Abstract
Background
Moderate sedation is an integral part of dental care delivery. Target-controlled infusion (TCI) has the potential to improve patient safety and outcome. We compared the effects of using TCI to administer remifentanil/manual bolus midazolam with manual bolus fentanyl/midazolam administration on patient safety parameters, drug administration times, and patient recovery times.
Methods
In this retrospective chart review, records of patients who underwent moderate intravenous sedation over 12 months in a private dental clinic were assessed. Patient indicators (pre-, intra-, and post-procedure noninvasive systolic and diastolic blood pressure, respiration, and heart rate) were compared using independent t-test analysis. Patient recovery time, procedure length, and midazolam dosage required were also compared between the two groups.
Results
Eighty-five patient charts were included in the final analysis: 47 received TCI-remifentanil/midazolam sedation, and 38 received manual fentanyl/midazolam sedation. Among the physiological parameters, diastolic blood pressure showed slightly higher changes in the fentanyl group (P = 0.049), respiratory rate changes showed higher changes in the fentanyl group (P = 0.032), and the average EtCO2 was slightly higher in the remifentanil group (P = 0.041). There was no significant difference in the minimum SpO2 levels and average procedure length between the fentanyl and remifentanil TCI pump groups (P > 0.05). However, a significant difference was observed in the time required for discharge from the chair (P = 0.048), indicating that patients who received remifentanil required less time for discharge from the chair than those who received fentanyl. The dosage of midazolam used in the fentanyl group was 0.487 mg more than that in the remifentanil group; however, the difference was not significant (P > 0.05).
Conclusion
The combination of TCI administered remifentanil combined with manual administered midazolam has the potential to shorten the recovery time and reduce respiration rate changes when compared to manual administration of fentanyl/midazolam. This is possibly due to either the lower midazolam dosage required with TCI remifentanil administration or achieving a stable, steady-state low dose remifentanil concentration for the duration of the procedure.
Keywords: Fentanyl; Midazolam; Moderate Sedation; Remifentanil, Target-Controlled Infusion
INTRODUCTION
Moderate procedural sedation (MPS), or conscious sedation, includes techniques and medications used to help patients withstand unpleasant or painful dental procedures [1]. Local anesthesia is the basis of pain management and control during dental procedures, whereas decreasing the patient’s perception of pain, lowering anxiety, and discomfort levels can be achieved through the administration of low-dose opioid analgesics, most commonly fentanyl, combined with a sedative agent, preferably a benzodiazepine agent, such as midazolam [2]. MPS allows patients to tolerate unpleasant or long dental procedures while breathing independently, maintaining protective reflexes, and response to verbal and tactile stimuli [3,4].
The effectiveness and safety of intravenous administration of benzodiazepines, including diazepam and midazolam, for conscious sedation, have been proven [5,6]. Their popularity in dentistry is attributed to their sedative and selective anxiolytic effects and wide safety margin [4]. Due to the lack of analgesic properties of benzodiazepines, a low-dose opioid agonist, such as fentanyl and remifentanil, should be supplemented. The safety of this drug combination has been well documented in the scientific literature and clinical practice [7,8,9]. Regarding the order of drug administration, Lobb et al. [10] showed that administering low-dose opioid fentanyl before midazolam reduced the required dosage.
Fentanyl, a short-acting opioid that tends to be 60–80 times more potent than morphine, has a rapid onset of analgesia and sedation, with its duration of action being 30–60 min [11]. Based on its unique metabolic properties, remifentanil has a rapid onset and offset of action and stable half-life compared with its alternatives [12]. Both agents are equipotent and provide similar analgesic and respiratory depressant effects while maintaining similar incidence and types of side effects [12,13].
Recently, the availability of precision administrant technology, such as target-controlled infusion (TCI) pumps, has made it possible to administer stable, steady-state drug concentrations within the plasma and at the effect-site or brain. The drug dosage is adjusted automatically by the pump microprocessor and pharmacokinetic model specific to the drug chosen, and the operator only has to enter patient parameters including age, weight, height, sex, and the desired plasma concentration (Cp). In this study, remifentanil concentration was fixed at ≤ 1.0 ng/mL [14,15].
The pharmacokinetic properties of remifentanil coupled with precision drug administration technology such as TCI may make remifentanil a preferred opioid for office-based ambulatory dental surgery, where decreased patient recovery time is required. Therefore, we aimed to compare the effects of TCI-remifentanil/midazolam and manual fentanyl/midazolam administration on patient safety parameters (peripheral oxygen saturation [SpO2], end-tidal carbon dioxide [EtCO2], systolic and diastolic blood pressures [SBP and DBP], heart rate [HR], respiratory rate [RR], administered midazolam dosage, and patient recovery time).
