Abstract
Aim
To investigate the reasons for disparity regarding the country-specific COVID-19-related case fatality rate (CFR) within the 30 countries of the European Economic Area (EEA).
Materials and methods
Data regarding population, area, COVID-19-associated infections/deaths, vaccination, life expectancy, elderly population, infant mortality, gender disparity, urbanization, gross domestic product (GDP), income per capita, health spending per capita, physicians, nursing personnel, hospital beds, ICU beds, hypertension, diabetes, obesity, and smoking from all EEA countries were collected from official sources on January 16, 2022. Correlation coefficients were computed, and optimal scaling using ridge regression was used to reach the most parsimonious multivariate model assessing any potential independent correlation of public health parameters with COVID-19 CFR.
Results
COVID-19 CFR ranges from 0.1% (Iceland) to 4.0% (Bulgaria). All parameters but population density, GDP, total health spending (% of GDP), ICU beds, diabetes, and obesity were correlated with COVID-19 CFR. In the most parsimonious multivariate model, elderly population rate (P = 0.018), males/total ratio (P = 0.013), nurses/hospital beds (P = 0.001), physicians/hospital beds (P = 0.026), public health spending (P = 0.013), smoking rate (P = 0.013), and unvaccinated population rate (P = 0.00005) were demonstrated to present independent correlation with COVID-19 CFR. In detail, the COVID-19 CFR is estimated to increase by 1.24 times in countries with vaccination rate of <0.34, 1.11 times in countries with an elderly population rate of ≥0.20, 1.14 times in countries with male ratio values ≥0.493, 1.12 times in countries spending <2,000$ annually per capita for public health, 1.14 and 1.10 times in countries with <2.30 nurses and <0.88 physicians per hospital bed, respectively, and 1.12 in countries with smoking ratio ≥0.22, while holding all other independent variables of the model constant.
Conclusion
COVID-19 CFR varies substantially among EEA countries and is independently linked with low vaccination rates, increased elderly population rate, diminished public health spending per capita, insufficient physicians and nursing personnel per hospital bed, and prevalent smoking habits. Therefore, public health authorities are awaited to consider these parameters in prioritizing actions to manage the SARS-CoV-2 pandemic.
Keywords: smoking, health spending, vaccination, european economic area, case fatality rate, covid-19
Introduction
COVID-19 case fatality rate (CFR), described as the ratio of COVID-19 associated deaths/confirmed SARS-CoV-2 infections, is a measure assessing the lethality of COVID-19 disease; CFR varies impressively within the 30 countries of the European Economic Area (EEA) [1]. Nevertheless, the imbalance in country-specific COVID-19 CFR is a worldwide phenomenon [2].
CFR does not account for the time from disease onset to death or total population; despite that, CFR is still difficult to be measured with accuracy. The main reason is that the confirmed SARS-CoV-2 infections are always less than actual cases, while COVID-19-associated deaths are far closer to the accurate number. Therefore, the current CFR is possibly overestimated. In fact, the more tests performed, the more SARS-CoV-2 infections are confirmed, minimizing the hazard of CFR overestimation [3]. In addition, CFR is often confused with the overall mortality rate (OMR), measured as the ratio of COVID-19-associated deaths/population/year. In fact, OMR is rather a measure of the individual risk of dying from the disease rather than reflecting the lethality of the disease [3]. Major risk factors for COVID-19 mortality were recognized. Age has been documented as a significant determinant of surviving from COVID-19; therefore, it would be reasonable to assume that the older a population gets, the more vulnerable it becomes [4]. In addition, the male sex has been reported to be at an increased risk of dying from COVID-19 [5]. Furthermore, comorbidities such as hypertension, diabetes, obesity, and smoking have been described as key contributors to an undesirable outcome [6]. Other parameters, such as medical [7], genetic [8], environmental [9], physical [10,11], mental/psychological [12], social [13], economical [14], and political [15], whose effect cannot be precisely determined, at least at an individual level, are believed to contribute to country-specific CFR disparities. Last, concerning vaccination for SARS-CoV-2, it has been reported that vaccination uptake is closely associated with elderly people saved, independently of the vaccine type administered [16]. Emerging data further support the efficacy and effectiveness of COVID-19 vaccines in terms of public health consequences [17].
Public health authorities rely on rigid data and optimal models to prioritize strategies for measures against COVID-19 spread, such as vaccination [18]. To contribute to these efforts, the present work aims to investigate the factors that potentially influence differences in country-specific CFR within EEA. This is done using data obtained from official sources to conclude the most parsimonious multivariate model assessing any potential independent correlation of SARS-CoV-2 vaccination coverage and public health parameters with COVID-19 CFR.
Materials and methods
Data regarding public health indicators from all 30 countries of the EEA were collected from official sources such as European Centre for Disease Prevention and Control (ECDC), Eurostat, WHO, Organization for Economic Co-operation and Development (OECD), World Bank Group, and Institut national d'études démographiques (INED). The timeframe of the study was from January 24, 2020, when the first documented case of SARS-CoV-2 infection was detected in Europe, to January 16, 2022, when all sources were accessed simultaneously [19]. A public health indicator was considered eligible if 1) it refers to either population demographics, or general health status, or general financial indices, or determinants of health and risk factors specially focused on COVID-19, or public health interventions, or public health services, or public health capacity; 2) it is population-based at the national level so as to allow comparisons between countries; 3) it can be retrieved from routinely available data; and 4) it derives from sources that ensure validity and reliability [20,21]. In detail, the following parameters were considered: Population [22], area [23], confirmed SARS-CoV-2 infections [1], COVID-19-associated deaths [1], infected population ratio (IFR, computed as the ratio of confirmed SARS-CoV-2 infections/population), CFR of COVID-19 (computed as the ratio of COVID-19-associated deaths/confirmed SARS-CoV-2 infections), total population vaccination rate for SARS-CoV-2 [24], life expectancy (years) [25], elderly population (>65 years; rate) [26,27], infant mortality (per 1,000 live births) [28-30], gender disparity (males rate) [31,32], population density (residents per km2) [33], urbanization (urban population rate) [34], gross domestic product (GDP; millions $) [35,36], income per capita ($) [37,38], health spending (% of GDP) [39,40], public health spending per capita ($) [41-43], private health spending per capita ($) [41-43], total health spending per capita ($) [41-43], physicians (per 1,000 residents) [44], nursing personnel (per 1,000 residents) [45-47], hospital beds (per 1,000 residents) [48-50], ICU beds (per 100,000 residents) [51], hypertension (rate) [52-53], diabetes (rate) [54-55], obesity (BMI >30 kg/m2; rate) [56,57], and smoking (rate) [58,59].
Statistics
Correlations between public health parameters (continuous variables) were approached by Spearman’s correlation coefficient ρ (rho) in case of either outlier detection or normality violation in either Kolmogorov-Smirnov or Shapiro-Wilk tests; else, Pearson’s correlation coefficient was alternatively preferred. Benjamini-Hochberg correction was applied when multiple hypotheses were tested simultaneously. Optimal scaling using ridge regression and 10x cross-validation was performed to assess any potential independent correlation of public health parameters (incorporated as independent ones after discretization into a maximum of seven categories) with CFR of COVID-19 (handled as continuous, dependent variable). All independent variables that presented either as P > 0.20 or tolerance ≤0.20 were not considered during the process towards the detection of the most parsimonious model. The level of statistical significance was set to P = 0.05. SPSS® Statistics 26.0.0.0 (IBM, Armonk, NY, USA) was used for statistical analysis. GraphPad Prism 9.3.1 was used to produce scattergrams and heat maps for visualization purposes. Concerning scattergrams, the ±95% confidence bands of the best-fit-line are depicted only in the case of statistically significant correlations.
