Abstract
Objective
To investigate how trends in incidence of anxiety and depressive disorders have been affected by the COVID-19 pandemic.
Design
Population-based cohort study.
Setting
Retrospective cohort study from 2018 to 2021 using the Information System for Research in Primary Care (SIDIAP) database in Catalonia, Spain.
Participants
3 640 204 individuals aged 18 or older in SIDIAP on 1 March 2018 with no history of anxiety and depressive disorders.
Primary and secondary outcomes measures
The incidence of anxiety and depressive disorders during the prelockdown period (March 2018–February 2020), lockdown period (March–June 2020) and postlockdown period (July 2020–March 2021) was calculated. Forecasted rates over the COVID-19 periods were estimated using negative binomial regression models based on prelockdown data. The percentage of reduction was estimated by comparing forecasted versus observed events, overall and by sex, age and socioeconomic status.
Results
The incidence rates per 100 000 person-months of anxiety and depressive disorders were 151.1 (95% CI 150.3 to 152.0) and 32.3 (31.9 to 32.6), respectively, during the prelockdown period. We observed an increase of 37.1% (95% prediction interval 25.5 to 50.2) in incident anxiety diagnoses compared with the expected in March 2020, followed by a reduction of 15.8% (7.3 to 23.5) during the postlockdown period. A reduction in incident depressive disorders occurred during the lockdown and postlockdown periods (45.6% (39.2 to 51.0) and 22.0% (12.6 to 30.1), respectively). Reductions were higher among women during the lockdown period, adults aged 18–34 years and individuals living in the most deprived areas.
Conclusions
The COVID-19 pandemic in Catalonia was associated with an initial increase in anxiety disorders diagnosed in primary care but a reduction in cases as the pandemic continued. Diagnoses of depressive disorders were lower than expected throughout the pandemic.
Keywords: COVID-19, primary care, epidemiology, anxiety disorders, depression & mood disorders
Strengths and limitations of this study.
This study was based on primary care data of 3.6 million people in Catalonia, Spain.
This study has quantified the impact of the COVID-19 pandemic on trends in incidence of anxiety and depressive disorders among adults living in Catalonia, Spain and how it differs by sex, age and socioeconomic status.
Forecasted rates were estimated based on data from 2 years and we validated our modelling approach in the year prior to the COVID-19 pandemic.
Our analysis investigates the COVID-19-related effects up to March 2021, providing data up to a year after the onset of the lockdown measures in Catalonia.
Introduction
The outbreak of the COVID-19 pandemic and the associated control measures have impacted many aspects of people’s lives. In Spain, a national lockdown was implemented on 14 March 2020, limiting mobility with few exceptions such as grocery shopping, health emergencies or essential work.1 The restrictions were gradually lifted following different de-escalation phases, which ended on 21 June 2020, when the so-called ‘new normality’ was re-established.2 Due to a resurgence of COVID-19 infections, new nationwide measures were implemented on 25 October 2020, including mobility restrictions and curfew hours, which were extended up to 9 May 2021.3
Studies based on self-reported surveys have provided evidence of elevated rates of anxiety, depression and stress in the initial stages of the pandemic.4–7 In Catalonia (a northern region in Spain), self-reported surveys performed in April–May 2020 found increased levels of anxiety and depression during the COVID-19 lockdown, especially among women and young adults.8 9 Conversely, healthcare contacts related to mental conditions substantially reduced in primary care, emergency departments and hospital settings after the lockdown announcement in March 2020.10 A discrepancy between increasing levels of mental health disorders and reductions in primary care diagnoses during the COVID-19 pandemic may well result in a substantial burden of ill health, as long delays in diagnosis are associated with negative health outcomes among adults with mood and/or anxiety disorders.11 12
To date, most evidence regarding the mental health impact of COVID-19 is from self-reported surveys performed during the initial stages of the pandemic. We do not know yet whether the survey results are mirrored in the rates of recorded incident diagnoses of common mental disorders in primary care and how they have evolved during the pandemic in Catalonia. The effects of the pandemic on mental health and well-being may well persist beyond lockdown measures, causing a long-term upsurge in number and severity of mental health problems as the pandemic continues.13 14 In this study, we aim to investigate how trends in incidence of anxiety and depressive disorders have been affected by the various stages of the COVID-19 pandemic 1 year after the onset of lockdown measures through analysis of a large primary care longitudinal dataset representative of the population living in Catalonia, Spain.
Methods
Study design
We conducted a cohort study based on primary care records from 1 March 2018 to 31 March 2021 in Catalonia, Spain. Time trends were assessed in three different periods: (1) the prelockdown period, from 1 March 2018 to 29 February 2020; (2) the lockdown period, from 1 March 2020 to 30 June 2020; and (3) the postlockdown period, from 1 July 2020 to 31 March 2021. The postlockdown period was divided into three trimesters, which were broadly aligned with the different stages of the pandemic in Catalonia: (1) easing of restrictions from 1 July 2020 to 30 September 2020; (2) implementation of new control measures from 1 October 2020 to 31 December 2020; and (3) extension of control measures and start of the vaccination campaign from 1 January 2021 to 31 March 2021. Of note, we only considered the first wave of the pandemic as the lockdown period, as it was the only wave in which a stay-at-home order was issued. Various restrictions continued to be imposed following this initial, strict lockdown.
Study participants, setting and data source
We used individual-level data from the Information System for Research in Primary Care (SIDIAP; www.sidiap.org) database, which is comprised of pseudo-anonymised electronic health records from approximately 80% of the population living in Catalonia. SIDIAP has been shown to be representative of the Catalan population in terms of geography, age and sex distributions.15 The database has been mapped to the Observational Medical Outcomes Partnership Common Data Model.16
All individuals aged 18 or older registered in the SIDIAP on 1 March 2018 were identified. Individuals with less than 1 year of history available were excluded so that the study participants had sufficient prior observation time to detect incident cases of anxiety and depressive disorders. Individuals with episodes of anxiety or depressive disorders prior to index date (ie, date of start of the cohort) were excluded. Individuals were observed until the event of interest, until they were transferred or died, or until the end of the study period.
Variables
Individuals’ age and sex were extracted. Information on socioeconomic status (SES) was available through the Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales (MEDEA) Deprivation Index, linked to each residential census area of the population.17 The deprivation index was only available for urban areas, defined as municipalities with more than 10 000 inhabitants and a population density greater than 150 habitants/km2; the remaining areas were considered rural areas. The deprivation index is categorised in quintiles, in which the first and fifth quintiles are the least and most deprived, respectively.
