Abstract
Capitalizing on a longitudinal cohort followed from gestation through adolescence (201 mother-child dyads), we investigate the contributions of severity and stability of both maternal depressive and perceived stress symptoms to adolescent psychopathology. Maternal depressive and perceived stress trajectories from pregnancy through adolescence were identified with latent class growth analyses, and associations with adolescent internalizing and externalizing symptoms were examined. For both depression and stress, the most common trajectory group comprised mothers displaying stable and low symptom levels over time, and adolescents of these mothers had the fewest internalizing and externalizing symptoms. Maternal membership to one or more aberrant trajectory groups predicted higher levels of internalizing and externalizing symptoms, determined by both maternal and adolescent self-report. This study indicates that profiles of multiple indicators of maternal psychopathology assessed across childhood, beginning prenatally, can provide critical additional insight into child psychopathology risk.
Keywords: maternal psychological distress, early adolescent internalizing symptoms, early adolescent externalizing symptoms, latent class growth analyses
Introduction
Compared to other species, even among our closest primate relatives, humans are unique in the amount of parental care required to raise offspring to reproductive age [1]. Children are heavily reliant on parents for many years of their lives and sensitive periods of brain development largely overlap with developmental stages during which the child is dependent on the mother [2]. Because both stressful and supportive rearing environments have existed throughout human history, natural selection has shaped developmental systems to respond to indicators of environmental conditions, and it is posited that parenting and other family processes serve as a primary indicator or a “weather forecast” for the developing child [3,4]. Consistent with these conceptual models is a body of work indicating that pre- and postnatal maternal behaviors and emotional states are principal determinants of offspring psychopathology [5,6,7,8,9,10].
The vast majority of studies examining maternal mental health and child development focus on a single diagnosis or symptom profile (e.g., depression, schizophrenia, stress), despite the high degree of comorbidity among different psychological disorders [11]. Furthermore, to date, most studies have focused only on maternal depression and associated child outcomes [9,12]. However, it is likely that exposure to multiple indicators of psychological distress exerts cumulative effects on children. This seems probable because children’s cumulative exposures to multiple environmental risk factors (e.g., maltreatment, low socioeconomic status) are associated with increased risk for developing subsequent psychopathology, such that those experiencing a higher number of risk factors display more severe symptomology [13,14,15].
In addition to assessing the singular versus cumulative effects of risk exposures in early life, increasing attention has also been paid to the consistency or patterns of those exposures over time. It recently has been argued that stability or patterns of maternal mental health across developmental periods may be an important determinant of child mental health [16,17,18]. Studies that have examined clinical diagnosis status at multiple postnatal developmental timepoints indicate that in addition to exposures to depressive episodes, the patterns and chronicity of those exposures also matter [19,20]. Building upon these findings are analytic methodologies allowing examination of latent trajectory classes of mental health symptoms over time to reveal distinct symptom profiles, rather than simply the presence or absence of a mental health diagnosis or symptom profile at a single timepoint (see Nandi, Beard, & Galea, 2009 [21] for a review). Marked consistencies exist across studies applying latent trajectory approaches to maternal depression. Children of mothers who exhibit stable and low profiles of psychological distress compared to those in other profile groups (e.g., chronically high, intermittent, increasing and decreasing) are at the lowest risk for psychopathology [22,23,24,25,26,27,28,29]. Notably, Cents et al. [24] demonstrated that trajectory modeling of maternal depressive symptoms was of added value in predicting child psychopathology compared to previous, more conventional approaches to characterizing maternal depression profiles including severity (defined as mean symptom scores across time) and chronicity (number of assessments at which the mother scored above the clinical cutoff). Taken together, these observations raise the question of whether examining trajectories of multiple indicators of maternal distress from the prenatal period through the transition period to early adolescence might reveal new insight into the associations between cumulative exposures to maternal mental health profiles and risk for child psychopathology.
The Current Study
Capitalizing on a longitudinal cohort followed prospectively from fetal life through early adolescence, the current study aims to expand beyond existing investigations of latent maternal mood profiles by examining the joint and separate contributions to child and preadolescent psychopathology of profiles of two maternal mental health indicators, perceived stress and depressive symptoms. We hypothesized that children of mothers with high levels of depressive or perceived stress symptoms from pregnancy through childhood would exhibit elevated internalizing and externalizing symptoms. We also expected cumulative associations between maternal psychological distress and child psychopathology such that children of mothers with greater levels of both depressive and perceived stress symptoms would experience the largest number of internalizing and externalizing symptoms.
Methods
Study Overview
Participants were mother-child dyads from prospective longitudinal studies of early life influences on development. Mood and stress were evaluated in mothers during pregnancy and postnatally until the child was an early adolescent.
Assessments of maternal depressive symptoms and perceived stress were conducted at five time points during pregnancy, 2-3 months after the child’s birth, when the child was 6-9 years of age (perceived stress only) and when the child was between 10-13 years of age (N = 271; see Figure S1). Child internalizing and externalizing symptoms were assessed when the children were between the ages of 10-13.
Participants
Eligibility criteria for this study included previous participation in one of two prospective longitudinal studies of prenatal and early life influences on development with identical eligibility criteria. Participants were originally recruited during pregnancy from Southern California obstetric clinics and were invited to participate if they were English-speaking and over the age of 18 with singleton pregnancies less than 20 gestational weeks. Women were excluded if they had any uterine or cervical abnormalities, neuroendocrine dysfunction, or if they self-reported tobacco, alcohol, or drug use during pregnancy. Mother-child pairs were included if child internalizing and externalizing outcome data were available at 10-13 years of age. Child outcome data were collected between 2013 and 2020. For complete descriptive information for mothers and children, see Table 1.
