Abstract
Background & aims
Concomitantly to the coronavirus disease 2019 (COVID-19), in the child population there was already another pandemic wave in progress: childhood obesity. Numerous studies in adults have been carried out and describe obesity as an independent risk and prognostic factor for the severity of COVID-19. This study aims to systematically review the literature on the relation between weight excess and the severity of COVID-19 in children and adolescents.
Methods
This systematic review was developed following the PRISMA standards (Preferred Reporting Items for Systematic Review and Meta-Analysis). The literature search was performed in September 2020, in the following databases: MEDLINE (via PubMed), Embase, Scopus, The Cochrane Library (Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials (CENTRAL)), Web of Science, BVS/LILACS and SciELO. Registration on the PROSPERO platform (International Prospective Registry of Systematic Reviews) can be found under the registration number: CRD42021230686.
Results
Of the 667 selected articles, 11 were included according to all agreed criteria, most of them being unicentric and American. In assessing the risk of bias and quality, following the criteria of the Newcastle–Ottawa Scale, eight studies achieved scores higher than 7. Only 5 studies sought to assess obesity and its relation with worse outcomes (such as need for pediatric intensive care unit (PICU), mechanical ventilation (MV), tracheostomy, hospital readmission and mortality), and out of these, only one article demonstrated this comorbidity as a prognostic factor for worse evolution of the COVID picture.
Conclusions
Few studies in the literature seek to assess excess weight and its relation with worse outcomes of COVID-19 in children and adolescents. Taking into account that there is already scientific evidence on this subject in adult patients, it is necessary to carry out more research in the pediatric age group.
Keywords: COVID-19, Corona virus, Child obesity, Overweight, Pediatric intensive care unit
1. Introduction
Although most children with COVID-19 experience mild illness, the spectrum of this disease is wide, and some children develop serious illness that leads to hospitalization, use of invasive mechanical ventilation and death [[1], [2], [3], [4], [5]]. Patients admitted to Pediatric Intensive Care Units (PICU) with COVID-19 may clinically manifest as Severe Acute Respiratory Syndrome (SRAG), not SRAG and Multisystem Inflammatory Syndrome in Children MIS-C [[6], [7], [8]].
COVID-19 is one of the leading causes of death, with incidence exceeding diabetes and other Diet-Related Non-Communicable Diseases (NCDs) [9]. Concomitant to COVID-19 pandemic, there was already another pandemic wave: childhood obesity [10]. Worldwide, the prevalence of weight excess (overweight and obesity) among people aged 5–19 years old reached more than 18% in 2016, totaling more than 340 million. In 2020, around 39 million children under 5 years of age were overweight [11].
Studies that have been available so far point to a relevant scientific evidence that excess weight is a risk factor for the development of severe forms of COVID-19 in adults [[12], [13], [14], [15], [16], [17], [18]]. The mechanisms that explain this relation are possibly attributed to a decrease in lung function, changes in the microbiota, increase in pro-inflammatory substances and changes in the immune response [19]. It seems essential to systematically evaluate whether weight excess in children and adolescents is a risk factor for the severity of COVID-19 with the data currently available. Understanding factors associated with severe COVID-19 disease in pediatrics could help inform prevention, control strategies.
2. Materials and methods
2.1. Search strategy and study selection criteria
This study is a systematic review, which had its project registered in the PROSPERO platform (International Prospective Registry of Systematic Reviews), under the registration number: CRD42021230686 [20]. A systematic search of studies was carried out in September 2020, in the following databases: MEDLINE (via PubMed), Embase, Scopus, The Cochrane Library (Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials (CENTRAL)), Web of Science, BVS/LILACS and SciELO. Date of publications was not limited/filtered. Search terms were determined through the MESH database, relevant systematic reviews, and meta-analysis. The final keywords were: ‘Child’ OR ‘Adolescent’ OR ‘Infant’ OR ‘Teen’ OR ‘Youth’ OR 'Pediatrics' OR ‘Pediatric’ OR ‘Paediatric’ OR ‘Baby’ OR 'Babies' OR ‘Toddler’ AND ‘Overweight’ OR ‘Obesity’ AND ‘2019-nCoV′ OR ‘COVID-19′ OR ‘SARS-CoV-2′ OR ′ (Wuhan AND coronavirus)'. Only a language filter was used, limiting it to English, Spanish and Portuguese.