Results
Descriptive statistics
As derived from sources referred to in the “Materials and Methods” section, all raw data are included in Table 1.
Table 1. Detailed data from EEA countries used in the study.
EEA: European Economic Area; GDP: Gross domestic product; OMR: Overall mortality rate; CFR: Case fatality rate.
| Country | SARS-CoV-2 Infections | COVID-19 Deaths | COVID-19 CFR | COVID-19 OMR | Unvaccinated Population Rate for SARS-CoV-2 | Life Expectancy | Elderly Population Rate | Infant Mortality Per 1,000 | Males Ratio | Population Density (Per km2) | Urbanization Rate | GDP (Million $) | Income Per Capita ($) | Health Spending as % of GDP | Public Health Spending Per Capita ($) | Private Health Spending Per Capita ($) | Physicians/Hospital Beds | Nurses/Hospital Beds | ICU Beds | Hypertension Rate | Diabetes Rate | Obesity Rate | Smoking Rate |
| Austria | 1392678 | 13450 | 0.0097 | 0.000761 | 0.26 | 81.3 | 0.190 | 3.4 | 0.493 | 107.6 | 0.59 | 430.95 | 35390 | 10.43 | 3892.83 | 1433.60 | 0.74 | 0.99 | 5.31 | 0.22 | 0.066 | 0.17 | 0.25 |
| Belgium | 2379053 | 28589 | 0.0120 | 0.001250 | 0.24 | 80.9 | 0.191 | 3.7 | 0.496 | 377.3 | 0.98 | 515.33 | 33880 | 10.66 | 3723.07 | 1189.63 | 0.57 | 2.13 | 4.97 | 0.17 | 0.048 | 0.16 | 0.21 |
| Bulgaria | 806977 | 31922 | 0.0396 | 0.002333 | 0.72 | 73.6 | 0.216 | 5.6 | 0.486 | 63.4 | 0.76 | 69.11 | 6830 | 7.13 | 397.64 | 292.27 | 0.57 | 0.64 | 5.95 | 0.27 | 0.067 | 0.13 | 0.38 |
| Croatia | 794190 | 13006 | 0.0164 | 0.001629 | 0.46 | 77.8 | 0.210 | 4.0 | 0.482 | 72.8 | 0.58 | 55.97 | 11720 | 6.98 | 843.93 | 170.25 | 0.64 | 1.12 | 3.99 | 0.37 | 0.052 | 0.23 | 0.36 |
| Cyprus | 218374 | 672 | 0.0031 | 0.000379 | 0.31 | 82.3 | 0.163 | 2.6 | 0.500 | 95.7 | 0.67 | 23.80 | 23770 | 7.01 | 836.52 | 1110.54 | 1.24 | 1.18 | 3.41 | 0.19 | 0.093 | 0.15 | 0.28 |
| Czechia | 2573945 | 36799 | 0.0143 | 0.001738 | 0.37 | 78.3 | 0.199 | 2.6 | 0.492 | 138.2 | 0.74 | 245.35 | 17340 | 7.83 | 1460.21 | 305.58 | 0.61 | 1.27 | 4.04 | 0.26 | 0.053 | 0.19 | 0.30 |
| Denmark | 1056389 | 3453 | 0.0033 | 0.000299 | 0.20 | 81.6 | 0.199 | 3.0 | 0.497 | 138.5 | 0.88 | 356.08 | 48150 | 9.96 | 5214.66 | 1002.11 | 1.62 | 4.12 | 2.47 | 0.19 | 0.056 | 0.16 | 0.16 |
| Estonia | 262482 | 1967 | 0.0075 | 0.000748 | 0.38 | 78.6 | 0.200 | 1.6 | 0.474 | 30.5 | 0.69 | 30.65 | 15010 | 6.73 | 1142.58 | 409.99 | 0.76 | 1.46 | 3.32 | 0.23 | 0.070 | 0.21 | 0.18 |
| Finland | 361553 | 1700 | 0.0047 | 0.000155 | 0.25 | 82.2 | 0.223 | 2.1 | 0.493 | 18.2 | 0.86 | 269.75 | 36050 | 9.15 | 3547.37 | 968.12 | 1.39 | 4.45 | 2.61 | 0.27 | 0.058 | 0.20 | 0.15 |
| France | 13240304 | 126530 | 0.0096 | 0.000948 | 0.25 | 82.3 | 0.204 | 3.8 | 0.484 | 106.1 | 0.81 | 2630.32 | 30610 | 11.06 | 3441.17 | 1248.91 | 0.54 | 1.97 | 3.00 | 0.17 | 0.054 | 0.14 | 0.28 |
| Germany | 7835451 | 115337 | 0.0147 | 0.000701 | 0.28 | 81.1 | 0.218 | 3.2 | 0.494 | 235.2 | 0.77 | 3846.41 | 35220 | 11.70 | 4251.03 | 1221.16 | 0.56 | 1.71 | 5.95 | 0.26 | 0.053 | 0.19 | 0.24 |
| Greece | 1612869 | 21732 | 0.0135 | 0.001028 | 0.31 | 81.2 | 0.223 | 3.7 | 0.491 | 82.4 | 0.80 | 189.41 | 16170 | 7.84 | 813.74 | 751.00 | 1.49 | 0.89 | 3.64 | 0.20 | 0.051 | 0.16 | 0.42 |
| Hungary | 1327014 | 40237 | 0.0303 | 0.002090 | 0.37 | 75.7 | 0.199 | 3.6 | 0.476 | 107.1 | 0.72 | 155.01 | 12680 | 6.35 | 747.53 | 334.27 | 0.52 | 0.79 | 4.21 | 0.32 | 0.06 | 0.24 | 0.28 |
| Iceland | 43768 | 43 | 0.0010 | 0.000059 | 0.23 | 83.1 | 0.144 | 1.1 | 0.502 | 3.6 | 0.94 | 21.71 | 36030 | 8.57 | 5379.65 | 1151.29 | 1.34 | 6.04 | 2.33 | 0.25 | 0.032 | 0.22 | 0.14 |
| Ireland | 1061116 | 6035 | 0.0057 | 0.000609 | 0.23 | 82.8 | 0.144 | 2.8 | 0.496 | 71.9 | 0.64 | 425.89 | 62980 | 6.68 | 4055.94 | 1433.13 | 1.19 | 4.51 | 2.69 | 0.12 | 0.052 | 0.26 | 0.18 |
| Italy | 8155645 | 140188 | 0.0172 | 0.001196 | 0.25 | 82.4 | 0.232 | 2.4 | 0.487 | 201.5 | 0.71 | 1886.45 | 24900 | 8.67 | 2208.52 | 780.48 | 1.27 | 1.87 | 2.60 | 0.20 | 0.051 | 0.11 | 0.23 |
| Latvia | 295961 | 4700 | 0.0159 | 0.001255 | 0.32 | 75.7 | 0.205 | 3.4 | 0.461 | 30.2 | 0.68 | 33.51 | 12150 | 6.58 | 657.77 | 441.91 | 0.61 | 0.85 | 3.09 | 0.32 | 0.078 | 0.22 | 0.32 |
