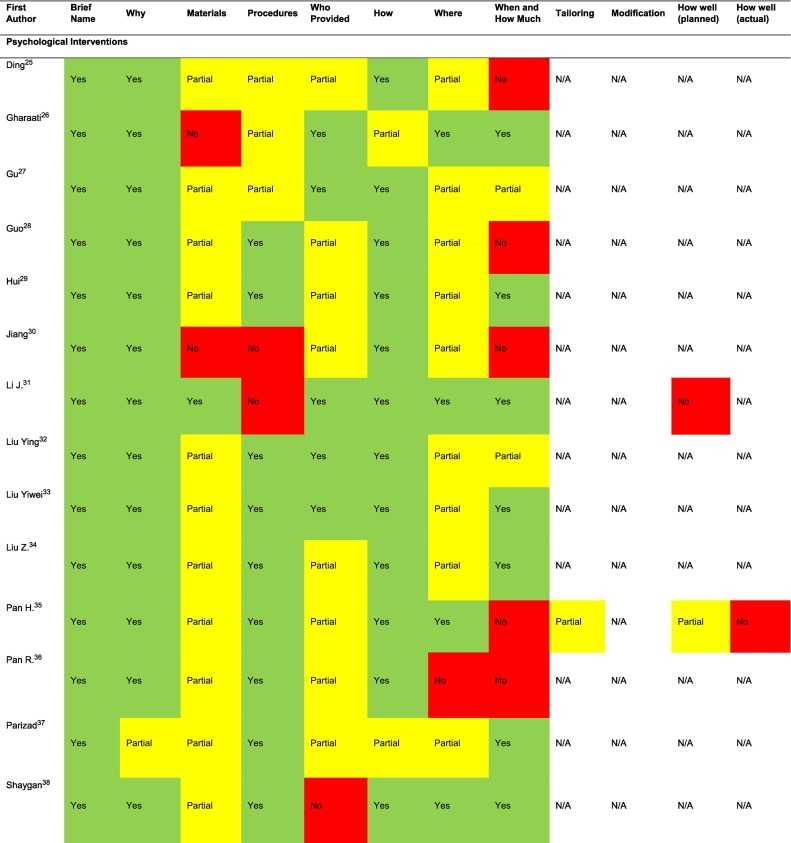
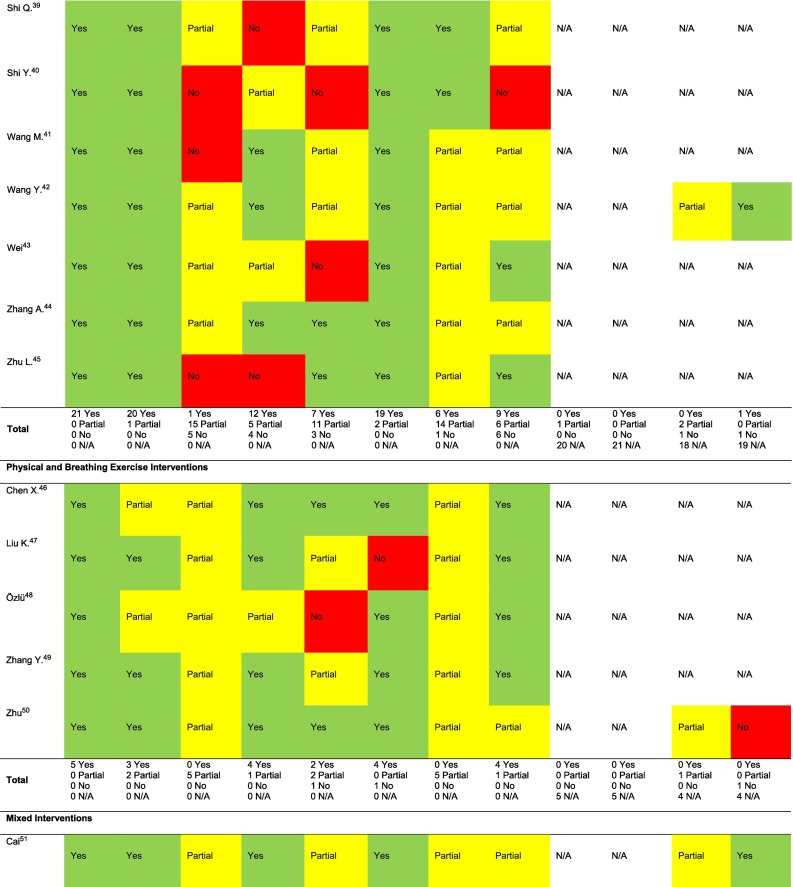
3.3.1. Verification, intervention reporting, risk of bias
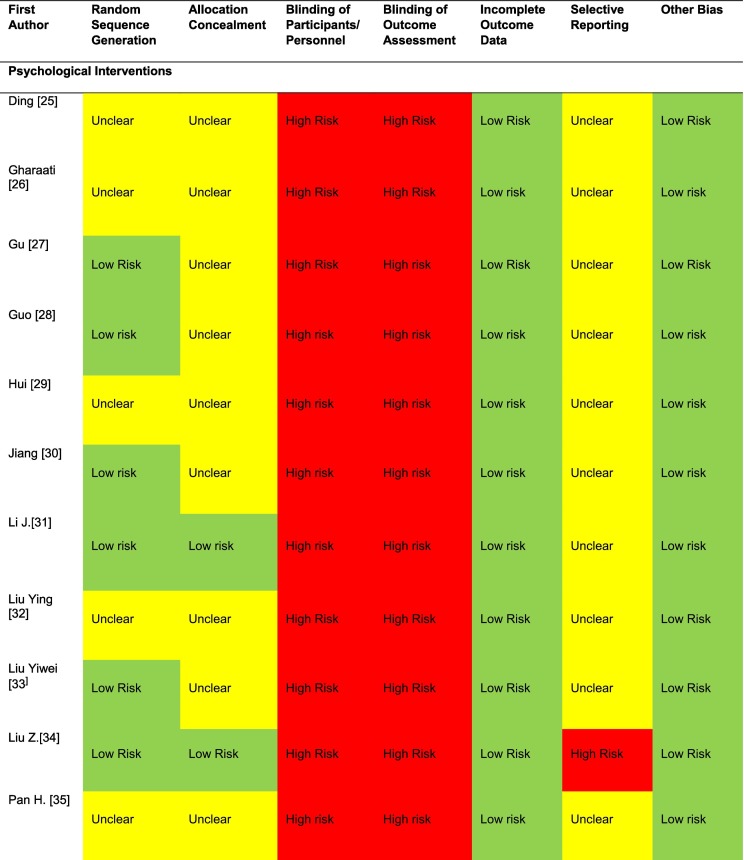
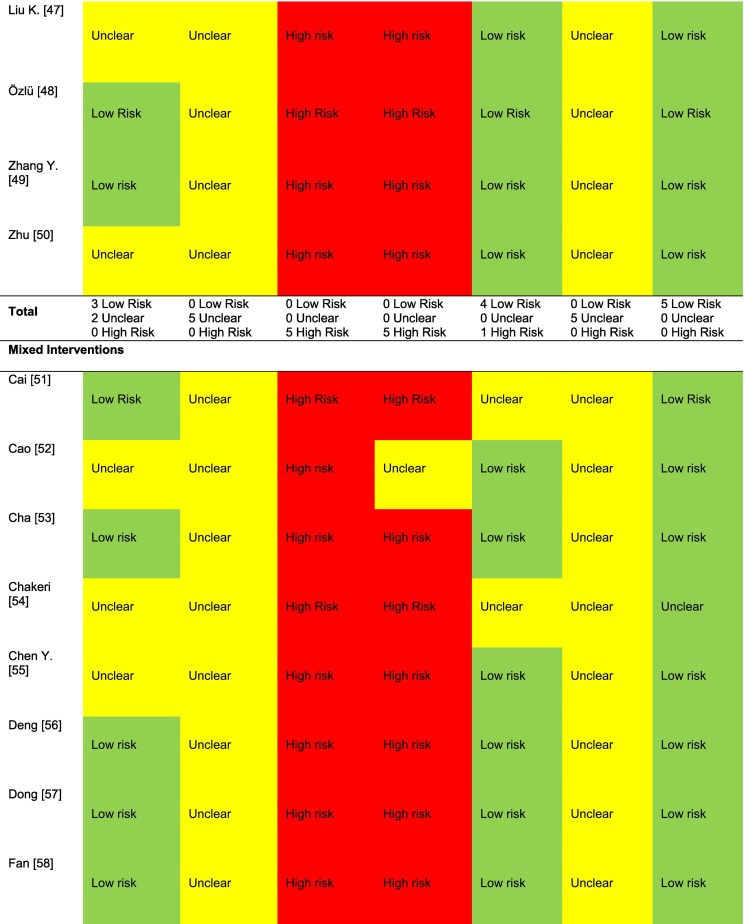
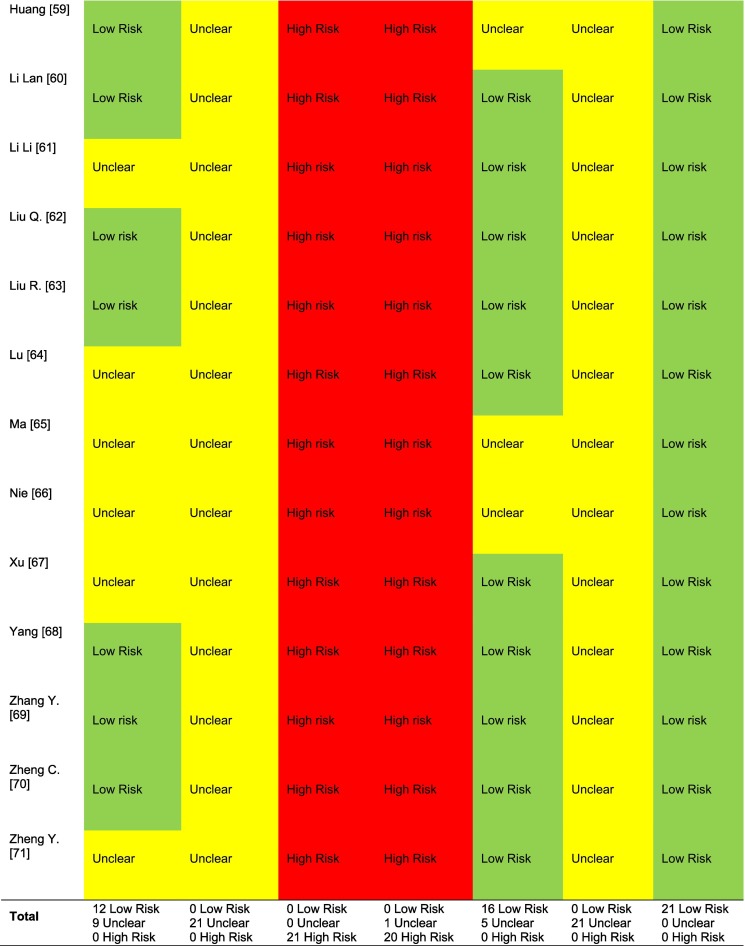
Out of the 21 trials, only 3 verified their results [31,37,38]. Few trials reported interventions in sufficient detail to fully understand what had occurred. Of the 8 main domains in the TIDieR checklist (4 additional domains were not applicable for most studies), all trials had 1–5 partially or not reported (median = 4). The number of trials that adequately reported was 21 (100%) for intervention name, 20 (95%) for rationale, 1 (5%) for materials used, 12 (57%) for procedures, 7 (33%) for provider, 19 (90%) for how administered, 6 (29%) for where administered, and 9 (43%) for when and how much provided. See Appendix D. Risk of bias was unclear or high in 20 of the 21 trials for blinding of participants and personnel and blinding of outcome assessment [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37],[39], [40], [41], [42], [43], [44], [45]], in 5 trials for random sequence generation [25,26,29,32,35], in 17 trials [[25], [26], [27], [28], [29], [30],32,33,35,36,[39], [40], [41], [42], [43], [44], [45]] for allocation concealment, in one trial for incomplete outcome data [43], and in all 21 trials for selective reporting as none were adequately registered pre-trial [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45]]. Excluding the “other bias” domain, the median number of the other 6 domains rated as unclear or high risk was 3. There were 3 trials [31,37,38], the same trials that were verified, that were rated as low risk on at least 4 domains and not high risk on any domains other than blinding. See Table 2 .