The outcome of the study was the incidence of anxiety or depressive disorders. Conditions were identified on the basis of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Clinical Modification (ICD-10-CM) codes of interest. The ICD-10-CM codes included for depressive disorders were F32 (major depressive disorder, single episode) and F33 (major depressive disorder, recurrent). All descendants were included except for the ones referring to episodes in partial or complete remission (F32.4, F32.5 and F33.4). For anxiety disorder, the F41 (other anxiety disorders) code and all its descendants were included. Detailed data of the ICD-10-CM codes included for each outcome are described in online supplemental table 1.
bmjopen-2021-057866supp001.pdf (698.3KB, pdf)
Statistical methods
We summarised the sociodemographic characteristics of the individuals included in the study, with counts and percentages for categorical variables and median and interquartile range (IQR) for continuous variables. We structured the data in a monthly time-series format with incident and person-months at risk aggregated with stratification by sex (men and women), age group (18–34, 35–64, >65 years) and SES (quintiles of MEDEA Deprivation Index). Incidence rates with 95% CI were calculated for each month and study period by dividing the number of first recorded cases of anxiety and depression by 100 000 person-months at risk, overall and stratified by sex, age group and SES. Incidence rate ratios (IRR) with 95% CI were calculated to compare the differences in the incidence of each strata of the population during the lockdown and postlockdown periods compared with the corresponding periods from March 2018 to March 2019.
We used negative binomial regression models to estimate the expected monthly incident cases from March 2020 to March 2021 using data collected in the prelockdown period. To account for possible seasonality and linear trends, we fitted calendar month as a categorical variable and time as a continuous variable. The number of months since the start of the study was considered as the unit of measurement for time.
The estimated number of underdiagnoses was calculated by subtracting the number of observed from the expected diagnoses. Reduction in diagnoses was calculated by dividing the number of underdiagnoses by the expected diagnoses and was estimated monthly and by study period (lockdown and postlockdown, overall and divided by trimesters). Reduction in diagnoses is expressed as percentage with 95% prediction interval (PI),18 as previously reported in a similar study.19
For each month during the COVID-19 study period, observed and expected incident counts were converted to rates using the observed person-month denominator. We plotted monthly expected rates and the corresponding 95% PI against the observed rates.
To validate our modelling approach, we developed a negative binomial model based on 2 years of history (from March 2017 to February 2019). We forecasted our expected values from March 2019 to February 2020, and checked if the values predicted from the model fell within the calculated 95% PI. We validated our approach for overall diagnoses and stratified by sex, age group and SES.
The SIDIAP version used for this analysis was from 15 June 2021. All analyses were performed in R V.4.0.4.
Patient and public involvement
This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Results
There were 5 811 652 adults registered in our data set on 1 March 2018 who were eligible to enter the study. We excluded 1 044 705 due to not being 18 years old; 87 740 due to having less than a year of clinical history; and 1 039 003 due to history of anxiety or depression disorders (online supplemental figure 1). We included 3 640 204 individuals, of whom 1 709 659 (47.0%) were women. The median age of the individuals on the index date was 47 years (IQR 35–63). A total of 310 546 (8.5%) individuals were lost to follow-up at the end of the study period. Detailed demographic data of the study population are included in online supplemental table 2.
Incidence trends
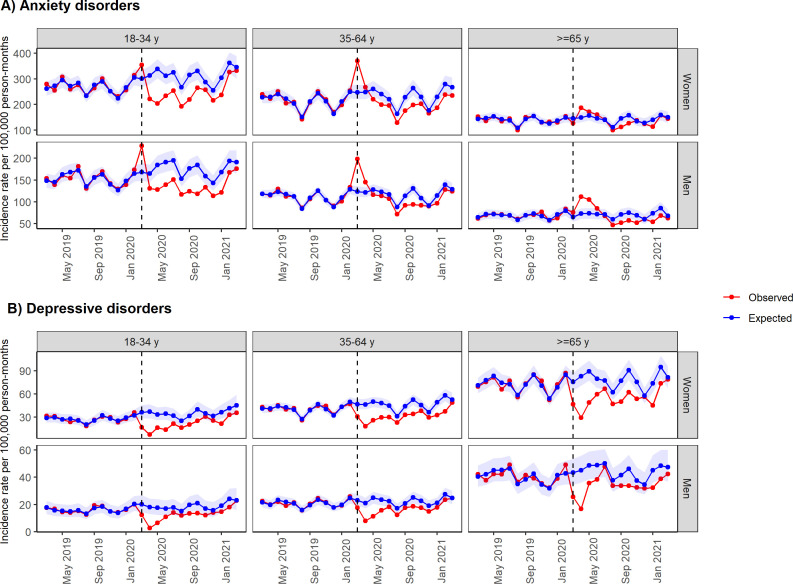
During the prelockdown period, the overall incidence rate per 100 000 person-months of anxiety or depressive disorders was 151.1 (95% CI 150.3 to 152.0) and 32.3 (31.9 to 32.6), respectively. During the lockdown period, the incidence rate of anxiety disorders increased up to 183.3 per 100 000 person-months (181.0 to 185.6), whereas the rate of depressive disorders sharply decreased to 21.1 per 100 000 person-months (20.4 to 21.9). The incidence rate of anxiety disorders substantially reduced from July to September 2020 (127.6 per 100 000 person-months (125.4 to 129.9)), but subsequently increased and exceeded the figures observed before the pandemic during the first trimester of 2021 (162.3 per 100 000 person-months (159.7 to 164.9)). Quarterly incidence rates (consisting of intervals of 3 months) of depressive disorders progressively recovered after the lockdown period and achieved the observed figures prior to the pandemic during the first trimester of 2021 (33.2 per 100 000 person-months (32.1 to 34.4)) (figure 1). To note, some data on quarterly incidence rates have been omitted in order to ensure the readability of the manuscript. Detailed data of incidence rates overall and stratified by sex, age group, and SES over the study periods are included in online supplemental tables 3–8.
Figure 1.
Expected and observed incidence rates of (A) anxiety and (B) depressive disorders in primary care in Catalonia (March 2018–March 2021). Points indicate monthly incidence rates of anxiety and depressive disorders. The number of expected cases (95% PI) was estimated with negative binomial models using data from 1 March 2018 to 29 February 2020. Shaded areas in blue represent 95% PI. The vertical lines show 1 March 2020. PI, prediction interval.
The IRRs comparing the differences in incidence of each strata of the population during the lockdown and postlockdown periods compared with the corresponding periods in 2018 and 2019 are shown in table 1. The IRRs of anxiety disorders were significantly higher during the lockdown period for all age groups and deprivation quintiles (ie, IRR range from 1.06 (1.01 to 1.11) to 1.38 (1.27 to 1.49) across sex and age groups) but reduced during the following trimester (ie, IRR range from 0.87 (0.78 to 0.97) to 0.97 (0.91 to 1.04) across sex and age groups). The incidence rates during the three trimesters of the postlockdown period were similar to those observed in the corresponding periods in 2018 and 2019 for all strata, with a few exceptions. Women aged 18–34 years obtained a significantly higher IRR during the last trimester of 2020 (1.14 (1.08 to 1.20)), whereas both women and men of the same age group obtained significantly higher IRRs from January to March 2021 compared with the corresponding period in 2019 (1.14 (1.08 to 1.19) and 1.07 (1.00 to 1.14), respectively). Significant reductions in the diagnosis of depressive disorders were found for all strata during the lockdown period (ie, IRR range from 0.58 (0.47 to 0.71) to 0.70 (0.64 to 0.76) across sex and age groups). These reductions were particularly pronounced among individuals aged 65 years or above (0.61 (0.56 to 0.67) in women and 0.69 (0.61 to 0.78) in men) and those living in the most deprived urban areas (0.55 (0.48 to 0.62)). The IRRs of depressive disorders increased during the following trimester and suggested no difference in risk from October 2020 to March 2021 compared with the corresponding period in 2018 and 2019.