| Liechtenstein | 6915 | 72 | 0.0104 | 0.000932 | 0.33 | 81.9 | 0.185 | 0.0 | 0.495 | 244.1 | 0.14 | 6.68 | 175814 | 5.57 | 3081.70 | 6788.97 | 2.47 | 1.06 | 1.45 | 0.30 | 0.047 | 0.11 | 0.25 |
| Lithuania | 559980 | 7618 | 0.0136 | 0.001378 | 0.31 | 75.1 | 0.199 | 3.3 | 0.463 | 44.6 | 0.68 | 55.89 | 14030 | 7.01 | 822.83 | 422.52 | 0.72 | 1.48 | 5.20 | 0.30 | 0.078 | 0.18 | 0.28 |
| Luxembourg | 121237 | 931 | 0.0077 | 0.000742 | 0.32 | 81.8 | 0.145 | 4.7 | 0.506 | 239.8 | 0.91 | 73.26 | 82250 | 5.37 | 5288.11 | 851.03 | 0.72 | 2.9 | 3.25 | 0.16 | 0.045 | 0.16 | 0.23 |
| Malta | 62387 | 500 | 0.0080 | 0.000490 | 0.15 | 82.6 | 0.185 | 6.7 | 0.501 | 1595.1 | 0.95 | 14.65 | 20410 | 8.95 | 1747.87 | 1005.19 | 0.88 | 2.12 | 3.34 | 0.18 | 0.066 | 0.28 | 0.20 |
| Netherlands | 3465463 | 21127 | 0.0061 | 0.000611 | 0.28 | 81.5 | 0.195 | 3.6 | 0.498 | 507.3 | 0.92 | 913.87 | 40160 | 10.17 | 3444.81 | 1860.37 | 1.20 | 3.73 | 2.62 | 0.16 | 0.053 | 0.14 | 0.12 |
| Norway | 472454 | 1381 | 0.0029 | 0.000129 | 0.28 | 83.3 | 0.175 | 2.1 | 0.505 | 17.3 | 0.83 | 362.52 | 68590 | 10.52 | 7029.85 | 1209.24 | 1.46 | 5.27 | 3.10 | 0.15 | 0.047 | 0.14 | 0.08 |
| Poland | 4265433 | 101419 | 0.0238 | 0.001355 | 0.43 | 76.6 | 0.182 | 3.8 | 0.485 | 123.6 | 0.6 | 594.16 | 12700 | 6.45 | 695.75 | 282.42 | 0.39 | 1.12 | 4.35 | 0.27 | 0.090 | 0.19 | 0.26 |
| Portugal | 1774477 | 19203 | 0.0108 | 0.000943 | 0.10 | 81.1 | 0.221 | 2.8 | 0.473 | 113.0 | 0.66 | 231.23 | 17070 | 9.53 | 1361.26 | 851.83 | 1.51 | 1.97 | 3.33 | 0.27 | 0.096 | 0.17 | 0.21 |
| Romania | 1875887 | 59150 | 0.0315 | 0.001559 | 0.59 | 74.2 | 0.189 | 5.8 | 0.486 | 82.7 | 0.54 | 248.72 | 8830 | 5.74 | 547.68 | 139.58 | 0.47 | 0.89 | 4.03 | 0.16 | 0.077 | 0.11 | 0.30 |
| Slovakia | 820682 | 9939 | 0.0121 | 0.000920 | 0.52 | 76.9 | 0.166 | 5.1 | 0.487 | 112.0 | 0.54 | 104.57 | 15180 | 6.96 | 1030.04 | 269.87 | 0.61 | 1.04 | 4.85 | 0.28 | 0.057 | 0.19 | 0.25 |
| Slovenia | 519714 | 6171 | 0.0119 | 0.001479 | 0.42 | 80.6 | 0.202 | 2.1 | 0.498 | 103.7 | 0.55 | 53.59 | 19720 | 8.52 | 1570.97 | 598.61 | 0.73 | 2.30 | 4.13 | 0.25 | 0.075 | 0.19 | 0.27 |
| Spain | 7930528 | 90620 | 0.0114 | 0.000967 | 0.18 | 82.4 | 0.196 | 2.6 | 0.491 | 93.8 | 0.81 | 1281.20 | 22350 | 9.13 | 1926.46 | 809.86 | 1.48 | 2.07 | 2.48 | 0.19 | 0.063 | 0.15 | 0.24 |
| Sweden | 1534797 | 15482 | 0.0101 | 0.000754 | 0.26 | 83.2 | 0.200 | 2.1 | 0.501 | 25.2 | 0.88 | 541.06 | 42570 | 10.87 | 5089.96 | 891.74 | 2.04 | 6.09 | 1.90 | 0.18 | 0.042 | 0.15 | 0.07 |
Based on the data of the present study, CFR varies impressively within the 30 countries of the EEA, ranging from a minimum of 0.1% in Iceland to a maximum of 4.0% in Bulgaria.
Of interest, COVID-19 OMR follows a similar pattern, ranging from 59 (Iceland) to 2,333 deaths per million residents per year (Bulgaria), given that 1.978 years elapsed from January 24, 2020, when the first documented case of SARS-CoV-2 infection was detected in Europe; OMR is strongly correlated with CFR (Spearman’s rho = 0.891, P = 4x10-11).
Correlations between analyzed parameters and COVID-19 CFR
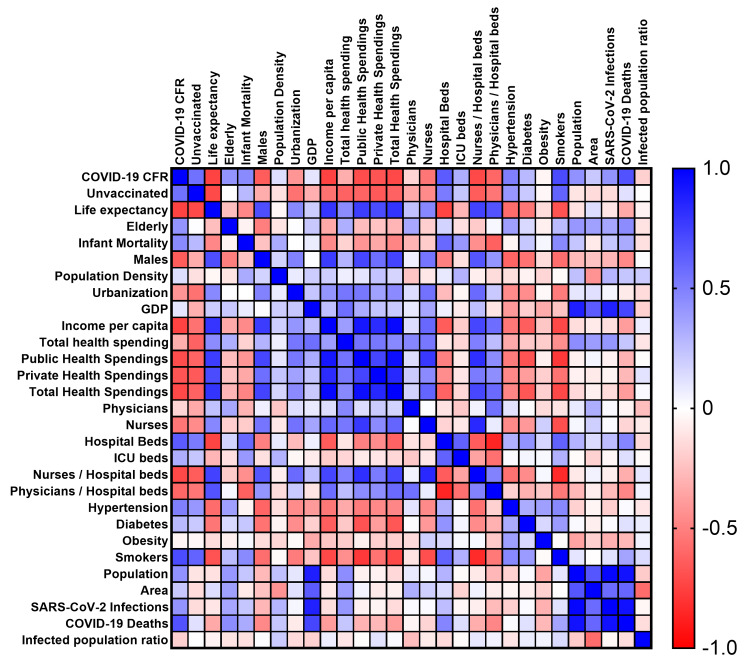
A detailed heat map depicting correlation coefficients between all parameters analyzed in the present study is provided in Figure 1. As COVID-19 CFR distribution deviates from normality (Kolmogorov-Smirnov P = 0.023; Shapiro-Wilk P = 0.001), the non-parametric Spearman's correlation coefficient ρ (rho) was used.
Figure 1. Heat map based on Spearman’s correlation coefficients including all parameters analyzed.
All parameters but infected population rate, population density, GDP, total health spending as % of GDP, ICU beds, diabetes, and obesity demonstrated a statistically significant correlation with COVID-19 CFR. Detailed data are presented in Table 2.
Table 2. Univariate analysis using Spearman's correlation coefficients between COVID-19 CFR and evaluated public health parameters; P-values have been corrected using the Benjamini-Hochberg correction.