Table 2.
Risk of bias for included RCTs.
3.3.2. Outcomes
Of the 21 trials, 20 reported anxiety symptoms [[25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37],[39], [40], [41], [42], [43], [44], [45]], 15 depression symptoms [[25], [26], [27], [28], [29], [30], [31],[33], [34], [35], [36],39,[41], [42], [43],45], 4 general mental health function [26,33,35,38], and 3 stress outcomes [26,31,38]. Hedges' g ranged from 0.24 to 17.87 for anxiety symptoms, 0.04 to19.61 for depression symptoms, 0.16 to 1.47 for mental health function, and 0.10 to 1.25 for stress. See Table 3 .
Table 3.
Outcomes of included trials.⁎
| First author | Anxiety |
Depression |
Mental Health Function |
Stress |
||||
|---|---|---|---|---|---|---|---|---|
| Measure | Hedges' g (95% CI) | Measure | Hedges' g (95% CI) | Measure | Hedges' g (95% CI) | Measure | Hedges' g (95% CI) | |
| Psychological Interventions | ||||||||
| Ding [25] | ZSAS | 7.00 (5.66, 8.34) | ZSDS | 4.89 (3.89, 5.89) | – | – | – | – |
| Gharaati [26] | DASS-21 | 0.76 (−0.00, 1.51) | DASS-21 | 1.07 (0.29, 1.85) | SCL-25 WHO-QOL |
0.42 (−0.32, 1.16) 0.16 (−0.57, 0.89) |
DASS-21 | 1.25 (0.45, −2.04) |
| Gu [27] | ZSAS | 0.72 (0.21, 1.24) | ZSDS | 0.63 (0.12, 1.14) | – | – | – | – |
| Guo [28] | ZSAS | 0.91 (0.37, 1.44) | ZSDS | 0.87 (0.33, 1.40) | – | – | – | – |
| Hui [29] | ZSAS | 3.50 (2.76, 4.23) | ZSDS | 2.40 (1.79, 3.01) | – | – | – | – |
| Jiang [30] | HAM-A | 7.60 (6.38, 8.82) | HAM-D | 7.90 (6.64, 9.17) | – | – | – | – |
| Li J. [31] | DASS-21 | 0.24 (−0.17, 0.65) | DASS-21 | 0.04 (−0.37, 0.45) | – | – | DASS-21 | 0.10 (−0.51, 0.31) |
| Liu Ying [32] | STAI (State) |
0.61 (0.27, 0.95) | – | – | – | – | – | – |
| Liu Yiwei [33] | GAD-7 | 1.70 (1.05, 2.36) | PHQ-9 | 1.70 (1.05, 2.36) | WHOQOL-BREF | 0.70 (0.12, 1.27) | – | – |
| Liu Z [34]. | HAM-A ZSAS |
1.70 (1.41, 1.99) 1.91 (1.61, 2.21) |
HAM-D ZSDS |
1.95 (1.65, 2.25) 1.79 (1.50, 2.09) |
– | – | – | – |
| Pan H. [35] | ZSAS | 4.06 (3.17, 4.96) | ZSDS | 3.33 (2.54, 4.12) | SF-36 | 1.47 (0.90, 2.05) | – | – |
| Pan R. [36] | ZSAS | 17.87 (13.37, 22.38) | ZSDS | 19.61 (14.68, 24.55) | – | – | – | – |
| Parizad [37] | STAI (State) STAI (Trait) |
0.72 (0.34, 1.11) 0.56 (0.18, 0.94) |
– | – | – | – | – | – |
| Shaygan [38] | – | – | – | – | CD-RISC | 0.49 (−0.09, 1.08) | PSS | 0.76 (0.17, 1.35) |
| Shi Q. [39] | ZSAS | 0.39 (−0.12, 0.91) | ZSDS | 2.51 (1.83, 3.19) | – | – | – | – |
| Shi Y. [40] | ZSAS | 0.89 (0.36, 1.43) | – | – | – | – | – | – |
| Wang M. [41] | HAM-A SCL-90 |
0.69 (0.04, 1.33) 1.18 (0.50, 1.86) |
HAM-D SCL-90 |
0.68 (0.04, 1.33) 1.08 (0.41, 1.75) |
– | – | – | – |
| Wang Y. [42] | HAM-A | 2.30 (1.73, 2.88) | HAM-D | 1.90 (1.36, 2.44) | – | – | – | – |
| Wei [43] | HAM-A | 0.93 (0.03, 1.84) | HAM-D | 0.98 (0.07, 1.89) | – | – | – | – |
| Zhang A. [44] | ZSAS | 1.00 (0.71, 1.29) | – | – | – | – | – | – |
| Zhu L. [45] | ZSAS | 0.41 (−0.01, 0.82) | ZSDS | 0.57 (0.15, 0.98) | – | – | – | – |
| Physical/ Breathing Exercise Interventions | ||||||||
| Chen X. [46] | ZSAS | 2.92 (1.85, 3.98) | ZSDS | 2.53 (1.54, 3.53) | – | – | – | – |
| Liu K. [47] | STAI | 1.09 (0.50, 1.67) | – | – | – | – | – | – |
| Özlü [48] | STAI (State) STAI (Trait) |
2.41 (1.78, 3.04) −0.40 (−0.89, 0.09) |
– | – | – | – | – | – |
| Zhang Y. [49] | ZSAS | 1.04 (0.23, 1.84) | ZSDS | 0.78 (0.00, 1.56) | – | – | – | – |
| Zhu [50] | ZSAS | 4.06 (3.28, 4.83) | ZSDS | 2.99 (2.35, 3.63) | – | – | – | – |
| Mixed Interventions | ||||||||
| Cai [51] | HAM-A | 1.81 (1.21, 2.42) | HAM-D | 2.50 (1.81, 3.18) | – | – | – | – |
| Cao [52] | HAM-A | 1.29 (0.92, 1.66) | HAM-D | 0.95 (0.59, 1.30) | – | – | – | – |
| Cha [53] | ZSAS | 3.48 (2.48, 4.47) | ZSDS | 0.99 (0.33, 1.66) | – | – | – | – |
| Chakeri [54] | STAI (State) | 3.05 (2.47, 3.63) | – | – | – | – | – | – |
| Chen Y. [55] | ZSAS | 0.45 (0.00, 0.89) | – | – | – | – | – | – |
| Deng [56] | ZSAS | 1.20 (0.64, 1.75) | ZSDS | 3.44 (2.64, 4.24) | – | – | – | – |
| Dong [57] | HAM-A | 1.61 (1.14, 2.09) | – | – | SF-36 | 1.76 (1.28, 2.25) | – | – |
| Fan [58] | ZSAS | 2.82 (2.26, 3.37) | ZSDS | 1.94 (1.46, 2.42) | – | – | – | – |
| Huang [59] | ZSAS | 6.74 (5.54, 7.93) | ZSDS | 2.72 (2.08, 3.36) | – | – | – | – |
| Li Lan [60] | ZSAS | 8.14 (6.58, 9.69) | HAM-D | 9.25 (7.50, 10.99) | – | – | – | – |
| Li Li [61] | ZSAS | 0.91 (0.53, 1.30) | ZSDS | 0.87 (0.49, 1.26) | SF-36 | 2.28 (1.81, 2.76) | – | – |
| Liu Q. [62] | ZSAS | 4.00 (3.44, 4.56) | ZSDS | 3.43 (2.93, 3.93) | – | – | – | – |
| Liu R. [63] | ZSAS | 2.12 (1.38, 2.87) | ZSDS | 3.15 (2.25, 4.04) | – | – | – | – |
| Lu [64] | ZSAS | 0.94 (0.56, 1.32) | ZSDS | 0.85 (0.48, 1.23) | SF-36 | 2.26 (1.80, 2.72) | – | – |
| Ma [65] | – | – | PHQ-9 | 3.60 (3.21, 4.00) | – | – | – | – |
| Nie [66] | GAD-7 | 2.72 (1.71, 3.73) | – | – | – | – | – | – |
| Xu [67] | ZSAS | 4.38 (3.56, 5.19) | ZSDS | 3.26 (2.59, 3.93) | – | – | – | – |
| Yang [68] | ZSAS | 26.98 (22.95, 31.01) | ZSDS | 15.20 (12.90, 17.50) | – | – | – | – |
| Zhang Y. [69] | ZSAS | 0.84 (−0.01, 1.69) | – | – | – | – | – | – |
| Zheng C. [70] | ZSAS | 1.30 (0.89, 1.71) | ZSDS | 2.23 (1.76, 2.71) | – | – | – | – |
| Zheng Y. [71] | ZSAS | 1.74 (1.14, 2.34) | ZSDS | 1.32 (0.75, 1.88) | – | – | – | – |
Abbreviations: CD-RISC = Connor-Davidson Resilience Scale; DASS-21 = Depression Anxiety and Stress Scale; GAD-7 = Generalized Anxiety Disorder scale; HAM-A = Hamilton Anxiety Rating Scale; HAM-D=Hamilton Depression Rating Scale; PHQ-9 = Patient Health Questionanaire-9; PSS=Perceived Stress Scale; SCL-25 = Symptoms Checklist-25; SCL-90 = Symptom Checklist-90; SF-36 = Short-Form-36 (SF-36) Health Survey; STAI = State Trait Anxiety Inventory; WHOQOL-BREF = World Health Organization Quality of Life Questionnaire-Brief; WHOQOL = World Health Organization Quality of Life Questionnaire; ZSAS = Zung Self-rating Anxiety Scale; ZSDS = Zung Self-rating Depression Scale.
