Abstract
This study aimed to assess the combined use of extraoral vibratory stimulation and extraoral cooling in reducing the pain (subjective and objective) of dental local anesthesia administration in children.
PubMed, Cochrane Central Register of Controlled Trials, and Ovid SP databases were searched up to July 2021. Article titles were screened and full-text evaluations of the selected articles were performed. Finally, seven studies (391 children, aged 4 – 12 years) were included in this qualitative and quantitative analysis. The pooled data determined the combined effect of extraoral vibration and extraoral cooling as a single measure. Extraoral vibration or cooling alone were not compared. The measured primary and secondary outcomes were pain perception and subjective and objective pain, respectively. When compared with the control, extraoral vibration and cooling resulted in significant differences in the mean combined data for the variables, pain perception, and pain reaction. Children’s subjective pain as measured by pain scores were reduced when extraoral vibration and cooling was used during local anesthesia administration (mean difference -3.52; 95% confidence interval [-5.06 - 1.98]) and objective pain (mean difference -1.46; 95% confidence interval [-2.95 - 0.02] ; mean difference -1.93; 95% confidence interval [-3.72 - 0.14]).
Within the confines of this systematic review, there is low-quality evidence to support the use of combined extraoral vibration and cooling for reducing pain (subjective and objective) during intraoral local anesthesia administration in children.
Keywords: Children, Cooling, External, Iintraoral, Local Anesthesia, Vibration
INTRODUCTION
Fear of pain due to needle pricks is high among children [1]. Reducing the discomfort during intraoral local anesthesia administration is considered the most challenging aspect of dentistry, especially in pediatric dental patients. Physical, psychological, and pharmaceutical methods, and their combinations have tried to address this pain. Pharmaceutical approaches include the application of topical anesthetics [2]. Psychological and behavioral modification methods including active distractions, deep breathing [3], Witaul [4], and eye movement distractions [5] have been tried. Passive distraction methods, such as audiovisual glasses and video distraction [6], have also been attempted with some success [7]. Other methods, such as precooling the injection site [8], warming the local anesthesia [9], buffering the local anesthesia [10], and camouflaging the syringe, have also been suggested [11]. Physical methods, such as vibration, are among the oldest methods and the most widely used, to alleviate needle prick discomfort during local anesthesia administration in children. The gate control theory by Melzak and Wall is a widely accepted pain theory that explains the mechanism underlying the vibratory effects in reducing pain perception. According to Melzak and Wall, vibration activateS A-beta fibers whose diameters are larger than A-delta and C fibers that transmit pain sensation from the periphery to the brain [12].
Vibratory stimuli can be delivered to the desired site, that is, the site of the needle prick, using both direct and indirect methods. Direct vibratory stimuli can be applied intraorally at the site of the needle prick. Direct vibratory stimulation can be achieved manually using a cotton roll [13], an SMV-Syringe Micro Vibrator instrument that snaps onto a syringe[14], or a dental vibe [12].
Indirect vibratory stimuli through extraoral vibratory stimulations may also be useful in alleviating pain during intraoral local anesthesia delivery, as reported in various studies.
Previous systematic reviews of direct intraoral vibration using different vibratory devices have shown that direct intraoral vibratory stimulations can reduce pain perception during intraoral local anesthesia administration [12]. Previous systematic reviews have suggested that precooling the injection site has the potential to reduce discomfort due to injection pain and local anesthesia administration [8].
Indirect extraoral vibratory stimulations are effective in reducing pain due to intraoral local anesthesia administration in a few studies. No systematic review has been conducted on the effects of indirect extraoral vibratory stimulations and extraoral cooling on injection pain. This systematic review aimed to evaluate the combined effect of extraoral vibration and cooling on pain during intraoral local anesthesia administration in children.
METHODS
Protocol and registration: This study was registered under the Prospero registration number CRD42021282192, and followed the PRISMA guidelines.
Eligibility criteria: The strategic search question was evaluated in PICO format “Does the combination of extraoral vibration and cooling have any effect on pain perception and reaction during dental injections in children”. Patients were children, aged between 3 and 17 years. The intervention consisted of a combined extraoral vibratory stimulus and cooling during an intraoral needle prick. The control group consisted of children who did not receive an extraoral vibratory stimulus or patients who received any other method of counter stimulation. An electronic database search was conducted. The search included all articles up to July, 2021. The search was based on a strategic question using the relevant MeSH terms [“extraoral vibration”] AND [“dental”] AND [“child”]. Quantitative data were analyzed using RevMan software, and a random-effects model was applied to calculate the mean difference.