METHODS
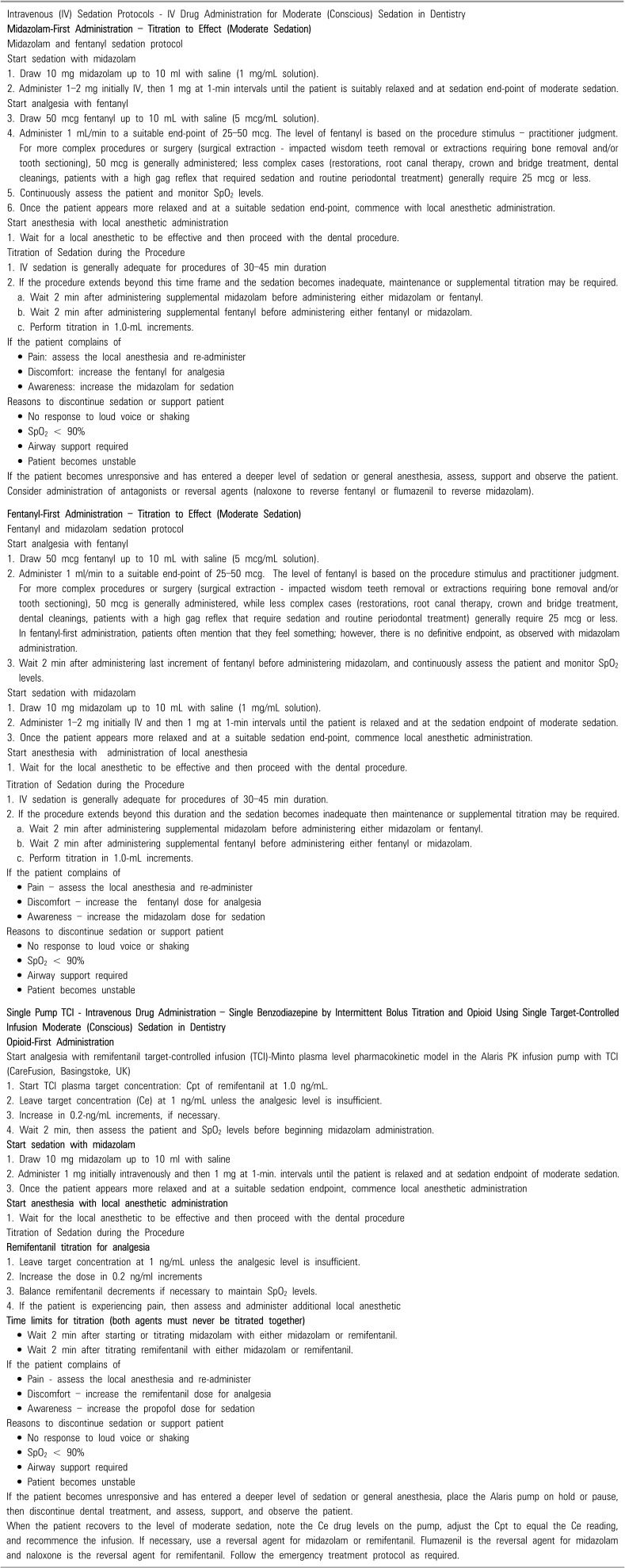
Ethical approval for this study was obtained from the University Research Ethics Office (Pro00075457). A retrospective chart review was conducted in a general dentistry clinic in Edmonton, Alberta, Canada, which utilized a combination of midazolam and a remifentanil TCI pump for procedures requiring moderate intravenous sedation over 12 months. These data were compared to those of patients who received fentanyl first without a TCI pump and then midazolam over a period of 9 months that was part of a previous study [10]. Chart data and sedation records were anonymized for data extraction, coding, and analysis. Appendix 1 presents the full sedation protocol used for both sedation approaches in the clinic.
1. Patients
The dental procedures performed on patients reviewed in this study were similar to those encountered at a general dental office that administers intravenous sedation: surgery; tooth removal; wisdom teeth removal; root canal treatment; restorative treatment such as fillings, crowns, and bridges; and cleaning. The procedures performed were recorded in the sedation monitoring documents for each patient. There were no selection or assignment criteria for charts reviewed in the study, only the next person with sedation of a given protocol within the research study timeline.
All patients received 3–5 L/min of supplemental O2 via a nasal cannula supplied by nasal prongs [16]. Capnography was performed and monitored using side-stream nasal prongs (Masimo Root Monitor, Masimo, California, USA). The most common amount of O2 was 3 L/min.
All patients were sedated to the level of moderate sedation as defined by the American Society of Anesthesiologists (ASA) [17]: response to a loud voice or light touch or ability to give a thumbs up if the rubber dam was in place, and inconvenience to speak verbally. This is the same responsiveness score as the modified Ramsay score for sedation/anesthesia, part of the UA–HERB documentation [18]. All patients were at level 3 or 4 (moderate sedation), and no patient was sedated deeper than moderate sedation or a Ramsay score of 3 or 4.
