ABSTRACT
The purpose of this study was to determine the sex differences in the overall prevalence of radiographic femoroacetabular impingement (FAI) deformity patients presenting with hip pain and to identify the most common radiographic findings in male and female patients. A geographic database was used to identify patients between the age of 14 and 50 years with hip pain from 2000 to 2016. A chart and radiographic review was performed to identify patients with cam, pincer and mixed-type FAI. A total of 374 (449 hips) out of 612 (695 hips) male patients and 771 (922 hips) out of 1281 (1447 hips) female patients had radiographic features consistent with FAI. Ninety-four male hips (20.9%) and 45 female hips (4.9%) had cam type, 20 male hips (4.5%) and 225 female hips (24.4%) had pincer type and 335 male hips (74.6%) and 652 female hips (70.7%) had mixed type. The overall prevalence of radiographic findings consistent with FAI in male and female patients with hip pain was 61.1% and 60.2%, respectively. Mixed type was the most prevalent. The most common radiographic finding for cam-type FAI was an alpha angle >55°, and the most common radiographic finding for pincer-type FAI was a crossover sign. Male patients were found to have a higher prevalence of cam-type deformities, whereas female patients were found to have a higher prevalence of pincer-type deformities.
INTRODUCTION
Femoroacetabular impingement (FAI) is a common cause of hip pain and is a known risk factor for hip osteoarthritis and total hip arthroplasty at a young age [1–9]. The diagnosis of FAI is based on clinical symptoms, physical examination findings and imaging abnormalities. Although there have been substantial advancements in FAI diagnostic imaging modalities such as computed tomography [10, 11] and magnetic resonance imaging [12, 13], the conventional radiograph remains the most common method in the initial evaluation of a patient with FAI [14, 15].
There are three types of FAI: cam, pincer and mixed. Cam-type FAI is characterized by an abnormal/aspheric morphology of the femoral head and pincer type is characterized by focal or global acetabular over-coverage. Mixed type consists of a combination of cam and pincer characteristics [4, 16–20]. Surgical and non-surgical treatment options are based on different types and severity of FAI; therefore, it is important to accurately identify the type of FAI [14]. Radiographic parameters include the crossover sign (COS), posterior wall sign (PWS), ischial spine sign (ISS), coxa profunda, protrusion acetabuli, lateral center edge angle (LCEA), Tönnis angle and alpha angle [7, 21–27]. Previous studies have described the radiographic findings of FAI in athletes [28–32], asymptomatic volunteers [33], adolescents [34] and a general population of patients with hip pain [35]. However, the prevalence of radiographic findings of FAI in patients with hip pain based on sex is understudied.
Therefore, the purpose of this study was 3-fold: (I) to determine the overall prevalence of radiographic FAI deformities in male and female patients presenting with hip pain, (II) to identify the most common radiographic findings in male and female patients with cam-type FAI and (III) to identify the most common radiographic findings in male and female patients with pincer-type FAI. This study involves a large cohort of patients with hip pain, which is unique. We are unaware of any prior study that reports the difference in prevalence based on the sex of FAI radiographic abnormalities in patients presenting to their physician with hip pain. Prior studies have evaluated asymptomatic patients in smaller cohorts. We hypothesized that the overall prevalence of radiographic findings consistent with FAI will be similar between males and females.
METHODS
A geographic-based cohort study was performed with the Rochester Epidemiology Project (REP) database in Olmsted County, MN, USA, which had a population of 144 260 in 2010. The REP is medical record linkage system that provides access to the complete medical records for all residents of Olmsted County, regardless of the medical facility in which the care was delivered [36]. Institutional review board approval (IRB#: 17-l004959, IRB Modification #: Mod17-004959-02) was obtained, and the REP was used to identify all patients in a geographic area who presented to a physician with hip pain and had an initial diagnosis of an International Classification of Diseases, Ninth Revision or Tenth Revision, diagnostic code of hip pain, hip impingement or hip joint disorders between January 2000 and December 2016. Only patients aged between 14 and 50 years were included. The upper age limit is consistent with prior studies on FAI [7, 37]. Patients with a history of avascular necrosis, trochanteric bursitis, hip fracture, pelvic fracture, previous hip surgery and/or hip dislocation were excluded.