Only studies that combined extraoral vibratory devices and cold application during intraoral local anesthesia delivery in children were included. Observational data, reviews, and case reports were omitted from the analysis. Articles on oral vibratory devices were omitted. Title and abstract outlines were screened, and relevant articles were imported to citation software (www.zotero.org) from the selected databases. Duplicates were removed. Titles that met our criteria were included in the qualitative analysis. Information extraction and analysis were performed independently by two examiners. The outcome measure was “pain perception and reaction”. Means and standard deviations were collected from individual studies.
Data synthesis: Fixed-or random-effect models were used to analyze the pooled mean data. The significance level was set at five percent.
Risk of bias [ RoB ] assessment: RoB was assessed using the Cochrane criteria.
RESULTS
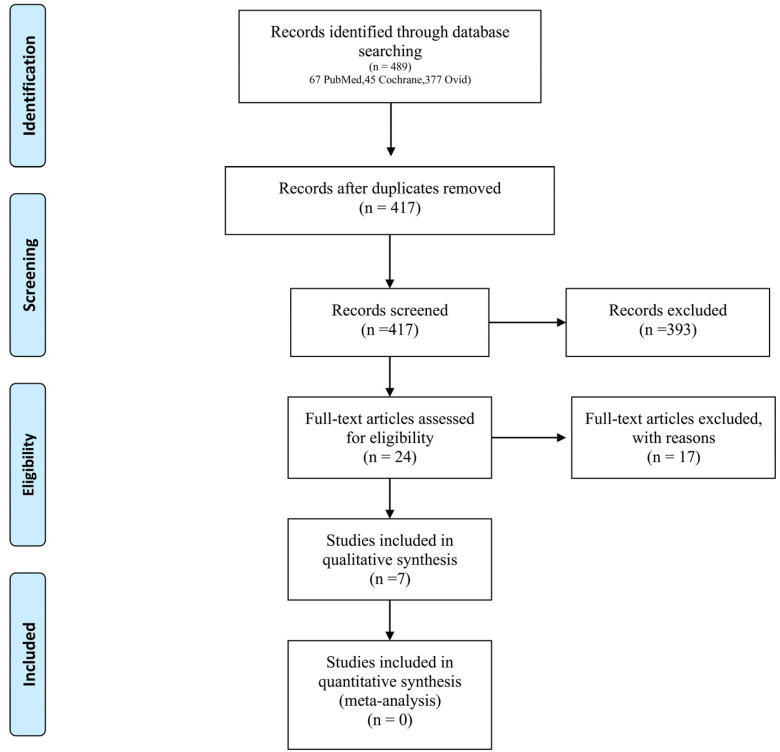
In the evaluated electronic databases, 489 articles were retrieved. Duplicates were excluded. A total of 417 articles were screened by the title and abstract. Of these, 24 articles were included for the full-text review. After the full-text analysis, 17 articles were excluded [13,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. The details of the excluded articles are listed in Table 1. Seven studies were included in the final analysis [31,32,33,34,35,36,37]. The search results are presented as a flowchart in Fig. 1.
Table 1. Table showing Excluded articles and reasons for exclusion.
| No | Excluded articles | Reasons for exclusion |
|---|---|---|
| 1. | Felemban, et al 2021 [20] | Intra-oral vibration was used |
| 2. | Menni, et al 2020 [22] | Intra-oral vibration was used |
| 3. | Salma, et al 2021 [25] | Intra-oral vibration was used and too in adults |
| 4. | Smorarek, et al 2020 [16] | Intra-oral vibration was used |
| 5. | Hassanein, et al 2020 [21] | Intra-oral vibration was used |
| 6. | Veneva, et al 2019 [30] | Intra-oral vibration was used |
| 7. | Tandon, et al 2018 [28] | Intra-oral vibration was used |
| 8. | Tung, et al 2018 [29] | Intra-oral vibration was used |
| 9. | Erdogan, et al 2018 [19] | Intra-oral vibration was used |
| 10. | Raslan, et al 2018 [24] | Intra-oral vibration was used |
| 11. | Shaefer, et al 2017 [26] | Intra-oral vibration was used |
| 12. | Bagherian, et al 2016 [13] | Intra-oral vibration was used |
| 13. | Shilpapriya, et al 2015 [27] | Intra-oral vibration was used |
| 14. | Elbay, et al 2015 [18] | Intra-oral vibration was used |
| 15. | Nasehi, et al 2015 [23] | Intra-oral vibration was used |
| 16. | Difelice, et al 2014 [17] | Intra-oral vibration was used |
| 17. | Ching, et al 2014 [15] | Intra-oral vibration was used |
Fig. 1. Flow chart.