2. Collected variables
Demographic information recorded included age, sex, smoking status, body mass index, ASA physical status classification, and blood SpO2 and EtCO2 levels. Patient indicators included pre-, intra-, and post-procedure SBP and DBP, RR, and HR.
Patients were monitored by an independent monitoring assistant, whose sole duty was to continuously observe the patient and monitor physiological changes using electronic monitoring equipment. The Masimo Root Monitor was used to monitor SpO2, CO2, capnography and capnogram, RR, HR, and noninvasive blood pressure, while a Philips MRx monitor/defibrillator (Phillips, USA) was used to control the three-lead electrocardiogram. The following data were recorded at 5-min intervals as the dependent variables for the study:
• RR
• Oxygen saturation rate – SpO2
• Capnography and end-tidal CO2 values
• Three-lead electrocardiogram
• HR
• noninvasive blood pressure
Three time durations were calculated for each patient: procedure length (start to end of the procedure), end to discharge from the chair (end of the procedure to patient’s ability to leave the chair to the waiting room), and end to discharge from office (end of the procedure to when the discharge criteria have been met).
After meeting the discharge criteria, patients stayed in the waiting room where additional observation was performed, instructions for care were given to patients’ caregivers, and often, patients were escorted to their transportation by staff. The criteria to determine the discharge of patients were the Modified Aldrete Score [19], and patients were not discharged until he/she achieved a score of > 8 out of 10. None of the patients undergoing sedation was left unattended during or after sedation.
3. Sedation procedure
All anesthesia was achieved with local anesthesia administered in the same dental office by three staff members (a dentist holding permit for intravenous sedation with training in TCI administration, certified dental assistant, and dedicated sedation assistant for monitoring of patient vitals). Opioids (fentanyl or remifentanil) were used for analgesia only and as part of the two-drug sedation regimen.
4. Fentanyl group
The administration of a single benzodiazepine (midazolam) and opioid analgesic (fentanyl) is a worldwide standard of care and is considered a traditional dental sedation regimen for moderate intravenous sedation in dental offices [20]. Fentanyl was administered at 5-µg/mL/min increments to a total of 25–50 µg. The dosage ranged between 25 and 50 µg based on the operator’s clinical judgment and treatment required (50 µg for more stimulating procedures such as wisdom teeth removal and 25 µg for less stimulating procedures such as fillings and root canals). Midazolam was administered at 1-mg/mL/min increments until patients reached a suitable sedation level of moderate sedation or a Ramsay score of 3 or 4. The dose of µg/kg of fentanyl or mg/kg of midazolam could be calculated; however, the results defeated the purpose of titration. The maximum dose of fentanyl administered was 50 µg for each patient.
5. Remifentanil group
Remifentanil in combination with midazolam was administered by TCI pump technology using the Alaris PK infusion pump with TCI and a pharmacokinetic software model, Minto model, targeting plasma concentration (CareFusion, Basingstoke, UK). First, remifentanil was administered at a fixed dose of ≤ 1.0 ng/mL. [21] The drug concentration maintained a stable steady-state concentration in the plasma and effect-site (brain) for the duration of sedation. The maximum remifentanil was 1.0 ng/mL. Midazolam was administered by intermittent hand-bolus administration at 1 mg/mL/min until a suitable level of sedation was achieved. As time went by and sedation level waned, 1 mg of midazolam was administered every 15–30 min to maintain an adequate level of drug for patients. The maximum total dose of midazolam was 10 mg. The total midazolam dose administered was also recorded for each patient at the end of the procedure.
6. Analysis
Analyses were conducted using IBM SPSS Statistics version 24 (IBM Corp., Armonk, NY, USA). Data were screened before statistical outliers were analyzed. Cases with outliers and potential entry errors were reviewed to determine whether single or all data points or entire cases were removed from the analysis. Differences pre-and post-procedure in SBP and DBP, RR, and HR were calculated as changes for analysis. Comparisons between the TCI-remifentanil/midazolam and manual-fentanyl/midazolam groups were performed using an independent t-test with an alpha of 0.05.
RESULTS
Eighty-four patient charts were reviewed. One chart from the fentanyl group was removed because the patient was less than 15 years old. For the chart information reviewed, 47 patients were included in the remifentanil group, while 37 patients were included in the fentanyl group. No charts had missing key demographic information, except one patient who had a missing ASA classification.
1. Patient demographics and physiological measures
The demographic information for both patient groups is summarized in Tables 1 and 2. Of these patients, 39% were men and 61% were women. Only eight patients in both groups were reported as smokers. All patients met the ASA physical classification criteria of 1 or 2. Patients’ ages ranged from 16 to 67 years, weight ranged from 49.3 to 131.5 kg, and body mass index ranged from 17 to 37. The groups did not significantly differ in any demographic variables (Table 1).