Table 1. Descriptive Statistics.
Sample characteristics by co-occurring trajectory group membership.
| Maternal Characteristics (N = 271)1 |
Overall sample | Stable-Low/ Stable-Low Trajectory Groups (n = 137) |
Stable-Low/Not Stable-Low Trajectory Groups (n = 60) |
Not Stable-Low /Not Stable-Low Trajectory Groups (n = 73) |
χ2/F |
|---|---|---|---|---|---|
| Age at delivery (M ± SD) | 30.5 ± 5.6 | 30.6 ± 5.3 | 30.6 ± 6.2 | 30.2 ± 5.6 | F(2, 267) = 0.13, p = .879 |
| Prenatal medical risk (M ± SD) | 0.4 ± 0.6 | 0.4 ± 0.6 | 0.3 ± 0.5 | 0.5 ± 0.7 | F(2, 255) = 2.44, p = .090 |
| Cohabitating with child’s father (%) | |||||
| Prenatal | 87.4 | 93.9 | 88.3 | 74.3 |
χ2 (2, N = 262) = 16.11, p <.001 χ2 (6, N = 198) = 23.30, p = 001 |
| Current | 69.7 | 75.2 | 80.9 | 48.0 | |
| Household income (M ±SD) | |||||
| Prenatal | 66,156 ± 31,502 | 72,218 ± 28,773 | 61,083 ± 33,371 | 59,063 ± 33,117 | F(2, 262) = 5.21, p = .006 |
| Current | 151,644 ± 173,093 | 183,898 ± 223,181 | 127,330 ± 83,562 | 107,239 ± 78,392 | F(2,190) = 3.87, p = .022 |
| Prenatal Income-to-needs ratio (M ± SD) | 448.1 ± 250.6 | 494.7 ± 236.8 | 394.8 ± 250.2 | 407.8 ± 262.8 | F(2,260) = 4.69, p = .010 |
| Education (%) | |||||
| High school or less Some college, Vocational, or | 14.8 | 12.5 | 17.3 | 16.7 | χ2 (8, N = 244) = 6.17, p =.628 |
| Associates degree | 37.3 | 33.3 | 41.4 | 40.9 | |
| Bachelor’s degree | 31.1 | 35.0 | 29.3 | 25.8 | |
| Graduate degree | 16.8 | 19.2 | 12.1 | 16.7 | |
| Race and ethnicity (%) | |||||
| Non-Hispanic White | 46.1 | 41.6 | 53.3 | 47.9 | χ2 (10, N = 270) = 9.88, p = .451 |
| Latinx | 28.0 | 33.6 | 26.7 | 19.2 | |
| Asian | 11.4 | 11.7 | 8.3 | 13.7 | |
| African American or Black | 5.2 | 5.1 | 5.0 | 5.5 | |
| Native American or Alaskan Native | 0.4 | 0.0 | 0.0 | 1.4 | |
| Multi-Ethnic | 8.9 | 48.0 | 6.7 | 12.3 | |
| Child Characteristics (N = 201) |
Overall sample | Stable-Low/ Stable-Low Trajectory Groups (n = 102) |
Stable-Low/ Not Stable-Low Trajectory Groups (n = 47) |
Not Stable-Low /Not Stable-Low Trajectory Groups (n = 52) |
|
| Age at child assessment (M ± SD) | 6.5 ± 0.2 | 6.5 ± 0.1 | 6.6 ± 0.2 | 6.5 ± 0.2 | F(2, 69) = 1.49, p = .233 |
| Age at early adolescent assessment (M ± SD) | 12.0 ± 0.9 | 12.0 ± 0.9 | 11.9 ± 0.9 | 12.1 ± 1.0 | F(2, 198) = 0.74, p = .478 |
| Sex (% male) | 51.7 | 52.9 | 51.1 | 50.0 | χ2 (2, N = 201) = 0.13, p = .937 |
| Percentage first born (%) | 47.8 | 52.0 | 36.2 | 50.0 | χ2 (2, N = 201) = 336, p = .187 |
| Race and etdnicity (%) | |||||
| Non-Hispanic White | 41.8 | 41.2 | 42.6 | 42.3 | χ2 (10, N = 201) = 15.59, p = .112 |
| Latinx | 37.8 | 42.2 | 36.1 | 30.7 | |
| Asian | 6.5 | 8.8 | 2.1 | 5.8 | |
| African American or Black | 2.5 | 1.0 | 2.1 | 5.8 | |
| Multi-Ethnic | 11.4 | 6.9 | 17.0 | 15.4 | |
| Birth Phenotype (N=201) |
Overall sample | Stable-Low/ Stable-Low Trajectory Groups (n = 102) |
Stable-Low/Not Stable-Low Trajectory Groups (n = 47) |
Not Stable-Low /Not Stable-Low Trajectory Groups (n = 52) |
|
| Gestational age at birth (M ± SD) | 39.3 ± 1.5 | 39.5 ± 1.1 | 39.4 ± 1.2 | 38.9 ± 2.2 | F(2, 197) = 3.19, p = .043 |
| Birth weight (g) (M ± SD) | 3,452 ± 518 | 3,469 ± 481 | 3,456 ± 552 | 3,416 ± 564 | F(2, 194) = 0.18, p = .840 |
Thirty-two women participated in the study with more than one pregnancy. To verify that the inclusion of these women did not alter our findings, we repeated our analyses after excluding pregnancy and child outcome data from mothers with more than one pregnancy. Cases with less comp lete data were removed. All associations between maternal psychological distress and child internalizing and externalizing symptoms were highly consistent with our original findings.
