Abstract
Background:
Seasonal influenza vaccine uptake in China is low. This study aims to assess the role of community healthcare workers (HCWs) in increasing vaccination among high risk groups in China.
Methods:
We analyzed data from four knowledge, attitude and practice (KAP) studies on seasonal influenza vaccination in China targeting guardians of young children, pregnant women, adults aged ≥60 years, and HCWs from 2012 to 2014.
Results:
Thirty-one percent of pregnant women and 78% adults aged ≥60 years reported willingness to follow HCWs’ recommendations for influenza vaccination. Guardians were more likely to vaccinate their children if they received HCWs’ recommendations (35% vs. 17%, p < 0.001). Community HCWs were more likely to recommend seasonal influenza vaccination than hospital HCWs (58% vs. 28%, p < 0.001).
Conclusion:
Study results suggest the value of incorporating community HCWs’ recommendation for seasonal influenza vaccination into existing primary public health programs to increase vaccination coverage among high risk groups in China.
Keywords: Seasonal influenza vaccine, Vaccination, Healthcare worker, Community, KAP
1. Introduction
The World Health Organization and the Chinese Center for Disease Prevention and Control recommend seasonal influenza vaccine for groups at high risk for severe illness and complications from influenza infection, including pregnant women, young children, older adults and adults with chronic diseases [1,2]. In China, vaccine uptake within these groups remains low [3–5]. Numerous factors contribute to low coverage. First, the seasonal influenza vaccine is not included in the national Expanded Program on Immunization (EPI) [6], but is available upon request, most often at cost (10–15 USD). Second, misconceptions about influenza risk and vaccine safety and efficacy are common [7–9]. While inadequate supply may contribute to low vaccine uptake in other countries, in China, from 2004 to 2009, an average of 25% of influenza vaccine was returned to manufacturers unused [10].
While studies in developed countries have shown that HCWs’ recommendations promote seasonal influenza vaccination [11–13], few studies have addressed the HCW’s role with respect to vaccination in China [14]. HCWs’ willingness to recommend vaccination in China may be influenced by reports of patient mistrust, and patient-on-doctor violence [15,16]. Within this context, our study assessed whether community HCWs, who provide primary public health services [17], have a role in increasing influenza vaccine coverage among high risk groups in China.
2. Methods
From 2012 to 2014, the United States (US) Centers for Disease Control and Prevention supported four knowledge, attitude and practice (KAP) studies on influenza infection and vaccination in China. We analyzed vaccination coverage, factors influencing influenza vaccination, preferred sources for information, whether HCWs recommended vaccination, and willingness to follow HCWs’ recommendations.
From October 2012 to January 2013, we conducted two cross-sectional surveys in Suzhou among guardians of children aged 6 months to 3 years at three vaccination clinics, and pregnant women at four prenatal clinics. Trained staff conducted face-to-face interviews using structured questionnaires.
In December 2014, we conducted a cross-sectional survey among adults aged ≥60 years at three senior centers in Ningbo. Participants completed self-administered questionnaires, with support from trained study staff.
In November 2013 and May 2014, we conducted two cross-sectional surveys among HCWs in Qingdao, recruiting all HCWs providing direct patient care on investigation days at 10 healthcare institutions. We defined two groups: community HCWs were those who worked at community health centers providing primary health services. Hospital HCWs were those who worked at secondary and tertiary hospitals and focused on curative medicine. Enrolled HCWs completed self-administered questionnaires.
3. Ethics statement
Fudan University, Suzhou CDC, Ningbo CDC and the Health Development Research Center received local IRB approval for their site’s survey. All survey participants provided verbal consent.
4. Results
4.1. KAP among guardians of children aged 6 months to 3 years
Among responding guardians, 86/323 (27%) reported receiving a HCW’s recommendation for influenza vaccination and 70/317 (22%) reported that their child was vaccinated in the prior year. Guardians who reported receiving a HCW recommendation were more likely to vaccinate their child than those who did not (35% vs. 17%, p < 0.001). The main reported reasons for not vaccinating their child were concerns for vaccine safety (62%), not receiving a HCW’s recommendation (37%); believing vaccination was unnecessary (25%), and limited vaccine effectiveness (23%). Reported preferences for information about vaccines included television (64%), internet (57%) and educational leaflets (51%).
4.2. KAP among pregnant women
Among 1673 pregnant women interviewed, 4% reported receiving a HCW recommendation for influenza vaccination in the prior year. None reported receiving the vaccine during pregnancy, and none planned to get vaccinated in the current year. The most common reasons reported for not getting vaccinated included fear of harm to the fetus (83%), vaccine safety for the pregnant woman herself (28%), and believing vaccination was unnecessary (22%). Preferred sources for vaccine information included television (56%), internet (39%), and doctors (34%). Nearly one third (31%) stated they would get vaccinated if they received a HCW’s recommendation.