Table 1. Demographic data for continuous variables in patients receiving fentanyl and remifentanil.
| Patient parameters | Groups | Number | Range | Minimum | Maximum | Mean ± SD | P Value |
|---|---|---|---|---|---|---|---|
| Age (yr) | Fentanyl | 37 | 51 | 16 | 67 | 32.65 ± 17.07 | 0.920 |
| Remifentanil | 47 | 50 | 16 | 66 | 33.02 ± 16.55 | ||
| Weight (kg) | Fentanyl | 37 | 82.2 | 49.3 | 131.5 | 74.07 ± 19.08 | 0.691 |
| Remifentanil | 47 | 66.7 | 49.4 | 116.1 | 72.58 ± 14.98 | ||
| BMI | Fentanyl | 37 | 20.0 | 17.0 | 37.0 | 24.82 ± 4.59 | 0.993 |
| Remifentanil | 47 | 17.0 | 18.0 | 35.0 | 24.83 ± 4.21 |
SD, Standard Deviation; yr, year.
Table 2. Demographic data for categorical variables in patients receiving fentanyl and remifentanil.
| Patient parameters | Number (%) | Total | P-Value | ||
|---|---|---|---|---|---|
| Fentanyl | Remifentanil | ||||
| Sex | 0.812 | ||||
| male | 14 (37.8) | 19 (40.4) | 33 | ||
| female | 23 (62.2) | 28 (59.6) | 51 | ||
| Smoking status | 0.275 | ||||
| No | 32 (86.5) | 44 (93.6) | 76 | ||
| Yes | 5 (13.5) | 3 (6.4) | 8 | ||
| ASA | 0.603 | ||||
| I | 30 (83.7) | 37 (78.7) | 67 | ||
| II | 6 (16.7) | 10 (21.3) | 16 | ||
ASA, American Society of Anesthesiologists.
The patient physiological parameters are presented in Table 3. For blood SpO2, three of 47 remifentanil patients had a SpO2 reading below 90. However, it quickly returned to safe oxygenation levels after patients were asked to take a deep breath; therefore, these were included in the analysis. The average reading was 95.35% and 97.41% in the fentanyl and remifentanil groups, respectively. The values of SBP and DBP are presented with the average, standard deviation, minimum and maximum.
Table 3. Summary of patient physiological parameters.
| Physiological Parameters | Fentanyl | Remifentanil | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | Min | Max | Mean ± SD | Min | Max | |
| Average SpO2 (%) | 95.35 ± 1.79 | 92.70 | 100.00 | 97.41 ± 2.46 | 91.38 | 100.00 |
| Average EtCO2 (mmHG) | 33.59 ± 5.05 | 21.00 | 42.00 | 38.09 ± 9.77 | 30.33 | 99.67 |
| SBP (mmHG) | 110.13 ± 10.59 | 94.33 | 141.00 | 119.29 ± 12.50 | 86.75 | 144.50 |
| DBP (mmHG) | 68.85 ± 9.69 | 56.00 | 100.33 | 74.71 ± 9.93 | 52.00 | 104.00 |
| Average Heart Rate (beats/min) | 72.65 ± 12.87 | 43.67 | 98.00 | 74.98 ± 11.94 | 54.33 | 104.00 |
| Average respiration rate (breaths/minute) | 16.29 ± 2.53 | 10.00 | 20.67 | 15.08 ± 2.23 | 11.33 | 20.00 |
DBP, diastolic blood pressure; EtCO2, end-tidal carbon dioxide; Max, maximum; Min, minimum; SBP, systolic blood pressure; SD, standard deviation; SpO2, peripheral capillary oxygen saturation.
2. Vital sign changes
To analyze changes in vital signs, changes in each value (range of each patient) were measured throughout the procedure to determine differences in SBP, DBP, HR, and RR. The lowest blood SpO2 value for each patient was recorded and compared. The average EtCO2 levels were analyzed to determine the carbon dioxide concentration. The results of the evaluation of changes in vital signs are displayed in Table 4. Among the physiological parameters, DBP changes were slightly higher in the fentanyl group (P = 0.049), RR changes were higher in the fentanyl group (P = 0.032), and average EtCO2 was slightly higher in the remifentanil group (P = 0.041). To ensure patient safety, verbal contact was maintained throughout the procedure. Oxygen desaturation (< 90%) occurred in three patients in the remifentanil group but was quickly reversed by asking patients to take a deep breath. Oxygen desaturation below 88% was not observed. Finally, no airway interventions were required. There was no significant difference in the minimum SpO2 levels between the groups (P > 0.05).
