Dear Editor,
We present the first Chinese case of poppers maculopathy. Poppers are a recreational substance of abuse which composes of a series of volatile alkyl nitrite. “Rush” is a kind of poppers, which was born in the United States and has been in existence for more than 30y. Inhalation of poppers provides a brief rush of euphoria, sexual arousal and relaxation of smooth muscles including the anal sphincter. There are approximate 20% male homosexual using poppers to enhance sexual pleasure in our country.
It is previously considered that the risk of poppers is low both physically and psychologically. However, a global drug survey showed that 12% respondents who were using or had used poppers believed that the use of poppers may have or definitely affected their eyesight[1]. Here we present, to our knowledge, the first reported case of poppers maculopathy in China. We obtained the written informed consent from the patient.
A 37-year-old Chinese man presented with blurred vision and central scotoma in both eyes for 7d. He admitted to regular use (at least twice or 3 times per month) rush poppers for the previous 7y. After inhaling the rush poppers, he had multiple transient blurred visions, and the symptom did not disappear since his last inhalation of rush poppers 7d ago. He did not smoke or drink and had no significant past medical, ophthalmic or family history. Slit-lamp examination was unremarkable, with normal fundus (Figure 1). Best-corrected visual acuity (BCVA) was 0.7 in the right eye and 0.5 in the left. His pupil reactions and color vision (Farnsworth D-15 test) were normal. Optical coherence tomography (OCT) revealed disruption of the ellipsoid zone confined to the fovea in both eyes (Figure 2A). Full-field electroretinography (ERG) showed normal. Multifocal electroretinography (mfERG) showed amplitude reduced at macular fovea of both eyes (Figure 3A). Visual field testing showed normal on the 5th day of the onset, while there was central scotoma of the left eye on the 17th day, the other eye was normal (Humphrey 24-2; Figure 4A).
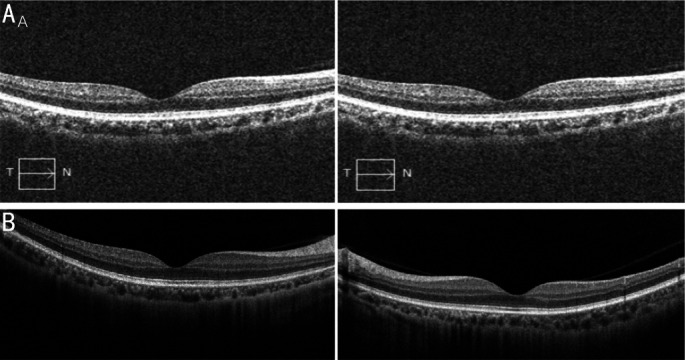
Figure 1. Fundus photography is generally normal.
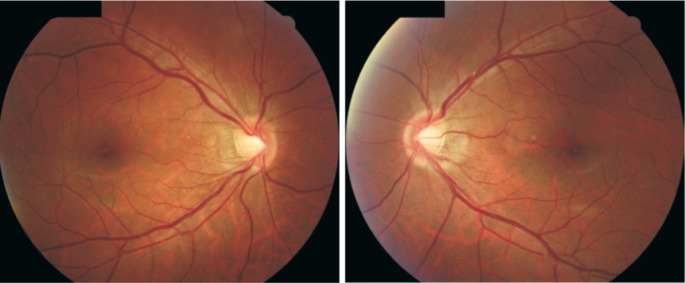
Figure 2. OCT scan of fovea.
A: 5d of the last inhalation of poppers, disruption of the foveal ellipsoid zone bilaterally; B: 2mo after the last inhalation of poppers, symptoms gradually improved and ellipsoid zone disruption returned to normal.
Figure 3. Multifocal electroretinography.