Characteristics of the included studies: All published studies from 2018-2021 are shown in Table 2. Five of the seven studies followed a parallel-arm design [31,32,34,35,36], and two used the split-mouth design [33,37]. A total of 391 children, aged 4-12 years, received different dental injections, including infiltrations (both maxillary and mandibular) [34,36], maxillary infiltration alone [37], mandibular infiltration alone [32], infiltration and blocks [35], or inferior alveolar nerve block alone [33]. Extraoral vibration and precooling were compared with no extraoral vibration and no precooling in 5 studies [31,32,33,36,37]. Extraoral vibration and precooling were compared with counter stimulation in one study [34]. Only extraoral vibration was performed in one study [35]. Extraoral vibration and cooling were delivered using the BUZZY device in 5 studies [31,32,34,36,37]. A custom device was used to deliver vibration in two studies [33,35]. Pain perception was evaluated in six studies [31,32,34,36,37]. Of these, four studies used the The Wong Baker faces pain rating scale (WB-FPRS) alone [32,36,37], and one study used the Visual Analog Scale (VAS) only [31]. Furthermore, one study used both the WB-FPRS and VAS [34].
Table 2. Characteristics of the included studies.
| No | Author year | Study design | Sample characteristics | Type of injection | Gauge of manual syringe used | Topical anesthesia | Intervention characteristic and comparison groups | Vibration instrument | Measuring Scales | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Sahiti, et al 2021 [34] | Randomized parallel-arm, single blinded, interventional, clinical trial | 100 children, aged 4 to 11 years | Infiltration | 23 gauge needle | 20% benzocaine | 50 – Extra oral Vibration + Cooling 50 – Counter stimulation |
Buzzy Counter stimulation with gentle mucosal vibration |
WBFPRS VAS VPT VCARS |
Extra oral Vibration + Cooling better |
| 2. | AlHareky, et al. 2021 [31] | Randomized parallel-arm, interventional, clinical trial Parlell arm design. | 51 children, aged 5 to 12 years | Maxillary buccal infiltration | 30 gauge needle | 20% benzocaine | 25 – Extra oral Vibration + Cooling 26 – No Extra oral Vibration + Cooling |
Buzzy | VAS FLACC SEM |
Extra oral vibration + Cooling better |
| 3. | Subramaniam and ghai 2021 [35] | Randomized parallel-arm, interventional, clinical trial | 40 children, aged 4 to 8 years | Both infiltrations and blocks | 26 or 30 gauge needle | Not menctioned | 20 – Extra oral Vibration 20 – No Extra oral Vibration |
Custom device | SEM | Extra oral vibration better |
| 4. | Suohu, et al. 2020 [36] | Randomized parallel-arm, interventional, clinical trial | 50 children, aged 5 to 12 years | Infiltrations | Not menctioned | Not menctioned | 25 – Traditional syringe with Extra oral Vibration + Cooling 26 – Traditional syringe without Extra oral Vibration + Cooling |
Buzzy | WBFPRS FLACC |
Extra oral vibration + Cooling better |
| 5. | Bilsin, et al. 2019 [32] | Randomized parallel-arm, interventional, control trial | 60 children, aged 7 to 12 years | Mandibular infiltrations | 30 gauge needle | - | 30 – Extra oral Vibration + Cooling 30 – No Extra oral Vibration + Cooling |
Buzzy | WBFPRS | Extra oral vibration + Cooling better |
| 6. | Alanazi, 2018 [37] | Split mouth randomised crossover study | 60 children, aged 7 years | Maxillary infiltrations | 30 gauge needle | 20% benzocaine | 30 – Extra oral Vibration + Cooling 30 – No Extra oral Vibration + Cooling |
Buzzy | Heart rate WBFPS FLACC |
Extra oral vibration + Cooling better |
| 7. | Hegde, 2019 [33] | Randomized crossover, split-mouth, clinical study | 30 children, aged 6-11 years. | Bilateral inferior alveolar nerve block | Not menctioned | Not menctioned | 30 – Extra oral Vibration 30 – No Extra oral Vibration |
Custom device | Heart rate WBFPS FLACC |
Extra oral vibration better |
*Abbreviations used in this table: FLACC, face, legs, activity, cry, and consolability scale; G1, group 1; G2, group 2; G3, group 3; SEM scale, sound, eye, motor scale; VAS, visual analog scale; VCARS, Venham's clinical anxiety rating scale; VPT, Venham's picture test; WB-FPR Scale, The Wong Baker faces pain rating scale.