Note. Stable-Low/Stable-Low trajectory groups comprises women who exhibited low and stable levels of both depressive and perceived stress symptoms, Stable-Low/Not Stable-Low trajectory groups comprises women who exhibited low and stable levels of either depressive symptoms or perceived stress symptoms, and Not Stable-Low/Not Stable-Low trajectory groups comprises women who did not exhibit low and stable levels of either depressive or perceived stress symptoms.
Procedure
Maternal Psychological Assessments
Maternal depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale Short Form (CESD-SF [30]). The scale contains 9 items measured on a four-point Likert scale. Participants are asked to rate depressive symptoms within a range of 0 (“rarely or none of the time (less than 1 day)) to 3 (“most or all of the time (5-7 days), with a higher total score (max. 27) indicating greater endorsement of depressive symptoms. The CES-D is internally consistent and has been validated for use in ethnically diverse pregnant samples [31].
The 10-item version of Cohen’s Perceived Stress Scale (PSS [32]) was used to measure generalized/non-specific stress. The scale contains items assessing perceived control over life events, confidence about handling personal problems, and ability to manage irritations. Responses on the 5-point Likert scale range from 0 (never) to 4 (almost always), with a maximum final score of 40. The PSS also has good internal consistency and has been used reliably with a range of samples, including pregnant women [8].
Child Internalizing and Externalizing
Child Behavior Checklist.
Maternal report of child internalizing and externalizing symptoms was assessed using the Child Behavior Checklist (CBCL) from the Achenbach System of Empirically Based Assessment (ASEBA). The ASEBA measures adaptive and maladaptive functioning. The CBCL displays high test retest stability and is internally consistent [33]. The Child Behavior Checklist (CBCL) has been used to predict psychopathology during adolescence, including anxiety, depressive, and disruptive behavior disorders [34]. The CBCL contains 113 items capturing a wide range of behaviors. Responses are made using a 3-point Likert scale from 0 (not true) to 2 (very true). The instrument contains eight empirically-based syndrome subscales. From the subscales, scores for three composite scales (Internalizing Behavior, Externalizing Behavior, and Total Problems) are calculated.
Youth Self Report.
Child self-report of internalizing and externalizing was measured using ASEBA’s Youth Self Report/11-18 (YSR) form. Initially designed for 11-18 year old children, the YSR also has been validated for use in younger children age 7-10 [35] suggesting it is appropriate for the 10-13-year-old children in the present study. It is a measure parallel to the CBCL, containing the same subscales and 3-point Likert response scale. The YSR also has high test retest stability and has good internal consistency [33].
Data Analysis
Maternal stress and mood trajectories.
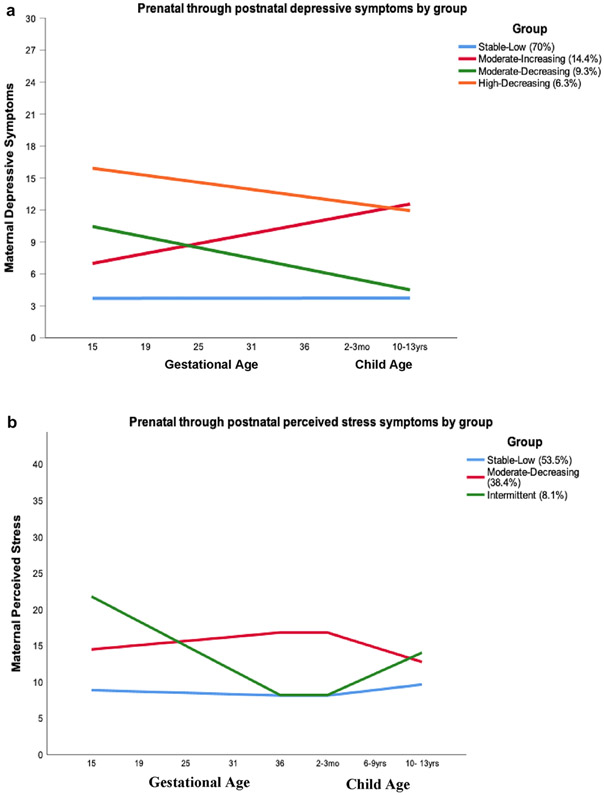
In preparation for investigating our aims, we conducted latent class growth analyses to identify distinct groups of subjects with different combinations of stress and depressive symptom trajectories from pregnancy through 13 years postpartum. These analyses were conducted for all available cases (N = 271), using full-information maximum likelihood with robust standard errors as the estimator. Models were tested successively, comparing bootstrapped parametric likelihood ratio test p values and Bayesian Information Criterion (BIC) values in each iteration to determine whether there was a statistically significant improvement in fit for the model with each additional class. The best fitting model was then selected for prenatal through postnatal depressive symptoms, which consisted of four latent trajectory groups; a stable-low symptoms group, a moderate-increasing symptoms group, a moderate-decreasing symptoms group, and a high-decreasing symptoms group (Figure 1A). The best fitting model for prenatal through postnatal perceived stress symptoms consisted of three groups; a stable-low symptoms group, a moderate-decreasing symptoms group, and an intermittent symptoms group (Figure 1B). The stable-low symptoms groups were the largest for both depressive and stress symptoms (70% and 53.5% of mothers, respectively). These analyses were conducted using Mplus, version 8.4. Additional details about the latent class models and model fit are provided in the supplement.