4.3. KAP among adults aged >60 years
Among 379 adults aged ≥60 years interviewed, 0.8% reported receiving the influenza vaccine in the prior year. The most common reasons for not getting vaccinated among those who responded (n = 268) were vaccination was unnecessary (33%), medical insurance did not pay for influenza vaccination (24%), and HCWs had not recommended vaccination (23%). Among all interviewed, 78% (296/379) reported willingness to get vaccinated if they received a HCW’s recommendation. Most (280/379, 74%) reported a preference for receiving health information from HCWs.
4.4. KAP among HCWs
Among 1852 HCWs approached, 1301 (70%) completed both surveys; among these, 17% were community HCWs.
Post-influenza season, 5% HCWs reported receiving influenza vaccination during the prior season. Main reasons for not getting vaccinated included concerns about vaccine safety (43%), perceiving vaccination as unnecessary (27%), having insufficient time for vaccination (24%), and believing the vaccine was ineffective (20%).
HCWs wanted to learn more about influenza disease severity (68%), populations most susceptible to influenza illness (52%), vaccine contraindications (72%), safety (72%) and effectiveness (71%). Preferred sources of information on vaccines included internet (76%), television/radio (75%), newspapers/books (55%), and colleagues (50%).
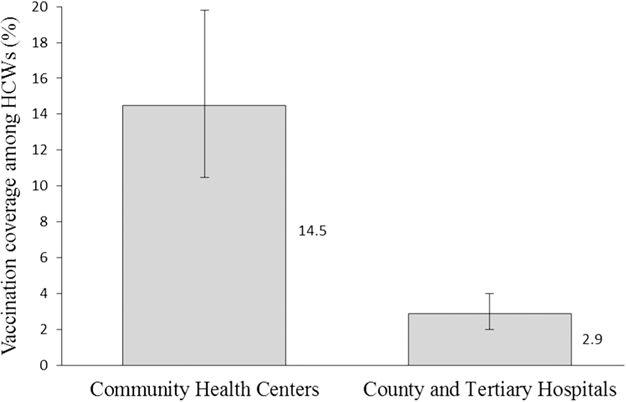
Among all 1301 HCWs, 8% reported always recommending influenza vaccination to patients during the prior influenza season. Community HCWs were more likely to be vaccinated than hospital HCWs (P < 0.01) (Fig. 1), and were also more likely to recommend vaccination to patients at least once in the prior season (58% vs. 28%, P < 0.001).
Fig. 1.
Proportion of healthcare workers vaccinated for seasonal influenza by hospital level, Qingdao, 2013–14 influenza season.
Seasonal influenza vaccination coverage and factors influencing vaccination among high risk groups and healthcare workers are summarized in Table 1.
Table 1.
Summary of seasonal influenza vaccination coverage and factors influencing seasonal influenza vaccination among four target populations: guardians of young children, pregnant women, adults aged 60 years and older and healthcare workers – China 2011–2014.
| Seasonal influenza vaccination factor | Guardians of children aged 6 months to 3 years n = 360 |
Pregnant women n = 1673 |
Adults ≥60 years of age n = 379 |
Healthcare workers n = 1301 |
|---|---|---|---|---|
|
| ||||
| Received seasonal influenza vaccine in past year | 22% (children vaccinated) (95% CI: 18–27%) | 0 (95% CI: < 0.2%) | 0.8% (95% CI: 0.3–2.3%) | 5% (95% CI: 4–6%) |
| Received HCWa recommendation for seasonal influenza vaccination in past year | 27% (95% CI: 23–32%) | 4% (95% CI: 2.8–4.6%) | Not asked | Not asked |
| Reported willingness to get vaccinated if HCW recommended vaccine | Not asked | 31% (95% CI: 29–33%) | 78% (95% CI: 74–82%) | N/A |
| Main barriers to vaccination reportedb | (1) Vaccine safety (62%) (2) No HCW recommendation (37%) (3) Vaccination not necessary (25%) (4) Limited vaccine effectiveness (23%) |
(1) Harm to fetus (83%) (2) Vaccine safety for pregnant women (28%) (3) Vaccination not necessary (22%) |
(1) Vaccination not necessary (33%) (2) Medical insurance does not cover influenza vaccine (24%) (3) No HCW recommendation (23%) (4) Vaccine safety (22%) |
(1) Vaccine safety (43%) (2) Vaccination not necessary (27%) (3) No time for vaccination (24%) (4) Limited vaccine effectiveness (20%) |
| Preferred resources for receiving vaccine information | (1) TV (64%) (2) Internet (57%) (3) Educational leaflets (51%) |
(1) TV (56%) (2) Internet (39%) (3) HCWs (34%) |
(1) HCWs (74%) (2) Community health lecture (41%) (3) TV/Radio (24%) (4) Friends/Family member (24%) |
(1) Internet (76%) (2) TV/Radio (75%) (3) Newspapers/books (55%) (4) Colleagues (50%) |
HCW – Healthcare worker.
