Abstract
Background
The impact of the COVID-19 pandemic on physical therapy services for people with multiple sclerosis (pwMS) is unknown. Therefore, the Special Interest Group for Mobility (SIG Mobility) of the European Network for Best Practice and Research in Multiple Sclerosis Rehabilitation (RIMS) has undertaken the initiative to examine the impact of the COVID-19 outbreak on physical therapy services and physical activity participation in pwMS across Europe, Israel and Australia.
Objective
To describe the impact of the COVID-19 outbreak on physical therapy practice from the perspective of the therapist.
Methods
An online survey was developed and conducted from December 2020 to July 2021. The survey (50 questions), included multiple-choice questions and open-ended responses.
Results
In total, 215 physical therapists (PT's) from 9 countries (Australia, Belgium, the Czech Republic, Ireland, Israel, Italy, Norway, Spain, and Turkey) participated in the study. The therapy most affected during the pandemic was aerobic training/conditioning exercises; 33.5% reported that these activities were either reduced or unavailable. In contrast, 15% of the PTs reported increased use of relaxation/mind body techniques and/or fatigue management programs during the pandemic. PTs reported a mixture of positive and negative feelings about the therapeutic sessions offered during the pandemic. Most reported positive feelings included “positive” (26.5%), and “optimistic” (24.7%). Negative feelings most frequently reported included “worried” (30.7%), and “hesitant” (20.9%). The PTs reported a 10% decrease in the use of hands-on techniques and a 10% increase in the use of oral instructions when treating moderately and severely pwMS during as compared to before the pandemic.
Conclusion
The COVID-19 pandemic has affected physical therapy services in pwMS internationally in terms of content, frequency of use and format.
Keywords: Multiple sclerosis, Physical therapy, COVID-19, International network, RIMS
1. Introduction
An unprecedented outbreak of a severe acute respiratory syndrome, the coronavirus infection, occurred in December 2019. This virus which originated in Wuhan, China, became known as the coronavirus disease (COVID-19) (Wu et al., 2020). On March 11, 2020, the World Health Organization (WHO) declared this outbreak a pandemic. As of January 2022, the virus remains active and has infected ∼300 million individuals globally and led to the untimely death of ∼5.5 million individuals worldwide (WHO coronavirus disease 2020).
The COVID-19 virus is overwhelming healthcare services and healthcare workers globally, including rehabilitation services. Bettger et al (2020) reported that in 63% of the twelve countries examined, rehabilitation services have come to a standstill due to a shift in the staff and/or resources to patients seriously affected by COVID-19 (Prvu Bettger et al., 2020). Due to this pandemic, the shortage of rehabilitation services for people with disabilities has been detrimental in terms of physical and mental health, thus, significantly impairing their quality of life (Prvu Bettger et al., 2020). A recent report from the United Nations stated that due to the COVID-19 pandemic, along with the shift of health priorities across the globe, many people with disabilities feel that they have been “left behind” (UN News March 19, 2020). According to a recent study survey of the CogEx research team, the majority of individuals with progressive MS reported some type of impact of the COVID-19 pandemic on their psychological well-being, although they reported hardly any change in regarding to symptoms of depression, anxiety and overall quality of life (Chiaravalloti et al., 2021).
A large proportion of people with multiple sclerosis (pwMS) use rehabilitation services on a regular basis (Beer, Khan, and Kesselring, 2012). A major part of rehabilitation for pwMS, in some cases the only service, is physical therapy. It has been observed that physical therapists (PTs) play an important role in providing guidance for improving functional mobility through physical activity, exercise, and adaptive equipment. According to a clinical bulletin published by the National MS Society, the ultimate role of the PT in aiding pwMS is to inspire hope, resilience, and happiness through movement (Rohrig, 2018). In addition, through the use of constructive touch coupled with movement, the PT can inspire health awareness, promote prevention strategies, introduce wellness concepts and assist with optimizing health care in the MS population (Rohrig, 2018).
The COVID-19 virus has hugely impacted the physical therapy profession. According to a special report from the American Physical Therapy Association in August 2020, (Impact of COVID-19 2020) many PTs have experienced reductions in working hours and income, mainly due to a decline in physician referrals and direct access visits. The use of telehealth and other video-based consultation has increased; however, technology challenges amongst patients and clinics remain a barrier; hence, face-to-face care remains more common and preferred (Impact of COVID-19 2020, Miller et al., 2021). The current information referring to the profession, in general, may not be accurate for the MS population. To date, the impact of the COVID-19 pandemic on physical therapy services for pwMS is unknown.
In order to clarify the current situation in the MS population, the Special Interest Group for Mobility (SIG Mobility) of the European Network for Best Practice and Research in MS Rehabilitation (RIMS) has undertaken the initiative. The main objective of the research group was to examine the impact of the COVID-19 outbreak on physical therapy services and physical activity participation in people with MS across Europe, Israel and Australia. In the present study, we will focus on the impact of the COVID-19 outbreak on physical therapy practice from the perspective of the therapist.
2. Methods
2.1. Survey development
Two online surveys, one for the therapist and the other for pwMS, were developed and conducted from December 2020 to July 2021, by the SIG Mobility group of RIMS. The primary research questions of the project were linked with the impact of the COVID-19 pandemic on: (1) physical activity participation (intensity, frequency and type) from the perspective of the patient; (2) the use of technologies for physical rehabilitation from the perspective of both the patient and therapist; (3) physical therapy practice for pwMS from the perspective of the therapist.
Project phases were set according to the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) (Eysenbach, 2004). Initially, in December 2020, the management aspects of the project were defined. The project coordinator convened those members of the SIG Mobility group who had expressed an interest to actively participate in the project. Interested members were grouped per country, and a primary investigator (PI) was selected for each country. Responsibilities of the PI-country included continuous communication with the local participants, other PIs, and the project coordinator. In parallel, a subgroup of four members was formed in order to produce the first draft of the online survey in the English language. Several versions of the first draft were distributed (via Google drive) between members of the subgroup, asking for their feedback until a final first draft accepted by all four members, was created. The online survey was partly based on previous survey research on physical therapy content, delivery and interventions in pwMS across Europe (Řasová et al., 2020, Martinková et al., 2018).