Pain reactions were evaluated in six studies [31,33,34,35,36,37]. The face, legs, activity, cry, and consolability scale (FLACC) and sound, eye, motor scale (SEM) were the most commonly used scales to measure pain reactions. Only FLACC was used in three studies [33,36,37]. Only SEM was used in one study [35]. Another study used both FLACC and SEM [31]. Moreover, heart rate was measured in two studies [33,37].
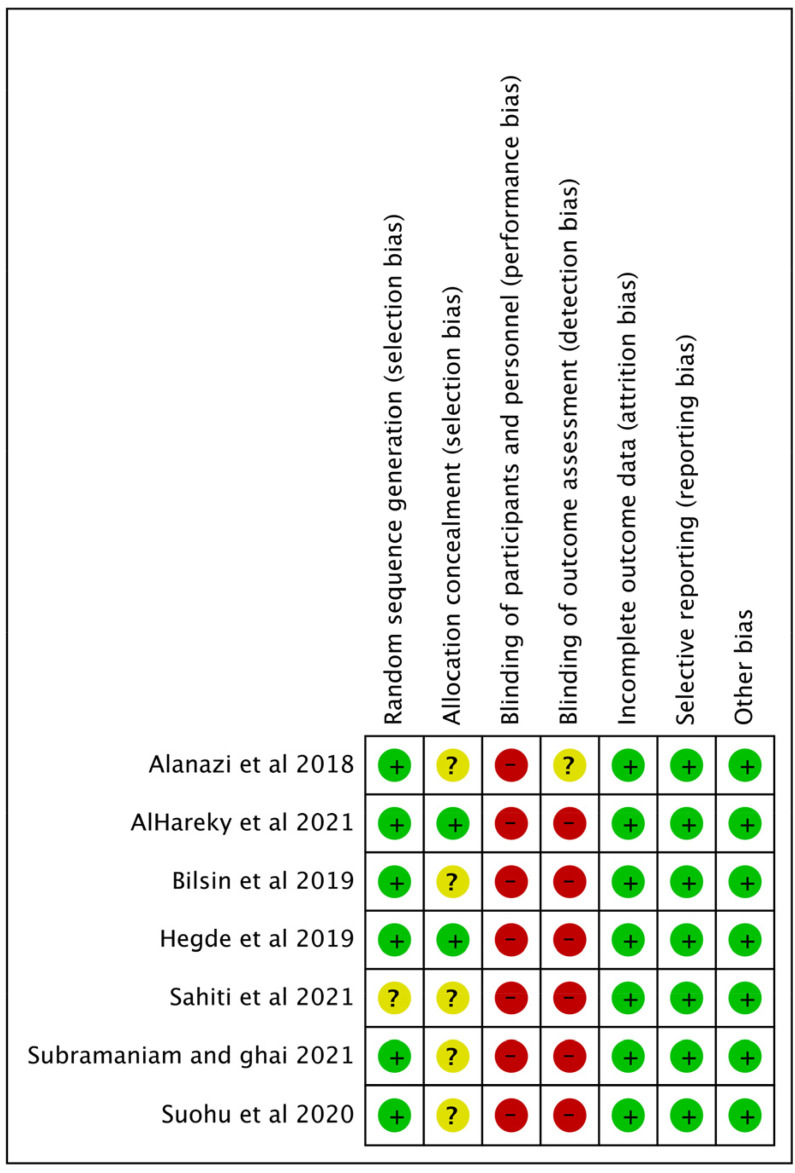
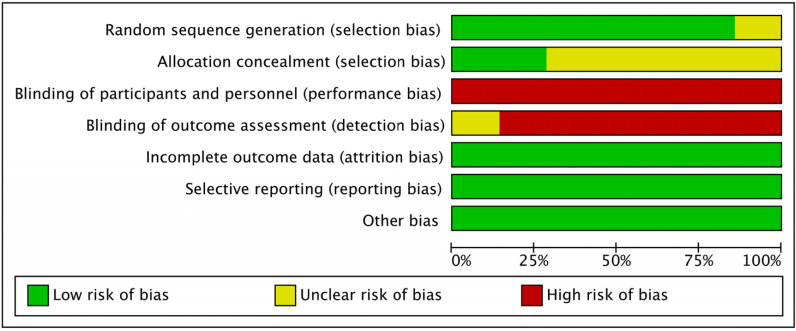
Risk of bias: Cochrane guidelines were followed to evaluate the risk of bias (Fig. 2 and Fig. 3). Randomization was performed in all included studies (n = 7) [31,32,33,34,35,36,37]. There was a single-blinded study [34]. In our opinion, blinding of participants is not feasible because the stimulation due to vibration can be perceived by children, and blinding of outcome assessment was not mentioned in any of the studies. All studies were free from other forms of bias.