CFR: Case fatality rate.
| Parameter | Spearman’s rho | P-value |
| Infected population (ratio) | -0.187 | 0.322 |
| Unvaccinated population (ratio) | 0.556 | 0.003 |
| Life expectancy (years) | -0.740 | 3x10-5 |
| Elderly population (ratio) | 0.418 | 0.036 |
| Gender disparity (males/total ratio) | -0.642 | 4x10-4 |
| Infant mortality (per 1,000 live births) | 0.459 | 0.011 |
| Population density (residents per km2) | 0.127 | 0.558 |
| Urbanization (ratio) | -0.416 | 0.036 |
| GDP (millions $) | 0.101 | 0.626 |
| Income per capita ($) | -0.738 | 3x10-5 |
| Total health spending (% of GDP) | -0.320 | 0.117 |
| Public health spending per capita ($) | -0.698 | 2x10-5 |
| Private health spending per capita ($) | -0.673 | 2x10-4 |
| Total health spending per capita ($) | -0.719 | 5x10-5 |
| Hospital beds (per 1,000 residents) | 0.517 | 4x10-4 |
| ICU beds (per 100,000 residents) | 0.316 | 0.117 |
| Physicians (per 1,000 residents) | -0.170 | 0.432 |
| Nurses (per 1,000 residents) | -0.539 | 0.004 |
| Physicians/Hospital beds (ratio) | -0.601 | 4x10-4 |
| Nurses/Hospital beds (ratio) | -0.715 | 9x10-6 |
| Physicians/ICU beds (ratio) | -0.363 | 0.048 |
| Nurses/ICU beds (ratio) | -0.484 | 0.007 |
| Hypertension (ratio) | 0.485 | 0.013 |
| Diabetes (ratio) | 0.274 | 0.179 |
| Obesity (ratio) | -0.030 | 0.876 |
| Smoking (ratio) | 0.705 | 7x10-5 |
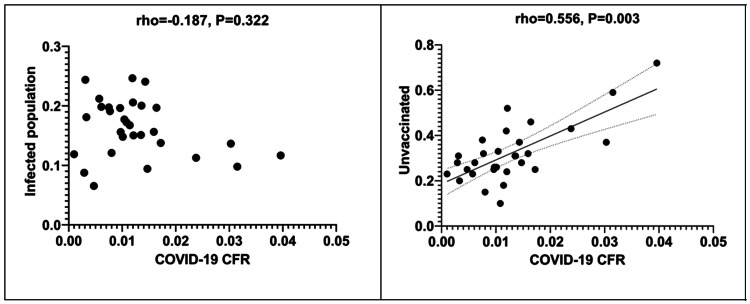
Scattergrams depicting correlations between the infected population rate and the unvaccinated population rate and COVID-19 CFR are shown in Figure 2.
Figure 2. Scattergrams depicting correlations between infected population rate as well as unvaccinated population rate and COVID-19 CFR.
CFR: Case fatality rate.
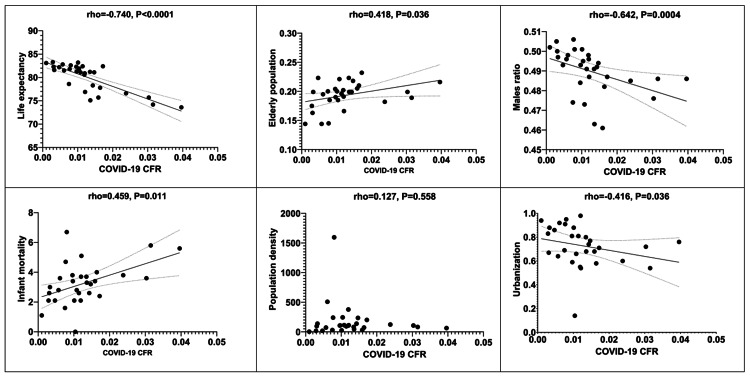
Similarly, scattergrams depicting correlations between demographics (life expectancy, elderly population rate, males ratio, infant mortality, population density, and urban population ratio) and COVID-19 CFR are shown in Figure 3.
Figure 3. Scattergrams depicting correlations between demographics and COVID-19 CFR.
CFR: Case fatality rate.
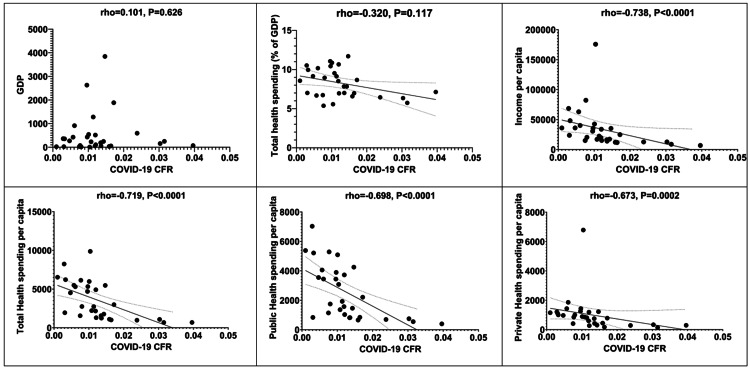
Moreover, scattergrams depicting correlations between financial indices (GDP, total health spending as % of GDP, income per capita, total health spending per capita, public health spending per capita, public health spending per capita, and private health spending per capita) and COVID-19 CFR are depicted in Figure 4.
Figure 4. Scattergrams depicting correlations between financial indices and COVID-19 CFR.
CFR: Case fatality rate.
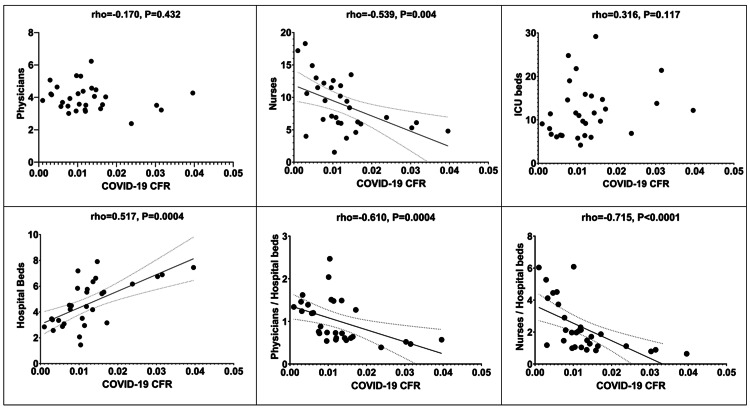
Concerning the potential relationship between personnel as well as infrastructure indices (physicians per 1,000 residents, nurses per 1,000 residents, ICU beds per 100,000 residents, hospital beds per 1,000 residents, physicians/hospital beds ratio, and nurses/hospital beds ratio) and COVID-19 CFR, the relevant scattergrams are depicted in Figure 5.
Figure 5. Scattergrams depicting correlations between personnel and infrastructure indices and COVID-19 CFR.
CFR: Case fatality rate.