The eligibility criteria were established following the PICOS principles (P: Participants; I: Intervention/Exposure; C: Comparison; O: Outcomes; S: Study Design). The study had to contain child and/or adolescent patients (from one month to 18 years old) with clinically or laboratory confirmed SARS-CoV-2 infection. Studies that mostly have a population that do not concern this review were excluded, such as patients with other viral infections, non-hospitalized patients, newborns and pregnant women.
Only original studies and full-text article citations were included. Meanwhile, studies in animal models or in vitro conditions, based on statistical simulation or use of artificial samples, studies evaluating adults only, as well as systematic reviews, experimental studies, letters to the editor, comments, editorials and case reports, were excluded. To avoid double-reporting of results, secondary publications such as metaanalyses and systematic literature reviews were not eligible for inclusion; however, the search terms included meta-analyses and systematic literature reviews to facilitate screening of references for the purpose of identifying potentially eligible primary publications that were not retrieved in the literature search.
2.2. Data selection
The references found in the databases were exported to the Mendeley platform to remove duplicate references and then to Rayyan for a first evaluation of titles, authors, research type and abstracts. Rayyan is a free web and mobile application designed to help expedite the initial screening of abstracts and titles using a process of semi-automation while incorporating a high level of usability [21]. Two reviewers independently selected articles that met the inclusion criteria, and a third reviewer resolved disagreements independently. Citations that did not meet the inclusion criteria described above were excluded.
2.3. Assessment of risk of bias
Two investigators independently assessed the quality of included studies according to the Newcastle–Ottawa Scale (NOS) [22]. All disagreements were resolved by consensus. High-quality studies were defined as studies that met a NOS score of at least 7.
2.4. Data extration
After the first phase of study selection, the articles were completely read, and two independent and blind reviewers (as for the evaluation of the other reviewer) evaluated them again individually, this time in full. At this point, a standardized data collection form was created, in which both reviewers fed information from each article studied. The following data were extracted from each eligible article: first author; publication date; countries; study design; gender; age; anthropometric data and different nutritional status classifications; exposure and comparators - the number of patients with weight excess; the number of patients without weight excess; mortality and severity of disease from each group; number of patients of each group that had PICU requirement, mechanical ventilation support required (and duration), extracorporeal membrane oxygenation requirement, length of hospital stay, length of PICU stay, and acute respiratory distress syndrome.
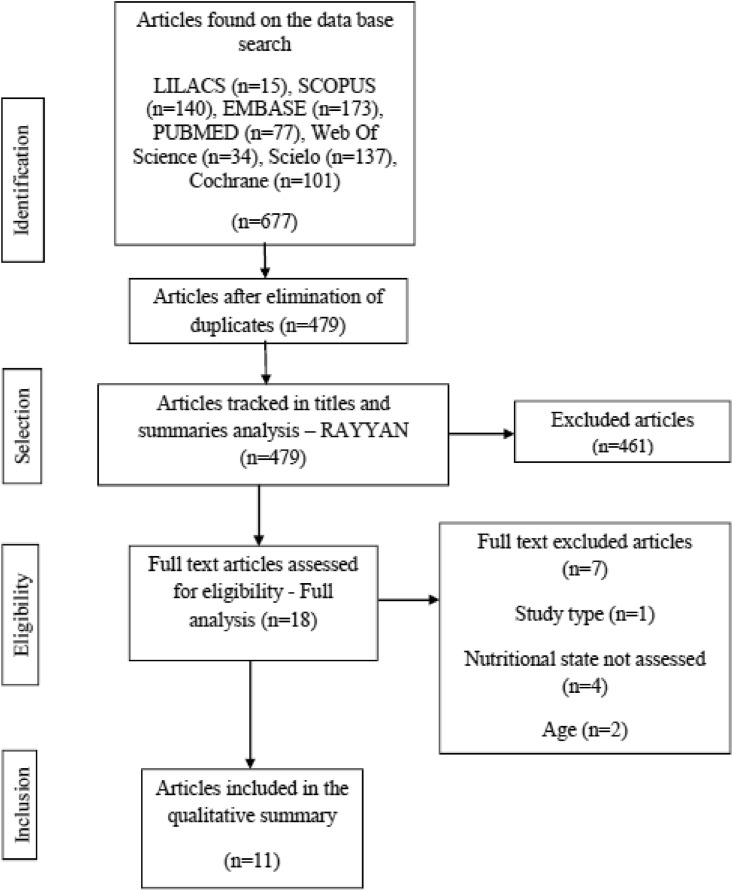
Three authors met after filling in all article data by the first two reviewers, and the discrepancies in opinions and understandings were resolved by discussion until consensus. None of the authors were blind to journal titles, authors, or study institutions. The study selection process is presented according to the flowchart suggested by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [23].