Figure 1.
a Latent trajectory groups of depressive symptoms in the prenatal through postpartum period (N = 270)
b Latent trajectory groups of perceived stress in the prenatal through postpartum period (N = 271)
Note. The largest group (n = 189, 70.0%) consisted of women who reported stable and low levels of depressive symptoms through pregnancy and postpartum (Stable-Low Group). The second largest trajectory pattern comprised women who started pregnancy with a low level of depressive symptoms that increased steadily through gestation and continued into the postpartum period (Moderate-Increasing Group; n = 39, 14.4%). Women who reported elevated depressive symptoms early in pregnancy with levels decreasing through gestation and into the postpartum period were clustered in the Moderate-Decreasing Group (n = 25, 9.3%). The fourth profile was characterized by relatively higher, but stable levels of symptoms across the pregnancy through postpartum time period (High-Decreasing Group) (n = 17, 6.3%). The group depressive symptom means at each time point are as follows: T1 (15 weeks’ gestation) M = 0.70, SD = 0.58; T2 (19 weeks’ gestation) M = 0.70, SD = 0.57; T3 (25 weeks’ gestation) M = 0.73, SD = 0.57; T4 (31 weeks’ gestation) M = 0.80, SD = 0.61; T5 (36 weeks’ gestation) M = 0.84, SD = 0.57; T6 (3 months postpartum) M = 0.59, SD = 0.55; T7 (child age 10-13) M = 0.56, SD = 0.51.
Note. Most women (n = 145, 53.5%) reported the pattern of stable and low levels of perceived stress from pregnancy through postpartum (Stable-Low Group). Women who reported moderate levels of perceived stress throughout the prenatal through postpartum period made up the second largest group (n = 104, 38.4%) (Moderate-Decreasing Group). The third and smallest group (n = 22, 8.1%) consisted of women with a more dynamic profile characterized by a decrease across gestation and an increase across the postnatal period (Intermittent Group). The group perceived stress means at each time point are as follows: T1 (15 weeks’ gestation) M = 1.30, SD = 0.65; T2 (19 weeks’ gestation) M = 1.27, SD = 0.66; T3 (25 weeks’ gestation) M = 1.20, SD = 0.72; T4 (31 weeks’ gestation) M = 1.26, SD = 0.73; T5 (36 weeks’ gestation) M = 1.27, SD = 0.69; T6 (3 months postpartum) M = 1.17, SD = 0.66; T7 (child age 6-9) M = 1.15, SD = 0.65; T8 (child age 10-13) M = 1.15, SD = 0.57.
Maternal stress and mood trajectories and adolescent outcomes.
We used univariate analyses of covariance (ANCOVA) to investigate whether maternal stress and depression latent trajectory groups separately predicted child and maternal report of internalizing and externalizing symptoms. Then, we examined whether consideration of maternal mental health trajectories of both depressive symptoms and stress together provides additional power to predict child internalizing and externalizing symptoms. Further, because of literature suggesting that there may be sexually dimorphic responses in exposures to prenatal and early life adversity [22,23,36], child sex by group interaction was examined. The results of these models are presented in the supplemental materials.
Covariates.
Based on previously established predictors of child mental health [15,37,38,39,40], child sex, income-to-needs ratio and maternal cohabitation with the child’s father were included as covariates in all analyses. The percentage of participants missing covariate data was 2.9% for income-to-needs ratio and maternal cohabitation with the child’s father. Child sex was not missing for any participants. Missing values for income-to-needs ratio were imputed through Expectation Maximization. Missing values for maternal cohabitation were single imputed to “not living with father.” Additional information about the relation of sociodemographic variables to the latent classes and child internalizing and externalizing symptoms is included in Table 1.
Results
Maternal Depressive Symptom Trajectories from Pregnancy Through Early Adolescence
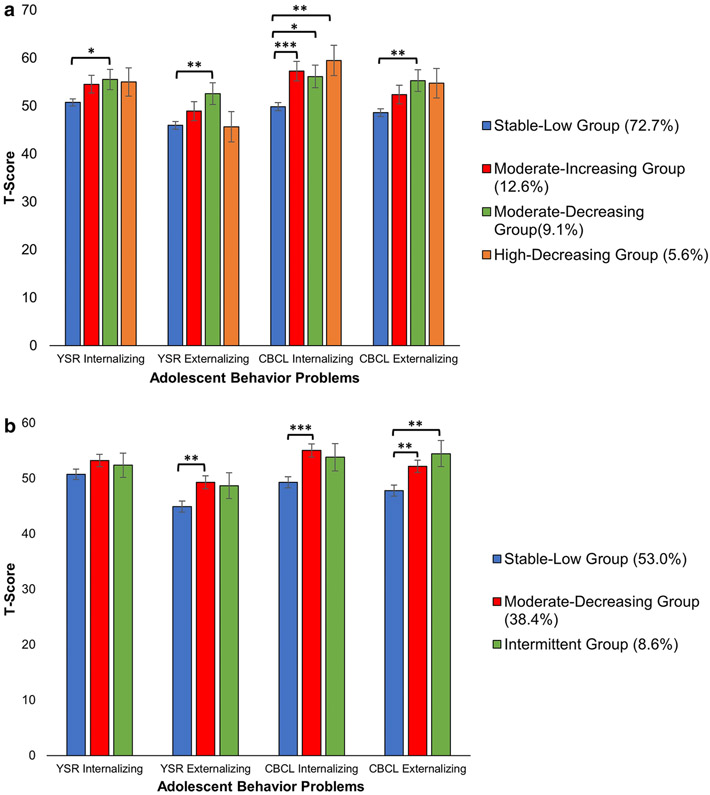
As shown in Figure 2A, mothers reporting stable and low depressive symptoms (Group 1) were most likely to have children with the lowest levels of internalizing and externalizing symptoms. Conversely, mothers belonging to any of the other three groups were more likely to have children with elevated levels of internalizing and externalizing symptoms. ANCOVAs confirmed group differences in both internalizing and externalizing symptoms according both to child self-report (internalizing: F(3, 188) = 2.64, p = .051, ηp2 = .04; externalizing: F(3, 188) = 2.87, p = .038, ηp2 = .04), and maternal report (internalizing: F(3, 191) = 7.48, p < .001, ηp2 = .11; externalizing: F(3, 191) = 4.05, p = .008, ηp2 = .06).