A thorough chart and radiographic review was performed on all patients. All radiographs were reviewed by attending- or senior resident–level orthopedic surgeons (H.P.M. and J.Z.). The first 100 radiographic reviews were evaluated by the two authors (H.P.M. and J.Z.) to ensure agreement. All patients underwent anteroposterior (AP) pelvic view (Fig. 1a and b) and lateral view (cross-table, frog-leg or 45° Dunn) radiographs upon initial assessment by a physician for hip pain. We evaluated for a pistol grip deformity on a standard AP pelvic view (Fig. 2a and b) and measured the alpha angle manually on a lateral radiographic view (cross-table, frog-leg or 45° Dunn) (Fig. 2c and d). We evaluated the COS (Fig. 3a and b), PWS (Fig. 3c and d), ISS (Fig. 3e and f), coxa profunda (Fig. 3g and h) and protrusio acetabuli (Fig. 4a and b) and measured the LCEA (Fig. 5a and b) and Tönnis angle (Fig. 6a and b) on a standard AP pelvic view. All methods of evaluation and measurement were described in a previous study [35]. Clohisy et al. [22] defined the standardized radiographic parameters that were used in this study. Radiographs not compliant with the parameters were not included.
Fig. 1.

Standard anteroposterior pelvic views of normal hips in male (a) and female (b), a yellow dash line connecting bilateral inferior margins of pelvic teardrops represents a horizontal baseline, a yellow dot best-fit circle represents the right femoral head contour, a red dot represents the center of femoral head, a red line represents anterior acetabular rim, a red dash line represents posterior acetabular rim, a red dot curve represents acetabuli fossa and a blue dash line represents ilioischial line.
Fig. 2.

Typical pistol grip deformity in male (a, arrow) and female (b, arrow), and a yellow dot best-fit circle represents the femoral head contour; Alpha angle > 55° in male (c) and female (d), frog leg view.
Fig. 3.
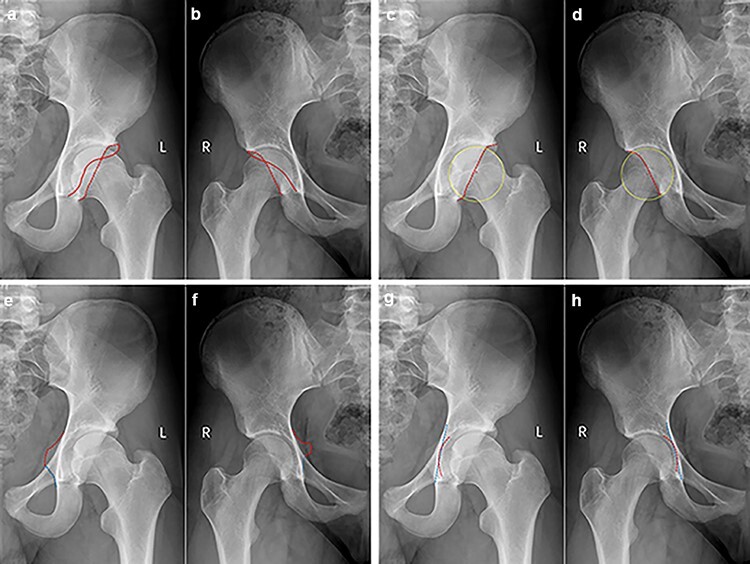
Cross-over sign in male (a) and female (b), red line represents anterior acetabular rim and red dash line represents posterior acetabularrim; Posterior wall sign in male (c) and female (d), yellow dot best-fit circle represents the femoral head contour, red point represents the center of femoral head and red dash line represents posterior acetabular rim; Ischial spine sign in male (e) and female (f), red dash line represents protrude ischial spine; and Coxa profunda in male (g) and female (h), red dash curve represents acetabuli fossa and blue dash line represents ilioischial line.
Fig. 4.