2.5. Data synthesis and statistical analysis
Two researchers analyzed and grouped data and the tabulation was performed in consensus. There was a lot of missing desired data, so an email was sent to the authors of the 18 selected articles for complete reading of the texts requesting more information. From these e-mails, we only received responses from six authors, but no further data were added. After all the tabulation, the third researcher finally revised the data.
2.6. Ethics
As this is a systematic review, using scientific articles available on the platforms, that is, without personal identification of the patient, the analysis and approval of the ethics committee were not necessary.
3. Results
3.1. Literature search
According to the eligibility strategies, 677 studies were selected in the initial research in seven different databases. After removal of duplicate citations, screening of the remaining titles and abstracts yielded a total of 479 potentially relevant articles. The PRISMA flow diagram shows the process of study selection (Fig. 1 ). At this stage, carried out on the Rayyan platform, and following the inclusion and exclusion criteria, only 18 works were left to be read in full. Evaluating the works in more detail, in the eligibility phase, 7 were excluded (the reasons for exclusion are summarised in Fig. 1).
Fig. 1.
Information flowchart of different stages of the systematic review.
3.2. General characteristics of the included studies
Eleven relevant articles were included in this review, of which 6 are retrospective cohorts, 4 case series and one control case. All studies are from 2020. Among the 11, most of them are unicentric and American. From all the studies, two ([24,25]) had a wide age range, which included many adults, but there were segmented data on children and adolescents, making it possible to collect data separately. It is noteworthy that none of the works focused on nutritional status, but 5 of them searched for relation between weight excess and severe COVID-19. Most presented an overview of COVID cases in pediatrics, and among some of the aspects evaluated, weight excess was included. Table 1 includes the summary of the included studies.
Table 1.
Summary of the studies included and their main data.
| Article | Study type | Total sample/Valid patients | Centers number/Location | Nutritional state – Criterion | Age (IQR, medium age) | Weight excess | PICU Necessity | Assessed outcomes | Searched for relation between weight excess and severe COVID-19 ∗ |
|---|---|---|---|---|---|---|---|---|---|
| Zahra Belhadjer et al. [30] | Retrospective cohort | 35/31 | 12 -France; 1 - Switzerland | Obesity = overweight = BMI >25 | 2-16 y; 10 y | 6 (17%) | 82,85% | MIS-C, ECMO, PICU, Mortality | |
| Philip Zachariah et al. [26] | Case series | 50/50 | 1- New York (USA) | Overweight p85-95/Obesity > p95 (CDC) | 6 d-21 y; NA | Total obesity 22%/Overweight 16% | NA | MV, ECMO, Mortality | ∗ |
| Jerry Y Chao et al. [27] | Retrospective cohort | 67/46 | 1- New York (USA) | Obesity = BMI >30 | 0.4–19.3 y; 13.1 y | 14 (30.4%) | 13 (28,3%) | ARDS, PICU, MV, Mortality | ∗ |
| Nadia Nathan et al. [37] | Retrospective cohort | 23/23 | 1 - France | BMI Z score | 0.1–17.6 y; 4.9 y | Obesity/Overweight 3 (13%) | 5/21 (24%) | Mortality, PICU, ARDS, MIS-C, MV | |
| William R. Otto et al. [32] | Retrospective cohort series | 7256/77 | NA - USA | NA | 1.1y-15.4 y; 9.9 y | 55/424 (13%) | 25/77 (32.9%) | Mortality, PICU, ARDS, MIS-C, MV, ECMO | |
| Yanli Wang et al. [24] | Retrospective control–case | 260/43 | 1 - China | BMI | 0.97y–13.83 y; 6.9 y | 18 average BMI | NA | MV, Mortality | ∗ |
| Sthepanie Lovinsky-Desir et al. [28] | Retrospective cohort | 1298/55 | 3 - New York (USA) | BMI >30 | Mean age 14 y between <21 y | 10/55 (18%) | NA | MV, Mortality | ∗ |