Table 1.
Incidence rate ratios of the first recorded cases of anxiety and depressive disorders stratified by sex, age group, and MEDEA Deprivation Index according to the study period
| Incidence rate ratio (95% CI) for each time period | ||||||||
| Anxiety disorders (n=196 933)* | Depressive disorders (n=40 020)* | |||||||
| Lockdown period (March–June 2020) | Postlockdown period 1 (July–September 2020) | Postlockdown period 2 (October–December 2020) | Postlockdown period 3 (January–March 2021) | Lockdown period (March–June 2020) | Postlockdown period 1 (July–September 2020) | Postlockdown period 2 (October–December 2020) | Postlockdown period 3 (January–March 2021) | |
| Overall | 1.19 (1.17 to 1.22) | 0.94 (0.92 to 0.96) | 1.00 (0.98 to 1.03) | 1.00 (0.98 to 1.03) | 0.64 (0.61 to 0.67) | 0.94 (0.89 to 0.99) | 0.95 (0.90 to 1.00) | 0.97 (0.93 to 1.02) |
| Sex | ||||||||
| Women | 1.17 (1.14 to 1.20) | 0.95 (0.92 to 0.97) | 1.05 (1.02 to 1.08) | 1.01 (0.98 to 1.04) | 0.64 (0.61 to 0.68) | 0.91 (0.85 to 0.97) | 0.97 (0.91 to 1.04) | 0.95 (0.89 to 1.01) |
| Men | 1.24 (1.20 to 1.27) | 0.94 (0.90 to 0.97) | 0.94 (0.91 to 0.98) | 1.00 (0.96 to 1.03) | 0.64 (0.59 to 0.69) | 1.00 (0.92 to 1.08) | 0.92 (0.84 to 1.00) | 1.01 (0.93 to 1.09) |
| Sex: women | ||||||||
| Age group (years) | ||||||||
| 18–34 | 1.06 (1.01 to 1.11) | 0.94 (0.89 to 1.00) | 1.14 (1.08 to 1.20) | 1.14 (1.08 to 1.19) | 0.60 (0.51 to 0.71) | 1.01 (0.84 to 1.21) | 1.17 (0.99 to 1.38) | 1.12 (0.96 to 1.31) |
| 35–64 | 1.25 (1.21 to 1.29) | 0.95 (0.91 to 0.99) | 1.02 (0.98 to 1.07) | 0.97 (0.93 to 1.00) | 0.70 (0.64 to 0.76) | 0.93 (0.84 to 1.02) | 0.99 (0.90 to 1.09) | 0.92 (0.85 to 1.01) |
| >65 | 1.10 (1.04 to 1.17) | 0.94 (0.87 to 1.01) | 0.97 (0.91 to 1.04) | 0.94 (0.88 to 1.01) | 0.61 (0.56 to 0.67) | 0.88 (0.79 to 0.97) | 0.90 (0.81 to 0.99) | 0.94 (0.85 to 1.03) |
| Sex: men | ||||||||
| Age group (years) | ||||||||
| 18–34 | 1.12 (1.06 to 1.18) | 0.97 (0.91 to 1.04) | 0.99 (0.92 to 1.06) | 1.07 (1.00 to 1.14) | 0.58 (0.47 to 0.71) | 1.00 (0.81 to 1.23) | 0.99 (0.81 to 1.22) | 1.09 (0.90 to 1.30) |
| 35–64 | 1.27 (1.22 to 1.32) | 0.93 (0.88 to 0.97) | 0.92 (0.88 to 0.97) | 0.98 (0.94 to 1.03) | 0.64 (0.57 to 0.71) | 0.94 (0.83 to 1.06) | 0.89 (0.80 to 1.01) | 1.03 (0.93 to 1.15) |
| >65 | 1.38 (1.27 to 1.49) | 0.87 (0.78 to 0.97) | 0.90 (0.81 to 1.00) | 0.85 (0.76 to 0.94) | 0.69 (0.61 to 0.78) | 1.11 (0.96 to 1.27) | 0.95 (0.82 to 1.09) | 0.95 (0.83 to 1.10) |
| MEDEA Deprivation Index | ||||||||
| First, least deprived | 1.11 (1.05 to 1.16) | 0.94 (0.88 to 1.01) | 1.04 (0.98 to 1.11) | 0.94 (0.89 to 1.00) | 0.70 (0.62 to 0.79) | 0.94 (0.81 to 1.08) | 0.88 (0.76 to 1.00) | 1.07 (0.94 to 1.22) |
| Second | 1.22 (1.17 to 1.28) | 0.90 (0.84 to 0.95) | 0.96 (0.90 to 1.02) | 1.00 (0.95 to 1.06) | 0.65 (0.57 to 0.73) | 0.94 (0.81 to 1.08) | 0.99 (0.86 to 1.13) | 0.92 (0.81 to 1.04) |
| Third | 1.19 (1.14 to 1.25) | 0.94 (0.88 to 1.00) | 1.00 (0.94 to 1.06) | 0.96 (0.91 to 1.02) | 0.67 (0.59 to 0.75) | 0.89 (0.77 to 1.02) | 1.05 (0.92 to 1.21) | 0.97 (0.85 to 1.10) |
| Fourth | 1.21 (1.15 to 1.27) | 0.93 (0.87 to 0.99) | 0.96 (0.91 to 1.02) | 0.98 (0.92 to 1.04) | 0.64 (0.56 to 0.72) | 1.04 (0.91 to 1.20) | 1.10 (0.96 to 1.26) | 1.05 (0.92 to 1.19) |
| Fifth, most deprived | 1.19 (1.14 to 1.25) | 0.90 (0.85 to 0.96) | 0.95 (0.90 to 1.02) | 1.01 (0.96 to 1.07) | 0.55 (0.48 to 0.62) | 1.01 (0.88 to 1.17) | 0.90 (0.79 to 1.03) | 0.97 (0.85 to 1.10) |
| Rural | 1.18 (1.13 to 1.24) | 0.96 (0.90 to 1.02) | 1.03 (0.97 to 1.09) | 1.03 (0.98 to 1.09) | 0.73 (0.65 to 0.81) | 1.02 (0.91 to 1.16) | 0.98 (0.86 to 1.11) | 1.06 (0.94 to 1.19) |
Incidence rate ratios were calculated by dividing the incidence rate obtained for each strata during the COVID-19 periods (lockdown and postlockdown periods) by the incidence rate obtained for the same time period in 2018 and 2019.
The MEDEA Deprivation Index is calculated at the census tract level in the urban areas of Catalonia and categorised in quintiles of deprivation.
*Total number of diagnoses from March 2018 to March 2021.
MEDEA, Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales.
Estimates of new diagnoses (March 2020–March 2021)
Incident diagnoses of anxiety disorders showed a sudden peak at the onset of the lockdown measures in Catalonia and accounted for an increase of 37.1% (95% PI 25.5 to 50.2) new diagnoses compared with the expected in March 2020 (figure 1A). However, the gap between the observed and the expected anxiety diagnoses during the lockdown period was not statistically significant (−2.5 (95% PI −12.5 to 6.9)). Conversely, a decrease of 19.3% (11.4 to 26.3) compared with the expected was found from July to September 2020. The reduction in incident cases was progressively recovered during the following two trimesters and accounted for a reduction of 15.8% (7.3 to 23.5) during the postlockdown period (table 2).