Outcomes are reported with positive signs favoring the intervention group.
Among the 3 verified RCTs [31,37,38] rated low risk of bias on 4 of 7 domains, one (N = 93) [31] compared daily cognitive behavioral therapy (4 weeks) to routine care in hospitalized patients with mild COVID-19 in China; it did not find significant reductions in anxiety symptoms (Hedges' g = 0.24, 95% CI -0.17 to 0.65), depressive symptoms (Hedges' g = 0.04, 95% CI -0.37 to 0.45), or stress (Hedges' g = 0.10, 95% CI -0.51 to 0.31). Another trial (N = 110) [37] tested twice daily guided imagery (5 days) against routine care among hospitalized patients in Iran with oxygen saturation > 90% and reported statistically significant reductions in state (Hedges' g = 0.72, 95% CI 0.34 to 1.11) and trait anxiety (Hedges' g = 0.56, 95% CI 0.18 to 0.94). A third trial (N = 48) [38] compared a multi-faceted online psychological intervention to an offer to receive telephone counselling among mild to severely infected patients in a general hospital in Iran. It reported a non-statistically significant reduction in mental health function (Hedges' g = 0.49, 95% CI -0.09 to 1.08) and a significant reduction in stress (Hedges' g = 0.76, 95% CI 0.17 to 1.35).
3.4. Physical and breathing exercise interventions
The number of participants in the 5 physical and breathing exercise trials [[46], [47], [48], [49], [50]] ranged from 14 to 40 (mean = 51.0; SD = 20.5; median = 51). The percentage of female participants ranged from 39% to 55%. Mean age ranged from 35 to 69 years. Two trials tested breathing exercises [47,50], and three tested physical exercises [46,48,49].
3.4.1. Verification, intervention reporting, risk of bias
None of the 5 trials were verified. Out of 8 core TIDieR domains, each trial had 3 to 5 partially or not reported (median = 3). The number of trials that adequately reported was 5 (100%) for intervention name, 3 (60%) for rationale, 0 (0%) for materials used, 4 (80%) for procedures, 2 (40%) for provider, 4 (80%) for how administered, 0 (0%) for where administered, and 4 (80%) for when and how much provided. See Appendix D. Risk of bias was unclear or high in 2 trials for random sequence generation [47,50], one for incomplete outcome reporting [46], and all 5 for allocation concealment, blinding of participants and personnel, blinding of outcome assessment, and selective outcome reporting [[46], [47], [48], [49], [50]]. Across trials, excluding “other bias”, the median number of the other 6 domains rated as unclear or high risk was 4. No trials were at low risk of bias for ≥4 of 7 domains. See Table 2.
3.4.2. Outcomes
Of the 5 trials, 5 reported anxiety symptom outcomes [[46], [47], [48], [49], [50]], and 3 reported depression symptom outcomes [46,49,50]. Hedges' g ranged from −0.40 to 4.06 for anxiety symptoms and 0.78 to 2.99 for depression symptoms (Table 3).
3.5. Mixed interventions
In the 21 mixed interventions, the number of participants ranged from 15 to 130 (mean = 92.6; SD =49.3; median = 88). The proportion of female participants ranged between 29% to 59%, and mean age ranged from 36 to 64. There were 12 trials that tested some combination of ‘humanized’ nursing involving psychological care or a dietary intervention [52,[54], [55], [56], [57], [58], [59],61,[64], [65], [66], [67]], 2 trials that assessed interventions with components of both music therapy and physical and breathing exercises [60,63], and 6 interventions of general medicine and health education or traditional Chinese medicine including acupoint massage [51,53,[68], [69], [70], [71]]. Intervention duration, frequency, and session length were inconsistently reported.
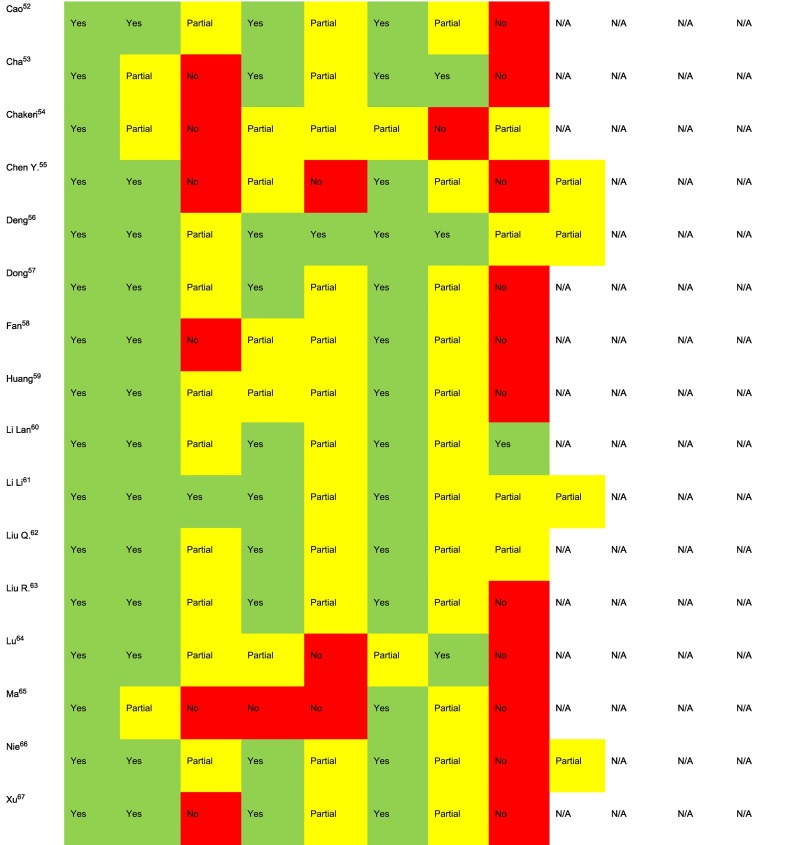
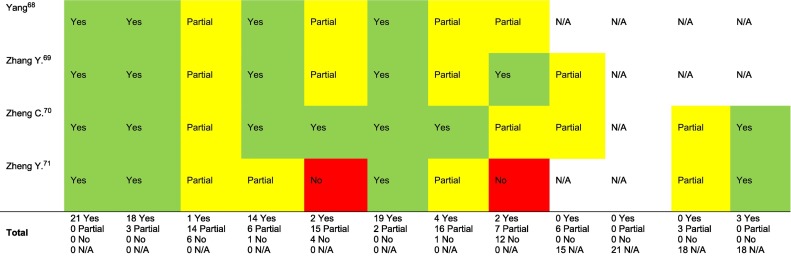
3.5.1. Verification, intervention reporting, risk of bias
Of the 21 trials, none were verified. Interventions were generally poorly described, and each trial had 3 to 5 of the 8 core TIDieR domains either partially or not at all reported (median = 4). The number of trials that adequately reported was 21 (100%) for intervention name, 18 (86%) for rationale, 1(5%) for materials used, 14 (60%) for procedures, 2 (9.5%) for provider, 19 (91%) for how administered, 4 (19%) for where administered, and 2 (10%) for when and how much provided. See Appendix D. For risk of bias, random sequence generation was unclear in 9 trials [52,54,55,61,[64], [65], [66], [67],71], and incomplete outcome data was unclear for 5 [51,54,59,65,66]. All 21 trials were rated as unclear or high risk for allocation concealment procedures, blinding of participants and personnel, blinding of outcome assessment, and selective reporting [[51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71]]. Across trials, excluding “other bias”, the median number of the other 6 domains rated as unclear or high risk was 4. No trials were at low risk of bias for ≥4 of 7 domains (Table 2).
