Abstract
A systematic literature review was completed to identify all peer-reviewed literature quantifying the association between short-term exposures of particulate matter < 2.5 microns (PM2.5), nitrogen dioxide (NO2), and sulfur dioxide (SO2) and COPD-related emergency department (ED) visits, hospital admissions (HA), and mortality. These results were then synthesized for each pollutant through meta-analyses with a random effects model. Sub-group meta-analyses were explored to study the impacts of selected lag/averaging times and health outcomes. A total of 37 studies satisfied our inclusion criteria, contributing a total of approximately 1,115,000 COPD-related acute events (950,000 HAs, 80,000 EDs, and 130,000 deaths) to our meta-estimates. A 10 ug/m3 increase in PM2.5 was associated with a 2.5% (95% CI: 1.6%–3.4%) increased risk of COPD-related ED and HA, a 10 ug/m3 increase in NO2 was associated with a 4.2% (2.5%–6.0%) increase, and a 10 ug/m3 increase in SO2 was associated with a 2.1% (0.7%–3.5%) increase. The strength of these pooled effect estimates, however, varied depending on the selected lag/averaging time between exposure and outcome. Similar pooled effects were estimated for each pollutant and COPD-related mortality. These results suggest an ongoing threat to the health of COPD patients from both outdoor particulates and gaseous pollutants. Ambient outdoor concentrations of PM2.5, NO2, and SO2 were significantly and positively associated with both COPD-related morbidity and mortality.
Keywords: environmental health, environmental epidemiology, air pollution, respiratory disease
Introduction
Chronic obstructive pulmonary disease (COPD), characterized by progressive irreversible airflow limitation and chronic inflammation of the lungs, is an increasingly prevalent disease in both developed and developing countries[1] and currently the fourth leading cause of death globally[2,3]. The disease represents an important economic burden for individual patients and healthcare systems [4], with estimated direct costs of $29.5 billion and indirect costs of $20.4 billion in the United States [1]. These costs are largely due to exacerbation of COPD, which in severe cases can result in emergency department (ED) visits, hospital admissions (HA), and death [5]. One potential trigger for such exacerbations is short-term exposures to outdoor air pollution [1]. In the past two decades, numerous epidemiologic studies have investigated the short-term effects of outdoor air pollution on this sensitive population by studying COPD-related morbidity (as ED and HA) and mortality [6]. Most of these studies report significant positive associations for exposures to particulate matter (PM), with conflicting evidence for the other USEPA criteria gaseous air pollutants, including nitrogen dioxide (NO2) and sulfur dioxide (SO2)[6].
Although meta-analysis [7] has been widely used to combine study results quantifying the association between short-term exposures to outdoor air pollution and overall respiratory disease related ED-HA and mortality, only four have estimated pooled effects among COPD patients [8–11]. Two of these looked specifically at PM10 exposures [8,9] and one focused solely on studies completed in China [10]. There has yet to be a systematic review of all existing literature and meta-analysis for two pollutants currently of great public health concern – NO2 and SO2. The lack of pooled risk estimates for these gaseous pollutants limits the ability to fully understand the impact that outdoor air pollution may have on COPD patients. In this study, a systematic literature review and meta-analysis were carried out to synthesize risk estimates for COPD-related morbidity and mortality outcomes due to short term exposures (up to a maximum of 7 days) to PM2.5, SO2 and NO2. Sub-group analyses were used to evaluate the implications that selected lag/averaging times between exposure and outcome had on pooled effect estimates, as well as to study differences in pooled effect estimates for various acute COPD-related outcomes.
Methods
Search Strategy
A comprehensive systematic literature review [12] was conducted in PubMed and Medline databases to identify relevant peer-reviewed articles. The following Medical Subject Heading (MeSH) criteria [13] were used in PubMed: (“Pulmonary Disease, Chronic Obstructive/ epidemiology”[Mesh]) AND ((“Air Pollution/adverse effects”[Mesh]) OR (“Air Pollutants/adverse effects”[Mesh]) OR (“Sulfur Dioxide”[Mesh]) OR (“Nitrogen Dioxide”[Mesh]) OR (“Particulate Matter”[Mesh])). The following key word criteria were used in Medline; (“Air Pollution” OR “Sulfur Dioxide” OR “Nitrogen Dioxide” OR “Particulate Matter”) AND (COPD OR “Chronic Obstructive Pulmonary Disease”) AND (Hospital* OR Emergency OR Mortality). Additional filters were added to both search strings and databases to limit results to studies published in English between the years 1995 and 2015. In addition, the titles of all references from all eligible studies captured in the PubMed/Medline searches, as well as those referenced in USEPA Integrated Science Assessment (ISA) documents for each pollutant [14–16], were reviewed.
Titles and abstracts for all identified articles were screened by two researchers (RD and DK). Any study that investigated the association between short-term outdoor air pollution exposures and COPD-related ED, HA, or mortality was retained for full text review. Of these studies eligible for full text review, any study which provided quantitative estimates for the association between short-term exposures to PM2.5, SO2, and NO2 and COPD-related ED, HA or mortality with measures of uncertainty (p-values or confidence intervals) was included and relevant information was extracted into an Excel database. One study [17] was excluded since it re-evaluated data included in an eligible study published at an earlier date [18]. We also excluded one study that did not provide sufficient information to estimate 95% confidence intervals [19] and another that did not explore or control for confounding [20].
Many studies investigated and reported results for different lag/averaging times, which is problematic for meta-analyses, where researchers must select one estimate of the magnitude of the association between exposure and disease from each individual study to inform the meta-effect estimate. Some studies identified in the air pollution-COPD literature specified an exposure window a priori, while others investigated numerous lag/averaging times and either reported all results or only those with the largest or most significant effect estimate. Choosing to report one effect estimate rather than another because of effect size or statistical significance could introduce bias into the meta-effect estimate [21]. Since there was little consistency in the exposure metrics presented among the eligible studies and limited information regarding their biologic mechanisms, results from several exposure categories were extracted from each study; 1) single day lags, up to a maximum of two days, 2) multi-day averages or distributed lags, up to a maximum of seven days, and 3) the strongest effects across all available lag and averaging times. When multiple estimates were available for any of these categories, the strongest result within that category was selected.
A majority of studies estimated exposures for these lag/averaging times using 24-hour daily average concentrations. When results were provided for multiple daily metrics (such as 1-hour daily maxima and 24-hour daily averages), only results based on 24-hour daily averages were included [22,23], with the exception of one study which only provided results using 1-hour daily maxima [24]. A number of studies estimated results across various cities [22, 25, 26, 27, 28, 28]. Some of these studies calculated effects using raw data from all cities, while others calculated effect estimates for each city and then combined the results in a meta-analysis model. Wherever possible, we included pooled multi-city effects. Two studies only reported effects stratified by season and the stratified season-specific estimates were included [30,31]. When studies reported results for different age groups, effect estimates from elderly populations (ages 65+) were selected [32,33].
Statistical Analyses
Since studies presented results for different units of concentration, a series of conversions were completed prior to pooling individual effects through meta-analysis. All results reported in parts per billion (ppb) were first converted to ug/m3, assuming standard pressure and temperature. Risk estimates were then further standardized to represent effects associated with a 10 ug/m3 increase in concentration in PM2.5, SO2, and/or NO2. A 10 ug/m3 increase was selected for all pollutants since it was the most commonly used unit of analysis across the studies included in our pooled effect estimates.