Figure 2.
a Child internalizing and externalizing behavior based on prenatal through postnatal maternal depressive symptom trajectory group membership
b Child internalizing and externalizing behavior based on maternal perceived stress class membership prenatally through postnatally
Note. Post-hoc comparisons were performed using the LSD test.
*p ≤ .05 **p ≤ .01 ***p ≤ .001
Maternal Perceived Stress Trajectories from Pregnancy Through Early Adolescence
Children whose mothers reported the pattern of stable and low perceived stress symptoms (Group 1) exhibited the fewest internalizing and externalizing symptoms compared with children whose mothers exhibited other patterns (Figure 2B). Differences based on maternal latent class profiles were present for maternal report of both internalizing and externalizing symptoms (F(2, 192) = 7.07, p = .001, ηp2 = .07; F(2, 192) = 6.18, p = .003, ηp2 = .06, respectively) and child self-report of externalizing symptoms (F(2, 189) = 4.31, p = .015, ηp2 = .04), but not for child self-report of low levels of internalizing symptoms (F(2, 189) = 1.53, p = .219, ηp2 = .02).
Examination of the Joint Contributions of Depressive Symptoms and Perceived Stress: Co-Occurring Trajectory Groups
To examine the joint contributions of latent trajectory group membership, we initially categorized women into 9 co-occurring trajectory groups based on their membership status for both perceived stress and depression (e.g., Stable-Low CES-D/Stable-Low PSS, Moderate-Decreasing CES-D/Stable-Low PSS, Stable-Low CES-D/Intermittent PSS, etc.). As presented in supplemental Table 1, for both maternal and child self-report of internalizing and externalizing symptoms, children whose mothers belonged to the Stable-Low CES-D/Stable-Low PSS group, exhibited the fewest symptoms. To minimize the number of statistical comparisons and create a variable reflecting stability and severity of symptoms, the sample was divided into the following three groups: those with membership in the stable-low groups for both depression and perceived stress (50.7%), those with membership in one stable-low group only (23.4%), and those who did not belong to a stable-low group for either depression or perceived stress (25.9%).
Children whose mothers reported stable and low levels of both depression and perceived stress exhibited the fewest symptoms of psychopathology (Figure 3). Specifically, these children had the lowest mean levels of internalizing and externalizing symptoms, according both to self and maternal report. In comparison, children whose mothers did not have membership in either of the stable-low groups for depression or stress, exhibited the highest levels of internalizing and externalizing symptoms. Finally, mothers who belonged to only one stable-low group for depression or stress had children with levels of internalizing and externalizing symptoms that fell between the symptom levels of children with mothers in the other two categories. ANCOVAs confirmed that the mean differences shown in Figure 3 were present for both child self-report (internalizing: F(2, 189) = 3.22, p = .042, ηp2 = .03; externalizing: F(2, 189) = 4.97, p = .008, ηp2 = .05), and maternal report (internalizing: F(2, 192) = 12.02, p < .001, ηp2 = .11; externalizing: F(2, 192) = 7.57, p = .001, ηp2 = .07).
Figure 3.
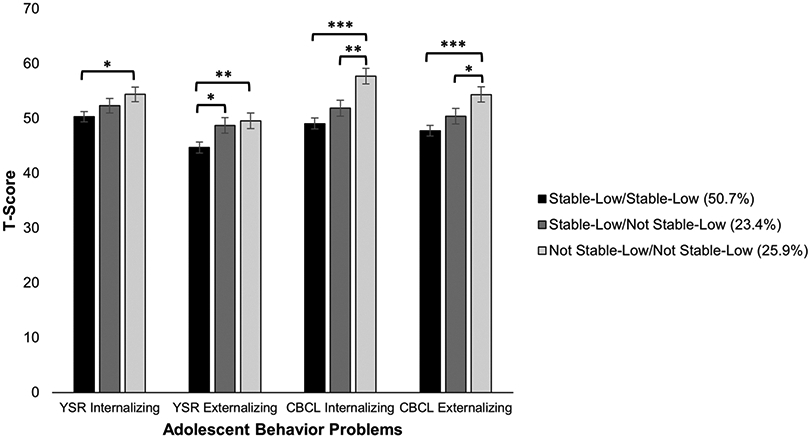
Child internalizing and externalizing behavior based on maternal group membership to the Stable-Low trajectory groups
Note. Mothers were grouped into the Stable-Low/Stable-Low trajectory group if they belonged to both of the stable, low symptoms trajectory groups for depression and stress (50.7%), the Stable-Low/Not Stable-Low trajectory group if they belonged to at least one stable, low symptoms group (23.4%), and the Not Stable-Low/Not Stable-Low trajectory group if they did not belong to either stable, low symptoms group (25.9%). Post-hoc comparisons were performed using the LSD test.