Cost and poor access were listed as options for main barriers to vaccination in the surveys to guardians, adults aged 60 years and older and HCWs, however only adults 60 years and older listed cost as one of the main barriers to vaccination. In 2014, the average cost of the seasonal influenza vaccine in China was 10–15 USD. Cost and access were not included as options in the vaccine barrier question to pregnant women.
5. Discussion
5.1. High risk groups in China cited similar reasons for not getting vaccinated for seasonal influenza, and all had suboptimal influenza vaccination coverage
A common barrier to vaccination was concern about vaccine safety. Another common barrier was perceiving vaccination as unnecessary (22–33%); 23% guardians also cited low vaccine effectiveness as a barrier. These findings, in addition to the low seasonal influenza vaccine coverage among children less than 3 years of age and adults aged ≥60 years, are consistent with prior studies conducted in China [4,5,7–9]. We also found minimal coverage among HCWs (5%) and none among pregnant women.
5.2. High risk groups reported willingness to follow HCWs' advice for vaccination, and HCWs' recommendations were associated with increased coverage
More than a third of pregnant women and three quarters of adults aged ≥60 years reported wanting to receive information from HCWs regarding vaccination. Further, 31% pregnant women and 78% adults aged ≥60 years stated they would get vaccinated if a HCW recommended vaccination. Similarly, 37% guardians listed not receiving a HCW’s recommendation as a main barrier to vaccination, and guardians who received a HCW recommendation were more likely to vaccinate their child. These findings are consistent with studies in the US and China [11–14,18], in which high risk groups expressed trust in their physician, whose recommendation was a strong determinant of influenza immunization uptake.
5.3. Community HCWs may offer a practical way to increase seasonal influenza vaccine uptake among high risk groups in China
Only 8% HCWs in Qingdao reported always recommending influenza vaccination, and only 4% pregnant women and 27% guardians of young children reported receiving a HCW’s recommendation for influenza vaccination in the prior year.
Several factors may prevent HCWs in China from routinely recommending influenza vaccination. First, in our study, HCWs themselves were not vaccinated due to concerns about vaccine safety, effectiveness, and perceiving vaccination as unnecessary. HCWs may also avoid recommending optional vaccines not included in EPI, such as influenza vaccine, to decrease risk of being held liable for adverse events.
Most HCWs, however, expressed interest in learning about vaccine contraindications, safety and effectiveness. As one Australian study found, improving HCWs’ knowledge in influenza infection and vaccination may increase the likelihood of their recommending influenza vaccine [19].
China’s health system may impact which HCWs are more likely to incorporate vaccine recommendations into their routine work. Community HCWs provide primary healthcare, disease prevention and health education, which target pregnant women, young children, older adults and adults with chronic diseases residing in the community [17]. Influenza vaccination services are usually offered at EPI clinics, which, in China, are most often located in community health centers. Therefore, when high risk groups receive recommendations from community HCWs, they have immediate access to on-site immunization. Although most HCWs in China do not routinely recommend seasonal influenza vaccination, we found that community HCWs were more likely than hospital HCWs to recommend vaccination and to get vaccinated themselves. These findings are consistent with studies conducted in the US and Australia [19,20].
6. Limitations
Our studies have several limitations. First, the convenient samples of high risk groups surveyed may not adequately represent these populations in the community. Second, vaccination status was self-reported and not verified through records. Finally, this study discusses just one component of what should become a multi-pronged strategy to increase seasonal influenza vaccination.
7. Recommendations
Our results suggest the utility of the following steps: (1) providing community HCWs with accurate information about influenza infection and seasonal influenza vaccination to ensure the knowledge required to make effective recommendations; (2) promoting annual influenza vaccination among community HCWs themselves; and (3) incorporating community HCWs’ recommendation for seasonal influenza vaccination into existing immunization, maternal healthcare, and chronic disease management programs in China.
Acknowledgements
We thank all counterparts who participated in the implementation of the four KAP studies. We also thank those who contributed to study design, including Luzhao Feng, Jiandong Zheng, Jeffrey McFarland, Mei Shang, Danielle Iuliano, and Mark Thompson. In addition, we acknowledge Lance Rodewald for his review of this manuscript.
Funding
This work was supported by the Cooperative Agreement Number 1U2GGH000961, funded by the Centers for Disease Control and Prevention. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Conflict of interest
None.