Pooled summary effects were estimated with Comprehensive Meta-Analysis software (Version 2.0) for each pollutant and outcome combination. Summary effects were calculated using the weighted mean of individual effects, with weights equal to the inverse of each study’s variance [34]. In order to account for between study variability, a random effects model was chosen a priori. The appropriateness of this decision was confirmed by evaluating heterogeneity statistics. Forest plots were developed in Microsoft Excel for each pollutant using the exposure category that provided the strongest summary effects (represented by the highest pooled relative risk, and discussed further below). In these plots, the size of the symbols represents the relative weight of that study when computing summary effects [34,35]. Additional sub-group analyses were completed to assess differences by health outcome. We required a minimum of three studies to calculate a pooled effect estimate.
Heterogeneity was examined using standard Q and I2 tests [36–38]. The Q statistic tests the null hypothesis of homogenous effect sizes [36] with a p<0.10 suggesting substantial heterogeneity between studies. The I2 statistic quantifies the percent of total variability in effect sizes due to variability between studies, rather than within study sampling error [36–38]. Consequently, a higher I2 suggests greater heterogeneity between studies. Summary effect estimates are expressed as relative risks (RR) for 10 ug/m3 increases in pollutant concentration. The RR was selected because it is an intuitive commonly used measure in public health literature.
Results
The initial literature searches completed in PubMed and Medline databases identified 296 and 329 citations, respectively (Figure 1). After duplicates were removed, a total of 534 articles were left for title and abstract review. After screening titles and abstracts to eliminate articles that were overviews/reviews of existing literature, clinical or animal studies, studies focused on unrelated exposures (such as occupational, indoor or tobacco smoke exposures), or studies evaluating unrelated outcomes (such as COPD onset, lung cancer, asthma, pulmonary function testing or self-reported respiratory symptoms) 103 articles were considered potentially eligible and their full text was obtained and reviewed. Of these studies, an additional 71 were excluded since they did not present quantitative effect estimates or provide sufficient detail to estimate 95% confidence intervals, were a re-analysis of data already captured in an eligible article published at an earlier date, focused solely on exposure assessment or analytical methods, or evaluated other outdoor air pollutants not included in this review (such as PM10, PM speciation, ozone, or proximity to traffic). Five additional studies were identified in the references of eligible articles and USEPA Integrated Science Assessment documents [14–16], resulting in a total of 37 studies for meta-analysis (Table 1).
Figure 1.
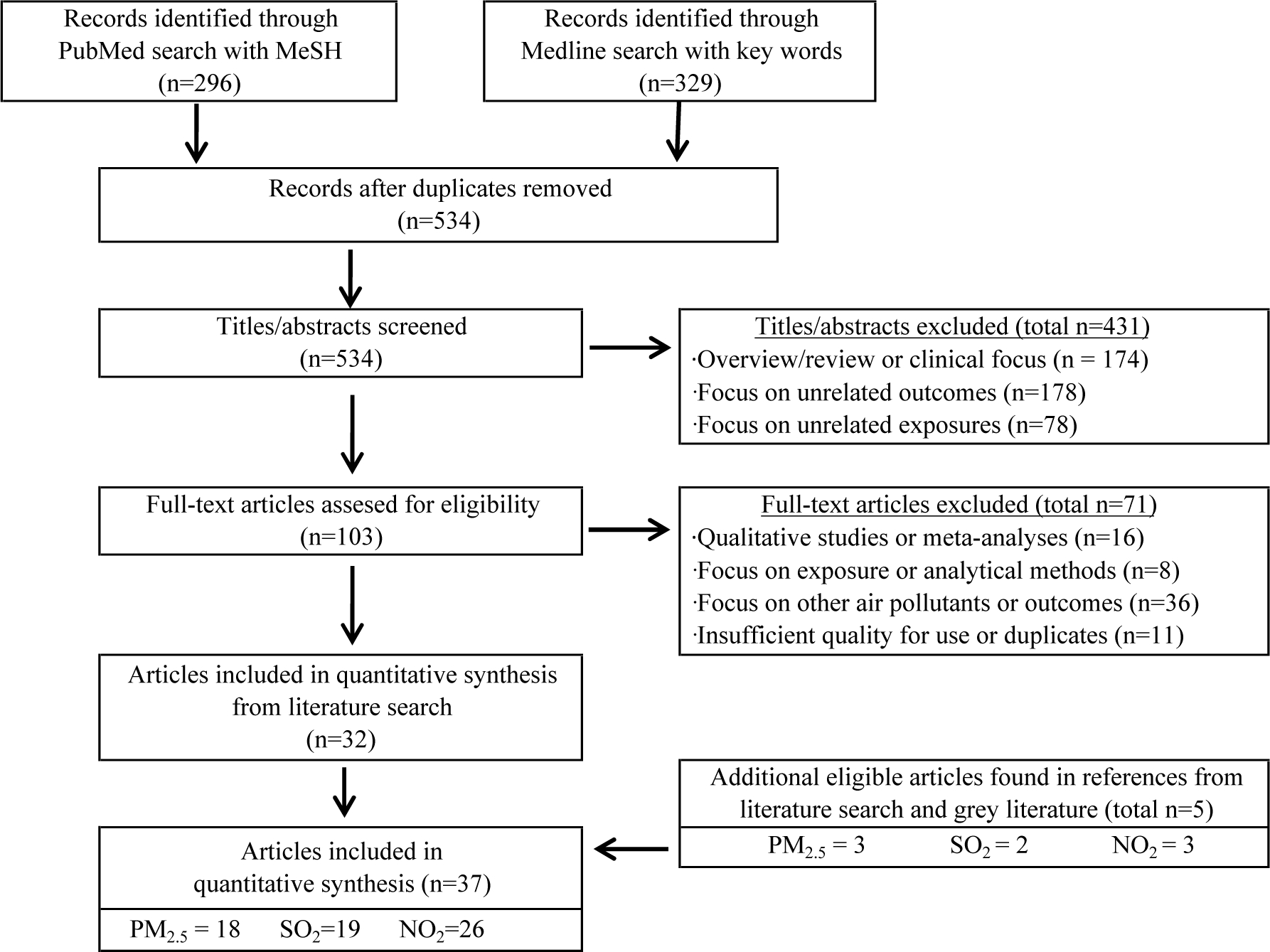
Summary of Systematic Literature Review
Table 1:
Summary of Studies Included in Meta-Analysis
| Study | Region | Pollutants | Design | Period | Outcome | Covariates Included in Modeling | ||
|---|---|---|---|---|---|---|---|---|
| SO2 | NO2 | PM2.5 | ||||||
|
| ||||||||
| Anderson et al. (1997) | Europe* | ✓ | ✓ | TS† | 1987–1992 | Hosp | A,B,C,D,E,F,G | |
| Arbex et al. (2009) | Brazil | ✓ | ✓ | TS | 2001–2003 | ED | A,B,C,D,E | |
| Belleudi et al. (2010) | Italy | ✓ | CC | 2001–2005 | Hosp | C,D,G,H | ||
| Chen et al. (2004) | Canada | ✓ | TS | 1995–1999 | Hosp | C, D | ||
| Cirera et al. (2012) | Spain | ✓ | ✓ | TS | 1995–1998 | ED | A,B,C,D,E,F,G, H | |
| Domincini et al. (2006) | USA* | ✓ | TS | 1999–2002 | Hosp | A,B,C,D,E | ||
| Faustini et al. (2012) | Italy | ✓ | ✓ | TS | 2005–2009 | Mort | A, C, E, G, H | |
| Faustini et al. (2013) | Italy | ✓ | CC | 2001–2005 | Hosp | A,B,C,D,G,H | ||
| Fischer et al. (2003) | Netherlands | ✓ | ✓ | TS | 1986–1994 | Mort | A, B,C,D,E,F,G | |
| Fusco et al. (2001) | Rome | ✓ | ✓ | TS | 1995–1997 | Hosp | A, C, D, E, F, G | |
| Garcia-Aymerich et al. (2000) | Spain | ✓ | ✓ | TS | 1985–1989 | Mort | A, C, D, G, H | |
| Halonen et al. (2008) | Finland | ✓ | ✓ | TS | 1998–2004 | ED | A, C, D, E, F, G, H | |
| Janssen et al. (2013) | Netherlands | ✓ | TS | 2008–2009 | Mort | A, B, C, D, E, F, G | ||