*p ≤ .05 **p ≤ .01 ***p ≤ .001
Discussion
We found that patterns of maternal mental health symptoms over a period of up to 13 years, beginning prenatally, are associated with internalizing and externalizing symptoms during early adolescence. There was remarkable consistency in the latent trajectory profiles of maternal depressive and perceived stress symptoms; in all cases, a stable-low group was identified, which comprised the majority of women. Maternal membership in both of the stable-low depression and stress trajectory groups consistently was associated with optimal child mental health in that these children exhibited the lowest levels of maternal and self-reported internalizing and externalizing symptoms. Children of mothers who did not belong to the stable-low group for either depression or stress displayed the greatest number of internalizing and externalizing symptoms, and children with mothers belonging to only one stable-low group had levels of internalizing and externalizing symptoms between the extreme groups. These observations are consistent with current conceptualizations of early life adversity that emphasize both magnitude of exposure and the stability or predictability of those exposures as representing distinct and meaningful dimensions of early childhood adversity [16,17,18,41].
These findings corroborate the existing literature on latent trajectories of maternal mood and also expand it in several ways. First, other studies have found associations between trajectories of stable and low maternal psychological distress symptoms and more optimal child emotional, behavioral, and neurodevelopmental outcomes [24,26,27,42,43,44,45]. Our study extends this work by examining latent trajectories of both maternal depression and perceived stress in relation to child internalizing and externalizing symptoms and shows that consideration of their joint contributions improves the prediction of risk for child psychopathology. Second, the current study found consistency between both child internalizing and externalizing symptoms in association with maternal psychological distress. These observations align with evidence that maternal depressive symptoms may be more broadly predictive of child psychopathology rather than unique internalizing and externalizing problems or diagnoses [46].
A key strength of the current study is the large, prospective sample followed from the prenatal period through child age 13. Additionally, a novel contribution is the characterization of longitudinal trajectories of maternal perceived stress, and the evidence that exposure to maternal perceived stress contributes to child psychopathology risk. Finally, the consistency of results across both maternal and child self-report of internalizing and externalizing symptoms gives us increased confidence in the findings.
A limitation of this study is that the current sample consists primarily of socioeconomically low-risk families. The nature of this sample may have contributed to the small to medium effect sizes that were observed between maternal and child psychopathology. Additionally, the majority of children in the current study had YSR and CBCL T-scores that were in the non-clinical range. The mean T-score for children of mothers in the High-Decreasing depression/Moderate-Decreasing stress trajectory group was the highest of all co-occurring trajectory groups at 63.0, which is in the borderline clinical range (Table S1). Therefore, our ability to generalize these findings to higher risk samples is limited. However, the fact that we found significant associations between maternal psychological distress and child psychopathology in a community sample with restricted ranges suggests that these associations may be further magnified in a clinical sample. Finally, the correlational nature of the study prevents us from concluding that exposure to maternal depression and stress plays a causal role in risk for psychopathology in children.
There are biological, neurological, and environmental pathways through which maternal psychological distress may associate with child psychopathology, depending on the developmental stage of exposure. For example, compromised maternal mental health during pregnancy likely affects fetal neurodevelopment through endocrine, immune, and/or epigenetic pathways [47,48,49]. Compromised maternal care in infancy and negative parent-child relationships in childhood also may serve as a pathway between maternal psychological distress and child emotional and behavioral outcomes [50,51]. For example, mothers experiencing depression may exhibit less sensitive parenting, which can elicit angry and hostile behaviors in children [52]. Additionally, children may learn to model negative maternal cognitions, behavior, and affect, resulting in internalizing and externalizing symptoms [53].
The current study has implications for the clinical assessment and treatment of both mothers and children suffering from mental health problems. Understanding how maternal mental health changes over time can help to identify children at risk for adverse outcomes. Similarly, the observation that cumulative exposures to maternal psychological distress beyond the pre- and postnatal periods have implications for child mental health, suggest that additional screening for maternal psychopathology at pediatric visits throughout childhood may prove to be beneficial for identifying mothers and children in need of mental health treatment.
The current study strongly supports a broad conceptualization of the role of maternal psychopathology--one that considers multiple indicators of psychopathology conjointly, as well as their stability over time. It also provides support for conceptual models emphasizing the potency of cumulative exposures to adversity during development, showing that cumulative effects can be detected by consideration of more than one indicator within the domain of maternal psychological distress. Given the large degree of overlap between sensitive periods of brain development and developmental stages that necessitate maternal care, consideration of maternal psychological distress across domains and across time can advance understanding of how maternal psychopathology shapes the developing brain and contributes to manifestations of child psychopathology.
Summary
Despite emerging dimensional models of psychopathology illustrating robust commonalities among many forms of mental illness, studies have focused primarily on maternal depressive symptoms and associated child psychosocial outcomes. Therefore, the current study investigated the cumulative contributions of both maternal depressive and perceived stress symptoms to psychopathology during the transition to adolescence with a longitudinal cohort followed from gestation through early adolescence. We found that, for both depression and stress, the largest latent trajectory group comprised mothers displaying stable and low symptom levels over time. Children of mothers in stable-low groups for both depression and stress exhibited the fewest internalizing and externalizing symptoms, those with mothers in one stable-low group displayed greater internalizing and externalizing symptoms, and those whose mothers were not members of either stable-low group demonstrated the highest internalizing and externalizing symptoms.