Table 2.
Estimated number of underdiagnosed anxiety and depressive disorders based on prelockdown data and percentage of reduction compared with expected, by lockdown and postlockdown period
| Lockdown period | Postlockdown period (by trimesters) | Postlockdown period (overall) | ||||||||
| March–June 2020 | July–September 2020 | October–December 2020 | January–March 2021 | July 2020–March 2021 | ||||||
| Estimated number of underdiagnoses, n (95% PI) | Reduction in cases*, % (95% PI) |
Estimated number of underdiagnoses, n (95% PI) | Reduction in cases, % (95% PI) |
Estimated number of underdiagnoses, n (95% PI) | Reduction in cases, % (95% PI) |
Estimated number of underdiagnoses, n (95% PI) | Reduction in cases, % (95% PI) |
Estimated number of underdiagnoses, n (95% PI) | Reduction in cases, % (95% PI) |
|
| Anxiety disorders | ||||||||||
| Overall | −586 (−2690 to 1783) | −2.5 (−12.5 to 6.9) | 2987 (1604 to 4469) | 19.3 (11.4 to 26.3) | 2552 (1141 to 4102) | 16.2 (8.0 to 23.7) | 2148 (485 to 3976) | 12.4 (3.1 to 20.8) | 7688 (3230 to 12547) | 15.8 (7.3 to 23.5) |
| Sex | ||||||||||
| Women | 212 (−1413 to 1983) | 1.4 (−10.8 to 12.0) | 1890 (816 to 3058) | 19.9 (9.7 to 28.6) | 1414 (312 to 2637) | 14.4 (3.6 to 23.9) | 1380 (110 to 2762) | 12.8 (1.2 to 22.7) | 4684 (1238 to 8457) | 15.5 (4.6 to 24.9) |
| Men | −771 (−1727 to 233) | −8.7 (−21.7 to 2.4) | 1146 (487 to 1858) | 19.0 (9.1 to 27.5) | 1156 (500 to 1853) | 19.4 (9.4 to 27.9) | 807 (69 to 1599) | 12.3 (1.2 to 21.8) | 3108 (1056 to 5310) | 16.8 (6.4 to 25.6) |
| Sex: women | ||||||||||
| Age group (years) | ||||||||||
| 18–34 | 895 (405 to 1420) | 19.7 (10.0 to 28.0) | 855 (510 to 1231) | 26.5 (17.7 to 34.2) | 479 (148 to 839) | 15.6 (5.4 to 24.5) | 390 (2 to 804) | 11.5 (0.1 to 21.1) | 1723 (660 to 2874) | 17.8 (7.7 to 26.5) |
| 35–64 | −497 (−1354 to 451) | −6.3 (−19.2 to 5.1) | 874 (336 to 1463) | 18.2 (7.9 to 27.1) | 816 (240 to 1466) | 15.6 (5.2 to 25.0) | 872 (203 to 1612) | 15.0 (3.9 to 24.5) | 2563 (779 to 4541) | 16.2 (5.5 to 25.4) |
| >65 | −186 (−464 to 112) | −8.2 (−23.5 to 4.4) | 161 (−30 to 364) | 10.9 (−2.3 to 21.7) | 119 (−76 to 332) | 7.7 (−5.7 to 18.9) | 118 (−95 to 346) | 7.5 (−7.0 to 19.3) | 398 (−201 to 1042) | 8.7 (−5.0 to 19.9) |
| Sex: men | ||||||||||
| Age group (years) | ||||||||||
| 18–34 | 337 (−10 to 698) | 11.3 (−0.4 to 20.9) | 552 (304 to 823) | 25.2 (15.7 to 33.4) | 506 (266 to 758) | 25.1 (15.0 to 33.5) | 350 (77 to 641) | 15.9 (4.0 to 25.7) | 1408 (647 to 2222) | 22.0 (11.5 to 30.8) |
| 35–64 | −783 (−1229 to −310) | −15.8 (−27.3 to −5.7) | 476 (183 to 791) | 15.1 (6.4 to 22.8) | 535 (232 to 855) | 16.5 (7.9 to 23.9) | 322 (−17 to 689) | 8.9 (−0.5 to 17.2) | 1332 (398 to 2335) | 13.3 (4.4 to 21.2) |
| >65 | −325 (−488 to −155) | −33.1 (−59.6 to −13.5) | 118 (0 to 244) | 17.1 (0.0 to 29.9) | 115 (2 to 240) | 16.9 (0.4 to 29.7) | 135 (9 to 269) | 18.6 (1.5 to 31.3) | 368 (11 to 753) | 17.5 (0.6 to 30.3) |
| MEDEA Deprivation Index | ||||||||||
| First, least deprived | −53 (−405 to 345) | −1.7 (−14.5 to 9.7) | 272 (43 to 533) | 13.9 (2.5 to 24.0) | 217 (−25 to 492) | 10.3 (−1.3 to 20.6) | 287 (5 to 611) | 12.2 (0.2 to 22.9) | 776 (23 to 1636) | 12.1 (0.4 to 22.5) |
| Second | −107 (−501 to 324) | −3.1 (−16.1 to 8.2) | 454 (194 to 738) | 20.9 (10.1 to 30.0) | 433 (153 to 727) | 17.9 (7.2 to 26.8) | 277 (−38 to 614) | 10.6 (−1.7 to 20.9) | 1165 (309 to 2079) | 16.2 (4.9 to 25.6) |
| Third | −191 (−619 to 260) | −5.4 (−19.8 to 6.5) | 484 (198 to 785) | 20.4 (9.5 to 29.4) | 347 (67 to 646) | 15.2 (3.3 to 25.0) | 417 (84 to 780) | 15.7 (3.6 to 25.8) | 1248 (349 to 2211) | 17.0 (5.4 to 26.7) |
| Fourth | −144 (−478 to 193) | −3.9 (−14.4 to 4.8) | 506 (282 to 741) | 20.9 (12.8 to 27.9) | 452 (211 to 692) | 18.1 (9.3 to 25.2) | 371 (113 to 644) | 14.0 (4.7 to 22.0) | 1330 (606 to 2077) | 17.5 (8.8 to 24.9) |
| Fifth, most deprived | −81 (−444 to 287) | −2.3 (−14.1 to 7.4) | 533 (287 to 790) | 22.5 (13.5 to 30.1) | 511 (269 to 760) | 21.3 (12.5 to 28.8) | 361 (81 to 653) | 13.7 (3.4 to 22.3) | 1405 (637 to 2203) | 19.0 (9.6 to 26.9) |
| Rural | −88 (−405 to 256) | −2.5 (−12.5 to 6.6) | 426 (197 to 676) | 17.2 (8.8 to 24.8) | 351 (126 to 590) | 14.6 (5.8 to 22.3) | 234 (−18 to 500) | 8.9 (−0.8 to 17.3) | 1011 (305 to 1766) | 13.5 (4.5 to 21.4) |
| Depressive disorders | ||||||||||
| Overall | 2419 (1856 to 3002) | 45.6 (39.2 to 51.0) | 821 (446 to 1209) | 23.8 (14.5 to 31.5) | 832 (445 to 1247) | 22.8 (13.6 to 30.7) | 804 (361 to 1281) | 19.8 (10.0 to 28.3) | 2458 (1252 to 3737) | 22.0 (12.6 to 30.1) |
| Sex | ||||||||||