| Kan et al. (2003) | Shanghai | ✓ | ✓ | TS | 2000–2001 | Mort | A, B, C, D, E | |
| Kloog et al. (2014) | USA* | ✓ | CC | 2000–2006 | Hosp | B,C,D | ||
| Ko et al. (2007) | Hong Kong | ✓ | ✓ | ✓ | TS | 2000–2004 | Hosp | A,B,C,D,E,F |
| Lee et al. (2007) | Taiwan | ✓ | ✓ | CC | 1996–2003 | Hosp | C,D | |
| Martins et al. (2002) | Brazil | ✓ | ✓ | TS | 1996–1998 | ED | A,C,D,E,H | |
| Meng et al. (2013) | China* | ✓ | ✓ | TS† | 2001–2008 | Mort | A,C,D | |
| Milutinovic et al. (2009) | Serbia | ✓ | TS | 2002 | ED | A,B,C,D,E | ||
| Morgan et al. (1998) | Sydney | ✓ | TS | 1990–1994 | Hosp | A,B,C,E,F, | ||
| Neuberger et al. (2007) | Austria | ✓ | ✓ | TS | 2000–2004 | Mort | A,B,C,D,E,G | |
| Peel et al. (2005) | Atlanta | ✓ | ✓ | ✓ | TS | 1993–2000 | ED | A,B,C,D,E,F,H |
| Qui et al. (2012) | Hong Kong | ✓ | TS | 2000–2005 | Hosp | A,C,D,E,F,G | ||
| Samoli et al. (2014) | Europe* | ✓ | TS† | 2001–2010 | Mort | B,C,E,F,G,H | ||
| Santus et al. (2012) | Italy | ✓ | ✓ | ✓ | CC | 2007–2008 | ED | C,D |
| Sauerzapf et al. (2009) | UK | ✓ | CC | 2006–2007 | Hosp | C,G,H | ||
| Slaughter et al. (2005) | Washington | ✓ | TS | 1995–2001 | ED | B,C,D,E | ||
| Stieb et al. (2009) | Canada* | ✓ | ✓ | ✓ | TS† | 1990–2002 | ED | A.B,C,D,E,F |
| Sunyer at al. (2001) | Spain | ✓ | CC | 1990–1995 | Mort | C,D,G | ||
| Tao et al. (2014) | China | ✓ | ✓ | TS | 2001–2004 | Hosp | A,C,D,E,H | |
| Tenias et al. (2002) | Spain | ✓ | ✓ | TS | 1994–1995 | ED | A,B,C,D,E,F,G | |
| To et al. (2015) | Canada | ✓ | ✓ | TS | 2012 | ED&Hosp | A,B,C,E,H | |
| Tsai et al. (2013) | Tokyo | ✓ | CC | 2006–2010 | Hosp | C,D | ||
| Valdez et al. (2012) | Chile | ✓ | TS | 1998–2007 | Mort | A,B,T,D,E | ||
| Wong et al. (2002) | Hong Kong | ✓ | ✓ | TS | 1995–1998 | Mort | A,B,C,D,E | |
| Yang et al. (2005) | Vancouver | ✓ | ✓ | TS | 1994–1998 | Hosp | C,D | |
Notes:
Design: “TS”= time series and “CC” = case crossover
Outcome: “ED” = COPD-related emergency department visits, “Hosp”=COPD-related hospitalizations and “Mort”=COPD-related mortality
Covariates: A=time trends, B=seasonality, C=temperature, D=humidity and/or barometric pressure, E=day of week, F=holidays G=influenza epidemics, H=other
Indicates multiple cities were evaluated
indicates that results were pooled across multiple cities via meta analysis methods (i.e., with random effects model)
Of the 37 eligible studies, eight were case-crossover and 29 were time series studies. Most of the time series studies were analyzed via poisson regression with generalized additive models, while the case-crossover studies were analyzed with conditional logistic regression. Nine studies focused on COPD-related ED, 17 on COPD-related HA, and 11 on COPD-related mortality. Effect estimates were available in 18 studies for PM2.5, 25 studies for NO2, and 19 studies for SO2. Nearly all of the studies controlled for seasonality and weather, while approximately half of the studies controlled for regional trends of influenza. Most of the time series studies controlled for long term trends with smoothing splines and several also controlled for the day of week and holidays. Six of the case-crossover studies used a time-stratified control sampling strategy while two followed bi-directional control sampling [63].
Air Pollution and COPD-Related Morbidity
All three pollutants were positively associated with COPD-related morbidity (as ED or HA), with excess risks ranging from 2% to 4% per 10 ug/m3 increase in concentration (Figure 2). For PM2.5, we estimated a relative risk (RR) of 1.025 (95% CI 1.016 to 1.034) per 10 ug/m3 in concentration using multi-day averages (I2=74, Q=22.6, p<0.001, and n=9 studies). When using single-day lags, we found a slightly weaker, but still positive association with COPD-related morbidity (RR=1.014, 95% CI 1.005 to 1.024) (Table 2). For NO2, we estimated an RR of 1.042 (95 % CI 1.025 to 1.060) per 10 ug/m3 in concentration using multi-day averages (I2=96, p-value for Q test <0.001, and n=9 studies). Similar to PM2.5, we found a slightly weaker but positive association for NO2 when using single day lags (RR=1.020, 95% CI 1.006 to 1.031). For SO2, we estimated an RR of 1.021 (95% CI 1.007 to 1.035) per 10 ug/m3 increase in concentration using single-day lags (I2=87, p-value for Q test <0.001, and n=11 studies). But, in contrast to PM2.5 and NO2, we found a weaker albeit still significantly positive association for SO2 when using multi-day averages (RR=1.012, 95% CI 1.000 to 1.023).
Figure 2.
