Abstract
Free vascularized fibular grafting was reported a favorable method to prevent the collapse of the femoral head. This study analyzed the mid- to long-term outcomes of avascular fibular grafting (AVFG) for osteonecrosis of the femoral head (ONFH) with 6- to 8-year follow-up. From March 2009 to March 2012, 34 patients (48 hips) were diagnosed with ONFH operated with AVFG in Jiangsu Province Hospital of traditional Chinese Medicine. We retrospectively reviewed the clinic outcomes of these patients and evaluated the differences in outcomes by diverse stages [Association Research Circulation Osseous (ARCO)] and types [China–Japan Friendship Hospital (CJFH) classification] annually. The hip survival rate, Harris hip score (HHS), activity level and imaging stability were calculated. The average follow-up time was 6.7 years. At the last follow-up, 34 of 48 hips survived totally. According to the ARCO stage, the overall clinical success rate for hip preserving were 76.0% (19/25) in II stage, 85.7% (12/14) in IIIA stage and 33.3% (3/9) in IIIB stage. Referring to the CJFH classification system, the hip survival rate were 100% (2/2) in M type, 90.9% (10/11) in C type, 77.8% (14/18) in L1 type, 57.1% (8/14) in L2 type and 0% (0/3) in L3 type. The mean visual analog scale (VAS) score, HHS and Western Ontario McMaster Osteoarthritis index (WOMAC) were significantly improved at the final follow-up compared with pre-operative values (P < 0.001). The AVFG operation can increase the hip function and improve patients’ lives quality. The mid- to long-term efficacy can satisfy fundamental life requirements, especially for those early-stage and small-scale patients who suffer ONFH to avoid or put off the time of total hip arthroplasty surgery.
Osteonecrosis of the femoral head (ONFH) is often with a progressive course, which primarily affects young adults and finally necessitates total hip arthroplasty (THA) [1]. It is estimated that there are ∼8.12 million people over the age of 15 with ONFH in China [2]. Various treatment protocols for ONFH have been attempted with diverse therapies and prognoses, such as medullary core decompression, hip arthroscopy, tantalum rod implantation, fibular support surgery, osteotomy, cell-based treatments and some medicines for instance bisphosphonate [3–6]. Nevertheless, it is no doubt that the preservation of the femoral head for several years or more remains the main goal of treatment for young patients.
In recent years, the free vascularized fibular grafting (FVFG) has been shown as a valuable operation for dealing with ONFH by providing revascularization, mechanical support and dynamic cells to the femoral head [7]. The traditional technique of this surgical management of ONFH, in which the vascular pedicle is dissected prior to osteotomy in the harvest of the vascularized fibular graft, the process may have some disadvantages including increase of surgery time, microvascular anastomosis and risk of the proximal femoral fracture [8].
Avascular fibular grafting (AVFG) for ONFH was used widely in the past two decades [9]. The advances of this operation included smaller trauma(without vascular anastomosis and usually use the allograft), simple technology, less complications and lower expense [10]. Researchers had reported the outcomes of a vascularized fibular grafting but the outcomes were various. Tetik et al. [11] found that the group treated by vascularized fibular grafting had significantly higher Harris hip score (HHS) and visual analog scale (VAS) score than the ones treated by non-vascularized fibular grafting in the mean follow-up of 12 months. Jie et al. [12] reported that autologous and allogeneic fibular grafts can attain equally good clinical outcomes and high survival rates in long-term follow-up. Plenty of literature researches reported that with choosing strictly indications the AVFG might have ideal clinic outcomes as well as FVFG [13]. Chen et al. [13] conducted research regarding a analysis of the necrosis of femoral head with Ficat II that had underwent Non-vascularized bone grafting operation for the treatment. At the final follow-up, 44 patients showed 81.8% of 7-year survival rate using conversion to THA as the end point. Another scholar compared the autograft implantation to the bone grafting through fenestration over femoral head and neck with an 8–40 months’ follow-up. Stage II B–IIIA according to the classification system of Association Research Circulation Osseous (ARCO) were selected in this study. At the last follow-up, the Harris hip aggregate score, pain score and range of motion score of patients under autograft implanting were all significantly superior to the bone grafting group [14]. Just like the study above, our experiences of clinical treatment showed that with thoroughly clearing the sequestrums and tightly impacted bone grafting, the AVFG operation can provide potent supporting for the femoral head to avoid the femoral head collapse. Our study aimed to assess the medium- to long-term clinical and radiological outcomes for this sort of surgery in patients of ARCO Stage II –IIIB and explore the optimum indications of this operation.