| Christine A. Capone et al. [38] | Case series | 33/33 | 1- New York (USA) | Overweight p85-95/Obesity p > 95 | 5.5 y-12.6 y; 8.6 y | Obesity 13 (39%)/Overweight 2 (6%) | 26/33 (79%) | MV, Mortality, MIS-C, PICU | |
| Roberta L. DeBiasi et al. [29] | Retrospective cohort | 177/44 | 1 - Washington (USA) | NA - Banco de dados | 0.1y-25.6 y; 9.6 y | 1/44 (2%) | 9/44 (20.4%) | Mortality, MV, MIS-C, PICU, ARDS | ∗ |
| Safiya Richardson et al. [25] | Case series | 5700/50 | 12 - New York (USA) | Obesity (BMI > or equal to 30)/Morbid (BMI > or equal to 35) | 0-10.7 y; 6.3 y | 1737/4170–41.7% | 7/46 (12.2%) | PICU, MV, Mortality | |
| Einat Blumfield et al. [33] | Retrospective cohort | 19/19 | 1 - New York (USA) | NA | 2 m-18 y; 8 y | 3 (15.8%) | 14/19 (73.7%) | Mortality, ARDS, MV, MIS-C, PICU |
Caption: IQR - Interquartile range; MIS-C - Multisystem inflammatory syndrome in children; ECMO - Extracorporeal membrane oxygenation; BMI - Body mass index; PICU - Pediatric intensive care unit; NA - Not available; USA–United States of America; CDC - Center for Disease Control; MV - Mechanical ventilation; ARDS - Acute Respiratory Distress Syndrome.
3.3. Quality and risk of bias assessment
In the assessment of risk of bias and quality of studies performed following the criteria of the Newcastle–Ottawa Scale, three of those included did not meet the quality criteria, reaching scores lower than 7, as shown in Table 2 . Nonetheless, these were included in the review as we consider that they contributed as evidence to the discussions about the studied topic.
Table 2.
Criteria of quality and risk of bias according to the Newcastle–Ottawa Scale.
| Study | Selection |
Comparability |
Outcome |
TOTAL |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness | Selection of non-exposed cohort | Ascertainment | Outcome demonstration | Comparability | Outcome Assessment | Follow-up length | Follow-up adequacy | ||
| Zahra Belhadjer et al. [30] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Philip Zachariah et al. [26] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Jerry Y Chao et al. [27] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Nadia Nathan et al. [37] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| William R. Otto et al. [32] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
| Yanli Wang et al. [24] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 6 | ||
| Sthepanie Lovinsky-Desir et al. [28] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Christine A. Capone et al. [38] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 6 | ||
| Roberta L. DeBiasi et al. [29] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 8 |
| Safiya Richardson et al. [25] | ☆ | ☆ | ☆ | ☆ | 4 | ||||
| Einat Blumfield et al. [33] | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | 7 | |
4. Discussion
After this extensive literature search, only 11 articles were selected. It highlights the difference in the supply of studies on COVID in pediatrics when compared to adults. Furthermore, the topic of nutritional assessment in children is an additional hurdle. Assessing the nutritional status of hospitalized patients by itself is already challenging, and this situation is even more complex when it comes to critically ill children. There are numerous ways to evaluate nutritionally pediatric patients. The most common is the classification guided by WHO. The studies included in this review did not have nutritional focus, therefore, most of the data regarding weight and BMI were from the collection of information from medical records, which can difficult the analysis. Another relevant information is that many studies included a wide range of age groups and the obesity criteria for each one were not always clarified.