3.5.2. Outcomes
Among the 21 trials, 20 reported anxiety symptom outcomes [[51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64],[66], [67], [68], [69], [70], [71]], 16 depression symptoms [[51], [52], [53],56,[58], [59], [60], [61], [62], [63], [64], [65],67,68,70,71], and 3 mental health function [57,61,64]. Hedges' g ranged from 0.45 to 26.98 for anxiety symptoms, 0.85 to 15.20 for depression symptoms and 1.76 to 2.28 for mental health function (Table 3).
4. Discussion
We investigated the effects of mental health interventions among patients with COVID-19 infection. We identified and extracted data from 47 eligible RCTs from China (N = 42), Iran (N = 4) and Turkey (N = 1), of which 21 tested psychotherapy interventions, 5 physical and breathing exercises, and 21 a combination of other types of interventions (e.g., “humanistic” nursing care). All trials were conducted in hospital settings and evaluated short-term, in-hospital mental health.
Overall, poor reporting and risk of bias limited our ability to draw conclusions about the effects of interventions. Of the 47 included trials, only 21 included contact information for authors, and institutional origin was unclear for many trials. Because of the very poor quality and uncertain origin of many trials, we attempted to contact authors to verify that trials had been conducted as reported and the accuracy of our extracted results; however, authors of only 3 trials verified results. We used the TIDieR tool to describe adequacy of intervention reporting. In each of the intervention categories (psychological, physical and breathing exercise, mixed), a median of 3 to 4 of 8 core TIDieR domains were partially or not at all reported. For risk of bias, across the 3 intervention categories, the median number of unclear or high risk of bias domains per trial was 3 for psychological interventions, 4 for physical and breathing exercises, and 4 for mixed interventions. Of the 47 trials, 25 (53%) reported SMD effect sizes greater than 2.0, which is several times the effect typically seen in mental health interventions, including in ICU settings [7].
Only 3 trials [31,37,38], all of psychological interventions, were rated as low risk of bias on at least 4 risk of bias domains. These same 3 trials were the only 3 trials for which authors verified results. A cognitive behavioral intervention (N = 93) reported Hedges' g effects between 0.04 and 0.24 (all not statistically significant) for anxiety symptoms, depressive symptoms, and stress; a guided imagery intervention (N = 110) reported significant reductions in state (Hedges' g = 0.72, 95% CI 0.34 to 1.11) and trait anxiety (Hedges' g = 0.56, 95% CI 0.18 to 0.94); and an online multicomponent intervention reported a non-statistically significant reduction in mental health function (Hedges' g = 0.49, 95% CI -0.09 to 1.08) and a significant reduction in stress (Hedges' g = 0.76, 95% CI 0.17 to 1.35). It is difficult, however, to draw generalizable conclusions from these studies. They tested different types of interventions and, although better conducted than other included trials, still had important methodological limitations.
While issues of poor study design, methodology and reporting of results were a pervasive issue in research prior to COVID-19, concerns have been raised about the exceptionally high volume and unprecedented poor quality of research being generated in COVID-19. This is especially the case in COVID-19 research among trials with time pressures and insufficient research infrastructure, particularly in the earlier phases of the pandemic, which contributed to the conduct and publication of many poorly designed studies with sample sizes too small to answer the research questions being posed [72]. The set of trials included in the present review exceed what we have seen prior to COVID-19 or in other areas of COVID-19 mental health (e.g., [13]) in terms of failing to provide minimally transparent reporting, verification of origin, overall study quality, and the unusually large effects reported. For comparison, over 50% of trials reported SMD effect sizes of 2.0 or greater versus only 1 of 11 (9%) trials in the most recent pre-COVID-19 systematic review of ICU-based interventions [7].
Previous systematic reviews have, however, also reported that there are few well-conducted and reported RCTs of interventions for hospitalized patients infected with acute illnesses [5,6]. The most recent systematic review [6], which included meta-analyses of effects of different types of interventions (exercise, psychosocial, information, diaries, other) reported that diary interventions significantly improved depression and anxiety but there were only two small trials included with 88 total participants. Meta-analysis of 4 RCTs (N = 231) found that exercise interventions did not improve anxiety or depression symptoms; but meta-analysis of 7 different RCTs (N = 664) found that exercise improved general mental health function.
The limited evidence available on interventions to support mental health in acutely hospitalized patients prior to COVID-19, coupled with the very poor quality of trials done during COVID-19, reduces the ability of health care providers to use trial evidence to guide their clinical care of patients hospitalized with COVID-19. Furthermore, the resources to provide in-hospital psychological care during COVID-19 may be limited due to demands on health care systems across the globe during the pandemic [73] as well as measures taken to reduce transmission. In the absence of actionable evidence, health care providers will need to rely on expert recommendations for ICU and other hospital care. These, generally, involve initial close attention to symptom stabilization, including strategies to manage pain, maintaining contact with loved ones through virtual calls, reduce fear and anxiety, and support sleep; the normalization of experiences; and reassurance that symptoms are expected to decrease in frequency and intensity with time. Types of interventions that may be helpful include stress reduction (e.g., breathing, meditative interventions), education, diaries, supportive therapy, and movement, as possible. As patients achieve increased stability, assessment of and strategies to address anxiety, depression, and posttraumatic stress can be initiated [74].
Well-designed and conducted, adequately powered trials for different interventions to support stress reduction and improve short- and long-term mental health among hospitalized acute care patients are desperately needed in the context of COVID-19 and otherwise. Additionally, interventions are needed to address mental health for people who experience long-term effects of COVID-19, as they appear to be at risk of negative cognitive and mental health outcomes [75,76]. We did not include studies done with people with long COVID-19 outside of hospital, but these trials would have been included in our main living systematic review, and as of February 11, 2022, no such trials had been identified.
There are several strengths of the present living systematic review. Firstly, it differs from prior systematic reviews as it investigated the effects of psychological interventions specifically among hospitalized COVID-19-infected patients based on randomized trials. Second, we included many more trials than have been included in any other review. Related to this, we included two Chinese databases in our search and included Chinese-language trials; these trials comprise the largest proportion of all trials that have been conducted. Third, we employed a rigorous methodology in conducting the present review based on best practices per the Cochrane Collaboration [77].
The findings of the current review must be interpreted in the context of limitations. Chiefly, the quality of reporting and conduct of included trials was very poor, generally. Documenting this rigorously is important for supporting health care providers to determine how usable the evidence might be and to underline the need for higher quality research in this area. We were not, however, able to use the evidence to make recommendations about which interventions may be effective in practice. Any other limitations are secondary to this main concern. For instance, we did not attempt to examine the possibility of publication bias. It is possible that well-conducted trials with disappointing outcomes may have been conducted, but we do not believe this is likely given the overall quality issues we uncovered. It is likely that producing well-designed and conducted trials of mental health interventions in the initial phases of the pandemic was simply not feasible; with less intense pressure on health care systems in more recent phases, it is possible that trials will be conducted that will be of better quality and greater utility. Additionally, all trials were from 3 countries. It is possible that more trials in later stages of the pandemic will be done in countries that normally conduct the largest numbers of mental health and other health care service trials [78].
In conclusion, the objective of the present review was to evaluate the effects of interventions to support mental health among hospitalized COVID-19 infected patients. Our inability to verify what occurred in the studies, very poor reporting and study quality, high risk of bias, and implausible reported effects, in many trials, did not allow us to draw conclusions about the likely effects of any included interventions. Our inability to draw conclusions from this evidence base is compounded by limitations in the quality of ICU-based mental health intervention trials available prior to COVID-19 [6,7]. Accordingly, our review highlights the importance of and need for carefully conducted and reported RCTs. Without trustworthy evidence, health care providers should use strategies that are considered best practice to help patients hospitalized with COVID-19 achieve symptom stability as quickly as possible and to prevent and address long term mental health ramifications. Trials are needed, both in general ICU contexts and, to the degree as possible as the COVID-19 pandemic continues, that test and compare procedures that are commonly used with acutely hospitalized patients, including different approaches for symptom stabilization and management, stress reduction, and psychological tools designed to support recovery [74]. The limitations in existing trials may highlight limitations in infrastructure. Multi-center collaborations with an ongoing commitment to adaptive trial designs, such as platform trials [79], might be considered to address the current lack of well-designed and conducted trials of interventions to support mental health in ICU settings, both prior to and during COVID-19.
Author contributions
AT: Formal analysis, Investigation, Writing – original draft, Writing – review & editing; YWa: Investigation, Writing – review & editing; KL: Investigation, Writing – review & editing; XJ: Investigation, Writing – review & editing; AK: Investigation, Data curation, Writing – review & editing; CH: Investigation, Writing – review & editing, Project administration; YS: Conceptualization, Investigation, Writing – review & editing, Project administration; YWu: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing; SF: Investigation, Writing – review & editing, Project administration; JTB: Methodology; Data curation; Writing – review & editing; SM: Investigation, Writing – review & editing; DBR: Conceptualization, Methodology, Investigation, Writing – review & editing; OB: Investigation, Writing – review & editing, Project administration; TDS: Investigation, Writing – review & editing; LL: Investigation, Writing – review & editing; ITV: Investigation, Writing – review & editing; BA: Conceptualization, Writing – review & editing; CF: Conceptualization, Writing – review & editing; MSM: Conceptualization, Writing – review & editing; SS: Conceptualization, Writing – review & editing; AB: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Supervision, Funding acquisition; BDT: Conceptualization, Methodology, Formal analysis, Investigation; Data curation; Writing – Original draft, Writing – review & editing, Supervision, Funding acquisition.