The second phase of the project (January-February 2021) focused on piloting and further editing the final version of the online survey. Starting with the initial draft, feedback was requested from all members, taking into account any requirements/restrictions of each participating country. Following the feedback of each participating country, the final version of the survey (for therapists) in the English language, totaling 50 questions, was affirmed (Supplementary 1). The survey included multiple-choice questions and open-ended responses; a response was mandatory for all questions. Key questions included: “How did COVID-19 affect the frequency of use of the following PT interventions during the pandemic (2020)?”; “Which format did you use for the following PT interventions (when applicable) during the pandemic (2020)?”; “How do you feel about delivering your PT interventions during the pandemic (2020)?”; “During a standard treatment, how much time do you use “hands-on” (manual) therapy, verbal instructions and demonstrations during the pandemic (2020)?”.
In order to clearly differentiate between the pre-pandemic and pandemic era we defined the pre-pandemic period as the year 2019 and pandemic era as the year 2020. This decision was made due to the fact that the first confirmed case of the COVID-19 pandemic was found in France, during January 2020, and subsequently, spread extensively across the continent. Moreover, due to the pattern of the COVID pandemic, characterized by a series of waves at different time points between countries, concurrently, with different governmental restrictions changing frequently, we did not match the therapist's response with the exact restriction per country. We, therefore, consider 2020 as the year of lockdowns, travel restrictions, and avoidance of face-to-face meetings. The time needed to complete the survey was estimated at 20 minutes. Information related to the purpose of the study, target population, ethical approval, data collection, storage, and privacy was described on the informed consent screen at the beginning of the survey.
The third phase took place during March-April 2021. The primary objectives of this phase included: (1) defining and implementing the strategy to translate the final survey version from English into local languages (i.e., a translation/back-translation process), some countries used the English version (2) applying for ethical approval (e.g., local adaptation of informed consent and privacy statement), (3) disseminating the survey (i.e., identification of the available online platforms, determining the period of time in which completion of the survey will be possible) and, (4) recruiting responders (e.g., mailing lists, number of reminders). Additional tasks achieved during the third phase included: (1) implementation of the online survey (in all languages) together with an integrity check (i.e., testing usability and technical operation); (2) Ethics approval to conduct the study and share anonymous data within the project group was obtained for each country; (3) establish the recruitment plan (i.e., define the launch date of the online survey per country, defining a period of 6-weeks for data collection, sending online reminders after week two and four, and deciding on local source/s of contacts).
Finally, during the fourth phase (May-July 2021), the PI-country was responsible for advertising/disseminating the online survey to all participating institutions in their countries (e.g., via local networks, professional organizations, personal contacts, social media). Furthermore, the survey (in several languages) was disseminated through the RIMS website https://www.eurims.org/. The survey was voluntary, and no incentives were offered. In parallel, working groups were established for data analysis and manuscript writing.
2.2. Data combination, cleaning and analysis
Members of the data analysis subgroup created an electronic datasheet using numeric codes across the data set of open-ended survey responses. Each PI-site received the electronic datasheet together with a codebook that included the codes and descriptions. After independently coding each country, the PI-site shared their coded datasheet with the study coordinator. Subsequently, all country representatives met online to resolve misunderstandings and/or instances of conflict. The final data sheet was analyzed using the IBM SPSS version 27.0 (IBM Corp, Armonk, New York, USA). Missing data were not included in the analysis. Descriptive statistics summarized the distribution of therapists’ responses in terms of age, gender, educational background, professional experience, type of workplace, and type of treatment (in/outpatient). The Wilcoxon signed-rank test determined changes in the format of the standard physical therapy treatment (i.e., hands-on, verbal instruction, demonstration) in the total sample, according to disability subgroups (mild/moderate/severe), and type of workplace (hospital/rehabilitation center, private practice). The difference in the use of therapeutic interventions (i.e., decreased use, increased use, no change), delivery mode (face-to-face, online, both), and feelings (i.e., worried, optimistic, anxious, stressed, etc.) among the PTs working in different types of workplace was investigated using the chi-squared test with a Bonferroni correction. The consequences of the COVID-19 pandemic on the use of therapeutic interventions, delivery mode, and feelings are presented as percentages.
3. Results
In total, 215 physical therapists from 9 countries (Australia, Belgium, the Czech Republic, Ireland, Israel, Italy, Norway, Spain, and Turkey) participated in the survey study. Characteristics and demographics of the responding PT's are presented in Table 1 . Most of the therapists originated from the Czech Republic, whereas the least originated from Australia. The majority of PTs were female (77.7%), aged 31-50. As for the educational background, 41.3% held a bachelor's degree, 33.2% a master's degree, 15.4% certified at a diploma level, and 10.1% held a doctoral degree. Most PTs’ (32.1%) professional experience ranged from 11 and 20 years and 30.7% over 20 years. In terms of the workplace, 38.7% of the PTs, at the time of the pandemic, were working in a rehabilitation hospital/center, mostly with outpatients (73.6%).
Table 1.