Table 4. Comparison of changes in vital signs and average blood SpO2 and EtCO2 levels between fentanyl and remifentanil groups.
| Patient indicators | Groups | Mean ± SD | t score | P |
|---|---|---|---|---|
| SBP change | Fentanyl | 8.83 ± 8.25 | -0.909 | .366 |
| Remifentanil | 11.4 ± 12.65 | |||
| DBP change | Fentanyl | 10.75 ± 9.71 | 1.996 | .049* |
| Remifentanil | 7.51 ± 4.77 | |||
| HR change | Fentanyl | 9.94 ± 7.39 | 0.181 | .857 |
| Remifentanil | 9.64 ± 7.80 | |||
| Respiratory rate changes per minute | Fentanyl | 6.75 ± 11.20 | 2.179 | .032* |
| Remifentanil | 2.87 ± 4.26 | |||
| Minimum SpO2 (%) | Fentanyl | 95.03 ± 2.75 | 0.383 | .705 |
| Remifentanil | 95.28 ± 3.11 | |||
| Average EtCO2 (mmHg) | Fentanyl | 33.59 ± 5.05 | -2.077 | .041* |
| Remifentanil | 38.09 ± 9.76 |
*P < .05
DBP, diastolic blood pressure; EtCO2, end-tidal carbon dioxide; HR, heart rate; SBP, systolic blood pressure; SD, standard deviation; SpO2, peripheral capillary oxygen saturation.
3. Duration comparison
Three points of comparison were evaluated for the duration of patients between the two sedation groups and are presented in Table 5. There was no significant difference in the average procedure length between the fentanyl and remifentanil TCI pump groups (P > 0.05). The procedures completed between the two sedation groups were statistically comparable. However, a significant difference was observed in the time required for discharge from the chair (P = 0.048), indicating that patients who received fentanyl required approximately 5 more minutes to be discharged from the chair. There were no differences in the time from the end of the procedure to discharge from the office (P > 0.05).
Table 5. Comparison of recovery time and procedure length between fentanyl and remifentanil groups.
| Time | Groups | Mean ± SD | t score | P |
|---|---|---|---|---|
| End to discharge from office | Fentanyl | 0:49:53.62 ± 0:18:22.96 | -.884 | .380 |
| Remifentanil | 0:45:58.38 ± 0:22:17.20 | |||
| End to discharge from chair | Fentanyl | 0:18:12.77 ± 0:09:18.09 | -2.008 | .048* |
| Remifentanil | 0:13:21.67 ± 0:12:42.82 | |||
| Procedure length | Fentanyl | 0:31:44.21 ± 0:18:20.14 | -1.549 | .125 |
| Remifentanil | 0:40:58.72 ± 0:32:51.30 |
*P < .05
Notes: End to discharge from chair; The time required for discharge from the chair after completion of dental treatment End to discharge from office; The time required for discharge from the office after completion of dental treatment
SD, standard deviation.
Finally, the total dosage of the drugs administered was compared with that of midazolam. The dosage of midazolam used in the fentanyl group (5.508 ± 1.078) was 0.487 mg more than that in the TCI/remifentanil group (5.021 ± 1.507); however, the difference was not significant (P = 0.095).
DISCUSSION
This retrospective observational study revealed that the application of TCI in the administration of remifentanil/midazolam in adults was associated with a quicker recovery time of 5 min (P = 0.048) and lower respiration changes than was manual infusion of fentanyl/midazolam (P = 0.032). Moreover, a higher variation in DBP in the fentanyl group (P = 0.049) and higher EtCO2 in the remifentanil group (P = 0.041) were found. Similar to our results, Hannam et al. found that administration of remifentanil combined with propofol results in a 16.7-mmHg increase in CO2 pressure due to the inhibitory effect of remifentanil on pCO2 removal [22]. Although a greater dosage of midazolam was required for patients who manually received fentanyl than for those who underwent the remifentanil/midazolam TCI technique, the difference was not significant and clinically irrelevant.
TCI use was associated with prolonged operation time, although the difference was not significant, possible because of the additional time required for setting up and using the TCI device and the lower number of setting changes in the manual administration group. Hsieh et al. [23] also found that the administration of propofol using TCI is more time-consuming than manual infusion of a sedative agent for electroconvulsive therapy, as the former takes time to set up in each treatment.
The recovery time (end of the dental procedure to patient discharge from the chair) was approximately 5 min longer in patients who received fentanyl/midazolam anesthesia, which could be attributed to the lower dose of midazolam received by patients in the remifentanil/midazolam TCI group. Similarly, a study conducted by Beers and Camporesi showed that remifentanil has a faster onset and recovery than fentanyl. Minimal alterations of the pharmacokinetics in patients with systemic disorders and ease of drug administration were among other favorable pharmacological aspects of remifentanil [24].
Changes in vital signs and average blood SpO2 levels were not significantly different between the groups. RR significantly changed in patients sedated with manual administration of fentanyl/midazolam. This could be explained in part by both the greater midazolam dosage required for sedation of patients in the fentanyl group and the pharmacokinetics of fentanyl itself.