| Women | 1596 (1078 to 2165) | 47.1 (37.6 to 54.7) | 596 (239 to 986) | 27.7 (13.3 to 38.7) | 559 (182 to 968) | 23.8 (9.2 to 35.0) | 632 (206 to 1102) | 24.1 (9.4 to 35.6) | 1788 (627 to 3056) | 25.1 (10.5 to 36.4) |
| Men | 830 (442 to 1261) | 43.2 (28.9 to 53.6) | 227 (−41 to 526) | 17.6 (−4.0 to 33.0) | 293 (18 to 600) | 22.2 (1.7 to 36.9) | 205 (−99 to 554) | 14.0 (−8.6 to 30.6) | 723 (−122 to 1680) | 17.8 (−3.8 to 33.4) |
| Sex: women | ||||||||||
| Age group (years) | ||||||||||
| 18–34 | 332 (211 to 475) | 61.5 (50.4 to 69.5) | 115 (29 to 208) | 34.1 (11.6 to 48.4) | 93 (0 to 199) | 23.2 (0.0 to 39.3) | 121 (14 to 249) | 26.9 (4.1 to 43.1) | 329 (43 to 656) | 27.7 (4.8 to 43.3) |
| 35–64 | 715 (499 to 942) | 45.1 (36.4 to 52.0) | 280 (136 to 437) | 28.2 (16.0 to 38.0) | 271 (119 to 436) | 24.4 (12.4 to 34.2) | 325 (148 to 516) | 25.4 (13.4 to 35.1) | 877 (403 to 1389) | 25.9 (13.9 to 35.7) |
| >65 | 549 (368 to 748) | 43.5 (34.1 to 51.2) | 201 (74 to 341) | 24.4 (10.6 to 35.3) | 195 (63 to 333) | 23.2 (8.9 to 34.0) | 186 (44 to 337) | 20.7 (5.8 to 32.2) | 582 (181 to 1011) | 22.7 (8.4 to 33.8) |
| Sex: men | ||||||||||
| Age group (years) | ||||||||||
| 18–34 | 176 (85 to 286) | 55.2 (37.3 to 66.7) | 58 (−7 to 136) | 25.1 (−4.2 to 44.2) | 60 (−7 to 140) | 25.5 (−4.2 to 44.6) | 44 (−34 to 138) | 15.7 (−17.0 to 37.1) | 161 (−48 to 414) | 21.7 (−9.0 to 41.6) |
| 35–64 | 409 (244 to 583) | 43.1 (31.1 to 51.9) | 122 (12 to 243) | 19.8 (2.4 to 33.0) | 164 (42 to 292) | 24.0 (7.5 to 36.0) | 72 (−58 to 212) | 9.9 (−9.8 to 24.6) | 357 (−4 to 747) | 17.7 (−0.2 to 31.0) |
| >65 | 245 (113 to 392) | 37.6 (21.7 to 49.1) | 47 (−46 to 147) | 10.6 (−13.0 to 26.9) | 69 (−17 to 168) | 17.1 (−5.4 to 33.5) | 89 (−7 to 204) | 19.4 (−1.9 to 35.5) | 205 (−70 to 519) | 15.7 (−6.8 to 32.0) |
| MEDEA Deprivation Index | ||||||||||
| First, least deprived | 315 (174 to 481) | 42.0 (28.6 to 52.5) | 134 (39 to 246) | 27.8 (10.1 to 41.4) | 148 (43 to 266) | 27.8 (10.0 to 40.9) | 103 (−15 to 242) | 17.9 (−3.3 to 33.8) | 385 (67 to 754) | 24.2 (5.3 to 38.4) |
| Second | 391 (241 to 556) | 49.2 (37.4 to 57.9) | 157 (55 to 273) | 30.3 (13.2 to 43.0) | 153 (46 to 275) | 26.7 (9.9 to 39.5) | 175 (49 to 321) | 27.2 (9.4 to 40.6) | 486 (150 to 869) | 27.9 (10.7 to 41.0) |
| Third | 309 (166 to 465) | 42.9 (28.8 to 53.1) | 101 (7 to 206) | 21.8 (1.9 to 36.3) | 60 (−34 to 166) | 13.0 (−9.3 to 29.3) | 77 (−38 to 202) | 14.1 (−8.8 to 30.1) | 237 (−65 to 574) | 16.2 (−5.6 to 31.8) |
| Fourth | 376 (231 to 539) | 49.9 (38.0 to 58.8) | 107 (8 to 220) | 22.2 (2.1 to 37) | 113 (9 to 231) | 21.3 (2.1 to 35.6) | 118 (4 to 255) | 20.1 (0.8 to 35.3) | 338 (21 to 706) | 21.1 (1.6 to 35.9) |
| Fifth, most deprived | 375 (204 to 575) | 52.9 (37.9 to 63.3) | 113 (0 to 247) | 24.5 (0.0 to 41.5) | 137 (9 to 286) | 26.0 (2.3 to 42.4) | 118 (−21 to 284) | 21 (−5.0 to 39.1) | 367 (−12 to 817) | 23.8 (−1.0 to 41.0) |
| Rural | 347 (197 to 515) | 39.7 (27.2 to 49.4) | 94 (−14 to 212) | 15.4 (−2.8 to 29.2) | 125 (17 to 244) | 20.6 (3.4 to 33.6) | 76 (−44 to 215) | 11.7 (−8.3 to 27.2) | 296 (−41 to 671) | 15.8 (−2.7 to 29.9) |
The estimated number of underdiagnoses was calculated by subtracting the observed diagnoses from the expected number of diagnoses (95% PI) estimated by negative binomial models.
Reduction in diagnoses (95% PI) was calculated by dividing the number of underdiagnoses by the expected diagnoses and was estimated by study period (lockdown and postlockdown, overall and divided by trimesters).
*Negative values indicate an increase in diagnoses. The MEDEA Deprivation Index is calculated at the census tract level in the urban areas of Catalonia and categorised in quintiles of deprivation.
MEDEA, Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales; PI, prediction interval.
New cases of depressive disorders substantially reduced compared with the expected at the onset of the lockdown measures, accounting for a reduction of 65.8% (95% PI 61.7 to 69.3) compared with the expected in April 2020 (figure 2B). Overall monthly incidence rates remained under the 95% PI from March 2020 to February 2021 (figure 1B). We estimated that the difference between the expected and the observed diagnoses accounted for a reduction of 45.6% (39.2 to 51.0) during the lockdown period compared with the expected. This reduction substantially decreased to 23.8% (14.5 to 31.5) from July 2020 to September 2020 and progressively diminished during the following two trimesters (table 2). Considering the three trimesters combined, the overall reduction of incident cases of the postlockdown period was 22.0% (12.6 to 30.1).
Figure 2.