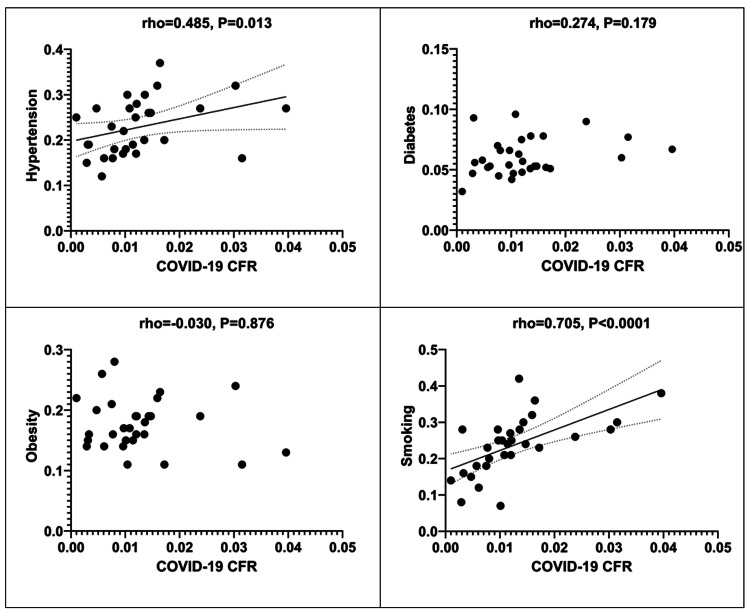
Lastly, the relevant scattergrams regarding the correlations between the examined comorbidity indices (hypertension, diabetes, obesity, and smoking) and COVID-19 CFR are provided in Figure 6.
Figure 6. Scattergrams depicting correlations between comorbidity indices and COVID-19 CFR.
CFR: Case fatality rate.
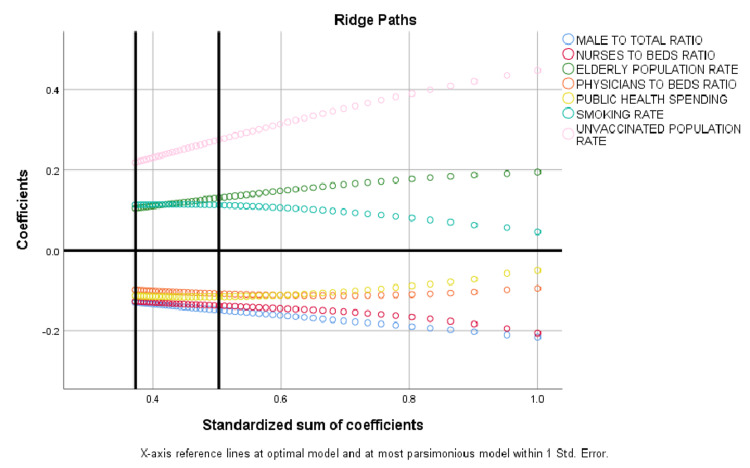
An attempt to construct the most parsimonious multivariate model revealed that seven variables including elderly rate, male ratio, nurses/hospital beds ratio, physicians/hospital beds ratio, public health spending, smoking, and unvaccinated population rate were demonstrated to present an independent correlation with COVID-19 CFR (Table 3).
Table 3. Multivariate analysis using optimal scaling and ridge regression; regularization R^2 = 0.667, overall ANOVA P = 0.006.
| Cut-off after discretization | Standardized coefficient | SE† | F | Tolerance | P-value | |
| Elderly population ratio (>65 years old) | <0.20 vs ≥0.20 | 0.105 | 0.050 | 4.332 | 0.848 | 0.018 |
| Male ratio | <0.493 vs ≥0.493 | -0.129 | 0.047 | 7.433 | 0.450 | 0.013 |
| Nurses/Hospital beds | <2.30 vs ≥2.30 | -0.127 | 0.033 | 15.137 | 0.206 | 0.001 |
| Physicians/Hospital beds | <0.88 vs ≥0.88 | -0.098 | 0.041 | 5.809 | 0.566 | 0.026 |
| Public health spending | <2000 vs ≥2000 | -0.113 | 0.041 | 7.525 | 0.270 | 0.013 |
| Smokers ratio | <0.22 vs ≥0.22 | 0.113 | 0.042 | 7.423 | 0.252 | 0.013 |
| Unvaccinated population ratio | <0.34 vs ≥0.34 | 0.219 | 0.052 | 17.470 | 0.702 | 5x10-5 |
The model was based on optimal scaling, discretization of independent variables into a maximum of seven categories, ridge regression regularization, and 10x cross-validation incorporating COVID-19 CFR as dependent variable (continuous) and all other parameters of interest as independent ones, explaining 66.7% of the variability (regularization R2 = 0.667) (Figure 7).
Figure 7. Ridge paths of the most parsimonious model; seven variables were demonstrated to present independent correlation with COVID-19 CFR.
CFR: Case fatality rate.
Low population vaccination rate is independently correlated with increased COVID-19 CFR
Unvaccinated population rate is correlated with increased COVID-19 CFR (Table 2). The most parsimonious model documented that vaccination rate revealed the strongest independent correlation with COVID-19 CFR when compared to the other six parameters included in the model. In detail, the present study has concluded that country-specific COVID-19-related CFR is estimated to increase by e0.219=1.24 times in case of vaccination rate <0.34 while holding all other independent variables of the model constant (Table 3). Controversially, the IFR has not been correlated with the CFR of the disease; this was not unexpected, as the IFR represents only a measure of the adequacy of testing and the virus spread [60].
Demographics and COVID-19 CFR: Elderly are vulnerable, whereas men might be the weaker sex
The elderly population (>65 years old) rate is linked with high CFR from COVID-19 (Table 2). This finding is consolidated as an elderly population rate ≥0.20 has been demonstrated to independently correlate with increased CFR from COVID-19 in multivariate analysis. Of note, the country-specific COVID-19 CFR is estimated to increase by e0.105=1.11 times in the case of elderly population rate ≥0.20 while holding all other independent variables of the model constant (Table 3).
The larger the men/total ratio, the higher CFR from COVID-19 was observed (Table 2). The male/total ratio has been shown to be independently correlated with increased country-specific CFR of COVID-19; an increase by e0.129=1.14 times is awaited in case of values ≥0.493 while holding all other independent variables of the model constant (Table 3).
Other demographics of interest such as life expectancy, infant mortality, and urbanization, though revealed a statistically significant correlation with COVID-19 CFR in univariate analysis (Table 2), failed to document its independent and potentially etiological nature (Table 3).
The more we invest in public health, the more lives we save: Fewer public health spending per capita is correlated with inflated COVID-19 CFR
The increased income per capita and total health spending per capita (either public or private) are correlated with lower COVID-19 CFR (Table 2). In multivariate analysis, the public health spending per capita, and not the private one, has been recognized as the most significant financial public health parameter to interfere with the disease. In that case, the COVID-19 CFR is estimated to increase by e0.113=1.12 times in the case of countries spending <2,000$ annually per capita for public health while holding all other independent variables of the model constant (Table 3). Interestingly, GDP is not linked with COVID-19 CFR, neither itself nor as % attributed to total health spending.
Country health profiles and COVID-19 CFR: a lesson to prioritize personnel rather than infrastructure
Both physicians and nurses, when considered as ratios to hospital beds or ICU beds, revealed a strong, negative relationship with COVID-19 CFR, despite that in absolute numbers, the relevant correlations are weaker (in case of nurses), or absent (in the case of physicians). Of note, ICU beds were not correlated with the outcome of interest, and hospital beds presented a positive correlation with CFR of COVID-19 (Table 2). When the multivariate analysis was performed, the number of nurses and physicians per hospital bed remained independently correlated with the CFR of COVID-19. According to the present model, COVID-19 CFR is estimated to increase by e0.127=1.14 and e0.098=1.10 times in the case of countries with <2.30 nurses and <0.88 physicians per hospital bed, respectively, while holding all other independent variables of the model constant (Table 3).
Smoking reserves a key role among comorbidities affecting COVID-19 CFR
Hypertension and smoking are the two most prominent public health issues regarding COVID-19 CFR (Table 2). Smoking retained an independent correlation with increased CFR of the disease in the multivariate analysis model. In countries with a smoking ratio ≥0.22, the COVID-19 CFR is awaited to increase by e0.113=1.12 while holding all other independent variables of the model constant (Table 3). Diabetes and obesity, though documented to be comorbidities affecting outcome after SARS-CoV-2 infection, failed to present a statistically significant correlation with COVID-19 CFR in univariate analysis (Table 2).