Supplementary Material
Footnotes
Compliance with Ethical Standards
The authors declare that they have no conflict of interest. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Publisher's Disclaimer: This AM is a PDF file of the manuscript accepted for publication after peer review, when applicable, but does not reflect postacceptance improvements, or any corrections. Use of this AM is subject to the publisher's embargo period and AM terms of use. Under no circumstances may this AM be shared or distributed under a Creative Commons or other form of open access license, nor may it be reformatted or enhanced, whether by the Author or third parties. See here for Springer Nature's terms of use for AM versions of subscription articles: https://www.springernature.com/gp/open-research/policies/accepted-manuscript-terms
References
- 1.Hahn-Holbrook J, Holbrook C, Haselton MG (2011) Parental precaution: Neurobiological means and adaptive ends. Neurosci Biobehav Rev 35(4):1052–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuzawa CW, Quinn EA (2009) Developmental origins of adult function and health: Evolutionary hypotheses. Annu Rev Anthropol 38:131–147 [Google Scholar]
- 3.Bateson P, Barker D, Clutton-Brock T, Debal D, D’Udine B, Foley RA et al. (2004) Developmental plasticity and human health. Nature 430:419–421 [DOI] [PubMed] [Google Scholar]
- 4.Belsky J, Steinberg L, Draper P (1991) Childhood experience, interpersonal development, and reproductive strategy: An evolutionary theory of socialization. Child Dev 62(4):647–670 [DOI] [PubMed] [Google Scholar]
- 5.Barker ED, Jaffee SR, Uher R, Maughan B (2011) The contribution of prenatal and postnatal maternal anxiety and depression to child maladjustment. Depress Anxiety 28:696–702 [DOI] [PubMed] [Google Scholar]
- 6.Davis EP, Sandman CA (2012) Prenatal psychobiological predictors of anxiety risk in preadolescent children. Psychoneuroendocrinology 37(8):1224–1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis EP, Hankin BL, Glynn LM, Head K, Kim DJ, Sandman CA (2020) Prenatal maternal stress, child cortical thickness, and adolescent depressive symptoms. Child Dev 91(2):e432–e450 [DOI] [PubMed] [Google Scholar]
- 8.Glynn LM, Howland MA, Sandman CA, Davis EP, Phelan M, Baram TZ et al. (2018) Prenatal maternal mood patterns predict child temperament and adolescent mental health. J Affect Disord 228:83–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D (2011) Maternal depression and child psychopathology: A meta-analytic review. Clin Child Fam Psychol Rev 14:1–27 [DOI] [PubMed] [Google Scholar]
- 10.Talge NM, Neal C, Glover V (2007) Antenatal maternal stress and long-term effects on child neurodevelopment: How and why? J Child Psychol Psychiatry 48(3-4):245–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessler RC, Wai TC, Demler O, Walters EE (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:617–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaffee SR, Sligo JL, McAnally HM, Bolton AE, Baxter JM, Hancox RJ (2020) Early-onset and recurrent depression in parents increases risk of intergenerational transmission to adolescent offspring. J Child Psychol Psychiatry doi: 10.1111/jcpp.13356 [DOI] [PubMed] [Google Scholar]
- 13.Appleyard K, Egeland B, van Dulmen MHM, Sroufe LA (2005) When more is not better: The role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry 46(3):235–245 [DOI] [PubMed] [Google Scholar]
- 14.Deater-Deckard K, Dodge KA, Bates JE, Pettit GS (1998) Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Dev Psychopathol 10:469–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evans GW, Cassells RC (2014) Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clin Psychol Sci 2(3):287–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glynn LM, Baram TZ (2019) The influence of unpredictable, fragmented parental signals on the developing brain. Front Neuroendocrinol 53:100736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ellis BJ, Figueredo AJ, Brumbach BH, Schlomer GL (2009) Fundamental dimensions of environmental risk. Nat 20(2):204–268 [DOI] [PubMed] [Google Scholar]
- 18.Hartman S, Sung S, Simpson JA, Schlomer GL, Belsky J (2018) Decomposing environmental unpredictability in forecasting adolescent and young adult development: A two-sample study. Dev Psychopathol 30(4):1321–1332 [DOI] [PubMed] [Google Scholar]
- 19.Hammen C, Brennan PA (2003) Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatr 60(3):253–258 [DOI] [PubMed] [Google Scholar]
- 20.Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. NICHD Early Child Care Research Network (1999) Dev Psychol 35(5):1297–1310 [DOI] [PubMed] [Google Scholar]
- 21.Nandi A, Beard JR, Galea S (2009) Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review. BMC Psychiatry 9(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ashman S, Dawson G, Panagiotides H (2008) Trajectories of maternal depression over 7 years: Relations with child psychophysiology and behavior and role of contextual risks. Dev Psychopathol 20(1):55–77 [DOI] [PubMed] [Google Scholar]
- 23.Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC (2009) A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. J Abnorm Psychol 118(3):479–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cents RAM, Diamantopoulou S, Hudziak JJ, Jaddoe VWV, Hofman A, Verhulst FC et al. (2013) Trajectories of maternal depressive symptoms predict child problem behaviour: The Generation R Study. Psychol Med 43:13–25 [DOI] [PubMed] [Google Scholar]