Expected and observed incidence rates of (A) anxiety and (B) depressive disorders stratified by sex and age group in primary care in Catalonia (March 2019–March 2021). Points indicate monthly incidence rates of anxiety and depressive disorders. The number of expected cases (95% PI) was estimated with negative binomial models using data from 1 March 2018 to 29 February 2020. Shaded areas in blue represent 95% PI. The vertical lines show 1 March 2020. PI, prediction interval; Y, years.
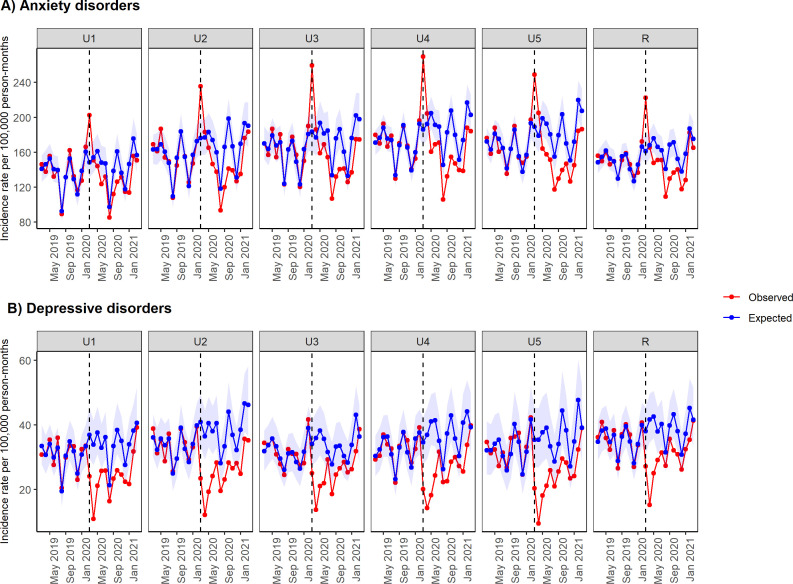
Patterns in anxiety and depressive disorders during the pandemic differ between demographic groups (table 2). The peak of diagnoses of anxiety disorders in March 2020 was particularly pronounced among individuals aged 35–64 years and men aged 18–34 years (figure 2A). Conversely, adults aged 65 or above had the largest absolute decrease in diagnoses of depressive disorders in April 2020 (figure 2B). Individuals aged 18–34 years had greater reductions in incident diagnoses of both outcomes during the lockdown and postlockdown periods, except for reductions during the first trimester of 2021, which were higher among men aged 65 years or above. In terms of sex, women accounted for higher reductions in diagnoses of anxiety (during the lockdown period) and depressive disorders (during the lockdown and postlockdown periods). For SES, we found a gradient in the incidence of anxiety disorders in March 2020, from low to high between the less and fourth most deprived urban areas (figure 3A). Conversely, most deprived urban areas accounted for higher reductions in anxiety disorders compared with the least deprived during the postlockdown period. Reductions in depressive disorders were higher among the most deprived urban areas compared with the least deprived ones in April 2020 (figure 3B) and during the lockdown period, but obtained similar values during the postlockdown period. Rural areas mostly accounted for lower reductions in diagnoses compared with urban areas. Reductions in diagnoses of anxiety and depressive disorders decreased during the first quarter of 2021 compared with the first trimester after the lockdown overall and stratified by sex, age group and SES, except for men aged 65 or above (table 2).
Figure 3.
Expected and observed incidence rates of (A) anxiety and (B) depressive disorders stratified by MEDEA Deprivation Index in primary care in Catalonia (March 2019–March 2021). Points indicate monthly incidence rates of anxiety and depressive disorders. The number of expected cases (95% PI) was estimated with negative binomial models using data from 1 March 2018 to 29 February 2020. Shaded areas in blue represent 95% PI. The vertical lines show 1 March 2020. The MEDEA Deprivation Index is calculated at the census tract level in the urban areas of Catalonia and categorised in quintiles of deprivation. It also includes a rural category for individuals living in rural areas. MEDEA, Mortalidad en áreas pequeñas Españolas y Desigualdades Socioeconómicas y Ambientales; PI, prediction interval; R, Rural; U, Urban.
Our validation approach obtained consistent performances overall and stratified by sex, age group and SES. Figures of monthly observed expected incidence rates and the corresponding 95% PI from March 2017 to February 2020 are included in online supplemental figures 2–4.
Discussion
In this large population-based cohort study, we observed large variations in the incidence of anxiety and depressive disorders diagnosed in primary care in Catalonia by the different periods of the COVID-19 pandemic. The incidence of anxiety disorders showed a sudden peak compared with the expected rates in March 2020 and was followed by a reduction in diagnoses during the next months. Conversely, the incidence of depressive disorders sharply decreased, reaching its minimum value in April 2020. Based on the observed data, the incidence of both disorders seemed to reach prelockdown levels in the first quarter of 2021. According to our model, which captures the underlying upward trend of diagnoses over time, the incidence of anxiety and depressive disorders did not fully reach what would have been expected. Although the negative impact on the incidence of anxiety and depressive disorders appeared to occur across all sex, age groups and SES, this was mostly pronounced among women, young adults and individuals living in the most deprived urban areas.
Similar studies performed in the UK have used the same modelling approach to forecast the incidence of anxiety and depressive disorders during lockdown and the first months of its aftermath.19 Carr et al20 found that, compared with the expected rates, the incidence of primary care-recorded depression and anxiety disorders reduced by 43.0% (95% CI 38.3 to 47.4) and 47.8% (44.3 to 51.2) in April 2020, respectively. In line with our findings, they found larger reductions among adults aged 18–64 years old and among patients registered in more deprived areas. Indeed, a similar study performed in a UK deprived population found a 50.0% reduction (95% CI 41.1 to 56.9) in the first diagnoses of common mental health problems between March and May 2020.20 Although reductions in diagnoses of depressive disorders reported in these studies are similar to those obtained in our study, the initial decline in diagnoses seemed to be larger in our setting (45.6% (95% PI 39.2 to 51.0) during the lockdown period; 65.8% (61.7 to 69.1) in April 2020). In contrast, none of these studies has found an increase in new cases of anxiety disorders at the onset of the pandemic. While the peak of anxiety disorders observed in our study overlaps with the reduction of healthcare contacts for the same disorders in March 2020,10 we cannot exclude the possibility that retrospective recording of diagnoses could have occurred once routine clinical practice was re-established. In addition, while Carr et al20 suggested that the incidence of mental health illness had returned to expected rates in England by September 2020, the monthly incidence rates obtained in our study remained under the 95% PI until February 2021. Although our study observed that the rates of anxiety and depressive disorders were increasing during the first trimester of 2021, it seems likely that the effects of the measures implemented to control the spread of the pandemic in our setting are still negatively affecting the diagnoses of these mental health conditions in primary care.