Funding
The living systematic review was funded by the Canadian Institutes of Health Research (CMS-171703; MS1-173070; GA4-177758) and McGill Interdisciplinary Initiative in Infection and Immunity Emergency COVID-19 Research Fund (R2–42). YWu was supported by a Fonds de recherche du Québec – Santé (FRQS) Postdoctoral Training Fellowship. DBR was supported by a Vanier Canada Graduate Scholarship. AB was supported by an FRQS senior researcher salary award. BDT was supported by a Tier 1 Canada Research Chair.
Data sharing
All data from the living systematic review are available in the present manuscript and its supplementary material or online (https://www.depressd.ca/research-question-3-intervention).
Declaration of Competing Interest
All authors completed the ICJME uniform disclosure form and declared no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years. All authors declare no other relationships or activities that could appear to have influenced the submitted work. No sponsor or funder was involved in the study design; in the collection, analysis and interpretation of the data; in the writing of the report; or in the decision to submit the paper for publication.
Appendix A. Search strategies
Ovid MEDLINE All
†New subject heading added to original search on January 27, 2021
-
1.
Quarantine/
-
2.
social isolation/ or loneliness/ or physical distancing/†
-
3.
psychology.fs. or psychology/
-
4.
Mental health/
-
5.
mental disorders/
-
6.
social stigma/
-
7.
Fear/
-
8.
Anxiety/
-
9.
Depression/
-
10.
Stress, Physiological/ or Stress, Psychological/
-
11.
Anger/
-
12.
Irritable Mood/
-
13.
Grief/
-
14.
burnout, psychological/ or burnout, professional/
-
15.
or/1–14
-
16.
(Quarantine* or Self-isolation or isolation or social distanc* or shelter*-in-place or psych* or mental health or mental illness* or mental disorder* or stigma or fear* or anxiety or anxious or depression or depressive or loneliness or stress* or trauma* or post-traumatic or posttraumatic or anger or mood* or irritability or irritable or emotional disturbance* or grief or burned out or burnout).tw,kf.
-
17.
((exp coronavirus/ or exp. coronavirus infections/ or (betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*).mp.) and (exp china/ or (china or chinese or hubei or wuhan).af.)) or (coronavirus* or corona virus* or betacoronavirus* or beta coronavirus*).mp.
-
18.
(severe acute respiratory syndrome coronavirus 2 or “SARS CoV-2” or “SARSCoV 2” or SARSCoV2 or cov2 or “sars 2” or COVID or “coronavirus 2” or covid19 or nCov or ((new or Novel) adj3 coronavirus*) or ncp).mp. or ((exp pneumonia/ or pneumonia.mp.) and wuhan.af.)
-
19.
17 or 18
-
20.
15 or 16
-
21.
19 and 20
-
22.
(“20,191,231” or 2020* or 2021*).dt,ez,da.
-
23.
21 and 22
Embase (Ovid)
-
1.
exp. coronavirinae/
-
2.
exp. Coronavirus infection/
-
3.
(betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*).mp.
-
4.
1 or 2 or 3
-
5.
exp. China/
-
6.
(china or chinese or hubei or wuhan).af.
-
7.
5 or 6
-
8.
4 and 7
-
9.
(betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*).mp.
-
10.
(severe acute respiratory syndrome coronavirus 2 or “SARS CoV-2” or “SARSCoV 2” or SARSCoV2 orcov2 or “sars 2” or COVID or “coronavirus 2” or covid19 or nCov or ((new or Novel) adj3 coronavirus*) or ncp).mp.
-
11.
(exp pneumoia/ or pneumonia.mp.) and wuhan.af.
-
12.
8 or 9 or 10 or 11
-
13.
quarantine/
-
14.
social isolation/ or isolation/ or patient isolation/
-
15.
loneliness/
-
16.
psychology/
-
17.
mental health/
-
18.
mental disease/
-
19.
social stigma/
-
20.
fear/
-
21.
anxiety/
-
22.
depression/
-
23.
physiological stress/ or mental stress/
-
24.
anger/
-
25.
irritability/
-
26.
exp grief/
-
27.
exp burnout/
-
28.
(mental disorder* or Quarantine* or Self-isolation or isolation or social distanc* or shelter*-in-place or psych* or mental health or mental illness* or stigma or fear* or anxiety or anxious or depression or depressive or loneliness or stress* or trauma* or post-traumatic or posttraumatic or anger or mood* or irritability or irritable or emotional disturbance* or grief or burned out or burnout).tw,kw.
-
29.
or/13-27
-
30.
12 and 29
-
31.
(“20,191,231” or 2020* or 2021*).dc.
-
32.
30 and 31
PsycINFO (Ovid)
-
1.
(coronavirus* or corona virus* or betacoronavirus* or beta coronavirus*).mp.
-
2.
(severe acute respiratory syndrome coronavirus 2 or “SARS CoV-2” or “SARSCoV 2” or SARSCoV2 or cov2 or “sars 2” or COVID or “coronavirus 2” or covid19 or nCov or ((new or Novel) adj3 coronavirus*) or ncp).mp. or ((exp pneumonia/ or pneumonia.mp.) and wuhan.af.)
-
3.
1 or 2
-
4.
(“20,191,231” or 2020* or 2021*).up.
-
5.
3 and 4
CINAHL
| Search ID# | Search Terms |
|---|---|
| S26 | S11 AND S25 |
| S25 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 |
| S24 | TI ((mental disorder* or Quarantine* or Self-isolation or isolation or social distanc* or shelter*-in-place or psych* or mental health or mental illness* or stigma or fear* or anxiety or anxious or depression or depressive or loneliness or stress* or trauma* or post-traumatic or posttraumatic or anger or mood* or irritability or irritable or emotional disturbance* or grief or burned out or burnout)) OR AB ((mental disorder* or Quarantine* or Self-isolation or isolation or social distanc* or shelter*-in-place or psych* or mental health or mental illness* or stigma or fear* or anxiety or anxious or depression or depressive or loneliness or stress* or trauma* or post-traumatic or posttraumatic or anger or mood* or irritability or irritable or emotional disturbance* or grief or burned out or burnout)) |
| S23 | (MH “Burnout, Professional”) |
| S22 | (MH “Grief+”) |
| S21 | (MH “Anger”) |
| S20 | (MH “Stress, Physiological”) OR (MH “Stress, Psychological”) |
| S19 | (MH “Depression”) |
| S18 | (MH “Anxiety”) |
| S17 | (MH “Fear”) |
| S16 | (MH “Stigma”) |
| S15 | (MH “Mental Health”) or (MH “Mental Disorders”) |
| S14 | (MH “Psychology”) |
| S13 | (MH “Social Isolation”) OR (MH “Loneliness”) or (MH “Social Distancing”) or (MH “Stay at Home Orders”) † |
| S12 | (MH “Quarantine”) |
| S11 | S7 OR S8 OR S9 OR S10 |
| S10 | ((MH “Pneumonia+”) or TI (pneumonia) OR AB (pneumonia)) AND (TI (wuhan) OR AB (wuhan) OR AF (wuhan)) |
| S9 | TI ((severe acute respiratory syndrome coronavirus 2 or “SARS CoV-2” or “SARSCoV 2” or SARSCoV2 or cov2 or “sars 2” or COVID or “coronavirus 2” or covid19 or nCov or ((new or Novel) N3 coronavirus*)) OR AB ((severe acute respiratory syndrome coronavirus 2 or “SARS CoV-2” or “SARSCoV 2” or SARSCoV2 or cov2 or “sars 2” or COVID or “coronavirus 2” or covid19 or nCov or ((new or Novel) N3 coronavirus*)) or (MH “Covid 19”) † |
| S8 | TI ((betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*)) OR AB ((betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*)) |
| S7 | S5 AND S6 |
| S6 | S1 OR S2 |
| S5 | S3 OR S4 |
| S4 | TI ((china or chinese or hubei or wuhan)) OR AB ((china or chinese or hubei or wuhan)) OR AF ((china or chinese or hubei or wuhan)) OR SO ((china or chinese or hubei or wuhan)) |
| S3 | (MH “China+”) |
| S2 | TI ((betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*)) OR AB ((betacoronavirus* or beta coronavirus* or coronavirus* or corona virus*)) |
| S1 | (MH “Coronavirus+”) OR (MH “Coronavirus Infections+”) |
Web of Science
TOPIC: (Quarantine* or “Self-isolation” or isolation or “social distanc*” or “shelter*-in-place” or psych* or “mental health” or “mental illness*” or “mental disorder*” or stigma or fear* or anxiety or anxious or depression or depressive or loneliness or stress* or trauma* or “post-traumatic” or posttraumatic or anger or mood* or irritability or irritable or “emotional disturbance*” or grief or “burned out” or burnout) AND TOPIC: ((coronavirus* or “corona virus*” or betacoronavirus* or “beta coronavirus*” or “severe acute respiratory syndrome coronavirus 2” or “SARS CoV-2” or “SARSCoV 2” or SARSCoV2 or cov2 or “sars 2” or COVID or “coronavirus 2” or covid19 or nCov or “Novel coronavirus*” or “new coronavirus*”)).
Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan = Year to date.
China National Knowledge Infrastructure
Restricted to disciplines: Medical and Public Health & Social science.
TI = (隔离 + 封城 + 社交距离+方舱 + 心理 + 心理健康+精神卫生+精神疾病+心理疾病+污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力 + 应激 + 创伤 + 创伤后 + 愤怒 + 情绪 + 心情 + 易怒 + 情绪障碍+心理障碍+哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(新冠 + 新型冠状) OR AB = (隔离 + 封城 + 社交距离+方舱 + 心理 + 心理健康+精神卫生+精神疾病+心理疾病+污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力 + 应激 + 创伤 + 创伤后 + 愤怒 + 情绪 + 心情 + 易怒 + 情绪障碍+心理障碍+哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(新冠 + 新型冠状).
Wanfang
题名:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病” + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病” + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”).