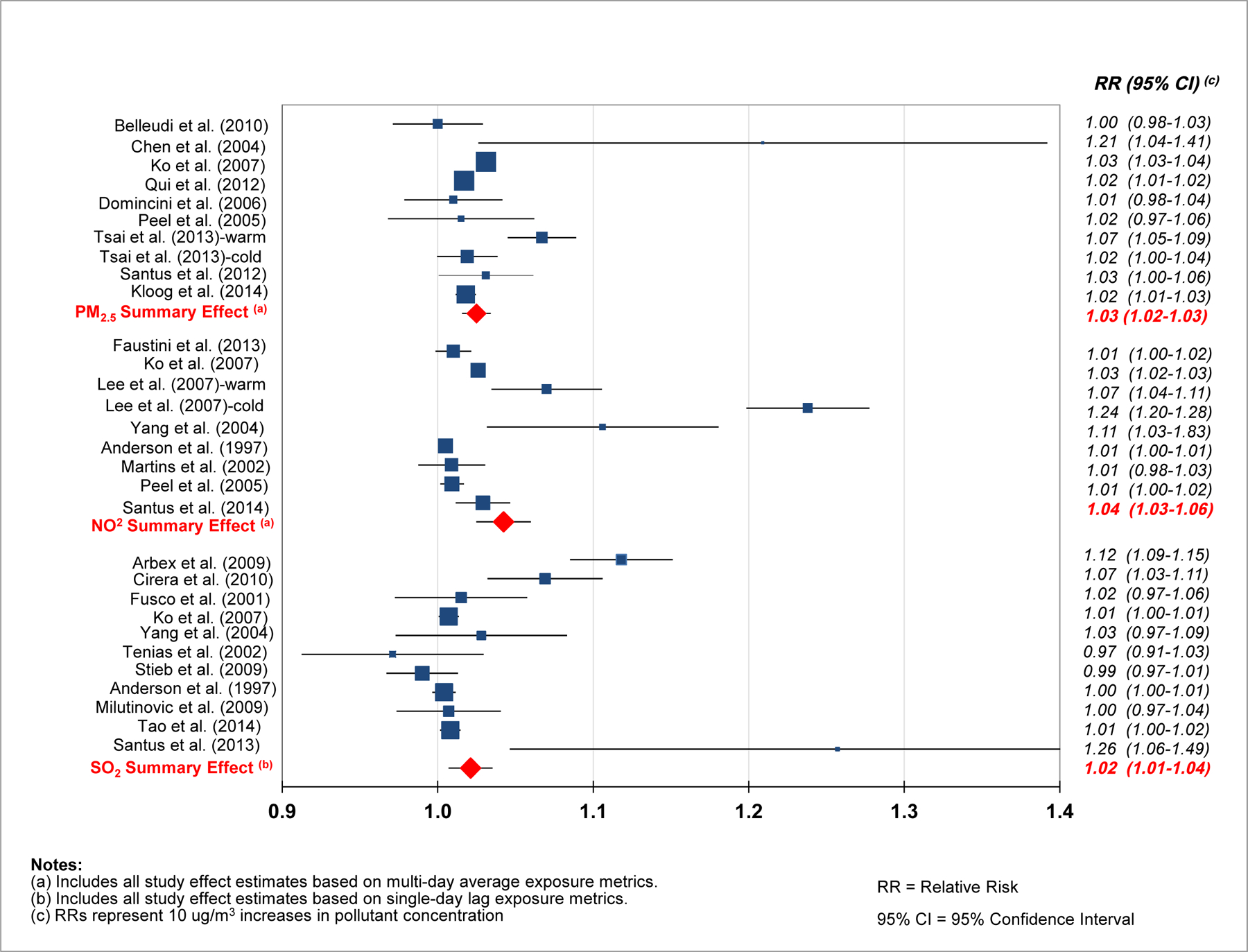
Outdoor Air Pollution and COPD Related ED Visits and HAs
Table 2:
Comparison of Pooled Effect Estimates by Exposure Metric
| Pollutant | Single Day Lags | Multi Day Averages | ||||
|---|---|---|---|---|---|---|
| # of Studies | Pooled Effect Estimate 1 | I2 statistic 2 | # of Studies | Pooled Effect Estimate 1 | I2 statistic 2 | |
| PM2.5 | 9 | 1.014 (1.005–1.024) | 76 | 10 | 1.025 (1.016–1.034) | 79 |
| NO2 | 15 | 1.020 (1.006–1.034) | 98 | 9 | 1.042 (1.025–1.060) | 96 |
| SO2 | 11 | 1.021 (1.007–1.035) | 87 | 9 | 1.012 (1.001–1.023) | 74 |
Notes:
Only studies evaluating COPD related emergency department visits (ED) and hospital admissions (HA) are included.
Summary effect estimates represent the relative risk of COPD-related ED/HA for a 10 ug/m3 increase in pollutant concentration
I2 represents the percentage of total variability in summary effect estimates that is due to variability between studies.
The Q statistic tests the hypothesis of homogeneity among effect sizes with p <0.10 suggesting heterogeneity between studies. All results shown in this table had p<0.001
In general, we found slightly stronger effect estimates for COPD-related morbidity (ED and HA) when using multi-day averages for both PM2.5 and NO2. For SO2, the reverse pattern was observed. The use of the strongest effect estimate available in each study produced similar results for each pollutant, suggesting that authors may preferentially report the strongest effects. Using the strongest effect estimates per study, we estimated an RR of 1.02 (95% CI 1.00 to 1.04) for PM2.5, an RR of 1.03 (95% CI 1.02 to 1.04) for NO2 and an RR of 1.02 (95 % CI 1.01 to 1.03) for SO2. Data not shown.
Subgroup Analyses: Morbidity and Mortality
Differences between morbidity (including EDs and HAs) and mortality outcomes were explored using the exposure category that produced the strongest pooled effects. Pooled effects for PM2.5 were two-fold higher for mortality (RR=1.048, 95% CI 1.019 to 1.078, based on 5 studies) than for morbidity, measured as ED or HA (RR=1.025, 95% CI 1.016 to 1.034, based on 10 studies). Conversely, stronger effects were calculated for NO2 when evaluating morbidity (RR=1.042, 95 CI 1.025 to 1.060, based on 9 studies) than for mortality (RR=1.030, 95% CI 1.016 to 1.045, based on 6 studies). However, confidence intervals were wide and overlapping. We did not identify enough mortality studies to investigate SO2 in this way.
Since there were not enough studies to compare ED with HA for each pollutant using the exposure metric that resulted in the greatest combined effect, these outcomes were compared using the strongest lag and averaging time across all studies. For SO2, we found stronger effects for ED (RR = 1.041, 95% CI 1.004 to 1.0879, and n=8 studies) than HA (RR of 1.010 (95% CI 1.002 to 1.019 and n=7 studies). For NO2, however, the pattern was reversed; ED showed a weaker effect (RR=1.010, 95% CI 1.002 to 1.018 and n=7 studies) than HA (RR=1.045, 95% CI 1.029 to 1.061). For PM2.5, we estimated similar effects for both outcomes; an RR of 1.023 (95% CI 1.002 to 1.043 and n=5 studies) for ED and an RR of 1.019 (95% CI 0.998 to 1.041 and n=10 studies) for HA.