Fig. 2. Risk of bias summary.
Fig. 3. Risk of bias graph.
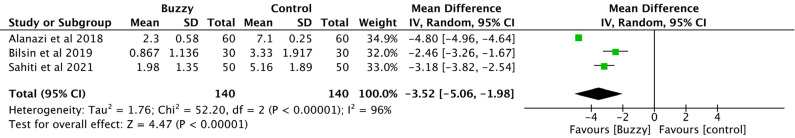
Effects of extraoral vibration and cooling on the primary outcome: Children’s perception of pain was evaluated in six studies [31,32,33,34,36,37]. Of these, four studies used the WB-FPS alone [32,33,36,37], and one study used the VAS only [31]. One study used both the WB-FPRS and VAS [34]. Considering all three studies, a significant decline in self-reported pain scores was reported with the use of extraoral vibration and precooling during local anesthesia administration with a mean difference of -3.52; 95% confidence interval [-5.06 -1.98] (Fig. 4).
Fig. 4. Pain perception (The Wong Baker FACES scale).
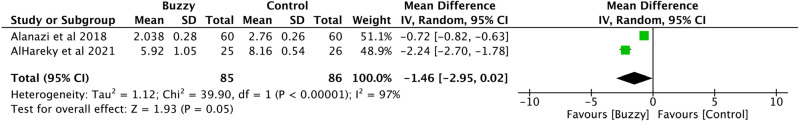
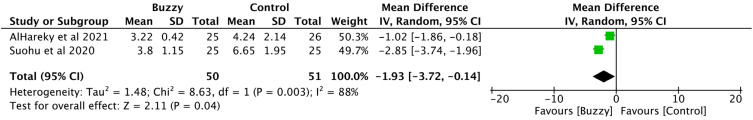
Effects of extraoral vibration and cooling on the secondary outcomes: Only a few studies reported pain reactions (objective pain, n = 6). FLACC was exclusively used in three studies [33,36,37]. SEM was used in one study [35]. Another study used both FLACC and SEM [31]. Few studies included a quantitative analysis. In the pooled mean results of two of the studies, a significant decline in pain reaction was reported with the use of extraoral vibration and precooling during local anesthesia administration, with a mean difference of -1.46; 95% confidence interval [-2.95 0.02], and SEM mean difference -1.93; 95% confidence interval [-3.72 -0.14] (Fig. 5 and Fig. 6).
Fig. 5. Pain reaction (Face, Legs, Activity, Cry, and Consolability Scale).
Fig. 6. Pain reaction (Sound, Eye, Motor scale).
DISCUSSION
Multiple modalities have been used to mitigate injection pain among children . Vibration is one such modality. The direct intraoral vibratory method has been proven to have a positive effect on pain reduction due to needle prick during intraoral injections [12]. This systematic review aimed to evaluate and quantify the effects of extraoral vibration and pre-cooling on pain reduction during local anesthesia administration in children.
Seven studies qualified for the final qualitative analysis. All studies were randomized controlled trials [31,32,33,34,35,36,37]. Five followed a parallel-arm design [31,32,34,35,36], and two used a split-mouth design [33,37]. Children in the qualified studies ranged in age, from 4 to 12 years.
The type of intraoral local anesthesia injections varied across the included studies, and included infiltration (both maxillary and mandibular) [34,36], maxillary infiltrations alone [37], mandibular infiltrations alone [32], infiltrations and blocks [35], and inferior alveolar nerve block alone [33]. The intervention groups used extraoral vibration with cooling [31,32,33,36,37], the control groups had no intervention [31,32,33,36,37], or use counter-stimulation [34]. Most of the studies used 26-or 30-gauge needles, apart from Sahiti et al. (2020). Sahiti et al. reported using 23-gauge needles [34]. The use of topical anesthesia (20% benzocaine) was reported in only two studies [31,34].
Child-reported pain scores for intraoral dental injections were assessed with and without extraoral vibration and cooling. Child-reported pain scores were assessed in six studies using the WB-FPRS scale. In these studies, self-reported pain scores were significantly lower in the extraoral vibration and cooling group than in the control group. In the pooled results of the three studies, a significant reduction in self-reported pain scores by the child was found to be associated with the use of extraoral vibration and precooling during local anesthesia administration mean difference -3.52; 95% confidence interval [-5.06 -1.98] (Fig. 4).