Demographics of the study sample
| Total (n=215) 100% | Australia (n=7) 3% | Belgium (n=9) 4% | Czech Republic (n=65) 30% | Ireland (n=14) 7% | Israel (n=10) 5% | Italy (n=30) 14% | Norway (n=30) 14% | Spain (n=32) 15% | Turkey (n=18) 8% | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age, years | ||||||||||
| 20-30 | 50 (23.4) | 1 (14.3) | 4 (44.4) | 10 (15.4) | 0 (0.0) | 3 (30.33) | 7 (23.3) | 7 (23.3) | 8 (25.0) | 10 (55.6) |
| 31-40 | 64 (29.9) | 3 (42.9) | 1 (11.1) | 23 (35.4) | 4 (28.6) | 4 (44.4) | 14 (46.7) | 4 (13.3) | 7 (21.9) | 4 (22.2) |
| 41-50 | 63 (29.4) | 2 (28.6) | 2 (22.2) | 21 (32.3) | 6 (42.9) | 2 (22.2) | 3 (10.0) | 12 (40.0) | 11 (34.4) | 4 (22.2) |
| 51-60 | 29 (13.6) | 1 (14.3) | 1 (11.1) | 10 (15.4) | 3 (21.4) | 0 (0.0) | 6 (20.0) | 3 (10.0) | 5 (15.6) | 0 (0.0) |
| Over 60 | 8 (3.7) | 0 (0.0) | 1 (11.1) | 1 (1.5) | 1 (7.1) | 0 (0.0) | 0 (0.0) | 4 (13.3) | 1 (3.1) | 0 (0.0) |
| Missing data | 1 (<0.01) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Gender | ||||||||||
| Male | 48 (22.3) | 1 (14.3) | 2 (22.2) | 12 (18.5) | 2 (14.3) | 2 (20.0) | 10 (33.3) | 11 (36.7) | 5 (15.6) | 3 (16.7) |
| Female | 167 (77.7) | 6 (85.7) | 7 (77.8) | 53 (81.5) | 12 (85.7) | 8 (80.0) | 20 (66.7) | 19 (63.3) | 27 (84.4) | 15 (83.3) |
| Missing data | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Education | ||||||||||
| Doctor of Philosophy (PhD) | 21 (10.1) | - | 0 (0.0) | 8 (12.3) | 4 (28.6) | 0 (0.0) | 1 (3.3) | 1 (3.3) | 0 (0.0) | 7 (38.9) |
| Master of Science (MSc) | 69 (33.2) | - | 6 (66.7) | 31 (47.7) | 1 (7.1) | 2 (20.0) | 5 (16.7) | 8 (26.7) | 9 (28.1) | 7 (38.9) |
| Bachelor of Science (BSc) | 86 (41.3) | - | 3 (33.3) | 10 (15.4) | 9 (64.3) | 8 (80.0) | 24 (80.0) | 20 (66.7) | 8 (25.0) | 4 (22.2) |
| Diploma | 32 (15.4) | - | 0 (0.0) | 16 (24.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.3) | 15 (46.9) | 0 (0.0) |
| Missing data | 7 (0.03) | 7 (100.0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Professional experience, years | ||||||||||
| 0-2 | 22 (10.2) | 0 (0.0) | 1 (11.1) | 7 (10.8) | 0 (0.0) | 3 (30.0) | 2 (6.7) | 2 (6.7) | 3 (9.4) | 4 (22.2) |
| 3-10 | 58 (27.0) | 2 (28.6) | 3 (33.3) | 18 (27.7) | 1 (7.1) | 4 (40.0) | 10 (33.3) | 6 (20.0) | 5 (15.6) | 9 (50.0) |
| 11-20 | 69 (32.1) | 5 (71.4) | 1 (11.1) | 24 (36.9) | 6 (42.9) | 0 (0.0) | 10 (33.3) | 11 (36.7) | 11 (34.4) | 1 (5.6) |
| Over 20 | 66 (30.7) | 0 (0.0) | 4 (44.4) | 16 (24.6) | 7 (50.0) | 3 (30.0) | 8 (26.7) | 11 (36.7) | 13 (40.6) | 4 (22.2) |
| Missing data | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Type of center | ||||||||||
| Acute hospital / center | 34 (16.0) | 0 (0.0) | 0 (0.0) | 20 (32.3) | 4 (28.6) | 0 (0.0) | 1 (3.3) | 1 (3.3) | 0 (0.0) | 8 (44.4) |
| Rehabilitation hospital / center | 82 (38.7) | 0 (0.0) | 7 (77.8) | 17 (27.4) | 0 (0.0) | 10 (100) | 11 (36.7) | 15 (50.0) | 17 (53.1) | 5 (27.8) |
| Community center / services | 40 (18.9) | 1 (14.3) | 0 (0.0) | 3 (4.8) | 5 (35.7) | 0 (0.0) | 8 (26.7) | 6 (20.0) | 14 (43.8) | 3 (16.7) |
| Private clinic / practice | 53 (25.0) | 4 (57.1) | 2 (22.2) | 22 (35.5) | 4 (28.6) | 0 (0.0) | 10 (33.3) | 8 (26.7) | 1 (3.1) | 2 (11.1) |
| Other | 3 (1.4) | 2 (28.6) | 0 (0.0) | 0 (0.0) | 1 (7.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Missing data | 3 (0.01) | 0 | 0 | 3 (0.05) | 0 | 0 | 0 | 0 | 0 | 0 |
| Type of treatment | ||||||||||
| Inpatients | 43 (20.7) | - | 2 (22.2) | 24 (36.9) | 2 (14.3) | 0 (0.0) | 6 (20.0) | 0 (0.0) | 6 (18.8) | 3 (16.7) |
| Outpatients | 153 (73.6) | - | 7 (77.8) | 36 (55.4) | 11 (78.6) | 10 (100) | 23 (76.7) | 30 (100.0) | 22 (68.8) | 14 (77.8) |
| Both | 12 (5.8) | - | 0 (0.0) | 5 (7.7) | 1 (7.1) | 0 (0.0) | 1 (3.3) | 0 (0.0) | 4 (12.5) | 1 (5.6) |
| Missing data | 7 (0.03) | 7 (100.0) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Values are presented n (%).