Our evidence supports that benzodiazepines such as midazolam decrease rr specifically when combined with opioids. The mechanism of action of midazolam in depressing respiration involves its agonist and antagonist effects on GABA and NMDA receptors, respectively. Despite the mild respiratory depressant effect of benzodiazepines, their combination with opioids results in additive or synergistic effects on respiration [25,26,27,28]. The application of TCI systems allows the computer’s pump control algorithm to precisely calculate the infusion rate necessary to achieve a predetermined drug concentration known as the target (Cptarget) in the plasma [29,30]. In other words, this system allows clinicians to focus on the concentration domain for intravenous drug delivery [31].
Fentanyl and other opioid agonists can also depress respiration by reducing the response to elevated plasma levels of CO2 and decreased plasma levels of O2 by acting on µ-opioid receptors at different sites, which leads to a reduction in the drive to breathe [25,32]. Slidharan et al. [33] demonstrated that the required dose of propofol combined with remifentanil to induce general anesthesia was significantly lower than that in combination with fentanyl. Moreover, they found that intravenous infusion of fentanyl in humans is likely to produce respiratory depression by decreasing the drive to breathe and creating mechanical resistance.
Mu et al. compared TCI and manual administration of propofol in children and reported that the TCI use was associated with greater dosages of propofol required for anesthesia in the studied population [15]. This result contrasts with our findings that TCI required fewer sedative agents. Mu’s finding can be attributed to the study population comprising children who require a high Cptarget at induction. As mentioned, a high initial target for induction is required to achieve rapid induction of anesthesia in children because of their probable excessive movements. Moreover, the anesthetic drugs used in our study were different.
Similarly, Bilgin et al. compared the effects of intravenous infusions of alfentanil, fentanyl, and remifentanil, finding that there were no significant differences in physiological parameters, including SBP, DBP, and HR at various stages of stereotactic brain biopsy [34].
In our study, oxygen desaturation (< 90%) occurred in three patients in the remifentanil group but was quickly reversed by asking patients to take a deep breath. No significant difference was observed in the minimum SpO2 between the fentanyl and remifentanil groups. A convincing mechanism for this side effect is airway closure due to a decrease in lung volume. Indeed, opioids affect respiratory muscle actions in anesthetized patients who can breathe spontaneously [35]. Our findings are consistent with the results of a study conducted by Maurtua et al. [36], who reported more oxygen desaturation in the remifentanil group than in the fentanyl group. Owing to the short half-life of remifentanil, this side effect does not appear to be clinically relevant.
Since the current study compared two methods of drug administration, it lacks information on other sedation strategies, which should be considered while interpreting the report’s findings. Without various comparator groups, it is unclear whether the favorable safety outcomes are solely due to the target-controlled infusion of remifentanil or midazolam.
Barends et al. [37] found that moderate-to-deep sedation (MDS) using propofol and remifentanil TCIs provides adequate sedation associated with a low incidence of catastrophic events related to sedation, comparable to other methods used for MDS. The present study also provides further support for the use of remifentanil TCI, a protocol-driven sedation method that, if provided by well-trained and equipped sedation practitioners under the indirect supervision of an anesthesiologist, is a safe and successful method of MDS for a wide range of patients and procedures. Moreover, the elimination of bolus injections reduces the potential for human error during administration.
In summary, the results of our study suggest that remifentanil TCI combined with midazolam can shorten patient recovery time and significantly lower RR changes, possibly because of the smaller dosage of midazolam required than that typically used in the manual administration of fentanyl/midazolam. Additionally, the depressing effect of fentanyl on respiration through acting on µ-opioid receptors at various sites can explain the greater RR changes among patients who received fentanyl/midazolam [25,32]. The availability of reversal agents for midazolam and remifentanil may mitigate any potential concerns regarding adverse events in a non-hospital dental care setting [38]. Future studies should consider two short-acting drugs (propofol and remifentanil) with precision drug administration by TCI using a larger population of dental patients to make definitive conclusions and determine whether TCI should be incorporated into the standard of care for moderate sedation.
ACKNOWLEDGEMENTS
Our study team acknowledges many staff members in assisting and contributing to this project: Madison Howey, Jacqueline Green, and all staff from the dental office where this study took place.
Appendix 1
Intravenous (IV) sedation protocols
Footnotes
- Doug Lobb: Conceptualization, Data curation, Formal analysis, Resources, Writing – review & editing.
- Nazila Ameli: Formal analysis, Writing – original draft, Writing – review & editing.
- Silvia Ortiz: Data curation, Formal analysis, Methodology, Project administration, Writing – original draft.
- Hollis Lai: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – review & editing.
FUNDING: No funding was received for this study.
DECLARATION OF INTERESTS: The authors have no conflicts of interest to declare.