In Catalonia, two studies have found declines in new all-cause diagnoses and primary care visits associated with diagnoses related to chronic conditions.21 22 Both studies found moderate reductions in diagnoses of mental health conditions, which were lower than the ones observed for other diagnosis groups. For instance, while the average decline in new all-cause diagnoses in 2020 compared with 2019 was 31.1%, the decline in mental health conditions was 27.5%.21 Although reductions have been reported across diagnostic groups,21 22 reductions in mental health diagnoses are particularly concerning as the effects of the pandemic have been estimated to account for an increase of 27.6% (95% CI 25.1 to 30.3) in cases of major depressive disorders and 25.6% (23.2 to 28.0) in cases of anxiety disorders globally in 2020.14 Indeed, the increased rates of anxiety and depressive disorders observed in our study during the first trimester of 2021 might be explained by the midterm effects of the pandemic on mental health, which could be gradually appearing, and the efforts of general practitioners (GPs) to adapt to the increasing demands for care.
Reductions in common mental health diagnoses might be explained by the disruption in the normal functioning of healthcare systems due to the COVID-19 pandemic. In Catalonia, non-essential health activities were interrupted during the lockdown in order to prioritise COVID-19 services, and health authorities advised against going to health centres except in the event of serious illness or urgent situations. Mental health services were also affected by the pandemic due to the relocation of healthcare professionals and temporary suspensions.23 Psychiatric inpatient units were largely reconverted to provide care to patients with COVID-19, and outpatient mental health visits were replaced by telephone consultations. Continuous dissemination of mass media messages reporting the strain on healthcare systems might have influenced healthcare-seeking behaviours, as people might have delayed seeking care in order to avoid overburdening the health systems or out of fear of contracting the disease.24 In such an extraordinary situation, low perceived legitimacy of mental issues might have also prevented those psychologically suffering to discern their emotional distress as an appropriate reason to seek care. In this line, we believe that a large number of people experiencing psychological distress might have developed coping strategies without seeking help in the public healthcare system. Prior evidence suggests that clinicians perceive the emotional distress of their patients but have difficulties in specifying standardised psychiatric diagnoses.25 26 Consultations with a recorded diagnosis of a psychological problem take longer27 and might require reassessment of suspected cases to increase accuracy.28 It seems likely that the diagnoses detected in primary care during the early months of the pandemic might account for more severe cases of mental health issues. In addition, it is important to emphasise the increasing use of telemedicine in Catalonia, where the share of telemedicine-based visits has increased to 56.2%, from 15.4% in the prepandemic year. While telemedicine has ensured the continuity of care of many healthcare processes during the pandemic, it might face limitations generating diagnoses that require more assessments.21
Our findings suggest that women, young adults and individuals living in the most deprived urban areas were affected disproportionately. The reductions among these subgroups are particularly concerning as they have been previously identified as experiencing worse mental health due to the pandemic.4 14 Moreover, the IRRs provided by our study suggest that individuals aged 18–34 years were the only age group with significant increases in cases of anxiety disorders during the last trimester of 2020 (women) and first trimester of 2021 (both women and men) compared with the same periods in 2018 and 2019. The worsening mental health among this subgroup can be likely attributed to the disruption of their daily life, including their access to education and employment opportunities, and their limited in-person interactions with peers.29
The reduced number of new diagnoses observed compared with the expected number obtained in this study is most likely to represent a large number of disorders that have gone undiagnosed and untreated. Possible consequences of this unmet need may include increased demand for mental health services, increased use of emergency departments for mental issues and heightened risk of suicide. Moreover, the economic impact of the pandemic will likely increase the risk of mental health problems and exacerbate healthcare disparities.30 Monitoring patterns in real-time primary care data of common mental disorders will provide crucial information to ensure health services can meet future demand, as primary healthcare centres carry the major burden of management and treatment of common mental health disorders in Spain.25 Data on psychotropic drug prescriptions and secondary care referrals can provide valuable information on the management of anxiety and depressive disorders during the COVID-19 pandemic. Indeed, data on psychotropic drug prescriptions are scarce. In Catalonia, trends in psychotropic drug prescriptions during the first months of the pandemic were similar to those observed for other medications and reported a brief increase in the number of dispensed drugs followed by a reduction in the number of medications prescribed and dispensed. However, reductions observed for psychotropic drugs were lower than those observed for other medications.10 Further research should also investigate the evolution of conditions over time using linkages to data from hospital emergency departments and outpatient mental health centres.
The main strengths of this study are the sample size and the real-world nature of the data. Our study provided data from a broadly representative setting and included more than 3.6 million people registered in primary care in Catalonia. The data used were obtained from primary care electronic health records, which have been shown to be a useful tool for research in many areas, including COVID-19.31 32 In order to strengthen our results we validated our modelling approach forecasting the expected diagnoses from 1 year prior to the pandemic, obtaining consistent predictions compared with observed figures. Moreover, our study investigates the COVID-19-related effects up to March 2021, providing data up to a year after the onset of the lockdown measures in Catalonia.
We acknowledge several limitations to our study. First, our data are limited to recorded diagnoses in primary care, with the absence of such a record taken to indicate the absence of disease. Our data do not capture cases among patients who directly accessed emergency care or those who were hospitalised, which might account for even more severe cases. It is therefore likely that this is an underestimate of episodes of anxiety and depressive disorders. Although our data do not include registers from mental health services, we believe diagnoses performed in these settings would not significantly alter our results as referrals for specialist care must be indicated by a GP in primary care and must be linked to a registered diagnosis. Second, reductions in diagnoses of anxiety and depressive disorders may have been underestimated as they were based on prepandemic data and did not take into consideration an increase of incident cases of psychological distress due to the pandemic. Third, the postlockdown period does not represent the return to prepandemic life. While the stay-at-home order was limited to the first wave of the pandemic in Spain, strict control measures were implemented afterwards.3 Lastly, some of the ICD-10-CM codes used in our study require several months of symptoms in order to be diagnosed. While we cannot account for the GP’s decision-making behaviour around coding, our study reflects diagnoses in primary care practice, which may differ from ICD-10-CM coding guidelines.
In conclusion, the sudden peak in primary care-recorded incident cases of anxiety disorders suggests increased mental distress at the onset of the lockdown measures in Catalonia. The marked reduction in incident diagnoses of anxiety and depressive disorders during the COVID-19 pandemic indicates untreated mental health problems given the increase in anxiety and depression observed in studies using self-reported data. Women, adults aged 18–34 years and individuals living in the most deprived areas might have greater levels of undetected need. Our findings may help to design public health interventions to target those particularly affected by the pandemic, as well as to prepare healthcare systems for greater demand for mental health services in the following months.
Supplementary Material
Acknowledgments
This study was carried out as part of the Doctoral Programme in Biomedical Research Methodology and Public Health at the Autonomous University of Barcelona. The authors would like to acknowledge the efforts of all public healthcare workers in Catalonia during this global pandemic crisis. The authors would also like to thank Daniel López-Codina and his team for assistance in fitting the model, and Miguel-Ángel Mayer for his contributions in the initial stages of the study.
Footnotes
Twitter: @raventosb, @ABerenguera, @Lauramedp, @TDuarte_Salles
Contributors: BR, EB and TD-S conceived and designed the study. SF-B, MA, EB and TD-S mapped the source data to the Observational Medical Outcomes Partnership Common Data Model. BR, EB and AP performed the statistical analysis. BR drafted the initial version of the manuscript. TD-S acts as a guarantor of the study. All authors interpreted the results, critically reviewed the manuscript and approved the final version for submission.