MATERIALS AND METHODS
We retrospectively reviewed our database of Jiangsu Province Hospital of Traditional Chinese Medicine during March 2009 to March 2012 and identified 34 patients with 48 AVFG operations, whose stage were at ARCO Stage II –IIIb of ONFH. Patients this study included were <55 years. All patients treated with using the same standard instruments and all operations were performed by a single, experienced surgeon. The patients included in the study consisted of 29 males with 40 hips and 5 females with 8 hips. Pathogenic factors included using glucocorticoid continuously, long-term alcohol consumption, trauma, hypercoagulable state (such as anticardiolipin antibodies syndrome) and idiopathic cases. Functional disorder of hip and hip pain occurred in all patients. The diagnosis of ONFH was based on symptoms, physical signs, previous relative medical history and relevant risk factors. In addition, anteroposterior (AP) and frog-leg lateral (FL) views of bilateral hip, computed tomography (CT) and magnetic resonance image were generally used in each patient to confirm the diagnosis and to refine the type. Diagnostic criteria are ‘Guidelines for the Clinical Diagnosis and Treatment of adult femur head necrosis (2019 edition)’ [15]. The survivorship was equal to the total percentage of the patients who remained in good condition and did not need to undergo the THA. The patients’ background and details are listed in Table I. The study was approved by the Clinical Trials and Biomedical Ethics Committee of Affiliated hospital of Nanjing University of Chinese Medicine, and written informed consent was obtained from all participants. All experiments were performed in accordance with relevant guidelines and regulations.
Table I.
Demographic characteristic of the patients
| Parameters | Average (range) |
|---|---|
| Total number | 34 patients (48hips) |
| Age (years) | 36. 97 (20–54) |
| Body mass index (kg/m2) | 23.32 (18.8–27.5) |
| Gender (male/female) | 29/5 |
| Classification | |
| ARCO | |
| Stage II | 25 |
| Stage IIIA | 14 |
| Stage IIIB | 9 |
| CJFH | |
| M | 2 |
| C | 11 |
| L1 | 18 |
| L2 | 14 |
| L3 | 3 |
Surgery was all performed under general anesthetic. Each patient was positioned supine with a bolster under the ipsilateral buttock. After skin preparation and sterile draping, a 7- to 8-cm length of incision along the Watson–Jones approach upper to the greater trochanter was performed. Once the greater trochanter was exposed, we performed the core decompression of the femoral head. Two centimeter down-ward to the tip of the greater trochanter, we inserted a 2.5 mm Kirschner pin toward anterior-lateral necrotic area of the femoral head till 0.5 cm underneath the subchondral bone. When the Kirschner pin positioned correctly under the C-arm X-ray machine, we detected the length of Kirschner pin inserted in the femoral neck and head, a matched self-designed hollow reamer was used to broach the tunnel along the pin till 0.5 cm below the subchondral bone. We applied different diameter of ‘T’ shape hand driller to broach the tunnel to 10–12 mm which was determined by the allograft non-vascularized fibular bone maximal breadth. The necrotic bone must be removed along the tunnel with a curet, especially in the lateral loading area. Subsequently, we performed tightly impaction bone grafting to the necrotic area with allogeneic bone granule which was loaded into a self-designed plugger. The crucial techniques of tightly impaction bone grafting were layer-by-layer and 360°impaction with differing sizes of straight and curved head impaction rod. The standard criterion of complete impaction bone grafting was that the density of the necrotic bone was equally increased and restoration of the femoral head normal shape under C-arm. Before allogeneic fibular implantation, we drilled bi-cortical crossed holes at 0.5 mm interval vertical to the axial of the allograft fibular with 2 mm Kirschner pin which was considered to be beneficial to the new formed repair bone creeping substitution (Fig. 1). And the tip of the allograft fibular was blunt and 40° slope processed with bone file which can decrease the mechanical stress through the increasing bony contact. The predisposed allograft fibular was inserted tightly into the well-prepared tunnel with the impaction rod till 0.5 cm below the subchondral bone through fluoroscopy and the protrude end was trimmed with bone rongeur. We closed the incision after complete sterile saline solution wash which prevent the heterotopic ossification in the surgical site and keep the drainage tube for 2 days. Weight-bearing was strictly prohibited after surgery and the quadriceps and iliopsoas muscles were trained in bed. X-ray was taken after 3 months for reexamination. If the internal structure of femoral head was stable, partial load can be carried out with a walking aid. Six months after surgery, the full weight-bearing was permitted.