References
- 1.Practice guidelines for moderate procedural sedation and analgesia 2018: a report by the american society of anesthesiologists task force on moderate procedural sedation and analgesia, the american association of oral and maxillofacial surgeons, american college of radiology, american dental association, american society of dentist anesthesiologists, and society of interventional radiology. Anesthesiology. 2018;128:437–479. doi: 10.1097/ALN.0000000000002043. [DOI] [PubMed] [Google Scholar]
- 2.Del Gaudio A, Ciritella P, Perrotta F, Puopolo M, Lauta E, Mastronardi P, et al. Remifentanil vs fentanyl with a target controlled propofol infusion in patients undergoing craniotomy for supratentorial lesions. Minerva Anestesiol. 2006;72:309–319. [PubMed] [Google Scholar]
- 3.Benzoni T, Cascella M. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2020. Jan, Procedural sedation.2020 Jul 4. PMID: 31869149. [PubMed] [Google Scholar]
- 4.Kapur A, Kapur V. Conscious sedation in dentistry. Ann Maxillofac Surg. 2018;8:320–323. doi: 10.4103/ams.ams_191_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finder RL, Moore PA. Benzodiazepines for intravenous conscious sedation: agonists and antagonists. Compendium. 1993;14:972, 974, 976–980. [PubMed] [Google Scholar]
- 6.Averley PA, Girdler NM, Bond S, Steen N, Steele J. A randomized controlled trial of pediatric conscious sedation for dental treatment using intravenous midazolam combined with inhaled nitrous oxide or nitrous oxide/sevoflurane. Anaesthesia. 2004;59:844–852. doi: 10.1111/j.1365-2044.2004.03805.x. [DOI] [PubMed] [Google Scholar]
- 7.Prabhudev AM, Chogtu B, Magazine R. Comparison of midazolam with fentanyl-midazolam combination during flexible bronchoscopy: a randomized, double-blind, placebo-controlled study. Indian J Pharmacol. 2017;49:304–311. doi: 10.4103/ijp.IJP_683_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan PM, Kienstra AJ, Cosgrove P, Vezzetti R, Wilkinson M. Safety and effectiveness of intranasal midazolam and fentanyl used in combination in the pediatric emergency department. Am J Emerg Med. 2019;37:237–240. doi: 10.1016/j.ajem.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 9.Lee B, Park JD, Choi YH, Han YJ, Suh DI. Efficacy and safety of fentanyl in combination with midazolam in children on mechanical ventilation. J Korean Med Sci. 2019;34:e21. doi: 10.3346/jkms.2019.34.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lobb D, Clarke A, Lai H. Administration order of midazolam/fentanyl for moderate dental sedation. J Dent Anesth Pain Med. 2018;18:47–56. doi: 10.17245/jdapm.2018.18.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galeotti A, Garret Bernardin A, D’Antò V, Ferrazzano GF, Gentile T, Viarani V, et al. Inhalation conscious sedation with nitrous oxide and oxygen as an alternative to general anesthesia in precooperative, fearful, and disabled pediatric dental patients: a large survey on 688 working sessions. Biomed Res Int. 2016;1:7289310. doi: 10.1155/2016/7289310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lacombe GF, Leake JL, Clokie CM, Haas DA. Comparison of remifentanil with fentanyl for deep sedation in oral surgery. J Oral Maxillofac Surg. 2006;64:215–222. doi: 10.1016/j.joms.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Gurbet A, Goren S, Sahin S, Uckunkaya N, Korfali G. Comparison of analgesic effects of morphine, fentanyl, and remifentanil with intravenous patient-controlled analgesia after cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:755–758. doi: 10.1053/j.jvca.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 14.Abad A. In: Anestesia total intravenosa. Principios básicos. Aguilera L, Abad A, editors. Madrid: SA delitografia; 2009. Sistema de Infusión; pp. 87–102. [Google Scholar]
- 15.Mu J, Jiang T, Xu XB, Yuen VM, Irwin MG. Comparison of target-controlled infusion and manual infusion for propofol anesthesia in children. Br J Anaesth. 2018;120:1049–1055. doi: 10.1016/j.bja.2017.11.102. [DOI] [PubMed] [Google Scholar]
- 16.Salinas Salmeron KS, Kim HJ, Seo KS. Effects site concentrations of propofol using target-controlled infusion in dental treatment under deep sedation among different intellectual disability types. J Dent Anesth Pain Med. 2019;19:217–226. doi: 10.17245/jdapm.2019.19.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status – historical perspectives and modern developments. Anaesthesia. 2019;74:373–379. doi: 10.1111/anae.14569. [DOI] [PubMed] [Google Scholar]
- 18.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2(5920):656–659. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–934. [PubMed] [Google Scholar]