References
- [1].World Health Organization. Vaccines against influenza. WHO position paper November 2012 (WHO, November 23 2012). WHO. [Google Scholar]
- [2].Feng L, Yang P, Zhang T, et al. Technical guidelines for the application of seasonal influenza vaccine in China (2014–2015). Hum Immunother 2015;11 (8):2077–101. 10.1080/21645515.2015.1027470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Chen L, Zhang J, Zu R, et al. Knowledge, attitudes and practices toward influenza among pregnant women: a cross-sectional survey in Suzhou, China. Options for the Control of Influenza VIII Abstract Book, 99; 2013 [Google Scholar]
- [4].Yu J, Wang ZG, Kang GD, et al. Survey on immunization status of category B vaccines among children in Jiangsu province. Jiangsu J Prev Med 2016;27 (2):153–5. [Google Scholar]
- [5].Zhou L, Su Q, Xu Z, et al. Seasonal influenza vaccination coverage rate of target groups in selected cities and provinces in China by season (2009/10 to 2011/12). Plos ONE 2013;8(9):e73724. 10.1371/journal.pone.0073724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Web version only, available at www.gov.cn/zhengce/content/2016-04/25/content_5067597.htm (Chinese). National Regulation for Vaccine Distribution and Administration (2016 version) [accessed 25 April 2017].
- [7].Wang J, Luo FJ, Ma JX, et al. Factors influencing pregnant women’s willingness to get influenza vaccine in Chaoyang District Women and Children Hospital (Chinese). CHIN J Vac Imm 2015;21(4):422–7. [Google Scholar]
- [8].Xiao HJ, Xu Y, Lin B, et al. Influenza vaccine uptake rate and influenza factors among children 6–59 months of age. J Nurs (Chinese) 2009;16(5A):13–5. [Google Scholar]
- [9].Chen QX, Nie YZ, Zhang JX, et al. Influential factors of influenza vaccination among the elderly in Foshan City (Chinses). Modern Preventive Med 2010;37 (11):2047–51. [Google Scholar]
- [10].Feng L, Mounts AW, Feng Y, et al. Seasonal influenza vaccine supply and target vaccinated population in China. 2004–2009. Vaccine. 2010;28(41):6778–82. 10.1016/j.vaccine.2010.07.064. [DOI] [PubMed] [Google Scholar]
- [11].Ding H, Black C, Ball S, et al. Influenza vaccination coverage among pregnant women — United States, 2014–15 Influenza Season. MMWR 2015;64 (36):1000–5. 10.15585/mmwr.mm6436a2. [DOI] [PubMed] [Google Scholar]
- [12].Hemingway CO, Poehling KA. Change in recommendation affects influenza vaccinations among children 6–59 months of age. Pediatrics 2004;114 (4):948–52. 10.1542/peds.2003-0509-F. [DOI] [PubMed] [Google Scholar]
- [13].Santibanez TA, Mootrey GT, Euler GL, et al. Behavior and beliefs about influenza vaccine among adults aged 50–64 years. Am. J. Health Behav. 2010. Jan-Feb;34(1):77–89. [DOI] [PubMed] [Google Scholar]
- [14].Wagner AL, Montgomery JP, Xu W, et al. Influenza Vaccination of adults with and without high-risk health conditions in China. J Public Health (Oxf) 2017;39(2):358–65. 10.1093/pubmed/fdw041. [DOI] [PubMed] [Google Scholar]
- [15].Tucker JD, Cheng Y, Wong B, et al. Patient-physician mistrust and violence against physicians in Guangdong Province, China: a qualitative study. BMJ Open 2015;5(10):e008221. 10.1136/bmjopen-2015-008221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wu D, Wang Y, Lam KF, et al. Health system reforms, violence against doctors and job satisfaction in the medical profession: a cross-sectional survey in Zhejiang Province, Eastern China. BMJ Open 2014;4(12):e006431. 10.1136/bmjopen-2014-006431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Web version only, available at www.gov.cn/zhengce/content/2016-04/25/content_5067597.htm. (Chinese) National Regulation for Vaccine Distribution and Administration (2016 version) [accessed 25 April 2017].
- [18].Shavell VI, Moniz MH, Conik B, et al. Influenza immunization in pregnancy: overcoming patient and health care provider barrier. Am J Obstet Gynecol 2012;207(3 suppl):S67–74. 10.1016/j.ajog.2012.06.077. [DOI] [PubMed] [Google Scholar]
- [19].Ridda I, Lindley IR, Gao Z, et al. Difference in attitudes, beliefs and knowledge of hospital health care workers and community doctors to vaccination of older people. Vaccine 2008;26(44):5633–40. 10.1016/j.vaccine.2008.07.070. [DOI] [PubMed] [Google Scholar]
- [20].Nichol KL, Zimmerman R. Generalist and subspecialist physicians’ knowledge, attitudes, and practices regarding influenza and pneumococcal vaccinations for elderly and other high-risk patients: a nationwide survey. Arch Intern Med 2001;161(22):2702–8. [DOI] [PubMed] [Google Scholar]