Pain reaction was evaluated in a few studies using FLACC and SEM [33,36,37]. In all the evaluated studies, the pain reaction was significantly lower in the extraoral vibration and cooling group than in the control group. In the pooled results of the two studies, a significant reduction in pain reaction by the child was found to be associated with the use of extraoral vibration and precooling during local anesthesia administration (FLACC, mean difference -1.46; 95% confidence interval [-2.95 0.02]; SEM mean difference -1.93; 95% confidence interval [-3.72 -0.14]) (Fig. 5 and Fig. 6).
Summary of evidence: Extraoral vibration plus cooling is a feasible and effective measure for pain reduction during local dental anesthesia administration in children. In comparison with the control group, significant differences were found in the pooled results of pain perception and reaction when combined extraoral vibration and cooling was used.
Limitations of the review: Blinding of participants is not feasible. In the included studies, extraoral vibration and cooling can be sensed by the children. The sources of extraoral vibration and cooling varied between the included studies. Combined extraoral vibration and cooling was delivered using BUZZY device in 5 studies [31,32,34,36,37] and a custom device was used to deliver vibration in two studies [33,35]. The location of intraoral local anesthesia administration was not the same in all studies. Few studies evaluated block injections, a few evaluated infiltrations alone, and other studies evaluated both infiltrations and blocks (both maxillary and mandibular) [34,36], maxillary infiltrations alone [37], mandibular infiltrations alone [32], infiltrations and blocks [35], and inferior alveolar nerve block alone [33]. Furthermore, only a few studies evaluated pain reactions [33,36,37].
Strengths of this study: Only studies reporting extraoral vibration plus cooling at the site of local anesthesia administration were assessed. To the best of our knowledge, this is the first systematic review to report an association between extraoral vibratory stimulus plus cooling, and pain perception during dental local anesthesia administration in children.
Directions for Future Research: 1. Future research should aim to optimize the magnitude of extraoral vibration for alleviating pain due to intraoral injections. 2. Studies on the effect of extraoral vibration plus cooling on the inferior alveolar nerve block exclusively, in children or adults, with adequate sample size, should be considered.
Conclusions: Based on the available results, the conclusions are as follows.
1. The use of extraoral vibration plus cooling as a counter-stimulatory measure is effective in reducing the pain perceived by children during intraoral local anesthesia administration.
2. The risk of bias was high in most of the studies. Therefore, the quality of evidence was considered low.
Footnotes
- Sunnypriyatham Tirupathi: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
- Neethu Nanda: Writing – review & editing.
- Sneha Pallepagu: Writing – review & editing.
- Sardhar Malothu: Writing – review & editing.
- Nilesh Rathi: Writing – review & editing.
- Rashmi singh Chauhan: Writing – review & editing.
- VakaJeevan Priyanka: Writing – review & editing.
- Rameshreddy Basireddy: Writing – review & editing.
FUNDING: The authors have no financial support or sponsorship to declare.
DECLARATION OF INTEREST: There are no conflicts of interest to declare.
References
- 1.Orenius T, LicPsych, Säilä H, Mikola K, Ristolainen L. Fear of injections and needle phobia among children and adolescents: an overview of psychological, behavioral, and contextual factors. SAGE Open Nurs. 2018;4:2377960818759442. doi: 10.1177/2377960818759442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee HS. Recent advances in topical anesthesia. J Dent Anesth Pain Med. 2016;16:237–244. doi: 10.17245/jdapm.2016.16.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peretz B, Gluck GM. Assessing an active distracting technique for local anesthetic injection in pediatric dental patients: repeated deep breathing and blowing out air. J Clin Pediatr Dent. 1999;24:5–8. [PubMed] [Google Scholar]
- 4.Kamath PS. A novel distraction technique for pain management during local anesthesia administration in pediatric patients. J Clin Pediatr Dent. 2013;38:45–47. doi: 10.17796/jcpd.38.1.265807t236570hx7. [DOI] [PubMed] [Google Scholar]