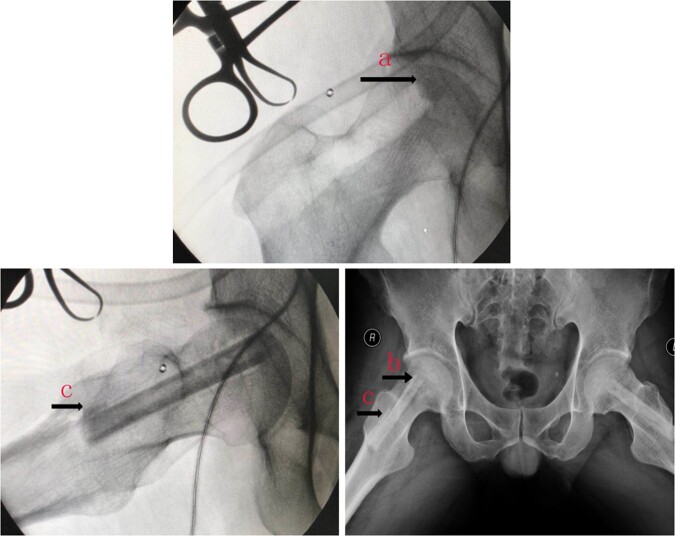
Fig. 1.
The density of compression implant should exceed the surrounding cancellous bone (arrow, a). The hole was drilled with Kirschner’s needle (arrow, b), Fill the outside of the passage to make it jam (arrow, c).
Statistical analysis
The pre- and post-treatment data within the same group were compared statistically using the Kruskal–Wallis test and Kaplan–Meier method. The data are represented by medians and CIs. All data were processed through SPSS16.0 and P values < 0.01 were considered as statistical significance.
RESULTS
A total of 34 hips performed well in all 48 hips followed up, which arthroplasty surgery was not required in the short term. Most of the femoral heads with successful hip preservation showed stable repairing in the head. About half (14/34) of the imaging showed slight collapse (≤1 mm), but with no clinic symptoms. These femoral heads were characterized by slight collapse, but the subchondral bone is well bonded to the repair area and is therefore structurally stable. All the hip joints with good efficacy had significant high density repair bands in the compression zone of bone graft. The restoration band edges were well integrated with the surrounding bone trabeculae, and there were no obvious bright lines around the restoration zone (Fig. 2). The proportion of imaging stable repair was well correlated with pre-operative China–Japan Friendship Hospital (CJFH) classification and was also associated with ARCO stage and necrotic area [16, 17].
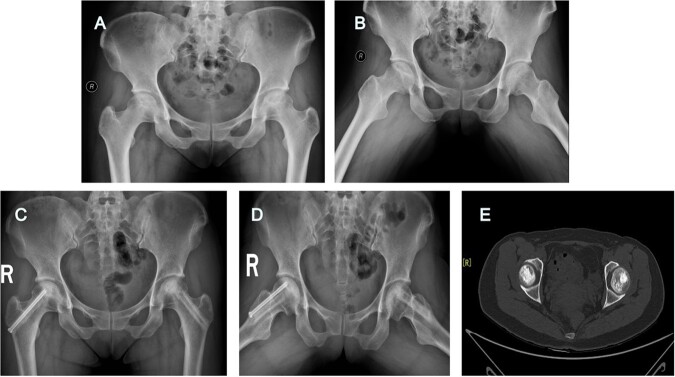
Fig. 2.
The patient’s pre-operative AP/FL film showed obvious sclerosing zone (A, B).6 years after surgery, no collapse was found, and a high-density restoration zone was found (C, D).CT shows that the implant has formed good integration with the surrounding bone (E).