Obesity and overweight varied from 13 to 39% and 6–16%, respectively. In the paper that included adults [24], obesity reached 41% of those studied, demonstrating a wide variation in the prevalence of this comorbidity. Among all studies, five [24,[26], [27], [28], [29]] sought to assess obesity and its relation with worse outcomes (such as need for PICU, MV, tracheostomy, hospital readmission and mortality). Of these, only one [26] found significant statistical evidence to describe this comorbidity as a prognostic factor for worse developments in COVID. This study considered as obese patients with a percentile above p95, with a total of 22% obese and 16% overweight. Weight excess was found among 20% of non-serious patients and 67% of severe cases, with a statistically significant difference in isolation.
In terms of severity of COVID-19 criteria there was great heterogeneity. The data that stood out the most as criteria for severity was the need for the PICU (12.2%–82.8% - corresponding to references 23 and 24) and need for ventilatory support (10–89% - corresponding to references [27,29]), due to a wide range of findings. This disparity in percentages may occur because many studies have compared patients with mild symptoms (and even those who are not hospitalized) to severe conditions, and also, some studies only presented severe cases of COVID-19 [30,31], increasing the severity data described. Even so, in most studies, mortality was null, with few exceptions ranging from 2.6% [32] to 10.5% [33].
Other serious situations reported were septic shock, need for orotracheal intubation, ARDS, vasopressor support, renal and/or liver failure, myocardial dysfunction, readmission to hospital or PICU and need for tracheostomy. Most studies did not describe how many patients developed ARDS, but among those that reported, there was a wide range from 1.3% [28] to 76.9% [27]. The incidence of MISC cases was 15% [32] to 100% [24,30]. The need for ECMO was not mentioned in 8 studies, while two studies brought this support in 2 and 2,6% of cases (respectively to references 25 and 28) and another one, with 28% [24] of use of this therapy. Not coincidentally, the study with the highest rate of ECMO (and 100% of MISC) addresses more deeply the cardiological aspects of severe COVID.
The length of hospital stay was widely discussed in most of the studies, and its average was 3–4 days. The hospitalization length in the studies ranged from 1 day [25] to 11 days [22], but there were reports of up to 30 days [25] or followed up after completion of the studies. The length of stay in the PICU was not described in 8 studies, with two having an average of 7 days [24,26] and one an average of 13 days [22]. These data corroborate the literature: cases of COVID-19, in pediatrics are usually milder than in adults, since studies with a higher mean of hospitalization are those that encompassed other age groups besides the one studied.
The higher risk tendency in obese population has been explained by several mechanisms, such as immune dysfunction, altered pulmonary physiology, and high angiotensin converting enzyme 2 (ACE2) expression [34]. Systemic inflammation, immune system impairment, sarcopenia, and preexisting associated conditions, such as respiratory, cardiovascular, and metabolic diseases related to obesity, could act as crucial factors linking nutritional status and the course and outcome of COVID19 [19]. Considering the risk of obesity, obese children with COVID-19 need close monitoring for clinical deterioration or progression to acute respiratory distress syndrome. Additionally, in obese children, lifestyle habit control and prevention through COVID-19 vaccination were emphasized.
4.1. Strengths and limitations
In 2021, COVID and chronic non-communicable diseases together total the main causes of death in the world [8]. The focus of this study was precisely to investigate whether excess weight (which causes many chronic diseases) can aggravate COVID-19 - this pandemic that has apparently intensified obesity itself, by increasing vulnerabilities and disparities in life behaviors, perpetuating a synergy of complex nutritional conditions [8]. Although some studies on risk factors for poor prognosis in children and adolescents with COVID-19 exist, to our knowledge, this is the first systematic review that focus to assess overweight as a prognostic factor for COVID in pediatrics.