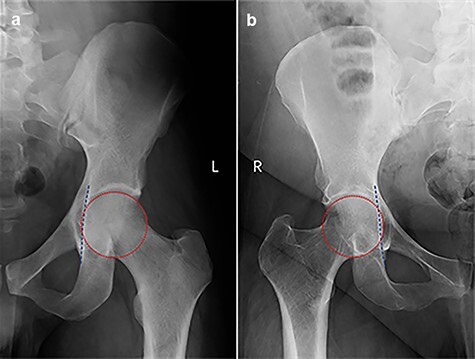
Protrusio acetabuli in male (a) and female (b), the best-fit circle represents the femoral head contour and the dashed line defines the ilioischial line.
Fig. 5.

LCEA≥40° in male (a) and female (b).
Fig. 6.

Tönnis angle << 0° in male (a) and female (b).
The radiographic findings associated with the three types of FAI were the following:
Cam type: typical pistol grip deformity and/or alpha angle >55° [21, 23, 24, 26].
Pincer type: COS [22–25, 27] and/or coxa profunda or protrusio acetabuli [7, 22, 25, 27] and/or LCEA ≥40° [7, 23, 25–27] and/or Tönnis angle <0° [22].
Mixed type: both cam and pincer type features.
Statistical analysis
Data were collected in a password-protected database. Chi-square Test, Fisher’s exact test and independent-sample T-test were performed on the quantity and percentage of all radiographic signs and parameters between male and female. Statistical significance was considered at the 0.05 level of probability. Analyses were performed using IBM SPSS Statistics Version 25 (IBM Corporation, Armonk, NY).
RESULTS
A total of 374 (449 hips; mean age, 28.6 ± 8.6) male patients of 612 (695 hips) and 771 (922 hips; mean age, 29.0 ± 8.4) female patients of 1281 (1447 hips) presenting with hip pain had radiographic features consistent with FAI criteria (Table I).
Table I.
Prevalence of radiographic FAI deformities in males and females
| n (%) | ||||
|---|---|---|---|---|
| Diagnosis | Male | Female | χ2 | P |
| Femoroacetabular impingement | 374/612 (61.1) | 771/1281 (60.2) | 0.148 | 0.701 |
The distribution of various types in these FAI patients is shown in Table II. There were 429 (94 + 335) hips with cam features (cam + mixed) and 355 (20 + 335) hips with pincer features (pincer + mixed) in males and 697 (45 + 652) hips with cam features (cam + mixed) and 877 (225 + 652) hips with pincer features (pincer + mixed) in females.
Table II.
Distribution of the three types of femoroacetabular impingement
| n (%) | ||||
|---|---|---|---|---|
| Type | Male | Female | χ2 | P |
| Cam | 94/449 (20.9) | 45/922 (4.9) | 85.427 | 0.000 |
| Pincer | 20/449 (4.5) | 225/922 (24.4) | 81.876 | 0.000 |
| Mixed | 335/449 (74.6) | 652/922 (70.7) | 2.271 | 0.132 |
Bold signifies statistical significance.
The prevalence of specific cam-type radiographic parameters is reported in Table III.
Table III.
Cam-type radiographic findings in male and female
| n (%) or angle (°) | ||||
|---|---|---|---|---|
| Signs and parameters | Male | Female | χ2/t | P |
| Typical pistol grip deformity | 328/449 (73.1) | 249/922 (27.0) | 262.65 | 0.000 |
| Alpha angle >55° | 399/449 (88.9) | 670/922 (72.7) | 46.116 | 0.000 |
| Mean alpha angle | 66.8° ± 12.2° (n = 449) |
59.6° ± 14.9° (n = 922) |
8.991 | 0.000 |
Bold signifies statistical significance.
The prevalence of specific cam-type radiographic parameters is reported in Table IV. Findings with a prevalence of >50% are listed in order as follows: COS, PWS and ISS in males and COS, coxa profunda, ISS and PWS in females.
Table IV.
