CURRENT STATE OF THE PROBLEM:WHERE WE ARE NOW
Oral management is an important, yet often neglected, part of rehabilitation medicine. Oral problems and poor oral health affect the decline in oral function resulting from aging and disease, lifestyle-related oral diseases, and frailty.1) Furthermore, the quality of life related to oral hygiene among nursing home residents in Germany was found to be significantly impaired.2) In recent years, as interest in oral management as part of rehabilitation has increased, new concepts, such as oral frailty,3) oral sarcopenia,4) and hospital-related oral problems,5) have been proposed.
Oral health problems are frequently observed in rehabilitation practice. Poor oral health is common among hospitalized patients, especially in malnourished older adults and in those with physical disabilities or cognitive impairment.6,7) More than 80% of hospitalized older patients experience oral hygiene problems.6,7) Furthermore, 71% of hospitalized rehabilitation patients and 91% of hospitalized acute care patients have impaired oral hygiene.1) The deterioration of oral health status in hospitalized older patients can be attributed to a variety of factors, including age, physical dependence, cognitive decline, malnutrition, sarcopenia, and multimorbidities.1) Another important factor is the lack of both knowledge and interest in oral health problems among healthcare professionals.
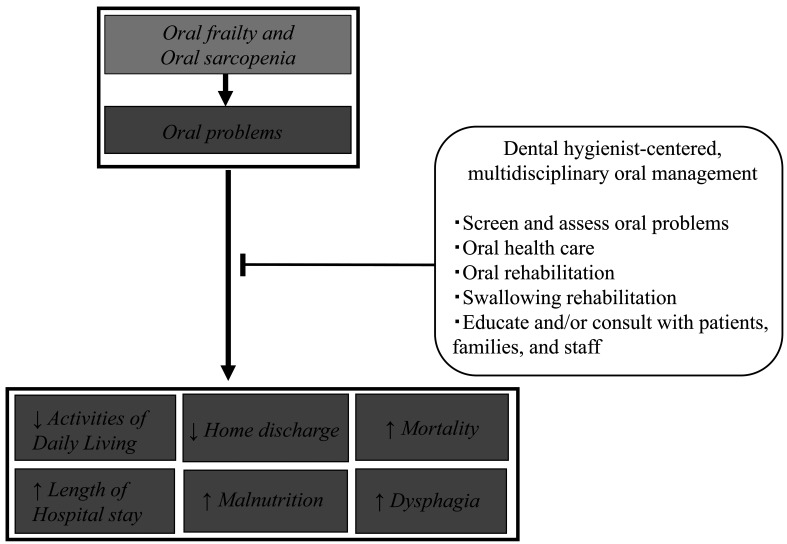
Oral problems have a negative impact on rehabilitation outcomes. Among inpatients undergoing convalescent rehabilitation, oral problems were independently associated with activities of daily living (ADLs), length of stay, home discharge, and in-hospital mortality after adjusting for age, sex, disease severity, nutritional status, comorbidities, and physical and cognitive dependence.6,7) Therefore, early detection of oral problems, treatment by dental professionals, education on oral management for non-dental professionals such as nurses and other medical staff, multidisciplinary oral rehabilitation, and medical and dental collaboration are essential.
DIRECTION TO AIM FOR:WHERE WE SHOULD GO
Because of the frequent occurrence of oral problems and their negative impact on health outcomes, oral management is crucial in the daily clinical practice of rehabilitation medicine. Furthermore, oral management is especially important in convalescent rehabilitation wards to increase physical independence and to facilitate discharge home. This applies particularly to patients post-stroke or post-hip fracture, the number of which is increasing with the aging population. Multidisciplinary oral management in convalescent rehabilitation wards should include oral rehabilitation, oral care, oral health promotion and education, medical and dental collaboration, and the assignment of a dental hygienist (DH) to the ward.