Discussion
This meta-analysis is the first to our knowledge to quantify the association between short-term exposures to NO2, and SO2 and COPD-related morbidity, with the exception of one meta-analysis that focused specifically on studies among Chinese populations [10]. Positive associations were observed for each of these gaseous pollutants, with significant excess risks estimated between 2% to 4% per 10 ug/m3 increase in concentration. We also estimated a significant 1.4% to 2.5% increased risk in COPD-related ED and HA per 10 ug/m3 increase in PM2.5 (depending on selected exposure metric), which is slightly weaker but within the same range as that reported in a recent meta-analysis for PM2.5 [11]. Li and colleagues estimated a 3% (95% CI 2%–5%, 15 studies, I2=88%) increase in risk for COPD-related morbidity per 10 ug/m3 increase in PM2.5 [11]. This is slightly stronger than our estimate and likely due to the selection of the strongest effect estimate across all available lag and averaging times for each individual study. As noted above, we believe this method may introduce bias; a better approach would be to use consistent lags or averaging times for all studies combined into a pooled effect estimate. We estimated pooled effects separately for exposures based on single-day lags and multiple day averages and found that the strength of summary effects varied by 50% or more depending on which exposure metric was used. We hypothesize that this important source of variability may be a function of a pollutant’s day to day variability and the biologic mechanism. Of the four meta-analyses found in recent literature that specifically focus on acute effects among COPD patients from short-term exposures to outdoor air pollution [8–11], none of them investigated differences due to the use of different exposure metrics. Our results highlight the sensitivity of pooled effect estimates to the choice of lag/averaging time..
Effects of PM2.5 and NO2 were stronger using multiday averages compared to single day estimates. The reverse pattern was observed for SO2; the effect was stronger when exposure was measured as a single day lag rather than an average of several days.
One possible reason for the observed differences in effect estimates by exposure metric is the pollutants’ biologic mechanisms. The mechanisms by which airway inflammation is exacerbated following short-term exposures to outdoor air pollution are not yet fully understood, although there are several reasonable hypotheses. PM exposures cause increased airway hyper responsiveness in rodents and production of reactive oxygen and inflammatory factors in alveolar macrophages in humans [9]. Longer lag/averaging times are biologically plausible for PM compared to gaseous pollutants considering the proposed effect of particles on allergic sensitization and lung immune defenses, which have been observed in controlled human exposure and experimental animal studies[16]. NO2 exposures can exacerbate existing respiratory disease by impairing the functions of epithelial cells and alveolar macrophages, contributing to airway inflammation [14]. Similar to PM, this process may be cumulative over days and therefore a longer time period would be more relevant than the shorter period captured by single day lags. SO2, on the other hand, is a highly reactive gas with a high degree of day to day variability [15]. Bronchoconstriction in healthy adult males has been observed after short-term exposures to ambient levels of SO2 [64], as well as in numerous animal studies [15]. SO2 is also a well-known respiratory irritant, with acute respiratory symptoms reported immediately upon exposure to elevated concentrations in controlled human studies [15].
Mortality from COPD was about twice as strongly associated with PM2.5 than morbidity (ED and HA) from COPD (RR=1.050, 95% CI 1.015 to 1.087 for mortality and RR=1.026, 95% CI 1.014 to 1.038 for morbidity). Li and colleagues recently reported similar effects from short-term exposures of PM2.5 on COPD related morbidity and mortality [11]. Zhu and colleagues, in a meta-analysis of Chinese studies, reported the reverse pattern for PM10 and acute COPD outcomes [8]. There are a number of reasons why this may have occurred. Firstly, PM10 and PM2.5 are different particle size fractions containing diverse chemical components and moderated by meteorology, topography, and human behavior in different ways [16]. Secondly, the PM2.5 studies included in this meta-analysis are more recent (by nearly a decade) than the PM10 studies evaluated [8]. The stronger association that we found for PM2.5 and COPD-related mortality, as compared to COPD-related ED-HA, may reflect improvements in disease management over the past decade, whereby patients are increasingly better at avoiding certain triggers and taking care of themselves. This could result in decreased risk of ED-HA through time, while the risk remains high for more severe outcomes like mortality. This discrepancy may also be due to differences in the study populations or geographic regions represented in our studies. For example, a recent meta-analysis quantifying the association between PM and mortality reported higher risk of mortality among elderly and those with a lower socioeconomic status compared to younger, wealthier and more educated populations[65]. Finally this difference may be due to differences in the rationale for selecting individual effect estimates from eligible journal articles by Zhu and colleagues and as we have done in this paper.
This study also found stronger effects from SO2 for COPD-related ED than HA. These results are consistent with a recent study that compared ED and HA data from air pollution time-series studies for various diseases (i.e., respiratory disease, cardiovascular disease, pneumonia, etc.)[66]. Researchers estimated slightly higher risk ratios for respiratory disease related ED than HA and attributed this to differences in the types of patients typically experiencing these visits; patients for ED were often younger, from poorer areas, and with less severe illness[66]. Researchers also mentioned that HAs typically include scheduled visits, where the timing is unlikely to be caused by air pollution, which could mislead and/or dampen results [66]. We did not, however, find the same trend for exposures to PM2.5 and NO2.
Limitations
Heterogeneity and bias are two important limitations to discuss in the context of this meta-analysis. While we investigated several importance sources of heterogeneity through stratum specific pooled effects with a random effects model, there was still likely to have been substantial variation between studies. This is reflected in high estimates of between study variance (as represented by I2, shown in Table 2), most of which were greater than 80%. Due to sample size limitations, we were not able to investigate important differences in study design, geography, air chemistry, meteorology, and population health characteristics. We were also not able to investigate the impacts of different exposure metrics on the effect estimates for mortality due to the limited numbers of available studies.
Due to the limited number of studies available within strata and the large number of results presented in each article, we were also not able to formally evaluate publication bias in a meaningful way. If positive studies were more likely to have been published, these results may have been biased away from the null. Bias could also occur within published studies if authors only chose to present the strongest effect estimates. We tried to avoid this by mostly including studies that focused specifically on COPD and therefore explored/presented results from various lag/averaging times for this particular population. We intentionally kept our search criteria in PubMed and Medline quite specific to capture studies specifically focused on COPD outcomes and exclude the larger scope time series studies that investigate all causes of ED, HA, and mortality but often only present results with the strongest effect estimates and/or highest level of statistical significance. Inclusion of estimates from such studies could be misleading and bias results away from the null.
Finally, it is important to remember that meta-estimates of the effects of pollutants on COPD necessarily represent single pollutant models, while of course the COPD populations are breathing urban air containing all these pollutants and more. Thus these estimates represent simplifications of the true impacts of urban air pollution on existing COPD.
Conclusion
A comprehensive meta-analysis can help researchers recognize and understand inconsistencies among studies, especially where available studies report varying associations for the same exposure and health outcome. In this study, we found consistently positive associations between PM2.5, NO2, and SO2 and COPD-related morbidity and mortality. Although there was important variability among study results, they varied within a relatively narrow range. Excess risks were estimated at approximately 2% to 3% (per 10 ug/m3), regardless of pollutant, exposure metric, or COPD outcome. Looking specifically at COPD-related morbidity, 23 of the 25 individual effect estimates were positive and 70% had 95% confidence intervals excluding the null (Figure 2). This is a strong body of evidence for outdoor concentrations of particulates (PM2.5), and gaseous pollutants (NO2, and SO2) as important risk factors for COPD.