Pincer-type radiographic findings in male and female
| N (%) | ||||
|---|---|---|---|---|
| Signs and parameters | Male | Female | χ2 | P |
| Crossover sign | 339/449 (75.5) | 723/922 (78.4) | 1.470 | 0.225 |
| Posterior wall sign | 281/449 (62.6) | 483/922 (52.4) | 12.727 | 0.000 |
| Ischial spine sign | 258/449 (57.5) | 507/922 (55.0) | 0.748 | 0.387 |
| Coxa profunda | 138/449 (30.7) | 706/922 (76.6) | 268.106 | 0.000 |
| Protrusio acetabuli | 1/449 (0.2) | 6/922 (0.7) | – | 0.437a |
| Tönnis angle <0° | 81/449 (18.0) | 231/922 (25.1) | 8.451 | 0.004 |
| Lateral center edge angle ≥40° | 54/449 (12.0) | 116/922 (12.6) | 0.086 | 0.770 |
Fisher’s exact test.
Bold signifies statistical significance.
DISCUSSION
An alpha angle >55° was the most common cam-type finding, and COS was the most common pincer type finding in both male and female patients. Additionally, the overall prevalence of radiographic findings consistent with FAI in male and female patients was 61.1% and 60.2%, respectively.
In the present investigation, mixed type was most common, which is consistent with previous studies [4, 19, 38–40]. Cam-type FAI was more common in male patients, while pincer type was more common in female patients. These findings are supported by the current literature which suggests that structural abnormalities in male FAI patients are more commonly present on the femur, while those in female FAI patients are more commonly present on the acetabulum [19, 38, 39, 41, 42].
A pistol grip deformity is a lateral osseous bump on the femoral head–neck junction (FHNJ) [43]. An increased alpha angle represents a prominence of the anterior FHNJ, which causes impingement of the anterior/anterosuperior femoral head–neck against the acetabulum [44]. Both a pistol grip deformity and an alpha angle >55° are associated with cam-type FAI [29, 45]. In the current investigation, more than two-thirds of male cam-type FAI patients (73.1%) had typical pistol grip deformities, while less than one-third of female cam-type FAI patients (27.0%) had pistol grip deformities. More male patients had an alpha angle >55° (88.9% versus 72.7%), and the mean alpha angle (66.8° ± 12.2° versus 59.6° ± 14.9°) was larger than that of female patients. Hooper et al. [34]. also found that cam deformities are more common and severe in male patients. In the present study, an increased alpha angle was more common than a pistol grip deformity in males and females.
Radiographic findings of COS and ISS were the first and third most common features in both male and female pincer hips. However, PWS was the second most common in male pincer hips, while coxa profunda was the second most common finding in female pincer hips. COS and PWS were first described by Reynolds et al. [46] in 1999, and the ISS was first described by Kalberer et al. [47] in 2008. These three signs can be used to diagnose acetabular retroversion, resulting in a prominent anterolateral edge of the acetabulum and potential anterolateral over-coverage [7, 48, 49]. Accordingly, these findings support the notion that the anterolateral over-coverage caused by acetabular retroversion might be the primary factor of pincer FAI in both males and females.
The prevalence of coxa profunda in pincer FAI was the fourth highest in males and the second highest in females. Both coxa profunda and protrusio acetabuli result in increased acetabular depth, causing global acetabular over-coverage [27, 50]. The deep socket potentially limits the movement of the femoral head in all directions and leads to a more circumferential pattern of impingement [38]. The presented findings suggest that global acetabular over-coverage is less common in pincer FAI than focal acetabular over-coverage resulting from acetabular retroversion. The prevalence of coxa profunda in males was less than that in females (30.7% versus 76.6%).
Both LCEA ≥40° and Tönnis angle <0° are indicators of superolateral acetabular over-coverage [51] and can be used to evaluate pincer-type FAI. In this study, the prevalences of an LCEA ≥40° and a Tönnis angle <0° in pincer FAI were 12.0% and 18.0% in males and were 12.6% and 25.1% in females, respectively. The relatively low prevalence of LCEA ≥40° and a Tönnis angle <0° suggests that the superolateral acetabular over-coverage is a less common cause of pincer FAI in both males and females.
The current investigation is not without limitations. The retrospective nature of the study affords inherent limitations. Dunn, cross-table and frog-leg lateral views were all used to measure alpha angles, but the measurement of alpha angles using all of these views has not been validated. In addition, only radiographs were evaluated so we were not able to identify cartilage and/or labral pathology. We were not able to confirm that all patients had symptoms and physical examination findings consistent with FAI. No treatment- or patient-reported outcomes were obtained in this study so we are unable to comment on the clinical relevance of each of these radiographic parameters. Despite these limitations, this study involves a large cohort of patients presenting to their physician with hip pain, which is unique. We are unaware of a prior study that reports the difference in prevalence based on the sex of FAI radiographic abnormalities in patients presenting to their physician with hip pain. Prior studies have evaluated smaller cohorts of asymptomatic patients.