We made several amendments to the original search strategies. Since the Wanfang database cannot export more than 5000 references at once, we broke the search strategies into two or more smaller search strings to get all the references. The four changes on September 1, 2020, September 28, 2020, October 15, 2020 and October 18, 2020 are all for this purpose.
To make this process more efficient, the disciplines of the China National Knowledge Infrastructure database were restricted to Medical and Public Health AND Social science subgroup 2 and those of Wanfang database were restricted to Medicine and Health AND Culture, Science, Education and PE disciplines on October 23, 2020.
September 1, 2020.
Wanfang
题名:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病” + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病” + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 抑郁 + 孤独 + 压力 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 抑郁 + 孤独 + 压力 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”).
September 28, 2020.
Wanfang
题名:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病” + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病” + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 抑郁 + 孤独 + 压力 + 应激 + 创伤+”创伤后”)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 抑郁 + 孤独 + 压力 + 应激 + 创伤+”创伤后”)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”).
October 15, 2020.
Wanfang
题名:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病”)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病”)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”).
October 18, 2020.
Wanfang
题名:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病”)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 心理+”心理健康”+”精神卫生”+”精神疾病”+”心理疾病”)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 孤独 + 压力)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 孤独 + 压力)*(“新冠”+”新型冠状”).
题名:(“隔离” + 封城+”社交距离” + 方舱 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”) + 摘要:(“隔离” + 封城+”社交距离” + 方舱 + 应激 + 创伤+”创伤后” + 愤怒 + 情绪 + 心情 + 易怒+”情绪障碍”+”心理障碍” + 哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(“新冠”+”新型冠状”).
October 23, 2020.
China National Knowledge Infrastructure
Restricted to disciplines: Medical and Public Health & Social science subgroup 2.
TI = (隔离 + 封城 + 社交距离+方舱 + 心理 + 心理健康+精神卫生+精神疾病+心理疾病+污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力 + 应激 + 创伤 + 创伤后 + 愤怒 + 情绪 + 心情 + 易怒 + 情绪障碍+心理障碍+哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(新冠 + 新型冠状) OR AB = (隔离 + 封城 + 社交距离+方舱 + 心理 + 心理健康+精神卫生+精神疾病+心理疾病+污名 + 耻辱 + 羞辱 + 恐惧 + 焦虑 + 抑郁 + 孤独 + 压力 + 应激 + 创伤 + 创伤后 + 愤怒 + 情绪 + 心情 + 易怒 + 情绪障碍+心理障碍+哀伤 + 悲伤 + 悲痛 + 悲哀 + 忧郁 + 倦怠)*(新冠 + 新型冠状).
Wanfang
Restricted to disciplines: Medicine and Health & Culture, Science, Education and PE.
题名:(“隔离” or 封城 or “社交距离” or 方舱 or 心理 or “心理健康” or “精神卫生” or “精神疾病” or “心理疾病” or 污名 or 耻辱 or 羞辱 or 恐惧 or 焦虑 or 抑郁 or 孤独 or 压力 or 应激 or 创伤 or “创伤后” or 愤怒 or 情绪 or 心情 or 易怒 or “情绪障碍” or “心理障碍” or 哀伤 or 悲伤 or 悲痛 or 悲哀 or 忧郁 or 倦怠) and (“新冠” or “新型冠状”) or 摘要:(“隔离” or 封城 or “社交距离” or 方舱 or 心理 or “心理健康” or “精神卫生” or “精神疾病” or “心理疾病” or 污名 or 耻辱 or 羞辱 or 恐惧 or 焦虑 or 抑郁 or 孤独 or 压力 or 应激 or 创伤 or “创伤后” or 愤怒 or 情绪 or 心情 or 易怒 or “情绪障碍” or “心理障碍” or 哀伤 or 悲伤 or 悲痛 or 悲哀 or 忧郁 or 倦怠) and (“新冠” or “新型冠状”).
MedRxiv (pre-prints).
Search 1: (isolation OR “mental health” OR “mental illness” OR “mental disorder”) AND (COVID OR covid19).
Search 2: (psychology OR psychological OR psychosocial OR anxiety OR depression OR stress or trauma) AND (COVID OR covid19).
Open Science Framework (pre-prints).
(isolation OR psychology OR psychological OR psychosocial OR “mental health” OR “mental illness” OR “mental disorder” OR anxiety OR depression OR stress or trauma) AND (coronavirus OR COVID OR covid19)
Appendix B. Coding manuals for inclusion and exclusion
Inclusion and Exclusion Coding Guides for Main Interventions Review Plus Additional Criteria for Present Report.
Title and Abstract Review:
Exclude: not original human data or a case study or case series. If it is clear from the title and abstract that the article is not an original report of primary data, but, for example, a letter, editorial, systematic review or meta-analysis, or it is a single case study or case series, then it is excluded. Studies reporting only on animal, cellular, or genetic data are also excluded. Conference abstracts are included.
Exclude: not a study of any population affected by the COVID-19 outbreak. Eligible studies must be initiated after China's first announcement to the WHO on December 31, 2019. If it is clear from the title or abstract that the study is not about any population affected by the COVID-19 outbreak, it is excluded. Studies that include fewer than 10 subjects, are excluded.
Exclude: intervention does not target mental health. If it is clear from the title or abstract that the study is not about an intervention or is an intervention, but the intervention does not primarily target mental health, then it will be excluded. Mental health must be the primary trial outcome if a primary outcome or outcomes are stated.
Exclude: not a randomized or non-randomized controlled trial (RCT) with eligible comparators: If it is clear from the title or abstract that the study is not a RCT or non-randomized controlled trial that compares an intervention designed to improve any aspect of mental health during the COVID-19 pandemic to (1) any inactive control condition (e.g., no treatment, waitlist control) or to (2) another eligible intervention designed to mental health, then it will be excluded.
Include: study eligible to be included in full-text review.
Full-text Review:
Exclude: not original human data or a case study or case series. If the article is not an original report of primary data, but, for example, a letter, editorial, systematic review or meta-analysis, or it is a single case study or case series, then it is excluded. Studies reporting only on animal, cellular, or genetic data are also excluded. Conference abstracts are included.
Exclude: not a study of any population affected by the COVID-19 outbreak. Eligible studies must be initiated after China's first announcement to the WHO on December 31, 2019. If the study is not about any population affected by the COVID-19 outbreak, it is excluded. Studies that include fewer than 10 subjects, are excluded.
Exclude: intervention does not target mental health. If the study is not about an intervention or is an intervention, but the intervention does not primarily target mental health, then it will be excluded. Mental health must be the primary trial outcome if a primary outcome or outcomes are stated.
Exclude: not a randomized or non-randomized controlled trial (RCT) with eligible comparators: If the study is not a RCT or non-randomized controlled trial that compares an intervention designed to improve any aspect of mental health during the COVID-19 pandemic to (1) any inactive control condition (e.g., no treatment, waitlist control) or to (2) another eligible intervention designed to mental health, then it will be excluded.
Include: study eligible for inclusion in systematic review.
Additional Criteria for Present Report: (1) randomized controlled trial; (2) population hospitalized due to COVID-19.
Appendix C. Protocol amendments
The series of living systematic reviews was designed and initiated quickly early in COVID-19, and several amendments were made that are relevant to the present sub-study. First, we changed the automatic daily search updates to weekly updates as of December 28, 2020 to allow for more efficient processing of studies. Second, on January 27, 2021 we made a change to the MEDLINE search strategy to include a new subject heading on physical distancing created for COVID-19. Third, we made several amendments to the Chinese-language search strategies to allow more efficient processing of studies (see Appendix A). Fourth, we added the TIDieR checklist to assess intervention reporting adequacy. Fifth, we clarified that we only included trials which began participant enrolment after December 31, 2019. Sixth, we did not include non-randomized trials. Such studies are highly prone to bias when intervention and control groups are self-selected or there is no control group. Results from pre-post analyses of non-randomized studies without a control group are not possible to interpret unless there is a precise knowledge of the natural trajectory of symptoms or if one can safely assume that symptoms will not change over time without intervention. Even in normal times, however, this is not the case for mental health trials, and the Cochrane Collaboration discourages inclusion of evidence from non-randomized studies in systematic reviews when conducting trials is feasible [1]. Seventh, because we encountered many trial reports of poor quality with seemingly implausible results, some with unclear origin, we added the author verification process.
-
[1]
Reeves BC, Deeks JJ, Higgins JPT, Shea B, Tugwell P, Wells GA. Chapter 24: Including non-randomized studies on intervention effects. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook. Accessed February 16, 2022.
Appendix D. Adequacy of reporting of interventions based on TIDieR checklist
Note: Not applicable (N/A).
References
- 1.World Health Organization Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/ Accessed February 16, 2022.
- 2.Inter-Agency Standing Committee Addressing Mental and Psychosocial Aspects of COVID-19 Outbreak. 2020. https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/interim-briefing-note-addressing-mental-health-and-psychosocial-aspects-covid-19-outbreak Accessed February 16, 2022.