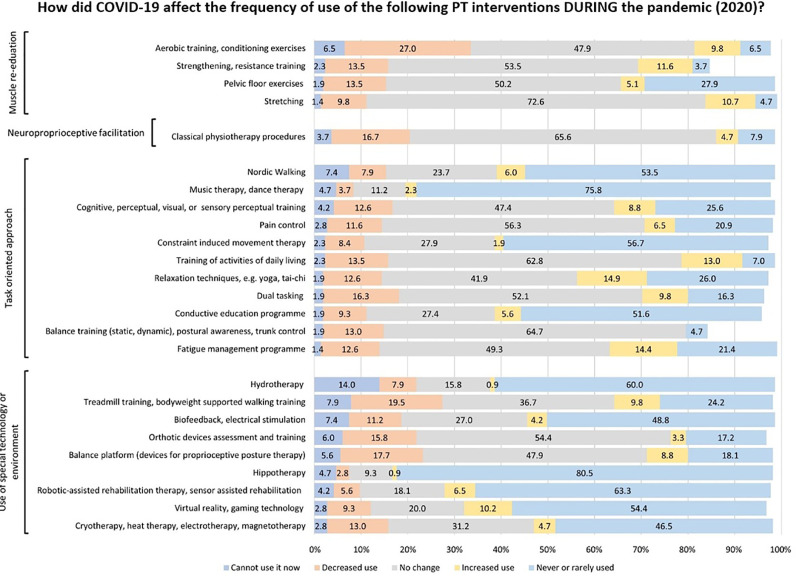
Fig. 1 details changes in the use of therapeutic items during the pandemic (2020) compared with the pre-COVID-19 period (2019). Most PTs reported that the COVID-19 pandemic affected their regular use of intervention tools/therapeutic approach. The item most affected during the pandemic was aerobic training/conditioning exercises; 33.5% of the responders, reported that these activities were either reduced or unavailable. Additional items that were frequently reported by the PTs as either cannot use know or decreased during the pandemic consisted mainly of technologies such as bodyweight supported walking (27.4%), computerized postural control training (23.3%), practice with orthotic devices (21.8%), and biofeedback/electrical stimulators (18.6%). Furthermore, 21.9% of the PTs reported that hydrotherapy sessions were either reduced or unavailable during the pandemic. Noteworthy, 14.9% of the PTs reported increased use of relaxation/mind-body techniques (i.e., yoga, tai-chi) during the pandemic; 14.4% reported an increase in fatigue management programs, and 13.0% reported an increase in activities of daily living training. In terms of workplace, no significant differences were found in the use of therapeutic interventions between workplace subgroups (p<0.05), except for aerobic training where the therapists in the private sector reported more often “cannot use it now” compared to those working in a hospital/rehabilitation center (p<0.05).
Fig. 1.
Changes in the use of physiotherapy therapeutic items during the pandemic (2020) compared with the pre-COVID-19 period (2019).
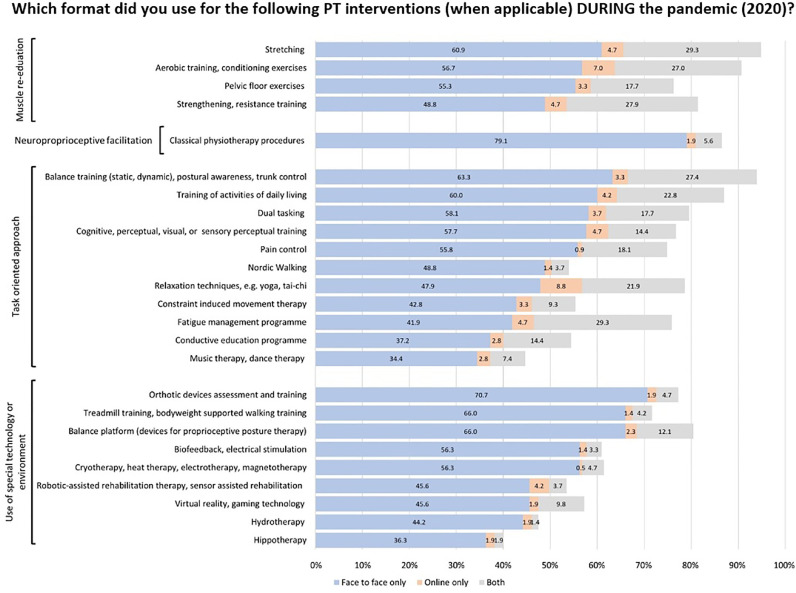
Fig. 2 presents the format of delivering physical therapy interventions. A large segment of therapeutic interventions was provided either in a hybrid format (i.e., combining face-to-face and online sessions) or solely online. A hybrid or solely online format was reported by approximately 30% of the PTs for sessions focusing on stretching, aerobic/resistance training, and conditioning exercises. Additional therapies with high proportions of respondents reporting delivery in either a hybrid or solely online format included: fatigue management (34%), balance training (30.7%), and relaxation/mind-body techniques (30.8%). The delivery format of therapeutic interventions involving technologies was face-to-face in most cases (Fig. 2). In terms of workplace, usage of a face-to-face format for aerobic training, stretching, and balance exercise was significantly higher in the private practice sector compared with the hospital/rehabilitation center sector (p<0.05).
Fig. 2.
Delivery format of therapeutic interventions during the COVID-19 pandemic (2020)
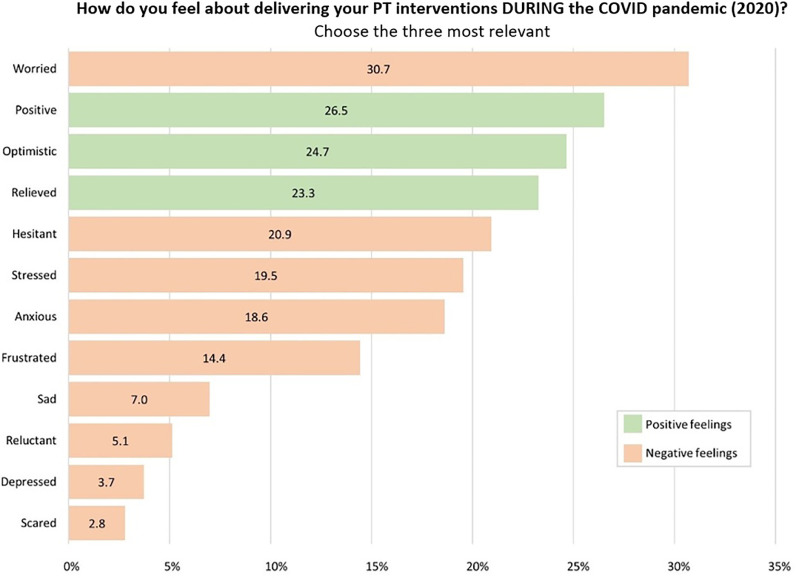
Fig. 3 presents the distribution of the PTs feelings regarding the delivery of physical therapy sessions during the COVID-19 pandemic. The PTs reported a mixture of positive and negative feelings vis-à-vis the therapeutic sessions offered during the pandemic. Frequently reported negative feelings included the terms “worried” (30.7%), “hesitant” (20.9%) “stressed” (19.5%), and “anxious” (18.6%). Positive feelings reported at a relatively high rate included “positive” (26.5%), “optimistic” (24.7%), and “relieved” (23.3%). No significant differences were observed in the therapists’ feelings between workplace subgroups (p<0.05), except for the term “stressed” which was selected significantly more by therapists working in a hospital/rehabilitation center (p<0.05).
