The impact of heart failure (HF) on patients, physicians, and hospital systems remains despite recent successes in pharmacologic and device-based treatments. Chronic HF represents one of the nation’s top health issues, leading to reduced patient quality of life, increased risks of hospitalization, increased health care utilization, and high incidence of patient morbidity and mortality. Titration of guideline-directed medical therapy and prevention of HF hospitalizations have been identified as key targets in the management of HF. Remote monitoring provides the opportunity to address both issues and has gained significant momentum during the COVID-19 pandemic. Device-based solutions to manage HF remotely, such as CardioMEMS and Boston Scientific HeartLogic, have demonstrated promise for the prevention of HF hospitalizations but are invasive and expensive. A noninvasive system for remote HF monitoring for easy at-home use, Audicor RPM has recently received a FDA Breakthrough Device designation.
HF management with the Audicor RPM is based on cardiac acoustic biomarkers (CABs) that are automatically generated from tens of simultaneously recorded electrocardiographic and heart sound data by means of machine learning algorithms developed on large independently validated clinical databases.1 The CABs most relevant for HF monitoring are electromechanical activation time (EMAT) (ie, QRS onset to the first heart sound interval) and third heart sound (S3) strength (Figure 1A). EMAT has been shown to be prolonged in patients with impaired left ventricular (LV) systolic function and correlates with LV max dP/dt.1 Moyers et al found that EMAT expressed as a proportion of the cardiac cycle (EMATc) >15% was significantly associated with LV dysfunction.2 The S3 is a specific marker of worsening HF in the presence of dyspnea and an independent predictor of adverse clinical outcomes, including the progression of HF.1
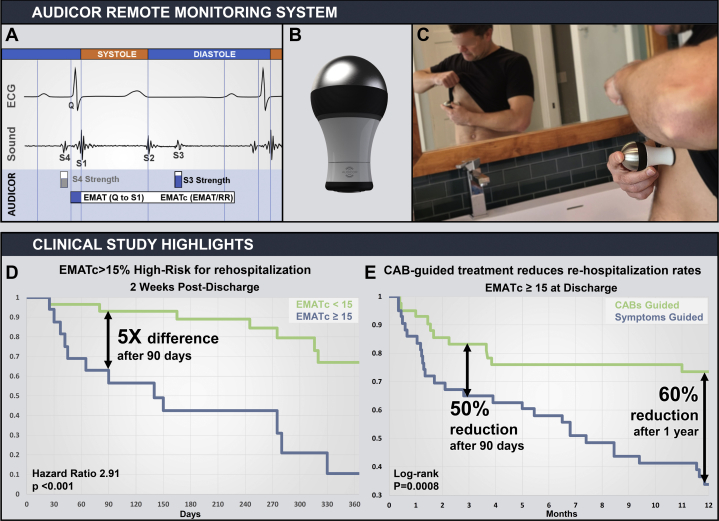
Figure 1.
Audicor Technology, Remote Patient Monitoring (RPM), and Key Clinical Evidence
(Top) (A) Audicor CABs; (B) Audicor RPM recording device; (C) patient taking a recording. (Bottom) Kaplan-Meier curves from (D) Chao et al4 and (E) Sung et al.5 CAB = cardiac acoustic biomarkers; ECG = electrocardiography; EMAT = electromechanical activation time; EMATc = proportion of electromechanical activation time relative to cardiac cycle; S3 = third heart sound.
Wang et al evaluated whether CABs could identify HF patients at high risk for mortality in an HF population (n = 474) followed for a mean of 484 days.3 There were 169 deaths (36%) with 126 (27%) due to cardiac causes. In a multivariate Cox regression analysis controlling for basic demographics, biomarkers, and medications, S3 strength remained an independent predictor for all-cause mortality. Kaplan-Meier analysis showed that subjects having abnormal CABs experienced significantly lower survival (52.2% vs 69.2%; P < 0.001) compared with subjects with CABs not exceeding the abnormal thresholds. The authors concluded that CABs can be a cost-effective and time-efficient tool to identify HF patients who might benefit from close monitoring and intervention and may improve assessment and decision making in HF management.