CONCLUSION
The overall prevalence of radiographic findings consistent with FAI in male and female patients with hip pain was 61.1% and 60.2%, respectively. Among the three types of FAI, mixed type was the most prevalent. The most common radiographic finding for cam-type FAI was an alpha angle >55°, and the most common radiographic finding for pincer-type FAI was a COS. Male patients were found to have a higher prevalence of cam-type deformities, whereas female patients were found to have a higher prevalence of pincer-type deformities.
ACKNOWLEDGEMENTS
The authors thank Zhefeng Chen, MD, of the Department of Orthopedic Surgery, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China, for his advice regarding the measurement and evaluation of radiographs.
Contributor Information
Jun Zhou, Department of Orthopedic Surgery, The First Affiliated Hospital of Soochow University, 296 Shizi St, Cang Lang Qu, Suzhou, Jiangsu, China.
Heath P Melugin, Department of Orthopedic Surgery, Mayo Clinic, 200 1st St SW, Rochester, MN 55905, USA.
Rena F Hale, Department of Orthopedic Surgery, Mayo Clinic, 200 1st St SW, Rochester, MN 55905, USA.
Bryant M Song, Department of Orthopedic Surgery, Mayo Clinic, 200 1st St SW, Rochester, MN 55905, USA.
Kelechi R Okoroha, Department of Orthopedic Surgery, Mayo Clinic, 200 1st St SW, Rochester, MN 55905, USA.
Bruce A Levy, Department of Orthopedic Surgery, Mayo Clinic, 200 1st St SW, Rochester, MN 55905, USA.
Aaron J Krych, Department of Orthopedic Surgery, Mayo Clinic, 200 1st St SW, Rochester, MN 55905, USA.
DATA AVAILABILITY
The data underlying this article are available in the article and in its online supplementary material.
FUNDING
Quattrone-Foderaro Musculoskeletal/Orthopedic Surgery Research Innovation Fund; the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
REFERENCES
- 1. Carton PF, Filan DJ. The clinical presentation, diagnosis and pathogenesis of symptomatic sports-related femoroacetabular impingement (SRFAI) in a consecutive series of 1021 athletic hips. Hip Int 2019; 29: 665–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eijer H, Hogervorst T. Femoroacetabular impingement causes osteoarthritis of the hip by migration and micro-instability of the femoral head. Med Hypotheses 2017; 104: 93–6. [DOI] [PubMed] [Google Scholar]
- 3. Kowalczuk M, Yeung M, Simunovic N et al. Does femoroacetabular impingement contribute to the development of hip osteoarthritis? A systematic review. Sports Med Arthrosc Rev 2015; 23: 174–9. [DOI] [PubMed] [Google Scholar]
- 4. Melugin HP, Hale RF, Zhou J et al. Risk factors for long-term hip osteoarthritis in patients with femoroacetabular impingement without surgical intervention. Am J Sports Med 2020; 48: 2881–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Menge TJ, Truex NW. Femoroacetabular impingement: a common cause of hip pain. Phys Sportsmed 2018; 46: 139–44. [DOI] [PubMed] [Google Scholar]
- 6. van Klij P, Heerey J, Waarsing JH et al. The prevalence of cam and pincer morphology and its association with development of hip osteoarthritis. J Orthop Sports Phys Ther 2018; 48: 230–8. [DOI] [PubMed] [Google Scholar]
- 7. Wyles CC, Heidenreich MJ, Jeng J et al. The John Charnley Award: redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res 2017; 475: 336–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smolders JMH, Speirs AD, Frei H et al. Higher patient activity level and subchondral stiffening in asymptomatic cam femoroacetabular impingement subjects. J Hip Preserv Surg 2018; 5: 259–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hale RF, Melugin HP, Zhou J et al. Incidence of femoroacetabular impingement and surgical management trends over time. Am J Sports Med 2021; 49: 35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dessouky R, Chhabra A, Zhang L et al. Cam-type femoroacetabular impingement—correlations between alpha angle versus volumetric measurements and surgical findings. Eur Radiol 2019; 29: 3431–40. [DOI] [PubMed] [Google Scholar]