This study identified some of the key challenges associated with synthesizing diverse air pollution literature and the implications that certain study design decisions have on meta-analyses. More specifically this study identified the sensitivity of these findings to the lag/averaging times for pollutants used in the air pollution-COPD literature. There are no agreed upon standards for how exposure data should summarized for epidemiologic studies. In the absence of strong biologic evidence, it would be difficult to set such standards. In the meantime, researchers are urged to clearly define and present exposure-response estimates using several alternative exposure metrics so that meta-analysts can investigate the effects of alternative metrics, as we have reported here.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. This research was supported in part by a grant from the U.S. National Institute for Environmental Health Sciences R21-ES017849 and a training grant from the U.S. National Institute for Occupational Safety and Health T01-OH008424.
Appendix 1:
Summary of Studies Included in Meta-Analysis
| Study | Region | SO2 | NO2 | PM2.5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Average Conc. (ug/m3) | Selected Single Day Lag | Selected Multi-day Average | Average Conc. (ug/m3) | Selected Single Day Lag | Selected Multi-day Average | Average Conc. (ug/m3) | Selected Single Day Lag | Selected Multi-day Average | ||
|
| ||||||||||
| Anderson et al. (1997) | Europe | 21 to 53 | 1 | 0 to 2 | 42 to 67 | 1 | 0 to 2 | -- | -- | -- |
| Arbex et al. (2009) | Brazil | 14 | 0 | -- | -- | -- | -- | -- | -- | -- |
| Belleudi et al. (2010) | Italy | -- | -- | -- | -- | -- | -- | 22.8 | 0 | 0 to 2 |
| Chen et al. (2004) | Canada | -- | -- | -- | -- | -- | -- | 7.7 | 0 | 0 to 2 |
| Cirera et al. (2012) | Spain | 32 | 0 | -- | 51 | 0 | -- | -- | -- | -- |
| Domincini et al. (2006) | USA | -- | -- | -- | -- | -- | -- | 13.4 | 1 | 0 to 2 |
| Faustini et al. (2012) | Italy | -- | -- | -- | 60 | -- | 0 to 5 | 20.2 | -- | 0 to 5 |
| Faustini et al. (2013) | Italy | -- | -- | -- | 46 to 66 | 0 | 0 to 1 | -- | -- | -- |
| Fischer et al. (2003) | Netherlands | 10* | -- | -- | 32* | -- | 0 to 6 | -- | -- | -- |
| Fusco et al. (2001) | Rome | 9.1 | 0 | -- | 87 | 0 | -- | -- | -- | -- |
| Garcia-Aymerich et al. (2000) | Spain | 36 to 46* | -- | 0 to 2 | 88 to 97* | -- | 0 to 2 | |||
| Halonen et al. (2008) | Finland | -- | -- | -- | 28* | 0 | 9.5* | 0 | -- | |
| Janssen et al. (2013) | Netherlands | -- | -- | -- | -- | -- | -- | 16.3 | 1 | 0 to 6 |
| Kan et al. (2003) | Shanghai | 42 | -- | -- | 32 | 0 | -- | -- | -- | -- |
| Kloog et al. (2014) | USA | -- | -- | -- | -- | -- | -- | 12 | -- | 0 to 1 |
| Ko et al. (2007) | Hong Kong | 15 | 0 | 0 to 5 | 51 | 0 | 0 to 3 | 36 | 1 | 0 to 5 |
| Lee et al. (2007) | Taiwan | 25 | -- | 0 to 2 | 51 | -- | 0 to 2 | -- | -- | -- |
| Martins et al. (2002) | Brazil | 19 | -- | 0 to 5 | 118 | -- | 0 to 2 | -- | -- | -- |
| Meng et al. (2013) | China | 18 to 50 | -- | 0 to 2 | 58 to 67 | -- | 0 to 2 | -- | -- | -- |
| Milutinovic et al. (2009) | Serbia | 16 | 1 | 0 to 1 | -- | -- | -- | -- | -- | -- |
| Morgan et al. (1998) | Sydney | -- | -- | -- | 28 | 1 | -- | -- | -- | -- |
| Neuberger et al. (2007) | Austria | -- | -- | -- | 31 | -- | 0 to 7 | 16 | -- | 0 to 7 |
| Peel et al. (2005) | Atlanta | 44 | -- | 0 to 2 | 87 | -- | 0 to 2 | 19 | -- | 0 to 2 |
| Qui et al. (2012) | Hong Kong | -- | -- | -- | -- | -- | -- | 39.4 | -- | 0 to 3 |
| Samoli et al. (2014) | Europe | -- | -- | -- | -- | -- | -- | 14 to 28 | -- | 0 to 5 |
| Santus et al. (2012) | Italy | 4.1 | 2 | 0 to 2 | 103 | 1 | 0 to 2 | 32.8 | 2 | 0 to 2 |
| Sauerzapf et al. (2009) | UK | -- | -- | -- | 23 | 1 | -- | -- | -- | -- |
| Slaughter et al. (2005) | Washington | -- | -- | -- | -- | -- | -- | 4.2 to 20 | 1 | -- |
| Stieb et al. (2009) | Canada | 3.7 to 20 | 1 | -- | 17 to 43 | 0 | -- | 6.7 to 9.8 | 1 | -- |
| Sunyer at al. (2001) | Spain | -- | -- | -- | 46 | 0 | -- | -- | -- | -- |
| Tao et al. (2014) | China | 79 | 3 | -- | 46 | 4 | -- | |||
| Tenias et al. (2002) | Spain | 27 | 0 | -- | 58 | 0 | -- | -- | -- | -- |
| To et al. (2015) | Canada | -- | -- | -- | 45 | 0 | -- | 14 | 0 | -- |
| Tsai et al. (2013) | Tokyo | -- | -- | -- | -- | -- | -- | 30 | -- | 0 to 2 |
| Valdez et al. (2012) | Chile | -- | -- | -- | -- | -- | -- | 34* | 0 | 0 to 1 |
| Wong et al. (2002) | Hong Kong | 17 | -- | -- | 56 | -- | 0 to 2 | -- | -- | -- |
| Yang et al. (2005) | Vancouver | 10.0 | 0 | 1 to 7 | 32 | 0 | 1 to 7 | -- | -- | -- |
Notes:
Indicates that value represents median concentration
Contributor Information
Rebecca DeVries, University of Massachusetts Lowell, Department of Work Environment, 1 University Avenue, Kitson Hall: Room 200P, Lowell, MA, USA
David Kriebel, Department of Work Environment, University of Massachusetts Lowell, Lowell, MA, USA
Susan Sama, Department of Work Environment, University of Massachusetts Lowell, Lowell, MA, USA
REFERENCES
- 1.Global Initiative for Chronic Lung Disease (GOLD). Global Strategy for Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. 2015.
- 2.World Health Organization. The Global Burden of Disease: 2004 Update; World Health Organization: Geneva, Switzerland. 2008. [Google Scholar]
- 3.World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). [Internet]. Available from: http://www.who.int/respiratory/copd/en/ (Accessed on May 5, 2015).