Discussion
To the best of our knowledge, this is the first study to describe the impact of SARS-CoV-2 vaccination coverage and several key public health indicators in country-specific COVID-19 CFR within the EEA. As a result, COVID-19 CFR varies substantially among EEA countries, and is independently linked with low vaccination rate (<0.34), elderly population rate (≥0.20), limited public health spending (<2,000 $ per capita), insufficient physicians per hospital beds ratio (<0.88), inadequate nursing personnel per hospital beds ratio (<2.30), and high prevalence of smoking habits (≥0.20). Vaccination coverage, public health financing, hospital staffing with both physicians and nursing personnel, and anti-smoking campaign planning are thus believed to be critical to prevent increased COVID-19 CFR.
It has been recognized that vaccination status is linked with lower death rates. In detail, even a single dose of mRNA BNT162b2 vaccine has been reported to reduce the risk of death significantly (OR: 0.51, 95% CI: 0.37-0.62). Moreover, the vaccine prevented 96.7% of COVID-19-related deaths in vaccinated individuals [61,62]. Both ChAdOx1-S and BNT162b2 vaccines retain 84.8% (95% CI: 76.2 to 90.3) and 91.9% (95% CI: 88.5 to 94.3) effectiveness in reducing the risk of death, respectively [63]. Abdul Taib NA et al. reported that the mortality rate among vaccinated people was consistently lower than those who were unvaccinated. Moreover, the mortality rate of those who received inactivated vaccines was higher than the recipients of the BNT162b2 and ChAdOx1 vaccines [64]. Countries such as Switzerland, USA, Chile, and England, being all outside EEA, offer paradigms of significantly higher death rates among the unvaccinated population, when compared with those who had been fully vaccinated against SARS-CoV-2, especially after booster dose [65]. Correspondingly, the present study has concluded that COVID-19-related CFR is estimated to increase by 24% in countries with vaccination rates <0.34.
According to a recently published study, almost half (~47%) of the variation observed in country-specific COVID-19 CFR is attributed to the country's age profile. In comparison, another 44% could not be explained [66]. An analysis of age-specific data from 20 countries from Europe and Northern America concluded that >80% of the variance of country-specific COVID-19 CFR could be attributed to the proportion of the elderly population (>75 years of age). However, the authors did not investigate the role of other parameters contributing to mortality from COVID-19 [67]. Abdul Taib NA et al. and Soneji S et al. concluded similar results [64,68]. Interestingly, García CN claimed that not the elderly population rate, but rather the institutionalization of elderly people in long-term care resources (as care homes) might explain the statistically significant contribution of aging to COVID-19 mortality [69]. Concerning gender disparity, male sex is linked with increased COVID-19 CFR worldwide [70]. This observation has been supported to be independent of age or comorbidities [71]. The issue of standardization not only to age but also to sex is further underlined, focusing primarily on the effect of the decreasing life expectancy in age and sex impact on taming COVID-19 mortality [72]. The present study has demonstrated that the country-specific COVID-19 CFR is estimated to increase by 11% and 14% in countries with elderly population rates ≥0.20 and male/total ratio ≥0.493, respectively.
The role of public health financing and access to health care in COVID-19 CFR has not been broadly investigated. Mackey K et al. report that African American/Black and Hispanic populations had experienced disproportionately higher rates of SARS-CoV-2 infection and COVID-19-related mortality but similar CFR [73]. Interestingly, strong positive associations of Black, American Indian, and Alaska Native versus White race and urban versus rural residence with SARS-CoV-2 CFR were observed, implying the existence of racial and geographic barriers concerning the accessibility of health care facilities [74]. However, whether differences in health care access and exposure risk may be driving higher infection and mortality rates yet remains unclear. Of interest, the present study underlined the major and independent positive impact of public health spending in attenuating COVID-19 CFR, estimating an increase by 12% in the case of countries spending <2,000$ annually per capita for public health.
A significant non-linear relationship between COVID-19 CFR and the number of physicians (P ≤0.001), and nurses and midwives (P ≤0.001) had been documented [75]. This finding is also in keeping with the present study results, which underlined that COVID-19 CFR is estimated to increase by 14% and 10% in the case of countries with <2.30 nurses and <0.88 physicians per hospital bed, respectively. The latter implies that adequacy is urged not only to upgrade the infrastructure level (hospital beds and ICU beds) but also to staff it with the required qualified nursing and medical personnel. Taken together with the already demonstrated beneficial impact that the increased public health spending has on taming COVID-19 CFR, it is reasonable to support that the available public health investments have to be prioritized towards recruiting additional nurses and physicians.
COVID-19 mortality rates were also associated with comorbidities, as described in a recently published study. However, the risk of death by specific comorbidity type has not been conclusively assessed [65]. Hypertension and diabetes have been reported to increase COVID-19 CFR; despite that the elderly had a higher CFR, the relevant risk ratios were more pronounced among the younger population [76]. Moreover, obesity has been demonstrated to be an independent risk and prognostic factor for the severity of the disease [77]. These observations seem to disagree with the findings of the present study, which reveal comparable country-specific CFR after adjustment for age and sex. However, detailed data concerning undiagnosed or uncontrolled hypertensive or diabetic patients that could further elucidate this issue are not available. On the other hand, smoking had been early recognized as a risk factor for dying from COVID-19, too. Compared to former and never smokers, current smokers were at greater risk of severe complications and higher mortality rate [78]. This is in keeping with the independent correlation between the smoking ratio and country-specific COVID-19 CFR observed by our study. In contrast, the increase of COVID-19 CFR attributable to smoking has been estimated to be 12% in countries presenting smokers ratio ≥0.22. Other factors that have not been included in the present study, such as air travelers (who might reflect mobility) or isolated territories (as isles), have been demonstrated to present a positive impact on mortality from COVID-19 [63]. Of interest, the tuberculosis rate was proposed to be associated with COVID-19 CFR [79]. A more complex model introduced population density, population density/GDP, urbanization ratio/GDP, hospital beds/GDP, the gender ratio among elderly (>80 years), population density/tuberculosis incidence, average temperature, and average temperature/GDP as prognosticators of logarithmic COVID-19 mortality [80].
OMR could be argued to provide a safer estimate of the risk of dying from COVID-19 when compared to CFR, considering that COVID-19-associated deaths are rigorously registered and the relevant population at risk might be precisely approached, as merely everyone had been eventually exposed to SARS-CoV-2. However, OMR is suitable neither as a measure of the disease's severity nor its lethality but rather as an estimate of individual risk of dying from the disease. Moreover, OMR depends on total population and time; the latter parameter is crucial considering that the period elapsed from SARS-CoV-2 infection to outcome, though generally short, may vary substantially. Under these circumstances, CFR and OMR could not be interchangeably used in practice, at least in the case of COVID-19 disease.
The major limitation of the present study is the inability to exhaustively examine all factors that potentially contribute to COVID-19 CFR. The main reason for this compromise is that too many variables usually produce multivariate models with over-fitting or collinearity issues. Especially, data regarding the specific SARS-CoV-2 variants or the time of seeking medical help from the onset of the disease are lacking, thus blurring the results as far as the potential contribution of these parameters to CFR is concerned. Additionally, it could be argued that a time-dependent analysis could offer a more realistic approach, given that COVID-19 CFR has been declining since May 2020 [81]. Moreover, the impact of psychological profile, social attitude, and compliance with governmental planning has not been taken into account, as precise measurements are unfeasible.