Chao et al investigated EMAT for prediction of HF readmission or cardiac mortality in patients hospitalized for acute HF (n = 45) and followed for 242 ± 156 days.4 CABs were initially assessed within 24 hours of admission, before discharge, and 2 weeks after discharge. Adverse events, death or readmission, occurred in 44% of patients. Using univariate Cox regression analysis, postdischarge EMATc predicted postdischarge adverse events (hazard ratio [HR]: 2.5; 95% CI: 1.58-3.97). After adjustment for covariates these predictions remained statistically significant. Kaplan-Meier survival analysis showed a statistically significantly reduced event-free survival for patients with prolonged postdischarge EMATc (Figure 1D).
A randomized control trial recently tested Audicor CAB-guided HF management vs symptom-guided management. The evaluated CABs were S3 strength and EMATc.5 Patients hospitalized for HF were randomized before discharge into the CAB-guided group (n = 114) or the symptom-guided group (n = 111). After a mean follow-up of 238 ± 141 days, a reduction in the primary end points was seen in the CAB-guided group vs the symptom-guided group (43 vs 61 events; P < 0.001). The time to first event favored the CAB-guided group (n = 225; HR: 0.61; 95% CI: 0.42-0.91; log-rank P = 0.013) over the control group and a similar benefit was seen in the subgroup of patients (Figure 1E) with a predischarge EMATc >15%, (n = 85; HR: 0.32; 95% CI: 0.16-0.65; log-rank P < 0.001).
The above studies were performed with the use of a commercially available Audicor device that adhered to the patient with standard electrodes. The novel Audicor RPM is a hand-held device intended for at-home use in HF management (Figures 1B and 1C) that uses the same commercially available algorithms and equivalent signal acquisition techniques as previous Audicor devices. Cardiac acoustic and electrical signals are acquired from a single position on the chest (V4). The device connects to the internet for Audicor cloud analysis, resulting in CAB trends available for clinician review with automated alerts for risk of HF decompensation based on fixed measurement thresholds, which can be customized per patient. This new system allows the previous CAB-guided HF management methods to be applied in a remote monitoring model with minimal physician involvement. Early identification of HF deterioration allows intervention and modification of medications, thus preventing hospital readmission.
A prospective randomized trial of the Audicor RPM system for remote (at-home) monitoring to evaluate the safety and effectiveness of CAB-guided HF management vs symptom-guided management on patients previously hospitalized for HF is under design development in collaboration with the FDA through the Breakthrough Device program. Eligible institutions, predominantly in the U.S., will begin enrolling patients in 2022.
Footnotes
Dr Fudim is a consultant for and member of the Scientific Advisory Board for Inovise Medical. Dr Mirro is the Medical Director of Inovise Medical. Dr Cheng is a consultant for Inovise Medical.
Editor’s Note: To view the authors’ full presentation at TCTMD Shark Tank, please visit https://www.jacc.org/journal/basic-translational/tht-2022-shark-tank.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Erne P. Beyond auscultation: acoustic cardiography in the diagnosis and assessment of cardiac disease. Swiss Med Wkly. 2008;138(31-32):439–452. doi: 10.4414/smw.2008.12308. [DOI] [PubMed] [Google Scholar]
- 2.Moyers B., Shapiro M., Marcus G.M., et al. Performance of phonoelectrocardiographic left ventricular systolic time intervals and B-type natriuretic peptide levels in the diagnosis of left ventricular dysfunction. Ann Noninvasive Electrocardiol. 2007;12:89–97. doi: 10.1111/j.1542-474X.2007.00146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang S., Liu M., Fang F., et al. Prognostic value of acoustic cardiography in patients with chronic heart failure. Int J Cardiol. 2016;219:121–126. doi: 10.1016/j.ijcard.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Chao T.F., Sung S.H., Cheng H.M., et al. Electromechanical activation time in the prediction of discharge outcomes in patients hospitalized with acute heart failure syndrome. Intern Med. 2010;49(19):2031–2037. doi: 10.2169/internalmedicine.49.3944. [DOI] [PubMed] [Google Scholar]
- 5.Sung S.H., Huang C.J., Cheng H.M., Huang W.M., Yu W.C., Chen C.H. Effect of acoustic cardiography-guided management on 1-year outcomes in patients with acute heart failure. J Card Fail. 2020;26(2):142–150. doi: 10.1016/j.cardfail.2019.09.012. [DOI] [PubMed] [Google Scholar]