- 4.Chapman KR., Mannino DM, Soriano JB, Vermeire PA, Buist AS, Thun MJ, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J 2006;27:188–207. [DOI] [PubMed] [Google Scholar]
- 5.Burt L, Corbridge S COPD Exacerbations. Evidence-based guidelines for identification, assessment, and management... second in a two-part series. Am J Nursing. 2013; 113(2):34–45. [DOI] [PubMed] [Google Scholar]
- 6.Ko F, Hui D Air Pollution and Chronic Obstructive Pulmonary Disease. Respirology 2012; 17:395–401. [DOI] [PubMed] [Google Scholar]
- 7.Glass G Primary, secondary and meta-analysis of research. Educational Researcher 1975;5(10):3–8. [Google Scholar]
- 8.Zhu R, Chen Y, Wu S, Deng F, Liu Y, Yao W The relationship between particulate matter (PM10) and hospitalizations and mortality of chronic obstructive pulmonary disease: A meta-analysis. COPD 2013;10(3):307–315. [DOI] [PubMed] [Google Scholar]
- 9.Song Q, Christiani D, Wang X, Ren J The global contribution of outdoor air pollution to the incidence, prevalence, mortality and hospital admission for chronic obstructive pulmonary disease: A systematic review and meta-analysis. Int J Environ Res Public Health 2014;11:11822–11832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai H, Tsang H, Wong C Meta-analysis of adverse health effects due to air pollution in Chinese populations. BMC Public Health 2013;13(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li MH, Fan LC, Mao B, Yang JW, Choi AM, Cao WJ, Xu JF Short term exposures to ambient fine particulate matter (PM2.5) increases hospitalizations and mortality of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Chest 2015;149(2):447–458. [DOI] [PubMed] [Google Scholar]
- 12.Pai M, McCulloch M, Gorman JD, Pai N, Enanoria W, Kennedy G, et al. Systematic reviews and meta-analyses. Natl Med J India 2004;17(2):86–95. [PubMed] [Google Scholar]
- 13.National Library of Medicine (NLM). Fact Sheet: Medical Subject Headings (MeSH). [Internet]. 2013. Available from: http://www.nlm.nih.gov/pubs/factsheets/mesh.html
- 14.USEPA. Integrated Science Assessment for Oxides of Nitrogen - Health Criteria. EPA/600/R-08/071, National Center for Environmental Assessment – RTP Division, Research Triangle Park, NC. 2008. July. [Google Scholar]
- 15.USEPA. Integrated Science Assessment for Sulfur Oxides - Health Criteria. EPA/600/R-08/047F, National Center for Environmental Assessment – RTP Division, Research Triangle Park, NC. 2008. September. [Google Scholar]
- 16.USEPA. Integrated Science Assessment for Particulate Matter, EPA/600/R-08/139F, National Center for Environmental Assessment - RTP Division, Research Triangle Park, NC. 2009. December. [Google Scholar]
- 17.Kan H, Chen B Air pollution and daily mortality in Shanghai: a time-series study. Arch Environ Health 2003;58(6):360–367. [PubMed] [Google Scholar]
- 18.Kan H, Chen B A case-crossover analysis of air pollution and daily mortality in Shanghai. J Occup Health 2003;45(2):119–124. [DOI] [PubMed] [Google Scholar]
- 19.Moolgavkar SH Air pollution and hospital admissions for chronic obstructive pulmonary disease in three metropolitan areas in the United States. Inhal Toxicol 2000;12(4);75–90. [DOI] [PubMed] [Google Scholar]
- 20.Hapcioglu B, Issever H, Kocyigit E, Disci R, Vatansever S, Ozdilli K The Effect of air pollution and metrological parameters on chronic obstructive pulmonary disease at an Istanbul hospital. Indoor Built Environ 2006;15:147–153. [Google Scholar]
- 21.Smith TJ, Kriebel D A Biologic Approach to Environmental Assessment and Epidemiology. Oxford: Oxford University Press. 2010. [Google Scholar]
- 22.Andersen HR, Spix C, Medina S, Schouten JP., Castellsague J, Rossi G, et al. Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: Results from the APHEA project. Eur Respir J 1997;10(5):1064–1071. [DOI] [PubMed] [Google Scholar]
- 23.Tenías JM, Ballester F, Pérez-Hoyos S, Rivera ML. Air pollution and hospital emergency room admissions for chronic obstructive pulmonary disease in Valencia, Spain. Arch Environ Health 2002;57(1):41–47. [DOI] [PubMed] [Google Scholar]
- 24.Martins CL, Latorre Mdo R, Saldiva PH., Braga AL Air pollution and emergency room visits due to chronic lower respiratory diseases in the elderly: An ecological time-series study in São Paulo, Brazil. J Occup Environ Med 2002;44(7):622–627. [DOI] [PubMed] [Google Scholar]
- 25.Slaughter JC, Kim E, Sheppard L, Sullivan JH, Larson TV, Claiborn C Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Expo Anal Environ Epidemiol 2005;15(2):153–159. [DOI] [PubMed] [Google Scholar]
- 26.Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. J Am Med 2006;295(10)L:1127–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stieb DM, Szyszkowicz M, Rowe BH, Leech JA Air pollution and emergency department visits for cardiac and respiratory conditions: A multi-city time-series analysis. Environ Health 2009;8(25). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meng X, Wang C, Cao D, Wong CH, Kan H Short-term effect of ambient air pollution on COPD mortality in four Chinese cities. Atmos Environt 2013;77:149–154. [Google Scholar]
- 29.Samoli E, Stafoggia M, Rodopoulou S, Ostro B, Alessandrini E, Basagana X, et al. Which specific causes of death are associated with short term exposure to fine and coarse particles in Southern Europe? Results from the MED-PARTICLES project. Environ Inter 2014;67:54–61. [DOI] [PubMed] [Google Scholar]
- 30.Lee IM, Tsai SS, Chang CC, Ho CK, Yang CY Air pollution and hospital admissions for chronic obstructive pulmonary disease in a tropical city: Kaohsiung, Taiwan. Inhal Toxicol 2007;19(5):393–398. [DOI] [PubMed] [Google Scholar]
- 31.Tsai SS, Chang CC & Yang CY Fine particulate air pollution and hospital admissions for chronic obstructive pulmonary disease: a case-crossover study in Taipei. Int J Environ Res Public Health 2013;10(1):6015–6026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Halonen JI, Lanki T, Yli-Tuomi T, Kulmala M, Tiittanen P, Pekkanen J Urban air pollution, and asthma and COPD hospital emergency room visits. Thorax 2008;63(7):635–641. [DOI] [PubMed] [Google Scholar]
- 33.Fischer P, Hoek G, Brunekreef B, Verhoeff A, van Wijnen J Air pollution and mortality in the Netherlands: are the elderly more at risk? Eur Respir J Suppl 2003;40:34S–38S. [DOI] [PubMed] [Google Scholar]
- 34.Borenstein M, Hedges L, Higgins J, Rothstein H Introduction to Meta-Analysis. John and Wiley Sons, Ltd., West Sussex, UK. 2009. [Google Scholar]
- 35.Schriger D, Altman D, Vetter JA, Heafner T, Moher D Forest plots in reports of systematic reviews: a cross-sectional study reviewing current practice. Int J Epidemiol 2010:39(2): 421–429. [DOI] [PubMed] [Google Scholar]