During an average of 6.7 years follow-up, Kaplan–Meier survival curve of the patients included in this study was consistently associated with pre-operative ARCO stage (Fig. 3). At 2 years follow-up, patients of ARCO stage were without fail completely. But, the survival rate of hips in this study was not exactly presenting positive correlation with ACRO stage. At the last follow-up, depending on the ARCO stage, the hip survival rate were 76.6% (19/25) in II stage, 85.7% (12/14) in IIIA stage and 33.3% (3/9) in IIIB stage (Table II). When compared with ARCO stage, Kaplan–Meier survival curve of hip joint during follow-up in this study had a better correlation with pre-operative CJFH classification system (Fig. 4). Referring to the CJFH classification system, the hip survival rate were 100% (2/2) in M type, 90.9% (10/11) in C type, 77.8% (14/18) in L1 type, 57.1% (8/14) in L2 type and 0% (0/3) in L3 type at the last follow-up (Table II).
Fig. 3.
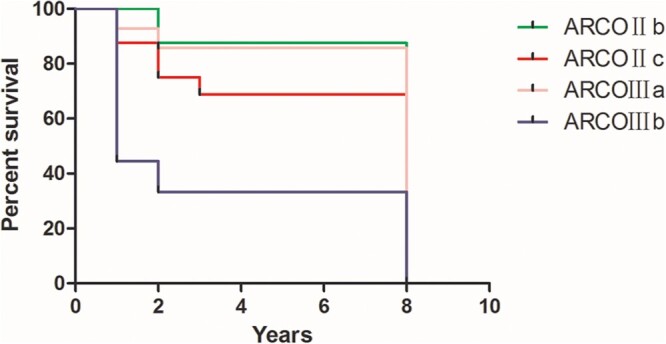
Kaplan–Meier survival curve according to ARCO stage.
Table II.
Difference of survivorship among the groups
| Groups | Surviver/total | Survival rates | Averagea | SD | 95% CI |
|---|---|---|---|---|---|
| ARCO | |||||
| Stage II | 19/25 | 76.0% | 6.720 | 0.461 | (5.816, 7.624) |
| Stage IIIA | 12/14 | 85.7% | 7.214 | 0.517 | (6.201, 8.227) |
| Stage IIIB | 3/9 | 33.3% | 4.111 | 0.922 | (2.304, 5.919) |
| Totality | 34/48 | 70.8% | 6.375 | 0.369 | (5.652, 7.098) |
| CJFHb | |||||
| M | 2/2 | 100.0% | – | – | – |
| C | 10/11 | 90.9% | 7.455 | 0.520 | (6.435, 8.474) |
| L1 | 14/18 | 77.8% | 6.778 | 0.542 | (5.716, 7.840) |
| L2 | 8/14 | 57.1% | 5.643 | 0.740 | (4.193, 7.092) |
| L3 | 0/3 | 0.0% | 2.333 | 0.333 | (1.680, 2.987) |
| Totality | 34/48 | 70.8% | 6.304 | 0.381 | (5.557, 7.052) |
If the estimate is limited, the maximum survival time is limited.
The CJFH M group survival rate was 100% which could not be calculated and was excluded.
Fig. 4.

Kaplan–Meier survival curve according to CJFH classification.
After AVFG, the majority of patients reported considerable relief of hip pain at night and better hip motion in daily activity and work. We found that the VAS score, HHS and Western Ontario McMaster Osteoarthritis index (WOMAC) of the patients were significantly improved compared with pre-operation (Table III). VAS scores were improved from 2.9 to 1.45 on average. And the overall HHS scores were improved from 51.5 to 85.5 on average at the last follow-up. The patient obtained significant improvement in pain and good hip function in all directions what the patient expects. In this study, pain was the main factor leading to failure of hip preservation, followed by decreased painless activity ability, especially the painless walking distance <200 m, which was disastrous for relatively young patients. During multiple post-operative follow-up visits, we found that the average Harris score of patients within 4 years decreased with the extension of follow-up time, and all failed hip preservation (14/48) underwent hip replacement within 4 years after surgery. However, no more hip preservation failure occurred from 4-year follow-up to the last follow-up in our study, and during this period the Harris score was basically stable (Fig. 5). Since some of the patients in this study had bilateral disease, any lesions on either side may affect pain and motor function score, causing Harris score to be interfered, so we conducted the intra-operative hip joint mobility separately, and evaluated the level of post-operative joint activity by percentage method to reflect the degree of joint matching. The results showed that the level of post-operative hip joint activity was significantly improved (Fig. 5).