- 25.Chae H, East P, Delva J, Lozoff B, Gahagan S (2020) Maternal depression trajectories relate to youths’ psychosocial and cognitive functioning at adolescence and young adulthood. J Child Fam Stud 29(12):3459–3469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kingston D, Kehler H, Austin MP, Mughai MK, Wajid A, Vemeyden L et al. (2018) Trajectories of maternal depressive symptoms during pregnancy and the first 12 months postpartum and child externalizing and internalizing behavior at three years. PLOS ONE 13(4):e0195365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matijasevich A, Murray J, Cooper PJ, Anselmi L, Barros AJD, Barros FC et al. (2015) Trajectories of maternal depression and offspring psychopathology at 6 years: 2004 Pelotas cohort study. J Affect Disord 174:424–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearson RM, Evans J, Kounali D (2013) Maternal depression during pregnancy and the postnatal period: Risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry 70(12):1312–1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wickham ME, Senthilselvan A, Wild CT, Hoglund WLG, Colman I (2015) Maternal depressive symptoms during childhood and risky adolescent health behaviors. Pediatrics 135(1):59–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santor DA, Coyne JC (1997) Shortening the CES-D to improve its ability to detect cases of depression. Psychol Assess 9(3):233–243 [Google Scholar]
- 31.Glynn LM, Sandman CA (2014) Evaluation of the association between placental corticotrophin-releasing hormone and postpartum depressive symptoms. Psychosom Med 76:355–362 [DOI] [PubMed] [Google Scholar]
- 32.Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396 [PubMed] [Google Scholar]
- 33.Achenbach T, Rescorla L (2001) Manual for the ASEBA School-Age Forms & Profiles: Child Behavior Checklist for Ages 6-18, Teacher’s Report Form, Youth Self-Report. [Google Scholar]
- 34.Petty CR, Rosenbaum JF, Hirshfeld-Becker DR, Henin A, Hubley S, LaCasse S et al. (2008) The child behavior checklist broad-band scales predict subsequent psychopathology: A 5-year follow-up. J Anxiety Disord 22(3):532–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ebesutani C, Bernstein A, Martinez JI, Chorpita BF, Weisz JR (2011) The youth self report: Applicability and validity across younger and older youths. J Clin Child Adolesc Psychol 40(2):338–346 [DOI] [PubMed] [Google Scholar]
- 36.Sandman CA, Glynn LM, Davis EP (2013) Is there a viability-vulnerability tradeoff? Sex differences in fetal programming. J Psychosom Res 75:327–335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peverill M, Dirks MA, Narvaja T (2021) Socioeconomic status and child psychopathology in the United States: A meta-analysis of population-based studies. Clin Psychol Rev 83:101933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eme R (1979) Sex differences in child psychopathology: A review. Psychol Bull 86(3):574–595 [PubMed] [Google Scholar]
- 39.Rutter M, Caspi A, Moffit TE (2003) Using sex differences in psychopathology to study causal mechanisms: unifying issues and research strategies. J Child Psychol Psychiatry 44(8):1092–1115 [DOI] [PubMed] [Google Scholar]
- 40.Kistner JA (2009) Sex differences in child and adolescent psychopathology: An introduction to the special section. J Clin Child Adolesc Psychol 38(4):453–459 [DOI] [PubMed] [Google Scholar]
- 41.Sandman CA, Davis EP, Glynn LM (2012) Prescient human fetuses thrive. Psychol Sci 23:93–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Betts KS, Williams GM, Najman JM, Alati R (2014) Maternal depressive, anxious, and stress symptoms during pregnancy predict internalizing problems in adolescence. Depress Anxiety 31:9–18 [DOI] [PubMed] [Google Scholar]
- 43.Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T (2007) Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Dev Psychol 43(5):1202–1215 [DOI] [PubMed] [Google Scholar]
- 44.Giallo R, Woolhouse H, Gartland D, Hiscock H, Brown S (2015) The emotional-behavioural functioning of children exposed to maternal depressive symptoms across pregnancy and early childhood: a prospective Australian pregnancy cohort study. Eur Child Adolesc Psychiatry 24:1233–1244 [DOI] [PubMed] [Google Scholar]
- 45.Irwin JL, Davis EP, Hobel CJ, Coussons-Read M, Dunkel Schetter C (2020) Maternal prenatal anxiety trajectories and infant developmental outcomes in one-year-old offspring. Infant Behav Dev 60:101468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swales DA, Snyder HR, Hankin BL, Sandman CA, Glynn LM, Davis EP (2020) Maternal depressive symptoms predict general liability in child psychopathology. J Clin Child Adolesc doi: 10.1080/15374416.2020.1723598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coussons-Read ME, Okun ML, Nettles CD (2007) Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain Behav Immun 21:343–350 [DOI] [PubMed] [Google Scholar]
- 48.Glover V, O’Donnell KJ, O’Connor TG, Fisher J (2018) Maternal stress, fetal programming, and mechanisms underlying later psychopathology—A global perspective. Dev Psychopathol 30:843–854 [DOI] [PubMed] [Google Scholar]
- 49.Peterson GF, Espel EV, Davis EP, Sandman CA, Glynn LM (2020) Characterizing prenatal maternal distress with unique prenatal cortisol trajectories. Health Psychol 39(11):1013–1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Belsky J, Pasco Fearon RM (2002) Early attachment security, subsequent maternal sensitivity, and later child development: Does continuity in development depend upon continuity of caregiving? Attach Hum Dev 4(3):361–387 [DOI] [PubMed] [Google Scholar]
- 51.Davis EP, Korja R, Karlsson L, Glynn LM, Sandman CA, Vegetabile B et al. (2019) Across continents and demographics, unpredictable maternal signals are associated with children’s cognitive function. EBioMedicine 46:256–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cummings EM, Davies PT (1994) Maternal depression and child development. J Child Psychol Psychiatry 35(1):73–122 [DOI] [PubMed] [Google Scholar]
- 53.Goodman SH, Gotlib IH (1999) Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychol Rev 106(3):458–490 [DOI] [PubMed] [Google Scholar]
- 54.Muthén LK, Muthén BO. Mplus user’s guide. 8th ed. Muthén & Muthén. (n.d.). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.