Fig. 3.
Distribution of the PTs feelings regarding the delivering of physical therapy sessions during the COVID-19 pandemic.
When treating mildly disabled pwMS, the PTs did not report any change in the content of a standard physical therapy session during the pandemic. However, in contrast, changes in the content of a standard session were reported when treating pwMS with moderate and severe disability. The PTs reported a 10% decrease in the use of hands-on techniques and a 10% increase in the use of oral instructions in these two disability subgroups. Nevertheless, these findings were found solely in therapists working in a hospital/rehabilitation sector. Table 2 presents the changes in the content of a standard physical therapy session during the pandemic according to the patient's level of disability and type of therapist workplace.
Table 2.
Changes in the content of a standard physical therapy treatment
| Total sample | Hospital / rehab center (n=156) | Private clinic / practice (n=53) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Before COVID-19 | During COVID-19 | p-value | Before COVID-19 | During COVID-19 | p-value | Before COVID-19 | During COVID-19 | p-value | |
| While working with mildly impaired pwMS (%) | |||||||||
| Hands-ona | 30 (20-50) | 30 (20-50) | 0.658 | 30 (13-50) | 30 (15-50) | 0.787 | 30 (20-50) | 30 (20-50) | 0.919 |
| Verbal instructionb | 40 (20-60) | 40 (30-60) | 0.191 | 40 (30-60) | 50 (30-60) | 0.327 | 40 (20-60) | 40 (25-70) | 0.326 |
| Demonstrtionc | 30 (20-50) | 30 (20-50) | 0.766 | 30 (20-40) | 30 (20-50) | 0.610 | 30 (20-50) | 30 (10-50) | 0.272 |
| While working with moderately impaired pwMS (%) | |||||||||
| Hands-ona | 50 (50-60) | 40 (40-60) | <0.001* | 50 (30-60) | 40 (30-60) | <0.001* | 50 (30-70) | 40 (25-60) | 0.095 |
| Verbal instructionb | 30 (30-50) | 40 (40-50) | 0.033* | 30 (20-50) | 40 (30-50) | 0.005* | 30 (20-40) | 30 (20-45) | 0.509 |
| Demonstrtionc | 20 (20-40) | 30 (30-40) | 0.312 | 20 (10-40) | 30 (20-40) | 0.269 | 20 (15-54) | 30 (20-50) | 0.877 |
| While working with severely impaired pwMS (%) | |||||||||
| Hands-ona | 70 (70-80) | 60 (60-80) | <0.001* | 70 (50-80) | 60 (40-80) | <0.001* | 70 (50-80) | 60 (40-80) | 0.233 |
| Verbal instructionb | 20 (20-40) | 22 (22-40) | <0.001* | 20 (10-40) | 30 (20-49) | <0.001* | 20 (10-43) | 24 (20-40) | 0.858 |
| Demonstrtionc | 20 (20-30) | 20 (20-40) | 0.043* | 20 (10-30) | 20 (10-40) | 0.056 | 20 (10-32) | 20 (10-40) | 0.720 |
*p<0.05; Wilcoxon signed-rank test.
Values are presented as median (interquartile range).
Hands-on includes manual therapy techniques and facilitation of movement using the therapist's hands on the patient's body.
Verbal instruction is defined as giving oral instructions and cueing to the patient regarding their exercises, gait, and any other type of functional movement patterns.
Demonstration is defined as physically showing the patient how to do an exercise or a functional movement pattern by demonstrating the movement first by the therapist.
4. Discussion
The main objective of the current study was to report on the impact of the COVID-19 outbreak on physical therapy services for pwMS internationally. This multicenter project is part of a larger research agenda to better understand the consequences of the COVID-19 pandemic on clinical and management aspects of MS rehabilitation. Specifically, members of the SIG Mobility group of RIMS were interested to explore the impact of the pandemic on physical therapy and physical activity in pwMS. This interest was reinforced following a recent survey study performed in Israel in the second half of 2020 demonstrating that 50.8% of the pwMS ceased or decreased their leisure-time physical activity during the COVID-19 pandemic. Moreover, 31.7% reported that their fitness level had also decreased during this period (Kalron et al., 2021). Since maintaining physical activity is one of the primary goals of PTs treating pwMS, we determined that it is very important to further explore this issue. In light of the ongoing COVID-19 pandemic situation, this need has increased.
According to the present online survey, during the COVID-19 pandemic, 6.5% stopped using aerobic exercise (as part of the physical therapy service) and 27% reported decreasing the use of aerobic training compared with the period prior to the pandemic. Similarly, resistance training and neuro-proprioceptive facilitation techniques were reduced, ∼20% reported reducing or not be able to use it at time of the pandemic. Importantly, although the present information is based solely on the therapists’ responses, we acknowledge that these findings are in accordance with the patient's responses, which will be further elaborated on in detail in a separate paper reporting on this project. Anyway, health professionals treating pwMS should be alarmed by these observations.