- 36.Huedo-Medina T, Sanchez-Meca J, Marin-Martinez F, Botella J Assessing heterogeneity in meta-analysis: Q statistic or I2 index? CHIP Documents. Paper 19. 2006. [Internet]. Available at: http://digitalcommons.uconn.edu/chip_docs_19. [DOI] [PubMed] [Google Scholar]
- 37.Higgins JPT & Thompson SG Quantifying heterogeneity in a meta-analysis. Statist. Med 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 38.Higgins JP, Green S Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series, John Wiley and Sons. 2008. [Google Scholar]
- 39.Arbex MA, de Souza Conceicao GM, Cendon SP, Arbex FF, Lopes AC, Moyses EP, et al. Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health 2009;63(1):777–783. [DOI] [PubMed] [Google Scholar]
- 40.Belleudi V, Faustini A, Stafoggia M, Cattani G, Marconi A, Perucci CA., et al. Impact of fine and ultrafine particles on emergency hospital admissions for cardiac and respiratory diseases. Epidemiology 2010;21(3):414–423. [DOI] [PubMed] [Google Scholar]
- 41.Chen Y, Yang Q, Krewski D, Shi Y, Burnett RT, McGrail K Influence of relatively low levels of particulate air pollution on hospitalization for COPD in elderly people. Inhal Toxicol 2004;16(1):21–25. [DOI] [PubMed] [Google Scholar]
- 42.Cirera L, Garcia-Marcos L, Gimenez J, Moreno-Grau S, Tobia A, Perez-Frenandez V, et al. Daily effects of air pollutants and pollen types on asthma and COPD hospital emergency visits in the industrial and Mediterranean Spanish city of Cartagena. Allergol Immunopathol 2012;40(4):231–237. [DOI] [PubMed] [Google Scholar]
- 43.Faustini A, Stafoggia M, Cappai G, Forastiere F Short-term effects of air pollution in a cohort of patients with chronic obstructive pulmonary disease. Epidemiology 2012;23(6):861–879. [DOI] [PubMed] [Google Scholar]
- 44.Faustini A, Stafoggia M, Colais P, Berti G, Bisanti L, Cadum E, et al. Air pollution and multiple acute respiratory outcomes. Eur Respir J 2013;42(2):304–313. [DOI] [PubMed] [Google Scholar]
- 45.Fusco D, Forastiere F, Michelozzi P, Spadea T, Ostro B, Arca M, et al. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur Respir J 2001;17(6):1143–1150. [DOI] [PubMed] [Google Scholar]
- 46.Garcia-Aymerich J, Tobías A, Anto JM, Sunyer J Air pollution and mortality in a cohort of patients with chronic obstructive pulmonary disease: A time series analysis. J Epidemiol Community Health 2000;54(1):73–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Janssen NA, Fischer P, Marra M, Ameling C, Cassee FR. Short-term effects of PM2.5, PM10 and PM2.5–10 on daily mortality in The Netherlands. Sci Total Environ 2013;463–464:20–26. [DOI] [PubMed] [Google Scholar]
- 48.Kloog I, Nordio F, Zanobetti A, Coull BA, Koutrakis P, Schwartz JD Short term effects of particle exposure on hospital admissions in the Mid-Atlantic states: a population estimate. PLoS One 2014;9(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ko FW, Tam W, Wong TW, Chan D, Tung Al., Lai C, et al. Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax 2007;62(9):780–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Milurinovic S, Nikic D Stosic L, Stankovic A, Bogdanovic D Short-term association between air pollution and emergency room admissions for chronic obstructive pulmonary disease in Nis, Serbia. Cent Eur J Public Health 2009;17(1):8–13. [DOI] [PubMed] [Google Scholar]
- 51.Morgan G, Corbett S, Wlodarczyk J Air pollution and hospital admissions in Sydney, Australia, 1990 to 1994. Am J Public Health 1998;88(12):1761–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Neuberger A Rabczenko D, Moshammer H Extended effects of air pollution on cardiopulmonary mortality in Vienna. Atmos Environ 2007;41(38):8549–8556. [Google Scholar]
- 53.Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology 2005;16(2):164–174. [DOI] [PubMed] [Google Scholar]
- 54.Qiu H, Yu IT, Tian L, Wang X, Tse LA, Tam W, et al. Effects of coarse particulate matter on emergency hospital admissions for respiratory diseases: a time-series analysis in Hong Kong. Environ Health Perspect 2012;120(4):572–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sauerzapf V, Jones AP, Cross J Environmental factors and hospitalization for chronic obstructive pulmonary disease in a rural county of England. J Epidemiol Community Health 2009;63(4):324–328. [DOI] [PubMed] [Google Scholar]
- 56.Santus P, Russo A, Madonini E, Allegra L, Blasi F, Centanni S, et al. How air pollution influences clinical management of respiratory diseases. A case-crossover study in Milan. Respir Res 2012;13:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sunyer J, Basagaña X Particles, and not gases, are associated with the risk of death in patients with chronic obstructive pulmonary disease. Int J Epidemiol 2001;30(5):1138–1140. [DOI] [PubMed] [Google Scholar]
- 58.Tao Y, Mi S, Zhou S, Wang S, Xie X Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ Pollut 2014;185:196–201. [DOI] [PubMed] [Google Scholar]
- 59.To T, Feldman L, Simatovic J, Gershon A, Dell S, Su J, et al. Health risk of air pollution on people living with major chronic diseases: a Canadian population-based study. BMJ Open 2015:5(9):e009075–e009075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Valdez A, Zanobetti A, Halonen J, Cifuentes L, Morata D, Schwartz J Elemental concentrations of ambient particles and cause specific mortality in Santiago, Chili: a time series study. Environ Health 2012:11(82). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wong T, Ram W, Yu T, Wong A Associations between daily mortalities from respiratory and cardiovascular disease and air pollution in Hong Kong, China. Occup Environ Med 2002;59(1):30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang Q, Chen Y, Krewski D, Burnett RT, Shi Y McGrail KM Effect of short-term exposure to low levels of gaseous pollutants on chronic obstructive pulmonary disease hospitalizations. Environ Res 2005;99(1):99–105. [DOI] [PubMed] [Google Scholar]
- 63.Whitaker H, Hocine M, Farrington P On case-crossover methods for environmental time series data. Environmetrics 2006;18(2):157–171. [Google Scholar]
- 64.Devalia JL, Rusznak C, Herdman MJ, Trigg CJ, Tarraf H, Davies RJ Effect of nitrogen dioxide and sulfur dioxide on airway response of mild asthmatic patients to allergen inhalation. Lancet. 1994;344(8938):1668–1671. [DOI] [PubMed] [Google Scholar]
- 65.Bell M, Zanobetti A, Domincini F Evidence on the vulnerability and susceptibility to health risks associated with short-term exposure to particulate matter: a systematic review and meta-analysis. Am J Epidemiol. 2013;178(6):865–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Winquist A, Klein M, Tolbert P, et al. 2012. “Comparison of emergency department and hospital admissions data for air pollution time-series studies”, Environmental Health, vol. 11, no.70. [DOI] [PMC free article] [PubMed] [Google Scholar]