Conclusions
In conclusion, COVID-19 CFR, which varies substantially among EEA countries, is independently correlated with low vaccination rate, increased elderly population rate, diminished public health spending per capita, insufficient physicians and nursing personnel per hospital beds, and prevalent smoking habits. Therefore, European and national public health authorities could consider these parameters when prioritizing actions for the management of the SARS-CoV-2 pandemic.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.European Centre for Disease Prevention and Control: COVID-19 situation dashboard. [ Jan; 2022 ];https://qap.ecdc.europa.eu/public/extensions/COVID-19/COVID-19.html 2022
- 2.Moving-average case fatality rate of COVID-19. [ Jan; 2022 ];https://ourworldindata.org/grapher/deaths-covid-19-vs-case-fatality-rate 2022
- 3.Mortality Frequency Measures. [ Jan; 2022 ];https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section3.html 2022
- 4.Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Eur J Epidemiol. 2020;35:1123–1138. doi: 10.1007/s10654-020-00698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sex-based differences in severity and mortality in COVID-19. Alwani M, Yassin A, Al-Zoubi RM, et al. Rev Med Virol. 2021;31:0. doi: 10.1002/rmv.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies. Mahamat-Saleh Y, Fiolet T, Rebeaud ME, et al. BMJ Open. 2021;11:0. doi: 10.1136/bmjopen-2021-052777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Differences in mortality in critically ill elderly patients during the second COVID-19 surge in Europe. Jung C, Fjølner J, Bruno RR, et al. Crit Care. 2021;25:344. doi: 10.1186/s13054-021-03739-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Genetic variants are identified to increase risk of COVID-19 related mortality from UK Biobank data. Hu J, Li C, Wang S, Li T, Zhang H. Hum Genomics. 2021;15:10. doi: 10.1186/s40246-021-00306-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Air pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19's morbidity and mortality. Comunian S, Dongo D, Milani C, Palestini P. Int J Environ Res Public Health. 2020;17:4487. doi: 10.3390/ijerph17124487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Sallis R, Young DR, Tartof SY, et al. Br J Sports Med. 2021;55:1099–1105. doi: 10.1136/bjsports-2021-104080. [DOI] [PubMed] [Google Scholar]
- 11.Palliative care and COVID-19 pandemic: retrospective study of factors associated with infection and death at an oncological palliative care reference center. de Oliveira LC, Rosa KS, Durante AL, et al. Am J Hosp Palliat Care. 2021;38:512–520. doi: 10.1177/1049909120986962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. Wang Q, Xu R, Volkow ND. World Psychiatry. 2021;20:124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Social inequalities and COVID-19 mortality in the city of São Paulo, Brazil. Ribeiro KB, Ribeiro AF, Veras MA, de Castro MC. Int J Epidemiol. 2021;50:732–742. doi: 10.1093/ije/dyab022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Socio-economic determinants of global COVID-19 mortalities: policy lessons for current and future pandemics. Ngepah N. Health Policy Plan. 2021;36:418–434. doi: 10.1093/heapol/czaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Democracy and Covid-19 mortality in Europe. [ Jan; 2022 ];Mazzucchelli R, Agudo Dieguez A, Dieguez Costa EM, Villarias NC. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-613678. Rev Esp Salud Publica. 2020 94:0. [PMC free article] [PubMed] [Google Scholar]
- 16.COVID-19 vaccination uptake strongly predicts averted deaths of older people across Europe (IN PRESS) Mattiuzzi C, Henry BM, Lippi G. Biomed J. 2022 doi: 10.1016/j.bj.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: a systematic review. Mohammed I, Nauman A, Paul P, et al. Hum Vaccin Immunother. 2022:1–20. doi: 10.1080/21645515.2022.2027160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Optimising health and economic impacts of COVID-19 vaccine prioritisation strategies in the WHO European Region: a mathematical modelling study. Liu Y, Sandmann FG, Barnard RC, et al. http://10.1016/j.lanepe.2021.100267. Lancet Reg Health Eur. 2022;12:100267. doi: 10.1016/j.lanepe.2021.100267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lescure FX, Bouadma L, Nguyen D, et al. Lancet Infect Dis. 2020;20:697–706. doi: 10.1016/S1473-3099(20)30200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mini-symposium — Public Health Observatories: public health indicators. Flowers J, Hall P, Pencheon D. Public Health. 2005;119:239–245. doi: 10.1016/j.puhe.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 21.Population-based health indexes: a systematic review. Kaltenthaler E, Maheswaran R, Beverley C. Health Policy. 2004;68:245–255. doi: 10.1016/j.healthpol.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 22.The World Bank: Population, total. [ Jan; 2022 ];https://data.worldbank.org/indicator/SP.POP.TOTL 2020
- 23.The World Bank: Land area. [ Jan; 2022 ];https://data.worldbank.org/indicator/AG.LND.TOTL.K2 2020
- 24.European Centre for Disease Prevention and Control: COVID-19 vaccine tracker. [ Jan; 2022 ];https://vaccinetracker.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html 2022
- 25.Eurostat Statistics Explained. [ Jan; 2022 ];https://ec.europa.eu/eurostat/statistics-explained/index.php 2022
- 26.Elderly population. [ Jan; 2022 ];https://data.oecd.org/pop/elderly-population.htm 2020
- 27.The World Bank: Population ages 65 and above (% of total population) [ Jan; 2022 ];https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS 2020
- 28.Infant mortality rates. [ Jan; 2022 ];https://data.oecd.org/healthstat/infant-mortality-rates.htm 2022
- 29.WHO: Number of deaths in children aged <5 years, by cause. [ Jan; 2022 ];https://www.who.int/data/gho/data/indicators/indicator-details/GHO/number-of-deaths 2022
- 30.Births, deaths and infant mortality. [ Jan; 2022 ];https://www.ined.fr/en/everything_about_population/data/europe-developed-countries/birth-death-infant-mortality/ 2021
- 31.Maternal, newborn, child and adolescent health and ageing. [ Jan; 2022 ];https://www.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/mca/sex-ratio-at-birth-(male-births-per-female-births) 2022
- 32.The World Bank: Population, female (% of total population) [ Jan; 2022 ];https://data.worldbank.org/indicator/SP.POP.TOTL.FE.ZS 2020
- 33.The World Bank: Population density (people per sq. km of land area) [ Jan; 2022 ];https://data.worldbank.org/indicator/EN.POP.DNST 2020
- 34.The World Bank: Urban population (% of total population) [ Jan; 2022 ];https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS 2020
- 35.Gross domestic product (GDP) [ Jan; 2022 ];https://data.oecd.org/gdp/gross-domestic-product-gdp.htm 2021
- 36.The World Bank: GDP (current US$) [ Jan; 2022 ];https://data.worldbank.org/indicator/NY.GDP.MKTP.CD 2020
- 37.Real GDP per capita. [ Jan; 2022 ];https://ec.europa.eu/eurostat/databrowser/view/sdg_08_10/default/table 2021
- 38.GDP per capita (current US$) [ Jan; 2022 ];https://data.worldbank.org/indicator/NY.GDP.PCAP.CD 2020
- 39.Health spending. [ Jan; 2022 ];https://data.oecd.org/healthres/health-spending.htm 2020
- 40.Current health expenditure (% of GDP) [ Jan; 2022 ];https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS 2019
- 41.Government expenditure on health. [ Jan; 2022 ]; https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Government_expenditure_on_health. 2020 [PubMed]