- 5.Tirupathi S, Krishna N, Rajasekhar S, Nuvvula S. Eye movement distraction: a new distraction technique for management of dental anxiety during intraoral local anesthesia administration in children. Int J Clin Pediatr Dent. 2019;12:507–509. doi: 10.5005/jp-journals-10005-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Custódio NB, Costa FDS, Cademartori MG, da Costa VPP, Goettems ML. Effectiveness of virtual reality glasses as a distraction for children during dental care. Pediatr Dent. 2020;42:93–102. [PubMed] [Google Scholar]
- 7.Monteiro J, Tanday A, Ashley PF, Parekh S, Alamri H. Interventions for increasing acceptance of local anaesthetic in children and adolescents having dental treatment. Cochrane Database Syst Rev. 2020;2:Cd011024. doi: 10.1002/14651858.CD011024.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tirupathi SP, Rajasekhar S. Effect of precooling on pain during local anesthesia administration in children: a systematic review. J Dent Anesth Pain Med. 2020;20:119–127. doi: 10.17245/jdapm.2020.20.3.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tirupathi SP, Rajasekhar S. Effect of warming local anesthesia solutions before intraoral administration in dentistry: a systematic review. J Dent Anesth Pain Med. 2020;20:187–194. doi: 10.17245/jdapm.2020.20.4.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tirupathi SP, Rajasekhar S. Buffered versus unbuffered local anesthesia for inferior alveolar nerve block injections in children: a systematic review. J Dent Anesth Pain Med. 2020;20:271–279. doi: 10.17245/jdapm.2020.20.5.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melwani AM, Srinivasan I, Setty JV, D R MK, Pamnani SS, Lalitya D. A clinical comparative study between conventional and camouflaged syringes to evaluate behavior and anxiety in 6-11-year-old children during local anesthesia administration-a novel approach. J Dent Anesth Pain Med. 2018;18:35–40. doi: 10.17245/jdapm.2018.18.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tirupathi SP, Rajasekhar S. The effect of vibratory stimulus on pain perception during intraoral local anesthesia administration in children: a systematic review and meta-analysis. J Dent Anesth Pain Med. 2020;20:357–365. doi: 10.17245/jdapm.2020.20.6.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bagherian A, Sheikhfathollahi M. Children's behavioral pain reactions during local anesthetic injection using cotton-roll vibration method compared with routine topical anesthesia: a randomized controlled trial. Dent Res J. 2016;13:272–277. doi: 10.4103/1735-3327.182189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shahidi Bonjar AH. Syringe micro vibrator [SMV]. a new device being introduced in dentistry to alleviate pain and anxiety of intraoral injections, and a comparative study with a similar device. Ann Surg Innov Res. 2011;5:1. doi: 10.1186/1750-1164-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ching D, Finkelman M, Loo CY. Effect of the DentalVibe injection system on pain during local anesthesia injections in adolescent patients. Pediatr Dent. 2014;36:51–55. [PubMed] [Google Scholar]
- 16.de Camargo Smolarek P, da Silva LS, Martins PRD, da Cruz Hartman K, Bortoluzzi MC, Chibinski ACR. The influence of distinct techniques of local dental anesthesia in 9- to 12-year-old children: randomized clinical trial on pain and anxiety. Clin Oral Investig. 2021;25:3831–3843. doi: 10.1007/s00784-020-03713-7. [DOI] [PubMed] [Google Scholar]
- 17.DiFelice MG, Vandewalle KS, Maller SC, Hancock RH. Effects of a vibratory device on pain from anesthetic injections. Compend Contin Educ Dent. 2014;35:246, 248. 50-1 passim. [PubMed] [Google Scholar]
- 18.Elbay M, Şermet Elbay Ü, Yıldırım S, Uğurluel C, Kaya C, Baydemir C. Comparison of injection pain caused by the DentalVibe Injection System versus a traditional syringe for inferior alveolar nerve block anaesthesia in paediatric patients. Eur J Paediatr Dent. 2015;16:123–128. [PubMed] [Google Scholar]
- 19.Erdogan O, Sinsawat A, Pawa S, Rintanalert D, Vuddhakanok S. Utility of vibratory stimulation for reducing intraoral injection pain. Anesth Prog. 2018;65:95–99. doi: 10.2344/anpr-65-02-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Felemban O, Oghli AR, Alsaati I, Alattas LK, Olwi AM, Bagher SM. The effect of DentalVibe on pain and discomfort during local anesthesia in children: a randomized clinical trial. Quintessence Int. 2021:434–443. doi: 10.3290/j.qi.b912695. [DOI] [PubMed] [Google Scholar]
- 21.Hassanein PH, Khalil A, Talaat DM. Pain assessment during mandibular nerve block injection with the aid of dental vibe tool in pediatric dental patients: a randomized clinical trial. Quintessence Int. 2020;51:310–317. doi: 10.3290/j.qi.a44145. [DOI] [PubMed] [Google Scholar]