There is a consensus amongst clinicians that physical activity, including aerobic and strength training, is imperative for pwMS (Dalgas et al., 2020). Emerging evidence has demonstrated that physical activity can improve walking performance, balance, cognition, fatigue, depression, and the pwMS’ quality of life (Dalgas and Stenager, 2012, Dalgas et al., 2019, Motl and Sandroff, 2015, Motl et al., 2017, Barry et al., 2016, Beckerman et al., 2010). Furthermore, Barry et al (Barry et al., 2016) demonstrated that exercise programs are potential immunomodulatory therapies targeting innate signaling mechanisms and modulating MS symptom development and progression. Therefore, any reduction in these activities due to the COVID-19 situation might worsen the health status of pwMS. We advise health professionals to encourage pwMS to continue (or start) with their regular exercise practice regardless of the availability of face-to-face physical therapy sessions. In addition, PT's are advised to offer pwMS new alternatives for aerobic/strength training that can be performed outside the traditional clinical environment.
Worth noting, during the pandemic, PTs reported an increase in the use of relaxation techniques/mind body techniques and fatigue management programs as part of the physical therapy services. We speculate that this increase is due to higher stress rates of pwMS during this COVID-19 pandemic. Since 2021, studies reporting on the impact of the COVID-19 pandemic on the mental load of pwMS have significantly increased (Giordano et al., 2021, Broche-Pérez et al., 2021, Garjani et al., 2021, Artemiadis, Anagnostouli, and Alexopoulos, 2011). The high prevalence of stress amongst pwMS is especially worrying since recent studies have demonstrated a linear relationship between increased stress and more disease activity (Bonavita et al., 2021, Taylor and Taylor-Piliae, 2017). Bonavita et al (2021) recently observed, via an online survey, that pwMS (n=612) have suffered more frequently from depression, high levels of stress, and less social support, compared with healthy adults (n=674) throughout the COVID-19 pandemic (Artemiadis, Anagnostouli, and Alexopoulos, 2011). An additional explanation for the increase in the use of relaxation/mind body techniques might be that these interventions are easy to deliver virtually for the therapist e.g. through a video online platform.
Consequently, techniques such as yoga and tai-chi may assist in alleviating pwMS’ stress. According to Taylors & Taylor-Piliae's systematic review, tai-chi is safe and positively impacts psychological functions, including a reduction in depression and fatigue in pwMS (Mohr et al., 2012). Moreover, there is strong evidence supporting the use of yoga and conservation/fatigue management programs in the management of MS-related fatigue (Miller and Soundy, 2017). Recently, Solianik et al (2021) demonstrated that a 10-week tai-chi intervention provided during the COVID-19 pandemic decreased depressive symptoms and cognition in older adults (Solianik et al., 2021). In the same context, a recent study found yoga as an effective self-management strategy to cope with stress, anxiety, and depression and maintain a feeling of wellbeing during the COVID-19 lockdowns (Sahni et al., 2021). Therefore, PTs should consider employing relaxation/mind-body techniques (face-to-face and/or online) during the pandemic and simultaneously explore their effect on mood and fatigue MS-related symptoms.
PTs reported a mixture of positive (i.e., optimistic, relieved) and negative (i.e., worried, hesitant, stressed, anxious, frustrated) feelings relating to their services during the pandemic. Research on the psychosocial impact of working during the COVID-19 pandemic amongst PTs (not specifically working in the field of MS) was performed in Poland, Spain, Italy, and the USA (Pniak et al., 2021, de Sire et al., 2021, Palacios-Ceña et al., 2021, Ditwiler, Swisher, and Hardwick, 2021, Tiwari et al., 2021). In these studies, most PTs noted challenges in discharging patients and planning patient/family education due to the impact of social isolation. Nevertheless, the PTs reported mixed feelings towards their work. Some reported a high prevalence of work-related burnout during the pandemic, noticeable amongst those working in clinical departments (Pniak et al., 2021, de Sire et al., 2021). At the same time, other PTs felt that the pandemic increased a sense of togetherness amongst the team members and promoted a greater appreciation for life and work (Tiwari et al., 2021). Interestingly, the term “stressed” was reported at higher rate by therapists working in a hospital/rehabilitation center compared to therapists working in the private sector. This finding might be explained by the therapists’ fear of being infected by the COVID-19 virus. As is well known, most patients severely infected by the disease were hospitalized for relatively long periods in these centers. We believe that the feelings reported by the PTs in this survey replicate those of the general physical therapy community. We, therefore, encourage health organizations to be aware of the psychosocial status of the PTs (as well as all other health professionals) treating pwMS during the COVID-19 pandemic and offer help/consultation in case of need.
We are aware that the present study is not free from limitations. Firstly, the survey does not focus on the reasons for the change in physical therapy practice, though this was implied to be due to the pandemic restrictions. We attribute this limitation to the method (online survey) by which the data were collected. Worth noting, while constructing the online survey, we tried to keep it as short as possible in order to reach a high response rate; however, concurrently, we needed to insert enough questions so as to receive sufficient data to answer our research questions. Secondly, there may have been an overrepresentation of PTs from the Czech Republic (30% of responders) which could be attributed to the time when this survey was disseminated, as it was closely aligned with a surge of COVID-19 in Eastern Europe, with the Czech Republic as one of the epicenters. Furthermore, due to several countries reporting on relatively small samples, we did not present the data according to each country, as this information would have been misleading. Finally, despite the fact that a panel of experts had formulated the online questionnaire, it would have been beneficial to utilize widespread, standardized, and validated scales. However, no such scales existed at the beginning of the study and the time frame was too short for a comprehensive development process of questionnaires.