- 42.Global Health Expenditure Database. [ Jan; 2022 ];https://apps.who.int/nha/database 2014
- 43.Health expenditure per capita. [ Jan; 2022 ];https://www.oecd-ilibrary.org/sites/154e8143-en/index.html?itemId=/content/component/154e8143-en 2021
- 44.The World Bank: Physicians (per 1,000 people) [ Jan; 2022 ];https://data.worldbank.org/indicator/SH.MED.PHYS.ZS 2022
- 45.Nursing and midwifery personnel density (per 1000 population) [ Jan; 2022 ];https://www.who.int/data/gho/data/indicators/indicator-details/GHO/nursing-and-midwifery-personnel-density-(per-1000-population) 2022
- 46.Nurses. [ Jan; 2022 ];https://data.oecd.org/healthres/nurses.htm 2020
- 47.Nurses and midwives (per 1,000 people) [ Jan; 2022 ];https://data.worldbank.org/indicator/SH.MED.NUMW.P3 2018
- 48.Hospital bed density. [ Jan; 2022 ];https://apps.who.int/gho/data/view.main.HS07v 2020
- 49.Hospital beds. [ Jan; 2022 ];https://data.oecd.org/healtheqt/hospital-beds.htm 2020
- 50.Hospital beds (per 1,000 people) [ Jan; 2022 ];https://data.worldbank.org/indicator/SH.MED.BEDS.ZS 2022
- 51.Intensive care beds capacity. [ Jan; 2022 ];https://www.oecd.org/coronavirus/en/data-insights/intensive-care-beds-capacity 2020
- 52.Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. NCD Risk Factor Collaboration (NCD-RisC) Lancet. 2021;398:957–980. doi: 10.1016/S0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.The global epidemiology of hypertension. Mills KT, Stefanescu A, He J. Nat Rev Nephrol. 2020;16:223–237. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Diabetes prevalence (% of population ages 20 to 79) [ Jan; 2022 ];https://data.worldbank.org/indicator/SH.STA.DIAB.ZS 2011
- 55.Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Lin X, Xu Y, Pan X, et al. Sci Rep. 2020;10:14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Proportion of overweight and of obese women, 2019 (%) [ Jan; 2022 ];https://ec.europa.eu/eurostat/statistics-explained/index.php?title=File:Proportion_of_overweight_and_of_obese_women,_2019_(%25).png 2019
- 57.Prevalence of obesity among adults, BMI ≥ 30. [ Jan; 2022 ];https://www.who.int/data/gho/indicator-metadata-registry/imr-details/2389 2022
- 58.Tobacco consumption statistics. [ Jan; 2022 ];https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Tobacco_consumption_statistics 2022
- 59.Prevalence of current tobacco use (% of adults) [ Jan; 2022 ];https://data.worldbank.org/indicator/SH.PRV.SMOK 2018
- 60.The positive rate: a crucial metric for understanding the pandemic. [ Mar; 2022 ];https://ourworldindata.org/coronavirus-testing 2020
- 61.Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on COVID-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. Lopez Bernal J, Andrews N, Gower C, et al. BMJ. 2021;373:0. doi: 10.1136/bmj.n1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Haas EJ, Angulo FJ, McLaughlin JM, et al. Lancet. 2021;397:1819–1829. doi: 10.1016/S0140-6736(21)00947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Duration of protection against mild and severe disease by COVID-19 vaccines. Andrews N, Tessier E, Stowe J, et al. N Engl J Med. 2022;386:340–350. doi: 10.1056/NEJMoa2115481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Characterisation of COVID-19 deaths by vaccination types and status in Malaysia between February and September 2021. Abdul Taib NA, Baha Raja D, Teo AK, et al. Lancet Reg Health West Pac. 2022;18:100354. doi: 10.1016/j.lanwpc.2021.100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.How do death rates from COVID-19 differ between people who are vaccinated and those who are not? [ Feb; 2022 ];https://ourworldindata.org/covid-deaths-by-vaccination 2021
- 66.Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. COVID-19 National Preparedness Collaborators. Lancet. 2022 doi: 10.1016/S0140-6736(22)00172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Older age groups and country-specific case fatality rates of COVID-19 in Europe, USA and Canada. Hoffmann C, Wolf E. Infection. 2021;49:111–116. doi: 10.1007/s15010-020-01538-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Population-level mortality burden from novel coronavirus (COVID-19) in Europe and North America. Soneji S, Beltrán-Sánchez H, Yang JW, Mann C. Genus. 2021;77:7. doi: 10.1186/s41118-021-00115-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Socioeconomic, demographic and healthcare determinants of the COVID-19 pandemic: an ecological study of Spain. García CN. BMC Public Health. 2021;21:606. doi: 10.1186/s12889-021-10658-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Health related factors contributing to COVID-19 fatality rates in various communities across the world. Shakor JK, Isa RA, Babakir-Mina M, Ali SI, Hama-Soor TA, Abdulla JE. J Infect Dev Ctries. 2021;15:1263–1272. doi: 10.3855/jidc.13876. [DOI] [PubMed] [Google Scholar]
- 71.Sex differences in case fatality rate of COVID-19: insights from a multinational registry. Alkhouli M, Nanjundappa A, Annie F, Bates MC, Bhatt DL. Mayo Clin Proc. 2020;95:1613–1620. doi: 10.1016/j.mayocp.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Beyond deaths per capita: comparative COVID-19 mortality indicators. Heuveline P, Tzen M. BMJ Open. 2021;11:0. doi: 10.1136/bmjopen-2020-042934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: a systematic review. Mackey K, Ayers CK, Kondo KK, et al. Ann Intern Med. 2021;174:362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Changes in the associations of race and rurality with SARS-CoV-2 infection, mortality, and case fatality in the United States from February 2020 to March 2021: A population-based cohort study. Ioannou GN, Ferguson JM, O'Hare AM, et al. PLoS Med. 2021;18:0. doi: 10.1371/journal.pmed.1003807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.A non-linear biostatistical graphical modeling of preventive actions and healthcare factors in controlling COVID-19 pandemic. Abdulla F, Nain Z, Karimuzzaman M, Hossain MM, Rahman A. Int J Environ Res Public Health. 2021;18:4491. doi: 10.3390/ijerph18094491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Estimation of case-fatality rate in COVID-19 patients with hypertension and diabetes mellitus in the New York state: a preliminary report. Ge Y, Sun S, Shen Y. Epidemiol Infect. 2021;149:0. doi: 10.1017/S0950268821000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Obesity as a predictor for a poor prognosis of COVID-19: a systematic review. Tamara A, Tahapary DL. Diabetes Metab Syndr. 2020;14:655–659. doi: 10.1016/j.dsx.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. Alqahtani JS, Oyelade T, Aldhahir AM, et al. PLoS One. 2020;15:0. doi: 10.1371/journal.pone.0233147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.COVID-19 case fatality rate and tuberculosis in a metropolitan setting. Rojas-Bolivar D, Intimayta-Escalante C, Cardenas-Jara A, Jandarov R, Huaman MA. J Med Virol. 2021;93:3273–3276. doi: 10.1002/jmv.26868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Demographic and public health characteristics explain large part of variability in COVID-19 mortality across countries. Hradsky O, Komarek A. Eur J Public Health. 2021;31:12–16. doi: 10.1093/eurpub/ckaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.The global case-fatality rate of COVID-19 has been declining since May 2020. Hasan MN, Haider N, Stigler FL, et al. Am J Trop Med Hyg. 2021;104:2176–2184. doi: 10.4269/ajtmh.20-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]