- 11. Zhang L, Wells JE, Dessouky R et al. 3D CT segmentation of CAM type femoroacetabular impingement-reliability and relationship of CAM lesion with anthropomorphic features. Br J Radiol 2018; 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lerch TD, Degonda C, Schmaranzer F et al. Patient-specific 3-D magnetic resonance imaging-based dynamic simulation of hip impingement and range of motion can replace 3-D computed tomography-based simulation for patients with femoroacetabular impingement: implications for planning open hip preservation surgery and hip arthroscopy. Am J Sports Med 2019; 47: 2966–77. [DOI] [PubMed] [Google Scholar]
- 13. Samim M, Eftekhary N, Vigdorchik JM et al. 3D-MRI versus 3D-CT in the evaluation of osseous anatomy in femoroacetabular impingement using Dixon 3D FLASH sequence. Skeletal Radiol 2019; 48: 429–36. [DOI] [PubMed] [Google Scholar]
- 14. Genovese E, Spiga S, Vinci V et al. Femoroacetabular impingement: role of imaging. Musculoskelet Surg 2013; 97: S117–26. [DOI] [PubMed] [Google Scholar]
- 15. Ranawat AS, Schulz B, Baumbach SF et al. Radiographic predictors of hip pain in femoroacetabular impingement. HSS J 2011; 7: 115–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Amanatullah DF, Antkowiak T, Pillay K et al. Femoroacetabular impingement: current concepts in diagnosis and treatment. Orthopedics 2015; 38: 185–99. [DOI] [PubMed] [Google Scholar]
- 17. Bedi A, Kelly BT. Femoroacetabular impingement. J Bone Joint Surg Am 2013; 95: 82–92. [DOI] [PubMed] [Google Scholar]
- 18. Ganz R, Gill TJ, Gautier E et al. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001; 83: 1119–24. [DOI] [PubMed] [Google Scholar]
- 19. Ganz R, Parvizi J, Beck M et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20. [DOI] [PubMed] [Google Scholar]
- 20. Haldane CE, Ekhtiari S, de Sa D et al. Preoperative physical examination and imaging of femoroacetabular impingement prior to hip arthroscopy—a systematic review. J Hip Preserv Surg 2017; 4: 201–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beall DP, Sweet CF, Martin HD et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol 2005; 34: 691–701. [DOI] [PubMed] [Google Scholar]
- 22. Clohisy JC, Carlisle JC, Beaule PE et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 2008; 90: 47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Griffin DR, Dickenson EJ, Wall PDH et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet 2018; 391: 2225–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guo Y, Zhang H, Qian H et al. Association of femoroacetabular impingement and delayed gadolinium-enhanced magnetic resonance imaging of cartilage: a population-based study. Arthritis Care Res (Hoboken) 2018; 70: 1160–8. [DOI] [PubMed] [Google Scholar]
- 25. Kutty S, Schneider P, Faris P et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop 2012; 36: 505–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li Y, Helvie P, Mead M et al. Prevalence of femoroacetabular impingement morphology in asymptomatic adolescents. J Pediatr Orthop 2017; 37: 121–6. [DOI] [PubMed] [Google Scholar]
- 27. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 2007; 188: 1540–52. [DOI] [PubMed] [Google Scholar]
- 28. Kapron AL, Peters CL, Aoki SK et al. The prevalence of radiographic findings of structural hip deformities in female collegiate athletes. Am J Sports Med 2015; 43: 1324–30. [DOI] [PubMed] [Google Scholar]
- 29. Kim J, Choi JA, Lee E et al. Prevalence of imaging features on CT thought to be associated with femoroacetabular impingement: a retrospective analysis of 473 asymptomatic adult hip joints. AJR Am J Roentgenol 2015; 205: W100–5. [DOI] [PubMed] [Google Scholar]