The influence of weight excess on the severity of children undergoing hospitalization is still not well understood [35,36]. In our study, the challenge of assessing excess weight in critically ill pediatric patients is reinforced. An important point to be raised is whether this relation was not found by temporality, considering that the number of critically ill children with COVID-19 is significantly lower than adults, as well as the prevalence of weight excess in the age group.
Regarding the methodology, the present study has the only limitation of having used the language filter. Although most scientific publications are presented in English regardless of the place of origin, maybe other points could be raised by different cultural and epidemiological analysis, because there was a lack of studies that better represent world diversity, especially regarding the prevalence of overweight. In addition, it is worth emphasizing that COVID-19 is very recent and the number of new scientific works published daily is significant. This systematic review did not find articles specifically deepened on the research topic, making meta-analysis impossible, which is also due to the heterogeneity of the data.
5. Conclusion
Our systematic review was unable to reach a more robust conclusion because only five studies sought to assess obesity and its relationship with worse outcomes of COVID-19 in children and adolescents (such as the need for PICU, MV, tracheostomy, hospital readmission, and mortality). Yet one found significant statistical evidence to describe this comorbidity as a prognostic factor for worse developments in COVID. Overweight was found among 20% of non-serious patients and 67% of severe cases.
It is very plausible that this relation will be confirmed as soon as more studies on the subject are published, leading to the numerous known mechanisms that already associate obesity with worse outcomes in other circumstances. Confirmation of this hypothesis could guide pediatric decision-making, providing opportunities for stratification of patients according to their risk and supporting optimized management strategies and use of resources to provide care to critically ill patients, as well as encouraging the priority of vaccination as a risk group, as it is with adult patients.
Authorship - CRediT author statement
MLOSK: Conceptualization, Methodology, Software, Formal analysis, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing, Visualization, Validation. GRHA: Conceptualization, Software, Validation, Formal analysis, Investigation, Resources, Writing - Review & Editing. CADC: Conceptualization, Methodology, Validation, Resources, Writing - Review & Editing, Supervision. FC: Conceptualization, Validation, Data Curation, Writing - Review & Editing, Project administration, Funding acquisition. PCRG: Conceptualization, Formal analysis, Writing - Review & Editing, Validation, Data Curation, Supervision.
Funding sources
This study was financed in part by the Higher Education Improvement Coordination (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil - CAPES) - Finance Code 001.
Declaration of competing interest
None to be declared.
Acknowledgements
This research was supported by the Higher Education Improvement Coordination (CAPES), Brazil.
References
- 1.Kim L., Whitaker M., O'Halloran A., Kambhampati A., Chai S.J., Reingold A., et al. Hospitalization rates and characteristics of children aged <18 Years hospitalized with laboratory-confirmed COVID-19 - COVID-NET, 14 States, March 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020 Aug;69(32):1081–1088. doi: 10.15585/mmwr.mm6932e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Preston L.E., Chevinsky J.R., Kompaniyets L., Lavery A.M., Kimball A., Boehmer T.K., et al. Characteristics and disease severity of US children and adolescents diagnosed with COVID-19. JAMA Netw Open. 2021;4(4):16–19. doi: 10.1001/jamanetworkopen.2021.5298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aramburu A. vol. 16. 2020. (Exceso de peso como factor pronóstico en pacientes con COVID-19. Ser Revis RÁPIDAS - Inst Nac SALUD - Unidad Análisis y Generación Evidencias en Salud Pública). [Google Scholar]
- 4.WHO . 2020. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. [Google Scholar]