- 3.Phua J., Weng L., Ling L., Egi M., Lim C.M., Divatia J.V., et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir. Med. 2020;8(5):506–517. doi: 10.1016/s2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crooke H., Raza S., Nowell J., Young M., Edison P. Long covid – mechanisms, risk factors, and management. BMJ. 2021;374 doi: 10.1136/bmj.n1648. [DOI] [PubMed] [Google Scholar]
- 5.Sudre C.H., Murray B., Varsavsky T., Graham M.S., Penfold R.S., Bowyer R.C., et al. Attributes and predictors of long COVID. Nat. Med. 2021;27(4):626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wade D.F., Moon Z., Windgassen S.S., Harrison A.M., Morris L., Weinman J.A. Non-pharmacological interventions to reduce ICU-related psychological distress: a systematic review. Minerva Anestesiol. 2016;82(4):465–478. https://www.minervamedica.it/it/riviste/minerva-anestesiologica/articolo.php?cod=R02Y2016N04A0465 [PubMed] [Google Scholar]
- 7.Geense W.W., van den Boogaard M., van der Hoeven J.G., Vermeulen H., Hannink G., Zegers M. Nonpharmacologic interventions to prevent or mitigate adverse long-term outcomes among ICU survivors: a systematic review and meta-analysis. Crit. Care Med. 2019;47(11):1607–1618. doi: 10.1097/ccm.0000000000003974. [DOI] [PubMed] [Google Scholar]
- 8.Yang Y., Sun S., Hu S., Tang C., Zhang Y., Lin H. Comparative effectiveness of multiple psychological interventions for psychological crisis in people affected by coronavirus disease 2019: a Bayesian network meta-analysis. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.577187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ding H., He F., Lu Y.G., Hao S.W., Fan X.J. Effects of non-drug interventions on depression, anxiety and sleep in COVID-19 patients: a systematic review and meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 2021;25(2):1087–1096. doi: 10.26355/eurrev_202101_24679. [DOI] [PubMed] [Google Scholar]
- 10.Elliott J.H., Synnot A., Turner T., Simmonds M., Akl E.A., McDonald S., et al. Living systematic review: 1. Introduction-the why, what, when, and how. J. Clin. Epidemiol. 2017;91:23–30. doi: 10.1016/j.jclinepi.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 11.Thombs B.D., Bonardi O., Rice D.B., Boruff J.T., Azar M., He C., et al. Curating evidence on mental health during COVID-19: a living systematic review. J. Psychosom. Res. 2020;133 doi: 10.1016/j.jpsychores.2020.110113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Living systematic review of mental health in COVID-19. https://www.depressd.ca/covid-19-mental-health Accessed February 18, 2022.
- 13.Bonardi O., Wang Y.T., Li K.X., et al. Effects of COVID-19 mental health interventions among children, adolescents, and adults not quarantined or undergoing treatment due to COVID-19 infection: a systematic review of randomized controlled trials. Can. J. Psychiatr. 2022 doi: 10.1177/07067437211070648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page M.J., McKenzie J., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. Vol. 372. 2021. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews.https://www.bmj.com/content/372/bmj.n71 n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization Rolling updates on coronavirus disease (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen Accessed February 18, 2022.
- 16.Balshem H., Helfand M., Schünemann H.J., Oxman A.D., Kunz R., Brozek J., et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 17.Berkman N.D., Lohr K.N., Ansari M.T., Balk E.M., Kane R., McDonagh M., et al. Grading the strength of a body of evidence when assessing health care interventions: an EPC update. J. Clin. Epidemiol. 2014;68(11):1312–1324. doi: 10.1016/j.jclinepi.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 18.Jüni P., Altman D.G., Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ. 2001;323(7303):42–46. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D., Hopewell S., Schulz K.F., Montori V., Gøtzsche P.C., Devereaux P.J., et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340 doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hernán M.A., Robins J.M. Chapman & Hall/CRC; Boca Raton: 2018. Causal inference: What if. [Google Scholar]
- 21.Cuijpers P. The challenges of improving treatments for depression. JAMA. 2018;320(24):2529–2530. doi: 10.1001/jama.2018.17824. [DOI] [PubMed] [Google Scholar]
- 22.Reeves B.C., Deeks J.J., JPT Higgins, Shea B., Tugwell P., Wells G.A. In: Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020) JPT Higgins, Thomas J., Chandler J., Cumpston M., Li T., Page M.J., et al., editors. Cochrane; 2020. Chapter 24: Including non-randomized studies on intervention effects.www.training.cochrane.org/handbook Available from. [Google Scholar]
- 23.Higgins J.P.T., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffmann T.C., Glasziou P.P., Boutron I., Milne R., Perera R., Moher D., et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348 doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 25.Ding C., Meng X., Xu Y., Zhang Z. Effect of psychological intervention on anxiety and depression of patients in the isolation ward of novel coronavirus pneumonia. Chin. Commun. Doctors. 2021;37(8):127–128. doi: 10.3969/j.issn.1007-614x.2021.08.061. [DOI] [Google Scholar]
- 26.Gharaati Sotoudeh H., Alavi S.S., Akbari Z., Jannatifard F., Artounian V. The effect of brief crisis intervention package on improving quality of life and mental health in patients with COVID-19. Iran. J. Psychiatry. 2020;15(3):205–212. doi: 10.18502/ijps.v15i3.3812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gu Y., Li C., Song Y., Lu G., Yan J. The effect of mindfulness decompression therapy based on live broadcast of Tencent conference on anxiety and depression in patients diagnosed with new coronary pneumonia. Chin. Nurs. Manag. 2021;21(5):707–712. doi: 10.3969/j.issn.1672-1756.2021.05.015. [DOI] [Google Scholar]
- 28.Guo H. Analysis of the effect of psychological nursing intervention for patients with new coronary pneumonia. Diet Health Care. 2020;7(28):223–224. [Google Scholar]
- 29.Hui J., Zeng P., Liang H., Sun J. The effect of psychological crisis intervention in the Neuman health system model on anxiety and depression in patients with new coronavirus pneumonia. Int. J. Psychiatry. 2020;47(4):637–641. doi: 10.13479/j.cnki.jip.2020.04.001. [DOI] [Google Scholar]
- 30.Jiang L. The effect of psychological intervention on COVID-19 patients with anxiety and depression. Jia You Yun Bao. 2020;2(14):155. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg1qeXliMjAyMDE0MTQ5GghzbW9mN3o5dQ%3D%3D [Google Scholar]
- 31.Li J., Li X., Jiang J., Xu X., Wu J., Xu Y., et al. The effect of cognitive behavioral therapy on depression, anxiety, and stress in patients with COVID-19: a randomized controlled trial. Front. Psychol. 2020;11 doi: 10.3389/fpsyt.2020.580827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu Y., Yang Y.Q., Liu Y., Pei S.L., Yang H.H., Wu J.J., et al. Effects of group psychological intervention combined with pulmonary rehabilitation exercises on anxiety and sleep disorders in patients with mild coronavirus disease 2019 (COVID-19) infections in a Fangcang hospital. Psychol. Health Med. 2022 doi: 10.1080/13548506.2021.1916956. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 33.Liu Y., Wu Y., Wang C., Zhang L., Xie S. Intervention effect of art therapy on mood, cognition and quality of life of patients with novel coronavirus pneumonia during isolation. Mod. Pract. Med. 2020;32(11):1393–1395. doi: 10.3969/j.issn.1671-0800.2020.11.044. [DOI] [Google Scholar]
- 34.Liu Z.F., Qiao D., Xu Y.F., Zhao W.T., Yang Y., Wen D., et al. The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: randomized controlled trial. J. Med. Internet Res. 2021;23(5):e26883. doi: 10.2196/26883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pan H. The effect of psychological nursing on anxiety and depression of patients with new coronary pneumonia. Yiyao Qianyan. 2020;10(16):184–185. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg55aXlxeTIwMjAxNjE1MxoIM2NqNWFsY3E%3D [Google Scholar]
- 36.Pan R. Psychological nursing experience of new coronary pneumonia. Diet Health. 2020;36:241. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg95aW5zYmoyMDIwMzYyMzEaCG12NDIyaXpy [Google Scholar]
- 37.Parizad N., Goli R., Faraji N., Mam-Qaderi M., Mirzaee R., Gharebaghi N., et al. Effect of guided imagery on anxiety, muscle pain, and vital signs in patients with COVID-19: a randomized controlled trial. Complement. Ther. Clin. Pract. 2021;43 doi: 10.1016/j.ctcp.2021.101335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shaygan M., Yazdani Z., Valibeygi A. The effect of online multimedia psychoeducational interventions on the resilience and perceived stress of hospitalized patients with COVID-19: a pilot cluster randomized parallel-controlled trial. BMC Psychiatry. 2021;21(1) doi: 10.1186/s12888-021-03085-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shi Q., Yuan Y., Miao C., Dong Y., Tao L. A clinical study of emotional nursing on the negative emotions of patients with new coronavirus pneumonia during treatment. World’s Latest Med. Inform. Abstr. (Contin. Electron. J.) 2020;20(87):278–280. doi: 10.3969/j.issn.1671–3141.2020.87.123. [DOI] [Google Scholar]
- 40.Shi Y. Exploring the psychological care effects of ICU patients during the epidemic of new coronavirus pneumonia. Smart Health. 2020;6(20):125–127. doi: 10.19335/j.cnki.2096-1219.2020.20.054. [DOI] [Google Scholar]
- 41.Wang M., Yang J., Zhao X., Ma J., Li J. The impact of empathy psychological intervention on the coping style and mental health maintenance of critically ill patients with novel coronavirus pneumonia. Lab. Med. Clin. 2020;17(23):3499–3501. doi: 10.3969/j.issn.1672-9455.2020.23.033. [DOI] [Google Scholar]