- 30. Langner JL, Black MS, MacKay JW et al. The prevalence of femoroacetabular impingement anatomy in Division 1 aquatic athletes who tread water. J Hip Preserv Surg 2020; 7: 233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ishoi L, Thorborg K, Kraemer O et al. The association between specific sports activities and sport performance following hip arthroscopy for femoroacetabular impingement syndrome: a secondary analysis of a cross-sectional cohort study including 184 athletes. J Hip Preserv Surg 2019; 6: 124–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jonasson P, Thoreson O, Sansone M et al. The morphologic characteristics and range of motion in the hips of athletes and non-athletes. J Hip Preserv Surg 2016; 3: 325–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Frank JM, Harris JD, Erickson BJ et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy 2015; 31: 1199–204. [DOI] [PubMed] [Google Scholar]
- 34. Hooper P, Oak SR, Lynch TS et al. Adolescent femoroacetabular impingement: gender differences in hip morphology. Arthroscopy 2016; 32: 2495–502. [DOI] [PubMed] [Google Scholar]
- 35. Zhou J, Melugin HP, Hale RF et al. The prevalence of radiographic findings of structural hip deformities for femoroacetabular impingement in patients with hip pain. Am J Sports Med 2020; 48: 647–53. [DOI] [PubMed] [Google Scholar]
- 36. Sanders TL, Pareek A, Desai VS et al. Low accuracy of diagnostic codes to identify anterior cruciate ligament tear in orthopaedic database research. Am J Sports Med 2018; 46: 2894–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hartofilakidis G, Bardakos NV, Babis GC et al. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br 2011; 93: 580–6. [DOI] [PubMed] [Google Scholar]
- 38. Beck M, Kalhor M, Leunig M et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 39. Bittersohl B, Steppacher S, Haamberg T et al. Cartilage damage in femoroacetabular impingement (FAI): preliminary results on comparison of standard diagnostic vs delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC). Osteoarthritis Cartilage 2009; 17: 1297–306. [DOI] [PubMed] [Google Scholar]
- 40. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg 2007; 15: 561–70. [DOI] [PubMed] [Google Scholar]
- 41. Leunig M, Juni P, Werlen S et al. Prevalence of cam and pincer-type deformities on hip MRI in an asymptomatic young Swiss female population: a cross-sectional study. Osteoarthritis Cartilage 2013; 21: 544–50. [DOI] [PubMed] [Google Scholar]
- 42. Okpala VB, Tennent DJ, Johnson AE et al. Sexual dimorphic features associated with femoroacetabular impingement. US Army Med Dep J 2018; 2-18: 65–73. [PubMed] [Google Scholar]
- 43. Jager M, Wild A, Westhoff B et al. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci 2004; 9: 256–63. [DOI] [PubMed] [Google Scholar]
- 44. Ipach I, Mittag F, Walter C et al. The prevalence of acetabular anomalies associated with pistol-grip-deformity in osteoarthritic hips. Orthop Traumatol Surg Res 2013; 99: 37–45. [DOI] [PubMed] [Google Scholar]
- 45. Chakraverty JK, Sullivan C, Gan C et al. Cam and pincer femoroacetabular impingement: CT findings of features resembling femoroacetabular impingement in a young population without symptoms. AJR Am J Roentgenol 2013; 200: 389–95. [DOI] [PubMed] [Google Scholar]
- 46. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 1999; 81: 281–8. [DOI] [PubMed] [Google Scholar]
- 47. Kalberer F, Sierra RJ, Madan SS et al. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res 2008; 466: 677–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Werner CM, Copeland CE, Ruckstuhl T et al. Radiographic markers of acetabular retroversion: correlation of the cross-over sign, ischial spine sign and posterior wall sign. Acta Orthop Belg 2010; 76: 166–73. [PubMed] [Google Scholar]
- 49. Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res 1999; 363: 93–9. [PubMed] [Google Scholar]
- 50. Larson CM. Arthroscopic management of pincer-type impingement. Sports Med Arthrosc Rev 2010; 18: 100–7. [DOI] [PubMed] [Google Scholar]
- 51. Nepple JJ, Brophy RH, Matava MJ et al. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy 2012; 28: 1396–403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.