- 5.Badal Sujan, Thapa Bajgain Kalpana, Badal Sujeena, Thapa Rama, Bishnu B., Bajgain M.J.S. Prevalence, clinical characteristics, and outcomes of pediatric COVID-19: a systematic review and meta-analysis. J Clin Virol. 2021;135 doi: 10.1016/j.jcv.2020.104715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sáfadi M.A., Kfouri R. de Á. 2021. Nota técnica - Dados Epidemiológicos da COVID-19 em Pediatria. Dep Científico Imunizações e Dep Científico Infectol • Soc Bras Pediatr. [Google Scholar]
- 7.Feldstein L.R., Tenforde M.W., Friedman K.G., Newhams M., Rose E.B., Dapul H., et al. Characteristics and outcomes of US children and adolescents with Multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. Jama. 2021:1–14. doi: 10.1001/jama.2021.2091. http://www.ncbi.nlm.nih.gov/pubmed/33625505 [Internet] Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nehab M.F., Meirelles A.F.V., Chaves C.R.M.M., Pereira C.D., Pacheco C.A.M.S., Britto J.A.A., et al. Inst Nac Saúde da Mulh da Criança e do Adolesc Fernandes Figueira; 2020. COVID-19 e Saúde da Criança e do Adolescente. [Google Scholar]
- 9.Huizar M.I., Arena R., Laddu D.R. The global food syndemic: the impact of food insecurity, Malnutrition and obesity on the healthspan amid the COVID-19 pandemic. Prog Cardiovasc Dis. 2021;64:105–107. doi: 10.1016/j.pcad.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pediatria SB de. Manual de Orientação - Obesidade na infância e adolescência. Manual De Metodologia Da Pesquisa Aplicada À Educação. 2019:1–56. [Google Scholar]
- 11.United Nations Children’s Fund (UNICEF) Geneva World Heal Organ; 2021. World Health Organization IB for R and DWB. Levels and trends in child malnutrition: key findings of the 2021 edition of the joint child malnutrition estimates. [Google Scholar]
- 12.Tamara A., Tahapary D.L. vol. 14. Clinical Research and Reviews; 2020. Obesity as a predictor for a poor prognosis of COVID-19: a systematic review; pp. 655–659. (Diabetes and metabolic syndrome). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Salud PM de S.I.N. 2020. Exceso de peso como factor pronóstico en pacientes con COVID-19 TT - excess weight as a prognostic factor in patients with COVID-19.https://fi-admin.bvsalud.org/document/view/85p7w [Internet] Available from: [Google Scholar]
- 14.Huang Y., Lu Y., Huang Y.M., Wang M., Ling W., Sui Y., et al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metab Clin Exp. 2020;113 doi: 10.1016/j.metabol.2020.154378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kompaniyets L., Goodman A.B., Belay B., Freedman D.S., Sucosky M.S., Lange S.J., et al. Body mass index and risk for COVID-19–related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death — United States, March–December 2020. MMWR Surveill Summ. 2021;70(10):355–361. doi: 10.15585/mmwr.mm7010e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussain A., Mahawar K., Xia Z., Yang W., El-hasani S. 2020. Obesity and mortality of COVID-19. Meta-analysis. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Földi M., Farkas N., Kiss S., Zádori N., Váncsa S., Szakó L., et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: a systematic review and meta-analysis. Obes Rev. 2020;(June):1–9. doi: 10.1111/obr.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicolau J., Ayala L., Sanchís P., Dotres K., Masmiquel L., Soler A., et al. Clin Nutr ESPEN J; 2021. Influence of nutritional status on clinical outcomes among hospitalized patients with COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fedele D., De Francesco A., Riso S., Collo A. vol. 81. Nutrition; 2021. p. 111016. (Obesity, malnutrition, and trace element deficiency in the coronavirus disease (COVID-19) pandemic: an overview). [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oliveira da Silva Kist Mayara Luí¬za, Drumond Costa Caroline Abud, Garcia Pedro Celiny Ramos, Francielly Crestani G.A. PROSPERO - Int Prospect Regist Syst Rev; 2021. Weight excess association with severity in children and adolescents with COVID-19 : a systematic review; pp. 1–6.https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021230686 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10. doi: 10.1186/s13643-016-0384-4. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NEWCASTLE - OTTAWA QUALITY ASSESSMENT SCALE - CASE CONTROL STUDIES. NOS [Internet]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp,