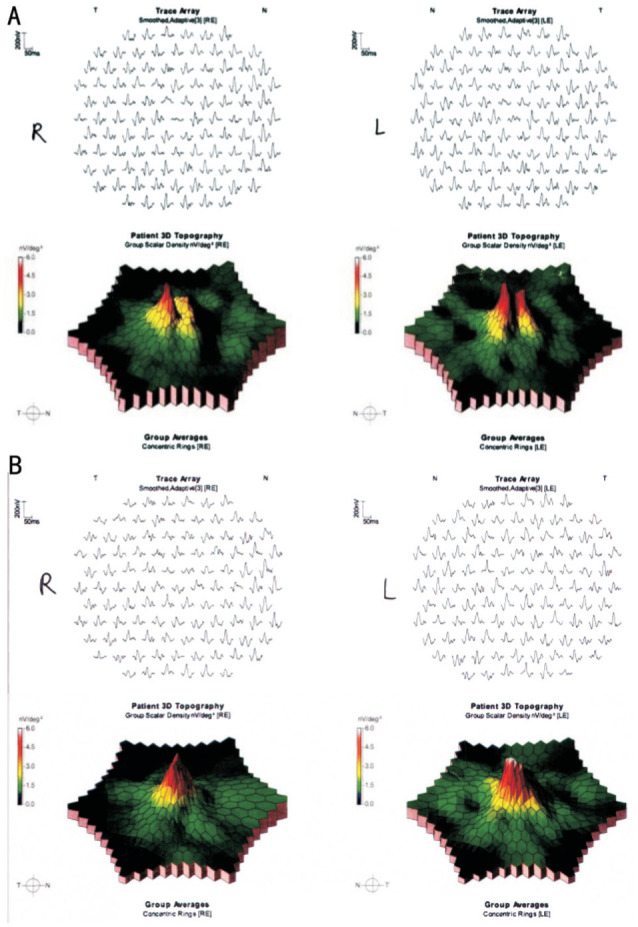
A: The three-dimensional topography of mfERG demonstrates a subnormal central region and the ERG traces of fovea were low; B: mfERG amplitudes were improved 2mo after poppers cessation for both central responses, obviously in the right eye.
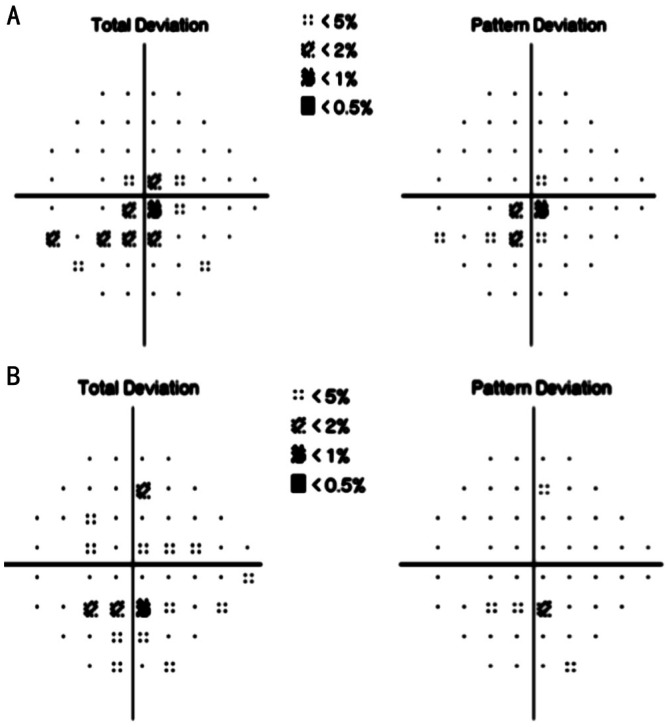
Figure 4. Visual field (Humphrey 24-2).
A: Left central scotoma can be seen on the 17th day of onset; B: Left central scotoma almost disappeared 2mo later.
The patient was advised to stop drug inhalation. With 2mo follow-up, the patient complained that the scotoma was disappeared. At the same time, his BCVA improved to 1.0 in the right eye and 0.8 in the left. OCT showed the photoreceptor layer of both eyes was return to normal (Figure 2B). mfERG showed improvement in both central regions, especially in the right eye (Figure 3B). The central scotoma on the left visual field was disappeared (Figure 4B).