- 22.Menni AC, Radhakrishna AN, Prasad MG. DentalVibe® versus lignocaine hydrochloride 2% gel in pain reduction during inferior alveolar nerve block in children. J Dent Anesth Pain Med. 2020;20:397–402. doi: 10.17245/jdapm.2020.20.6.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nasehi A, Bhardwaj S, Kamath AT, Gadicherla S, Pentapati KC. Clinical pain evaluation with intraoral vibration device during local anesthetic injections. J Clin Exp Dent. 2015;7:e23–e27. doi: 10.4317/jced.51643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raslan N, Masri R. A randomized clinical trial to compare pain levels during three types of oral anesthetic injections and the effect of Dentalvibe®. on injection pain in children. Int J Paediatr Dent. 2018;28:102–110. doi: 10.1111/ipd.12313. [DOI] [PubMed] [Google Scholar]
- 25.Salma RG, Alsayeh A, Maneea AB, Alrassan F, Almarshad A. The effectiveness of electronic pulsed soft tissue vibration compared with topical anaesthesia in reducing the pain of injection of local anaesthetics in adults: a randomized controlled split-mouth clinical trial. Int J Oral Maxillofac Surg. 2021;50:407–415. doi: 10.1016/j.ijom.2020.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Shaefer JR, Lee SJ, Anderson NK. A vibration device to control injection discomfort. Compend Contin Educ Dent. 2017;38:e5–e8. [PubMed] [Google Scholar]
- 27.Shilpapriya M, Jayanthi M, Reddy VN, Sakthivel R, Selvaraju G, Vijayakumar P. Effectiveness of new vibration delivery system on pain associated with injection of local anesthesia in children. J Indian Soc Pedod Prev Dent. 2015;33:173–176. doi: 10.4103/0970-4388.160343. [DOI] [PubMed] [Google Scholar]
- 28.Tandon S, Kalia G, Sharma M, Mathur R, Rathore K, Gandhi M. Comparative Evaluation of Mucosal Vibrator with topical anesthetic gel to reduce pain during administration of local anesthesia in pediatric patients: an in vivo study. Int J Clin Pediatr Dent. 2018;11:261–265. doi: 10.5005/jp-journals-10005-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tung J, Carillo C, Udin R, Wilson M, Tanbonliong T. Clinical performance of the dentalVibe® injection system on pain perception during local anesthesia in children. J Dent Child. 2018;85:51–57. [PubMed] [Google Scholar]
- 30.Veneva E, Cholakova R, Raycheva R, Belcheva A. Efficacy of vibrotactile device DentalVibe in reducing injection pain and anxiety during local anaesthesia in paediatric dental patients: a study protocol for a randomised controlled clinical trial. BMJ Open. 2019;9:e029460. doi: 10.1136/bmjopen-2019-029460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.AlHareky M, AlHumaid J, Bedi S, El Tantawi M, AlGahtani M, AlYousef Y. Effect of a vibration system on pain reduction during injection of dental anesthesia in children: randomized clinical trial. Int J Dent. 2021;2021:8896408. doi: 10.1155/2021/8896408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bilsin E, Güngörmüş Z, Güngörmüş M. The Effıcacy of External cooling and vibration on decreasing the pain of local anesthesia injections during dental treatment in children: a randomized controlled study. J Perianesth Nurs. 2020;35:44–47. doi: 10.1016/j.jopan.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Hegde KM, R N, Srinivasan I, D R MK, Melwani A, Radhakrishna S. Effect of vibration during local anesthesia administration on pain, anxiety, and behavior of pediatric patients aged 6-11 years: a crossover split-mouth study. J Dent Anesth Pain Med. 2019;19:143–149. doi: 10.17245/jdapm.2019.19.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sahithi V, Saikiran KV, Nunna M, Elicherla SR, Challa RR, Nuvvula S. Comparative evaluation of efficacy of external vibrating device and counterstimulation on child's dental anxiety and pain perception during local anesthetic administration: a clinical trial. J Dent Anesth Pain Med. 2021;21:345–355. doi: 10.17245/jdapm.2021.21.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Subramaniam P, Ghai SK. Efficacy of an innovative device in reducing discomfort during local anesthesia administration in children: a clinical study. Int J Clin Pediatr Dent. 2021;14:353–356. doi: 10.5005/jp-journals-10005-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suohu T, Sharma S, Marwah N, Mishra P. A comparative evaluation of pain perception and comfort of a patient using conventional syringe and buzzy system. Int J Clin Pediatr Dent. 2020;13:27–30. doi: 10.5005/jp-journals-10005-1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alanazi KJ, Pani S, AlGhanim N. Efficacy of external cold and a vibrating device in reducing discomfort of dental injections in children: a split mouth randomised crossover study. Eur Arch Paediatr Dent. 2019;20:79–84. doi: 10.1007/s40368-018-0399-8. [DOI] [PubMed] [Google Scholar]