Oral rehabilitation is the rehabilitation of oral function and has been shown to improve quality of life.8) Oral exercise programs that focus on strengthening chewing, salivation, and swallowing effectively improve oral function.9) Prosthetic rehabilitation improves oral health-related quality of life, oral–facial esthetics, and masticatory function.10) Moreover, oral function training combined with nutritional supplements improves the nutritional status of malnourished older patients in nursing homes.11) Resistance training of the tongue improves tongue pressure and swallowing function in patients after stroke.9) Other exercises such as jaw opening, self-training of oral function, and Shaker exercises improve swallowing function and reduce aspiration pneumonia.1) Oral health promotion and education have a beneficial impact on patients with oral problems. A 3-month oral function promotion program improved oral function and oral hygiene-related quality of life in older adults.12)
Medical and dental collaboration is important for rehabilitation. Perioperative oral function management by dental staff can reduce the risk of postoperative pneumonia and is covered by health insurance in Japan. Collaboration between dentists and non-dental healthcare providers may improve oral health outcomes for people with limited access to oral healthcare services. Convalescent rehabilitation wards generally do not include full-time dentists, but it is possible to work with local dental associations to have dentists dispatched from nearby dental clinics to provide inpatient oral management. However, in rehabilitation medicine, there is insufficient knowledge and interest in medical–dental collaboration and oral health management. Dentists tend to focus on the diagnosis and treatment of oral diseases and overlook general health issues. Correspondingly, physicians, nurses, and rehabilitation therapists tend not to address the oral health problems of their patients. Therefore, there is an urgent need to educate rehabilitation medical professionals on the importance of oral health care.
HOW TO GET THERE: THE EXPECTEDROLE OF DENTAL HYGIENISTS INCONVALESCENT REHABILITATION
Given the increasing need for oral health management in rehabilitation medicine, it is important for DHs to be actively involved in convalescent rehabilitation. DHs are qualified oral healthcare professionals and play a central role in rehabilitation collaboration. The roles of DHs in convalescent rehabilitation include screening and assessment of oral health and function; provision of oral health care; oral and swallowing rehabilitation; treatment in inter-professional collaboration; and patient, family, and staff education and counseling (Fig. 1).1) According to a recent study published in Japan on patients in convalescent rehabilitation wards, oral health care by DHs improves not only oral status, swallowing function, and nutritional status but also ADLs, home discharge rates, and in-hospital mortality.13,14) Furthermore, in stroke patients with oral problems at the time of admission, improvement of oral problems during hospitalization in convalescent rehabilitation wards was independently and positively associated with improvement in ADLs and dysphagia.15)
Fig. 1.
Dental hygienist-centered multidisciplinary oral management and the expected outcomes for patients with oral frailty, oral sarcopenia, and oral problems.
Based on these findings, early detection of oral problems, early oral hygiene management by dentists and DHs, and medical and dental cooperation are necessary for convalescent rehabilitation. Therefore, DHs are essential for promoting oral health management in convalescent rehabilitation wards through multidisciplinary cooperation. However, at present, there is no reimbursement for the assignment of DHs to convalescent rehabilitation wards in Japan. We hope that, in the future, reimbursement for the assignment of DHs to these wards will improve the quality of multidisciplinary oral management in convalescent rehabilitation, which will surely contribute to maximizing the improvement of patient outcomes.