To our knowledge, nitric oxide (NO) regulates photoreceptor metabolism in rods and cones primarily through activation of guanylate cyclase, a key enzyme of phototransduction. It is widely suspected that the potential cause of retinal damage linked to inhalation of poppers is high concentration of NO. Experimental studies showed that high doses of NO induce apoptotic cell death in photoreceptors[2]. There is another hypothesis that poppers cause rapid widespread dilation of blood vessels, as well as blood vessels in the eye, which causes an increase in intraocular pressure and damage to retina.
After poppers inhalation, patients present with similar symptoms such as blurred vision, fluctuating vision, central scotoma, photophobia, and phosphenes, and most of them have both eyes suffered. The fundus manifestations are varied, which can be normal, yellowish-white spots, or even vitelliform lesions at the fovea. OCT provides the most valuable diagnostic test, showing disruption or attenuation of the ellipsoid zone in both foveae. All patients with pathognomonic changes on OCT imaging should be asked about inhalation of poppers.
mfERG is also a useful tool for detecting the location and extent of retinal dysfunction, particularly in the diagnosis of retinal toxicity confined to the central retina. In some drug-reduced retinopathies, such as chloroquine and hydroxychloroquine, mfERG is considered an objective examination of retinal function that can provide earlier detection of retinal damage[3]. As a case reported that OCT abnormality appeared 3mo later than visual symptoms and acuity loss following poppers inhalation[4], mfERG can be a significant method for early screening of poppers retinal toxicity and monitoring of disease progression or recovery after drug cessation.
Some other ancillary testings should be considered, such as visual field examination that central or paracentral scotomas are possibly seen with normal peripheral fields, but these abnormalities may not appear in the early stage of the disease. Color vision examination is also helpful to distinguish macular diseases from optic nerve diseases.
Clinical features and ellipsoid zone disruption on OCT of poppers macular lesions are similar to photic injury, the two conditions can only be reliably distinguished by the history of excess light[5]. Therefore, it is crucial to document the relevant drug history and light exposure. Adult-onset occult macular dystrophy should be another differential diagnosis as the normal fundus and similar structural changes in the ellipsoid zone, but the patients with occult macular dystrophy usually have progressive decrease of visual acuity and red-green color defect[6]. If the patient has yolk-like lesions at the fovea, it needs to be differentiated from best vitelliform macular dystrophy.
The prognosis of poppers maculopathy is variable. When they ceased using poppers, most patients may achieve complete or partial resolution[1], while others experience no improvement. The final results may be related to the duration, frequency and type of drug inhalation.
Acknowledgments
Conflicts of Interest: Guo ST, None; Jiang LB, None.
REFERENCES
- 1.Davies AJ, Borschmann R, Kelly SP, Ramsey J, Ferris J, Winstock AR. The prevalence of visual symptoms in poppers users: a global survey. BMJ Open Ophthalmol. 2017;1(1):e000015. doi: 10.1136/bmjophth-2016-000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clemens CR, Alten F, Loos D, Uhlig CE, Heiduschka P, Eter N. Poppers maculopathy or retinopathy? Eye (Lond) 2015;29(1):148–149. doi: 10.1038/eye.2014.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dettoraki M, Moschos MM. The role of multifocal electroretinography in the assessment of drug-induced retinopathy: a review of the literature. Ophthalmic Res. 2016;56(4):169–177. doi: 10.1159/000446321. [DOI] [PubMed] [Google Scholar]
- 4.Davies AJ, Kelly SP, Naylor SG, Bhatt PR, Mathews JP, Sahni J, Haslett R, McKibbin M. Adverse ophthalmic reaction in poppers users: case series of ‘poppers maculopathy’. Eye (Lond) 2012;26(11):1479–1486. doi: 10.1038/eye.2012.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luis J, Virdi M, Nabili S. Poppers retinopathy. BMJ Case Rep. 2016;2016:bcr2016214442. doi: 10.1136/bcr-2016-214442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsang SH, Sharma T. Occult macular dystrophy. Adv Exp Med Biol. 2018;1085:103–104. doi: 10.1007/978-3-319-95046-4_19. [DOI] [PubMed] [Google Scholar]