5. Conclusions
The COVID-19 pandemic has affected physical therapy services in pwMS in terms of content and format. According to the online survey, which included over 200 PTs from nine countries, there has been a reduction in the sessions that had focused on aerobic and strength training. On the other hand, there has been an increase in sessions focusing on relaxation/mind body techniques. Furthermore, the delivery of sessions using an online format has seemed to increase amongst PTs treating pwMS. Physical therapists reported a mixture of positive and negative feelings towards their work. In light of the ongoing pandemic situation, we believe that the results may guide decision makers and impact on the future of physical therapy services in pwMS during and after pandemics. A specific interest is whether and which changes will remain once the COVID-19 pandemic reaches an end. Further work from our research group will present data on the impact of the pandemic on physical therapy practice and physical activity participation from the perspective of pwMS.
CRedit Authorship contribution statement
Turhan Kahraman: Conceptualization, Formal analysis, Data Curation, Writing - Review & Editing. Kamila Rasova: Conceptualization, Methodology, Writing - Review & Editing. Johanna Jonsdottir: Conceptualization, Writing - Review & Editing. Carme Santoyo Medina: Conceptualization, Methodology, Writing - Review & Editing Daphne Kos: Conceptualization, Methodology, Writing - Review & Editing. Susan Coote: Conceptualization, Writing - Review & Editing. Andrea Tacchino: Conceptualization, Writing - Review & Editing. Tori Smedal: Conceptualization, Writing - Review & Editing. Ellen Christin Arntzen: Conceptualization, Writing - Review & Editing. Gillian Quinn: Conceptualization, Methodology, Writing - Review & Editing. Yvonne Learmonth: Conceptualization. Ludovico Pedulla: Conceptualization. Lousin Moumdjian: Conceptualization, Methodology, Data Curation, Writing - Review & Editing, Supervision, Project administration. Alon Kalron: Conceptualization, Methodology, Writing - Original Draft, Supervision.
Funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors thank the participants, organizations and the individuals listed for their support for the study; Asiye Tuba Ozdogar, Zuhal Abasiyanik, Yonca Zenginler Yazgan, Sapir Alster Dreyer, Antoine Vanbeylen, Deborah Severijns, Erica Grange, Sandra Fernández from the Federación Española de Esclerosis Múltiple, Gisela Carrés, Roger Meza, Ingrid Galan, Dolors Fàbregas Montserrat Janer, Samuel Sànchez, Gaizka Loyola, Noemí Martínez, Gloria Yaya, Marta Lordán and Eugènia Lacasa from Fundació Esclerosi Múltiple (FEM) and Pedro Carrascal, Iratxe Elorriaga and Erika Otxoa from Asociación de Esclerosis Múltiple de Bizkaia, Jan Harald Aarseth, Inger Elise Engelund, Britt Normann, Marietta van der Linden.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.msard.2022.103799.
Appendix. Supplementary materials
References
- Artemiadis AK, Anagnostouli MC, Alexopoulos EC. Stress as a risk factor for multiple sclerosis onset or relapse: a systematic review. Neuroepidemiology. 2011;36:109–120. doi: 10.1159/000323953. [DOI] [PubMed] [Google Scholar]
- Barry A, Cronin O, Ryan AM, Sweeney B, Yap SM, O'Toole O, et al. Impact of exercise on innate immunity in multiple sclerosis progression and symptomatology. Front Physiol. 2016;7:194. doi: 10.3389/fphys.2016.00194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckerman H, de Groot V, Scholten MA, Kempen JC, Lankhorst GJ. Physical activity behavior of people with multiple sclerosis: understanding how they can become more physically active. Phys. Ther. 2010;90:1001–1013. doi: 10.2522/tj.0090345. [DOI] [PubMed] [Google Scholar]
- Beer S, Khan F, Kesselring J. Rehabilitation interventions in multiple sclerosis: an overview. J Neurol. 2012;259(9):1994–2008. doi: 10.1007/s00415-012-6577-4. [DOI] [PubMed] [Google Scholar]
- Bonavita S, Sparaco M, Russo A, Borriello G, Lavorgna L. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID-19 pandemic. Eur J Neurol. 2021;28:3396–3402. doi: 10.1111/ene.14697. [DOI] [PubMed] [Google Scholar]
- Broche-Pérez Y, Jiménez-Morales RM, LO Monasterio-Ramos, Vázquez-Gómez LA, Fernández-Fleites Z. Fear of COVID-19, problems accessing medical appointments, and subjective experience of disease progression, predict anxiety and depression reactions in patients with Multiple Sclerosis. Mult Scler Relat Disord. 2021;53 doi: 10.1016/j.msard.2021.z3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiaravalloti ND, Amato MP, Brichetto G, Chataway J, Dalgas U, DeLuca J, Meza C, Moore NB, Feys P, Filippi M, Freeman J, Inglese M, Motl R, Rocca MA, Sandroff BM, Salter A, Cutter G, Feinstein A. CogEx Research Team. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J. Neurol. 2021;268(5):1598–1607. doi: 10.1007/s00415-020-10160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalgas U, Hvid LG, Kwakkel G, Motl RW, de Groot V, Feys P, et al. Moving exercise research in multiple sclerosis forward (the MoXFo initiative): Developing consensus statements for research. Mult. Scler. 2020;26:1303–1308. doi: 10.1177/1352458520910360. [DOI] [PubMed] [Google Scholar]
- Dalgas U, Langeskov-Christensen M, Stenager E, Riemenschneider M, Hvid LG. Exercise as medicine in multiple sclerosis-time for a paradigm shift: Preventive, symptomatic, and disease-modifying aspects and perspectives. Curr. Neurol. Neurosci. Rep. 2019;19:88. doi: 10.1007/s11910-019-1002-3. [DOI] [PubMed] [Google Scholar]