Table III.
Baseline and outcomes of the last follow-up
| Variable | Pre-operation (range) | Last follow-up (range) | p values |
|---|---|---|---|
| VAS score | 2.7 ± 0.4 (2.0–3.5) | 1.4 ± 0.92 (0–2.8) | p < 0.001 |
| Hip Harris score | 53.33 ± 8.28 (41–73) | 83.41 ± 6.62 (73–93) | p < 0.001 |
| WOMAC | |||
| Pain | 20.27 ± 4.60 (12.6–27.5) | 10.56 ± 3.99 (5.5–18.4) | p < 0.001 |
| Stiffness | 4.96 ± 2.89 (0–10.0) | 3.29 ± 2.35 (0–8.0) | P = 0.006 |
| Function | 110.97 ± 19.50 (80.0–143.0) | 74.95 ± 19.45 (45.0–120.0) | p < 0.001 |
Except stiffness *p = 0.006, other p<0.001.
Fig. 5.
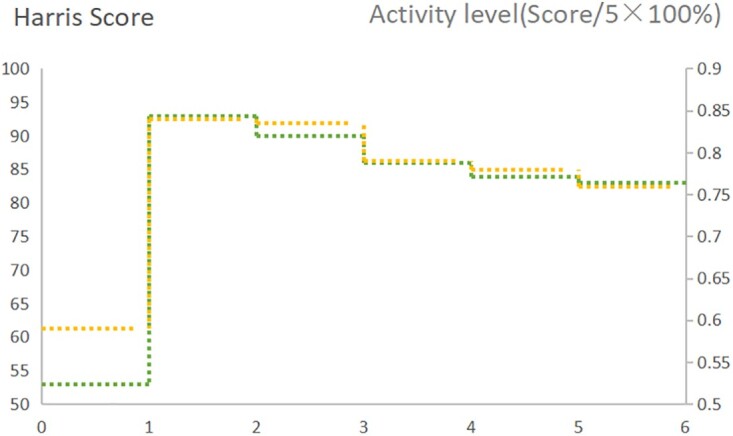
Relationship between Harris score and follow-up time (green-dotted line). Relationship between Harris activity level and follow-up time (yellow-dotted line).
DISCUSSIONS
Postponing or avoiding hip replacement has positive significance in younger patients with femoral head necrosis. At present, it is believed that the femoral head necrosis is difficult to complete the self-repair by two main factors: blood transport disorder and mechanical collapse [18]. Based on this pathophysiological understanding, it is obvious that the main objective of hip preservation surgery should be to restore blood flow in the head and maintain mechanical stability.
In hip preservation operation methods, free vascularized fibular graft is considered to provide good arterial blood supply in the head through anastomosis of vessels while providing support. The clinical efficacy of this surgery had been reported in many literatures, but its efficacy varies greatly among different reports. The reason for this difference may be that the surgical method has higher requirements on the surgical technique and the surgeons’ different understanding of indications. At present, it is relatively certain that the early- and middle-stage femoral head necrosis before collapse may have higher intermediate and long-term success rate [19]. William et al. used vascularized fibular graft in a clinical study on long-term efficacy of femoral head necrosis in the early and middle period before collapse. Among them, 49 of 65 hips (75%) had surviving for at least 10 years. At last follow-up, 39 of 65 hips (60%) had surviving FVFG, with a mean graft survival time of 15 years (range, 10.5–26.1 years). In total, 26 of the 65 hips with FVFG (40%) underwent conversion to THA at a mean of 8 years post-operatively [20]. Another large sample clinical study using a vascularized fibular graft for early to mid-late femoral head necrosis, a total of 407 patients (518 hips) were included. The follow-up ranged from 3 to 10 years with an average of 5.0 years. In comparison with the pre-operative data, the radiographic evaluation showed no changes in 255 patients (331 hips, 57.3%), improvement in 116 patients (195 hips, 33.7%) and progression in 36 patients (52 hips, 9.0%). Among the patients with progression status, 20 patients (23 hips) had THA [21]. In this study, we used the minimally invasive AVFG treating the ARCO Stage II –IIIB patients, for an average follow-up of 6.7 years, the total survival rate reached 70% (34/48).6 of the 14 collapse cases were IIIB stage, to eliminate which the success rate reached 79.5% (31/39). According to the CJFH classification, in addition to the full head necrosis of the L3 type all three cases confirmed failure (which three cases were all ARCO IIIB stage), the overall hip preservation success rate of other types reached 75.5% (34/45). These data above were not inferior to those with vascularized fibula grafts. Therefore, for the advanced femoral head necrosis with incomplete-head type, the avascular allograft fibular transplantation may achieve the same good long-term hip preservation effect as the vascular fibular transplantation, and has the advantages of less trauma, shorter operative time and fewer complications.