- 42.Wang Y., Li X., Chen J., Li F., Ge X., Li J., et al. Nursing effects of targeted psychological intervention in patients with new coronavirus pneumonia and its impact on treatment compliance. Diet Health. 2020;37:142–143. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNzIzEg95aW5zYmoyMDIwMzcxMzIaCDNwMndkZHh4 [Google Scholar]
- 43.Wei N., Huang B.C., Lu S.J., Hu J.B., Zhou X.Y., Hu C.C., et al. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J. Zhejiang Univ. Sci. B. 2020;21(5):400–404. doi: 10.1631/jzus.B2010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang A., Wei S., Hu C., Luo F., Yang R. Analysis of the effect of pneumonia no. 1 prescription combined with shared decision-making psychological counseling therapy in the treatment of mild and common new coronary pneumonia. Contemp. Med. Forum. 2021;19(1):89–91. doi: 10.3969/j.issn.2095-7629.2021.01.062. [DOI] [Google Scholar]
- 45.Zhu L., Ye J., Zhang C., Chen L., Liu Q., Zhao Y., et al. Effect of acceptance and commitment therapy on depression and anxiety in patients with new coronavirus pneumonia. Pract. Clin. Med. 2020;21(10):76–78. doi: 10.13764/J.CNKI.LCSY.2020.10.025. [DOI] [Google Scholar]
- 46.Chen X., Chen Y., Pan X. The effect of bed Baduanjin on the mental health of patients with novel coronavirus pneumonia (COVID-19) Chin. J. Convalescent Med. 2020;29(11):1137–1139. doi: 10.13517/j.cnki.ccm.2020.11.006. [DOI] [Google Scholar]
- 47.Liu K., Chen Y., Wu D., Lin R., Wang Z., Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement. Ther. Clin. Pract. 2020;39 doi: 10.1016/j.ctcp.2020.101132. N.PAG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Özlü İ., Öztürk Z., Karaman Özlü Z., Tekin E., Gür A. The effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID-19: a randomized controlled study. Perspect Psychiatr Care. 2021;57(4):1791–1797. doi: 10.1111/ppc.12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Y., Rao J. The effect of health qigong Yijinjing on the psychological status of patients with new coronavirus pneumonia. Pract. Clin. Med. 2020;21(08):81–83. doi: 10.13764/j.cnki.lcsy.2020.08.027. [DOI] [Google Scholar]
- 50.Zhu L.H., Huang M., Li M., Wang M. Application of cognitive behavioral intervention in the psychological intervention of patients with novel coronavirus pneumonia. Infect. Dis. Inform. 2020;33(05):452–455. doi: 10.3969/j.issn.1007-8134.2020.05.017. [DOI] [Google Scholar]
- 51.Cai L., Li L., Liu J. Evaluation of the role of general practice in the prevention and treatment of new coronavirus pneumonia. World’s Latest Med. Inform. Abstracts (Contin. Electron. J.) 2020;20(98):76–77. doi: 10.3969/j.issn.1671-3141.2020.98.038. [DOI] [Google Scholar]
- 52.Cao X., Zhang Y., Peng J., Sun K. The effect of humanistic care in alleviating anxiety and depression in patients with severe pneumonia caused by the new coronavirus. Chin. Commun. Doctors. 2020;36(27):137–138. doi: 10.3969/j.issn.1007-614x.2020.27.067. [DOI] [Google Scholar]
- 53.Cha F., Peng M., Li L. The influence of family participatory humanized nursing on the negative emotions of patients with common new coronavirus pneumonia. J. Hubei Univ. (Med. Ed.) 2020;37(3):102–104. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEhVoYm16ZHh4Yi15eGIyMDIwMDMwMjYaCGFwNXVwZnBi [Google Scholar]
- 54.Chakeri A., Jalali E., Ghadi M.R., Mohamadi M. Evaluating the effect of nurse-led telephone follow-ups (tele-nursing) on the anxiety levels in people with coronavirus. J. Family Med. Prim. Care. 2020;9(10):5351–5354. doi: 10.4103/jfmpc.jfmpc_847_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen Y. The influence of humanized nursing on the anxiety and satisfaction of patients with new coronary pneumonia. Home Med. 2020;2020(4):319–320. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg1qdHl5MjAyMDA0NDc1GghleGZnMWV6dQ%3D%3D [Google Scholar]
- 56.Deng K., Yuan X., Ren Y., Hu L. Intervention effect of personalized psychological care combined with patient mutual assistance on patients with new coronavirus pneumonia. J. Yangtze Univ. (Self Sci. Ed.) 2020;17(4):101–104. [Google Scholar]
- 57.Dong W., Cui P. The impact of humanistic care on the negative emotion, hope level and quality of life of patients with new coronary pneumonia. Front. Med. 2020;10(18):152–153. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg55aXlxeTIwMjAxODExMRoIMXc0NDg0c2Q%3D [Google Scholar]
- 58.Fan S. Study on the application effect of systematic nursing in patients with suspected new coronary pneumonia. Sci. Health. 2020;23(10):150. http://www.suduzz.com/html/80159787.html [Google Scholar]
- 59.Huang Y., Yu L. Psychological nursing experience on the pessimism of patients with new coronavirus pneumonia. Health Guide. 2020;32:92–93. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNzIzEhF5c2Jqem4teDIwMjAzMjEwNxoINGhxczZjZmk%3D [Google Scholar]
- 60.Li L., Ni J., Jiao J., Li D., Xiao Y., Chen O., et al. Clinical nursing observation on improving negative emotion of patients with novel coronavirus pneumonia by Wuxing music and Liuzi Jue. J. Tradit. Chin. Med. Univ. Hunan. 2021;41(05):765–769. doi: 10.3969/j.issn.1674-070X.2021.05.021. [DOI] [Google Scholar]
- 61.Li L. Observation on the effect of high-quality nursing application in the nursing of new coronary pneumonia. Chin. Commun. Phys. 2020;36(27):144–145. doi: 10.3969/j.issn.1007-614x.2020.27.070. [DOI] [Google Scholar]
- 62.Liu Q. Application of psychological nursing intervention in patients with mild illness in COVID-19 isolation ward. Diet Health. 2020;7(35):170–171. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg95aW5zYmoyMDIwMzUyMTIaCGNnZWl2YWl6 [Google Scholar]
- 63.Liu R., Liu Y., Fu W., Feng J., Zhao X., Gao P. Analysis of the influence of psychological nursing on the nursing effect and satisfaction of patients with new coronavirus pneumonia. Air Force Med. J. 2020;36(03):270–271. doi: 10.3969/j.issn.2095-3402.2020.03.024. [DOI] [Google Scholar]
- 64.Lu X. Analysis of the effect of high-quality nursing application in nursing care of new coronary pneumonia. Diet Health. 2021;2:190. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNzIzEg95aW5zYmoyMDIxMDIxODMaCDhsaHh5amdx [Google Scholar]
- 65.Ma J. Analysis of the intervention effect and satisfaction of high-quality nursing based on humanistic care on patients with COVID-19. Health Guide. 2020;31:136–137. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEhF5c2Jqem4teDIwMjAzMTE1NRoIenRqZm4yZnQ%3D [Google Scholar]
- 66.Nie Y., Wang Y. The impact of humanistic intensive care on the self-efficacy of patients with new coronary pneumonia. Home Med. 2020;4:340–341. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNTIxEg1qdHl5MjAyMDA0NTA1GghybDI3czRvNw%3D%3D [Google Scholar]
- 67.Xu Y., Liu Y. Application of humanistic care in the nursing of patients with novel coronavirus pneumonia. Diet Health. 2020;7(35):210–211. https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjEwNzIzEg95aW5zYmoyMDIwMzUyNjMaCDcyYmpxcWpy [Google Scholar]
- 68.Yang Z. Analysis of the effect of traditional Chinese medicine syndrome differentiation nursing combined with acupoint massage on anxiety and depression of patients in Fangcang shelter hospitals. World Latest Med. Inform. 2021;21(4):287–289. [Google Scholar]
- 69.Zhang Y., Jin C., Zhang F., Chen S., Wu D. The effect of problem-solving care model on the hope and anxiety of patients with novel coronavirus pneumonia. Chin. J. Nurs. 2020;55(S1):598–600. [Google Scholar]
- 70.Zheng C., Wang J., Liu G., Cui H., Wan L., Ni J. Atlas menu-based health education for patients with new coronavirus infection. J. PLA Hosp. Manag. 2021;28(04):354–357. doi: 10.16770/J.cnki.1008-9985.2021.04.020. [DOI] [Google Scholar]
- 71.Zheng Y., Chen S., Lai X., Zhao G. Application of humanistic care with characteristics of traditional Chinese medicine in the treatment of patients with new coronavirus (2019-nCoV) pneumonia. Med. Theory Pract. 2021;34(10):1760–1762. doi: 10.19381/j.issn.1001-7585.2021.10.065. [DOI] [Google Scholar]
- 72.Glasziou P., Sanders S., Hoffmann T. Waste in covid-19 research. BMJ. 2020;369 doi: 10.1136/bmj.m1847. [DOI] [PubMed] [Google Scholar]
- 73.Tangcharoensathien V., Bassett M.T., Meng Q., Mills A. Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York state. BMJ. 2021;32 doi: 10.1136/bmj.n83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jutte J.E., Jackson J.C., Hopkins R.O. In: Psychological and cognitive impact of critical illness. Bienvenu O.J., Hopkins R.O., Jones C., editors. Oxford University Press; 2017. Rehabilitation psychology insights for treatment of critical illness survivors. [DOI] [Google Scholar]
- 75.del Rio C., Collins L.F., Malani P. Long-term health consequences of COVID-19. JAMA. 2020;324(17):1723–1724. doi: 10.1001/jama.2020.19719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Greenhalgh T., Knight M., A’Court C., Buxton M., Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370 doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 77.JPT Higgins, Thomas J., Chandler J., Cumpston M., Li T., Page M.J., et al., editors. Cochrane handbook for systematic reviews of interventions version 6.2 (updated february 2021) Cochrane; 2021. www.training.cochrane.org/handbook Available from. [Google Scholar]
- 78.Azar M., Riehm K.E., Saadat N., et al. Evaluation of journal registration policies and prospective registration of randomized clinical trials of nonregulated health care interventions. JAMA Intern. Med. 2019;179(5):624–632. doi: 10.1001/jamainternmed.2018.8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Park J.J.H., Harari O., Dron L., Lester R.T., Thorlund K., Mills E.J. An overview of platform trials with a checklist for clinical readers. J. Clin. Epidemiol. 2020;125:1–8. doi: 10.1016/j.jclinepi.2020.04.025. [DOI] [PubMed] [Google Scholar]