- Dalgas U, Stenager E. Exercise and disease progression in multiple sclerosis: Can exercise slow down the progression of multiple sclerosis? Ther Adv Neurol Disord. 2012;5:81–95. doi: 10.1177/1756285611430719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Sire A, Marotta N, Raimo S, Lippi L, Inzitari MT, Tasselli A, et al. Psychological distress and work environment perception by physical therapists from southern Italy during COVID-19 pandemic: The C.A.L.A.B.R.I.A Study. Int. J. Environ. Res. Public Health. 2021;18:9676. doi: 10.3390/ijerph18189676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ditwiler RE, Swisher LL, Hardwick DD. Professional and ethical issues in United States acute care physical therapists treating patients with COVID-19: Stress, walls, and uncertainty. Phys. Ther. 2021;101:pzab122. doi: 10.1093/ptj/pzab122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J. Med. Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garjani A, Hunter R, Law GR, Middleton RM, Tuite-Dalton KA, Dobson R, et al. Mental health of people with multiple sclerosis during the COVID-19 outbreak: A prospective cohort and cross-sectional case-control study of the UK MS Register. Mult. Scler. 2021 doi: 10.1177/13524585211020435. [DOI] [PubMed] [Google Scholar]
- Giordano A, Cetta I, Orrico M, Montini F, Sangalli F, Colombo B, et al. Stress related to COVID-19 pandemic as a trigger for disease activity in multiple sclerosis: a case report. Neurol Sci. 2021;42:3969–3971. doi: 10.1007/s10072-021-05442-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Impact of COVID-19 . American Physical Therapy Association; 2020. on the Physical Therapy profession.https://aptac.memberclicks.net/assets/APTA_impact-of-covid-19-on-physical-therapy-profession.pdf Available from. [Google Scholar]
- Kalron A, Dolev M, Greenberg-Abrahami M, Menascu S, Frid L, Avrech-Shezifi S, et al. Physical activity behavior in people with multiple sclerosis during the COVID-19 pandemic in Israel: Results of an online survey. Mult Scler Relat Disord. 2021;47:02603. doi: 10.1016/j.msard.2020.102603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinková P, Freeman J, Drabinová A, Erosheva E, Cattaneo D, Jonsdottir J, et al. Physiotherapeutic interventions in multiple sclerosis across Europe: Regions and other factors that matter. Mult Scler Relat Disord. 2018;22:59–67. doi: 10.1016/j.msard.2018.03.005. [DOI] [PubMed] [Google Scholar]
- Miller MJ, Pak SS, Keller DR, Barnes DE. Evaluation of Pragmatic Telehealth Physical Therapy Implementation During the COVID-19 Pandemic. Phys. Ther. 2021;101(1):pzaa193. doi: 10.1093/ptj/pzaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller P, Soundy A. The pharmacological and non-pharmacological interventions for the management of fatigue related multiple sclerosis. J. Neurol. Sci. 2017;381:41–54. doi: 10.1016/j.jns.2017.08.012. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Lovera J, Brown T, Cohen B, Neylan T, Henry R, et al. A randomized trial of stress management for the prevention of new brain lesions in MS. Neurology. 2012;79:412–419. doi: 10.1212/WNL.0b013e3182616ff9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motl RW, Sandroff BM. Benefits of exercise training in multiple sclerosis. Curr. Neurol. Neurosci. Rep. 2015;15:62. doi: 10.1007/s11910-015-0585-6. [DOI] [PubMed] [Google Scholar]
- Motl RW, Sandroff BM, Kwakkel G, Dalgas U, Feinstein A, Heesen C, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017;16:848–856. doi: 10.1016/S1474-4422(17)30281-8. [DOI] [PubMed] [Google Scholar]
- Palacios-Ceña D, Fernández-de-Las-Peñas C, Florencio LL, Palacios-Ceña M, de-la-Llave-Rincón AI. Future challenges for physical therapy during and after the COVID-19 Pandemic: A qualitative study on the experience of physical therapists in Spain. Int. J. Environ. Res. Public Health. 2021;18:8368. doi: 10.3390/ijerph18168368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pniak B, Leszczak J, Adamczyk M, Rusek W, Matłosz P, Guzik A. Occupational burnout among active physiotherapists working in clinical hospitals during the COVID-19 pandemic in south-eastern Poland. Work. 2021;68:285–295. doi: 10.3233/WOR-203375. [DOI] [PubMed] [Google Scholar]
- Prvu Bettger J, Thoumi A, Marquevich V, De Groote W, Rizzo Battistella L, Imamura M, et al. COVID-19: maintaining essential rehabilitation services across the care continuum. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Řasová K, Freeman J, Cattaneo D, Jonsdottir J, Baert I, Smedal T, et al. Content and Delivery of Physical Therapy in Multiple Sclerosis across Europe: A Survey. Int. J. Environ. Res. Public Health. 2020;17(3):886. doi: 10.3390/ijerph17030886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrig M. National MS Society; 2018. Physical Therapy in MS.https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_Physical-Therapy-in-MS-Rehabilitation.pdf Available from. [Google Scholar]
- Sahni PS, Singh K, Sharma N, Garg R. Yoga an effective strategy for self-management of stress-related problems and wellbeing during COVID19 lockdown: A cross-sectional study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0245214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solianik R, Mickevičienė D, Žlibinaitė L, Čekanauskaitė A. Tai chi improves psychoemotional state, cognition, and motor learning in older adults during the COVID-19 pandemic. Exp. Gerontol. 2021;150 doi: 10.1016/j.exger.2021.11363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor E, Taylor-Piliae RE. The effects of Tai Chi on physical and psychosocial function among persons with multiple sclerosis: A systematic review. Complement. Ther. Med. 2017;31:100–108. doi: 10.1016/j.ctim.2017.03.001. [DOI] [PubMed] [Google Scholar]
- Tiwari D, Naidoo K, Chatiwala N, Bartlo PL, Triola A, Ong B, et al. Exploratory analysis of physical therapy process of care and psychosocial impact of the COVID-19 pandemic on physical therapists. Phys. Ther. 2021;101:pzab088. doi: 10.1093/ptj/pzab088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UN News . UN News; March 19, 2020. Preventing discrimination against people with disabilities in COVID-19 response.https://news.un.org/en/story/2020/03/1059762 Available from. [Google Scholar]
- WHO coronavirus disease . World Health Organization; Geneva: 2020. (COVID-19) dashboard.https://covid19.who.int/ Available from. [Google Scholar]
- Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.