Footnotes
CONFLICTS OF INTEREST: The authors report no conflicts of interest
REFERENCES
- 1.Shiraishi A,Wakabayashi H,Yoshimura Y: Oral management in rehabilitation medicine: oral frailty, oral sarcopenia, and hospital-associated oral problems. J Nutr Health Aging 2020;24:1094–1099. 10.1007/s12603-020-1439-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klotz AL,Hassel AJ,Schröder J,Rammelsberg P,Zenthöfer A: Oral health-related quality of life and prosthetic status of nursing home residents with or without dementia. Clin Interv Aging 2017;12:659–665. 10.2147/CIA.S125128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanaka T,Takahashi K,Hirano H,Kikutani T,Watanabe Y,Ohara Y,Furuya H,Tetsuo T,Akishita M,Iijima K: Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci 2018;73:1661–1667. 10.1093/gerona/glx225 [DOI] [PubMed] [Google Scholar]
- 4.Shiraishi A,Yoshimura Y,Wakabayashi H,Tsuji Y. Prevalence of stroke-related sarcopenia and its association with poor oral status in post-acute stroke patients: implications for oral sarcopenia. Clin Nutr 2018;37:204–207. [DOI] [PubMed]
- 5.Terezakis E,Needleman I,Kumar N,Moles D,Agudo E: The impact of hospitalization on oral health: a systematic review. J Clin Periodontol 2011;38:628–636. 10.1111/j.1600-051X.2011.01727.x [DOI] [PubMed] [Google Scholar]
- 6.Shiraishi A,Yoshimura Y,Wakabayashi H,Tsuji Y: Poor oral status is associated with rehabilitation outcome in older people. Geriatr Gerontol Int 2017;17:598–604. 10.1111/ggi.12763 [DOI] [PubMed] [Google Scholar]
- 7.Shiraishi A,Yoshimura Y,Wakabayashi H,Tsuji Y,Shimazu S,Jeong S: Impaired oral health status on admission is associated with poor clinical outcomes in post-acute inpatients: a prospective cohort study. Clin Nutr 2019;38:2677–2683. 10.1016/j.clnu.2018.11.020 [DOI] [PubMed] [Google Scholar]
- 8.McKenna G,Allen PF,Hayes M,DaMata C,Moore C,Cronin M: Impact of oral rehabilitation on the quality of life of partially dentate elders in a randomized controlled clinical trial: 2 year follow-up. PLoS One 2018;13:e0203349. 10.1371/journal.pone.0203349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim HJ,Lee JY,Lee ES,Jung HJ,Ahn HJ,Kim BI: Improvements in oral functions of elderly after simple oral exercise. Clin Interv Aging 2019;14:915–924. 10.2147/CIA.S205236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peršić S,Čelebić A: Influence of different prosthodontic rehabilitation options on oral health-related quality of life, orofacial esthetics and chewing function based on patient-reported outcomes. Qual Life Res 2015;24:919–926. 10.1007/s11136-014-0817-2 [DOI] [PubMed] [Google Scholar]
- 11.Kikutani T,Enomoto R,Tamura F,Oyaizu K,Suzuki A,Inaba S: Effects of oral functional training for nutritional improvement in Japanese older people requiring long-term care. Gerodontology 2006;23:93–98. 10.1111/j.1741-2358.2006.00104.x [DOI] [PubMed] [Google Scholar]
- 12.Cho EP,Hwang SJ,Clovis JB,Lee TY,Paik DI,Hwang YS: Enhancing the quality of life in elderly women through a programme to improve the condition of salivary hypofunction. Gerodontology 2012;29:e972–e980. 10.1111/j.1741-2358.2011.00594.x [DOI] [PubMed] [Google Scholar]
- 13.Shiraishi A,Yoshimura Y,Wakabayashi H,Tsuji Y,Yamaga M,Koga H: Hospital dental hygienist intervention improves activities of daily living, home discharge and mortality in post-acute rehabilitation. Geriatr Gerontol Int 2019;19:189–196. http://www.ncbi.nlm.nih.gov/pubmed/30517977 10.1111/ggi.13583 [DOI] [PubMed] [Google Scholar]
- 14.Suzuki R,Nagano A,Wakabayashi H,Maeda K,Nishioka S,Takahashi M,Momosaki R: Assignment of dental hygienists improves outcomes in Japanese rehabilitation wards: a retrospective cohort study. J Nutr Health Aging 2020;24:28–36. 10.1007/s12603-019-1284-9 [DOI] [PubMed] [Google Scholar]
- 15.Shiraishi A,Yoshimura Y,Wakabayashi H,Nagano F,Bise T,Shimazu S: Improvement in oral health enhances the recovery of activities of daily living and dysphagia after stroke. J Stroke Cerebrovasc Dis 2021;30:105961. 10.1016/j.jstrokecerebrovasdis.2021.105961 [DOI] [PubMed] [Google Scholar]