In this study, we found that in general, the mid- to long-term success rate of hip preservation by using a vascularized fibular was relatively ideal. The main factor affecting clinical efficacy were choosing suitable indications. According to this study, based on the ARCO stage, the mid- to long-term success rate of hip preservation were IIIA>II >IIIB. The cause of Stage IIIA had a better curative effect than that of II may due to dead bone cleaning scope of this surgery was relatively small and the effectively support area of fibula was limited. In addition, the granule bone grafting may has an advantage for small-scale bone repair. By radiographic follow-up, we found that although the IIIa stage had been a slight collapse under the cartilage, but by clearing the dead bone and pressing the bone graft tightly, the collapse of the cartilage surface can be restored to a certain extent, and long-term stability can be achieved in imaging. Therefore, this surgery can still obtain ideal curative effect for patients which had mild collapse but with relatively small necrosis area. The success rate of hip preservation based on CJFH classification was M > C > L1 > L2 > L3. Necrosis of the lateral column and large area of necrosis were main factors associated with poor prognosis. Three patients of type L3 with extensive femoral head necrosis all had hip replacement within 2 years. We do not recommend this surgery for these patients.
CONCLUSIONS
The AVFG operation can increase the hip function and delay the disease progression. For proper indications and understanding key points, the operation has ideal mid- to long-term clinical effect. At the same time, compared with vascularized fibular graft, this operation is relatively simple and the complications are seldom.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
FUNDING
This study was supported by the National Science Foundation for Young Scientists of China (grant no. 81804117).
CONSENT FOR PUBLICATION
All authors have seen the article and approved it to submit to your journal.
AUTHORS’ CONTRIBUTIONS
P.Y. was responsible for data analysis and article writing. X.L. contributed to data collection and language editing. G.-Q.S., X.-Y.L. and X.W. contributed to the data collection. B.D. was responsible for the study design and correspondence. All authors read and approved the final article.
ACKNOWLEDGMENTS
We want to express our sincere appreciation for all the patients that joined this study.[aQ Please check that funding is recorded in a separate funding section if applicable. Use the full official names of any funding bodies, and include any grant numbers.
CONFLICT OF INTEREST STATEMENT
None declared.
Contributor Information
Peng Yuan, Nanjing University of Chinese Medicine, Nanjing, Jiangsu 210000, China.
Xin Liu, Jiangsu Provincial Hospital of Traditional Chinese Medicine, Nanjing Jiangsu 210000, China.
Bin Du, Jiangsu Provincial Hospital of Traditional Chinese Medicine, Nanjing Jiangsu 210000, China.
Guang-Quan Sun, Jiangsu Provincial Hospital of Traditional Chinese Medicine, Nanjing Jiangsu 210000, China.
Xu Wang, Nanjing University of Chinese Medicine, Nanjing, Jiangsu 210000, China.
Xuan-Ye Lin, Nanjing University of Chinese Medicine, Nanjing, Jiangsu 210000, China.