Funding: TD-S acknowledges receiving financial support from Instituto de Salud Carlos III (ISCIII; Miguel Servet 2021: CP21/00023).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. In accordance with the current European and national law, the data used in this study are only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online (https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure) or by contacting SIDIAP (sidiap@idiapjgol.org).
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This project was approved by the Clinical Research Ethics Committee of the IDIAPJGol (project code: 21/052-PCV).
References
- 1.Boletín oficial del estado (BOE). Real Decreto 463/2020, de 14 marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. Available: https://boe.es/buscar/act.php?id=BOE-A-2020-3692 [Accessed 27 May 2021].
- 2.Boletín oficial del estado (BOE). Real Decreto 555/2020, de 5 de junio, POR El que se prorroga el estado de alarma declarado por el real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. Available: https://www.boe.es/diario_boe/txt.php?id=BOE-A-2020-5767 [Accessed 27 May 2021].
- 3.Boletín oficial del estado (BOE). Real Decreto 926/2020, de 25 de octubre, por el que Se declara el estado de alarma para contener la propagación de infecciones causadas por el SARS-CoV-2. Available: https://www.boe.es/buscar/doc.php?id=BOE-A-2020-12898 [Accessed 27 May 2021].
- 4.O'Connor RC, Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 2021;218:326–33. 10.1192/bjp.2020.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.González-Sanguino C, Ausín B, Castellanos Miguel Ángel, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 2020;87:172–6. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang C, Pan R, Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo M, Guo L, Yu M, et al. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res 2020;291:113190. 10.1016/j.psychres.2020.113190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacques-Aviñó C, López-Jiménez T, Medina-Perucha L, et al. Gender-Based approach on the social impact and mental health in Spain during COVID-19 lockdown: a cross-sectional study. BMJ Open 2020;10:e044617. 10.1136/bmjopen-2020-044617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jané-Llopis E, Anderson P, Segura L, et al. Mental ill-health during COVID-19 confinement. BMC Psychiatry 2021;21:194. 10.1186/s12888-021-03191-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Departament de Salut. Generalitat de Catalunya . Informe breu núm 42: Efectes del confinament en La salut mental. Available: https://catsalut.gencat.cat/ca/detalls/noticies/2021-02-08-informe-breu-num-42-efectes-confiament-salut-mental [Accessed 27 May 2021].
- 11.Ghio L, Gotelli S, Marcenaro M, et al. Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. J Affect Disord 2014;152-154:45–51. 10.1016/j.jad.2013.10.002 [DOI] [PubMed] [Google Scholar]
- 12.Cheung R, O'Donnell S, Madi N, et al. Factors associated with delayed diagnosis of mood and/or anxiety disorders. Health Promot Chronic Dis Prev Can 2017;37:137–48. 10.24095/hpcdp.37.5.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United Nations . United nations policy brief: COVID-19 and the need for action on mental health. Available: https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf [Accessed 14 Feb 2021].
- 14.COVID-19 Mental Disorders Collaborators . Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021;398:1700–12. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García-Gil MDM, Hermosilla E, Prieto-Alhambra D, et al. Construction and validation of a scoring system for the selection of high-quality data in a Spanish population primary care database (SIDIAP). Inform Prim Care 2011;19:135–45. 10.14236/jhi.v19i3.806 [DOI] [PubMed] [Google Scholar]
- 16.Voss EA, Makadia R, Matcho A, et al. Feasibility and utility of applications of the common data model to multiple, disparate observational health databases. J Am Med Inform Assoc 2015;22:553–64. 10.1093/jamia/ocu023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Felícitas Domínguez-Berjón M, Borrell C, Cano-Serral G, et al. Construcción de un índice de privación a partir de datos censales en grandes ciudades españolas (Proyecto Medea). Gaceta Sanitaria 2008;22:179–87. 10.1157/13123961 [DOI] [PubMed] [Google Scholar]
- 18.Kümmel A, Bonate PL, Dingemanse J, et al. Confidence and prediction intervals for pharmacometric models. CPT Pharmacometrics Syst Pharmacol 2018;7:360–73. 10.1002/psp4.12286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams R, Jenkins DA, Ashcroft DM, et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. Lancet Public Health 2020;5:e543–50. 10.1016/S2468-2667(20)30201-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carr MJ, Steeg S, Webb RT, et al. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health 2021;6:e124–35. 10.1016/S2468-2667(20)30288-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pifarré I Arolas H, Vidal-Alaball J, Gil J, et al. Missing diagnoses during the COVID-19 pandemic: a year in review. Int J Environ Res Public Health 2021;18:5335. 10.3390/ijerph18105335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lopez Segui F, Hernandez Guillamet G, Pifarré Arolas H, et al. Characterization and identification of variations in types of primary care visits before and during the COVID-19 pandemic in Catalonia: big data analysis study. J Med Internet Res 2021;23:e29622. 10.2196/29622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ayuso-Mateos JL, Mediavilla R, McGreevy KR, et al. Informing the response to COVID-19 in Spain: priorities for mental health research. Revista de Psiquiatría y Salud Mental 2021;14:79–82. 10.1016/j.rpsm.2021.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lazzerini M, Barbi E, Apicella A, et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4:e10–11. 10.1016/S2352-4642(20)30108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bellón JA, Conejo-Cerón S, Rodríguez-Bayón A, et al. Enfermedades mentales comunes en atención primaria: dificultades diagnósticas Y terapéuticas, Y nuevos retos en predicción Y prevención. Informe SESPAS 2020. Gaceta Sanitaria 2020;34:20–6. 10.1016/j.gaceta.2020.05.013 [DOI] [PubMed] [Google Scholar]
- 26.Cepoiu M, McCusker J, Cole MG, et al. Recognition of depression by non-psychiatric physicians--a systematic literature review and meta-analysis. J Gen Intern Med 2008;23:25–36. 10.1007/s11606-007-0428-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hutton C, Gunn J. Do longer consultations improve the management of psychological problems in general practice? A systematic literature review. BMC Health Serv Res 2007;7:71. 10.1186/1472-6963-7-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet 2009;374:609–19. 10.1016/S0140-6736(09)60879-5 [DOI] [PubMed] [Google Scholar]
- 29.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health 2020;4:421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020;7:813–24. 10.1016/S2215-0366(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prieto-Alhambra D, Balló E, Coma E, et al. Filling the gaps in the characterization of the clinical management of COVID-19: 30-day hospital admission and fatality rates in a cohort of 118 150 cases diagnosed in outpatient settings in Spain. Int J Epidemiol 2021;49:1930–9. 10.1093/ije/dyaa190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burn E, Tebé C, Fernandez-Bertolin S, et al. The natural history of symptomatic COVID-19 during the first wave in Catalonia. Nat Commun 2021;12:777. 10.1038/s41467-021-21100-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-057866supp001.pdf (698.3KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. In accordance with the current European and national law, the data used in this study are only available for the researchers participating in this study. Thus, we are not allowed to distribute or make publicly available the data to other parties. However, researchers from public institutions can request data from SIDIAP if they comply with certain requirements. Further information is available online (https://www.sidiap.org/index.php/menu-solicitudesen/application-proccedure) or by contacting SIDIAP (sidiap@idiapjgol.org).