- 20.Fenn NE, 3rd, Plake KS. Opioid and benzodiazepine weaning in pediatric patients: review of current literature. Pharmacotherapy. 2017;37:1458–1468. doi: 10.1002/phar.2026. [DOI] [PubMed] [Google Scholar]
- 21.Eleveld DJ, Colin P, Absalom AR, Struys MMRF. Target-controlled-infusion models for remifentanil dosing consistent with approved recommendations. Br J Anaesth. 2020;125:483–491. doi: 10.1016/j.bja.2020.05.051. [DOI] [PubMed] [Google Scholar]
- 22.Hannam JA, Borrat X, Trocóniz IF, Valencia JF, Jensen EW, Pedroso A, et al. Modeling respiratory depression induced by remifentanil and propofol during sedation and analgesia using a continuous noninvasive measurement of pCO2. J Pharmacol Exp Ther. 2016;356:563–573. doi: 10.1124/jpet.115.226977. [DOI] [PubMed] [Google Scholar]
- 23.Hsieh ML, Lu YT, Lin CC, Lee CP. Comparison of the target-controlled infusion and the manual infusion of propofol anesthesia during electroconvulsive therapy: an open-label randomized controlled trial. BMC Psychiatry. 2021;21:71. doi: 10.1186/s12888-021-03069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beers R, Camporesi E. Remifentanil update: clinical science and utility. CNS Drugs. 2004;18:1085–1104. doi: 10.2165/00023210-200418150-00004. [DOI] [PubMed] [Google Scholar]
- 25.Pattinson KT. Opioids and the control of respiration. Br J Anaesth. 2008;100:747–758. doi: 10.1093/bja/aen094. [DOI] [PubMed] [Google Scholar]
- 26.Southerland JH, Brown LR. Conscious intravenous sedation in dentistry: a review of current therapy. Dent Clin North Am. 2016;60:309–346. doi: 10.1016/j.cden.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 27.Dahan A, Nieuwenhuijs D, Olofsen E, Sarton E, Romberg R, Teppema L. Response surface modeling of alfentanil-sevoflurane interaction on cardiorespiratory control and bispectral index. Anesthesiology. 2001;94:982–991. doi: 10.1097/00000542-200106000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Nieuwenhuijs DJ, Olofsen E, Romberg RR, Sarton E, Ward D, Engbers F, et al. Response surface modeling of remifentanil–propofol interaction on cardiorespiratory control and bispectral index. Anesthesiology. 2003;98:312–322. doi: 10.1097/00000542-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Egan TD, Westphal M, Minto CF, Schnider TW. Moving from dose to concentration: as easy as TCI! Br J Anaesth. 2020;125:847–849. doi: 10.1016/j.bja.2020.08.033. [DOI] [PubMed] [Google Scholar]
- 30.Egan TD. An intellectual framework for drug administration methods in anesthesia: three practice domains. Anesth Analg. 2018;127:817–819. doi: 10.1213/ANE.0000000000003601. [DOI] [PubMed] [Google Scholar]
- 31.Egan TD. Target-controlled drug delivery: progress toward an intravenous “vaporizer” and automated anesthetic administration. Anesthesiology. 2003;99:1214–1219. doi: 10.1097/00000542-200311000-00031. [DOI] [PubMed] [Google Scholar]
- 32.Hill R, Santhakumar R, Dewey W, Kelly E, Henderson G. Fentanyl depression of respiration: comparison with heroin and morphine. Br J Pharmacol. 2020;177:254–266. doi: 10.1111/bph.14860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sridharan K, Sivaramakrishnan G. Comparison of fentanyl, remifentanil, sufentanil and alfentanil in combination with propofol for general anesthesia: a systematic review and meta-analysis of randomized controlled trials. Curr Clin Pharmacol. 2019;14:116–124. doi: 10.2174/1567201816666190313160438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bilgin H, Başağan Moğol E, Bekar A, Işçimen R, Korfali G. A comparison of effects of alfentanil, fentanyl, and remifentanil on hemodynamic and respiratory parameters during stereotactic brain biopsy. J Neurosurg Anesthesiol. 2006;18:179–184. doi: 10.1097/01.ana.0000210998.10410.2e. [DOI] [PubMed] [Google Scholar]
- 35.Drummond GB, Lafferty B. Oxygen saturation decreases acutely when opioids are given during anesthesia. Br J Anaesth. 2010;104:661–663. doi: 10.1093/bja/aeq076. [DOI] [PubMed] [Google Scholar]
- 36.Maurtua MA, Pursell A, Damron K, Sonal P. Remifentanil: pharmacokinetics, pharmacodynamics, and current clinical applications. Clin Med Rev Case Rep. 2020;7:304 [Google Scholar]
- 37.Barends CRM, Driesens MK, van Amsterdam K, Struys MMRF, Absalom AR. Moderate-to-deep sedation using target-controlled infusions of propofol and remifentanil: adverse events and risk factors: a retrospective cohort study of 2937 procedures. Anesth Analg. 2020;131:1173–1183. doi: 10.1213/ANE.0000000000004593. [DOI] [PubMed] [Google Scholar]
- 38.Tylleskar I, Skulberg AK, Skarra S, Nilsen T, Dale O. Pharmacodynamics and arteriovenous difference of intravenous naloxone in healthy volunteers exposed to remifentanil. Eur J Clin Pharmacol. 2018;74:1547–1553. doi: 10.1007/s00228-018-2545-y. [DOI] [PubMed] [Google Scholar]