REFERENCES
- 1. Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 2014; 22: 455–64. [DOI] [PubMed] [Google Scholar]
- 2. Tan B, Li W, Zeng P et al. Epidemiological study based on china osteonecrosis of the femoral head database. Orthop Surg 2021; 13: 153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Papavasiliou Athanasios V, Triantafyllopoulos I, Paxinos O et al. The role of cell therapies and hip arthroscopy in the management of osteonecrosis: an update. J Hip Preserv Surg 2018; 5: 202–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Onggo JR, Nambiar M, Onggo JD et al. Outcome of tantalum rod insertion in the treatment of osteonecrosis of the femoral head with minimum follow-up of 1 year: a meta-analysis and systematic review. J Hip Preserv Surg 2020; 7: 329–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gaudiani MA, Samuel LT, Mahmood B et al. Subchondral insufficiency fractures of the femoral head: systematic review of diagnosis, treatment and outcomes. J Hip Preserv Surg 2020; 7: 85–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tripathy SK, Goyal T, Sen RK. Management of femoral head osteonecrosis: current concepts. Indian J Orthop 2015; 49: 28–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ryan SP, Wooster B, Jiranek W et al. Outcomes of conversion total hip arthroplasty from free vascularized fibular grafting. J Arthroplasty 2019; 34: 88–92. [DOI] [PubMed] [Google Scholar]
- 8. Meloni MC, Hoedemaeker WR, Fornasier V. Failed vascularized fibular graft in treatment of osteonecrosis of the femoral head. A histopathological analysis. Joints 2016; 4: 24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lakshminarayana S, Dhammi IK, Jain AK et al. Outcomes of core decompression with or without nonvascularized fibular grafting in avascular necrosis of femoral head: short term followup study. Indian J Orthop 2019; 53: 420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Soucacos PN, Beris AE, Malizos K et al. Treatment of avascular necrosis of the femoral head with vascularized fibular transplant. Clin Orthop Relat Res 2001; 386: 120–30. [DOI] [PubMed] [Google Scholar]
- 11. Tetik C, Başar H, Bezer M et al. Comparison of early results of vascularized and non-vascularized fibular grafting in the treatment of osteonecrosis of the femoral head. Acta Orthop Traumatol Turc 2011; 45: 326–34. [DOI] [PubMed] [Google Scholar]
- 12. Jie K, Feng W, Li F et al. Long-term survival and clinical outcomes of non-vascularized autologous and allogeneic fibular grafts are comparable for treating osteonecrosis of the femoral head. J Orthop Surg Res 2021; 16: 109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Changjun C, Donghai L, Xin Z et al. Mid- to long-term results of modified non-vascularized allogeneic fibula grafting combined with core decompression and bone grafting for early femoral head necrosis. J Orthop Surg Res 2020; 15: 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Keizer SB, Kock NB, Dijkstra PD et al. Treatment of avascular necrosis of the hip by a non-vascularised cortical graft. J Bone Joint Surg Br 2006; 88: 460–6. [DOI] [PubMed] [Google Scholar]
- 15. Zhao D, Zhang F, Wang B et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version). J Orthop Translat 2020; 21: 100–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yoon BH, Mont MA, Koo KH et al. The 2019 revised version of association research circulation osseous staging system of osteonecrosis of the femoral head. J Arthroplasty 2020; 35: 933–40. [DOI] [PubMed] [Google Scholar]
- 17. Xia T, Wei W, Zhang C et al. Hip preservation experience of avascular necrosis of femoral head according to China-Japan Friendship Hospital classification. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2020; 34:10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Calori GM, Mazza E, Colombo A et al. Core decompression and biotechnologies in the treatment of avascular necrosis of the femoral head. EFORT Open Rev 2017; 2: 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fang T, Zhang EW, Sailes FC et al. Vascularized fibular grafts in patients with avascular necrosis of femoral head: a systematic review and meta-analysis. Arch Orthop Trauma Surg 2013; 133:1–10. [DOI] [PubMed] [Google Scholar]
- 20. Eward WC 1, Rineer CA, Urbaniak JR et al. The vascularized fibular graft in precollapse osteonecrosis-is long-term hip preservation possible? Clin Orthop Relat Res 2012; 470: 2819–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gao YS, Chen SB, Jin DX et al. Modified surgical techniques of free vascularized fibular grafting for treatment of the osteonecrosis of femoral head: results from a series of 407 cases. Microsurgery 2013; 33: 646–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.