- 23.Moher D., Liberati A., Tetzlaff J., Altman D.G.T.P.G. Preferred reporting Items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y., Zhu F., Wang C., Wu J., Liu J., Chen X., et al. Pediatr Infect Dis J; 2020. Children hospitalized with severe COVID-19 in Wuhan.https://www.cochranelibrary.com/central/doi/10.1002/central/CN-02123498/full [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 25.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA, J Am Med Assoc. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85084133173&doi=10.1001%2Fjama.2020.6775&partnerID=40&md5=e752964877871064c09709317dd7c20f [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zachariah P., Johnson C.L., Halabi K.C., Ahn D., Sen A.I., Fischer A., et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a Children's hospital in New York city, New York. JAMA Pediatr. 2020 Jun doi: 10.1001/jamapediatrics.2020.2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chao J.Y., Derespina K.R., Herold B.C., Goldman D.L., Aldrich M., Weingarten J., et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a tertiary care medical center in New York city. J Pediatr. 2020 Aug;223:14–19.e2. doi: 10.1016/j.jpeds.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lovinsky-Desir S., Deshpande D.R., De A., Murray L., Stingone J.A., Chan A., et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146(5):1027–1034. doi: 10.1016/j.jaci.2020.07.026. https://www.embase.com/search/results?subaction=viewrecord&id=L2007573402&from=export [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeBiasi R.L., Song X., Delaney M., Bell M., Smith K., Pershad J., et al. Severe coronavirus disease-2019 in children and young adults in the Washington, DC. Metropolitan Region. J Pediatr. 2020;vol. 223:199–203. doi: 10.1016/j.jpeds.2020.05.007. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85085326648&doi=10.1016%2Fj.jpeds.2020.05.007&partnerID=40&md5=c6e39e142b0897ae5ff0537fda97a805 [Internet] e1. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Belhadjer Z., Méot M., Bajolle F., Khraiche D., Legendre A., Abakka S., et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation. 2020 May;142(5) doi: 10.1161/CIRCULATIONAHA.120.048360. [DOI] [PubMed] [Google Scholar]
- 31.Capone C.A., Subramony A., Sweberg T., Schneider J., Shah S., Rubin L., et al. Northwell Health COVID-19 Research Consortium Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. 2020;224:141–145. doi: 10.1016/j.jpeds.2020.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Otto W.R., Geoghegan S., Posch L.C., Bell L.M., Coffin S.E., Sammons J.S., et al. The epidemiology of severe acute respiratory syndrome coronavirus 2 in a pediatric healthcare network in the United States. J Pediatric Infect Dis Soc. 2020;1–7 doi: 10.1093/jpids/piaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blumfield E., Levin T.L. COVID-19 in pediatric patients: a case series from the Bronx, NY. Pediatr Radiol. 2020 Sep;50(10):1369–1374. doi: 10.1007/s00247-020-04782-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou Y., Chi J., Lv W., Wang Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (Covid-19) Diabetes Metab Res Rev. 2021;37(2) doi: 10.1002/dmrr.3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Costa C.A.D., Mattiello R., Forte G.C., Andrades G.R.H., Crestani F., Dalenogare I.P., et al. Clinical outcomes in critically ill children with excess weight: a retrospective cohort study. Nutr Clin Pract. 2021;36(2):449–455. doi: 10.1002/ncp.10541. [DOI] [PubMed] [Google Scholar]
- 36.Alipoor E., Hosseinzadeh-Attar M.J., Yaseri M., Maghsoudi-Nasab S., Jazayeri S. Association of obesity with morbidity and mortality in critically ill children: a systematic review and meta-analysis of observational studies. Int J Obes. 2019;43(4):641–651. doi: 10.1038/s41366-019-0319-y. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 37.Nathan N., Prevost B., Sileo C., Richard N., Berdah L., Thouvenin G., et al. The wide spectrum of COVID-19 clinical presentation in children. J Clin Med. 2020 Sep;9(9) doi: 10.3390/jcm9092950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Capone C.A., Subramony A., Sweberg T., Schneider J., Shah S., Rubin L., et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. 2020;224:141–145. doi: 10.1016/j.jpeds.2020.06.044. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85089538276&doi=10.1016%2Fj.jpeds.2020.06.044&partnerID=40&md5=20a9167f66ee19ac5f05d03a7d47b065 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]